Abstract
Viruses have evolved many mechanisms by which to evade and subvert the immune system to ensure survival and persistence. However, for each method undertaken by the immune system for pathogen removal, there is a counteracting mechanism utilized by pathogens. The new and emerging role of microvesicles in immune intercellular communication and function is no different. Viruses across many different families have evolved to insert viral components in exosomes, a subtype of microvesicle, with many varying downstream effects. When assessed cumulatively, viral antigens in exosomes increase persistence through cloaking viral genomes, decoying the immune system, and even by increasing viral infection in uninfected cells. Exosomes therefore represent a source of viral antigen that can be used as a biomarker for disease and targeted for therapy in the control and eradication of these disorders. With the rise in the persistence of new and reemerging viruses like Ebola and Zika, exploring the role of exosomes become more important than ever.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-016-0450-6) contains supplementary material, which is available to authorized users.
Key Words: Exosomes, microvesicles, multivesicular bodies, “back fusion”, ESCRT
Introduction
In the struggle to maintain health, the immune system has evolved several mechanisms to protect the host from pathogens. Foremost is the ability to differentiate self from pathogen, but tools are also required to mobilize components of the immune system in response to threats. Therefore, intercellular communication is key in this process. Until 30 years ago, cell-to-cell signaling was encompassed by transfer of chemokines, cytokines, and direct cell contact. The discovery of vesicles being shed from the surface of reticulocytes as a mechanism for iron transfer forever changed how the field of immunology understood cellular communication [1, 2]. Since then, the understanding of how microvesicles (MVs) contribute to immunity and pathogenicity has exploded. However, pathogens have evolved in concert with the immune system and have developed methods to subvert and co-opt this form of intercellular communication to evade the immune system and aid spread. The cross-over and interaction between MVs, and specifically exosomes, and viruses will be the subject of this review.
The term “microvesicles” (MVs) has undergone an evolution despite there being overwhelming evidence that their secretion is conserved across all kingdoms [3]. In preferred terminology, MVs include vesicles ranging in size from 100 to 1000 nm that are shed from the plasma membrane, as well as exosomes, which range in size from 30 to 100 nm and originate within microvesicular bodies (MVBs) [4, 5]. For the purposes of this review, we will focus our discussion on exosomes; however, there are several excellent reviews in the literature that address extracellular vesicles as a whole [6–11]. In appearance, exosomes are unilamellar vesicles composed of a lipid bilayer that have a homogenous cup-shaped appearance on scanning electromicroscopy [3, 12]. To date, they can be shown to originate from almost every cell type studied, including, but not limited to, T cells [13], B cells [14, 15], dendritic cells [16], neurons [17], astrocytes [18, 19], endothelial cells [20], smooth muscle cells [21], oligodendrocytes [22], and reticulocytes [2, 23]. The wide variety of cells that can excrete exosomes also dictates the wide array of materials in which they can be isolated: saliva, plasma, urine, cerebrospinal fluid, bronchial alveolar lavage, and serum [24]. The contents of exosomes are just as varied and depend heavily on the cells from which they originate but can be considered broadly to include proteins, mRNAs, microRNAs (miRNAs), lipids, and carbohydrates. Once released, the components within exosomes can influence the local microenvironment or spread through circulation to locations far removed from their origin. Indeed, exosomes have been shown to cross the blood–brain barrier [25], perhaps pointing to their role in allowing coordination with the immune system in even immune-privileged sites [26]. This aspect of exosome biology is especially important, as there are many instances in which viral proteins can be isolated, but the virus itself is difficult to detect. The presence of viral antigens in the absence of viral detection may be better understood through an understanding of exosome biogenesis and uptake.
Exosome Biogenesis
As aforementioned, exosomes originate in MVBs (late endosomes), which are a component of the endocytic pathway. MVBs contain intraluminal vesicles (ILVs) that range in size from 30 to 100 nm and can be targeted for 2 separate fates: lysosomal degradation or fusion with the plasma membrane, after which release of ILVs to the extracellular environment occurs and at which point they are termed exosomes [4, 27]. In a process called “back fusion”, ILVs deliver plasma membrane invaginations (through clathrin-mediated and clathrin-independent endocytosis) to the endosomal network, making them (and therefore exosomes) capable of carrying both intracellular and extracellular materials [8, 28, 29]. Indeed, exosomes are seen as an exciting avenue for their capability in giving snapshots of the microenvironment, and serving as a good source of biomarkers. Part of this advantage is owing to the large cross-over between exosome biogenesis and egress, pathogen entry, and normal macromolecule entry and cycling within the cell [23, 27, 28].
The exact intracellular signals that direct ILVs to the plasma membrane for release are still under investigation and will be discussed briefly here. Endosomal sorting complexes required for transport (ESCRT) machinery has been studied in its role for directing ubiquitin-labeled proteins into endosomes for delivery into MVBs, and, as such, ESCRT proteins, like Alix and TSG101, are enriched in exosomes [30, 31]. Lipid raft-associated proteins such as transferrin and caveolins, and other proteins involved in membrane trafficking, like the tetraspanins CD9, CD63, and CD81, which have been shown to bind to ESCRT machinery, are also enriched in exosomes [32–34]. There are now several databases that exist that list the assortment of materials that can be found in exosomes (Vesiclepedia, EVPedia, and Exocarta) [7, 35, 36].
However, ESCRT is not the only method by which exosome formation can occur as there are also ESCRT-independent methods by which proteins, lipids, and RNA can enter the endosomal pathway. For example, oligodendrocytes direct exosome formation via the ceramide pathway [37], while other cell types rely on oligomerization of tetraspanin complexes [8, 38, 39]. Furthermore, while knockdown of some ESCRT components may abrogate exosome production, it does not completely knock it out [40, 41]. Indeed, Rab GTPases, a known family of conserved proteins that regulate vesicular trafficking and membrane fusion events, are also involved in exosome formation as denoted by their high abundance in isolated exosomes [23, 42]. Several are implicated in the release of exosomes, including Rab11, Rab27, Rab5, Rab35, and Rab7, depending on cell type [8, 23]. Rab 27a, in particular, regulates the fusion of MVBs at the plasma membrane to release ILVs [8, 23, 43]. Knockdown of Rab 27a inhibits exosome secretion from tumor cell lines [4, 43]. There are several other Rabs that have also proven essential through a diminution in exosome levels after their knockdown, including Rab 2B, Rab9A, Rab5A, and Rab27b [4]. Being GTPases, the activation of each Rab is dependent on an influx of calcium, as is the case for Rab 11 in the K562 cell line, which may involve SNARE complexes [44–46]. Altogether, there are clearly several players within the cell that contribute to the endosomal compartment and, ultimately, to the release of exosomes, further emphasizing the importance of this pathway in normal biology. As such, it is not at all surprising that intracellular pathogens like viruses have also evolved mechanisms to incorporate their viral content at each stage of exosome formation.
Fate of Exosomes
Once in the extracellular space, exosomes can bind to neighboring cells, bind locally, travel passively through the bloodstream for a more paracrine destination, or be taken up by marginal zone phagocytes in the spleen and liver [4, 47]. Once released, they can have several fates, all of which dictate their downstream function. This can best be exemplified when analyzing the immune system and cancer cell biology, both of which have been extensively studied in the field of exosome biology. Importantly, the contents of exosomes have been shown to have activity in recipient cells [48], and are not just a means for removal of cellular waste material, as was first hypothesized, although this is still an important function [49]. First, exosomes can either be internalized or captured at the cell surface where they remain [4]. Both of these outcomes have been observed in dendritic cells [50]. Segura et al. [51] observed CD8+ dendritic cells capture exosomes via dendritic cell (DC) lymphocyte function-associated antigen 1 (LFA-1) at the surface for presentation of exosome-borne major histocompatibility complex (MHC)–peptide complexes to CD4+ T cells. These T cells could then be activated by exosomal antigens [52], a process that is much more efficient in the presence of DCs [4, 53, 54]. This process was dependent on intracellular adhesion molecule 1 (ICAM-1) expression on exosomes and is termed “cross-dressing” [55]. Another method by which DCs could capture exosomal antigens is through internalization, processing, and repackaging of endocytosed exosomal antigens into the endosomal pathway for representation on DC MHC II to naïve CD4+ T cells [50]. This process was documented in elegant experiments by Morelli et al. [50]. Activation of CD8+ T cells is also possible but requires the presence of DCs capable of “cross-presentation”, that is, internalization of exosomal antigens followed by processing and representation on MHC I. This has been documented for the activation of tumor-specific cytotoxic T lymphocytes with tumor-derived exosomes [56]. Additionally, exosomes can be taken up by phagocytosis or pinocytosis where the contents can have direct consequences on gene expression of the recipient cells [57]. For example, regulatory T cells produce exosomes with miRNA profiles that directly downregulate inflammation in recipient cells [58]. Indeed, phagocytic uptake of exosomes can occur via phosphatidylserine on the surface of the vesicles via interaction with T-cell immunoglobulin and mucin domain-containing molecule (TIM)-4 on phagocytic cells [59, 60]. It has been shown that phagocytosis of exosomes from MT4, a human T-cell lymphotropic virus type I (HTLV-1) infected cell line, was reduced with the addition of TIM-4, but not TIM-1, antibodies [61]. This is intriguing as both TIM-1 and TIM-4 are known to serve has viral entry receptors for hepatitis A virus (HAV), Ebola, and several enveloped viruses [62, 63].
Viral manipulation of Exosomal Pathway
Remembering that exosomes originate in the endosomal compartment, viruses that enter via endocytosis are likely to co-opt exosomal communication; indeed, this proves to be the case. Members of the Flaviviridae family, including important human pathogens like Dengue, West Nile virus (WNV), hepatitis C virus (HCV), and the recently pandemic Zika virus, all enter via receptor-mediated or clathrin-mediated endocytosis [31, 64, 65]. HCV, Dengue, WNV and Zika virus then enter late endosomes after “back-fusion” of ILVs with this compartment, at which point the viral genome is dumped into the cytoplasm [66, 67]. However, in the case of HCV, it is known that the viral genome can remain in ILVs and be secreted within exosomes, where they can operate as infectious particles [68, 69]. As noted in Table 1, there is very little difference in size between viruses and exosomes, making observations of infectivity from exosomes difficult to substantiate. Thus, to remove the possibility of viruses accounting for observed infections, Longatti et al. [69] utilized exosomes isolated from an HCV subgenomic replicon cell line, which lacks viral structural proteins and therefore cannot produce virions. By using a transwell assay, they showed that they were able to infect Hu7 cells after exposure to these shed exosomes without the need for direct cell–cell contact. Further, this infection was inhibited by an exosomal release inhibitor, a sphingomyelinase inhibitor. Thus far, HCV is the only member of the Flaviviridae family, known to incorporate genomic RNA into exosomes. Only hepatitis A virus (HAV), a nonenveloped picornavirus, is believed to use this mode of transmission as well [70]. However, it raises the possibility of other, yet unstudied, viruses utilizing the endosomal/exosomal system as a means for delivery of viral message to uninfected cells. Indeed, this possibility was discussed in a review by Izquierdo et al. [71] of HIV and exosomes, and first dubbed the “Trojan Horse” hypothesis by Gould et al. in 2003 [72]. Gould et al. [72] hypothesize that with the similarities between HIV assembly and egress and exosome biogenesis, HIV has evolved to co-opt the exosome system and infect cells through packaging of the viral genome [72]. It is a theory supported by observations that HIV virions are released with exosomes and have enhanced infectivity in the presence of these vesicles [73]. However, this mechanism occurred via uptake of DCs, which subsequently transferred endocytosed HIV to closely associated uninfected T cells [74]. Specifically, HIV is endocytosed via DC sign into the endocytic pathway and trafficked back to the cell surface in intact DCs for presentation to T cells. However, direct packaging of HIV genome into exosomes has not been observed. Indeed, most research suggests that HIV budding is from the plasma membrane and not from the endosomal pathway [75, 76].
Table 1.
Basic differences between exosomes and viruses
| Exosomes | Viruses | |
|---|---|---|
| Size | 30–100 nm | 2 = 0400 nm (depending on virus) |
| Shape | Uniform, cup-shaped | Variable |
| Charge | Usually lacking charge | Uniform, charged |
As mentioned, several viruses enter via the endocytic pathway. While some, like the flaviviruses, proceed through ILVs, some, like HIV, completely subvert this process and instead are closely associated with the ESCRT, lipid raft domains, and Rab GTPases that are involved in exosome trafficking [8]. For example, HIV Gag has been shown to interact with tetraspanins, especially CD63 and CD81, to aid in virion egress [77]. Human herpes virus (HHV)-6 virions have been visualized by electron microscopy in MVBs and egress by the exosomal release pathway [78]. The viral glycoprotein gB was shown to colocalize with CD63, although whether this relationship is necessary for association of HHV-6 virions and ILVs was unclear. However, HHV-6 infection dramatically increased MVB formation, indicating the endosomal/exosomal pathway as important for HHV-6 infection and assembly [78]. Although the authors did not propose a mechanism by which viral components were incorporated in exosomes, the close association of the virus with exosomes in the endosomal pathway begs the question of whether HHV-6 components are also packaged in exosomes, and requires further investigation.
Beyond interactions with tetraspanins, there are still other viruses that are capable of hitching onto the ESCRT complex to facilitate transportation of virus particles to the plasma membrane. For example, influenza A virus, respiratory syncytial virus (RSV), and certain Bunyaviruses attach to Rab11a vesicles to get to the plasma membrane for egress [8, 79–81]. Human cytomegalovirus (HCMV) is known to increase Rab27a, which, as noted earlier, is essential for MVB fusion with the plasma membrane [82]. The mechanism and ultimate change to exosome production is as yet unknown, but Rab27a could be found in association with its viral envelope [82]. HIV also interacts with Rab27a, and increases its levels, as well as those of several other components of the ESCRT machinery [8, 83–85]. This is to be expected considering the aforementioned importance of ESCRT and exosome formation in HIV assembly and egress. Herpes simplex virus 1 (HSV1) is yet another virus that interacts with Rab27a. The interaction occurred through GSSHV-UL46, a viral tegument protein, in oligodendrocytes [86]. Viral glycoproteins gH and gD also interacted with Rab27a, and the importance of this association with Rab27a was proven in this paper by a decrease in viral production with Rab27a knockdown [86]. Whether this involved a decrease in exosome production, and how important this was for the lifecycle of HSV1, was not discussed at that time.
The movement of vesicles in the endosomal pathway as they track to and from the plasma membrane provides several opportunities for viral sabotage. Thus far, we have noted that viruses can enter the endosomal pathway just by viral fusion and entry into the cell. It was also noted that some viruses can hijack members of the ESCRT and vesicular trafficking machinery, and thereby integrate viral components into exosomes, owing to both close proximity and opportunity. This is important as endosomal trafficking allows for cellular contents, such as MHC II and tetraspanins to recycle through the cell and potentially incorporate other cellular proteins for representation at the plasma membrane. Thus, this process of “back fusion” may allow the entry of viral proteins that are being processed within the cell or even are targeted for the endosomal compartment. Additionally, viruses that require proximity to the nucleus and/or endoplasmic reticulum, such as herpesviruses and other DNA viruses, will also follow this route and thereby potentially have components incorporated into exosomes at this step [31, 87]. As stated, whether this process is natural happenstance due to proximity versus direct targeting is still under investigation but will be explored via the various examples mentioned herein.
HIV
HIV, which has been noted to take advantage of several steps in exosome biogenesis, has been shown to incorporate transactivating response (TAR) RNA into exosomes [88, 89]. The uptake of exosomal TAR in recipient cells can downregulate apoptosis and is postulated to have a role in supporting HIV infection. Importantly, TAR RNA was still able to be detected in exosomes isolated from the serum of HIV-positive patients on highly active antiretroviral therapy, indicating that even with antiretroviral therapy, short transcripts remain present in these exosomes [90]. Indeed, the same group later went on to find that exosomal TAR RNA could stimulate proinflammatory cytokines in recipient cells through activation of the nuclear factor kappa b pathway [89]. In a separate study, the HIV Nef protein was found in released exosomes [91]. Later uptake of these Nef+ exosomes led to increased susceptibility of naïve T cells to HIV infection [91, 92]. Indeed, another report found that exosomes from HIV-infected cells could reactivate HIV in latently infected cells [93]. Exosomal Nef has also been shown to increase T-cell apoptosis in vitro, which may contribute to the CD4+ T-cell depletion in AIDS pathogenesis [85]. Interestingly, Nef expression in CD4+ T cells was also noted to decrease CD4 and MHC I export to released exosomes [94]. The authors postulated that this decreases the ability of CD4+ T cells to inhibit HIV infection in uninfected cells by using exosomes as decoys to soak up HIV virions. This would further explain how Nef+ exosomes enhance HIV infectivity. More recently, Luo et al. [95] dispute the incorporation of Nef into exosomes at all, despite several reports finding motifs within Nef that are necessary for exosomal incorporation [96, 97]. It is a subject that requires further investigation. Nevertheless, it is clear that HIV has evolved mechanisms to alter the cellular microenvironment to its advantage through exosomal cellular communication.
HTLV
Like HIV, there are several other viruses that also seemingly target viral RNAs and proteins for exosomal export. HTLV-1, another human retrovirus and the cause of adult T-cell leukemia and HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP), has also been shown to incorporate viral proteins into shed exosomes. Jaworski et al. [98] found that HTLV-1-infected cell lines shed exosomes containing Tax, a pleiotropic transactivating protein implicated in the immune dysregulation associated with infection [99, 100]. Tax appears to be targeted for exosome entry by ubiquitination [98, 101], which was noted earlier to be an important target for ESCRT machinery. Indeed, prior studies have shown Tax colocalization with organelles undergoing exocytosis [102, 103].
Exosomes shed from HTLV-1+ cell lines were found to also contain viral mRNA and miRNAs such as tax and hbz [98]. Additionally, exosomes shed from HTLV-1-infected cell lines showed a different cell miRNA profile, as well as a unique set of host proteins and lipids, than was seen in those shed by uninfected cell lines. In as-yet-unpublished work from our laboratory in collaboration with Dr. Kashanchi, it was further demonstrated that HTLV-1 Tax could be found in exosomes isolated from the cerebrospinal fluid of some patients with HAM/TSP, while exosomes from uninfected controls were completely negative. Additionally, cultured, unstimulated peripheral blood mononuclear cells from patients with HAM/TSP were shown to shed exosomes that contained Tax protein, as well as Tax mRNA. Unlike the cell lines, however, no detectable HBZ mRNA could be isolated from exosomes (unpublished data). This may have functional consequences as HTLV-1 is a cell-associated virus and shedding of viral antigens may contribute to the inflammatory immune response. Indeed, it has previously been shown that extracellular Tax can have damaging consequences for neurons [102, 104], although neither study specifically implicated exosomes. Once Tax protein or tax mRNA enter recipient cells, it can stimulate the production of proinflammatory cytokines, like interleukin (IL)-6 and tumor necrosis factor-α [105]. Importantly, initial results from our laboratory indicate that cells that take up these exosomes can become targets for lysis by HTLV-1-specific cytotoxic T cells.
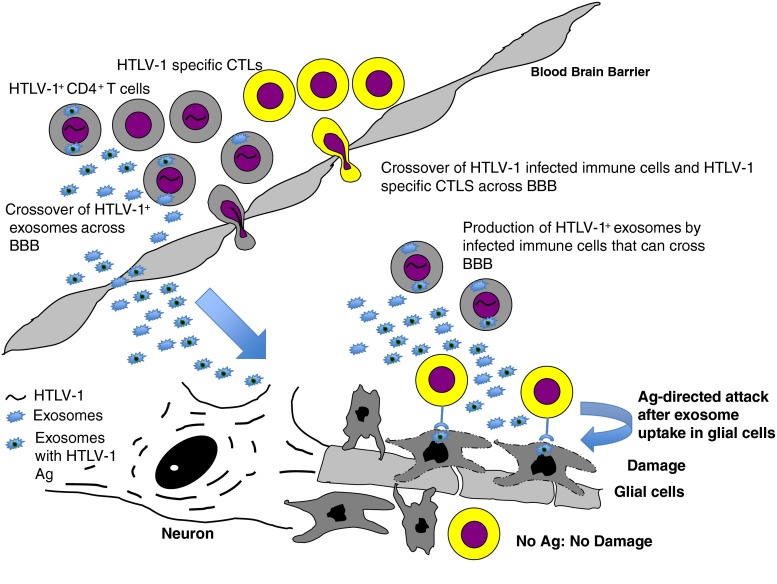
Of interest in the pathogenesis of HAM/TSP is the lack of documented infection of resident neuronal cells. While astrocytes and microglia can be infected in vitro, they have not been shown to be infected in vivo [106]. Moreover, the loss of oligodendrocytes that occurs with disease progression cannot be explained by active infection. One postulation is that the proinflamatory environment contributes to their eventual breakdown, while others have proposed direct targeting of oligodendrocytes due to a mechanism of molecular mimicry of Tax to a neuronal protein [107–109]. Exosomal Tax may therefore ultimately explain both possibilities by contributing to the inflammatory cytokine production through packaging of these cytokines, as well as induction in recipient cells (Fig. 1). Additionally, exosomal Tax uptake in uninfected cells could explain targeting by HTLV-1-specific T cells in the presence of aseptic resident neuronal cells. Clearly, further research must be undertaken to further elucidate the role of exosomes in the disease progression of HAM/TSP and potential targeting of therapeutics.
Fig. 1.
HTLV-1 Immunopathogenesis
HSV1
As mentioned, HSV1 is also known to interact with the ESCRT complex through viral tegument proteins and glycoproteins. Though this relationship with Rab27a has not yielded an observed consequence to exosomal production or content, viral proteins can also be found in exosomes shed from infected cells. HSV infection results in the release of a variety of MVs from the cell, most prominent of which are L particles, which are composed of virus envelope and tegument but lack viral genome and capsid proteins [110, 111]. They are noninfectious on their own but have been shown to increase infectivity overall possibly through the transference of factors that increase susceptibility in uninfected cells [112, 113].
In contrast, exosomes shed from HSV1-infected cells express the tetraspanins known to be enriched on exosomes, CD9, CD63, and CD81 [114]. In addition to viral transcripts, HSV1 appears to direct the incorporation of certain host products into examples. An example of this is the Stimulator of INF genes (STING) protein. It was found not only to be upregulated with HSV infection in Vero cells, but also found to be shuttled out of cells in association with CD9 [115]. The authors demonstrated that STING was packaged in exosomes and delivered to uninfected cells. It was postulated that in addition to viral miRNAs also packaged in exosomes, such as miR-H5, miR-H3, and miR-H6, these exosomes could exert a negative effect on viral spread and potentially host–host infection by increasing host survival [114]. Conversely, immediate early transcripts such as ICP27 and late transcripts like VP16 can also be found in exosomes, thereby promoting spread and latency [115]. Additionally, HSV gB has been shown to colocalize with human leukocyte antigen-DR in exosomes shed from cells [3, 116]. Shuttling of this MHC to exosomes reduced the ability of cells to present peptide to the immune system and was postulated to serve as important mechanism promoting viral latency. There is more work to be done in terms of characterizing the effects of packaging host and viral products into exosomes. More importantly, it would be of interest to determine if patients that progress to central nervous system (CNS) disease or reactivation in the CNS have different exosome profiles compared with patients that remain latently infected. Of note, a literature search did not yield research on the association of exosomes with varicella zoster virus pathogenesis, although the role of exosomes in HSV1 pathogenesis suggests that additional research into this area would be warranted.
Epstein–Barr Virus
In addition to HSV1, several other herpesviruses also influence exosomal content. As mentioned, this may be owing to the proximity of herpes virus transcription with the ESCRT pathway as other cellular products enter via “back fusion” [31, 117]. Epstein–Barr virus (EBV) and Kaposi’s sarcoma herpes virus (KSHV) have been the most studied, owing to the role of exosomes in the propogation of EBV- and KSHV-associated cancers, including nasopharyngeal sarcomas and Kaposi’s sarcoma, respectively.
Latent membrane protein 1 (LMP1) was first discovered to be exported in exosomes isolated from EBV+ cancer cells [118]. As a signal transduction protein, uptake of LMP1+ exosomes was found to inhibit natural killer cell activity and T-cell activation and proliferation [32, 119, 120]. Additionally, similar to HSV1, EBV is able to promote the incorporation of host proteins into exosomes. Galectin-9 can be found in exosomes released from EBV+ cells and can induce the apoptosis of EBV-specific T cells, signifying a method by which EBV actively avoids detection by the immune system through exosomes [23, 121]. Furthermore, epidermal growth factor and fibroblast growth factor-2, both activated in association with LMP-1-mediated transformation, are shuttled into exosomes in LMP-1+ cells [10, 122]. This may represent a mechanism by which EBV cancers alter the microenvironment to increase propagation and survival of transformed cells. Still further evidence exists for EBV promoting packaging of viral miRNAs. These miRNAs are then able to decrease target genes like CXCL11, which is an immunoregulatory gene important for antiviral activity [23]. EBV further evades immune detection by the shuttling of important immune effectors like IL-1β, IL-18, and IL-33, into exosomes and out of the cell [123]. In this way, EBV also targets exosomes as a “trash receptacle”. Taken together, all of these modulations to the exosomal pathway increase the survival and transformative abilities of EBV. Indeed, the transfer of viral antigens in the absence of active viral infection may lead to other consequences. A recent report by Baglio et al. [124] found that EBV EBER1, a viral small RNA, could be found in exosomes and that these exosomes, in turn, aberrantly activated DCs that were found in EBV-negative skin lesions of patients with lupus patients. This indicates a new potential mode of pathogenesis in autoimmune disease and other diseases where viral infection has been implicated, but a causal link has been difficult to verify. Furthermore, exosomes may serve as a potential tool for screening these affected individuals.
Another gamma herpes virus, KSHV or HHV-8, was also found to modulate the microenvironment through the packaging of viral factors in exosomes. Exosomes produced by infected cells were demonstrated to carry both KSHV and host-derived miRNA. Exposure to patient-derived exosomes increased cell migration and IL-6 production in recipient endothelial cells [125]. Additionally, like EBV, KSHV reprogrammed the cell profile of infected B cells [126]. Infection promoted a switch to glycolytic metabolism, and glycolysis by-products like pyruvate kinase and lactate dehydrogenase were packaged into exosomes [7, 127].
CMV
HHV-5, or CMV, is a betaherpesvirus. Like all of the herpes viruses, it is able to infect cells and establish latency. It is an especially important pathogen considered in transplant medicine, as CMV infection or CMV discordance between donor and recipient can lead to increased rates of organ rejection [128–130]. Previous reports have shown that infected epithelial cells can produce exosomes that stimulate allogeneic donor memory CD4+ T cells [20]. The authors proposed that this was a potential contributor to allograft rejection in transplant recipients. In addition to promoting an activated immune response, CMV infection can also increase the release of DC-SIGN on exosomes in complex with the viral glycoprotein gB [131]. DC-SIGN is a C-type lectin family member that is necessary for virus uptake [132]. It was shown that this release mediated infection of myeloid DCs by CMV and increased overall CMV infectivity [131].
HHV-6, another betaherpesvirus, has already been discussed in terms of the viral association with the endosomal pathway and MVBs. Additionally, HHV-6 was later detected to increase MHC I transfer to released exosomes in addition to viral particles [133]. MHC I downregulation is a well-known mechanism for immunoevasion employed by many classes of pathogens. This insight, gained by studying HHV-6, may point to shuttling of MHC I and MHC II to exosomes as an evolutionarily conserved mechanism that is used by many viruses.
Human Papilloma Virus
Exosome biology plays a large role in tumor pathogenesis. Thus, it is not surprising that so many oncogenic viruses have been shown to subjugate exosomal communication. Human papilloma virus (HPV) has several different serotypes, some of which are more associated with cervical cancer-like HPV type 16 and 18. In investigating patients with tumorigenic versus benign subtypes, differential miRNA content in exosomes was noted. Indeed, the miRNA profile of exosomes isolated from cells infected with pathogenic HPV strains were enriched for miRNA that controlled cell proliferation and apoptosis [134]. Although there was no evidence for the incorporation of viral oncogenes E6/E7 in released exosomes, the levels of E6/E7 were important in dictating the miRNA profile of released exosomes [8, 135]. Owing to this discrepancy in the profile of exosomes shed from oncogenic versus benign strains, there is a clinical trial currently underway at the National Institutes of Health to investigate the utility of screening salivary exosomes in patients at risk for HPV oropharyngeal carcinoma (https://clinicaltrials.gov/ct2/show/NCT02147418). Indeed, the importance of exosomes has been reinforced by a recent study in which normal cells were immortalized after incubation with exosomes derived from breast cancer cells [136].
HAV
HAV is a nonenveloped picorna virus that usually causes a mild gastrointestinal illness but which can, at times, lead to hepatitis with full clearance of the virus after infection. Interestingly, HAV has been shown to hijack endosomal membranes for encapsulation upon release [137]. These enveloped viruses are fully infectious and aid HAV in immunoevasion as they are protected from antibody neutralization [138]. Although envelopment of previously naked virus particles is different to the strategy taken by HCV, which incorporates naked viral genome into exosomes, both HAV and HCV co-opt the exosomal system for evasion from the adaptive arm of the immune system. Indeed, hepatitis B virus, which is a hepadnavirus, also hijacks exosomal communication. On HBV infection, cellular release of MVs is dramatically increased. However, these MVs are characterized as subviral particles and contain viral surface antigens but no viral genome and are therefore noninfectious [139]. The subviral particles can, however, serve as decoys to the immune system as they are able to absorb antibodies that might otherwise inhibit viral particles [32].
Bunyaviruses
Bunyaviridae is a family of enveloped, negative-stranded viruses that includes the hantavirus, nairovirus, orthobunyavirus, phlebovirus, and tospovirus genera. Of these, hantavirus and phlebovirus have clinical significance as human pathogens, including hanta pulmonary virus and Rift Valley fever virus (RVFV), respectively. Interestingly, recent reports suggest that the phlebovirus family can modulate the immune system via exosomes. Exosomes isolated from cells infected with RVFV not only contained viral RNA and proteins, but also immune cells exposed to these exosomes underwent apoptosis [140]. This suggests a mechanism for immune persistence early in the disease, as exosomes were detected prior to virion release [140]. Another phelebovirus, a newly recognized virus called severe fever with thrombocytopenia syndrome virus, also utilizes exosomes. Severe fever with thrombocytopenia syndrome virus was found to package virions within CD63+ extracellular vesicles (exosomes), which allowed for efficient receptor-independent uptake by neighboring cells [141]. Of note, pheleboviruses also have DC-SIGN as a receptor [142] , which has been shown to be packaged into exosomes for uptake in uninfected cells by CMV [131]. Further investigation should be undertaken to observe if a similar mechanism for viral spread is employed by phleboviruses and bunyaviruses in general. There is currently no literature describing hantaviruses and exosomes, although this topic obviously warrants further investigation for the role of extracellular vesicles in Hanta pulmonary virus syndrome.
Discussion
As can be seen by the wide variety of viruses discussed in this review, there are several different viruses spread across different genera that take advantage of exosomal communication. While some cloak viral antigens to aid in viral spread, others increase shuttling of disadvantageous host products that would hinder viral infection into exosomes. Others utilize exosomes as decoys to the immune system and, counterintuitively, some viruses also seem to prime a directed immune response to inhibit spread. The examples presented by these viruses illustrate the many ways exosomal communication is important for immune function and maintenance of the cellular microenvironment. The one unifying factor is that all of the viruses present, except for HAV and the phleboviruses, are able to establish latency in the host. Thus, the question becomes: Does their ability to manipulate exosomal contents allow these viruses to establish latency, or does long-term infection favor the ability to isolate exosomes while transient infections have been largely ignored due to the belief that immune clearance negates the risk of exosomes? Indeed, the example of RVFV indicates that exosomes may play an early role in the viral spread of transient infections. Of note, the line between latency and transient infection is becoming blurred in the cases of Zika and Ebola, which have shown a remarkable ability to reappear in previously convalescent patients. Furthermore, the examples in this review highlight the ability of exosomes to increase not only viral spread, but also the type of cells that can be infected. This becomes an important consideration as we attempt to understand how viruses are able to establish and maintain viral reservoirs and “pockets of infection” in cells not normally believed to be permissive.
Ebola, chikungunya virus, avian flu, and Zika virus are just a few of the new and re-emerging viruses that are characterized by transient infection. However, in the cases of Ebola and Zika virus, scientists are discovering that virus and viral proteins can still be isolated months after the initial infection from immune privileged sites like the eye and semen [143–145]. All of these viruses pose serious health threats to the human population, and both Zika and Ebola have been of concern owing to increasing evidence of CNS disease [146–148]. Thus, an understanding of how these agents persist in these spaces and cause damage is imperative. As noted in this review, exosomes are a potential source of antigen that can easily cross the endothelial barriers protecting immune privileged sites. Additionally, in the case of Zika virus, which is a flavivirus, there is already precedence for other members of this virus family altering exosomal contents. Therefore, there is a high likelihood that this ability to incorporate viral contents into exosomes is a shared mechanism for immune evasion amongst the entire family, and warrants investigation. Considering the troubling consequences of Zika infection in pregnancy, screening for exosomes in prospective mothers might be a useful tool for evaluation of risks to the fetus. This is an attractive prospect as the ability to detect Zika virus by reverse transcription polymerase chain reaction is optimal 5–7 days after symptom onset and while the patient is still viremic (http://www.cdc.gov/zika/hc-providers/qa-pregnant-women.html). Additional testing involves detection of IgM; however, there is cross-reactivity with other flaviviruses like Dengue virus and WNV, and therefore it is not specific. A method that targets particles, such as exosomes, that can cross the placenta and that could still be detected after the window of viremia would be useful. Exosomes represent a potential biomarker that can be used in this way. Furthermore, exosome analysis may prove to be important in understanding Ebola pathophysiology as Alix, the ESCRT protein important in directing proteins to endosomes, is necessary for viral budding [149].
Overall, exosomes represent an exciting new avenue with which to explore in viral pathology, one that current evidence suggests plays a role in both transient and latent virus infection. The possibility of screening exosomes in viral disease presents a noninvasive technique for the management and treatment of patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
Acknowledgments
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Trams EG, Lauter CJ, Salem N, Jr, Heine U. Exfoliation of membrane ecto-enzymes in the form of micro-vesicles. Biochim Biophys Acta. 1981;645(1):63–70. doi: 10.1016/0005-2736(81)90512-5. [DOI] [PubMed] [Google Scholar]
- 2.Johnstone RM, Bianchini A, Teng K. Reticulocyte maturation and exosome release: transferrin receptor containing exosomes shows multiple plasma membrane functions. Blood. 1989;74(5):1844–1851. [PubMed] [Google Scholar]
- 3.Lai FW, Lichty BD, Bowdish DM. Microvesicles: ubiquitous contributors to infection and immunity. J Leukoc Biol. 2015;97(2):237–245. doi: 10.1189/jlb.3RU0513-292RR. [DOI] [PubMed] [Google Scholar]
- 4.Robbins PD, Morelli AE. Regulation of immune responses by extracellular vesicles. Nat Rev Immunol. 2014;14(3):195–208. doi: 10.1038/nri3622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Pol E, Boing AN, Harrison P, Sturk A, Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol Rev. 2012;64(3):676–705. doi: 10.1124/pr.112.005983. [DOI] [PubMed] [Google Scholar]
- 6.van Dongen HM, Masoumi N, Witwer KW, Pegtel DM. Extracellular vesicles exploit viral entry routes for cargo delivery. Microbiol Mol Biol Rev. 2016;80(2):369–386. doi: 10.1128/MMBR.00063-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwab A, Meyering SS, Lepene B, et al. Extracellular vesicles from infected cells: potential for direct pathogenesis. Front Microbiol. 2015;6:1132. doi: 10.3389/fmicb.2015.01132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alenquer M, Amorim MJ. Exosome biogenesis, regulation, and function in viral infection. Viruses. 2015;7(9):5066–5083. doi: 10.3390/v7092862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chahar HS, Bao X, Casola A. Exosomes and their role in the life cycle and pathogenesis of RNA viruses. Viruses. 2015;7(6):3204–3225. doi: 10.3390/v7062770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meckes DG., Jr Exosomal communication goes viral. J Virol. 2015;89(10):5200–5203. doi: 10.1128/JVI.02470-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wurdinger T, Gatson NN, Balaj L, Kaur B, Breakefield XO, Pegtel DM. Extracellular vesicles and their convergence with viral pathways. Adv Virol. 2012;2012:767694. doi: 10.1155/2012/767694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li XB, Zhang ZR, Schluesener HJ, Xu SQ. Role of exosomes in immune regulation. J Cell Mol Med. 2006;10(2):364–375. doi: 10.1111/j.1582-4934.2006.tb00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blanchard N, Lankar D, Faure F, et al. TCR activation of human T cells induces the production of exosomes bearing the TCR/CD3/zeta complex. J Immunol. 2002;168(7):3235–3241. doi: 10.4049/jimmunol.168.7.3235. [DOI] [PubMed] [Google Scholar]
- 14.Raposo G, Nijman HW, Stoorvogel W, et al. B lymphocytes secrete antigen-presenting vesicles. J Exp Med. 1996;183(3):1161–1172. doi: 10.1084/jem.183.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Escola JM, Kleijmeer MJ, Stoorvogel W, Griffith JM, Yoshie O, Geuze HJ. Selective enrichment of tetraspan proteins on the internal vesicles of multivesicular endosomes and on exosomes secreted by human B-lymphocytes. J Biol Chem. 1998;273(32):20121–20127. doi: 10.1074/jbc.273.32.20121. [DOI] [PubMed] [Google Scholar]
- 16.Thery C, Regnault A, Garin J. P et al. Molecular characterization of dendritic cell-derived exosomes. Selective accumulation of the heat shock protein hsc73. J Cell Biol. 1999;147(3):599–610. doi: 10.1083/jcb.147.3.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faure J, Lachenal G, Court M, et al. Exosomes are released by cultured cortical neurones. Mol Cell Neurosci. 2006;31(4):642–648. doi: 10.1016/j.mcn.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Basso M, Bonetto V. Extracellular vesicles and a novel form of communication in the brain. Front Neurosci. 2016;10:127. doi: 10.3389/fnins.2016.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang G, Dinkins M, He Q, et al. Astrocytes secrete exosomes enriched with proapoptotic ceramide and prostate apoptosis response 4 (PAR-4): potential mechanism of apoptosis induction in Alzheimer disease (AD) J Biol Chem. 2012;287(25):21384–21395. doi: 10.1074/jbc.M112.340513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walker JD, Maier CL, Pober JS. Cytomegalovirus-infected human endothelial cells can stimulate allogeneic CD4+ memory T cells by releasing antigenic exosomes. J Immunol. 2009;182(3):1548–1559. doi: 10.4049/jimmunol.182.3.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Comelli L, Rocchiccioli S, Smirni S, et al. Characterization of secreted vesicles from vascular smooth muscle cells. Mol Biosyst. 2014;10(5):1146–1152. doi: 10.1039/c3mb70544g. [DOI] [PubMed] [Google Scholar]
- 22.Kramer-Albers EM, Bretz N, Tenzer S, et al. Oligodendrocytes secrete exosomes containing major myelin and stress-protective proteins: Trophic support for axons? Proteomics Clin Appl. 2007;1(11):1446–1461. doi: 10.1002/prca.200700522. [DOI] [PubMed] [Google Scholar]
- 23.Schorey JS, Cheng Y, Singh PP, Smith VL. Exosomes and other extracellular vesicles in host-pathogen interactions. EMBO Rep. 2015;16(1):24–43. doi: 10.15252/embr.201439363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boukouris S, Mathivanan S. Exosomes in bodily fluids are a highly stable resource of disease biomarkers. Proteomics Clin Appl. 2015;9(3-4):358–367. doi: 10.1002/prca.201400114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang T, Martin P, Fogarty B, et al. Exosome delivered anticancer drugs across the blood-brain barrier for brain cancer therapy in Danio rerio. Pharm Res. 2015;32(6):2003–2014. doi: 10.1007/s11095-014-1593-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El Andaloussi S, Lakhal S, Mager I, Wood MJ. Exosomes for targeted siRNA delivery across biological barriers. Adv Drug Deliv Rev. 2013;65(3):391–397. doi: 10.1016/j.addr.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 27.Murk JL, Stoorvogel W, Kleijmeer MJ, Geuze HJ. The plasticity of multivesicular bodies and the regulation of antigen presentation. Semin Cell Develop Biol. 2002;13(4):303–311. doi: 10.1016/S1084952102000605. [DOI] [PubMed] [Google Scholar]
- 28.Bissig C, Gruenberg J. ALIX and the multivesicular endosome: ALIX in Wonderland. Trends Cell Biol. 2014;24(1):19–25. doi: 10.1016/j.tcb.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 29.Pegtel DM, van de Garde MD, Middeldorp JM. Viral miRNAs exploiting the endosomal-exosomal pathway for intercellular cross-talk and immune evasion. Biochim Biophys Acta. 2011;1809(11-12):715–721. doi: 10.1016/j.bbagrm.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 30.Matsuo H, Chevallier J, Mayran N, et al. Role of LBPA and Alix in multivesicular liposome formation and endosome organization. Science. 2004;303(5657):531–534. doi: 10.1126/science.1092425. [DOI] [PubMed] [Google Scholar]
- 31.Nour AM, Modis Y. Endosomal vesicles as vehicles for viral genomes. Trends Cell Biol. 2014;24(8):449–454. doi: 10.1016/j.tcb.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meckes DG, Jr, Raab-Traub N. Microvesicles and viral infection. J Virol. 2011;85(24):12844–12854. doi: 10.1128/JVI.05853-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gan X, Gould SJ. Identification of an inhibitory budding signal that blocks the release of HIV particles and exosome/microvesicle proteins. Mol Biol Cell. 2011;22(6):817–830. doi: 10.1091/mbc.E10-07-0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sampey GC, Meyering SS, Asad Zadeh M, Saifuddin M, Hakami RM, Kashanchi F. Exosomes and their role in CNS viral infections. J Neurovirol. 2014;20(3):199–208. doi: 10.1007/s13365-014-0238-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalra H, Simpson RJ, Ji H, et al. Vesiclepedia: a compendium for extracellular vesicles with continuous community annotation. PLoS Biol. 2012;10(12) doi: 10.1371/journal.pbio.1001450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim DK, Kang B, Kim OY, et al. EVpedia: an integrated database of high-throughput data for systemic analyses of extracellular vesicles. J Extracell Vesicles 2013;2. [DOI] [PMC free article] [PubMed]
- 37.Trajkovic K, Hsu C, Chiantia S, et al. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319(5867):1244–1247. doi: 10.1126/science.1153124. [DOI] [PubMed] [Google Scholar]
- 38.van Niel G, Charrin S, Simoes S, et al. The tetraspanin CD63 regulates ESCRT-independent and -dependent endosomal sorting during melanogenesis. Develop Cell. 2011;21(4):708–721. doi: 10.1016/j.devcel.2011.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perez-Hernandez D, Gutierrez-Vazquez C, Jorge I, et al. The intracellular interactome of tetraspanin-enriched microdomains reveals their function as sorting machineries toward exosomes. J Biol Chem. 2013;288(17):11649–11661. doi: 10.1074/jbc.M112.445304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stuffers S, Sem Wegner C, Stenmark H, Brech A. Multivesicular endosome biogenesis in the absence of ESCRTs. Traffic. 2009;10(7):925–937. doi: 10.1111/j.1600-0854.2009.00920.x. [DOI] [PubMed] [Google Scholar]
- 41.Tamai K, Tanaka N, Nakano T, et al. Exosome secretion of dendritic cells is regulated by Hrs, an ESCRT-0 protein. Biochem Biophys Res Commun. 2010;399(3):384–390. doi: 10.1016/j.bbrc.2010.07.083. [DOI] [PubMed] [Google Scholar]
- 42.Schwartz SL, Cao C, Pylypenko O, Rak A, Wandinger-Ness A. Rab GTPases at a glance. J Cell Sci. 2007;120(Pt 22):3905–3910. doi: 10.1242/jcs.015909. [DOI] [PubMed] [Google Scholar]
- 43.Ostrowski M, Carmo NB, Krumeich S, et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat Cell Biol. 2010;12(1):19–30. doi: 10.1038/ncb2000. [DOI] [PubMed] [Google Scholar]
- 44.Savina A, Fader CM, Damiani MT, Colombo MI. Rab11 promotes docking and fusion of multivesicular bodies in a calcium-dependent manner. Traffic. 2005;6(2):131–143. doi: 10.1111/j.1600-0854.2004.00257.x. [DOI] [PubMed] [Google Scholar]
- 45.Colombo M, Raposo G, Thery C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu Rev Cell Develop Biol. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 46.Fader CM, Sanchez DG, Mestre MB, Colombo MI. TI-VAMP/VAMP7 and VAMP3/cellubrevin: two v-SNARE proteins involved in specific steps of the autophagy/multivesicular body pathways. Biochim Biophys Acta. 2009;1793(12):1901–1916. doi: 10.1016/j.bbamcr.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 47.Montecalvo A, Shufesky WJ, Stolz DB, et al. Exosomes as a short-range mechanism to spread alloantigen between dendritic cells during T cell allorecognition. J Immunol. 2008;180(5):3081–3090. doi: 10.4049/jimmunol.180.5.3081. [DOI] [PubMed] [Google Scholar]
- 48.Lagana A, Russo F, Veneziano D, et al. Extracellular circulating viral microRNAs: current knowledge and perspectives. Front Genet. 2013;4:120. doi: 10.3389/fgene.2013.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thebaud B, Stewart DJ. Exosomes: cell garbage can, therapeutic carrier, or trojan horse? Circulation. 2012;126(22):2553–2555. doi: 10.1161/CIRCULATIONAHA.112.146738. [DOI] [PubMed] [Google Scholar]
- 50.Morelli AE, Larregina AT, Shufesky WJ, et al. Endocytosis, intracellular sorting, and processing of exosomes by dendritic cells. Blood. 2004;104(10):3257–3266. doi: 10.1182/blood-2004-03-0824. [DOI] [PubMed] [Google Scholar]
- 51.Segura E, Guerin C, Hogg N, Amigorena S, Thery C. CD8+ dendritic cells use LFA-1 to capture MHC-peptide complexes from exosomes in vivo. J Immunol. 2007;179(3):1489–1496. doi: 10.4049/jimmunol.179.3.1489. [DOI] [PubMed] [Google Scholar]
- 52.Thery C, Duban L, Segura E, Veron P, Lantz O, Amigorena S. Indirect activation of naive CD4+ T cells by dendritic cell-derived exosomes. Nat Immunol. 2002;3(12):1156–1162. doi: 10.1038/ni854. [DOI] [PubMed] [Google Scholar]
- 53.Vincent-Schneider H, Stumptner-Cuvelette P, Lankar D, et al. Exosomes bearing HLA-DR1 molecules need dendritic cells to efficiently stimulate specific T cells. Int Immunol. 2002;14(7):713–722. doi: 10.1093/intimm/dxf048. [DOI] [PubMed] [Google Scholar]
- 54.Admyre C, Johansson SM, Paulie S, Gabrielsson S. Direct exosome stimulation of peripheral human T cells detected by ELISPOT. Eur J Immunol. 2006;36(7):1772–1781. doi: 10.1002/eji.200535615. [DOI] [PubMed] [Google Scholar]
- 55.Segura E, Nicco C, Lombard B, et al. ICAM-1 on exosomes from mature dendritic cells is critical for efficient naive T-cell priming. Blood. 2005;106(1):216–223. doi: 10.1182/blood-2005-01-0220. [DOI] [PubMed] [Google Scholar]
- 56.Wolfers J, Lozier A, Raposo G, et al. Tumor-derived exosomes are a source of shared tumor rejection antigens for CTL cross-priming. Nat Med. 2001;7(3):297–303. doi: 10.1038/85438. [DOI] [PubMed] [Google Scholar]
- 57.Mulcahy LA, Pink RC, Carter DR. Routes and mechanisms of extracellular vesicle uptake. J Extracell Vesicles 2014;3. [DOI] [PMC free article] [PubMed]
- 58.Okoye IS, Coomes SM, Pelly VS, et al. MicroRNA-containing T-regulatory-cell-derived exosomes suppress pathogenic T helper 1 cells. Immunity. 2014;41(1):89–103. doi: 10.1016/j.immuni.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zakharova L, Svetlova M, Fomina AF. T cell exosomes induce cholesterol accumulation in human monocytes via phosphatidylserine receptor. J Cell Physiol. 2007;212(1):174–181. doi: 10.1002/jcp.21013. [DOI] [PubMed] [Google Scholar]
- 60.Miyanishi M, Tada K, Koike M, Uchiyama Y, Kitamura T, Nagata S. Identification of Tim4 as a phosphatidylserine receptor. Nature. 2007;450(7168):435–439. doi: 10.1038/nature06307. [DOI] [PubMed] [Google Scholar]
- 61.Feng D, Zhao WL, Ye YY, et al. Cellular internalization of exosomes occurs through phagocytosis. Traffic. 2010;11(5):675–687. doi: 10.1111/j.1600-0854.2010.01041.x. [DOI] [PubMed] [Google Scholar]
- 62.Moller-Tank S, Maury W. Phosphatidylserine receptors: enhancers of enveloped virus entry and infection. Virology. 2014;468-470:565–80. doi: 10.1016/j.virol.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rhein BA, Brouillette RB, Schaack GA, Chiorini JA, Maury W. Characterization of human and murine T-cell immunoglobulin mucin domain 4 (TIM-4) IgV domain residues critical for Ebola virus entry. J Virol 2016 Apr 27. [DOI] [PMC free article] [PubMed]
- 64.Smit JM, Moesker B, Rodenhuis-Zybert I, Wilschut J. Flavivirus cell entry and membrane fusion. Viruses. 2011;3(2):160–171. doi: 10.3390/v3020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hamel R, Dejarnac O, Wichit S, et al. Biology of Zika virus infection in human skin cells. J Virol. 2015;89(17):8880–8896. doi: 10.1128/JVI.00354-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Nour AM, Li Y, Wolenski J, Modis Y. Viral membrane fusion and nucleocapsid delivery into the cytoplasm are distinct events in some flaviviruses. PLoS Pathog. 2013;9(9) doi: 10.1371/journal.ppat.1003585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cohen FS. How viruses invade cells. Biophys J. 2016;110(5):1028–1032. doi: 10.1016/j.bpj.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ramakrishnaiah V, Thumann C, Fofana I, et al. Exosome-mediated transmission of hepatitis C virus between human hepatoma Huh7.5 cells. Proc Natl Acad Sci U S A. 2013;110(32):13109–13113. doi: 10.1073/pnas.1221899110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Longatti A, Boyd B, Chisari FV. Virion-independent transfer of replication-competent hepatitis C virus RNA between permissive cells. J Virol. 2015;89(5):2956–2961. doi: 10.1128/JVI.02721-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Longatti A. The dual role of exosomes in hepatitis A and C virus transmission and viral immune activation. Viruses. 2015;7(12):6707–6715. doi: 10.3390/v7122967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Izquierdo-Useros N, Naranjo-Gomez M, Erkizia I, et al. HIV and mature dendritic cells: Trojan exosomes riding the Trojan horse? PLoS Pathog. 2010;6(3) doi: 10.1371/journal.ppat.1000740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gould SJ, Booth AM, Hildreth JE. The Trojan exosome hypothesis. Proc Natl Acad Sci U S A. 2003;100(19):10592–10597. doi: 10.1073/pnas.1831413100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wiley RD, Gummuluru S. Immature dendritic cell-derived exosomes can mediate HIV-1 trans infection. Proc Natl Acad Sci U S A. 2006;103(3):738–743. doi: 10.1073/pnas.0507995103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Piguet V, Steinman RM. The interaction of HIV with dendritic cells: outcomes and pathways. Trends Immunol. 2007;28(11):503–510. doi: 10.1016/j.it.2007.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yandrapalli N, Muriaux D, Favard C. Lipid domains in HIV-1 assembly. Front Microbiol. 2014;5:220. doi: 10.3389/fmicb.2014.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Woodward CL, Cheng SN, Jensen GJ. Electron cryotomography studies of maturing HIV-1 particles reveal the assembly pathway of the viral core. J Virol. 2015;89(2):1267–1277. doi: 10.1128/JVI.02997-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Madison MN, Okeoma CM. Exosomes: implications in HIV-1 pathogenesis. Viruses. 2015;7(7):4093–4118. doi: 10.3390/v7072810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mori Y, Koike M, Moriishi E, et al. Human herpesvirus-6 induces MVB formation, and virus egress occurs by an exosomal release pathway. Traffic. 2008;9(10):1728–1742. doi: 10.1111/j.1600-0854.2008.00796.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bruce EA, Digard P, Stuart AD. The Rab11 pathway is required for influenza A virus budding and filament formation. J Virol. 2010;84(12):5848–5859. doi: 10.1128/JVI.00307-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rowe RK, Suszko JW, Pekosz A. Roles for the recycling endosome, Rab8, and Rab11 in hantavirus release from epithelial cells. Virology. 2008;382(2):239–249. doi: 10.1016/j.virol.2008.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Utley TJ, Ducharme NA, Varthakavi V, et al. Respiratory syncytial virus uses a Vps4-independent budding mechanism controlled by Rab11-FIP2. Proc Natl Acad Sci U S A. 2008;105(29):10209–10214. doi: 10.1073/pnas.0712144105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fraile-Ramos A, Cepeda V, Elstak E, van der Sluijs P. Rab27a is required for human cytomegalovirus assembly. PLoS One. 2010;5(12) doi: 10.1371/journal.pone.0015318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gerber PP, Cabrini M, Jancic C, et al. Rab27a controls HIV-1 assembly by regulating plasma membrane levels of phosphatidylinositol 4,5-bisphosphate. J Cell Biol. 2015;209(3):435–452. doi: 10.1083/jcb.201409082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Meng B, Ip NC, Prestwood LJ, Abbink TE, Lever AM. Evidence that the endosomal sorting complex required for transport-II (ESCRT-II) is required for efficient human immunodeficiency virus-1 (HIV-1) production. Retrovirology. 2015;12:72. doi: 10.1186/s12977-015-0197-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lenassi M, Cagney G, Liao M, et al. HIV Nef is secreted in exosomes and triggers apoptosis in bystander CD4+ T cells. Traffic. 2010;11(1):110–122. doi: 10.1111/j.1600-0854.2009.01006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bello-Morales R, Crespillo AJ, Fraile-Ramos A, Tabares E, Alcina A, Lopez-Guerrero JA. Role of the small GTPase Rab27a during herpes simplex virus infection of oligodendrocytic cells. BMC Microbiol. 2012;12:265. doi: 10.1186/1471-2180-12-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Krummenacher C, Carfi A, Eisenberg RJ, Cohen GH. Entry of herpesviruses into cells: the enigma variations. Adv Exp Med Biol. 2013;790:178–195. doi: 10.1007/978-1-4614-7651-1_10. [DOI] [PubMed] [Google Scholar]
- 88.Narayanan A, Iordanskiy S, Das R, et al. Exosomes derived from HIV-1-infected cells contain trans-activation response element RNA. J Biol Chem. 2013;288(27):20014–20033. doi: 10.1074/jbc.M112.438895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sampey GC, Saifuddin M, Schwab A, et al. Exosomes from HIV-1-infected cells stimulate production of pro-inflammatory cytokines through trans-activating response (TAR) RNA. J Biol Chem. 2016;291(3):1251–1266. doi: 10.1074/jbc.M115.662171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jaworski E, Saifuddin M, Sampey G, et al. The use of Nanotrap particles technology in capturing HIV-1 virions and viral proteins from infected cells. PLoS One. 2014;9(5) doi: 10.1371/journal.pone.0096778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Campbell TD, Khan M, Huang MB, Bond VC, Powell MD. HIV-1 Nef protein is secreted into vesicles that can fuse with target cells and virions. Ethn Dis. 2008;18(2 Suppl. 2):S2-14-9. [PMC free article] [PubMed] [Google Scholar]
- 92.Arenaccio C, Chiozzini C, Columba-Cabezas S, et al. Exosomes from human immunodeficiency virus type 1 (HIV-1)-infected cells license quiescent CD4+ T lymphocytes to replicate HIV-1 through a Nef- and ADAM17-dependent mechanism. J Virol. 2014;88(19):11529–11539. doi: 10.1128/JVI.01712-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Arenaccio C, Anticoli S, Manfredi F, Chiozzini C, Olivetta E, Federico M. Latent HIV-1 is activated by exosomes from cells infected with either replication-competent or defective HIV-1. Retrovirology. 2015;12:87. doi: 10.1186/s12977-015-0216-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.de Carvalho JV, de Castro RO, da Silva EZ, et al. Nef neutralizes the ability of exosomes from CD4+ T cells to act as decoys during HIV-1 infection. PLoS One. 2014;9(11) doi: 10.1371/journal.pone.0113691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Luo X, Fan Y, Park IW, He JJ. Exosomes are unlikely involved in intercellular Nef transfer. PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0124436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ali SA, Huang MB, Campbell PE, et al. Genetic characterization of HIV type 1 Nef-induced vesicle secretion. AIDS Res Hum Retroviruses. 2010;26(2):173–192. doi: 10.1089/aid.2009.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Campbell PE, Isayev O, Ali SA, et al. Validation of a novel secretion modification region (SMR) of HIV-1 Nef using cohort sequence analysis and molecular modeling. J Mol Model. 2012;18(10):4603–4613. doi: 10.1007/s00894-012-1452-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jaworski E, Narayanan A, Van Duyne R, et al. Human T-lymphotropic virus type 1-infected cells secrete exosomes that contain Tax protein. J Biol Chem. 2014;289(32):22284–22305. doi: 10.1074/jbc.M114.549659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Romanelli MG, Diani E, Bergamo E, et al. Highlights on distinctive structural and functional properties of HTLV Tax proteins. Front Microbiol. 2013;4:271. doi: 10.3389/fmicb.2013.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Currer R, Van Duyne R, Jaworski E, et al. HTLV tax: a fascinating multifunctional co-regulator of viral and cellular pathways. Front Microbiol. 2012;3:406. doi: 10.3389/fmicb.2012.00406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shembade N, Harhaj EW. Role of post-translational modifications of HTLV-1 Tax in NF-kappaB activation. World J Biol Chem. 2010;1(1):13–20. doi: 10.4331/wjbc.v1.i1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Alefantis T, Mostoller K, Jain P, Harhaj E, Grant C, Wigdahl B. Secretion of the human T cell leukemia virus type I transactivator protein tax. J Biol Chem. 2005;280(17):17353–17362. doi: 10.1074/jbc.M409851200. [DOI] [PubMed] [Google Scholar]
- 103.Alefantis T, Jain P, Ahuja J, Mostoller K, Wigdahl B. HTLV-1 Tax nucleocytoplasmic shuttling, interaction with the secretory pathway, extracellular signaling, and implications for neurologic disease. J Biomed Sci. 2005;12(6):961–974. doi: 10.1007/s11373-005-9026-x. [DOI] [PubMed] [Google Scholar]
- 104.Cowan EP, Alexander RK, Daniel S, Kashanchi F, Brady JN. Induction of tumor necrosis factor alpha in human neuronal cells by extracellular human T-cell lymphotropic virus type 1 Tax. J Virol. 1997;71(9):6982–6989. doi: 10.1128/jvi.71.9.6982-6989.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dhib-Jalbut S, Hoffman PM, Yamabe T, et al. Extracellular human T-cell lymphotropic virus type I Tax protein induces cytokine production in adult human microglial cells. Ann Neurol. 1994;36(5):787–790. doi: 10.1002/ana.410360516. [DOI] [PubMed] [Google Scholar]
- 106.Lepoutre V, Jain P, Quann K, Wigdahl B, Khan ZK. Role of resident CNS cell populations in HTLV-1-associated neuroinflammatory disease. Front Biosci. 2009;14:1152–1168. doi: 10.2741/3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kubota R, Nagai M, Kawanishi T, Osame M, Jacobson S. Increased HTLV type 1 tax specific CD8+ cells in HTLV type 1-asociated myelopathy/tropical spastic paraparesis: correlation with HTLV type 1 proviral load. AIDS Res Hum Retroviruses. 2000;16(16):1705–1709. doi: 10.1089/08892220050193182. [DOI] [PubMed] [Google Scholar]
- 108.Levin MC, Lee SM, Morcos Y, Brady J, Stuart J. Cross-reactivity between immunodominant human T lymphotropic virus type I tax and neurons: implications for molecular mimicry. J Infect Dis. 2002;186(10):1514–1517. doi: 10.1086/344734. [DOI] [PubMed] [Google Scholar]
- 109.Irish BP, Khan ZK, Jain P, et al. Molecular mechanisms of neurodegenerative diseases induced by human retroviruses: a review. Am J Infect Dis. 2009;5(3):231–258. doi: 10.3844/ajidsp.2009.231.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rixon FJ, Addison C, McLauchlan J. Assembly of enveloped tegument structures (L particles) can occur independently of virion maturation in herpes simplex virus type 1-infected cells. J Gen Virol. 1992;73(Pt 2):277–284. doi: 10.1099/0022-1317-73-2-277. [DOI] [PubMed] [Google Scholar]
- 111.McLauchlan J, Rixon FJ. Characterization of enveloped tegument structures (L particles) produced by alphaherpesviruses: integrity of the tegument does not depend on the presence of capsid or envelope. J Gen Virol. 1992;73(Pt 2):269–276. doi: 10.1099/0022-1317-73-2-269. [DOI] [PubMed] [Google Scholar]
- 112.McLauchlan J, Addison C, Craigie MC, Rixon FJ. Noninfectious L-particles supply functions which can facilitate infection by HSV-1. Virology. 1992;190(2):682–688. doi: 10.1016/0042-6822(92)90906-6. [DOI] [PubMed] [Google Scholar]
- 113.Heilingloh CS, Kummer M, Muhl-Zurbes P, et al. L particles transmit viral proteins from herpes simplex virus 1-infected mature dendritic cells to uninfected bystander cells, inducing CD83 downmodulation. J Virol. 2015;89(21):11046–11055. doi: 10.1128/JVI.01517-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kalamvoki M, Deschamps T. Extracellular vesicles during Herpes Simplex Virus type 1 infection: an inquire. Virol J. 2016;13(1):63. doi: 10.1186/s12985-016-0518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kalamvoki M, Du T, Roizman B. Cells infected with herpes simplex virus 1 export to uninfected cells exosomes containing STING, viral mRNAs, and microRNAs. Proc Natl Acad Sci U S A. 2014;111(46):E4991–E4996. doi: 10.1073/pnas.1419338111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Temme S, Eis-Hubinger AM, McLellan AD, Koch N. The herpes simplex virus-1 encoded glycoprotein B diverts HLA-DR into the exosome pathway. J Immunol. 2010;184(1):236–243. doi: 10.4049/jimmunol.0902192. [DOI] [PubMed] [Google Scholar]
- 117.Lee CP, Liu PT, Kung HN, et al. The ESCRT machinery is recruited by the viral BFRF1 protein to the nucleus-associated membrane for the maturation of Epstein-Barr Virus. PLoS Pathog. 2012;8(9) doi: 10.1371/journal.ppat.1002904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Flanagan J, Middeldorp J, Sculley T. Localization of the Epstein-Barr virus protein LMP 1 to exosomes. J Gen Virol. 2003;84(Pt 7):1871–1879. doi: 10.1099/vir.0.18944-0. [DOI] [PubMed] [Google Scholar]
- 119.Dukers DF, Meij P, Vervoort MB, et al. Direct immunosuppressive effects of EBV-encoded latent membrane protein 1. J Immunol. 2000;165(2):663–670. doi: 10.4049/jimmunol.165.2.663. [DOI] [PubMed] [Google Scholar]
- 120.Nanbo A, Kawanishi E, Yoshida R, Yoshiyama H. Exosomes derived from Epstein-Barr virus-infected cells are internalized via caveola-dependent endocytosis and promote phenotypic modulation in target cells. J Virol. 2013;87(18):10334–10347. doi: 10.1128/JVI.01310-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Klibi J, Niki T, Riedel A, et al. Blood diffusion and Th1-suppressive effects of galectin-9-containing exosomes released by Epstein-Barr virus-infected nasopharyngeal carcinoma cells. Blood. 2009;113(9):1957–1966. doi: 10.1182/blood-2008-02-142596. [DOI] [PubMed] [Google Scholar]
- 122.Meckes DG, Jr, Shair KH, Marquitz AR, Kung CP, Edwards RH, Raab-Traub N. Human tumor virus utilizes exosomes for intercellular communication. Proc Natl Acad Sci U S A. 2010;107(47):20370–20375. doi: 10.1073/pnas.1014194107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ansari MA, Singh VV, Dutta S, et al. Constitutive interferon-inducible protein 16-inflammasome activation during Epstein-Barr virus latency I, II, and III in B and epithelial cells. J Virol. 2013;87(15):8606–8623. doi: 10.1128/JVI.00805-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Baglio SR, van Eijndhoven MA, Koppers-Lalic D, et al. Sensing of latent EBV infection through exosomal transfer of 5'pppRNA. Proc Natl Acad Sci U S A. 2016;113(5):E587–E596. doi: 10.1073/pnas.1518130113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chugh PE, Sin SH, Ozgur S, et al. Systemically circulating viral and tumor-derived microRNAs in KSHV-associated malignancies. PLoS Pathog. 2013;9(7) doi: 10.1371/journal.ppat.1003484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Naranatt PP, Krishnan HH, Svojanovsky SR, Bloomer C, Mathur S, Chandran B. Host gene induction and transcriptional reprogramming in Kaposi's sarcoma-associated herpesvirus (KSHV/HHV-8)-infected endothelial, fibroblast, and B cells: insights into modulation events early during infection. Cancer Res. 2004;64(1):72–84. doi: 10.1158/0008-5472.CAN-03-2767. [DOI] [PubMed] [Google Scholar]
- 127.Meckes DG, Jr, Gunawardena HP, Dekroon RM, et al. Modulation of B-cell exosome proteins by gamma herpesvirus infection. Proc Natl Acad Sci U S A. 2013;110(31):E2925–E2933. doi: 10.1073/pnas.1303906110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kuo HT, Ye X, Sampaio MS, Reddy P, Bunnapradist S. Cytomegalovirus serostatus pairing and deceased donor kidney transplant outcomes in adult recipients with antiviral prophylaxis. Transplantation. 2010;90(10):1091–1098. doi: 10.1097/TP.0b013e3181f7c053. [DOI] [PubMed] [Google Scholar]
- 129.McDevitt LM. Etiology and impact of cytomegalovirus disease on solid organ transplant recipients. Am J Health Syst Pharm. 2006;63(19 Suppl. 5):S3–S9. doi: 10.2146/ajhp060377. [DOI] [PubMed] [Google Scholar]
- 130.Roux A, Mourin G, Fastenackels S, et al. CMV driven CD8(+) T-cell activation is associated with acute rejection in lung transplantation. Clin Immunol. 2013;148(1):16–26. doi: 10.1016/j.clim.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 131.Plazolles N, Humbert JM, Vachot L, Verrier B, Hocke C, Halary F. Pivotal advance: The promotion of soluble DC-SIGN release by inflammatory signals and its enhancement of cytomegalovirus-mediated cis-infection of myeloid dendritic cells. J Leukoc Biol. 2011;89(3):329–342. doi: 10.1189/jlb.0710386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Halary F, Amara A, Lortat-Jacob H, et al. Human cytomegalovirus binding to DC-SIGN is required for dendritic cell infection and target cell trans-infection. Immunity. 2002;17(5):653–664. doi: 10.1016/S1074-7613(02)00447-8. [DOI] [PubMed] [Google Scholar]
- 133.Ota M, Serada S, Naka T, Mori Y. Expression of MHC class I molecule in HHV-6B-infected cells. Microbiol Immunol 2014;58(2):Februarycover. [DOI] [PubMed]
- 134.Wang X, Wang HK, Li Y, et al. microRNAs are biomarkers of oncogenic human papillomavirus infections. Proc Natl Acad Sci U S A. 2014;111(11):4262–4267. doi: 10.1073/pnas.1401430111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Honegger A, Schilling D, Bastian S, et al. Dependence of intracellular and exosomal microRNAs on viral E6/E7 oncogene expression in HPV-positive tumor cells. PLoS Pathog. 2015;11(3) doi: 10.1371/journal.ppat.1004712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Melo SA, Sugimoto H, O'Connell JT, et al. Cancer exosomes perform cell-independent microRNA biogenesis and promote tumorigenesis. Cancer Cell. 2014;26(5):707–721. doi: 10.1016/j.ccell.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Feng Z, Hensley L, McKnight KL, et al. A pathogenic picornavirus acquires an envelope by hijacking cellular membranes. Nature. 2013;496(7445):367–371. doi: 10.1038/nature12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Feng Z, Li Y, McKnight KL, et al. Human pDCs preferentially sense enveloped hepatitis A virions. J Clin Invest. 2015;125(1):169–176. doi: 10.1172/JCI77527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chai N, Chang HE, Nicolas E, Han Z, Jarnik M, Taylor J. Properties of subviral particles of hepatitis B virus. J Virol. 2008;82(16):7812–7817. doi: 10.1128/JVI.00561-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ahsan NA, Sampey GC, Lepene B, et al. Presence of viral RNA and proteins in exosomes from cellular clones resistant to Rift Valley fever virus infection. Front Microbiol. 2016;7:139. doi: 10.3389/fmicb.2016.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Silvas JA, Popov VL, Paulucci-Holthauzen A, Aguilar PV. Extracellular vesicles mediate receptor-independent transmission of novel tick-borne Bunyavirus. J Virol. 2016;90(2):873–886. doi: 10.1128/JVI.02490-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lozach PY, Kuhbacher A, Meier R, et al. DC-SIGN as a receptor for phleboviruses. Cell Host Microbe. 2011;10(1):75–88. doi: 10.1016/j.chom.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 143.Varkey JB, Shantha JG, Crozier I, et al. Persistence of Ebola virus in ocular fluid during convalescence. N Engl J Med. 2015;372(25):2423–2427. doi: 10.1056/NEJMoa1500306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Uyeki TM, Erickson BR, Brown S, et al. Ebola virus persistence in semen of male survivors. Clin Infect Dis. 2016;62:1552–1555. doi: 10.1093/cid/ciw202. [DOI] [PubMed] [Google Scholar]
- 145.Atkinson B, Hearn P, Afrough B, et al. Detection of Zika virus in semen. Emerg Infect Dis. 2016;22(5):940. doi: 10.3201/eid2205.160107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Malkki H. CNS infections: Zika virus infection could trigger Guillain-Barre syndrome. Nat Rev Neurol. 2016;12(4):187. doi: 10.1038/nrneurol.2016.30. [DOI] [PubMed] [Google Scholar]
- 147.Garcez PP, Loiola EC, Madeiro da Costa R, et al. Zika virus impairs growth in human neurospheres and brain organoids. Science. 2016;352:816–818. doi: 10.1126/science.aaf6116. [DOI] [PubMed] [Google Scholar]
- 148.Williamson PR, Nash TE, Williamson KC, Nath A. CNS infections in 2015: emerging catastrophic infections and new insights into neuroimmunological host damage. Lancet Neurol. 2016;15(1):17–19. doi: 10.1016/S1474-4422(15)00359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Han Z, Madara JJ, Liu Y, et al. ALIX rescues budding of a double PTAP/PPEY L-domain deletion mutant of Ebola VP40: a role for ALIX in Ebola virus egress. J Infect Dis. 2015;212(Suppl. 2):S138–S145. doi: 10.1093/infdis/jiu838. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)