Abstract
Introduction
Young adolescent women in sub-Saharan Africa are three to four times more likely to be HIV-positive than boys or men. One of the relationship dynamics that is likely to be associated with young women's increased vulnerability to HIV is transactional sex. There are a range of HIV-related risk behaviours that may drive this vulnerability. However, to date, limited epidemiological data exist on the role of transactional sex in increasing HIV acquisition, especially among young women in sub-Saharan Africa. Our paper presents data on the prevalence of self-reported engagement in transactional sex and explores whether transactional sex is associated with increased risk of HIV infection among a cohort of young, rural, sexually active South African women. We also explore whether this relationship is mediated through certain HIV-related risk behaviours.
Methods
We analyzed baseline data from a phase III trial of conditional cash transfers for HIV prevention of 693 sexually active, school-going young women aged 13–20 years in rural South Africa. We examined the association between young women's engagement in transactional sex and HIV infection. Transactional sex is defined as a non-commercial, non-marital sexual relationship whereby sex is exchanged for money and/or gifts. We explored whether this relationship is mediated by certain HIV-related risk behaviours. We used logistic and multinomial regression and report unadjusted and adjusted odds ratios with 95% CI.
Results
Overall, 14% (n=97) of sexually active young women reported engaging in transactional sex. Engagement in transactional sex was associated with an increased risk of being HIV-positive (aOR: 2.5, CI: 95% 1.19–5.25, p=0.01). The effect size of this association remained nearly unchanged when adjusted for certain other dimensions of HIV risk that might help explain the underlying pathways for this relationship.
Conclusions
This study provides quantitative support demonstrating that transactional sex is associated with HIV infection in young women. Even though the specific variables tested do not mediate the relationship, a potential explanation for this association may be that the men with whom young women are having sex belong to networks of sexually connected individuals who are at a “high risk” for HIV infection. The results highlight the importance of structural intervention approaches that can alter the context of young women's HIV risk.
Keywords: transactional sex, structural drivers, HIV, adolescent women, young women, sub-Saharan Africa, risky sexual behaviours
Introduction
The HIV epidemic in South Africa is one of the largest in the world [1,2] and is largely heterosexually transmitted [3]. Young women of child-bearing age have a significantly higher HIV prevalence (5.6% vs. 0.7%) [4–6] and incidence (2.5% vs. 0.6%) [4,7,8] than males of the same age. In addition to increased biological vulnerability of young women, relational risk factors, such as age-disparate relationships, engagement in transactional sex and violence within partnerships [9–11], as well as individual risk behaviours – such as inconsistent condom use, number of partners and age at sexual debut – have been found to be associated with young women's risk of HIV infection [12].
Transactional sex has received increasing attention in the public health literature, as it is believed to be an important contributing factor to the high HIV infection rates observed among young women in sub-Saharan Africa [13,14]. There is currently a wide-ranging debate on the definition of transactional sex, but it is defined here as a non-marital sexual relationship where men and women exchange sex for, or in anticipation of, material possessions or favours (such as money, clothing, transportation and school fees). It is considered to be sex framed outside of prostitution or sex work by those who participate in the exchange and can be differentiated by the negotiating process, that is, in transactional sex there is no up-front negotiation or pre-determined payment and a wide range of goods (money, but also gifts, favours) may be exchanged [13], whereas in sex work, there is an explicit up-front negotiation of the terms of the exchange [10]. In addition, women engaging in transactional sex seldom identify themselves as sex workers. Reflecting economic and social roles within many high HIV prevalence countries, it is predominantly men who provide and women who receive these material benefits in transactional sexual encounters [10,15–17]. This dynamic might in turn render young women vulnerable to HIV. Reporting of transactional sex is varied as indicated by evidence from population-based Demographic and Health Surveys (DHS) data of transactional sex in the past year from 12 sub-Saharan African countries which suggest that the prevalence of transactional sex ranges from 2 to 26.6% across settings [18]. The academic literature highlights that factors associated with transactional sex are complex; demographic and socio-economic factors can be an important determinant, with young women using sex to access essential resources, including food and school fees. In addition, peer or family pressure, as well as young women's aspirations for acquiring expensive goods or connections to boost their status may also be important motivating factors [19,20].
It is not just the transactional aspect that makes such sexual encounters potentially risky for HIV acquisition. Transactional sex might overlap with a range of factors that have been shown to be associated with HIV acquisition – such as sexual relations between a younger woman and an older man (who is more likely to be HIV-positive) [9,21,22], sex under the influence of alcohol or drugs [23,24], having multiple sexual partners or engaging in a relationship with a man who concurrently has other partners [25–27]. Together, these factors might reflect aspects of a transactional relationship that may make young women vulnerable to HIV infection. In addition, partnership dynamics, such as unequal power within a relationship, may undermine condom use thereby increasing HIV risk [28–30].
Despite the potential for transactional sex to increase HIV risk, there is limited quantitative data demonstrating an association in young women: only two studies, both from South Africa, showed evidence of an association in young women [10,31]. Results from the cross-sectional analysis of a quasi-experimental community-based survey in Kwa-Zulu Natal and Eastern Cape provinces involving 2624 young women, aged 15–24 years, showed that young women who reported having engaged in transactional sex have almost twice the odds of being HIV seropositive as compared with those who do not report engaging in transactional sex [31]. In another prospective cohort study of South African women (n=1077) aged 15–26 years, Jewkes et al. found that young women who reported having transactional sex with a once-off partner or with an ongoing secondary partner had higher HIV incidence than those not engaging in transactional sex (this result remained after adjusting for number of partners and age difference between partners) [10].
To help address this shortage of quantitative studies examining the relationship between transactional sex and HIV infection, particularly in young women, our paper presents data on the prevalence of self-reported engagement in transactional sex and examines whether transactional sex is associated with an increased risk of HIV infection among a cohort of young, rural, sexually active South African women. We also examine whether this relationship is mediated through certain HIV-related risk behaviours.
Methods
Study setting and data collection
This paper is a secondary analysis of cross-sectional data collected during baseline interviews with participants from a phase III, individually randomized conditional cash transfer (CCT) trial in rural South Africa (HPTN 068) [32,33]. Participants at the baseline interview were sexually active, school-going young women who reported ever having had vaginal and/or anal sex. Data collection was conducted from March 2011 to December 2012 in the sub-district of Agincourt in rural Mpumalanga Province, northeast South Africa, an area with high levels of poverty, unemployment and labour migration [34–36]. The Medical Research Council (MRC)/Wits University Rural Public Health and Health Transitions Research Unit runs the Agincourt Health and Socio-Demographic Surveillance System (AHDSS) in this area, and this was the platform for identifying eligible households and young women [37]. The purpose of the trial was to determine whether providing cash transfers to young women and their households – conditional on school attendance – reduces HIV incidence among young women. The intervention involved individually randomizing young women aged 13–20 years to receive a monthly cash transfer, conditional on school attendance. Study participants were eligible for inclusion in the trial if they were females aged 13–20 years; enrolled in grades 8, 9, 10 or 11 at selected schools in the AHDSS study site; and had a bank or post office account to receive the transfer. The participants were excluded if they were pregnant or married at baseline. Both parental/legal guardian consent and young woman consent/assent were required to participate. As part of the enrolment process, after completing the baseline interview, young women underwent pre-test counselling and then blood samples were collected and tested for HIV and HSV-2 infection. The total sample size of the trial was 2533 young women and their parent/guardian (with one young woman per household enrolled); the sample subset for this paper was 693 sexually active young women.
The exposure variable is young women who report engaging in transactional sex and the outcome variable is HIV infection.
Ethical approval for the secondary analysis was provided by the London School of Hygiene and Tropical Medicine Research Ethics Committee, and for the main trial by the University of North Carolina at Chapel Hill Institutional Review Board, the Human Research Ethics Committee (Medical) at the University of Witwatersrand, Johannesburg, and the Departments of Health and Education, Mpumalanga Province, South Africa, where the research was conducted.
Measurement tools
Young women completed computer-based questionnaires which were primarily self-administered using Audio-Computer Assisted Self-Interviewing (ACASI) and parents/guardians completed interviewer-administered, structured, computer-based household questionnaires. Information on household and socio-economic characteristics (household questionnaire) and socio-demographic background, sexual experiences and partner history (young women's questionnaire) were included in the questionnaires. Due to the personal nature of some of the questions in the young women's questionnaire (i.e. details of sexual relationships), these questions were filled out by young women directly. Both the parent/guardian and young woman's interviews were conducted in the language preferred by the participant – in the local language, xiTsonga, or English. The questionnaires were translated into xiTsonga by bilingual researchers and checked for linguistic appropriateness, comprehension and cultural relevance and then back-translated from xiTsonga into English to ensure accuracy and fidelity to meaning.
Conceptual framework and variables
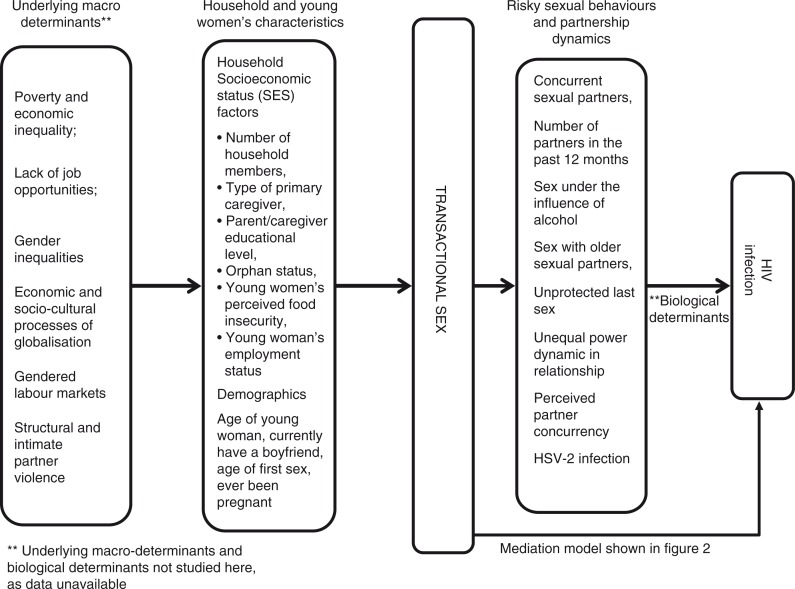
We use a modified version of the proximate-determinants framework [38] (see Figure 1) which acknowledges underlying structural and proximate factors that contribute to HIV risk, to guide our selection of confounding and mediating variables. Our conceptual framework recognizes the influence of factors such as demographic and socio-economic factors on young women's engagement in transactional sex and how certain partner dynamics or relationship characteristics might potentially mediate the relationship between transactional sex and HIV infection. While this paper is focused on the relationship between young women's engagement in transactional sex and HIV infection, a forthcoming paper explores socio-demographic factors associated with young women's engagement in transactional sex and was part of the first author's doctoral research [39].
Figure 1.
Underlying and proximate determinants associated with transactional sex and pathways through which transactional sex affects HIV risk.
Biological variables
The outcome variable HIV serostatus at baseline was assessed with two HIV rapid tests [40] done in parallel with the FDA-approved Uni-gold™ Recombigen® HIV (Trinity Biotech plc, Bray, Co. Wicklow, Ireland) and Determine™ HIV-1/2 (Alere Medical Co.Ltd, Matsudo-shi, Chiba, Japan) test. If both of the HIV rapid tests were non-reactive, no further testing was done. If one or both of the HIV rapid tests was reactive, a CD4 cell count was performed and confirmatory test was performed using an FDA-cleared Western blot test. Further details on HIV testing have been described in the HPTN 068 study protocol and the baseline paper [32,33]. HSV-2 infection testing was performed using the Herpes Simplex Virus Type 2 IgG ELISA assay (Kalon Biological, LTD Guildford, UK), with an index cut-off of 1.5 normalized optical density units. If the HSV-2 test was positive, no further HSV-2 testing was done at the study site at follow-up visits. HSV-2 results were confirmed retrospectively at the HPTN Laboratory Centre.
Main exposure variable
The main exposure variable was “having had transactional sex,” shortened to “transactional sex” and coded as a binary variable (yes/no) for sex in exchange for money and/or gifts. We asked the young woman about her sexual and relationship history with her three most recent partners, starting with the most recent partner. The four steps carried out to derive the transactional sex variable were:
Variable “transactional sex for money” coded 1 if participant said yes to “Did you feel like you had to have sex with [initials] because they gave you money”?;
Variable “transactional sex for gifts” coded 1 if participant said yes to “Did you feel like you had to have sex with [initials] because they gave you things (such as airtime, cell phone, groceries, clothes or shoes, perfume or lotions, make-up, cool-drinks, sweets or chips, CDs, DVDs or videos, alcohol or drugs, flowers, other (specify))”?;
Variable “transactional sex for money and gifts” coded 1 if participant had said yes to question (1) “Did you feel like you had to have sex with [initials] because they gave you money”? and question (2) “Did you feel like you had to have sex with [initials] because they gave you things”?;
The final variable “transactional sex for money and/or gifts” coded 1 if participant said yes to “Did you feel like you had to have sex with [initials] because they gave you money”? or “Did you feel like you had to have sex with [initials] because they gave you gifts or both gifts and money”?
Mediating variables
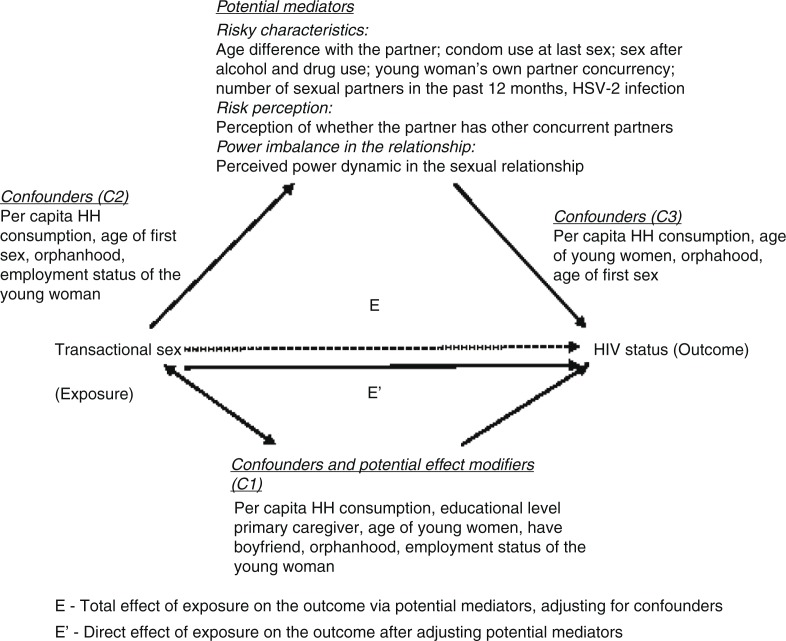
Potential mediators around partner characteristics and certain relationship dynamics were selected based on a review of the literature, as shown in our proximate-determinants conceptual framework (Figure 1) and their possible role as mechanisms through which transactional sex works to affect HIV infection. These are age difference between partners, condom use at the last sexual encounter, sex under the influence of alcohol or drugs, partner concurrency by young women and her perception of partner concurrency, number of sexual partners in the past 12 months and sexual relationship power dynamics [9,23,41]. In addition, we included HSV-2 infection in the mediation analysis as young women engaging in transactional sex are more likely to be HSV-2 infected [42] and HSV-2 infection has shown to increase the risk of HIV infection [43]. Figure 2 illustrates the hypothesized mediation conceptual model between young women's engagement in transactional sex and HIV. We have described the construction of each of these variables in detail in Appendix 1.
Figure 2.
Hypothesized mediation model between young women's engagement in transactional sex and HIV infection.
Other variables
We selected the following variables from the conceptual framework as confounders based on the literature and our bivariate analysis: the age of young women, age of first sex, employment status of young women, per capita household consumption (as a measure of household living standards), educational level of primary caregiver and orphan status. Please see Appendix 1 for details on how each variable was constructed.
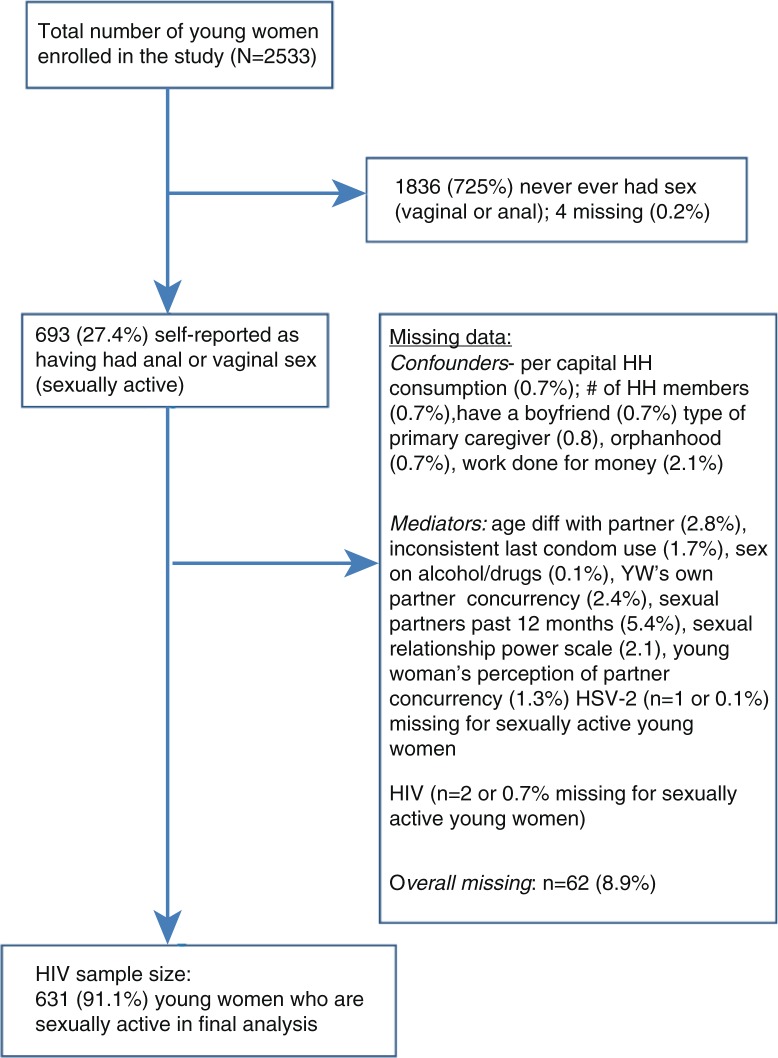
Missing data
There were little missing data in this dataset. With the exception of the variable, number of sexual partners in the past 12 months (where missing data were ~5%), almost all the exposure variables had less than 3% missing data. This includes cases where young women have “refused to answer.” The response “don't know” was also coded as missing, as the percentage of this response code was exceedingly small. No attempt was made to replace missing data and only individuals with complete data were included in the final models. Please see Figure 3 for flowchart on final sample size.
Figure 3.
Flowchart for final sample size in analysis between transactional sex and HIV infection.
Statistical analysis
Descriptive statistics were used to summarize the socio-demographic characteristics of the sample (see Table 1) and the prevalence and patterns of young women ever having engaged in transactional sex. Logistic regression models were fitted to obtain unadjusted odds ratios for the relationship between self-reported transactional sex and HIV infection.
Table 1.
Selected socio-demographic, partnership characteristics and sexual behaviours among sexually active young women (aged 13–20 years) (n=693)
| Sexually active (%) | |
|---|---|
| Socio-demographic characteristics | |
| Age of young woman (n=693) | |
| 13–15 years | 151 (21.8) |
| 16–20 years | 542 (78.2) |
| Per capita household consumptiona (n=693) | |
| Low | 220 (31.7) |
| Medium | 279 (40.3) |
| High | 194 (28.0) |
| Number of household members (n=693) | |
| 2–3 members | 87 (12.5) |
| 4–5 members | 233 (33.6) |
| 6–7 members | 220 (31.7) |
| ≥ 8 members | 153 (22.1) |
| Type of primary caregiver (n=692) | |
| Mother | 471 (68.1) |
| Father | 22 (3.2) |
| Brother/sister | 65 (9.4) |
| Other blood relative | 134 (19.4) |
| Educational level of primary caregiver (n=692) | |
| None | 176 (25.4) |
| Primary | 196 (28.3) |
| Secondary | 164 (23.7) |
| Matric or tertiary | 128 (18.5) |
| Adult basic education | 28 (4.1) |
| Orphan status (n=684) | |
| Parents alive | 475 (69.4) |
| One or both parents dead | 209 (30.6) |
| Young women's perceived food insecurityb (n=684) | |
| No | 412 (60.2) |
| Yes | 272 (39.8) |
| Partnership characteristics and sexual behaviours | |
| Currently have a boyfriend (n=693) | |
| No | 151 (21.8) |
| Yes | 542 (78.2) |
| Lifetime sexual partners (n=648) | |
| 1 | 353 (54.5) |
| 2 | 163 (25.1) |
| 3 | 61 (9.4) |
| 4–11 | 71 (11.0) |
| Sexual partners in the past 12 months (n=660) | |
| 1 | 520 (78.8) |
| 2 | 97 (14.7) |
| > 3 | 43 (6.5) |
| Age of first sex (n=634) | |
| Up to 15 years | 127 (20.0) |
| 15 years and above | 507 (80.0) |
| Ever been pregnant (n=663) | |
| No | 460 (69.4) |
| Yes | 203 (30.6) |
| Transactional sex | |
| Transactional sex (n=693) | |
| No | 596 (86) |
| Yes | 97 (14) |
| Breakdown of percentages by money | |
| or gifts or bothc (n=97) | |
| Sex in exchange for money | 58 (59.8) |
| Sex in exchange for gifts | 24 (24.7) |
| Sex in exchange for money and gifts | 15 (15.5) |
| Employment characteristics | |
| Work done for money (n=683) | |
| No | 534 (78.2) |
| Yes | 149 (21.8) |
| Main reasons for working (n=147) | |
| Want money for myself | 82 (55.8) |
| Support my family | 37 (25.2) |
| Something to do | 25 (17.0) |
| Way to meet friends | 3 (2.04) |
| Primary type of work (n=147) | |
| Sewing, hair, baking and brewing | 29 (19.7) |
| Child care | 18 (12.2) |
| Factory worker | 14 (9.5) |
| Working in a shop | 12 (8.2) |
| Other | 12 (8.2) |
| Small business assistant | 11 (7.5) |
| Domestic worker | 11 (7.5) |
| Mining | 9 (6.1) |
| Clerical and office work | 8 (5.4) |
| Transport | 6 (4.1) |
| Farm worker | 5 (3.4) |
| Informal selling | 5 (3.4) |
| Sex work | 4 (2.7) |
| Tavern or restaurant | 2 (1.4) |
| Tourism/game parks | 1 (0.7) |
| Primary source of money in the past 12 months | |
| Family | 203 (30.2) |
| Job | 180 (26.8) |
| Didn't have any money | 73 (10.9) |
| Grants (child support, disability) | 69 (10.3) |
| Boyfriend or partner | 51 (7.6) |
| Friends | 35 (5.2) |
| Begging/shoplifting, etc. | 21 (3.1) |
| Sex work | 18 (2.7) |
| Other | 12 (1.8) |
| Selling drugs | 9 (1.3) |
Measure of household living standards
young women worried about having enough food for her and her family in the past 12 months
among sexually active young women who responded yes to question on transactional sex.
Using logistic or multinomial logistic regression for binary and categorical mediators, respectively, we calculated odds ratios for the relationship between transactional sex and each potential mediating variable. Unadjusted models were fitted, as well as models adjusted for potential confounders for this association. Per capita household consumption, HSV-2 and orphan status were tested as potential effect modifiers. Overall, associations between transactional sex and each categorical potential mediating variable were assessed using the likelihood-ratio test (LRT). In this and all subsequent models, we accounted for clustering at the school level by using cluster-robust standard errors.
Mediation analysis
We used traditional mediation analysis [45] to test whether our hypothesized variables around partnership dynamics and relationship characteristics mediated the association between transactional sex and HIV. First, we estimated the total effect of the exposure on the outcome, by developing a logistic regression model for the association between transactional sex and HIV, adjusting for all potential confounders. Next, we estimated the direct effect of transactional sex on HIV by fitting a logistic regression model that included the potential mediating variable(s) and any further exposure–mediator or mediator–outcome confounders. A comparison of the total and direct effects estimated by these two models allows an assessment of the extent to which the association is mediated by the hypothesized variable(s). Each potential mediator was first considered individually and then all mediators were considered together in the same model.
Our final models only included cases with no missing data for each of the chosen mediating variables yielding a sample of 631 sexually active participants (24.9% of total n=2533 or 91.1% of sexually active women, total n=693).
Results
Characteristics of the population
The age of young women in the study sample ranged from 13 to 20 years (Table 1). From the overall sample (n=2533), just over a quarter (n=693 or 27.4%) of young women reported being sexually active, of which 78.2% were between 16 and 20 years. The mean age of first sex (vaginal and/or anal sex) in this sample was 14.7 years. Close to 30% of sexually active young women reported ever being pregnant and 6.2% (n=43) were HIV-positive. Among sexually active young women, close to 20% lived in large households with eight or more family members and almost 40% reported that they were worried that their household did not have enough food in the past year. The primary caregiver for most young women (68.1%) was their mother and a quarter of primary caregivers had never attended school; a little over a quarter (28.3%) had completed primary school and a little less than a quarter had completed secondary school (23.7%). In terms of financial independence, 21.8% of sexually active young women reported working for cash. More than half (55.8%) of these sexually active young women cited financial independence as their main reason for working. Of the young women who were sexually active, 78.2% reported having a current boyfriend, and 45.5% of sexually active young women had at least two or more sexual partners in their lifetime and 21.2% had more than two sexual partners in the past 12 months.
Overall, 14% (n=97) of sexually active young women or 3.8% of young women from the entire sample (n=2533) reported feeling as though they had to engage in “sex for money, gifts or both” (transactional sex). The majority of transactional sexual relationships were only with the current partner (67%), in comparison with one or both previous partners. Almost 60% (n=57) of young women in transactional relationships reported their current partner as their main partner with the remaining 40% (n=40) as casual partners. The majority of items were received from primary partners with 60% having received money, 25% having received gifts (such as cosmetics or airtime) and approximately 15% having received both money and gifts.
Unadjusted analysis between transactional sex and HIV
Of those young women who reported ever engaging in transactional sex, 12.4% (n=12) were HIV-positive compared with 5.2% (n=31) of those who did not report transactional sex. The unadjusted analysis indicates that young women who reported that they felt they had to engage in sex because they received money or gifts had increased odds of being HIV-positive (OR: 2.6, CI: 95%: 1.28–5.36, p=0.01) (see Table 3).
Table 3.
Unadjusted analysis and effect of transactional sex on HIV adjusted for confounders among sexually active women (n=631a)
| TS–HIV | uOR | 95% CI | p* | aORb | 95% CI | p* |
|---|---|---|---|---|---|---|
| No | Reference | 0.01 | Reference | 0.01 | ||
| Yes | 2.6 | 1.28–5.36 | 2.5 | 1.19–5.25 |
uOR, unadjusted odds ratio.
Records with missing data excluded
adjusted for confounders (age of young woman, having a boyfriend, per capita household consumption, educational level of primary caregiver, age of first sex, orphan status and work done for money).
P-value estimation through likelihood-ratio test; p<0.05 significant.
Transactional sex and mediators (partnership characteristics and relationship dynamics)
Table 2 shows unadjusted and adjusted results from the analysis of the association between transactional sex (exposure) and each of the potential variables that are hypothesized to mediate the relationship (as indicated in Figure 3) between transactional sex and HIV. The adjusted results show that young women who reported engaging in transactional sex have three times higher odds of having sex while drunk (aOR: 3.1, CI: 95% 1.55–5.71, p=0.002) and almost double the odds of engaging in concurrent partnerships (aOR: 1.86, CI: 95% 1.18–2.91, p=0.01). They also report lower scores on the Sexual Relationship Power Scale (SRPS) relative to the high score after adjusting for confounders (aOR: 1.73, CI: 95% 0.96–3.12, p=0.06) compared with those who do not report engaging in transactional sex.
Table 2.
Odds ratios from logistic/multinomial logistic regression analysis of the association between transactional sex and each mediating variable for relationship characteristics and partnership dynamics (n=693)
| Outcome | uOR | 95% CI | p* | aORa | 95% CI | p* |
|---|---|---|---|---|---|---|
| Age difference with partnerb | ||||||
| >Five years older versus up to five years older | 0.37 | 0.51 | ||||
| No TS | Reference | Reference | ||||
| TS | 1.35 | 0.69–2.66 | 1.33 | 0.40–1.58 | ||
| Same age/younger versus up to five years older | 0.56 | 0.51 | ||||
| No TS | Reference | Reference | ||||
| TS | 1.22 | 0.62–2.38 | 1.25 | 0.43–2.61 | ||
| Condom use at last sex | 0.37 | 0.33 | ||||
| No TS | Reference | Reference | ||||
| TS | 1.25 | 0.76–2.04 | 1.27 | 0.77–2.10 | ||
| Sex on alcohol or drugs | 0.01 | 0.001 | ||||
| No TS | Reference | Reference | ||||
| TS | 2.56 | 1.32–4.98 | 3.10 | 1.55–5.71 | ||
| Young women's partner concurrency | 0.07 | 0.01 | ||||
| No TS | Reference | Reference | ||||
| TS | 1.83 | 1.18–2.84 | 1.86 | 1.18–2.91 | ||
| Sexual Relationship Power Scaleb | ||||||
| Medium power versus high power | 0.73 | 0.70 | ||||
| No TS | Reference | Reference | ||||
| TS | 0.91 | 0.2–1.56 | 0.52 | 0.51–1.56 | ||
| Low power versus high power | 0.09 | 0.06 | ||||
| No TS | Reference | Reference | ||||
| TS | 1.63 | 0.93–2.86 | 1.73 | 0.96–3.12 | ||
| Young women's perception of partner concurrencyb | ||||||
| Concurrent partnership versus no concurrent partner | 0.06 | 0.06 | ||||
| No TS | Reference | Reference | ||||
| TS | 0.60 | 0.34–1.03 | 0.59 | 0.34–1.03 | ||
| Don't know versus no concurrent partner | 0.09 | 0.10 | ||||
| No TS | Reference | Reference | ||||
| TS | 0.63 | 0.37–1.09 | 0.63 | 0.36–1.09 | ||
| Sexual partners past 12 months | ||||||
| Two partners versus one partner | ||||||
| No TS | Reference | Reference | ||||
| TS | 0.98 | 0.52–1.85 | 0.95 | 0.92 | 0.48–1.77 | 0.81 |
| > Three partners versus one partner | ||||||
| No TS | Reference | Reference | ||||
| TS | 1.98 | 0.93–4.23 | 0.08 | 1.91 | 0.86–4.21 | 0.11 |
Unadjusted odds ratio estimation through logistic regression; all records with missing data excluded.
Adjusted for confounders: per capita household consumption, educational level of primary caregiver, having a boyfriend, age of first sex, age of young women and being an orphan
categorical variables – performed multinomial regression TS.
P-value calculation through likelihood-ratio test; p<0.05 significant.
Mediation analysis between transactional sex and HIV
Table 3 shows the unadjusted analysis (mentioned above) and the effect of transactional sex on HIV, after adjusting for potential confounders in the sub-sample of young women with no missing data on all potential mediators (total effect). After adjusting for confounders, young women who report engaging in transactional sex have two and a half times higher odds of being HIV-positive (aOR: 2.5, CI: 95% 1.19–5.25, p=0.01).
Table 4 shows the direct effect of transactional sex on HIV not mediated by the hypothesized variables, first presented by each mediator individually and then all potential mediators together, adjusted for confounders. Little difference exists between the adjusted estimates of the direct effect of transactional sex and HIV on each of the different mediators (models one to eight) with odds ratios ranging from 2.4 to 2.6. The overall adjusted model including all mediators demonstrates that young women who engage in transactional sex had almost triple the odds of being HIV-positive (aOR: 2.6, CI: 95%: 1.16–5.63, p=0.02).
Table 4.
Effect of transactional sex (TS) on HIV adjusted for confounders and mediators (n=631a)
| Variables | AORb | 95% CI | p* | |
|---|---|---|---|---|
| Model 1 | TSb+Age diff with partner | 0.02 | ||
| No | Reference | |||
| Yes | 2.4 | 1.23–5.86 | ||
| Model 2 | TSb+condom use at last sex | 0.01 | ||
| No | Reference | |||
| Yes | 2.5 | 1.27–5.93 | ||
| Model 3 | TSb+sex under alcohol/drugs | 0.01 | ||
| No | Reference | |||
| Yes | 2.5 | 1.27–6.03 | ||
| Model 4 | TSb+YW's partner concurrency | 0.02 | ||
| No | Reference | |||
| Yes | 2.4 | 1.22–5.77 | ||
| Model 5 | TSb+Sexual Relationship Power Scale | 0.01 | ||
| No | Reference | |||
| Yes | 2.6 | 1.30–6.17 | ||
| Model 6 | TSb+YW's perception of partner concurrency | 0.01 | ||
| No | Reference | |||
| Yes | 2.5 | 1.26–5.95 | ||
| Model 7 | TSb+sexual partners last 12 months | 0.01 | ||
| No | Reference | |||
| Yes | 2.6 | 1.28–6.12 | ||
| Model 8 | TSb+HSV-2 infection | |||
| No | Reference | |||
| Yes | 2.5 | 0.98–5.35 | 0.02 | |
| Overallb | TSb+all mediators | 0.02 | ||
| No | Reference | |||
| Yes | 2.6 | 1.16–5.63 |
Records with missing data excluded
adjusted for all confounders (age of young woman, having a boyfriend, per capita household consumption, educational level of primary caregiver, age of first sex, orphan status and work done for money)
adjusted for all mediators (age difference with partner, condom use at last sex, sex under the influence of alcohol and drugs, young women's own partner concurrency, sexual relationship power scale (SRPS), perception of partner's concurrency, sexual partner in the last 12 months, HSV-2 infection).
P-value calculated through likelihood-ratio test; p<0.05 significant.
Thus, the estimated total effect presented earlier (Table 3) of transactional sex and HIV had an odds ratio of 2.5 and the direct effect (Table 4) had an odds ratio of 2.6. Given that there is little variation in the two results, it appears that none of the hypothesized variables mediate the association between transactional sex and HIV infection.
Discussion
This cross-sectional analysis explored the prevalence of transactional sex and the relationship between transactional sex and HIV risk among a sample of sexually active secondary school girls aged 13–20 years from rural Mpumalanga, South Africa. The results show that transactional sex was associated with almost three-fold increased odds of being HIV-positive, after controlling for other risk factors. These data are consistent with observations from other settings with young women in South Africa [10,31].
Surprisingly, however, we found that the association between transactional sex and HIV was not mediated by any of the sexual risk behaviours that might help to explain the underlying pathways of HIV risk. For example, in this study, the age difference with the partner and young women's number of sexual partners do not appear to mediate the relationship between transactional sex and HIV infection. This is counter to expectation because previous research has shown that age difference with partners is associated with higher HIV risk and that young women who engage in transactional sex tend to have more sexual partners than other women [9,46]. This lack of mediation needs to be interpreted cautiously, however, as the measures used to capture certain concepts (e.g. transactional sex or sex under the influence of alcohol/drugs) still need appropriate validation. Furthermore, given the cross-sectional nature of the data, we do not know whether any of the risky sexual behaviours are the same as they were at the time of actual infection with HIV. The findings therefore highlight the need to further explore the potential pathways through which transactional sex may increase young women's risk of HIV through longitudinal data that are collected at more than one point in time [10].
The question then arises as to what other aspects of transactional sex might make it risky for HIV. It is plausible that these relationships might be part of higher risk networks and young women are made vulnerable through the underlying risk of the men that they choose to have sex with (with high risk not being marked solely by age). This corroborates work conducted by Prudden et al. Their analysis suggests that young females with multiple partners serve as a network to high-risk male partners that render them vulnerable to HIV [47]. This also aligns with evidence from DHS data that suggest that paying for sex was associated with HIV-positive serostatus among young men and a higher number of lifetime sexual partners was associated with HIV-positive serostatus among young women [48]. Hence, developing an understanding of the aspects of transactional relationships that are high risk for HIV (in terms of exposure to a network of men that are considered high risk, irrespective of the age difference) needs to be explored further [41].
Our analysis also suggests that young women who reported transactional sex are more likely to have scored low on the SRPS, to ever have had sex under the influence of alcohol or drugs and to have concurrent partners. A low score on the SRPS indicates less power in terms of relationship control, negotiation or decision-making. Thus, even though the specific variables tested did not mediate the relationship between transactional sex and HIV, there may be more complex ways in which some factors (e.g. low partnership equity, lack of consistent condom use or use of alcohol) affect HIV risk. For example, the receipt of gifts or money from a partner is often a normal part of adolescent romantic relationships in sub-Saharan Africa: accessing money or items may be a key motivating factor in such unions [49,50]. It was difficult to assess whether material gain was the primary motivation for sex in the young woman's relationship because of the way the questions on transactional sex were asked in the baseline survey (“if she feels like she had to have sex to receive money and/or gifts”). Thus, depending on how the relationship is perceived by either party (as being transactional rather than gift-based) has implications for understanding power dynamics within a relationship and can explain the low score in the SRPS among young women. For example, where there is financial motivation, women may find it hard to negotiate condom use due to the material nature of the negotiation. Alternatively, when love is the primary motivation, women may either want to get pregnant or have difficulties negotiating condom use as this may suggest a lack of trust in a partner with whom they are in love [51]. In addition, research suggests that women who receive gifts or money informally have less negotiating power than sex workers who explicitly negotiate the terms of each sexual encounter. As the exchange is not openly discussed, men may feel entitled to have sex on their terms, leaving young girls and women with little power to assert their own preferences for monogamy or protected sex [10,52]. Future rounds of the HPTN 068 survey included questions around primary motivations for engaging in transactional sex in order to capture the specific risky aspects of transactional sexual relationships that are associated with HIV risk.
Furthermore, literature from Cape Town, South Africa, suggests that alcohol may affect HIV risk through means other than its direct effect on sexual inhibition [24]. Ethnographic research suggests that some young women who frequent shebeens (township bars) do so with the expressed intention of finding men to pay for their drinks [16] and that sexual encounters usually follow [53]. Furthermore, other cross-sectional evidence from HPTN068 suggests that frequenting alcohol outlets was associated with increased sexual risk among young women [54]. It may be that men who frequent shebeens have certain characteristics and behaviours that increase their risk of being HIV-positive [55]. Indeed, other studies show evidence of clustering of risks in men: those who engage in transactional relationships may be substantially more controlling, patriarchal and violent than other men [27,56]. Thus, frequenting bars may increase women's risk because it brings them in contact with these particular types of men who are more likely to be HIV-positive [11,55] and these young women might agree to riskier sex (e.g. unprotected sex), and be less able to refuse it, when drunk.
This study had a number of strengths and limitations. In contrast to other studies, this analysis is based on a biological measure of HIV, not self-reported sexual behaviours as proxy measures for HIV, which are subject to recall bias and false reports [57]. In addition, since this research was embedded in a large randomized controlled trial funded by the HIV Prevention Trials Network (HPTN), the data were subject to rigorous quality checks [33]. However, we recognize that this paper is a secondary analysis of data and that there are limitations to how certain measures, such as transactional sex, have been conceptualized and measured. Hence, we need to take this into consideration when interpreting the findings. It is also important to mention that there are currently no validated measures of transactional sex. The first and second authors are members of an international working group (www.strive.lshtm.ac.uk/themes/transactional-sex-and-hiv) to develop better measures of transactional sex, and efforts are underway to try to improve measurement using methods, such as cognitive field-based testing, but this is work in progress.
The cross-sectional nature of the data makes the assessment of causality problematic. For example, it is difficult to assess the timing of transactional sex in relation to the acquisition of HIV. In addition, as the exposure and outcome are being measured at the same point in time, it is difficult to make a definitive case for a variable being either a confounder or mediator. For example, the decision for whether number of sexual partners should be considered as a confounder or mediator depends on how the transactional sex variable is conceptualized. If transactional sex is conceptualized as something that pre-dates most sexual activity (i.e. there is some inclination to engage in transactional sex), then one can make the case for this driving the number of sexual partners, and sexual partners would be considered to be a mediator. If, however, the motivation to engage in transactional sex is driven by the number of sexual partners (i.e. the more sexual partners a young woman has, more likely she is to engage further in transactional sex), the number of sexual partners could be a confounder of the association between transactional sex and HIV. Based on the conceptual framework, we have conceptualized the number of sexual partners as a potential mediator; as intuitively given the current context in rural South Africa where economic opportunities are circumscribed, young women are inclined to engaging in transactional sex with multiple sexual partners to fulfil their wants and needs, hence putting themselves at risk for HIV.
Furthermore, the importance of social desirability bias that plays an important role in self-reported sexual behaviours might also account for the lack of mediation in our results [58]. For instance, the expected direction of social desirability bias is that respondents will over-report condom use and under-report the number of sexual partners [59]. Even the questions around transactional sex generally tends to be under-reported as, unlike female sex workers who self-identify as sex workers, young women engaging in transactional sex seldom disclose that they have exchanged sex for money. Despite the use of methods, such as ACASI in this study, which eliminate the need for respondents to report socially undesirable answers face-to-face, it is important to acknowledge the important role that social desirability bias might play when interpreting these findings and in drawing conclusions.
As transactional sex and all the potential confounding and mediating variables are self-reported, recall bias is an issue. Question time-frames were chosen to be consistent with other studies (where applicable) and to facilitate recall (e.g. sexual partners over the past 12 months? Or condom use in the last sexual encounter?). However, individuals seldom have perfect recall of sexual events even over short time-frames and we recognize that this is a limitation. Self-completion of the questionnaire resulted in some missing data on some items. No attempts have been made to replace missing values. However, missing data were relatively uncommon and so would not be expected to cause substantial bias in the analysis that was conducted. Misclassification of transactional sex, confounding factors and mediators could lead to bias in the estimate of the total and direct effect of transactional sex on HIV and hence to incorrect conclusions regarding the extent of mediation. However, to the extent possible, we believe that all variables used in the analysis were measured as accurately as possible given the context and so significant bias is unlikely. We are confident that the presented models have been appropriately constructed and fit the data well. However, there might still be unmeasured confounding of the transactional sex–HIV relationship that needs to be considered when interpreting findings [60].
Conclusions
In conclusion, this paper lends quantitative support to the assertion that transactional sex is both fairly prevalent and an important factor in HIV risk among young women in South Africa. However, it calls into question the pathways put forward as mechanisms through which transactional sex increases HIV acquisition. The conceptualization and measurement of transactional sex is complex and efforts are underway to try to improve measurement in order to ensure that these measures have validity and are reliable. Furthermore, future surveys need to be supplemented with questions that capture primary motivations behind such relationships. This will enable a better understanding of aspects of transactional sex relationships that contribute to HIV risk. In addition, longitudinal studies that examine the complex pathways through which transactional sex may increase HIV risk will mitigate challenges of reverse causality from cross-sectional data. A potential explanation for what makes transactional sex risky for HIV may be the networks of sexually connected individuals who are considered “high risk” for HIV and the underlying risk of the men that young women have chosen as partners. Hence, adopting a structural approach that can alter the context of young people's HIV risk by moving beyond individual-level measures of knowledge towards addressing economic and structural factors that underlie HIV risk are important [61].
Acknowledgements
The authors would especially like to thank the young women and their guardians for their participation in this study, as well as the field staff and analysts at HPTN 068 and the Agincourt HDSS who spent many months collecting the data and organizing the study. Without the time and generosity of both participants and the field staff, this work would not have been possible. For this we are very grateful.
Appendix 1
Description and construction of variables
Mediating variables
We used the following steps for deriving and categorizing each measure:
Age difference with partner was calculated by first asking the age of each of the three most recent sexual partners, calculating the age difference with each partner, then calculating the mean of the three age differences to obtain a single age difference variable. This was then categorized into three groups: up to five years older than young woman; more than five years older than young woman and same age or younger than young woman. For the analysis, the category “up to five years older than young woman” served as the reference group.
Condom use at last sex with any partner was measured as a binary variable (no/yes) from the question “Did you use a condom with [initials] the last time you had sex?”
Sex on alcohol or drug use was recorded as a binary variable (no/yes) and was constructed from the questions: “Have you ever had sex while you were drunk on alcohol?” and “Have you ever had sex while you were high on drugs?”
A Sexual Relationship Power Scale (SRPS) (12 items, Cronbach's alpha=0.83), previously shown to be associated with incident HIV among in South African women [10,15] was used to measure relationship power equity. Items included questions around relationship control and decision-making dominance. Each item was assessed on a 3-point Likert scale and the measure was scored from 0 to 24 and categorized into tertiles. For the analysis, the tertile with the lowest power equity served as the reference group.
Young women's own partner concurrency was recorded as binary and coded as “1” if the woman reported additional partners during any of her last three relationships. The variable was constructed from the question: “During the time that you and […] have had a sexual relationship, have you had any other sexual partners?”
Young women's perception of her partner's concurrency was categorical and constructed from the question for any of her three partners. “As far as you know, during the time that you and [initials] have had a sexual relationship, has [initials] had any other sexual partners, such as girlfriends, wives or sex workers?” The categories were: no (concurrent partner), yes (concurrent partner) and don't know.
Young women's number of sexual partners in the past 12 months was recorded from 0 to 15 and was categorized into four groups: 0, 1, 2, >3.
Other variables
The age of young women was recorded as a continuous variable from 13 to 20 years and was re-categorized into two groups of 13–15 years and 16–20 years for equal sample size in each category.
The age of first vaginal and/or anal sex was constructed from the questions “How old were you when you first had vaginal sex? How old were you when you first had anal sex?” and re-categorized into two groups –<15 years and 15 years and older.
Employment status of the young woman was recorded as a binary variable and constructed from the question “Did you do any work for pay or family gain, including payment in kind such as food or housing?”
Per capita household consumption as a measure of living standards was calculated using the module on food and non-food spending and consumption in the household questionnaire. This was done by summing all household spending and consumption on food and non-food items and by dividing it by the number of household members (total spending and consumption per capita) [44]. A categorical household consumption measure was then obtained by dividing this measure into deciles [1–10]. For this analysis, we re-categorized the variable from deciles to three groups for total amount spending/consumption per capita: low (ranging from $1.3 to $15.4), medium (ranging from $15.5 to $32.6) and high (above $32.10).
Educational level of primary caregiver was measured as a categorical variable with four categories: none, primary, secondary, matric (year 12) and adult basic education. We measured orphan status (defined as either one or both parents deceased), as binary and constructed it from the question on if the mother was alive and if the father was alive.
Competing interests
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Authors' contributions
MR, CW, LH and AP conceived and designed the study. MR and RJS analyzed the data, and MR, CW, LH, AP, RJS, AS, CM, SDM, KK, FG, JH and EPM OL wrote the paper. AP, CM, KK and FG designed the parent study, and FG, JH, EPM, OL and AS were in charge of collection, storage, laboratory testing and analysis of data from the parent study. MR, CW, LH, AP, RJS, AS, CM, SDM, KK, FG, JH EMP and OL contributed to the interpretation of findings, critical review of manuscript and approval of final manuscript.
Funding
This research was supported by the STRIVE research programme consortium funded by UKaid from the Department for International Development. However, the views expressed do not necessarily reflect the department's official policies. Overall support for the HIV Prevention Trials Network (HPTN) was provided by the National Institute of Allergy and Infectious Diseases (NIAID), the National Institute of Mental Health (NIMH) and the National Institute on Drug Abuse (NIDA) of the National Institutes of Health (NIH) under Award Numbers UM1AI068619 (HPTN Leadership and Operations Center), UM1AI068617 (HPTN Statistical and Data Management Center) and UM1AI068613 (HPTN Laboratory Center). Additional funding was provided in part by the Division of Intramural Research, NIAID. The study was also funded under Award Number 5R01MH087118-02 and R24 HD050924 to the Carolina Population Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Allergy and Infectious Diseases or the National Institutes of Health.
References
- 1.UNAIDS. UNAIDS; Joint United Nations Programme on HIV/AIDS (UNAIDS); 2012. Global report: UNAIDS report on the global AIDS epidemic. [Google Scholar]
- 2.UNAIDS. Global AIDS response progress report [Internet] 2012. [cited 2015 Oct 10]. Available from: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_ZA_Narrative_Report.pdf.
- 3.Gilbert L, Walker L. Treading the path of least resistance: HIV/AIDS and social inequalities a South African case study. Soc Sci Med. 2002;54(7):1093–110. doi: 10.1016/s0277-9536(01)00083-1. [DOI] [PubMed] [Google Scholar]
- 4.Dellar RC, Dlamini S, Karim QA. Adolescent girls and young women: key populations for HIV epidemic control. J Int AIDS Soc. 2015;18(2 Suppl 1):19408. doi: 10.7448/IAS.18.2.19408. doi: http://dx.doi.org/10.7448/IAS.18.2.19408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson CM, Wright PF, Safrit JT, Rudy B. Epidemiology of HIV infection and risk in adolescents and youth. J Acquir Immune Defic Syndr. 2010;54(Suppl 1):S5–6. doi: 10.1097/QAI.0b013e3181e243a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cowan F, Pettifor A. HIV in adolescents in sub-Saharan Africa. Curr Opin HIV AIDS. 2009;4(4):288–93. doi: 10.1097/COH.0b013e32832c7d10. [DOI] [PubMed] [Google Scholar]
- 7.Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, et al. Cape Town, South Africa: HSRC Press; 2014. South African National HIV prevalence, incidence and behaviour survey, 2012. [DOI] [PubMed] [Google Scholar]
- 8.Rehle T, Johnson L, Hallett T, Mahy M, Kim A, Odido H, et al. A comparison of South African National HIV incidence estimates: a critical appraisal of different methods. PLoS One. 2015;10(7):e0133255. doi: 10.1371/journal.pone.0133255. doi: http://dx.doi.org/10.1371%2Fjournal.pone.0133255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ott MQ, Barnighausen T, Tanser F, Lurie MN, Newell ML. Age-gaps in sexual partnerships: seeing beyond “sugar daddies.”. AIDS. 2011;25(6):861–3. doi: 10.1097/QAD.0b013e32834344c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jewkes R, Dunkle K. Transactional sex and HIV incidence in a cohort of young women in the stepping stones trial. J AIDS Clin Res [Internet] 2012;3(5) [cited 2013 Nov 19] Available from: http://www.omicsonline.org/2155-6113/2155-6113-3-158.digital/2155-6113-3-158.html. [Google Scholar]
- 11.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–8. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 12.Jama Shai N, Jewkes R, Levin J, Dunkle K, Nduna M. Factors associated with consistent condom use among rural young women in South Africa. AIDS Care. 2010;22(11):1379–85. doi: 10.1080/09540121003758465. [DOI] [PubMed] [Google Scholar]
- 13.Stoebenau K, Nixon SA, Rubincam C, Willan S, Zembe YZN, Tsikoane T, et al. More than just talk: the framing of transactional sex and its implications for vulnerability to HIV in Lesotho, Madagascar and South Africa. Global Health. 2011;7(1):34. doi: 10.1186/1744-8603-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mojola S. Love, money, and HIV: becoming a Modern African woman in the age of AIDS. Oakland, CA: University of California Press; 2014. [Google Scholar]
- 15.Dunkle KL, Jewkes RK, Brown HC, Gray GE, Mcintryre JA, Harlow SD. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med. 2004;59:1581–92. doi: 10.1016/j.socscimed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Wojcicki JM. “She drank his money”: survival sex and the problem of violence in taverns in the Gauteng Province, South Africa. Med Anthropol Q. 2002;16(3):267–93. doi: 10.1525/maq.2002.16.3.267. [DOI] [PubMed] [Google Scholar]
- 17.MacPherson EE, Sadalaki J, Njoloma M, Nyongopa V, Nkhwazi L, Mwapasa V, et al. Transactional sex and HIV: understanding the gendered structural drivers of HIV in fishing communities in Southern Malawi. J Int AIDS Soc. 2012;15(Suppl 1):1–9. doi: 10.7448/IAS.15.3.17364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chatterji M, Murray N, London D, Anglewicz P. The factors influencing transactional sex among young men and women in 12 sub-Saharan African countries. Soc Biol. 2004;52(1–2):56–72. doi: 10.1080/19485565.2002.9989099. [DOI] [PubMed] [Google Scholar]
- 19.Zembe YZ, Townsend L, Thorson A, Ekström AM. “Money talks, bullshit walks” interrogating notions of consumption and survival sex among young women engaging in transactional sex in post-apartheid South Africa: a qualitative enquiry. Global Health. 2013;9:28. doi: 10.1186/1744-8603-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stoebenau K, Nair RC, Rambeloson V, Rakotoarison PG, Razafintsalama V, Labonté R. Consuming sex: the association between modern goods, lifestyles and sexual behaviour among youth in Madagascar. Global Health. 2013;9:13. doi: 10.1186/1744-8603-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelly RJ, Gray RH, Sewankambo NK, Serwadda D, Wabwire-Mangen F, Lutalo T, et al. Age differences in sexual partners and risk of HIV-1 infection in rural Uganda. J Acquir Immune Defic Syndr. 2003;32(4):446–51. doi: 10.1097/00126334-200304010-00016. [DOI] [PubMed] [Google Scholar]
- 22.Beauclair R, Delva W. Is younger really safer? A qualitative study of perceived risks and benefits of age-disparate relationships among women in Cape Town, South Africa. PLoS One. 2013;8(11):e81748. doi: 10.1371/journal.pone.0081748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Norris AH, Kitali AJ, Worby E. Alcohol and transactional sex: how risky is the mix? Soc Sci Med. 2009;69(8):1167–76. doi: 10.1016/j.socscimed.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 24.Watt MH, Aunon FM, Skinner D, Sikkema KJ, Kalichman SC, Pieterse D. “Because he has bought for her, he wants to sleep with her”: alcohol as a currency for sexual exchange in South African drinking venues. Soc Sci Med. 2012;74(7):1005–12. doi: 10.1016/j.socscimed.2011.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Epstein H, Morris M. Concurrent partnerships and HIV: an inconvenient truth. J Int AIDS Soc. 2011;14(1):13. doi: 10.1186/1758-2652-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lenoir CD, Adler NE, Borzekowski DLG, Tschann JM, Ellen JM. What you don't know can hurt you: perceptions of sex-partner concurrency and partner-reported behavior. J Adolesc Health. 2006;38(3):179–85. doi: 10.1016/j.jadohealth.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 27.Dunkle K, Jewkes R. Transactional sex and economic exchange with partners among young South African men in the rural Eastern Cape: prevalence, predictors, and associations with gender-based violence. Soc Sci Med. 2007;65(6):1235–48. doi: 10.1016/j.socscimed.2007.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luke N. Age and economic asymmetries in the sexual relationships of adolescent girls in sub-Saharan Africa. Stud Fam Plann. 2003;34(2):67–86. doi: 10.1111/j.1728-4465.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- 29.Pulerwitz J, Amaro H, De Jong W, Gortmaker SL, Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14(6):789–800. doi: 10.1080/0954012021000031868. [DOI] [PubMed] [Google Scholar]
- 30.Eaton L, Flisher AJ, Aarø LE. Unsafe sexual behaviour in South African youth. Soc Sci Med. 2003;56(1):149–65. doi: 10.1016/s0277-9536(02)00017-5. [DOI] [PubMed] [Google Scholar]
- 31.Pettifor AE, Kleinschmidt I, Levin J, Rees HV, MacPhail C, Madikizela-Hlongwa L, et al. A community-based study to examine the effect of a youth HIV prevention intervention on young people aged 15–24 in South Africa: results of the baseline survey. Trop Med Int Health. 2005;10(10):971–80. doi: 10.1111/j.1365-3156.2005.01483.x. [DOI] [PubMed] [Google Scholar]
- 32.Pettifor A, MacPhail C, Selin A, Gomez-Olive FX, Rosenberg M, Wagner RG, et al. HPTN 068: a randomized control trial of a conditional cash transfer to reduce HIV infection in young women in South Africa – study design and baseline results. AIDS Behav. 2016 doi: 10.1007/s10461-015-1270-0. doi: http://dx.doi.org/10.1007/s10461-015-1270-0 [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pettifor A. A Study of the HIV Prevention Trials Network, HPTN 068 Study protocol. 2012. HPTN 068 effects of cash transfer for the prevention of HIV in young South African women. Unpublished. [Google Scholar]
- 34.Agincourt Health & Population Unit. South Africa: Agincourt Health & Population Unit; 2011. Changing lives in rural South Africa: annual research brief. [Google Scholar]
- 35.Madhavan S, Townsend N. The social context of children's nutritional status in rural South Africa. Scand J Public Health Suppl. 2007;69:107–17. doi: 10.1080/14034950701355700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collinson M, Tollman S, Kahn K. Migration, settlement change and health in post-apartheid South Africa: triangulating health and demographic surveillance with national census data. Scand J Public Health Suppl. 2007;69:77–84. doi: 10.1080/14034950701356401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kahn K, Collinson MA, Gómez-Olivé FX, Mokoena O, Twine R, Mee P, et al. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol. 2012;41(4):988–1001. doi: 10.1093/ije/dys115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boerma JT, Weir SS. Integrating demographic and epidemiological approaches to research on HIV/AIDS: the proximate-determinants framework. J Infect Dis. 2005;191(Suppl 1):S61–7. doi: 10.1086/425282. [DOI] [PubMed] [Google Scholar]
- 39.Ranganathan M. The London School of Hygiene and Tropical Medicine. London, UK: University of London; 2014. Transactional sex among young women in rural South Africa: socio-demographic factors, motivations and association with HIV infection [PhD thesis] [Google Scholar]
- 40.World Health Organization. Geneva, Switzerland: World Health Organization; 2004. Rapid HIV tests: guidelines for use in HIV testing and counselling services in resource-constrained settings. [Google Scholar]
- 41.Halperin DT, Epstein H. Concurrent sexual partnerships help to explain Africa's high HIV prevalence: implications for prevention. Lancet. 2004;364:4–6. doi: 10.1016/S0140-6736(04)16606-3. [DOI] [PubMed] [Google Scholar]
- 42.Corey L, Wald A, Celum CL, Quinn TC. The effects of the herpes simplex virus-2 on HIV-1 acquisition and transmission: a review of two overlapping epidemics. Acquir Immune Defic Syndr. 2004;35:435–45. doi: 10.1097/00126334-200404150-00001. [DOI] [PubMed] [Google Scholar]
- 43.Karim QA, Kharsany ABM, Leask K, Ntombela F, Humphries H, Frohlich J, et al. Prevalence of HIV, HSV-2 and pregnancy among high school students in rural KwaZulu-Natal, South Africa: a bio-behavioural cross-sectional survey. Sex Transm Infect. 2014;90(8):620–6. doi: 10.1136/sextrans-2014-051548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O'Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data. Washington, DC: World Bank; 2008. [Google Scholar]
- 45.Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol. 2013;42(5):1511–19. doi: 10.1093/ije/dyt127. [DOI] [PubMed] [Google Scholar]
- 46.Pettifor AE, Rees HV, Kleinschmidt I, Steffenson AE, MacPhail C, Hlongwa-Madikizela L, et al. Young people's sexual health in South Africa: HIV prevalence and sexual behaviors from a nationally representative household survey. AIDS. 2005;19(14):1525–34. doi: 10.1097/01.aids.0000183129.16830.06. [DOI] [PubMed] [Google Scholar]
- 47.Prudden HJ, Beattie TS, Bobrova N, Panovska-Griffiths J, Mukandavire Z, Gorgens M, et al. Factors Associated with Variations in Population HIV Prevalence across West Africa. Findings from an Ecological Analysis. PLoS One. 2015;10(12):e0142601. doi: 10.1371/journal.pone.0142601. doi: http://dx.doi.org/10.1371/journal.pone.0142601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Choudhry V, Ambresin A, Nyakato VN, Agardh A. Transactional sex and HIV risks evidence from a cross-sectional national survey among young people in Uganda. Glob Health Action. 2015;8:27249. doi: 10.3402/gha.v8.27249. doi: http://dx.doi.org/10.3402/gha.v8.27249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Poulin M. Sex, money, and premarital partnerships in southern Malawi. Soc Sci Med. 2007;65(11):2383–93. doi: 10.1016/j.socscimed.2007.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wamoyi J, Wight D, Plummer M, Mshana GH, Ross D. Transactional sex amongst young people in rural northern Tanzania: an ethnography of young women's motivations and negotiation. Reprod Health. 2010;7(1):2. doi: 10.1186/1742-4755-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.MacPhail C, Campbell C. “I think condoms are good but, aai, I hate those things”: condom use among adolescents and young people in a Southern African township. Soc Sci Med. 2001;52(11):1613–27. doi: 10.1016/s0277-9536(00)00272-0. [DOI] [PubMed] [Google Scholar]
- 52.Meekers D, Calves AE. “Main” girlfriends, girlfriends, marriage and money: the social context of HIV risk behaviour in sub-Saharan Africa. Heal Transit Cent. 1997;7:361–75. [PubMed] [Google Scholar]
- 53.Woolf-King SE, Maisto SA. Alcohol use and high-risk sexual behaviour in sub-Saharan Africa: a narrative review. Arch Sex Behav. 2011;40(1):17–42. doi: 10.1007/s10508-009-9516-4. [DOI] [PubMed] [Google Scholar]
- 54.Rosenberg M, Pettifor A, Van Rie A, Thirumurthy H, Emch M, Miller WC, et al. The relationship between alcohol outlets, HIV risk behavior, and HSV-2 infection among South African young women: a cross-sectional study. PLoS One. 2015;10(5):e0125510. doi: 10.1371/journal.pone.0125510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Skinner D, et al. Gender-based violence, alcohol use, and sexual risk among female patrons of drinking venues in Cape Town, South Africa. J Behav Med. 2013;36(3):295–304. doi: 10.1007/s10865-012-9423-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jewkes R, Morrell R, Sikweyiya Y, Dunkle K, Penn-Kekana L. Transactional relationships and sex with a woman in prostitution: prevalence and patterns in a representative sample of South African men. BMC Public Health. 2012;12(1):325. doi: 10.1186/1471-2458-12-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fishbein M, Pequegnat W. Evaluating AIDS prevention interventions using behavioural and biological outcome measures. Sex Transm Dis. 2000;27(2):101–10. doi: 10.1097/00007435-200002000-00008. [DOI] [PubMed] [Google Scholar]
- 58.Weinhardt LS, Forsyth AD, Carey MP, Jaworski BC, Durant LE. Reliability and validity of self-report measures of HIV-related sexual behaviour: progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27(2):155–80. doi: 10.1023/a:1018682530519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vanderweele TJ, Vansteelandt S. Odds ratios for mediation analysis for a dichotomous outcome. Am J Epidemiol. 2010;172(12):1339–48. doi: 10.1093/aje/kwq332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harrison A, Newell M-L, Imrie J, Hoddinott G. HIV prevention for South African youth: which interventions work? A systematic review of current evidence. BMC Public Health. 2010;10:102. doi: 10.1186/1471-2458-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]