Abstract
Purpose
To investigate the impact of end-systolic imaging on quality of right coronary magnetic resonance angiography (MRA) in comparison to diastolic and to study the effect of RR interval variability on image quality.
Materials and Methods
The right coronary artery (RCA) of 10 normal volunteers was imaged at 3T using parallel imaging (sensitivity encoding [SENSE]). Navigator-gated three-dimensional (3D) gradient echo was used three times: 1) end-systolic short acquisition (SS): 35-msec window; 2) diastolic short (DS): middiastolic acquisition using 35-msec window; and 3) diastolic long (DL): 75-msec diastolic acquisition window. Vectorcardiogram (VCG) data was used to analyze RR variability. Vessel sharpness, length, and diameter were compared to each other and correlated with RR variability. Blinded qualitative image scores of the images were compared.
Results
Quantitative and qualitative parameters were not significantly different and showed no significant correlation with RR variability.
Conclusion
Imaging the RCA at 3T during the end-systolic rest period using SENSE is possible without significant detrimental effect on image quality. Breaking away from the standard of imaging only during diastole can potentially improve image quality in tachycardic patients or used for simultaneous imaging during both periods in a single scan.
Keywords: coronary MRA, 3T, systolic imaging, RR variability, parallel imaging
A major technical challenge for coronary magnetic resonance angiography (MRA) is cardiac motion (1). Adverse effects of this motion on image quality can be minimized by acquiring images during the most quiescent mid-diastolic period of the cardiac cycle (2– 4) which is typically found in middiastole. This relative motion-free period occurs after relaxation of the ventricles at approximately 75% of the cardiac cycle, and depending on the heart rate, lasts for an average of 187 msec (range 66 –330 msec) (1). Both coronary MRA (2– 4) and computed tomography angiography (CTA) dose modulation (5) protocols are usually set to acquire images or reconstruct images during this period of the cardiac cycle. However, at the end of ventricular systole, (approximately 34% of the cardiac cycle) there is another relatively quiescent period that lasts for approximately 118 msec (range 0 –223 msec) (1).
Though both of these periods’ lengths have an inverse relationship with the heart rate (1), the duration of systole is less affected by heart rate variability than that of diastole (6). For example, an increase of 10% in heart rate from 70 to 77 beats per minute (BPM) should shorten diastasis, on average, from 458 msec to 395 msec (63 msec or 14%) but only change systole from 399 msec to 384 msec (15 msec or 4%) (7). Hence, for subjects with high beat-to-beat variability in their RR interval lengths, the temporal position of the middiastolic period may be more variable than that of the end-systolic period.
For these reasons, end-systolic imaging may be an alternative to more conventional diastolic imaging as a way to minimize the adverse effects of RR variability. However, the abbreviated systolic rest period necessitates image data collection in a very short acquisition window, which typically prolongs scanning time. In the present study, we used parallel imaging (sensitivity encoding [SENSE]) at 3T to abbreviate the systolic image data acquisition window to 35 msec. The purpose of this study was to investigate the impact of end-systolic imaging on the quality of right coronary MRA in comparison to more conventional diastolic imaging. Simultaneously, the effect of RR variability on image quality was studied for both end-systolic and late diastolic data acquisitions.
MATERIALS AND METHODS
The right coronary artery (RCA) of 10 healthy adult subjects (three males, 23–45 years old) was imaged on a 3T Intera scanner (Philips Medical System, Best, The Netherlands) using a six element cardiac coil for signal reception. All subjects provided informed consent to be included in the study, which was approved by the Institutional Review Board. Initial scout scans were performed as previously described by Stuber et al (8). An axial midventricular vector electrocardiographic (VCG)-gated (9) cine-balanced steady-state free precession (SSFP) sequence was used to determine the most quiescent periods at end systole and end diastole (TR = 3.6 msec, TE = 1.8 msec, α = 45°, 50 frames per second). The cine images were analyzed using the “FREEZE” tool (research software, (10)) to automatically identify optimum end-systolic and diastolic quiescent periods with a duration of 35 msec. Additionally, a 75-msec quiescent period during diastole was identified. The values produced by the FREEZE tool were entered in the scan parameters as the trigger delay for coronary acquisitions. These values were used to acquire two sets of 3D segmented k-space gradient-echo low resolution, navigator, and VCG-gated whole-heart scans for localization of the RCA at end-systole and in middiastole. For volume targeting of the RCA, a previously reported three-point planscan tool was used (11). A 3D navigator-gated and vector electrocardiographic (VCG) R-wave triggered sequence with adiabatic T2-Prep (12) and fat saturation was then used to image the RCA of each subject in three different scans, applied in random order using the following parameters:
End-systolic short acquisition (SS): ~35 msec acquisition window at end-systole. TR = 7.6 msec, TE = 2.2 msec, α = 20°, turbo factor or lines per heartbeat = 5, SENSE factor = 2, field of view (FOV) of 270 × 270 mm, scan matrix of 380 × 245, in-plane resolution of 1.1 × 0.7 mm and slice thickness of 3 mm. The images were reconstructed to a matrix size of 512 × 512 (interpolation) with a resultant voxel size of 0.53 × 0.53 × 1.5 mm3.
Diastolic short acquisition (DS): middiastolic acquisition with the same imaging parameters as SS.
Diastolic long acquisition (DL): ~75 msec acquisition window with the same imaging parameters except using a doubled turbo factor of 10 and half the scan time.
Since the targeted vessel had to be imaged three times in the same volunteer; to shorten the total scan time, only the RCA was imaged since it encounters the most displacement during the cardiac cycle (1). Based on a prior publication by Johnson et al (1), the mean end-systolic rest period minus one standard deviation (SD) was 40 msec by biplanar X-ray angiography. Hence our choice of 35 msec for both the SS and DS acquisition windows. By simply doubling the turbo factor used for these acquisitions, we achieve an acquisition window of approximately 75 msec, which is well within the range of that commonly used for coronary MRA in general (8,13,14).
To assess the subjects’ RR interval length variability, the VCG and other physiological traces were recorded in nine of the 10 subjects. In the one subject VCG data was not collected due to a software malfunction. In the current study, arrhythmia rejection was not used since a further prolongation of the total scanning time (15) may not easily have been tolerated by the study subjects. The scanner-labeled R-peaks found in the traces were used to calculate RR interval lengths throughout the various coronary acquisitions. The RR variability was measured as the SD of the RR interval length (in msec and as a percent). For each of the three coronary acquisitions on each patient an RR variability value was calculated and all the values were averaged together to generate one final estimate of RR variability per volunteer. To verify the appropriateness of the SD as a measure of the variability, i.e., that the underlying distribution of interval lengths is normal, a quantile-quantile plot was used. Briefly, the mean and SD of the RR intervals was calculated and used to generate a simulated Gaussian distribution. The plot of the actual data versus the simulated distribution in quantiles (fraction of points above a given value, ranging from 0 to 100 %) and a linear regression were used to judge the quality of the fit. Only scans R2 > 0.98 were utilized for calculating the RR-interval variability for each volunteer. All coronary scans met this criterion. The Soapbubble tool (16) was then used to quantify vessel sharpness, entire visible vessel length, and vessel diameter of the reformatted RCA images. The signal-to-noise (SNR) and contrast-to-noise (CNR) ratios were not determined on purpose since noise statistics are not easily obtained on SENSE images. The reformatted images were also randomized and evaluated by two blinded readers for assessment of image quality. A previously described score of 1–4 (17) was assigned to each image by each reader individually and as a consensus read. A score of 1, indicated poor image were the coronary artery is visible, however, with markedly blurred borders or edges; 2, good image were the coronary artery is visible with moderately blurred borders or edges; 3, very good image were the coronary artery is visible with mildly blurred borders or edges; and 4, excellent image were the coronary artery is visible with sharply defined borders or edges. A paired student’s t-test with Bonferroni correction was used to compare vessel sharpness, and vessel length, while a Wilcoxon test was used for statistical comparison of the image quality scores. A linear regression analysis was used to correlate RR variability in msec to these three parameters. A P value of less than 0.05 was considered statistically significant.
RESULTS
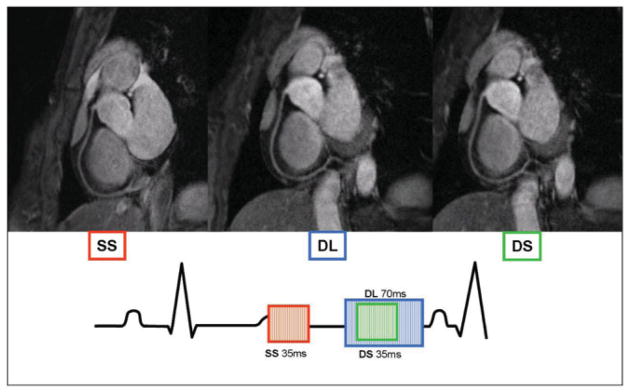
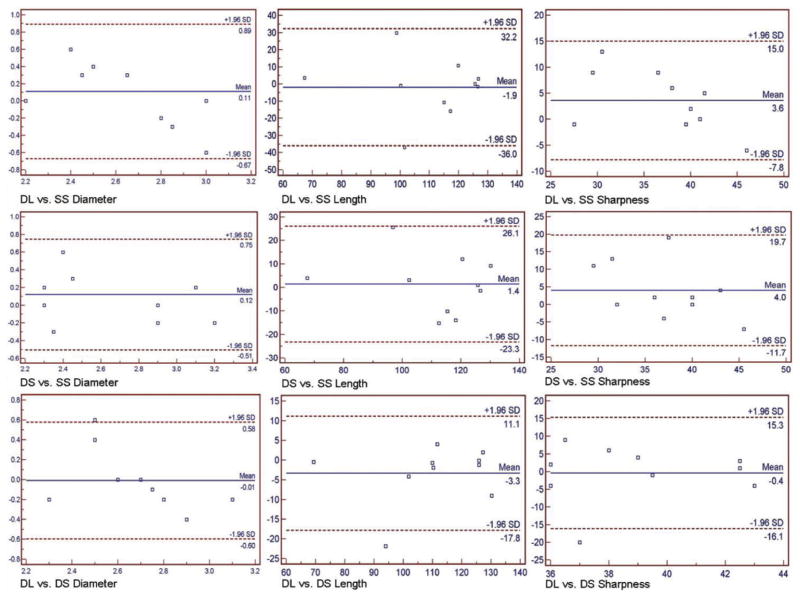
The RCA was imaged successfully in all 10 subjects using a short acquisition window during diastole and systole, and a prolonged acquisition window during diastole. An example that shows an RCA obtained with all three techniques is shown in Fig. 1. The scan time was approximately six minutes and three minutes for the short (DS, SS) and long (DL) window acquisitions, respectively. The mean trigger delay determined by the FREEZE tool for acquiring SS images was 305 msec (±60 msec), for DS images it was 668 msec (±85 msec), and for DL images it was 642 msec (±106 msec). The average vessel length, diameter, vessel sharpness, and consensus score for each technique is shown in Table 1. No statistically significant difference was found when comparing these three approaches (P = not significant [NS]). Bland Altman analysis plots (Fig. 2) demonstrate the close agreement between the techniques.
Figure 1.
Coronary MRA of the RCA obtained in the same subject in diastole using a long (blue frame) and short (green frame) acquisition window. Image acquired using a short acquisition window at end-systole (red frame). Same color scheme is used on the electrocardiogram tracing to indicate position of acquisition in the RR interval. DL = diastolic and long acquisition window, DS = diastolic and short acquisition window, SS = systolic and short acquisition window.
Table 1.
Mean and standard deviation of vessel length, sharpness and average image quality score for the three different acquisitions.
| DL | DS | SS | |
|---|---|---|---|
| Vessel Length | 109mm ± 20mm | 112mm ± 18mm | 111mm ± 21mm |
| Vessel Diameter | 2.7mm ± 0.2mm | 2.7mm ± 0.3mm | 2.6mm ± 0.4mm |
| Vessel Sharpness | 39% ± 5% | 39% ± 5% | 35% ± 8% |
| Consensus Image Quality Score | 2.4 | 2.4 | 2.7 |
DL=diastolic & long acquisition window; DS=diastolic & short acquisition window, SS=systolic & short acquisition window. All p=none significant
Figure 2.
Bland Altman analysis plots demonstrating agreement between the three different techniques when comparing vessel length (mm), diameter (mm), and sharpness (%). The Y axis is the difference between the techniques and X axis is their average. The blue line is the mean difference and red dotted line is 1.96 SD. DL = diastolic and long acquisition window; DS = diastolic and short acquisition window, SS = systolic and short acquisition window.
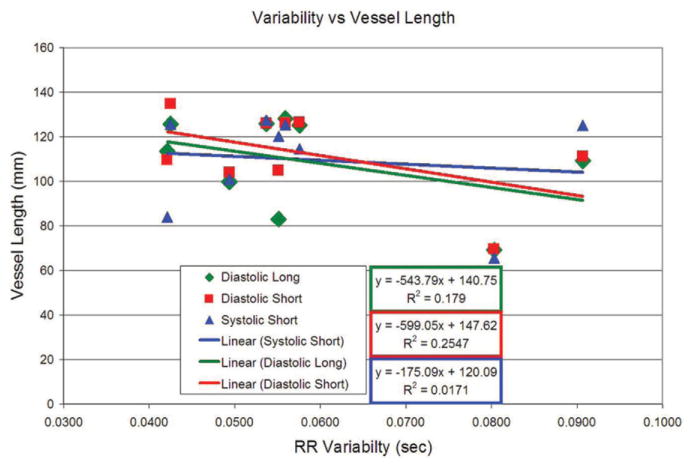
The subjects’ heart rates ranged from 55 to 100 (average 75.5 ± 13.8) BPM with a mean RR variability ranging from 42 to 91 msec with an average of 59 ± 16 msec. Of particular note, none of the qualitative parameters showed a statistically significant correlation with RR variability. The regression lines in Fig. 3 do appear to suggest a trend for reduced vessel length as a function of RR variability for diastolic RCA imaging compared to the systolic images (Fig. 3). However, if the points at RR variability of 0.08 second are removed (where the vessel lengths are the shortest) the regression lines will be essentially flat. Thus a significant relationship between RCA length and imaging at the diastolic vs. systolic phases was not established.
Figure 3.
Linear regression fits for vessel length compared to RR variability. There is an apparent trend for end-systolic short window (SS) acquisitions to be more robust in the face of RR interval variability than diastolic acquisitions. However, this trend is nonsignificant and probably results from outlying data points where the vessel length is shortest corresponding to 0.08-sec RR variability on the X-axis.
DISCUSSION
3D coronary MRA with free-breathing is a valuable non-invasive tool for the evaluation of coronary artery disease (18,19), without the use of radiation and potentially nephrotoxic contrast agents. However, the sensitivity and specificity of these techniques at 1.5T has not reached that of coronary CTA which has been reported to be as high as 95% and 98%, respectively (20). This is probably attributable to the lower SNR resulting in inferior spatial and temporal resolution compared to CT. With the advent of commercial 3T scanners, it was anticipated that these coronary MRA shortcomings might be at least partially overcome. This is due to the improved SNR that results from increased strength of the static magnetic field at 3T (8,14). However, this improved SNR did not have a significant positive effect on coronary image quality or accuracy for the detection of coronary artery disease (14). Therefore, it might be more useful to exploit this higher SNR at 3T for the improvement of temporal resolution and/or shorten overall scan time, thereby, improving image quality of the coronary arteries. This approach requires utilization of parallel imaging in the form of SENSE (21), which effectively reduces SNR. However at 3T such a reduction might be tolerated due to the SNR reserve. This concept has been demonstrated by Huber et al (22) where coronary image quality was preserved despite the two-fold reduction of scan time achieved by using SENSE at 3T. Utilizing SENSE at 3T has also been shown to be a valuable combination to shorten acquisition widows allowing for simultaneous acquisition of the right and left coronary arteries using two different 3D slabs during diastole without compromising image quality (23).
This study extends the utility of such a combination by demonstrating the feasibility of imaging the RCA at 3T during the end-systolic rest period. To date, this has never been demonstrated at 3T or 1.5T using the free-breathing technique utilized in this study. Duerinckx and Atkinson (24) did, however, demonstrate the feasibility of coronary MRA imaging during peak systole at 1.5T. In their study, Duerinckx and Atkinson (24) utilized breath-holding techniques and acquired images during peak systole using a fixed trigger delay of 150 msec irrespective of heart rate which is a different approach compared to our study were we employed free-breathing techniques and a trigger delay of approximately 305 msec (±60 msec) for end-systolic imaging; which was determined by the subjects’ heart rate and cardiac motion analysis (using the FREEZE tool). More importantly, we used a shorter acquisition window of 35 msec only for end-systolic imaging as apposed to the 117 msec window employed by Duerinckx and Atkinson (24). The use of a shortened acquisition window was made possible by taking simultaneous advantage of SENSE and the increased SNR available at 3T. By using such a short acquisition window, imaging during the abbreviated quiescent end-systolic period does not have a significant detrimental effect on image quality as demonstrated by vessel sharpness, length and diameter and subjective scoring of image quality. Utilizing such a short acquisition window comes at the expense of an increase in scan time which may carry the risk of patient bulk motion and/or diaphragmatic drift. A resultant decrease in navigator efficiency and a reduced image quality may therefore be expected. However, by also including DS acquisitions with imaging time equivalent to that of the SS acquisitions, we have demonstrated that shortening the acquisition window does not significantly affect image quality. The lack of SNR measurement is a relative limitation of this study. However, this may have been a misleading measurement because of the use of SENSE, which results in a high variability of noise across the FOV. Since the same parameters and SENSE were used for all the acquisitions, it was felt that changing the turbo factor should not significantly affect SNR and that vessel sharpness, length, diameter, and subjective image quality score would be good indicators of any deleterious impact of imaging at end-systole. Another limitation is that we did not test the effects of RR variability rejection algorithms on image quality. This would have required scanning the subjects’ RCA six times in one setting which would have doubled the overall scan time and may have added motion artifacts due to subjects’ discomfort.
Although, there is no statistically significant effect of RR variability on all three techniques, imaging during end-systole appears to be least affected by such variability as suggested by the vessel length comparisons shown in Fig. 3. This is probably because the variability affects the longer diastolic aspect of the cardiac cycle more than the shorter systolic aspect which would have less room for change from one heart beat to the next. However, we do acknowledge that this trend is nonsignificant and may be attributable to only a few outlying data points. Nonetheless, we have demonstrated that end-systolic imaging using a short acquisition window is a valuable alternative, which has to be considered in individuals with RR variabilities or in patients with short or nonexistent middiastolic rest periods. Further studies in tachycardic patients will be needed to define these advantages more clearly.
In conclusion imaging during the middiastolic period has been successful enough that it is an integral part of both MR and CT angiography strategies. This study demonstrates that it is possible to break away from the standard of imaging during diastole only. This is made possible by exploiting the higher SNR at 3T, which allows for the implementation of SENSE to utilize shorter acquisition windows without any detrimental effect on image quality. Acquisition at end-systole can potentially improve image quality in tachycardic patients with short RR intervals or in patients with high heart rate variability. Another potential application is simultaneous imaging during both periods in a single scan to acquire, for example, the slab targeting the left coronary artery during end-systole and the RCA during diastole. Further studies using the coronary artery disease population would be beneficial to further identify any potential advantages of imaging during end-systole.
Footnotes
Dr. Stuber is compensated as a consultant by Philips Medical Systems NL, the manufacturer of equipment described in this manuscript. The terms of this arrangement have been approved by the Johns Hopkins University in accordance with its conflict of interest policies.
References
- 1.Johnson KR, Patel SJ, Whigham A, Hakim A, Pettigrew RI, Oshinski JN. Three-dimensional, time-resolved motion of the coronary arteries. J Cardiovasc Magn Reson. 2004;6:663–673. doi: 10.1081/jcmr-120038086. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Watts R, Mitchell I, et al. Coronary MR angiography: selection of acquisition window of minimal cardiac motion with electrocardiography-triggered navigator cardiac motion prescanning—initial results. Radiology. 2001;218:580–585. doi: 10.1148/radiology.218.2.r01fe46580. [DOI] [PubMed] [Google Scholar]
- 3.Hofman MB, Wickline SA, Lorenz CH. Quantification of in-plane motion of the coronary arteries during the cardiac cycle: implications for acquisition window duration for MR flow quantification. J Magn Reson Imaging. 1998;8:568–576. doi: 10.1002/jmri.1880080309. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Vidan E, Bergman GW. Cardiac motion of coronary arteries: variability in the rest period and implications for coronary MR angiography. Radiology. 1999;213:751–758. doi: 10.1148/radiology.213.3.r99dc41751. [DOI] [PubMed] [Google Scholar]
- 5.Schoenhagen P, Halliburton SS, Stillman AE, et al. Noninvasive imaging of coronary arteries: current and future role of multi-detector row CT. Radiology. 2004;232:7–17. doi: 10.1148/radiol.2321021803. [DOI] [PubMed] [Google Scholar]
- 6.Richard A, Hull E. Essentials of electrocardiography. New York: Macmillan; 1941. [Google Scholar]
- 7.Weissler AM, Harris WS, Schoenfeld CD. Systolic time intervals in heart failure in man. Circulation. 1968;37:149–159. doi: 10.1161/01.cir.37.2.149. [DOI] [PubMed] [Google Scholar]
- 8.Stuber M, Botnar RM, Fischer SE, et al. Preliminary report on in vivo coronary MRA at 3 Tesla in humans. Magn Reson Med. 2002;48:425–429. doi: 10.1002/mrm.10240. [DOI] [PubMed] [Google Scholar]
- 9.Fischer SE, Wickline SA, Lorenz CH. Novel real-time R-wave detection algorithm based on the vectorcardiogram for accurate gated magnetic resonance acquisitions. Magn Reson Med. 1999;42:361–370. doi: 10.1002/(sici)1522-2594(199908)42:2<361::aid-mrm18>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 10.Ustun A, Desai M, Abd-Elmoniem KZ, Schar M, Stuber M. Automated identification of minimal myocardial motion for improved image quality on MR angiography at 3 T. AJR Am J Roentgenol. 2007;188:W283–W290. doi: 10.2214/AJR.06.0334. [DOI] [PubMed] [Google Scholar]
- 11.Stuber M, Botnar RM, Danias PG, et al. Double-oblique free-breathing high resolution three-dimensional coronary magnetic resonance angiography. J Am Coll Cardiol. 1999;34:524–531. doi: 10.1016/s0735-1097(99)00223-5. [DOI] [PubMed] [Google Scholar]
- 12.Nezafat R, Stuber M, Ouwerkerk R, Gharib AM, Desai MY, Pettigrew RI. B1-insensitive T2 preparation for improved coronary magnetic resonance angiography at 3 T. Magn Reson Med. 2006;55:858–864. doi: 10.1002/mrm.20835. [DOI] [PubMed] [Google Scholar]
- 13.Sakuma H, Ichikawa Y, Chino S, Hirano T, Makino K, Takeda K. Detection of coronary artery stenosis with whole-heart coronary magnetic resonance angiography. J Am Coll Cardiol. 2006;48:1946–1950. doi: 10.1016/j.jacc.2006.07.055. [DOI] [PubMed] [Google Scholar]
- 14.Sommer T, Hackenbroch M, Hofer U, et al. Coronary MR angiography at 3.0 T versus that at 1.5 T: initial results in patients suspected of having coronary artery disease. Radiology. 2005;234:718–725. doi: 10.1148/radiol.2343031784. [DOI] [PubMed] [Google Scholar]
- 15.Leiner T, Katsimaglis G, Yeh EN, et al. Correction for heart rate variability improves coronary magnetic resonance angiography. J Magn Reson Imaging. 2005;22:577–582. doi: 10.1002/jmri.20399. [DOI] [PubMed] [Google Scholar]
- 16.Etienne A, Botnar RM, Van Muiswinkel AM, Boesiger P, Manning WJ, Stuber M. “Soap-Bubble” visualization and quantitative analysis of 3D coronary magnetic resonance angiograms. Magn Reson Med. 2002;48:658–666. doi: 10.1002/mrm.10253. [DOI] [PubMed] [Google Scholar]
- 17.McConnell MV, Khasgiwala VC, Savord BJ, et al. Comparison of respiratory suppression methods and navigator locations for MR coronary angiography. AJR Am J Roentgenol. 1997;168:1369–1375. doi: 10.2214/ajr.168.5.9129447. [DOI] [PubMed] [Google Scholar]
- 18.Kim WY, Danias PG, Stuber M, et al. Coronary magnetic resonance angiography for the detection of coronary stenoses. N Engl J Med. 2001;345:1863–1869. doi: 10.1056/NEJMoa010866. [DOI] [PubMed] [Google Scholar]
- 19.Sakuma H, Ichikawa Y, Suzawa N, et al. Assessment of coronary arteries with total study time of less than 30 minutes by using whole-heart coronary MR angiography. Radiology. 2005;237:316–321. doi: 10.1148/radiol.2371040830. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann MH, Shi H, Schmitz BL, et al. Noninvasive coronary angiography with multislice computed tomography. JAMA. 2005;293:2471–2478. doi: 10.1001/jama.293.20.2471. [DOI] [PubMed] [Google Scholar]
- 21.Pruessmann KP, Weiger M, Scheidegger MB, Boesiger P. SENSE: sensitivity encoding for fast MRI. Magn Reson Med. 1999;42:952–962. [PubMed] [Google Scholar]
- 22.Huber ME, Kozerke S, Pruessmann KP, Smink J, Boesiger P. Sensitivity-encoded coronary MRA at 3T. Magn Reson Med. 2004;52:221–227. doi: 10.1002/mrm.20062. [DOI] [PubMed] [Google Scholar]
- 23.Huber ME, Kozerke S, Boesiger P. Improved artery delineation in dual-stack coronary magnetic resonance angiography using parallel imaging at 3 T. J Magn Reson Imaging. 2005;21:443–448. doi: 10.1002/jmri.20277. [DOI] [PubMed] [Google Scholar]
- 24.Duerinckx A, Atkinson DP. Coronary MR angiography during peak-systole: work in progress. J Magn Reson Imaging. 1997;7:979–986. doi: 10.1002/jmri.1880070608. [DOI] [PubMed] [Google Scholar]