Abstract
Pain is a life-long symptom in sickle cell disease (SCD) and a predictor of disease progression and mortality, but little is known about its molecular mechanisms. Here, we characterized pain in a targeted knockin mouse model of SCD (TOW mouse) that exclusively expresses human alleles encoding normal α- and sickle β-globin. TOW mice exhibited ongoing spontaneous pain behavior and increased sensitivity to evoked pain compared with littermate control mice expressing normal human hemoglobins. PKCδ activation was elevated in the superficial laminae of the spinal cord dorsal horn in TOW mice, specifically in GABAergic inhibitory neurons. Functional inhibition and neuron-specific silencing of PKCδ attenuated spontaneous pain, mechanical allodynia, and heat hyperalgesia in TOW mice. Furthermore, we took a hematopoietic stem cell transplantation approach to generating a SCD model in PKCδ-deficient mice. Neither spontaneous pain nor evoked pain was detected in the mice lacking PKCδ despite full establishment of SCD phenotypes. These findings support a critical role of spinal PKCδ in the development of chronic pain in SCD, which may become a potential target for pharmacological interventions.
Introduction
Sickle cell disease (SCD) is a deadly hereditary blood disorder, characterized by sickle-shaped red blood cells (rbc), anemia, and multiple organ failure (1). Pain is a hallmark and a predictor of disease progression and mortality in SCD. Besides acute painful vaso-occlusive crises, SCD is also accompanied by intractable chronic pain. This persistent, and often unrelieved, pain starts early in childhood and continues throughout life (2). Over half of patients reported experiencing chronic pain on more than 50% of the diary days and a third on 95% of days (3).
The neurobiological mechanisms of chronic pain in SCD remain unclear, which markedly limits effective pain management and the quality of life in patients with SCD. Transgenic mouse models have provided new insights into SCD research. Several studies have been started to characterize pain behaviors in Berkeley mice, a model of a severe form of SCD, which exhibit heat hyperalgesia, cold, and mechanical allodynia (4–6). However, Berkeley mice demonstrate unbalanced synthesis of β- and α-globin chains, indicating these mice are β-thalassemic (7). Moreover, the copy number of the transgene is not controllable and may differ greatly. Recently, another transgenic SCD mouse strain (TOW) that was originally created by T.M. Townes’ group became available to the research community (8). TOW mice were created by targeted knockin where the mouse α- and β-globin genes were replaced by the human α- and human Aγ and βS (sickle) globin genes, respectively. Mimicking humans with SCD, TOW mice complete the fetal hemoglobin switch after birth (9). Homozygous TOW mice for the human βS allele (hβS/hβS) remain viable for up to 18 months, but develop extensive rbc sickling, severe anemia, and multiple organ damage, similar to what is seen in the human disease (10).
In the present study, the TOW humanized mouse model of SCD is validated as a valuable rodent model for studying 2 distinctive pain components (nonevoked ongoing pain and evoked pain) in SCD and offers us the opportunity to gain insights into PKCδ-based mechanisms and intervention targets for chronic pain in SCD.
Results and Discussion
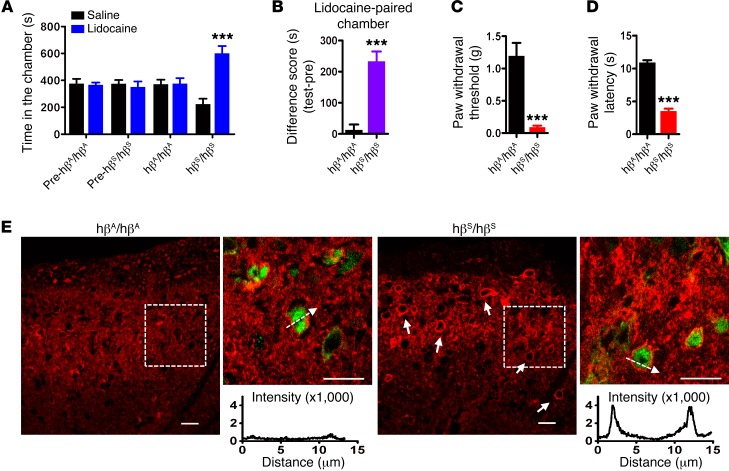
As a prevalent manifestation in patients with SCD, ongoing or nonevoked pain is rarely investigated in preclinical settings. We have validated the use of negative reinforcement to detect ongoing spontaneous pain in mice with persistent tissue or nerve injuries, where nonrewarding analgesics (e.g., lidocaine) can elicit conditioned place preference (CPP) (11, 12). Here, we applied the CPP paradigm to investigate ongoing spontaneous pain. TOW mice spent significantly more time in lidocaine-paired chambers (601 ± 54 s) than in saline-paired chambers (223 ± 40 s) after single-trial conditioning (P < 0.001, Figure 1A). In contrast, nonsickle control hβA/hβA mice spent similar amounts of time in lidocaine-paired chambers (374 ± 42 s) or saline-paired chambers (370 ± 34 s, Figure 1A). The CPP difference scores (Figure 1B), indicative of chronic pain severity, were on the same order of magnitude as those in mice after spinal nerve ligation (11), which is in agreement with the clinical observation of high pain scores in SCD (2). The result was not due to changes in locomotor function, as we found no differences in open field activity or rotarod performance between TOW and control mice (Supplemental Figure 1; supplemental material available online with this article; doi:10.1172/JCI86165DS1). This is the first direct evidence, to our knowledge, that SCD is accompanied by nonevoked spontaneous pain in mice.
Figure 1. TOW mice exhibited ongoing spontaneous pain, evoked pain, and activation of spinal PKCδ.
(A) Lidocaine (0.04%, i.t.) induced CPP in TOW (hβS/hβS) SCD mice. TOW mice spent significantly more time in lidocaine-paired chambers, whereas nonsickle control mice showed no chamber preference. (B) Difference scores between test time and preconditioning (pre) time confirmed that hβS/hβS, but not hβA/hβA, mice developed lidocaine CPP. (C) TOW mice displayed significantly reduced paw withdrawal threshold to von Frey filaments when compared with hβA/hβA mice. (D) In response to noxious radiant heat, TOW mice showed significantly shorter paw withdrawal latency compared with hA/hβA mice. Data were analyzed by ANOVA followed by Dunnett’s t test. Two-way ANOVA (pairing vs. treatment) and post hoc Bonferroni’s test were used to analyze CPP data. Difference scores were analyzed by 2-tailed paired t test. ***P < 0.001 vs. hβA/hβA. n = 8/group. (E) Immunohistochemistry showed plasma membrane translocation of PKCδ (indicated by solid arrows) in the superficial lamina region of the dorsal spinal cord in TOW, but not hβA/hβA, mice. PKCδ fluorescent intensity across representative cells (indicated by dashed arrows) is shown. Red, PKCδ; green, NeuN. Scale bars: 20 μm. n = 15 slices from 3 mice.
We next determined the nociceptive responses of TOW mice toward evoked mechanical and thermal stimuli. As compared with control mice (1.20 ± 0.20 g), TOW mice displayed significantly reduced pain threshold (0.09 ± 0.03 g) to normally innocuous von Frey filament probing (P < 0.001, Figure 1C), indicative of the presence of tactile allodynia. In addition, TOW mice exhibited shortened response latency to noxious heat stimuli applied to the hind paw (3.52 ± 0.38 s in TOW mice vs. 10.91 ± 0.36 s in control mice, P < 0.001, Figure 1D), indicating the presence of thermal hyperalgesia.
To investigate the underlying mechanisms of chronic pain in SCD, we examined PKC-mediated nociceptive signaling. We have identified PKCδ as a dual mediator of both spontaneous pain and evoked pain in peripheral neuropathy produced by paclitaxel (13). Therefore, it is compelling to investigate whether PKCδ-dependent mechanisms are relevant for chronic pain in SCD. First, we evaluated spinal PKCδ activity in TOW mice by analyzing PKCδ plasma membrane translocation. The immunoreactivity of PKCδ was primarily found in the superficial laminae of the spinal cord dorsal horn (Figure 1E). In control mice, PKCδ distributed evenly across plasma membrane and cytosol (Figure 1E). In contrast, prominent membrane enrichment of PKCδ, indicative of its activation, was observed in the superficial laminae of the spinal cord dorsal horn in TOW mice (Figure 1E). All cells with PKCδ translocation are positive for NeuN immunoreactivity (Supplemental Figure 2). On the other hand, 83% ± 7% of NeuN-positive cells had substantial PKCδ translocation (total 450 cells were imaged from 3 mice, 5 slides/mouse). Western blotting analysis also showed significant membrane translocation of PKCδ from cytosol and increased levels of phosphorylated PKCδ (p-PKCδ) in TOW mice (Supplemental Figure 3), which are consistent with hyperactivation of spinal PKCδ in TOW mice, correlating with the persistent pain state. Furthermore, PKCδ translocation occurred in GABAergic inhibitory neurons (VGAT+), but not in glutamatergic excitatory ones (VGLUT2+) (Supplemental Figure 4). Activation of PKC decreases GABA transport activity by reducing the latter’s cell surface expression (14) or catalytic efficiency (15), which suggests PKCδ may promote chronic pain in SCD through deactivation of inhibitory GABAergic mechanisms.
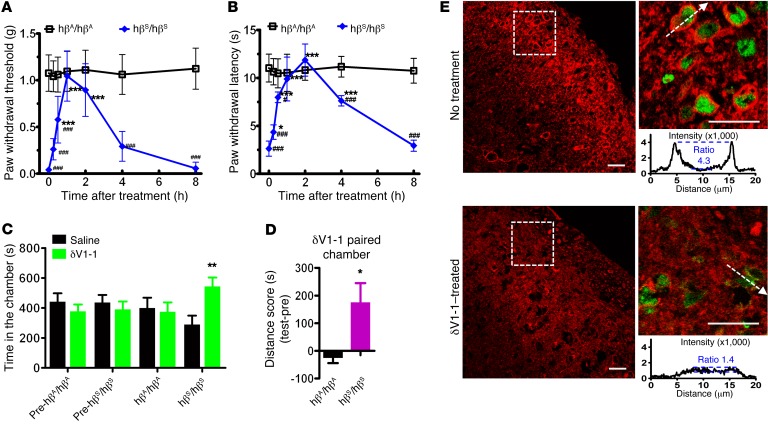
To identify the functional relevance of PKCδ in sickle cell pain, we directly targeted PKCδ in TOW and control mice by several complementary approaches. Corresponding to the amino acids 8–17 in the C2 domain of PKCδ, δV1-1 peptide is a highly selective inhibitor of PKCδ, which acts by competing for binding to its anchoring protein RACKδ (16). Mechanical hypersensitivity in TOW mice was transiently but effectively suppressed by a single intrathecal (i.t.) administration of δV1-1 (3 nmole). The peak antiallodynic effect was observed at 1 hour when the paw withdrawal threshold in TOW mice was restored to a level that was indistinguishable from that in control mice (Figure 2A). δV1-1 also significantly attenuated thermal hyperalgesia in TOW mice, with a quick onset in 15 minutes and peak antihyperalgesic effect at 2 hours, which lasted for at least 4 hours (Figure 2B). On the other hand, δV1-1 did not alter mechanical or thermal sensitivity in control mice, confirming a previous report that PKCδ does not participate in acute pain signaling (17).
Figure 2. PKCδ inhibition transiently attenuated chronic pain in TOW mice.
Mechanical (A) and thermal (B) sensitivities before (0) and after the injection of δV1-1 (3 nmole, i.t.). *P < 0.05, ***P < 0.001 vs. 0; ###P<0.001 vs. hβA/hβA. n = 8/group. (C) TOW mice spent significantly more time in δV1-1– than saline-paired chambers, whereas hβA/hβA mice spent similar amounts of time in both chambers. (D) Difference scores confirmed the presence of chamber preference to δV1-1 in TOW but not hβA/hβA mice. *P < 0.05; **P < 0.01. n = 8/group. (E) In TOW mice, plasma membrane translocation of PKCδ (indicated by dashed arrows across representative cells and corresponding fluorescent intensity plots) was abolished 30 minutes after δV1-1 injection. Red, PKCδ; green, NeuN. Scale bars: 20 μm. n = 15 slices from 3 mice. Data were analyzed by ANOVA followed by Dunnett’s t test. Two-way ANOVA (pairing vs. treatment) and post hoc Bonferroni’s test were used to analyze CPP data. Difference scores were analyzed by 2-tailed paired t test.
We next determined the participation of spinal PKCδ in ongoing pain. If the latter is mediated by PKCδ, it is expected that PKCδ inhibition would suppress ongoing pain and produce CPP in TOW mice. After being paired with δV1-1 for 30 minutes, TOW mice showed a strong preference for δV1-1–paired (543 ± 60 s) over saline-paired chambers (289 ± 60 s, P < 0.01, Figure 2C), illustrating that δV1-1 induced CPP in TOW mice. In contrast, control mice spent similar amounts of time in saline chambers (399 ± 69 s) and δV1-1 chambers (375 ± 62 s). The significant difference score (P < 0.05) generated in TOW, not control, mice confirmed the involvement of PKCδ in ongoing spontaneous pain in SCD (Figure 2D).
Enhanced spinal PKCδ translocation in TOW mice (membrane/cytosolic intensity ratio: 4.1 ± 1.2) was suppressed by δV1-1 (1.8 ± 0.7, P < 0.001) 30 minutes after injection (Figure 2E; 450 NeuN[+] cells from 3 mice/group, 5 slides/mouse). The effective inhibition of PKCδ by δV1-1 in vivo was also confirmed by Western blotting analysis, where both PKCδ translocation and p-PKCδ were reduced by δV1-1(Supplemental Figure 3). These biochemical data confirmed PKCδ inhibition by δV1-1, suggesting a causative role of PKCδ in evoked and ongoing pain associated with SCD.
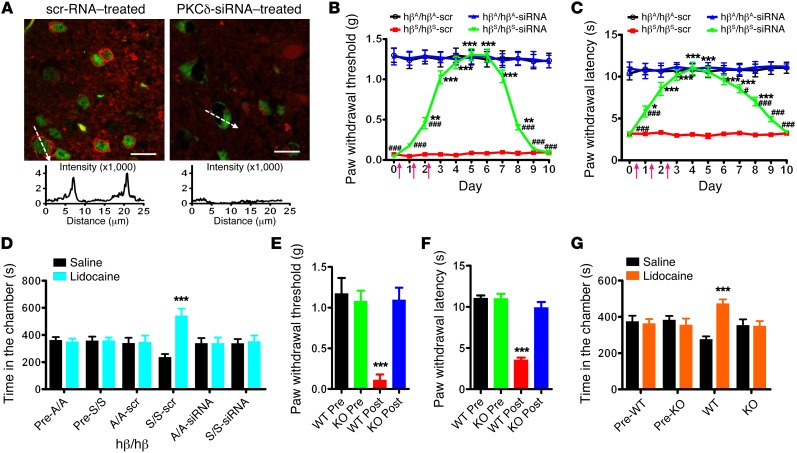
To ascertain the type of cells with PKCδ translocation, we selectively targeted neuronal PKCδ by delivering PKCδ siRNA to TOW mice in complex with RVG-9R, a chimeric peptide derived from rabies virus glycoprotein. RVG-9R enables siRNA selective binding to neurons and enhances knockdown efficiency of siRNA (18, 19). Neuronal-specific knockdown of PKCδ was observed in the spinal cord dorsal horn of TOW mice treated with RVG/siRNA for 3 days (Figure 3A and Supplemental Figure 5). Meanwhile, significant reversal of mechanical allodynia and heat hyperalgesia in TOW mice was achieved and lasted for 8 days (Figure 3, B and C). Ongoing spontaneous pain was assessed on day 4 when lidocaine elicited CPP in TOW mice treated with RVG/scrambled RNA, but not in TOW mice treated with RVG/siRNA (Figure 3D). Neuronal-specific PKCδ silencing by RVG/siRNA abolished CPP difference scores in TOW mice (Supplemental Figure 6). These data validated the essential role of neuronal PKCδ in mediating evoked and ongoing spontaneous pain in SCD.
Figure 3. Sickle cell pain behaviors in mice after neuronal PKCδ silencing and in PKCδ-KO mice.
(A) Spinal delivery of RVG-9R/PKCδ-siRNA (2 μg/d for 3 days, i.t.) specifically knocked down PKCδ (red) in NeuN-positive (green) cells. Scale bars: 20 μm. n = 15 slices from 3 mice. PKCδ fluorescent intensity across representative cells (indicated by dashed arrows) is illustrated in the chart. Mechanical (B) and thermal (C) sensitivities were tested before and after siRNA treatments. Arrows denote siRNA injections. *P < 0.05, **P < 0.01, ***P < 0.001 vs. hβS/hβS-scr; #P < 0.05, ###P < 0.001 vs. hβA/hβA-siRNA. n = 8/group. (D) When tested on day 4, lidocaine produced CPP in TOW mice treated with RVG-9R/scrambled (scr) RNA duplex, not RVG-9R/PKCδ-siRNA. ***P < 0.001. n = 6/group. (E) Mechanical allodynia and (F) thermal hyperalgesia developed in PKCδ-WT mice, not PKCδ-KO mice, after hematopoietic stem cell transplant from donor TOW mice. ***P < 0.001 vs. pre. n = 6/group. (G) Lidocaine produced CPP paradigm in PKCδ-WT mice, not PKCδ-KO mice, 4 weeks after transplant. ***P < 0.001. n = 6/group. Data were analyzed by ANOVA followed by Dunnett’s t test. Two-way ANOVA (pairing vs. treatment) and post hoc Bonferroni’s test were used to analyze CPP data
To rule out the possibility of nonspecific or incomplete targeting of PKCδ, we took another innovative approach to generating sickle cell anemia in Pkcd–/– (PKCδ-KO) mice by hematopoietic stem cell transplantation. After being conditioned with a lethal dose of total body irradiation, PKCδ-KO mice or WT littermates received bone marrow cells harvested from TOW mice. The donor hematopoietic stem cells carrying the human sickle β-globin gene were able to reconstitute the hematopoietic system of recipient mice and produce sickle cell anemia (Supplemental Figure 7). Stable engraftment was observed as early as 2 weeks after the transplant by PCR analysis (Supplemental Figure 8). Typical hematologic defects and systematic signs of SCD were established in recipient PKCδ-KO and WT mice 4 weeks after the transplant when the recipient PKCδ-KO or WT mice no longer produced mouse hematocytes, but expressed human sickle hemoglobin (Supplemental Figure 9 and Supplemental Table 1). This manipulation provided a unique approach to superimposing a TOW SCD model on a PKCδ-KO background, allowing complete deletion of PKCδ in the central nervous system and a separation neuronal mechanism of pain from that of the disease itself.
Before transplant, baseline mechanical and thermal sensitivities were not different between PKCδ-WT and PKCδ-KO mice (Figure 3, E and F). When tested 4 weeks after the transplant, recipient WT mice exhibited significantly decreased thresholds to von Frey filament probing (Figure 3E) and shortened withdrawal latencies to radiant heat stimulus (Figure 3F), which were consistent with the expression of evoked pain phenotype in SCD. In contrast, transplanted PKCδ-KO mice did not show changes in either mechanical or thermal sensitivity when compared with pretransplant baseline (Figure 3, E and F), although SCD phenotypes were fully established at that time (Supplemental Figure 9 and Supplemental Table 1).
When PKCδ-KO and WT mice were subject to the CPP test 4 weeks after transplant, recipient WT mice spent significantly more time in lidocaine-paired chambers (474 ± 23 s vs. 277 ± 15 s, P < 0.001, Figure 3G), indicating the presence of ongoing pain. In contrast, transplanted PKCδ-KO mice showed no preference for saline-paired (354 ± 32 s) or lidocaine-paired (350 ± 26 s) chambers. The difference score confirmed the existence of ongoing spontaneous pain in transplanted PKCδ-WT, but not PKCδ-KO, mice (Supplemental Figure 10). These data indicated that PKCδ is required for the initiation/development of sickle cell pain, since ongoing and evoked pain behaviors were no longer associated with SCD in transplanted PKCδ-KO mice.
In summary, we have characterized ongoing spontaneous pain, mechanical allodynia, and thermal hyperalgesia in TOW mice that closely mimic SCD in humans (8). This is the first report, to our knowledge, of the presence of ongoing spontaneous pain in a preclinical sickle cell model. Moreover, we found that spinal PKCδ, specifically that in GABAergic inhibitory neurons, is a critical mechanism for the generation and maintenance of ongoing and evoked pain in TOW mice.
While we specifically investigated PKCδ in sickle cell pain, additional studies will be necessary to determine the role of other kinases that may function alone or in concert with PKCδ for pain in SCD. For example, p38 mitogen–activated protein kinase and PKCε have been identified as mechanisms for neuropathic pain development and hyperalgesic priming (13, 20, 21). Equally important is identifying downstream effectors for PKCδ. As cold allodynia is an integral pain subtype in SCD with great clinical relevance (6), it is of great interest to investigate the regulation of cold sensors, such as transient receptor potential melastatin 8 (TRPM8) and transient receptor potential cation channel A1 (TRPA1), by spinal PKCδ in future studies (22).
Hematopoietic stem cell transplant in transgenic mice employed here may be a particularly powerful approach to elucidating central mechanisms in sickle cell pain. In this case, the vital role of CNS PKCδ in sickle cell pain was revealed. The technique can be readily applied to studying other genes. Our findings offer insights into sickle cell pain mechanisms and may ultimately lead to translational research targeting PKCδ for alleviating chronic pain in SCD.
Methods
Detailed information is available in the Supplemental Methods.
Statistics.
Data are expressed as mean ± SEM. Statistical comparisons among multiple groups were analyzed by ANOVA followed by Dunnett’s t test. Two-way ANOVA (pairing vs. treatment) was applied followed by Bonferroni’s test to analyze CPP data. Difference scores and pre/posttransplant data were analyzed using 2-tailed, paired t test. A P value of less than 0.05 was considered statistically significant.
Study approval.
All in vivo studies were carried out in accordance with the NIH Guide for the Care and Use of Laboratory Animals (National Academies Press. 2011.) after approval by the University of Illinois at Chicago IACUC.
Author contributions
YH and ZJW designed research, analyzed data, and wrote the paper. YH, JN, and RW performed experiments. REM, ROM, DJW, and JD offered advice and contributed to manuscript editing.
Supplementary Material
Acknowledgments
The study was supported by a grant from the National Heart, Lung, and Blood Institute (NHLBI) (R01HL098141). Y. He is a Sickle Cell Scholar supported by grant U01HL117658 from the NHLBI.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Reference information:J Clin Invest. 2016;126(8):3053–3057. doi:10.1172/JCI86165.
Contributor Information
Ying He, Email: yhe8@uic.edu.
Jonathan Nazari, Email: jnazari2@uic.edu.
Rui Wang, Email: rwang51@uic.edu.
Joseph DeSimone, Email: jdesimon@uic.edu.
References
- 1.Bunn HF. Pathogenesis and treatment of sickle cell disease. N Engl J Med. 1997;337(11):762–769. doi: 10.1056/NEJM199709113371107. [DOI] [PubMed] [Google Scholar]
- 2.Wilkie DJ, et al. Patient-reported outcomes: descriptors of nociceptive and neuropathic pain and barriers to effective pain management in adult outpatients with sickle cell disease. J Natl Med Assoc. 2010;102(1):18–27. doi: 10.1016/S0027-9684(15)30471-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith WR, et al. Daily assessment of pain in adults with sickle cell disease. Ann Intern Med. 2008;148(2):94–101. doi: 10.7326/0003-4819-148-2-200801150-00004. [DOI] [PubMed] [Google Scholar]
- 4.Hillery CA, et al. Transient receptor potential vanilloid 1 mediates pain in mice with severe sickle cell disease. Blood. 2011;118(12):3376–3383. doi: 10.1182/blood-2010-12-327429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kohli DR, et al. Pain-related behaviors and neurochemical alterations in mice expressing sickle hemoglobin: modulation by cannabinoids. Blood. 2010;116(3):456–465. doi: 10.1182/blood-2010-01-260372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang ZJ, Molokie RE, Wilkie DJ. Does cold hypersensitivity increase with age in sickle cell disease? Pain. 2014;155(12):2439–2440. doi: 10.1016/j.pain.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paszty C, et al. Transgenic knockout mice with exclusively human sickle hemoglobin and sickle cell disease. Science. 1997;278(5339):876–878. doi: 10.1126/science.278.5339.876. [DOI] [PubMed] [Google Scholar]
- 8.Wu LC, Sun CW, Ryan TM, Pawlik KM, Ren J, Townes TM. Correction of sickle cell disease by homologous recombination in embryonic stem cells. Blood. 2006;108(4):1183–1188. doi: 10.1182/blood-2006-02-004812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Townes TM. Gene replacement therapy for sickle cell disease and other blood disorders. Hematology Am Soc Hematol Educ Program. 2008:193–196. [DOI] [PubMed] [Google Scholar]
- 10.Hanna J, et al. Treatment of sickle cell anemia mouse model with iPS cells generated from autologous skin. Science. 2007;318(5858):1920–1923. doi: 10.1126/science.1152092. [DOI] [PubMed] [Google Scholar]
- 11.He Y, Tian X, Hu X, Porreca F, Wang ZJ. Negative reinforcement reveals non-evoked ongoing pain in mice with tissue or nerve injury. J Pain. 2012;13(6):598–607. doi: 10.1016/j.jpain.2012.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corder G, et al. Constitutive mu-opioid receptor activity leads to long-term endogenous analgesia and dependence. Science. 2013;341(6152):1394–1399. doi: 10.1126/science.1239403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.He Y, Wang ZJ. Nociceptor βII, Δ, and ε isoforms of PKC differentially mediate paclitaxel-induced spontaneous and evoked pain. J Neurosci. 2015;35(11):4614–4625. doi: 10.1523/JNEUROSCI.1580-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beckman ML, Bernstein EM, Quick MW. Multiple G protein-coupled receptors initiate protein kinase C redistribution of GABA transporters in hippocampal neurons. J Neurosci. 1999;19(11): doi: 10.1523/JNEUROSCI.19-11-j0006.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deken SL, Beckman ML, Boos L, Quick MW. Transport rates of GABA transporters: regulation by the N-terminal domain and syntaxin 1A. Nat Neurosci. 2000;3(10):998–1003. doi: 10.1038/79939. [DOI] [PubMed] [Google Scholar]
- 16.Qvit N, Mochly-Rosen D. The many hats of protein kinase CΔ: one enzyme with many functions. Biochem Soc Trans. 2014;42(6):1529–1533. doi: 10.1042/BST20140189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao C, Leitges M, Gereau RW., 4th Isozyme-specific effects of protein kinase C in pain modulation. Anesthesiology. 2011;115(6):1261–1270. doi: 10.1097/ALN.0b013e3182390788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar P, et al. Transvascular delivery of small interfering RNA to the central nervous system. Nature. 2007;448(7149):39–43. doi: 10.1038/nature05901. [DOI] [PubMed] [Google Scholar]
- 19.Berta T, et al. Extracellular caspase-6 drives murine inflammatory pain via microglial TNF-α secretion. J Clin Invest. 2014;124(3):1173–1186. doi: 10.1172/JCI72230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reichling DB, Levine JD. Critical role of nociceptor plasticity in chronic pain. Trends Neurosci. 2009;32(12):611–618. doi: 10.1016/j.tins.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jin SX, Zhuang ZY, Woolf CJ, Ji RR. p38 mitogen-activated protein kinase is activated after a spinal nerve ligation in spinal cord microglia and dorsal root ganglion neurons and contributes to the generation of neuropathic pain. J Neurosci. 2003;23(10):4017–4022. doi: 10.1523/JNEUROSCI.23-10-04017.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Premkumar LS, Raisinghani M, Pingle SC, Long C, Pimentel F. Downregulation of transient receptor potential melastatin 8 by protein kinase C-mediated dephosphorylation. J Neurosci. 2005;25(49):11322–11329. doi: 10.1523/JNEUROSCI.3006-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.