ABSTRACT
Military activities in hot environments pose 2 competing demands: the requirement to perform realistic training to develop operational capability with the necessity to protect armed forces personnel against heat-related illness. To ascertain whether work duration limits for protection against heat-related illness restrict military activities, this study examined the heat strain and risks of heat-related illness when conducting a military activity above the prescribed work duration limits. Thirty-seven soldiers conducted a march (10 km; ∼5.5 km h−1) carrying 41.8 ± 3.6 kg of equipment in 23.1 ± 1.8°C wet-bulb globe temperature. Body core temperature was recorded throughout and upon completion, or withdrawal, participants rated their severity of heat-related symptoms. Twenty-three soldiers completed the march in 107 ± 6.4 min (Completers); 9 were symptomatic for heat exhaustion, withdrawing after 71.6 ± 10.1 min (Symptomatic); and five were removed for body core temperature above 39.0°C (Hyperthermic) after 58.4 ± 4.5 min. Body core temperature was significantly higher in the Hyperthermic (39.03 ± 0.26°C), than Symptomatic (38.34 ± 0.44°C; P = 0.007) and Completers (37.94 ± 0.37°C; P<0.001) after 50 min. Heat-related symptom severity was significantly higher among Symptomatic (28.4 ± 11.8) compared to Completers (15.0 ± 9.8, P = 0.006) and Hyperthermic (13.0 ± 9.6, P = 0.029). The force protection provided by work duration limits may be preventing the majority of personnel from conducting activities in hot environments, thereby constraining a commander's mandate to develop an optimised military force. The dissociation between heat-related symptoms and body core temperature elevation suggests that the physiological mechanisms underpinning exhaustion during exertional heat stress should be re-examined to determine the most appropriate physiological criteria for prescribing work duration limits.
KEYWORDS: armed forces, body core temperature, exertional heat stress, heat strain, heat-related illness, military, work table
Introduction
The effects of heat exposure on the human body can have disastrous consequences for the unsuspecting and unprepared individual. The physiological strain associated with work in the heat can cause symptoms of heat exhaustion including fatigue, weakness, dizziness, confusion, and fainting; consequently personnel become incapacitated by heat exhaustion and require a period of recovery before returning to work.1 In more severe cases, an excessive elevation in the core temperature of the body impairs central nervous system function and causes body tissue damage, with many cases being fatal.2,3 Countless stories of military endeavors have ended with significant impairment of an individual's ability to work in conditions of high heat stress.4,5 Therefore, preventing these heat-related illnesses is not only crucial to the health of the individual but also in maintaining the operational capability of the armed forces in hot environments.
To protect armed forces personnel against heat-related illnesses (force protection), military training activities are often conducted in accordance with a Work Table.6 A Work Table is a risk management tool that sets limits to the duration of work periods dependant on the environmental conditions (Wet-Bulb Globe Temperature; WBGT), work intensity, and protective clothing worn by personnel.7,8 Work duration limits are based on biophysical modeling 9,10 of the rate of elevation in body core temperature during a period of work and are aligned with evidence-based assumptions of the risk of heat-related illness corresponding to this level of body core temperature elevation. Specifically, current work duration limits implemented by the Australian Army assume an elevation in body core temperature of 1.5°C, from 37.0–38.5°C. This physiological limit originates from the accumulation of heat strain during exercise at fixed work-rates,11-13 volitional exhaustion was observed to rarely occur below a body core temperature of 38.0°C, but termination always transpired prior to 40°C, with approximately 20% of these personnel becoming exhausted at 38.5°C.11-13 In addition, this criterion also aims to minimise the likelihood of any soldier experiencing an excessive elevation in body core temperature. When the body core temperature of an average soldier reaches 38.5°C, normal inter-individual variation of ± 0.2–0.4°C14-16 would result in the majority of individuals reaching a body core temperature in the range of 38.0–39.0°C, with only a small proportion of personnel rising above 39.0°C. Therefore, these limits minimise both the risk of heat exhaustion and help to prevent any soldier experiencing an excessive elevation in body core temperature.
In contrast to these physiological criteria underpinning the Work Table limits, recent evidence has shown that body core temperature in excess of 39.0°C during exertional heat stress is tolerable without sequelae, morbidity, or mortality.17-19 This was demonstrated by 18 military personnel who performed a 25-km march carrying 26 kg of equipment, taking on average 4 h 17 min including self-selected rest periods.18 In conditions that were in excess of the WBGT and work duration limits of Australia's Work Table guidance, peak body core temperature was 39.0 ± 0.9°C throughout the march, with the highest recorded at 40.3°C, and yet there were no symptoms of heat exhaustion reported with all participants completeing the march successfully. Similarly, soldiers completing a 21-km road race (unloaded) in 107 ± 9 min recorded peak body core temperature of 39.8 ± 0.5°C, with an individual as high as 40.7°C.19 Again, in-spite of the conditions being in excess of Australia's Work Table limits, all participants were asymptomatic for heat exhaustion and heat stroke.
The potential for personnel to tolerate work beyond the Work Table limits has raised concerns that the limits may be unnecessarily restrictive. While the Work Table provides an important framework for managing the risks of heat-related illnesses, the limitation to the duration of work periods may also lead to decreased operational capability if training activities are prohibited. For example, a primary requirement of Australian Army personnel is to perform a forced-march while carrying heavy loads of military equipment. Combat Arms personnel must be able to complete a 10-km forced-march carrying 40 kg in less than 1 h 50 min to pass their minimum performance standards. Examining the parameters of this activity shows that for it to be conducted in accordance with the Work Table the environmental conditions must be below 22°C WBGT. However, an evaluation of the meteorological data over the past decade at training locations in Australia (Australian Bureau of Meteorology) revealed that the environmental conditions were rarely below this level throughout the year. Consequently, performance of forced-march assessments would be restricted to only certain months of the year. It was clear from these observations that the Work Table poses considerable limitations to the conduct of military training activities and creates a dilemma for achieving a balance between force protection and operational capability in the Australian environment. Anecdotally, many commanders report that the Work Table prevents soldiers from effectively training in the heat, and as a result there is concern that they will not be appropriately physically and mentally acclimatised for operational activities, leaving them unprepared for deployment to conflict zones in hot environments where Work Table guidance cannot be strictly enforced. Therefore, it has been proposed that the Work Table is too conservative for the Australian context and attention has been directed to determining if the limits could be raised without substantively elevating the risk of heat-related illness. Therefore, the aim of this study was to examine the heat strain and risk of heat-related illness to personnel conducting a routine military training activity above the prescribed limits of the Work Table.
Methods
Thirty-seven male Royal Australian Infantry soldiers (body mass: 81.2 ± 9.9 kg; height: 180.0 ± 6.0 cm) volunteered to participate in this study. The participants were informed of the requirements of the trial and had the opportunity to raise any questions or concerns before providing written consent to participate. The Australian Defense Force Human Research Ethics Committee approved the measures and procedures used in this study.
Baseline measures of body stature, body composition and aerobic capacity were recorded for all participants within the 4 d prior to commencing the trial. Body composition (skeletal muscle mass: 40.6 ± 4.7 kg; fat mass: 10.5 ± 4.4 kg) was measured by whole-body Bio-electrical Impedance Analysis (InBody 230, BioSpace, USA). Participants performed the Bio-electrical Impedance Analysis assessment in temperate conditions (˜23°C) during the morning in a well-rested state; having completed no prior exercise that day. Wearing only underwear, participants stood on the scales with their bare feet touching the electrode plates. Participants grasped the hand electrodes and were instructed to remain standing still for the duration of the measurement, approximately 30 s. Individualised height and age data were entered into the system, which measured body mass and estimated skeletal muscle mass and total body fat mass. Maximal aerobic power (VO2max) was 48.7 ± 4.5 mL kg−1 min−1, estimated through a maximal effort on the 20-m shuttle run test.20 Participants wore t-shirt, shorts and athletic shoes for the test, which was performed on a flat and hard surface. Running between 2 markers spaced 20 m apart, participants progressively increased their speed in-time with an audio cue. The test was completed when the participant could no longer keep up with the timing requirement. Heart rate was measured (Polar Team 2, Polar Electro Inc., NY, USA) at rest before the test and maximal heart rate was recorded at the final completed stage of the test.
Participants performed a forced march of up to 10 km, commencing in a rested thermoneutral state at 5:30 am, wearing a combat uniform (including t-shirt, long-sleeve camouflage shirt and trousers, socks, and boots). The insulation and evaporative resistance of the clothing system were 0.212°C·m2/W and 0.031 kPa·m2/W respectively, measured in accordance with standards of the American Society for Testing and Materials.21,22 Participants carried 41.8 ± 3.6 kg of military equipment including a pack and weapon for the duration of the forced march, measured immediately prior to commencing the march. The march was conducted over a flat surface and paced at approximately 5.5 km h−1 with timing feedback given every 2.5 km. Although participants commenced the march in groups, separated by 5-min intervals, their effort was individually paced, as they were not required to remain in their group formation. The work rate of this activity for the average participant of 81 kg body mass was predicted to be approximately 600 Watts.23
Physiological strain including body core temperature and heart rate were monitored during the march (Equivital EQ02, Hidalgo, UK). Participants were fitted with a correctly sized chest harness dependant on their chest circumference. The harness housed a data logger on the chest under the left arm for recording body core temperature (1-min intervals) and heart rate (5-s intervals) throughout the forced march. Participants ingested a temperature sensor (Jonah, Minimitter, USA) at least 7 hours prior to starting the march. Heart rate data were not always reliable due to technical difficulties with the equipment. Consequently all heart rate data was visually inspected and data discarded if the values were too high or too low to be physiologically plausible. If this process removed more than 50% of a given participants data then that participant was excluded from heart rate analysis. Of those participants for whom the data was deemed acceptable (n = 18) the heart rate recorded in the final 10 min of the march, and the corresponding heart rate reserve, were utilised in the analysis.
The environmental conditions were recorded at 10-min intervals throughout the march (QT34, Quest Technologies, USA). The mean dry-bulb, wet-bulb, and black globe temperatures were 24.2 ± 1.6°C, 21.9 ± 0.9°C, and 27.3 ± 5.4°C respectively. The WBGT rose through the range of 20.8–26.2°C, averaging 23.1 ± 1.8°C over the course of the march. The Work Table stipulates duration limits of 180 min, 100 min, or 75 min in the WBGT ranges of 21–22°C, 23–24°C, and 25–26°C respectively. Since the forced march was paced to be completed in approximately 110 min, the highest WBGT the Work Table would recommend for this activity was 22°C. Since the environmental conditions rose above this limit, it was anticipated that the heat strain of participants may be slightly higher than the physiological assumptions underpinning the Work Table, resulting in a proportion of personnel either experiencing symptoms of heat-related illness or a high body core temperature.
At the completion of the forced march participants rated the severity of environmental symptoms pertinent to work in the heat.24 This questionnaire lists 22 symptoms that are associated with the experience of heat-related illnesses and required participants to rate the severity on a 6-point scale from 0–5, with the ratings ranging from: “not at all,” “slight,” “somewhat,” “moderate,” “quite a bit,” to “extreme.” The rating for each symptom was aggregated to provide a single index of symptoms rating for each participant. The sum of the ratings provides an indication of the overall perception of the effects of heat strain on health and performance, with higher ratings indicating greater impairment.
For the safety of participants, body core temperature was checked every 2.5 km and if found to be above 39.0°C the individual was removed from the forced-march. Also, individuals were eliminated from the forced march if they exhibited signs and symptoms of heat illness and were identified by, or presented themselves to, the military physical training instructors on the course. In either case of a high body core temperature or signs and symptoms these participants were then required to take-off any external load and clothing and rest in the shade. These precautions were in place to ensure that no participants experienced a heat-related injury during the trial. It also allowed the determination of the proportion of participants who reached this level of heat strain within the time-frame stipulated by the Work Table.
Participants were grouped according to their forced march outcomes, these were; Hyperthermic - participants who were removed from the march for reaching a body core temperature above 39.0°C, Symptomatic - those experiencing signs and symptoms of heat illness during the force march and, Completers - those who completed the march. A one-way analysis of variance was used to test for differences between the groups. When a significant main effect was found, Tukey's post-hoc test was performed to determine the location of group differences. Pearson correlation was used to describe the relationship between body core temperature response and heat-related symptoms. Data are reported as mean and standard deviation unless otherwise stated, with statistical significance accepted at P < 0.05.
Results
Despite each outcome group commencing the march with a similar resting body core temperature (Completers: 37.29 ± 0.22°C; Symptomatic: 37.45 ± 0.28°C; Hyperthermic: 37.43 ± 0.34°C; P = 0.226), march duration varied considerably. Twenty-three (62%) participants completed the march in 107 ± 6.4 min, working for significantly longer than 9 (24%) participants who withdrew due to heat-related signs and symptoms after 71.6 ± 10.1 min (P = 0.000), and 5 (14%) Hyperthermic participants who were removed after 58.4 ± 4.5 min (P = 0.000). The Symptomatic group also working significantly longer than the Hyperthermic (P = 0.008). All participants returned to normal physiological limits upon rest and fluid replenishment.
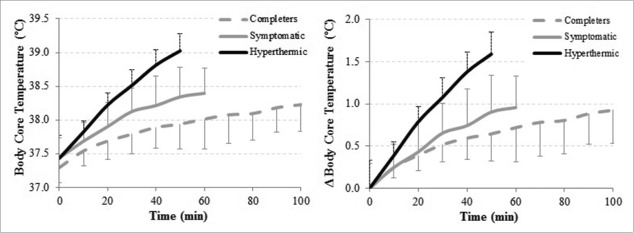
After the first 50 min and prior to any participants withdrawing from the march (Fig. 1), the Hyperthermic group had the greatest body core temperature (39.03 ± 0.26°C), significantly higher than both the Symptomatic (38.34 ± 0.44°C; P = 0.007) and Completer (37.94 ± 0.37°C; P<0.001) groups. The difference between the Symptomatic and Completer groups was also statistically significant (P = 0.026). However, when analyzed as the change in body core temperature from resting, the difference between the Completer and Symptomatic groups was no longer significant (Completers: 0.64 ± 0.32°C; Symptomatic: 0.90 ± 0.33°C; P = 0.130). The Hyperthermic group exhibited a significantly greater change in body core temperature (1.59 ± 0.37°C) at the 50 min time point compared to the Completer (P<0.001) and Symptomatic (P = 0.002) groups.
Figure 1.
Absolute (left) and delta (right) body core temperature during the march for each outcome category.
At the time when participants were withdrawn or finished the march the Hyperthermic group had the highest body core temperature (39.11 ± 0.19°C), significantly greater than the Completer (38.23 ± 0.37°C; P < 0.001) and Symptomatic (38.41 ± 0.37°C; P = 0.003) groups, which were not significantly different to each other (P = 0.419). Similarly, the change in body core temperature was significantly greater for the Hyperthermic group (1.68 ± 0.23°C) than the Completers (0.94 ± 0.37°C; P < 0.001) and the Symptomatic groups (0.96 ± 0.34°C; P = 0.003), which were not significantly different to each other (P = 0.979).
No significant differences in heart rate (as measured during the final 10 min of the march) were observed between each of the 3 outcome groups (Completers: 163.7 ± 11.0 beats.min−1; Symptomatic: 157.0 ± 15.6 beats.min−1; Hyperthermic: 178.3 ± 10.0 beats.min−1; P = 0.089). Similarly, when calculated as a percentage of heart rate reserve (%HRR) there were no differences between each of the outcome groups (Completers: 70.6 ± 11.7 %HRR; Symptomatic: 68.3 ± 29.9 %HRR; Hyperthermic: 78.4 ± 17.2 %HRR; P = 0.761).
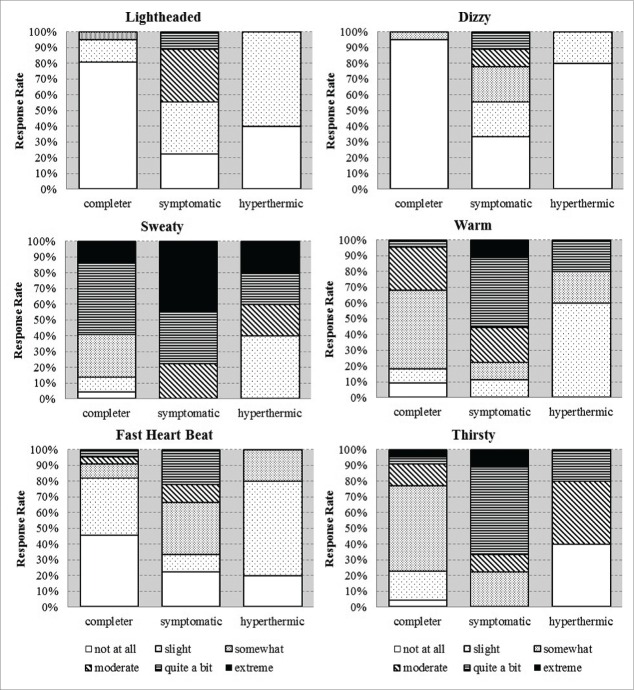
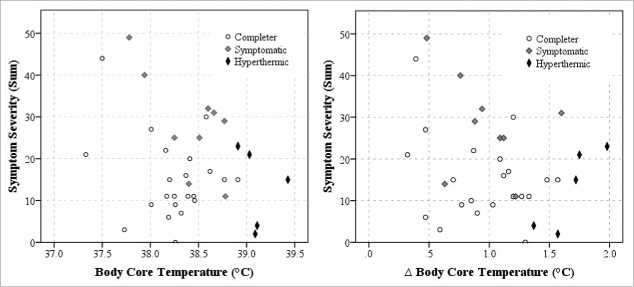
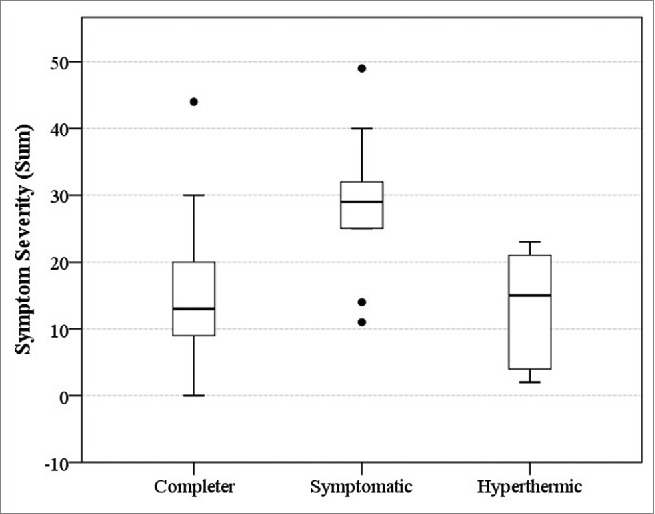
The Symptomatic group reported significantly higher rating of severity for environmental symptoms (28.4 ± 11.8) compared to the Completers (15.0 ± 9.8, P = 0.006) and the Hyperthermic groups (13.0 ± 9.6, P = 0.029) (Fig. 2). Specifically, the Symptomatic group reported proportionally greater severity of symptoms such as light-headedness, dizziness, warmth, perceived fast heart rate, sweatiness, and thirst (Fig. 3). The Hyperthermic group reported a similar symptom experience, up until their withdrawal, as those who went on to complete the march (P = 0.919). The correlations between heat-related symptom severity and final body core temperature (r = −0.271; P = 0.110) and the change in body core temperature (r = −0.253; P = 0.137) were insignificant (Fig. 4).
Figure 2.
The sum of environmental symptoms severity for the march outcome groups (Solid line represents the median, the box represents the interquartile range (25–75% of the sample), the whiskers represent the bounds of 95% of the sample, and the single dots represent outliers – individuals whose data was 1.5–3 times outside the interquartile range).
Figure 3.
Cumulative percentage of symptom severity rating across the march outcome groups for selected symptoms including lightheaded, dizzy, sweaty, warm, fast heart rate, and thirsty.
Figure 4.
Relationship between final body core temperature (left) and delta body core temperature (right) with symptom severity.
In-spite of the different outcome groups, there was little difference in their individual characteristics or amount of load carried (Table 1). The only significant difference between the groups was the lower percentage body fat of the Hyperthermic participants.
Table 1.
Individual characteristics and load carriage across the march outcome groups.
| Completers (n = 23) | Symptomatic (n = 9) | Hyperthermic (n = 5) | |
|---|---|---|---|
| Height (m) | 1.8 (0.07) | 1.8 (0.05) | 1.8 (0.05) |
| Mass (kg) | 82.6 (10.2) | 79.9 (7.4) | 76.9 (12.2) |
| Muscle Mass (kg) | 41.0 (4.8) | 39.5 (3.8) | 40.3 (6.4) |
| Fat Mass (kg) | 11.2 (4.5) | 10.9 (4.2) | 6.9 (2.1) |
| Body Fat (%) | 13.3 (4.3) | 13.6 (4.6) | 8.8 (1.7)* |
| VO2max (mL kg−1 min−1) | 48.8 (4.8) | 47.9 (5.4) | 49.6 (1.2) |
| Load Carriage (kg) | 42.4 (3.3) | 40.5 (3.7) | 40.5 (4.7) |
Data are presented as: mean (standard deviation);
P < 0.05. VO2max - Maximal aerobic power.
Discussion
A clear dissociation between heat-related symptom severity and body core temperature elevation was observed in the present study. This finding is in contrast to the physiological assumptions underpinning the work duration limits of the Work Table. In addition, the majority of participants were able to complete the activity even though it was conducted in environmental conditions warmer than the Work Table guidance would permit. Together, these findings suggest that the level of force protection provided by the Work Table limits, derived through assumptions of body core temperature elevation and the associated risk of heat-related illness, may be preventing the majority of personnel from conducting activities in hot environments and thereby constraining a commander's mandate to develop a resilient and optimised military force. However, caution must be exercised before forgoing the current Work Table limits, as it remains unclear if the Hyperthermic group would have progressed to a dangerously high body core temperature.
Completers
The majority of soldiers (62%) were able complete the march even though the environmental conditions were above those prescribed by the Work Table guidance for this training activity. They were asymptomatic for heat-related illness and their body core temperature response was less than 39.0°C. These findings lend support for the anecdotal observations of commanders claiming that the Work Table guidance is too restrictive and does not allow them to develop their operational capability for hot environments. It is possible that this group could continue to conduct work at this rate, or conduct more demanding work for an equivalent period of time, which would offer the commander greater flexibility when directing personnel to conduct activities. In essence, the Work Table recommendations appear to be more concerned with identifying the “weakest links” rather than optimising the training stimulus and enhancing the overall operational capability of the Defense Force. Consequently, the majority of personnel would have been prevented from conducting a training activity that they were capable of completing. This finding suggests that the Work Table guidance is weighted toward force protection for personnel who are most susceptible to heat-related illness.
Symptomatic
The symptoms experienced to a proportionately greater severity by the Symptomatic group (Fig. 3) are suggestive of the underlying physiological mechanisms of heat exhaustion. To facilitate regulation of body core temperature during work in the heat, increases in cutaneous blood flow25 combined with the onset of sweating26 causes participants to feel warm and sweaty all over.27 Increased fluid loss through sweating causes a progressive dehydration and the sensation of thirst.28 Dehydration and a redistribution of blood flow to the cutaneous vasculature can compromise central venous pressure and mean arterial pressure and lead to a decrease in blood flow to the brain, which would contribute to participants feeling lightheaded and dizzy.29 These physiological mechanisms explain why participants experienced certain symptoms of heat-related illness. However, not all participants experienced this sequence of physiological events.
The observation that a proportion (24%) of participants experienced the symptoms of heat exhaustion necessitating cessation of the activity was in agreement with the physiological assumptions underpinning the Work Table. The physiological assumptions originate from studies of heat strain during exercise at fixed work-rates where exhaustion rarely occurred at body core temperatures less than 38.0°C but always less than 40°C; with approximately 20% of personnel becoming exhausted at 38.5°C.1,11-13 Since the present findings demonstrate the anticipated rate of heat-related illness commensurate with the physiological assumptions, there is evidence to propose that the Work Table guidance is enabling a level of force protection. This is because the present forced-march activity was conducted in environmental conditions which rose above the Work Table guidance. As such, adherence to the Work Table guidance would have reduced the potential for heat-related illness to develop. However, a key finding of the present study was the disassociation between body core temperature elevation and signs and symptoms of heat-related illness. That is to say, the Hyperthermic group exhibited higher body core temperature yet without symptoms, while the Symptomatic group experienced symptoms without an excessive elevation in body core temperature (Figs. 1 and 4). The body core temperature associated with exhaustion has long been considered to be an important marker of tolerance to work in the heat;10-12 an assumption that underpins the Work Table guidance. However, the disconnect between body core temperature and signs and symptoms observed in the present and other studies1,18,19 suggests it is a coincident relationship and that body core temperature elevation may be separate from the development of heat exhaustion during externally paced work activities, as opposed to a driving factor.
Hyperthermic
To shed light on the potential disconnect between body core temperature and symptoms, a closer examination of the Hypethermic group's response is required. Two conflicting points of view can be drawn from the Hyperthermic group: was their elevation in body core temperature an indication of impending heat stroke? Or was their lack of symptoms an indication that they were not at risk of heat-related illness? Since these participants were removed from the present study upon reaching a body core temperature of 39.0°C, it remains unclear which category they fall into. However, insight into both of these potential outcomes can be gained from a discussion of the scientific literature.
Several reasons can be proposed that would suggest the body core temperature elevation of the Hyperthermic group indicates they are at risk of developing heat stroke. Firstly, the Hyperthermic group exhibited a 2–3 times greater rate of elevation in body core temperature (compared to the Symptomatic and Completer groups) yet they did not experience the signs and symptoms of heat exhaustion any more than the Completers. Similar observations have been made during an acclimatisation study where participants were requested to stop exercising upon reaching a body core temperature of 39.5°C yet in 63% of cases this was not accompanied by signs and symptoms of heat exhaustion.1 These findings highlight that the development of hyperthermia cannot be accurately perceived by those working in the heat. A second factor which raises the risks for the Hyperthmic group is that body core temperature is not routinely monitored during military training activities. Consequently the development of hyperthermia, imperceptible to the individual in the absence of signs and symptoms, will also progress undetected by commanders. Therefore it is plausible that commanders would instruct the Hyperthermic group in the same way as the Completers, with the potential development of dangerously high body core temperature. For these reasons cases of heatstroke in military activities, often occurring within 2 hours of commencing physical exertion,30 are commonly associated with highly motivated and apparently healthy individuals who continue to work until collapse.2,3,30 Therefore it is foreseeable that the rate of elevation in body core temperature in this study's Hyperthermic participants may be an indication of an impending risk of heat stroke. If this is the case, then adherence to the Work Table guidance is critical to safeguarding against heat-related illnesses.
In contrast to this assertion that a high body core temperature is an indication of impending collapse with heat stroke, a growing body of evidence is showing that body core temperature in excess of 39.0°C, and with several individuals in excess of 40.0°C, during exertional heat stress is tolerable without sequelae, morbidity, or mortality.17-19 In-spite of the conditions being in excess of Australia's Work Table limits in these studies, all participants of a loaded march (25 km)18 or unloaded running (21 km)19 activities were asymptomatic for heat exhaustion and heat stroke. Even though the Hyperthermic participants in the present study exhibited a much greater change in body core temperature in the first 50 min of the march compared to the Completers, the change was similar to those observed elsewhere, raising from 37.4°C to ∼39.0°C in approximately 30 min.19 Since the Hyperthermic participants of the present study were also asymptomatic, these findings appear to offer support for concluding that they were not at risk of heat-related illness.
To reconcile the differences between these disparate conclusions it is important to understand the differences between the studies. Two key differences can be identified between the present study and previous studies showing heat-related illness to develop at body core temperature in the range of 38.0–39.0°C,1,11-13 and the studies showing personnel are asymptomatic in-spite of high body core temperature elevation.18,19 These include the opportunity to self-pace the work activity and the maximal aerobic capacity of the study participants. When personnel were able to change their pace or take rest breaks, they were able to tolerate the work and complete the activity.17,18 Alternatively, when the work was externally paced,3,10-12 as in the current study, a proportion of personnel experienced symptoms of heat-related illness, and exposed a further proportion to the potential for a dangerously high body core temperature to develop. A study comparing fixed-paced to self-paced work in the heat demonstrated that self-paced workers can maintain a lower body core temperature,31 although this is not always the case for the military population.32 However, appropriate guidance based on feedback from individual physiological responses has been shown to improve pacing strategies and reduce thermal strain during work in the heat.33
The maximal aerobic capacity of the present study's participants may also have contributed to the disparities with the conclusions of similar studies. The average VO2max of participants in the studies showing personnel are asymptomatic in-spite of high body core temperature elevation was 56 and 59 mL kg−1 min−1,18,19 much higher than in this study (Table 1). Since greater aerobic capacity is known to raise the body core temperature tolerated at exhaustion34 and is associated with reduced risk of heat-related illness,35 this may also account for some of the disparities observed between the studies. However within the present study there was minimal difference in the individual characteristics of the outcome groups (Table 1). This is likely due to the homogenous nature of the study sample, with the range in individual characteristics such as aerobic fitness and body composition being narrower than those studies which found these parameters to be associated with heat intolerance or elevated risk of heat-related illness.34,35 A similar lack of association has also been reported in other studies.1,33
Future research directions
To optimise the balance between force protection and operational capability into the future, the present study has highlighted several observations that require further investigation. Firstly, the dissociation between heat-related symptoms and body core temperature highlighted by the present study suggests that the physiological mechanisms underpinning exhaustion during work in the heat should be re-examined to determine the most appropriate physiological criteria to use for the determination of work duration limits. Combined with the potential for hyperthermia to develop imperceptible to the individual and commanders in the absence of heat-related symptoms, the findings provide a strong impetus to direct research toward understanding the factors that could be used to identify these susceptible individuals prior to commencing military training activities. Furthermore, research should determine the potential for the Symptomatic personnel to improve heat tolerance through acclimatisation training. Repeated exposure to work in the heat has been shown to reduce symptoms and improve tolerance times.1 Therefore, an avenue to promote operational capability could be to direct Symptomatic personnel to specialized training and allow the more tolerant personnel to work to higher levels of heat stress. Finally, further research should explore the potential for self-pacing of military training activities. Removing time constraints and fixed work intensities may help to reduce the risk of collapse with heat stroke or being overcome by the symptoms of heat-exhaustion provided adequate training and guidance is provided to personnel.
Conclusions
The present study provides evidence to show that the force protection provided by the Work Table may be preventing the majority of personnel from conducting activities in hot environments and thereby constraining a commander's mandate to develop a resilient and optimised military force. However, caution must be exercised before forgoing the Work Table limits. The importance of this was highlighted by a small proportion of personnel who exhibited greater rates of body core temperature elevation. In-spite of the lack of symptoms of heat-related illness there was a credible risk that they could continue work until collapse since the training activity was at a fixed-paced. The dissociation between symptoms of heat-related illness and body core temperature elevation observed in the present study suggests that the physiological mechanisms underpinning exhaustion during exertional heat stress should be re-examined to determine the most appropriate physiological criteria for establishing work duration limits.
Abbreviations
- VO2max
Maximal aerobic power
- WBGT
Wet-Bulb Globe Temperature
- %HRR
Percentage of Heart Rate Reserve
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- [1].Armstrong LE, Hubbard RW, Kraemer WJ, Deluca JP, Christensen EL. Signs and symptoms of heat exhaustion during strenuous exercise. Annals of Sports Med 1987; 3:182-9 [Google Scholar]
- [2].Heled Y, Rav-Acha M, Shani Y, Epstein Y, Moran D. The “Golden Hour” for Heatstroke Treatment. Military Med 2004; 169:184-6; PMID:15080235; http://dx.doi.org/ 10.7205/MILMED.169.3.184 [DOI] [PubMed] [Google Scholar]
- [3].Rav-Acha M, Hadad E, Epstein Y, Heled Y, Moran DS. Fatal exertional heart stroke: A case series. Am J Med Sci 2004; 328:84-7; PMID:15311166; http://dx.doi.org/ 10.1097/00000441-200408000-00003 [DOI] [PubMed] [Google Scholar]
- [4].Bricknell MCM. Heat Illness in the Army in Cyprus. Occup Med 1996; 46:304-12; PMID:8854710; http://dx.doi.org/ 10.1093/occmed/46.4.304 [DOI] [PubMed] [Google Scholar]
- [5].Goldman RF. Introduction to Heat-Related Problems in Military Operations In: Pandolf KB, Burr RE, eds. Medical Aspects of Harsh Environments. Washington: Borden Institute, 2001:3-49 [Google Scholar]
- [6].Sawka MN, Pandolf KB. Physical Exercise in Hot Climates: Physiology, Performance, and Biomedical Issues In: Pandolf KB, Burr RE, eds. Medical Aspects of Harsh Environments. Washington: Borden Institute, 2001:87-133 [Google Scholar]
- [7].Blanchard L, Santee WR. Comparison of USARIEM strain decision aid to mobile decision aid and standard army guidelines for warm weather training (T08-07). Natick: US. Army Research Institute of Environmental Medicine 2008; 46:1-46. [Google Scholar]
- [8].US. Department of Defence Heat stress control and heat casualty management (TB MED 507/AFPAM 48-152(I)) Washington DC: Departments of the Army and Air Force, 2003. [Google Scholar]
- [9].Gonzalez RR, McLellan TM, Withey WR, Chang SK, Pandolf KB. Heat strain models applicable for protective clothing systems: comparison of core temperature response. J Appl Physiol 1997; 83:1017-32; PMID:9292490 [DOI] [PubMed] [Google Scholar]
- [10].Kraning KK, Gonzalez RR. A mechanistic computer simulation of human work in heat that accounts for physical and physiological effects of clothing, aerobic fitness and progressive dehydration. J Thermal Biol 1997; 22:331-42; http://dx.doi.org/ 10.1016/S0306-4565(97)00031-4 [DOI] [Google Scholar]
- [11].Montain SJ, Sawka MN, Cadarette BS, Quigley MD, McKay JM. Physiological tolerance to uncompensable heat stress: effects of exercise intensity, protective clothing, and climate. J Appl Physiol 1994; 77:216-22; PMID:7961236 [DOI] [PubMed] [Google Scholar]
- [12].Sawka M, Latzka W, Montain S, Cadarette B, Kolka M, Kraning K, Gonzalez R. Physiologic tolerance to uncompensable heat: intermittent exercise, field vs laboratory. Med Sci Sports Exerc 2001; 33:422-30; PMID:11252069; http://dx.doi.org/ 10.1097/00005768-200103000-00014 [DOI] [PubMed] [Google Scholar]
- [13].Sawka MN, Young AJ, Latzka WA, Neufer PD, Quigley MD, Pandolf KB. Human tolerance to heat strain during exercise: Influence of hydration. J Appl Physiol 1992; 73:368-75; PMID:1506393 [DOI] [PubMed] [Google Scholar]
- [14].Havenith G, van Middendorp H. The relative influence of physical fitness, acclimatization state, anthropometric measures and gender on individual reactions to heat stress. Eur J Appl Physiol 1990; 61:419-27; http://dx.doi.org/ 10.1007/BF00236062 [DOI] [PubMed] [Google Scholar]
- [15].Lisman P, Kazman JB, O'Connor F, Heled Y, Duester PA. Heat tolerance testing: Association between heat intolerance and anthropometric and fitness measurements. Mil Med 2014; 179:1339-46; PMID:25373064; http://dx.doi.org/ 10.7205/MILMED-D-14-00169 [DOI] [PubMed] [Google Scholar]
- [16].Coso JD, Hamouti N, Ortega J, Fernandez-Elias V, Mora-Rodriguez R. Relevance of individual characteristics for thermoregulation during exercise in a hot-dry environment. Eur J Appl Physiol 2011; 111:2173-81; PMID:21305382; http://dx.doi.org/ 10.1007/s00421-011-1847-x [DOI] [PubMed] [Google Scholar]
- [17].Ely BR, Ely MR, Cheuvront SN, Kenefick RW, DeGroot DW, Montain SJ. Evidence against a 40°C core temperature threshold for fatigue in humans. J Appl Physiol 2009; 107:1519-25; PMID:19713430; http://dx.doi.org/ 10.1152/japplphysiol.00577.2009 [DOI] [PubMed] [Google Scholar]
- [18].Nolte HW, Noakes TD, van Vuuren B. Trained humans can exercise safetly in extreme dry heat when drinking water ad libitum. J Sports Sci 2011; 29:1233-41; PMID:21780852; http://dx.doi.org/ 10.1080/02640414.2011.587195 [DOI] [PubMed] [Google Scholar]
- [19].Lee JKW, Nio AQX, Lim CL, Teo EYN, Bryne C. Thermoregulation, pacing and fluid balance during mass participantion distance running in a warm and humid evnrionment. Eur J Appl Physiol 2010; 109:887-98; PMID:20237797; http://dx.doi.org/ 10.1007/s00421-010-1405-y [DOI] [PubMed] [Google Scholar]
- [20].Ramsbottom R, Brewer J, Williams C. A progressive shuttle run test to estimate maximal oxygen uptake. Br J Sports Med 1988; 22:141-4; PMID:3228681; http://dx.doi.org/ 10.1136/bjsm.22.4.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].American Society for Testing and Materials Standard Test Method for Measuring Thermal Insulation of Clothing Using a Heated Manikin. Pennsylvania, ASTM International: F1291-10, 2010. [Google Scholar]
- [22].American Society for Testing and Materials Standard Test Method for Measuring the Evaporative Resistance of Clothing Using a Sweating Manikin. Pennsylvania, ASTM International: F2370–10, 2010. [Google Scholar]
- [23].Pandolf KB, Givoni B, Goldman RF. Predicting energy expenditure with loads while standing or walking very slowly. J Appl Physiol 1977; 43:577-81; PMID:908672 [DOI] [PubMed] [Google Scholar]
- [24].Sampson JB, Kobrick JL, Johnson RF. Measurement of subjective reactions to extreme environments: The environmental symptoms questionnaire. Military Psychol 1994; 6:215-33; http://dx.doi.org/ 10.1207/s15327876mp0604_2 [DOI] [Google Scholar]
- [25].Gonzalez-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol 1999; 86:1032-9; PMID:10066720 [DOI] [PubMed] [Google Scholar]
- [26].Buono MJ, Maupin CJ. Relationship between sweat gland recruitment and esophageal temperature during exercise-induced hyperthermia. J Thermal Biol 2003; 28:381-4; http://dx.doi.org/ 10.1016/S0306-4565(03)00021-4 [DOI] [Google Scholar]
- [27].Fukazawa T, Havenith G. Differences in comfort perception in relation to local and whole body skin wettedness. Eur J Appl Physiol 2009; 106:15-24; PMID:19159949; http://dx.doi.org/ 10.1007/s00421-009-0983-z [DOI] [PubMed] [Google Scholar]
- [28].Greenleaf JE. Problem: thirst, drinking behavior, and involuntary dehydration. Med Sci Sports Exerc 1992; 24:645-56; PMID:1602937; http://dx.doi.org/ 10.1249/00005768-199206000-00007 [DOI] [PubMed] [Google Scholar]
- [29].Wessely S, Nickson J, Cox B. Symptoms of low blood pressure: a population study. BMJ 1990; 301:362-5; PMID:2400856; http://dx.doi.org/ 10.1136/bmj.301.6748.362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Epstein Y, Moran DS, Shapiro Y, Sohar E, Shemer J. Exertional heat stroke: A case series. Med Sci Sports Exerc 1999; 31:224-8; PMID:10063810; http://dx.doi.org/ 10.1097/00005768-199902000-00004 [DOI] [PubMed] [Google Scholar]
- [31].Wyndham CH. The effects of heat stress upon human productivity. Arch Sci Physiol 1973; 27:A491-A7 [PubMed] [Google Scholar]
- [32].Soule RG, Pandolf KB, Goldman RF. Voluntary march rate as a measure of work output in the heat. Ergonomics 1978; 21:455-62; PMID:679933; http://dx.doi.org/ 10.1080/00140137808931742 [DOI] [PubMed] [Google Scholar]
- [33].Buller MJ, Welles AP, Stevens M, Leger J, Gribok A, Jenkins OC, Friedl KE, Rumpler W. Automated guidance from phsyiological sensing to reduce thermal-work strain levels on a novel task Body Sensor Networks Conference 2015. Cambridge, USA, 2015 [Google Scholar]
- [34].McLellan TM. The importance of aerobic fitness in determining tolerance to uncompensable heat stress. Comp Biochem Physiol A Mol Integr Physiol 2001; 128:691-700; http://dx.doi.org/ 10.1016/S1095-6433(01)00275-6 [DOI] [PubMed] [Google Scholar]
- [35].Wallace RF, Kriebel D, Punnett L, Wegman DH, Wenger CB, Gardner JW, Kark JA. Risk factors for recruit exertional heat illness by gender and training period. Aviat Space Environ Med 2006; 77:415-21 [PubMed] [Google Scholar]