Abstract
Background and Objectives
Cerebrovascular disease is a leading cause of mortality and morbidity in Korea. Understanding of cerebrovascular disease mortality trends is important to reduce the health burden from cerebrovascular diseases. We examined the changing pattern of mortality related to cerebrovascular disease in Korea over 30 years from 1983 to 2012.
Subjects and Methods
Numbers of deaths from cerebrovascular disease, hemorrhagic stroke, and cerebral infarction were obtained from the national Cause of Death Statistics. Crude and age-adjusted mortality rates were calculated for men and women for each year. Penalized B-spline methods, which reduce bias and variability in curve fitting, were used to identify the trends of 30-year mortality and identify the year of highest mortality.
Results
During the 30 years, cerebrovascular disease mortality has markedly declined. The age-adjusted cerebrovascular disease mortality rate has decreased by 78% in men and by 68% in women. In the case of hemorrhagic stroke, crude mortality peaked in 2001 but age-adjusted mortality peaked in 1994. Between 1994 and 2012, age-adjusted mortality from hemorrhagic stroke has decreased by 68% in men and 59% in women. In the case of cerebral infarction, crude and age-adjusted mortality rates steeply increased until 2004 and 2003, respectively, and both rates decreased rapidly thereafter.
Conclusion
Cerebrovascular disease mortality rate has significantly decreased over the last 30 years in Korea, but remains a health burden. The prevalence of major cardiovascular risk factors are still highly prevalent in Korea.
Keywords: Cerebrovascular disorders, Stroke, Mortality, Trends, Korea
Introduction
Cerebrovascular disease mortality ranks as the second most common cause of death around the world,1) but, in Korea, cerebrovascular disease is the leading cause of death among single -organ diseases.2),3) Every year approximately 105000 people experience a new or recurrent stroke and more than 26000 people die.2) Fortunately, there have been great improvements in the management of stroke over the last decades. Among the Organization for Economic Cooperation and Development (OECD) member countries, Korea recorded the lowest in-hospital, 30-day case-fatality rate for ischemic stroke and the third lowest rate for hemorrhagic stroke in 2009.2),4) Understanding cerebrovascular disease mortality trends is important to reduce the health burden. Mortality trends of cerebrovascular diseases have been reported in many countries including Korea.5),6),7) However, there are only a few studies reporting long-term trends in mortality from cerebrovascular diseases in the Korean population. Thus, we examined the 30-year changing pattern of cerebrovascular disease mortality in Korea to further understand and quantify recent trends in mortality by analyzing the Cause of Death statistics from Statistics Korea.
Subjects and Methods
Annual mortality data were obtained from the Korean Statistical Information Service managed by Statistics Korea (former the Korea National Statistical Office). Mortality statistics with cause of death information have been available since 1983. Causes of death were coded according to the International Classification of Disease, 10th Revision. For the purpose of this study, deaths from cerebrovascular disease (I60-69) were further classified into hemorrhagic stroke (I60-62), cerebral infarction (I63), unspecified stroke (I64), and other cerebrovascular diseases (I65-69). Hemorrhagic stroke included subarachnoid hemorrhage (I60), intracerebral hemorrhage (I61), and other nontraumatic intracranial hemorrhage (I62). Mortality rates from total heart diseases (I00-13 and I20-51) and ischemic heart disease (I20-25) were previously reported.8)
Crude and age-adjusted mortalities were calculated only for cerebrovascular disease, hemorrhagic stroke, and cerebrovascular disease, because reported numbers of deaths from unspecified stroke and other cerebrovascular diseases showed great fluctuation in the 1990s and early 2000s, probably due to changes in classifying causes of death. We calculated age-adjusted mortality through a direct standardization method using the age distribution of the Korean population in 2000 as the standard population. We analyzed data using 10-year age intervals and the same population structure for standardization in men and women to compare mortality by sex. We also presented penalized B-Splines to explore the non-linear pattern of the crude death rate and age-adjusted death rate per 100000 over time in years. Penalized regression methods are used to quantify the notion of roughness of a curve through a suitable penalty function and the necessary compromise between bias and variability in curve fitting can be explicit in estimation of the problem.9)
Results
Numbers of deaths from cerebrovascular disease
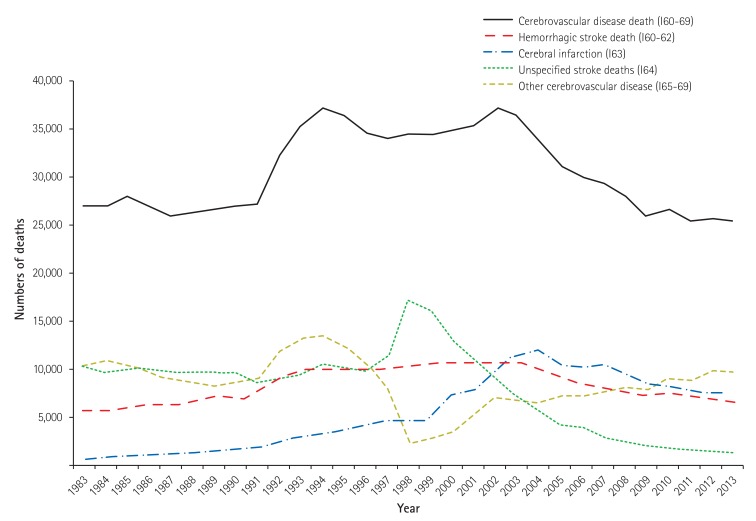
Table 1 and Fig. 1 show the number of deaths from cerebrovascular diseases for each year. The absolute number of deaths from cerebrovascular disease did not change much between 1983 and 1990, but it increased rapidly in the early 1990s then stayed high until 2002. However, after 2002, the number of deaths from cerebrovascular disease has consistently declined. The number of deaths from cerebrovascular disease was 26922 in 1983, peaked at 37131 in 1994, and decreased to 25447 by 2013. Number of deaths from hemorrhagic stroke peaked in 2002, while deaths from cerebral infarction reached its peak in 2004. In 1983, deaths from hemorrhagic stroke (n=5549) were almost 8 times more common than deaths from cerebral infarction (n=703). However, since 2003, cerebral infarction has been the most common cause of death among cerebrovascular diseases. The number of deaths from unspecified stroke increased steeply between 1996 and 1998, but it rapidly decreased until recently since 1998.
Table 1. Numbers of deaths from cerebrovascular diseases.
| Year | Cerebrovascular disease (I60-69) | Hemorrhagic stroke (I60-62) | Cerebral infarction (I63) | Unspecified stroke (I64) | Other cerebrovascular disease (I65-69) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Men | Women | Total | Men | Women | Total | Men | Women | Total | Men | Women | Total | Men | Women | |
| 1983 | 26922 | 14749 | 12173 | 5549 | 3190 | 2359 | 703 | 381 | 322 | 10254 | 5713 | 4541 | 10416 | 5465 | 4951 |
| 1984 | 26919 | 14551 | 12368 | 5623 | 3160 | 2463 | 758 | 416 | 342 | 9736 | 5298 | 4438 | 10802 | 5677 | 5125 |
| 1985 | 27883 | 15047 | 12836 | 6235 | 3484 | 2751 | 1070 | 579 | 491 | 10117 | 5479 | 4638 | 10461 | 5505 | 4956 |
| 1986 | 26966 | 14513 | 12453 | 6371 | 3557 | 2814 | 1172 | 626 | 546 | 9941 | 5347 | 4594 | 9482 | 4983 | 4499 |
| 1987 | 25984 | 13693 | 12291 | 6230 | 3371 | 2859 | 1181 | 612 | 569 | 9570 | 5087 | 4483 | 9003 | 4623 | 4380 |
| 1988 | 26234 | 13722 | 12512 | 6679 | 3606 | 3073 | 1238 | 614 | 624 | 9680 | 5064 | 4616 | 8637 | 4438 | 4199 |
| 1989 | 26505 | 13848 | 12657 | 7230 | 3788 | 3442 | 1533 | 820 | 713 | 9574 | 4947 | 4627 | 8168 | 4293 | 3875 |
| 1990 | 27039 | 13902 | 13137 | 6909 | 3590 | 3319 | 1681 | 898 | 783 | 9808 | 5081 | 4727 | 8641 | 4333 | 4308 |
| 1991 | 27152 | 13680 | 13472 | 7535 | 3908 | 3627 | 1897 | 1035 | 862 | 8739 | 4298 | 4441 | 8981 | 4439 | 4542 |
| 1992 | 32236 | 15642 | 16594 | 8969 | 4486 | 4483 | 2495 | 1297 | 1198 | 9125 | 4458 | 4667 | 11647 | 5401 | 6246 |
| 1993 | 35216 | 16943 | 18273 | 9802 | 4817 | 4985 | 2803 | 1433 | 1370 | 9450 | 4607 | 4843 | 13161 | 6086 | 7075 |
| 1994 | 37131 | 17793 | 19338 | 10022 | 5001 | 5021 | 3149 | 1644 | 1505 | 10502 | 4995 | 5507 | 13458 | 6153 | 7305 |
| 1995 | 36416 | 17300 | 19116 | 9868 | 4822 | 5046 | 3767 | 1915 | 1852 | 10337 | 4988 | 5349 | 12444 | 5575 | 6869 |
| 1996 | 34590 | 16508 | 18082 | 10052 | 4906 | 5146 | 4111 | 2090 | 2021 | 9788 | 4661 | 5127 | 10639 | 4851 | 5788 |
| 1997 | 33966 | 16467 | 17499 | 9946 | 4917 | 5029 | 4449 | 2299 | 2150 | 11565 | 5553 | 6012 | 8006 | 3698 | 4308 |
| 1998 | 34464 | 16555 | 17909 | 10197 | 5045 | 5152 | 4451 | 2275 | 2176 | 17201 | 8037 | 9164 | 2615 | 1198 | 1417 |
| 1999 | 34374 | 16390 | 17984 | 10653 | 5200 | 5453 | 4944 | 2498 | 2446 | 16151 | 7426 | 8725 | 2626 | 1266 | 1360 |
| 2000 | 34754 | 16537 | 18217 | 10695 | 5240 | 5455 | 7357 | 3496 | 3861 | 13324 | 6224 | 7100 | 3378 | 1577 | 1801 |
| 2001 | 35295 | 17035 | 18260 | 10766 | 5270 | 5496 | 7987 | 3839 | 4148 | 11219 | 5409 | 5810 | 5323 | 2517 | 2806 |
| 2002 | 37067 | 17511 | 19556 | 10839 | 5318 | 5521 | 10027 | 4686 | 5341 | 9126 | 4212 | 4914 | 7075 | 3295 | 3780 |
| 2003 | 36396 | 17176 | 19220 | 10751 | 5265 | 5486 | 11479 | 5257 | 6222 | 7202 | 3311 | 3891 | 6964 | 3343 | 3621 |
| 2004 | 34003 | 16166 | 17837 | 9874 | 4837 | 5037 | 11793 | 5430 | 6363 | 5768 | 2669 | 3099 | 6568 | 3230 | 3338 |
| 2005 | 31195 | 14886 | 16309 | 9098 | 4405 | 4693 | 10664 | 4988 | 5676 | 4226 | 1990 | 2236 | 7207 | 3503 | 3704 |
| 2006 | 29951 | 14460 | 15491 | 8526 | 4150 | 4376 | 10177 | 4767 | 5410 | 4005 | 1960 | 2045 | 7243 | 3583 | 3660 |
| 2007 | 29277 | 13941 | 15336 | 8030 | 3965 | 4065 | 10693 | 4904 | 5789 | 2944 | 1391 | 1553 | 7610 | 3681 | 3929 |
| 2008 | 27932 | 13553 | 14379 | 7733 | 3877 | 3856 | 9582 | 4444 | 5138 | 2568 | 1283 | 1285 | 8049 | 3949 | 4100 |
| 2009 | 25836 | 12648 | 13188 | 7207 | 3586 | 3621 | 8475 | 4010 | 4465 | 2113 | 1047 | 1066 | 8041 | 4005 | 4036 |
| 2010 | 26514 | 12865 | 13649 | 7503 | 3717 | 3786 | 8164 | 3791 | 4373 | 1908 | 943 | 965 | 8939 | 4414 | 4525 |
| 2011 | 25404 | 12185 | 13219 | 7112 | 3518 | 3594 | 7860 | 3520 | 4340 | 1653 | 828 | 825 | 8779 | 4319 | 4460 |
| 2012 | 25744 | 12380 | 13364 | 6767 | 3337 | 3430 | 7490 | 3469 | 4021 | 1554 | 706 | 848 | 9933 | 4868 | 5065 |
| 2013 | 25447 | 12096 | 13351 | 6710 | 3318 | 3392 | 7558 | 3468 | 4090 | 1387 | 629 | 758 | 9792 | 4681 | 5111 |
Fig. 1. Number of deaths from cerebrovascular disease.
Crude and age-adjusted mortality from cerebrovascular disease
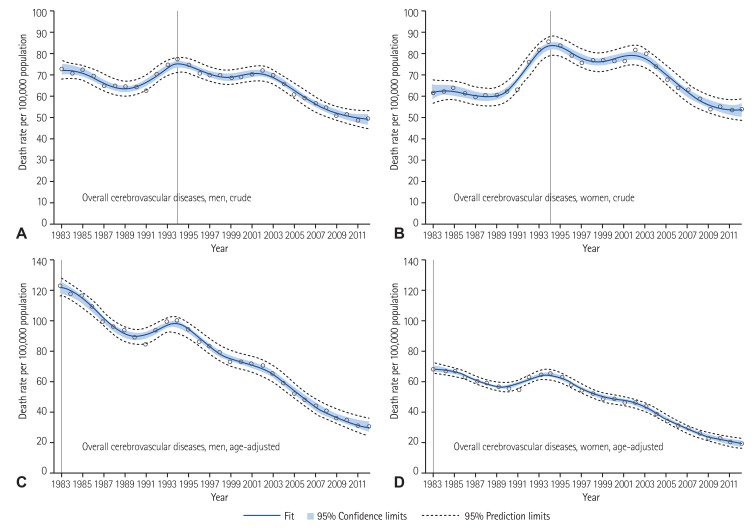
The crude mortality rate from cerebrovascular disease showed fluctuating patterns until 2002, but thereafter it decreased. In the 1980s, the crude mortality rate for men was higher than for women, but the gender difference gradually decreased and has reversed since 1991. The crude mortality rate from cerebrovascular disease in 1983 was 73.3 per 100000 in men and 61.5 per 100000 women. In 2012, the crude mortality rate per 100000 was 49.2 for men and 53.1 for women. After the highest crude mortality rate in 1994, there were 33% and 14% mortality decreases in men and women, respectively, until 2012.
Age-adjusted mortality rates from cerebrovascular disease has decreased too, until recently, but the rate has been always higher in men than in women. In 1983, the age-adjusted mortality rate for men was about 2 times higher than for women (124.3 vs. 68.1 per 100000). But the sex difference has gradually reduced to 28.7 per 100000 men and 17.2 per 100000 women in 2012 (Fig. 2).
Fig. 2. Crude and age-adjusted mortality from cerebrovascular diseases fitted by Penalized B-Splines method. (A) Crude mortality from cerebrovascular diseases in men. (B) Crude mortality from cerebrovascular diseases in women. (C) Age-adjusted mortality from cerebrovascular diseases in men. (D) Age-adjusted mortality from cerebrovascular diseases in women.
Crude and age-adjusted mortality from hemorrhagic stroke
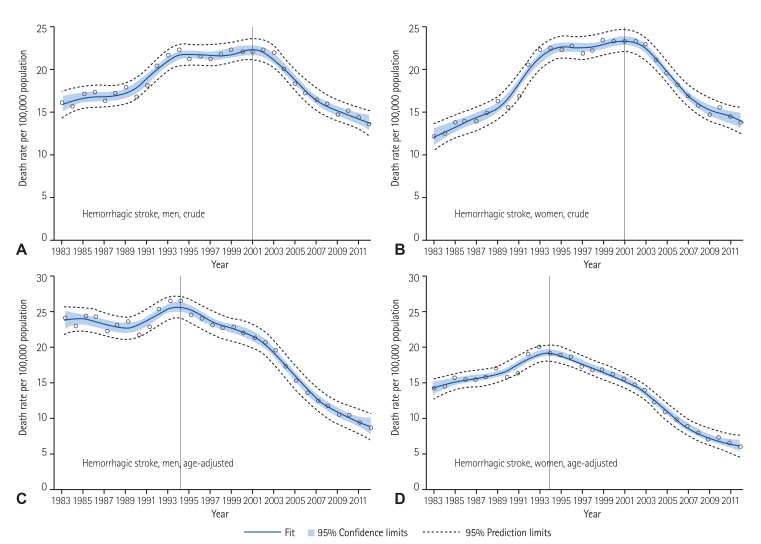
Crude mortality rate from hemorrhagic stroke showed upward trends between 1983 and 2001. But, after 2001, the rate has rapidly decreased. The crude mortality rate for men was higher than for women until 1991, but thereafter the rate for women was higher than men. In 1983, the crude mortality rate from hemorrhagic stroke per 100000 was 15.8 for men and 11.9 for women, but the corresponding rate was 13.3 for men and 13.7 for women in 2012. After the highest mortality rate in 2001, there was about a 39.8% decrease in men and 41.5% decrease in women until 2012.
Age-adjusted hemorrhagic stroke mortality rate peaked in 1994, then the rate decreased in both men and women. Unlike crude mortality, the age-adjusted mortality rate has been consistently higher in men than in women. The age-adjusted hemorrhagic stroke mortality rate per 100000 was 24.4 for men and 14.2 for women in 1983. However, the corresponding rate decreased to 8.6 for men and 5.8 for women by 2012. After the highest age-adjusted mortality rate in 1994, there was a 68.1% decrease in men and a 41.5% decrease in women until 2012 (Fig. 3). It is also notable that crude hemorrhagic stroke mortality peaked in 2001, but the age-adjusted mortality peaked much earlier in 1994.
Fig. 3. Crude and age-adjusted mortality from hemorrhagic stroke fitted by Penalized B-Splines method. (A) Crude mortality from hemorrhagic stroke in men. (B) Crude mortality from hemorrhagic stroke in women. (C) Age-adjusted mortality from hemorrhagic stroke in men. (D) Age-adjusted mortality from hemorrhagic stroke in women.
Crude and age-adjusted mortality rates from cerebral infarction
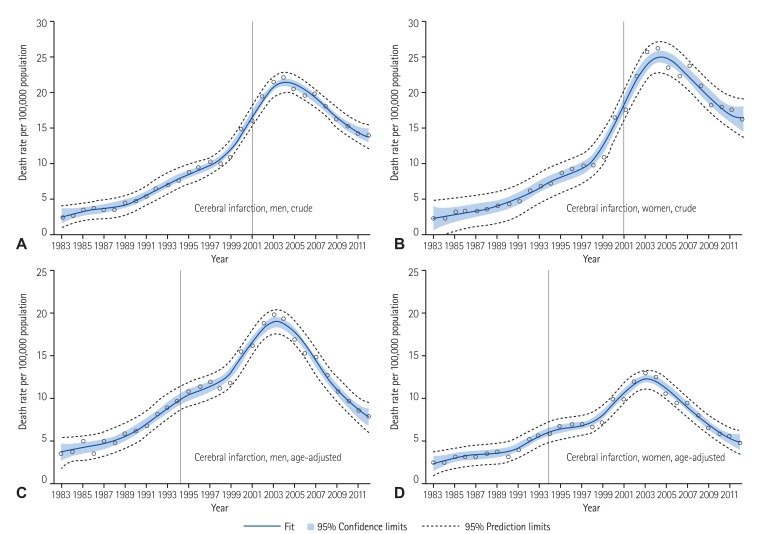
Crude mortality rate from cerebral infarction increased until 2004. But, thereafter, the rate has rapidly decreased. Crude mortality rate per 100000 was 1.9 for men and 1.6 for women in 1983, which increased to 22.3 in men and 26.3 for women in 2004, then decreased to 13.8 for men and 16 for women by 2012. After the highest age-adjusted mortality rate in 2004, there was a 30.7% decrease in men and 32.2% decrease in women.
Age-adjusted cerebral infarction mortality rates peaked in 2003. Unlike crude mortality, the age-adjusted cerebral infarction mortality rate has been consistently higher in men than in women. After the highest age-adjusted mortality in 2003, there was about 61.8% decrease in men and 65.6% decrease in women (Fig. 4). Figures without penalized regression splines for cerebrovascular diseases are provided as supplemental data (Supplementary Figs. 1 to 3 in the online-only Data Supplement).
Fig. 4. Crude and age-adjusted mortality from cerebral infarction fitted by Penalized B-Splines method. (A) Crude mortality from cerebral infarction in men. (B) Crude mortality from cerebral infarction in women. (C) Age-adjusted mortality from cerebral infarction in men. (D) Age-adjusted mortality from cerebral infarction in women.
Discussion
Our study reports the death rate of major cerebrovascular diseases in the Korean population and their trends over the last 30 years. The age-standardized mortality rate from cerebrovascular diseases has significantly decreased since 1983 in Korea and the decline in mortality from cerebrovascular diseases was more prominent in men than women. Over the last three decades, the age-adjusted mortality rate from cerebrovascular diseases decreased, but temporarily increased between 1991 and 1993. This fluctuation might be due to changes of classification of the Cause of Death Statistics in Korea. During the same time period, deaths from hypertensive disease (I10-I15) significantly decreased.8)
In most developed countries, cerebrovascular disease had been among the leading causes of death in the past, but it has decreased in recent decades.10),11) In particular, Australia, New Zealand, and the UK showed a continuous decline in cerebrovascular disease mortality since 1950. The United States showed a steep declining trend since the 1970s and the trend was more prominent in men than women.10),11),12) Among Asian countries, Japan had the highest cerebrovascular disease mortality in the 1950s (433 per 100000 in men in 1957), but the rate significantly decreased to less than 100 per 100000 by 2004.6),10) Recent studies reported that the stroke mortality rate of Korea was double that of Japan in the beginning of the 2000s,10) although both Japan and Korea showed decreasing mortality trends for stroke at that time.13)
A number of studies reported the accelerated decline in stroke mortality during the late 1970s and the early 1980s. Among them, some earlier studies reported declining trends in the stroke incidence rate as well as stroke fatalities during the 1970s,14),15) suggesting that the effect of stroke incidence rate on stroke mortality.14) However, there was no significant association between stroke mortality and stroke incidence in Sweden.15) This study reported that a decline of mortality from stroke may be due to a decline of smoking and blood pressure (BP) together with an increase in the use of anti-hypertensive treatments rather than changes of stroke incidence.15) Accordingly, it may be because acute stroke events have become less severe and the survival rate of stroke patients is increasing.
The successful control of risk factors may have contributed to declining incidence and fatality of stroke, which may lead to the decreasing trends of stroke mortality.16),17) In most populations, hypertension is the most attributable factor for cerebrovascular disease.18),19),20) In a previous study analyzing data from 1998-2011 available in the Korea National Health Nutrition Examination Survey (KNHANES),21) the age-adjusted prevalence of hypertension decreased by 0.2 to 0.3 percent annually. The study reported that mean systolic BP level decreased by 8 mmHg in men and by 10 mmHg in women during this period which suggested that decreasing BP was largely due to lowered BP levels among patients with diagnosed hypertension.21) The improved BP control might contribute to the remarkable decrease in stroke mortality in Korea. In another systematic review of data from Korean or other populations, the attributable risk of hypertension for ischemic stroke was 19.9 to 30.5% in men and 17.1 to 26.6% in women.22) At ages 40 to 69, usual BP is directly related to stoke mortality in a meta-analysis of clinical trials.23) On the other hand, a few studies were unconvincing that improvement in control of hypertension resulted in a decline of mortality from stroke.24) However, according to a meta-analysis of clinical trials in 1992, anti-hypertensive treatment reduced fatal strokes by 33% and cardiovascular mortality by 22%.25),26) The use of cholesterol-lowering medications also decreased stroke risk and mortality in observational studies and clinical trials.27),28) Improved acute stroke management might also contribute to the mortality decline.7) Between 1998 and 2002, the prevalence of hypertension decreased, whereas the prevalence of hypercholesterolemia significantly increased in both sexes.4) Smoking rate decreased only in men, whereas the prevalence of diabetes did not change over time. Another study reported epidemiologic trends of ischemic stroke between 2002 and 2010, by analyzing data from the Korean Stroke Registry.29) Patient's age steadily increased, while prevalence of risk factors such as hypertension, diabetes, and smoking declined. Although cerebrovascular disease mortality rate has decreased over the last 30 years, cerebrovascular disease still remains a great burden to society and is a major cardiovascular risk factor prevalent among Koreans. To further reduce the burden of cerebrovascular disease, we need to monitor the trends of mortality from cerebrovascular disease and its subcategories, because management and prevention strategies for different stroke types vary.
The major strength of the present study is that it analyzed nationwide mortality data covering 30 years in the Korean population. But, there are also several limitations to be discussed. First, validity of cause of death can be debated. The Statistics Korea report annually the Cause of Death Statistics, and the database are primarily based on the death certificates. A previous study retrospectively compared the Cause of Death Statistics with hospital medical records, and reported the overall accuracy of causes of death as 91.9%.30) Second, there are still a significant number of deaths recorded without underlying causes in the Death Statistics. In 2012, 9.4% of deaths were classified as unknown, although the deaths by unknown causes are decreasing. Thus there is a possibility of underestimation of mortality from cerebrovascular disease. Third, the reported number of cerebrovascular deaths can be influenced by the health care system. Over the last decades, Korea experienced marked improvement in medical service accessibility and health care technologies. These changes might affect the reported number of cerebrovascular diseases. Lastly, there is no available nationwide data on the incidence of cerebrovascular disease, so we cannot explore the underlying causes of changing mortality trends.
In conclusion, cerebrovascular disease mortality has significantly decreased over the last 30 years, but remains a great health burden and the prevalence of major for cardiovascular risk factors are still highly prevalent in Korea. We need to continuously monitor the trends of mortality from cerebrovascular disease and its subcategories to further reduce cerebrovascular disease burdens.
Acknowledgments
This work was supported by the Korean Health Technology R&D Project, Ministry of Health & Welfare, Korea (HI13C0715).
Footnotes
The authors have no financial conflicts of interest.
Supplementary Materials
The online-only Data Supplement is available with this article at http://dx.doi.org/10.4070/kcj.2016.46.4.507.
Crude and age-adjusted mortality from cerebrovascular disease (I60-I69).
Crude and age-adjusted mortality from hemorrhagic stroke (I60-62).
Crude and age-adjusted mortality rates from cerebral infarction (I63).
References
- 1.Deaton C, Froelicher ES, Wu LH, Ho C, Shishani K, Jaarsma T. The global burden of cardiovascular disease. Eur J Cardiovasc Nurs. 2011;10(Suppl 2):S5–S13. doi: 10.1016/S1474-5151(11)00111-3. [DOI] [PubMed] [Google Scholar]
- 2.Hong KS, Bang OY, Kang DW, et al. Stroke statistics in Korea: part I. Epidemiology and risk factors: a report from the Korean stroke society and clinical research center for stroke. J Stroke. 2013;15:2–20. doi: 10.5853/jos.2013.15.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee KS, Park JH. Burden of disease in Korea during 2000-10. J Public Health (Oxf) 2014;36:225–234. doi: 10.1093/pubmed/fdt056. [DOI] [PubMed] [Google Scholar]
- 4.Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998-2012. Int J Cardiol. 2014;174:64–72. doi: 10.1016/j.ijcard.2014.03.163. [DOI] [PubMed] [Google Scholar]
- 5.Levi F, Chatenoud L, Bertuccio P, Lucchini F, Negri E, La Vecchia C. Mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world: an update. Eur J Cardiovasc Prev Rehabil. 2009;16:333–350. doi: 10.1097/HJR.0b013e328325d67d. [DOI] [PubMed] [Google Scholar]
- 6.Sarti C, Rastenyte D, Cepaitis Z, Tuomilehto J. International trends in mortality from stroke, 1968 to 1994. Stroke. 2000;31:1588–1601. doi: 10.1161/01.str.31.7.1588. [DOI] [PubMed] [Google Scholar]
- 7.Towfighi A, Saver JL. Stroke declines from third to fourth leading cause of death in the United States: historical perspective and challenges ahead. Stroke. 2011;42:2351–2355. doi: 10.1161/STROKEAHA.111.621904. [DOI] [PubMed] [Google Scholar]
- 8.Lee SW, Kim HC, Lee HS, Suh I. Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J. 2015;45:202–209. doi: 10.4070/kcj.2015.45.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Costa MJ. Penalized spline models and applications [dissertation] Coventry (UK): University of Warwick; 2008. [Google Scholar]
- 10.Mirzaei M, Truswell AS, Arnett K, Page A, Taylor R, Leeder SR. Cerebrovascular disease in 48 countries: secular trends in mortality 1950–2005. J Neurol Neurosurg Psychiatry. 2012;83:138–145. doi: 10.1136/jnnp-2011-300408. [DOI] [PubMed] [Google Scholar]
- 11.Thom TJ, Epstein FH. Heart disease, cancer, and stroke mortality trends and their interrelations. An international perspective. Circulation. 1994;90:574–582. doi: 10.1161/01.cir.90.1.574. [DOI] [PubMed] [Google Scholar]
- 12.Klag MJ, Whelton PK, Seidler AJ. Decline in US stroke mortality. Demographic trends and antihypertensive treatment. Stroke. 1989;20:14–21. doi: 10.1161/01.str.20.1.14. [DOI] [PubMed] [Google Scholar]
- 13.Suh I. Cardiovascular mortality in Korea: a country experiencing epidemiologic transition. Acta Cardiol. 2001;56:75–81. doi: 10.2143/AC.56.2.2005621. [DOI] [PubMed] [Google Scholar]
- 14.Garraway WM, Whisnant JP, Drury I. The continuing decline in the incidence of stroke. Mayo Clin Proc. 1983;58:520–523. [PubMed] [Google Scholar]
- 15.Harmsen P, Tsipogianni A, Wilhelmsen L. Stroke incidence rates were unchanged, while fatality rates declined, during 1971-1987 in Göteborg, Sweden. Stroke. 1992;23:1410–1415. doi: 10.1161/01.str.23.10.1410. [DOI] [PubMed] [Google Scholar]
- 16.Lackland DT, Roccella EJ, Deutsch AF, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 2014;45:315–353. doi: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carter KN, Anderson CS, Hackett ML, Barber PA, Bonita R Auckland Regional Community Stroke Study Group. Improved survival after stroke: is admission to hospital the major explanation? Trend analyses of the Auckland Regional Community Stroke Studies. Cerebrovasc Dis. 2007;23:162–168. doi: 10.1159/000097054. [DOI] [PubMed] [Google Scholar]
- 18.Kannel WB. Framingham study insights into hypertensive risk of cardiovascular disease. Hypertens Res. 1995;18:181–196. doi: 10.1291/hypres.18.181. [DOI] [PubMed] [Google Scholar]
- 19.Neaton JD, Wentworth DN, Cutler J, Stamler J, Kuller L. Risk factors for death from different types of stroke. Multiple Risk Factor Intervention Trial Research Group. Ann Epidemiol. 1993;3:493–499. doi: 10.1016/1047-2797(93)90103-b. [DOI] [PubMed] [Google Scholar]
- 20.O'Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 21.Kim HC, Oh SM. Noncommunicable diseases: current status of major modifiable risk factors in Korea. J Prev Med Public Health. 2013;46:165–172. doi: 10.3961/jpmph.2013.46.4.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park TH, Kim MK, Lee KB, et al. Population attributable risk of major risk factors for ischemic stroke in the Korean population. Korean J Stroke. 2008;10:125–133. [Google Scholar]
- 23.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 24.Bonita R, Beaglehole R. Increased treatment of hypertension does not explain the decline in stroke mortality in the United States, 1970-1980. Hypertension. 1989;13(5 Suppl):I69–I73. doi: 10.1161/01.hyp.13.5_suppl.i69. [DOI] [PubMed] [Google Scholar]
- 25.Thijs L, Fagard R, Lijnen P, Staessen J, Van Hoof R, Amery A. A meta-analysis of outcome trials in elderly hypertensives. J Hypertens. 1992;10:1103–1109. doi: 10.1097/00004872-199210000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Lever AF, Ramsay LE. Treatment of hypertension in the elderly. J Hypertens. 1995;13:571–579. doi: 10.1097/00004872-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Ní Chróinín D, Asplund K, Åsberg S, et al. Statin therapy and outcome after ischemic stroke: systematic review and meta-analysis of observational studies and randomized trials. Stroke. 2013;44:448–456. doi: 10.1161/STROKEAHA.112.668277. [DOI] [PubMed] [Google Scholar]
- 28.Koton S, Schneider AL, Rosamond WD, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312:259–268. doi: 10.1001/jama.2014.7692. [DOI] [PubMed] [Google Scholar]
- 29.Jung KH, Lee SH, Kim BJ, et al. Secular trends in ischemic stroke characteristics in a rapidly developed country: results from the Korean Stroke Registry Study (secular trends in Korean stroke) Circ Cardiovasc Qual Outcomes. 2012;5:327–334. doi: 10.1161/CIRCOUTCOMES.111.963736. [DOI] [PubMed] [Google Scholar]
- 30.Won TY, Kang BS, Im TH, Choi HJ. The study of accuracy of death statistics. J Korean Soc Emerg Med. 2007;18:256–262. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Crude and age-adjusted mortality from cerebrovascular disease (I60-I69).
Crude and age-adjusted mortality from hemorrhagic stroke (I60-62).
Crude and age-adjusted mortality rates from cerebral infarction (I63).