Abstract
Background
Orthopaedic surgery lags behind other surgical specialties in terms of gender diversity. The percentage of women entering orthopaedic residency persistently remains at 14% despite near equal ratios of women to men in medical school classes. This trend has been attributed to negative perceptions among women medical students of workplace culture and lifestyle in orthopaedics as well as lack of exposure, particularly during medical school when most women decide to enter the field. Since 2012, The Perry Initiative, a nonprofit organization that is focused on recruiting and retaining women in orthopaedics, had conducted extracurricular outreach programs for first- and second-year female medical students to provide exposure and mentoring opportunities specific to orthopaedics. This program, called the Medical Student Outreach Program (MSOP), is ongoing at medical centers nationwide and has reached over 300 medical students in its first 3 program years (2012–2014).
Questions/purposes
(1) What percentage of MSOP participants eventually match into orthopaedic surgery residency? (2) Does MSOP impact participants’ perceptions of the orthopaedics profession as well as intellectual interest in the field?
Methods
The percentage of program alumnae who matched into orthopaedics was determined by annual followup for our first two cohorts who graduated from medical school. All program participants completed a survey immediately before and after the program that assessed the impact of MSOP on the student’s intention to pursue orthopaedics as well as perceptions of the field and intellectual interest in the discipline.
Results
The orthopaedic surgery match rate for program participants was 31% in our first graduating class (five of 16 participants in 2015) and 28% in our second class (20 of 72 participants in 2016). Pre/post program comparisons showed that the MSOP influenced students’ perceptions of the orthopaedics profession as well as overall intellectual interest in the field.
Conclusions
The results of our study suggest that The Perry Initiative’s MSOP positively influences women to choose orthopaedic surgery as a profession. The match rate for program alumnae is twice the percentage of females in current orthopaedic residency classes. Given these positive results, MSOP can serve as a model, both in its curricular content and logistic framework, for other diversity initiatives in the field.
Introduction
As a specialty, orthopaedic surgery is struggling in its efforts to recruit more women into the profession. Currently, orthopaedic surgery ranks the lowest among all specialties with regard to percentage of female residents and practicing surgeons [1]. The reasons for this are multifactorial involving exposure to the specialty, available mentors, preconceived ideas about physical demands, and lifestyle as well as others [3, 7, 8].
Although the percentage of female residents in orthopaedic surgery has increased modestly over the past two decades, it has not kept pace with other surgical subspecialties and has plateaued at 14% [1] despite near equal (47%) representation of females in the medical student body [2]. Recent studies shed some light on these trends, indicating that negative perceptions of workplace culture and lifestyle in orthopaedics persist among female medical students [6, 7]. Furthermore, women are more likely to decide to pursue orthopaedics during clinical rotations in medical school as opposed to men who are more likely to decide on orthopaedics before entrance into medical school or clinical rotations [4]. Taken together, this suggests that medical school is a critical window of opportunity for recruiting women into the field.
The Perry Initiative is a nonprofit organization that is focused on recruiting and retaining women in orthopaedics. Since 2009, the organization, governed by practicing women engineers and surgeons, has conducted out-of-school time programs for women in high school, college, and medical school. Beginning in 2012, The Perry Initiative launched the Medical Student Outreach Program (MSOP) targeting first- and second-year female medical students at medical schools nationwide. MSOP consists of hands-on curriculum and lectures guided predominantly by female residents and attending surgeons. The purpose of this study is to present early findings on the impact of MSOP programs on recruitment of women into orthopaedic residency. Specifically, we were interested in addressing the following questions: (1) What percentage of MSOP participants eventually match into orthopaedic surgery residency? (2) Does MSOP impact participants’ perceptions of the orthopaedics profession as well as intellectual interest in the field?
Materials and Methods
MSOP is a 3-hour exposure program for first- (MS-1) and second-year (MS-2) women medical students. MSOP is conducted year-round at medical centers nationwide, most frequently in locations where MS-1 and MS-2 students can be recruited from multiple medical schools in a geographic region. In 2012, two MSOP programs were held, reaching a total of 26 students; in 2013, there were four programs, reaching 65 students; and, in 2014, there were 11 programs reaching 227 students. Each MSOP can accommodate up to 30 students, and to date, all interested students were admitted to the program. The MSOP curriculum consists of 90 minutes of lecture from women orthopaedic surgeons and residents and 90 minutes of hands-on mock orthopaedic surgery (“Sawbones” laboratory). Lectures explicitly address the following issues: (1) stereotypes and misconceptions about orthopaedic practice; (2) orthopaedic subspecialties; (3) academic and prior experience expectations to get into orthopaedic residency; and (4) work-life balance. The hands-on portion of MSOP is presented as a case study of appropriate treatment of a midshaft femur fracture, and students practice both external fixator and intramedullary nailing techniques. Basic power tool training is also included before the Sawbones laboratories.
To assess the impact of MSOP programming on recruitment into orthopaedic residency, two separate evaluations were performed. First, all MSOP alumnae who were potentially eligible for the residency match in our first two medical school graduation classes (2015 and 2016) were contacted by email. They were asked whether they had participated in the match, whether they were successfully matched, and, if so, whether they had matched into orthopaedic surgery. Second, a pre/post program survey (Table 1) was administered to all MSOP participants in paper form immediately before and after the program. The survey examined each participant’s intention to pursue orthopaedic surgery, intellectual interest in the subject matter (orthopaedics, surgery, and musculoskeletal care), and perceptions about the field of orthopaedic surgery. The latter focused specifically on issues that were identified in a prior study [6] to be factors in womens’ decisions to pursue orthopaedics, including lifestyle, workforce diversity, length of training, financial rewards, physical demands, and competitiveness. Matched (pre/post) survey data were collected for 206 participants in MSOP programs from 2012 to 2014. Survey responses were mapped to a 5-point Likert scale and compared pre/post program using one-way, repeat-measures analysis of variance (JMP Pro v12.1; SAS Institute Inc, Cary, NC, USA).
Table 1.
Excerpts from the survey instrument for pre/post program evaluation of Medical Student Outreach Program (MSOP) participants*
| Question | Response options |
|---|---|
| 1. How intellectually interested are you in the following? The Musculoskeletal System Surgical Techniques Orthopaedic Surgery |
5-point Likert Scale Very Disinterested (1), Disinterested (2), Neutral (3), Interested (4), Very Interested (5) |
| 2. How do you perceive orthopaedic surgery with regard to the following? Lifestyle During/After Training Work Force Diversity Within the Specialty Length of Training Financial Rewards Physical Demands Competitiveness |
5-point Likert Scale Very Unfavorable (1), Unfavorable (2), Neutral (3), Favorable (4), Very Favorable (5) |
| 3. Were you interested in orthopaedic surgery before participating in the program? | Yes, No, Undecided |
| 4. Did this program have any impact on your intentions to pursue orthopaedic surgery? | 5-point Likert Scale Very Negative (1), Negative (2), No Impact (3), Positive (4), Very Positive (5) |
| 5. (If No or Undecided for Q3) How likely are you now to select orthopaedic surgery as a specialty? | 5-point Likert Scale Definitely Not (1), Not Very Likely (2), Could Go Either Way (3), Likely (4), Very Likely (5) |
*These excerpts focus on factors influencing choice of medical specialty as well as perceptions of orthopaedics.
Results
MSOP Participants’ Success in the Orthopaedic Match
Sixteen program alumnae were eligible for the residency match in 2015, and 72 were confirmed to be eligible in 2016. Five alumnae matched in orthopaedic surgery in 2015 and 20 in 2016, yielding annual match rates of 31% (five of 16) and 28% (20 of 72), respectively.
MSOP and Participants’ Perceptions of Orthopaedics
Pre/post program survey data indicated that 57% (117 of 205) of the program attendees were interested in orthopaedics before attending the program, and the program had a “positive” or “very positive” impact on their intentions to pursue orthopaedics in 45% (92 of 205) and 48% (98 of 205) of the cases, respectively. Of those participants who had no intention of pursuing orthopaedics (12% [11 of 88]) or were undecided on a residency (31% [27 of 88]), 96% (37 of 38) said that the program had a “very positive” (34% [13 of 38]) or “positive” (62% [24 of 38]) impact on their intentions to pursue orthopaedics. Of this cohort, 25% (nine of 37) are now “likely” or “very likely” to pursue orthopaedic residency with an additional 66% (24 of 37) stating that they were neutral on pursuing orthopaedics.
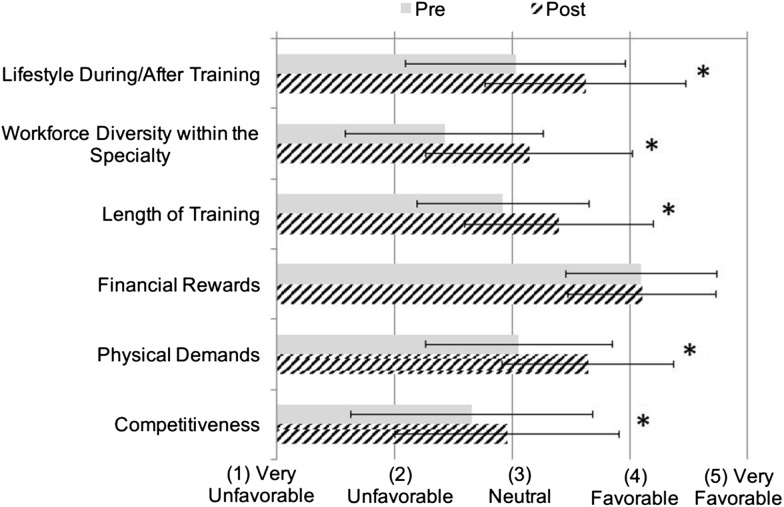
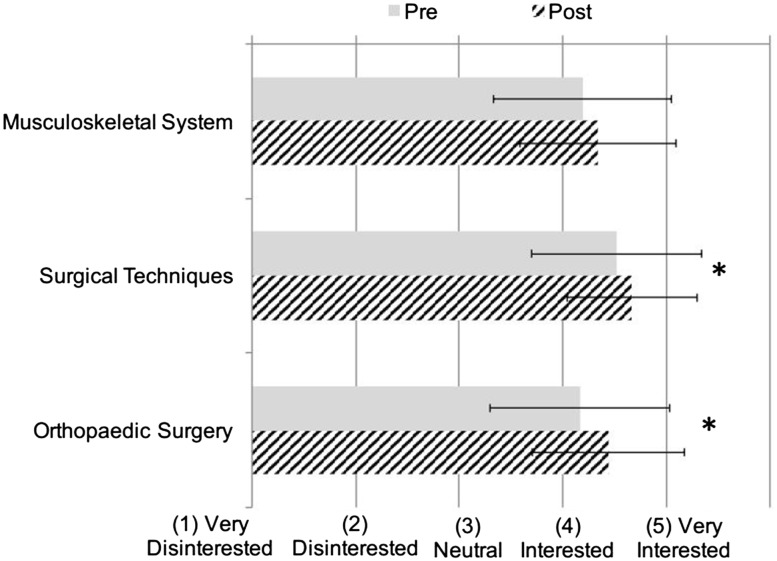
Pre/post program survey data also indicated that the MSOP influenced students’ perceptions of the orthopaedics profession as well as overall intellectual interest in the field. Survey results showed positive shifts in participants’ perceptions of orthopaedics in terms of lifestyle, workforce diversity, length of training, physical demands, and competitiveness (p < 0.05 for all outcomes; Fig. 1). There was also greater intellectual interest in surgical techniques and orthopaedic surgery as a result of program participation (p = 0.001 for both measures; Fig. 2).
Fig. 1.
This figure presents pre/post program survey responses to the question, “How do you perceive orthopaedic surgery with regards to the following?” The asterisk (*) represents a statistically significant difference with p < 0.05 for repeat-measures analysis of variance (N = 206; df = 1).
Fig. 2.
This figure presents pre/post program survey responses to the question, “How intellectually interested are you in the following?” The asterisk (*) represents a statistically significant difference with p < 0.05 for repeat-measures analysis of variance (N = 206; df = 1).
Discussion
The results of our study suggest that The Perry Initiative’s MSOP positively influences women to choose orthopaedic surgery as a profession. The match rate for program alumnae (28%–31%) is twice the percentage of females in orthopaedic residency classes over the past decade (14%) [1]. Pre/post program survey results indicate that MSOP substantively and positively shifts participants’ intellectual interest in orthopaedics as well as their perceptions of the profession in terms of lifestyle, workforce diversity, and competitiveness. Prior work has shown that women medical students view orthopaedics more negatively on these particular issues than their male counterparts [6, 7]. MSOP appears to positively shift these perceptions, at least in the short term, which may lead to the higher than average residency match rate for program alumnae.
The results of this study are inherently preliminary, and there are some limitations that should be addressed. First, with the rapid expansion of our program, the majority of our alumnae has not yet completed medical school and will match into residency in the coming years. We are thus relying on the positive responses from our pre/post program surveys in projecting that the program will continue to yield orthopaedic residency match rates that are greater than the national average. Second, match results were self-reported and, although we can estimate when alumna may be eligible for the match based on their medical school year at the time of the program, there is no publically accessible repository for match results. For this reason, our match rates for 2015 and 2016 only included program alumnae who confirmed that they participated in the match. Lastly, our long-term results, specifically the match rate, does discern between women who were interested in orthopaedics a priori the program and those who were influenced by MSOP to pursue orthopaedics. The matriculation rate for females who are interested in orthopaedics as MS-1 or MS-2 students is currently unknown and would be the best point of comparison. Regardless, the true effect of our program will be evident within the next 2 years given that the larger cohorts of program alumnae, eg, 227 participants in 2014, will be qualified to match in 2017 to 2019. If the program’s match rate remains at 30%, the influx of women from the program will be large enough to notably increase the percentage of females in the nationwide residency class.
MSOP was intentionally designed to provide timely, substantive exposure to careers in orthopaedic surgery. Prior research has shown that the majority of women medical students choosing surgical careers decide on this pathway during medical school, particularly after rotating in orthopaedic surgery [4]. Multiple investigators have stressed the importance of hands-on exposure and career mentoring for women in the field [4–7]; and having a role model of the same sex has been shown to be more important for women than men in recruitment into orthopaedic surgery [6]. Taken together, this prior work suggests that women need to be recruited into orthopaedic surgery both before and during medical school and that outreach efforts should include both hands-on exposure and mentoring from current women in the field.
The strength of The Perry Initiative’s MSOP is that it follows these suggested practices of early intervention and mentoring. As such, MSOP can serve as a model, both in its curricular content and logistic framework, for other diversity initiatives in the field. The program is logically scalable and relatively economical compared with other interventions, and, anecdotally, we have found that the nationwide presence of MSOP has unified and amplified individual practicing women surgeons’ mentoring efforts, particularly as it is conducted in partnership with organizations such as the Ruth Jackson Orthopaedic Society and the American Association of Orthopaedic Surgeons. Given the uneven distribution of female orthopaedic residents and attendings nationally [9] and the fact that many medical school programs do not offer substantive exposure to the discipline [4], MSOP offers medical students their only opportunity to network with female role models in the field and gain hands-on exposure to orthopaedic surgical techniques.
Despite the inherently preliminary nature of this study, our results suggest that targeted outreach to women in their early medical school years can positively influence interest, perceptions, and, ultimately, recruitment into orthopaedic residency. Future work will focus on expanding the MSOP program to achieve the overall recruiting targets for the field as well as ongoing monitoring of the impact of our programming efforts on gender diversity in orthopaedics.
Footnotes
The Perry Initiative is underwritten through support from Chevron (San Ramon, CA, USA) and Sawbones (Vashon Island, WA, USA). Programmatic support provided by Acumed (Hillsboro, OR, USA), Stryker (Kalamazoo, MI, USA), DePuy Synthes (Warsaw, IN, USA), Medtronic (Minneapolis, MN, USA), and Zimmer Biomet (Warsaw, IN, USA). Member support from the Ruth Jackson Orthopaedic Society, American Association of Orthopaedic Surgeons, and Orthopaedic Research and Education Foundation; and infrastructural and personnel support for the organization provided by University of Delaware Departments of Mechanical and Biomedical Engineering and Office of Undergraduate Research and Experiential Learning (Newark, DE, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
This work was performed at The Perry Initiative, Newark, DE, USA.
References
- 1.Association of American Medical Colleges. Distribution of Residents by Specialty, 2003 Compared to 2013. Available at: www.aamc.org/download/411784/data/2014_table2.pdf. Accessed May 2016.
- 2.Association of American Medical Colleges. The State of Women in Academic Medicine: the Pipeline and Pathways to Leadership, 2013–2014. Available at: https://members.aamc.org/eweb/upload/The%20State%20of%20Women%20in%20Academic%20Medicine%202013-2014%20FINAL.pdf. Accessed May 2016.
- 3.Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: a prospective analysis. Orthopedics. 2011;34:e919–e932. [DOI] [PubMed]
- 4.Bernstein J, Dicaprio MR, Mehta S. The relationship between required medical school instruction in musculoskeletal medicine and application rates to orthopaedic surgery residency programs. J Bone Joint Surg Am. 2004;86:2335–2338. [DOI] [PubMed]
- 5.Burnley CS, Burkett GL. Specialization: are women in surgery different? J Am Med Womens Assoc. 1986;41(144–1447):151–152. [PubMed] [Google Scholar]
- 6.Day CS, Lage DE, Ahn CS. Diversity based on race, ethnicity, and sex between academic orthopaedic surgery and other specialties. J Bone Joint Surg Am. 2010;92:2328–2335. doi: 10.2106/JBJS.I.01482. [DOI] [PubMed] [Google Scholar]
- 7.Hill JF, Yule A, Zurakowski D, Day CS. Residents’ perceptions of sex diversity in orthopaedic surgery. J Bone Joint Surg Am. 2013;95:e1441–e1446. [DOI] [PubMed]
- 8.Johnson AL, Sharma J, Chinchilli VM, Emery SE, McCollister Evarts C, Floyd MW, Kaeding CC, Lavelle WF, Marsh JL, Pellegrini VD Jr, Van Heest AE, Black KP. Why do medical students choose orthopaedics as a career? J Bone Joint Surg Am. 2012;94:e78. [DOI] [PubMed]
- 9.Van Heest AE, Agel J. The uneven distribution of women in orthopaedic surgery resident training programs in the United States. J Bone Joint Surg Am. 2012;94:e9. doi: 10.2106/JBJS.J.01583. [DOI] [PubMed] [Google Scholar]