Abstract
Purpose
Systematic family-centered cancer care is needed. We conducted a randomized controlled trial of family therapy, delivered to families identified by screening to be at risk from dysfunctional relationships when one of their relatives has advanced cancer.
Patients and Methods
Eligible patients with advanced cancer and their family members screened above the cut-off on the Family Relationships Index. After screening 1,488 patients or relatives at Memorial Sloan Kettering Cancer Center or three related community hospice programs, 620 patients (42%) were recruited, which represented 170 families. Families were stratified by three levels of family dysfunction (low communicating, low involvement, and high conflict) and randomly assigned to one of three arms: standard care or 6 or 10 sessions of a manualized family intervention. Primary outcomes were the Complicated Grief Inventory-Abbreviated (CGI) and Beck Depression Inventory-II (BDI-II). Generalized estimating equations allowed for clustered data in an intention-to-treat analysis.
Results
On the CGI, a significant treatment effect (Wald χ2 = 6.88; df = 2; P = .032) and treatment by family-type interaction was found (Wald χ2 = 20.64; df = 4; P < .001), and better outcomes resulted from 10 sessions compared with standard care for low-communicating and high-conflict groups compared with low-involvement families. Low-communicating families improved by 6 months of bereavement. In the standard care arm, 15.5% of the bereaved developed a prolonged grief disorder at 13 months of bereavement compared with 3.3% of those who received 10 sessions of intervention (Wald χ2 = 8.31; df = 2; P =.048). No significant treatment effects were found on the BDI-II.
Conclusion
Family-focused therapy delivered to high-risk families during palliative care and continued into bereavement reduced the severity of complicated grief and the development of prolonged grief disorder.
INTRODUCTION
An important clinical goal is to support the families of patients with advanced cancer and eventually assist them in bereavement. Two broad approaches are used: educational and instrumental support to caregivers1 and psychosocial care to the family as a whole.2 The latter is more challenging—to be truly responsive to a family’s needs.3,4 The well-functioning family, with effective communication and mutual support, has low psychosocial morbidity3-6 and can be aided by a single meeting during palliative care to define treatment goals.7 Families with more complex needs, however, warrant early recognition and continued support to prevent morbid outcomes.5,6,8 Oncology has not had an evidence-based model for such family-centered care.
To address this problem, we developed a method of screening patients with advanced cancer and their families to define their relational functioning.9 This permits differentiation of well-functioning families from those at risk of poorer outcomes. As proof of concept, we conducted a randomized controlled trial (RCT) of the efficacy of family therapy delivered to at-risk palliative care families.10,11 This model, Family-Focused Grief Therapy (FFGT), significantly reduced distress, optimized social adjustment, and reduced rates of clinical depression in bereavement for those family members most distressed during palliative care. This preventive model of support for families who are usually considered challenging delivered beneficial outcomes.12
To replicate this work, we screened a cohort of 1,809 American patients and confirmed our ability to recognize families at risk.13 Three patterns of family relationships are found in these families: low communication (21%), low involvement (5%), and high conflict (6%).13 We then conducted a three-arm, multicenter RCT that randomly assigned families to receive standard care (SC) or six sessions or 10 sessions of FFGT. In this paper, we report the main outcome findings for bereaved family members.
PATIENTS AND METHODS
Study Design and Participants
Our RCT design stratified families by severity of family dysfunction and randomly assigned families across three intervention arms. Family members received follow-up at 6 and 13 months of bereavement. Primary outcomes were the Complicated Grief Inventory, Abbreviated (CGI) and the Beck Depression Inventory II (BDI). The study was registered with clinicaltrials.gov in December 2007.
Participants.
We screened patients with a survival prognosis of less than 1 year (on the basis of judgment of the treating oncologist) and their relatives for individual perceptions of relational functioning using the Family Relationships Index (FRI).5,9 Eligibility criteria were perception by one family member of reduced relational functioning, defined by an FRI of ≤ 9 out of 12 or a cohesion subscale < 4; geographic accessibility to treatment; children age 12 years or older who were able to complete questionnaires; and willingness of at least three family members, including the patient with cancer, to attend therapy.
Sites.
Participants were recruited between January 2006 and December 2011 from Memorial Sloan Kettering Cancer Center (n = 540), Calvary Hospital (n = 46), Visiting Nursing Service of New York (n = 22), and Beth Israel Hospice Service (n = 12). The protocol was approved by each site’s institutional review board for the conduct of ethical research.
Random Assignment and Masking
Random assignment was conducted independently by the Memorial Sloan Kettering Cancer Center protocol participant registration system. Masking was not possible for the research assistants who collected outcome data, because the longitudinal relationship with participants helped sustain retention to follow-up assessments.
Procedures
Participants were screened in outpatient clinics or homes for hospice care. When individual consents and baseline data were completed, families were randomly assigned to SC or to six or 10 therapy sessions.
The FRI is a well-validated, 12-item scale with good sensitivity to detect families that carry members with distress, depression, and poor coping.14,15 Families with low communication have FRI scores of 8 to 9; low involvement families have FRI scores of 5 to 7; high conflict families have FRI scores of 0 to 4.4,5,10
Interventionists came from the disciplines of social work, psychology, and psychiatry and were trained to deliver the manualized FFGT therapy. Sessions were audio-recorded, and 69% (327 of 474 available audio-recordings) were independently coded by three blinded assessors by using the FFGT fidelity measure.11 Peer group supervision of therapists was conducted weekly by study leaders (D.W.K., T.I.Z., M.L., L.L.), who received fidelity ratings from coders. We demonstrated our ability to train 32 therapists to competently deliver this intervention.16
FFGT has been described in two books.17,18 Families tell the story of illness. Therapists explore each family’s communication, cohesiveness, and conflict resolution alongside family values, beliefs, roles, and expectations. The same FFGT model was applied in both six- and 10-session arms.
Therapy occurred once per week for the first two meetings, then 2 weeks later for the third meeting, 1 month later for the fourth, 2 months after that for the fifth, and 3 months later for the sixth and final session.
Outcomes
The CGI is derived from its well-validated, longer version19,20 and identifies the grief symptoms proposed as criteria for prolonged grief disorder (PGD). Cronbach’s α was .885. Eleven items evaluate the frequency and intensity of grief symptoms on a five-point Likert scale. Caseness for PGD is determined by disabling separation distress; psychosocial or occupational dysfunction; and at least five of nine symptoms that prove impairment or that are experienced daily for at least 6 months of bereavement.21
The BDI-II22 is a well-validated, 21-item measure of depressive symptoms. Cronbach’s α was .911. A threshold of 20 or greater corresponds to moderate and severe depression and was used to designate caseness.23
Follow-up assessments were conducted at 6 and 13 months after death; the latter was used to avoid confounding by the anniversary of the death. When the patient improved and outlived the prognosis (17 patients [13%] did not die), CGI could not be completed; BDI was completed at 6 and 13 months after therapy.
Statistical Analysis
We used an intention-to-treat approach. The primary end points were CGI and BDI scores assessed from bereaved family members at 6 and 13 months after death. Statistical power was calculated a priori, by assuming family size of three members, intraclass correlation of 0.1 between members, and type 1 error rate of .05. With clustering into three levels of family functioning, 55 families per strata would provide 80% power for two-sided tests to detect an effect size of .33 on the BDI on the basis of the 2006 trial.11
Generalized estimating equations (GEE) were used to account for the hierarchical (correlated) outcomes, including two repeated-measures outcomes per person (6 and 13 months), and for persons nested within families.24 An exchangeable working correlation was assumed so that different family members shared the same within-family correlation. The GEE modeled the outcome reported by the bereaved family members nested within family clusters, adjusting for fixed effects of site, family type (three FRI categories), random assignment (SC or six-session or 10-session FFGT), time (6 and 13 months), and a two-way interaction between family type and random assignment. The BDI analysis included baseline BDI scores as covariates. Postbereavement BDI and CGI scores were also dichotomized into clinical cases, and a similar GEE model was fitted. An identity link function was used for continuous outcomes (BDI and CGI scores), and logit was used for binary outcomes (BDI and CGI cases). Statistical hypothesis tests were based on the Wald χ2 test. Adjusted P values were calculated to control for multiple statistical tests by using the simulated linear step-up method of Benjamini and Hochberg (1995)25 or by using empirically simulated results that exceed the fifth percentile of the 20,000 simulated distributions. Simulated multiple comparison adjustments have the advantage of not requiring statistical assumptions that may not be tenable. All modeling of the clustered data was conducted with the GENMOD and MULTITEST procedures in the statistical software package SAS (Version 9.2; SAS Institute, Cary, NC).
RESULTS
Participation
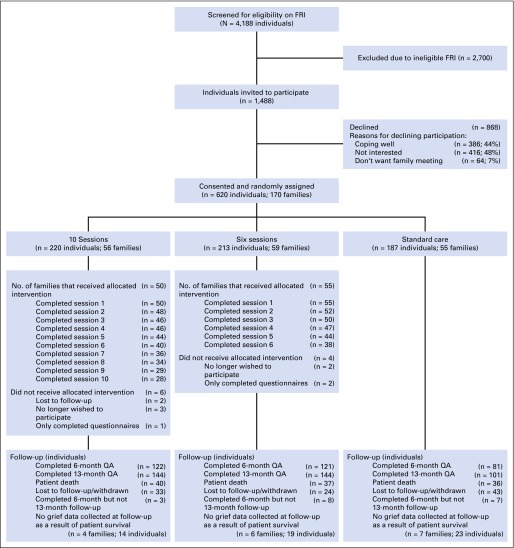
From 1,488 eligible individuals, 620 (42%) consented, which represented 170 families (mean, 3.6 individuals per family). Common reasons for refusal were disinterest, satisfactory coping, and preference not to meet as a family. As seen in the CONSORT diagram (Fig 1), 55 families were assigned to SC, 59 to six-session therapy, and 56 to 10-session therapy. A total of 91% (105 of 115 families) began therapy; retention rates were 82% (94 of 115 families) for completion of half, 64% (38 of 59 families) for completion of all six assigned sessions, and 50% (28 of 56) for completion of all 10 sessions.
Fig 1.
Consort diagram of study participants. FRI, Family Relationships Index; QA, questionnaire
Table 1 shows participant characteristics. Patients were middle aged, and offspring were mostly young adults. The sample was mostly Judeo-Christian, half were employed, and 59% married. The major cancer types that affected patients were upper gastrointestinal, including pancreatic (n = 85 [65%]); melanoma (n =13 [10%]); lung (n = 10 [8%]); breast (n = 5 [4%]); and other cancers (n = 17 [13%]). Most patients underwent a surgical procedure (90%) and received chemotherapy (89%) or radiation therapy (40%).
Table 1.
Sociodemographic Features of Study Participants (N = 620)
| Feature | Total No. (%) of Participants* | No. (%) of Participants by Intervention Type | ||
|---|---|---|---|---|
| Standard Care | Six-Session Arm | 10-Session Arm | ||
| No. of families | 170 | 55 | 59 | 56 |
| No. of individuals | 620 | 187 | 213 | 220 |
| Mean age, years | ||||
| Patients | 130 (21.0) | 55.07 | 52.81 | 58.47 |
| Partners | 112 (18.1) | 57.70 | 54.80 | 60.35 |
| Other relatives | 378 (60.9) | 33.83 | 37.58 | 40.98 |
| Sex | ||||
| Female | 372 (60.0) | 108 (57.8) | 130 (61.0) | 134 (60.9) |
| Male | 248 (40.0) | 79 (42.2) | 83 (39.0) | 86 (39.1) |
| Marital status | ||||
| Married/cohabitating | 369 (59.6) | 111 (59.4) | 124 (58.2) | 134 (60.9) |
| Single | 202 (32.6) | 65 (34.8) | 69 (32.4) | 68 (30.9) |
| Separated/divorced | 32 (5.2) | 9 (4.8) | 11 (5.2) | 12 (5.5) |
| Widowed | 17 (2.7) | 2 (1.0) | 9 (4.2) | 6 (2.7) |
| Ethnicity | ||||
| Hispanic | 68 (11) | 26 (13.9) | 11 (5.2) | 31 (14.1) |
| Non-Hispanic | 549 (88.5) | 161 (86.1) | 200 (93.9) | 188 (85.5) |
| Race | ||||
| White | 507 (81.8) | 157 (84.0) | 177 (83.1) | 173 (78.6) |
| Black | 61 (9.8) | 14 (7.5) | 24 (11.3) | 23 (10.5) |
| Asian | 20 (3.2) | 6 (3.2) | 5 (2.3) | 9 (4.1) |
| Other | 11 (1.8) | 1 (0.5) | 2 (0.9) | 8 (3.6) |
| Religious status | ||||
| Catholic | 243 (39.2) | 84 (44.9) | 64 (30.0) | 95 (43.2) |
| Jewish | 145 (23.4) | 46 (24.6) | 55 (25.8) | 44 (20.0) |
| Christian | 141 (22.7) | 32 (17.1) | 64 (30.0) | 45 (20.5) |
| Other | 39 (6.3) | 9 (4.8) | 11 (5.2) | 19 (8.6) |
| None | 50 (8.1) | 15 (8.0) | 18 (8.5) | 17 (7.7) |
| Employment status | ||||
| Employed | 313 (50.5) | 87 (46.5) | 99 (46.5) | 127 (57.7) |
| Unemployed | 89 (14.4) | 34 (18.2) | 29 (13.6) | 26 (11.8) |
| Retired | 89 (14.4) | 20 (10.7) | 35 (16.4) | 34 (15.5) |
| Student | 77 (12.4) | 24 (12.8) | 35 (16.4) | 18 (8.2) |
| Disabled | 52 (8.3) | 22 (11.8) | 15 (7.1) | 15 (6.8) |
| Family type | ||||
| Low communicating | ||||
| Individuals | 191 (30.8) | 52 (27.8) | 61 (28.6) | 78 (35.5) |
| Families | 53 (31.2) | 17 (30.9) | 17 (28.8) | 19 (33.9) |
| Low involvement | ||||
| Individuals | 313 (50.5) | 102 (54.5) | 110 (51.6) | 101 (45.9) |
| Families | 84 (49.4) | 27 (49.1) | 31 (52.5) | 26 (46.5) |
| High conflict | ||||
| Individuals | 116 (18.7) | 33 (17.7) | 42 (19.8) | 41 (18.6) |
| Families | 33 (19.4) | 11 (20.0) | 11 (18.7) | 11 (19.6) |
NOTE. Feature refers to that of the individual unless families are specified.
Column numbers do not add up to full sample size in some categories because of missing data.
Outcomes
In Table 2, for prolonged grief symptoms (ie, CGI), we examined the summary scores and found a treatment effect (P =.032) and a treatment by family-type interaction (P < .001; independent of time). To better understand this interaction, post hoc analyses (aggregated over time) showed that the interactional effect was explained by outperformance of SC by 10 sessions in low-communicating families versus in low-involvement families (adjusted P < .001) and in high-conflict families versus low-involvement families (adjusted P = .039). Additional post hoc analyses showed greater benefits from 10 sessions than from SC within low-communicating families; this difference emerged by 6 months (adjusted P = .0104) and was maintained at 13 months (adjusted P = .017). Within high-conflict families, a similar pattern was suggested; however, no difference was statistically significant. For BDI, no significant treatment effect or treatment by family-type interaction was found.
Table 2.
Effects of Treatment, Family Type, and Treatment by Family-Type Interaction on Complicated Grief and Depression in Bereaved Family Members
| Family Type and Treatment for Complicated Grief and Depression | Mean (SD) of Participants | Mean (95% CI) | Analyzed Effecta | ||||
|---|---|---|---|---|---|---|---|
| Baseline | 6-Month Bereavement | 13-Month Bereavement | Post-Bereavement Model-Estimated Average 6-13 Months | Treatment | Family Type | Treatment by Family-Type at Average of 6-13 Months | |
| CGIb | Wald χ2 = 6.88; df = 2; P = .032 | Wald χ2 = 4.01; df = 2; P = .135 | Wald χ2 = 20.64; df = 4; P < .001c | ||||
| Low communicating | |||||||
| SC | NAd | 23.6 (7.8) | 22.5 (7.9) | 23.16 (20.06 to 26.25) | |||
| Six sessions | 20.2 (9.5) | 22.6 (6.6) | 22.54 (20.18 to 24.90) | ||||
| 10 sessions | 17.6 (6.9)e | 17.0 (6.9)fg | 17.58 (15.25 to 19.91)h | ||||
| Low involvement | |||||||
| SC | NAd | 19.2 (7.0) | 16.8 (6.4) | 18.08 (15.60 to 20.56) | |||
| Six sessions | 19.9 (6.3) | 19.0 (6.9) | 19.59 (17.54 to 21.65) | ||||
| 10 sessions | 21.1 (7.9) | 19.7 (6.9) | 20.70 (18.37 to 23.03) | ||||
| High conflict | |||||||
| SC | NAd | 20.9 (8.1) | 20.4 (9.8) | 21.63 (17.40 to 25.87) | |||
| Six sessions | 20.7 (6.0) | 18.1 (6.8) | 20.19 (17.41 to 22.97) | ||||
| 10 sessions | 19.3 (8.3)i | 17.1 (6.9)j | 17.63 (14.40 to 20.85)k | ||||
| BDIl | Wald χ2 = 1.00; df = 2; P = .608 | Wald χ2 = 8.47; df = 2; P = .0145 | Wald χ2 = 4.25; df = 4; P = .374 | ||||
| Low communicating | |||||||
| SC | 13.3 (7.7) | 12.1 (10.6) | 10.9 (11.2) | 10.08 (6.77 to 13.39) | |||
| Six sessions | 13.6 (6.6) | 11.6 (7.1) | 12.8 (9.0) | 11.24 (8.44 to 14.05) | |||
| 10 sessions | 7.7 (7.1) | 7.0 (6.8) | 6.6 (6.5) | 9.49 (6.89 to 12.10) | |||
| Low involvement | |||||||
| SC | 12.2 (8.9) | 11.5 (10.6) | 8.8 (8.6) | 10.26 (7.39 to 13.14) | |||
| Six sessions | 12.0 (8.6) | 10.1 (7.7) | 9.7 (9.1) | 9.83 (7.27 to 12.39) | |||
| 10 sessions | 14.3 (9.6) | 13.6 (9.5) | 11.0 (9.3) | 11.02 (8.47 to 13.58) | |||
| High conflict | |||||||
| SC | 16.8 (11.5) | 12.4 (8.6) | 11.9 (7.8) | 8.82 (5.92 to 11.73) | |||
| Six sessions | 14.2 (9.6) | 11.0 (7.1) | 10.2 (9.8) | 8.60 (5.78 to 11.43) | |||
| 10 sessions | 10.3 (7.0) | 6.0 (6.9) | 5.7 (6.8) | 7.01 (4.73 to 9.28) | |||
NOTE. Unless noted in the footnotes, all other post hoc pairwise comparisons were nonsignificant.
Abbreviations: BDI, Beck Depression Inventory II; CGI, Complicated Grief Inventory, Abbreviated; NA, not available; SC, standard care.
Analyzed treatments were SC and six sessions or 10 sessions of family intervention. Treatment by family-type interaction on complicated grief was assessed with the CGI; BDI was used to assess depression
CGI analysis used data from 416 family members nested within 151 families.
To better understand the treatment by family-type interaction, we contrasted the treatment effect (10 sessions v SC, aggregating as per generalized estimated equations default over 6 and 13 months) between the following family types: low-communicating versus low-involvement families (−8.20; 95% adjusted CI, −12.32 to −4.08; adjusted P < .001); high-conflict versus low-involvement families (−6.63; 95% adjusted CI, −12.46 to −0.79; adjusted P = .039); high-conflict versus low-communicating families (1.57; 95% CI, −4.61 to 7.76; adjusted P =.618). A lower CGI score indicated a better outcome; thus, a negative score was the expected direction of contrast. In high-conflict families, the model-estimated treatment effect was −4 (17.63 minus 21.63), which, when contrasted against that of low-involvement families, yielded an overall estimate of −6.63 (−4 plus −2.62, after rounding). These post hoc analyses suggest that the treatment by family-type interaction resulted from greater benefits gained by low-communicating and high-conflict families than by low-involvement families in a comparison of 10-session interventions with SC. High-conflict families did not gain greater benefits than low-communicating families; their respective gains were similar.
CGI not assessed prior to death of patient.
Post hoc analyses, for CGI, within low-communicating families: at 6 months of bereavement, post hoc 10-session intervention compared with SC: mean estimated difference = −6.14 (95% adjusted CI, −11.32 to −0.97); adjusted P = .0104.
Post hoc analyses, for CGI, within low-communicating families: at 13 months of bereavement, post hoc 10 sessions compared with six sessions: mean estimated difference = −4.96 (95% adjusted CI, −9.21 to −071); adjusted P = .009.
Post hoc analyses, for CGI, within low-communicating families: at 13 months of bereavement, post hoc 10-session intervention compared with SC: mean estimated difference = −5.58 (95% adjusted CI, −10.60 to −0.56); adjusted P = .017.
Post hoc analyses, for CGI, within low-communicating families at an average of 6 to 13 months of bereavement, post hoc 10-session intervention compared with SC: mean estimated difference = −5.70 (95% adjusted CI, −10.01 to −1.40); adjusted P = .004.
Post hoc analyses, for CGI within conflictual families: at 6 months of bereavement, post hoc 10-session intervention compared with SC: mean estimated difference = −4.43 (95% adjusted CI, −10.27 to 1.41); adjusted P = .228.
Post hoc analyses, for CGI within conflictual families: at 13 months of bereavement, post hoc 10-session intervention compared with SC: mean estimated difference = −4.194 (95% adjusted CI, −11.690 to 3.302); adjusted P = .503.
Post hoc analyses, for CGI within conflictual families: at an average of 6 to 13 months of bereavement, post hoc 10-session intervention compared with SC: mean estimated difference = −3.961 (95% adjusted CI, −10.60 to 2.68); adjusted P = .378.
BDI analysis used data from 417 family members nested within 151 families; also, baseline BDI score was included as a covariate.
In Table 3, using the threshold for clinical cases on the CGI categorically, which represents a diagnosis of PGD, 15.5% family members showed caseness in SC, 12.1% in six sessions, and 3.3% in 10 sessions at 13 months of bereavement (P = .048). By combining moderate and severe levels of BDI caseness (see the Measures section) at 13 months of bereavement, the rate of clinical cases was 21% in SC compared with 11% after 10 sessions of FFGT (P = .07).
Table 3.
Observed Clinical Cases in Prolonged Grief Disorder and Depression Among Family Members in Three Intervention Conditions Over Time
| Caseness by Test and Time Point* | Family Members by Intervention Type % (No./Total No.)† | GEE Effect‡ | ||
|---|---|---|---|---|
| Standard Care | Six-Session FFGT | 10-Session FFGT | ||
| CGI | ||||
| Baseline§ | ||||
| 6-month bereavement | 19.3 (11/57) | 12.3 (13/106) | 8.9 (9/101)‖ | Treatment main effect: Wald χ2 = 8.31; df = 2; P = .016; adjusted P = .048 |
| 13-month bereavement | 15.5 (13/84) | 12.1 (15/124) | 3.3 (4/122)¶ | |
| BDI | ||||
| Baseline | 18 (23/125) | 21 (33/156) | 17 (26/155) | Baseline to 6 months: Wald χ2 = 2.63; P = .105; adjusted P = .105 |
| 6-month bereavement | 20 (15/74) | 10 (12/116) | 16 (19/116) | |
| 13-month bereavement | 21 (20/97) | 14 (19/138) | 11 (15/136) | Baseline to 13 months: Wald χ2 = 3.92; P =.047; adjusted P = .0705 |
Abbreviations: BDI, Beck Depression Inventory II; CGI, Complicated Grief Inventory; FFGT, family-focused grief therapy; GEE, generalized estimating equations.
CGI caseness applied criteria for prolonged grief disorder. BDI caseness was defined by combining cases with severe BDI scores of 29 or greater and moderate BDI scores of 20 or greater.
Test statistics were based on a GEE model of BDI caseness as a function of five covariates: study stratification factors (site and family type), treatment assignment, time (eg, 6 months v baseline), and a fifth covariate of a treatment-by-time interaction. The Wald χ2 statistics were from the Wald test for the treatment by time-interaction (eg, for BDI, 6 months v baseline and 13 months v baseline; for CGI, 6 months v 13 months).
Denominators differed because of varied family sizes and because of more surviving patients in the standard care arm (n = 7 surviving patients with 23 family members) than in the 10-session arm (n = 4 surviving patients with 14 family members) and in the six-session arm (n = 6 surviving patients with 19 family members).
CGI data not collected before death.
Post hoc analyses at 6-month bereavement for 10-session FFGT versus standard care: odds ratio, 0.442; 95% adjusted CI, 0.129 to 1.380; adjusted P = .238.
Post hoc analyses at 13-month bereavement for 10-session FFGT versus standard care: odds ratio, 0.182; 95% adjusted CI, 0.043 to 0.773; adjusted P = .014.
DISCUSSION
FFGT reduced CGI for low-communicating and high-conflict families but not for low-involvement families. The findings were robust for low-communicating families, where real gains were evident by 6 months of bereavement. Ten sessions achieved more effects than did six sessions of therapy. The low-involvement families choose distance to cope and did not benefit from family therapy.
Attachment disorders are implicated as risk factors that predispose people to PGD, and family therapy, which opens up communication, targets these relational processes. FFGT did not prevent major depression, a diagnosis for which antidepressants may be more important. Of interest, therapy was delivered to families from a variety of cultural backgrounds with apparent effectiveness; clinical accounts of these have been published elsewhere.26-28 The addition of FFGT to a comprehensive psychosocial care program can be argued to be cost effective, given that this is dispersed over 18 months and simultaneously reaches several family members.
In the real world, engagement of families is challenging, especially those featuring troubled relationships.29 The 42% rate of acceptance of our invitation to participate is modest, but this response rate was limited by the burdens of research. It is noteworthy that 91% commenced family therapy, 82% completed half of the sessions, and 50% to 64% completed all of the sessions. These are satisfactory markers of the feasibility of the model, which was taught to 32 therapists who delivered it faithfully.16 Our results do offer reassurance that it is worthwhile to target families who would be considered difficult.
A number of limitations exist with this complex study. Not all families completed their allocated sessions. Furthermore, our screening procedures relied on available patients and relatives and did not include perspectives of relatives who were less active in caregiving. Because nearly half of families who met FRI eligibility declined enrollment, our sample comprised help-seeking families who saw value in convening. The level of morbidity may be higher than evident here. Embedding family support into palliative care services may be necessary to overcome the barriers inherent in a clinical trial. Finally, power was based on testing the effect of the different doses of therapy rather than on a full interaction effect with family types. Family recruitment is challenging and restricts larger studies.
FFGT has helped to reduce PGD in families who might otherwise be difficult to care for. Given that bereavement is a major life event that results in morbid consequences for 20% of bereaved relatives,30-33 this model of family-centered care shows considerable promise.
Supplementary Material
Acknowledgment
We thank the families, therapists, research assistants, and clinical staff who contributed so much to the conduct of this study.
GLOSSARY TERMS
- psychosocial:
the psychological (emotional) and social aspects of a disease and its treatment. Some of the psychosocial aspects of cancer are its effects on patients' feelings, moods, beliefs, the way they cope, and relationships with family, friends, and coworkers.
Footnotes
Supported by National Cancer Institute RO1 Grant No. CA 115329 awarded to D.W.K.
Terms in blue are defined in the glossary, found at the end of this article and online at www.jco.org.
Authors' disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
AUTHOR CONTRIBUTIONS
Conception and design: David W. Kissane, Yuelin Li
Financial support: David W. Kissane
Administrative support: David W. Kissane
Provision of study materials or patients: David W. Kissane, Shira Hichenberg
Collection and assembly of data: David W. Kissane, Talia I. Zaider, Shira Hichenberg, Tammy Schuler, Lisa Lavelle, Francesca Del Gaudio
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Randomized Controlled Trial of Family Therapy in Advanced Cancer Continued Into Bereavement
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
David W. Kissane
No relationship to disclose
Talia I. Zaider
No relationship to disclose
Yuelin Li
No relationship to disclose
Shira Hichenberg
No relationship to disclose
Tammy Schuler
Consulting or Advisory Role: Kantar Health
Marguerite Lederberg
No relationship to disclose
Lisa Lavelle
No relationship to disclose
Rebecca Loeb
No relationship to disclose
Francesca Del Gaudio
No relationship to disclose
REFERENCES
- 1.Hudson PL, Aranda S, Kristjanson LJ. Meeting the supportive needs of family caregivers in palliative care: Challenges for health professionals. J Palliat Med. 2004;7:19–25. doi: 10.1089/109662104322737214. [DOI] [PubMed] [Google Scholar]
- 2.Loscalzo M, Clark K, Pal S, et al. Role of biopsychosocial screening in cancer care. Cancer J. 2013;19:414–420. doi: 10.1097/PPO.0b013e3182a5bce2. [DOI] [PubMed] [Google Scholar]
- 3.Kissane DW, Bloch S, Burns WI, et al. Psychological morbidity in the families of patients with cancer. Psychooncology. 1994;3:47–56. [Google Scholar]
- 4.Kissane DW, Bloch S, Burns WI, et al. Perceptions of family functioning and cancer. Psychooncology. 1994;3:259–269. [Google Scholar]
- 5.Kissane DW, Bloch S, Dowe DL, et al. The Melbourne Family Grief Study, I: Perceptions of family functioning in bereavement. Am J Psychiatry. 1996;153:650–658. doi: 10.1176/ajp.153.5.650. [DOI] [PubMed] [Google Scholar]
- 6.Kissane DW, Bloch S, Onghena P, et al. The Melbourne Family Grief Study, II: Psychosocial morbidity and grief in bereaved families. Am J Psychiatry. 1996;153:659–666. doi: 10.1176/ajp.153.5.659. [DOI] [PubMed] [Google Scholar]
- 7.Gueguen JA, Bylund CL, Brown RF, et al. Conducting family meetings in palliative care: Themes, techniques, and preliminary evaluation of a communication skills module. Palliat Support Care. 2009;7:171–179. doi: 10.1017/S1478951509000224. [DOI] [PubMed] [Google Scholar]
- 8.Kissane DW, Bloch S, McKenzie M, et al. Family grief therapy: A preliminary account of a new model to promote healthy family functioning during palliative care and bereavement. Psychooncology. 1998;7:14–25. doi: 10.1002/(SICI)1099-1611(199801/02)7:1<14::AID-PON313>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 9.Kissane DW, McKenzie M, McKenzie DP, et al. Psychosocial morbidity associated with patterns of family functioning in palliative care: Baseline data from the family focused grief therapy controlled trial. Palliat Med. 2003;17:527–537. doi: 10.1191/0269216303pm808oa. [DOI] [PubMed] [Google Scholar]
- 10.Kissane DW, McKenzie M, Bloch S, et al. Family focused grief therapy: A randomized, controlled trial in palliative care and bereavement. Am J Psychiatry. 2006;163:1208–1218. doi: 10.1176/ajp.2006.163.7.1208. [DOI] [PubMed] [Google Scholar]
- 11.Chan EK, O’Neill I, McKenzie M, et al. What works for therapists conducting family meetings: treatment integrity in family-focused grief therapy during palliative care and bereavement. J Pain Symptom Manage. 2004;27:502–512. doi: 10.1016/j.jpainsymman.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Kissane D, Lichtenthal WG, Zaider T. Family care before and after bereavement. Omega (Westport) 2007-2008;56:21–32. doi: 10.2190/om.56.1.c. [DOI] [PubMed] [Google Scholar]
- 13.Schuler TA, Zaider TI, Li Y, et al. Typology of perceived family functioning in an American sample of patients with advanced cancer. J Pain Symptom Manage. 2014;48:281–288. doi: 10.1016/j.jpainsymman.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ozono S, Saeki T, Inoue S, et al. Family functioning and psychological distress among Japanese breast cancer patients and families. Support Care Cancer. 2005;13:1044–1050. doi: 10.1007/s00520-005-0816-5. [DOI] [PubMed] [Google Scholar]
- 15.Edwards B, Clarke V. The validity of the family relationships index as a screening tool for psychological risk in families of cancer patients. Psychooncology. 2005;14:546–554. doi: 10.1002/pon.876. [DOI] [PubMed] [Google Scholar]
- 16.Del Gaudio F, Zaider TI, Brier M, et al. Challenges in providing family-centered support to families in palliative care. Palliat Med. 2012;26:1025–1033. doi: 10.1177/0269216311426919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kissane DW, Bloch S: Family Focused Grief Therapy. Buckingham, UK: Open University Press, 2002. [Google Scholar]
- 18. Kissane DW, Parnes F (eds): Bereavement Care for Families. New York, NY, Routledge, 2014. [Google Scholar]
- 19. doi: 10.1016/0165-1781(95)02757-2. Prigerson HG, Maciejewski PK, Reynolds CF III, et al: Inventory of complicated grief: A scale to measure maladaptive symptoms of loss. Psychiatry Res 59:65-79, 1995. [DOI] [PubMed] [Google Scholar]
- 20. Prigerson HG, Vabderwerker LC, Maciejewski PK: A case for inclusion of prolonged grief disorder in DSM-V, in Stroebe M, Hansson R, Schut H, Stroebe W (eds): Handbook of Bereavement Research and Practice: Advances in Theory and Intervention. Washington, DC, American Psychological Association, 2008, pp 165-186. [Google Scholar]
- 21.Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. 2009;6:e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beck AT, Steer RA, Brown GK: Manual for the Beck Depression Inventory II. San Antonio, TX, Psychological Corp, 1996. [Google Scholar]
- 23.Beck AT, Steer RA, Ball R, et al. Comparison of Beck Depression Inventories IA and II in psychiatric outpatients. J Pers Assess. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 24.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;1986:13–22. [Google Scholar]
- 25.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
- 26.Del Gaudio F, Hichenberg S, Eisenberg M, et al. Latino values in the context of palliative care: Illustrative cases from the Family Focused Grief Therapy trial. Am J Hosp Palliat Care. 2013;30:271–278. doi: 10.1177/1049909112448926. [DOI] [PubMed] [Google Scholar]
- 27.Mondia S, Hichenberg S, Kerr E, et al. The impact of Asian-American value systems on palliative care: Illustrative cases from the Family Focused Grief Therapy Trial. Am J Hospice Palliat Med. 2011;2011 doi: 10.1177/1049909111426281. [DOI] [PubMed] [Google Scholar]
- 28. Kissane DW, Boucher B, Del Gaudio F: Culture and grief in families, in Kissane DW, Parnes F (eds): Bereavement Care for Families. New York, NY, Routledge, 2014, pp 107-122. [Google Scholar]
- 29. Lichtehthal WG, Sweeney C: Families at risk of complicated bereavement, in Kissane DW, Parnes F (eds): Bereavement Care for Families. New York, NY, Routledge, 2014, pp 249-265. [Google Scholar]
- 30. Stroebe W, Stroebe MS: Determinants of adjustment to bereavement in younger widows and widowers, in Stroebe MS, Stroebe W, Hansson RO (eds): Handbook of Bereavement Theory, Research, and Intervention. Cambridge, United Kingdom, Cambridge University Press, 1993, pp 208-226. [Google Scholar]
- 31. Jacobs S: Defining the range and magnitude of the clinical complications of bereavement, in Jacobs S: Pathologic Grief: Maladaptation to Loss. Washington, DC, American Psychiatric Press, 1993, pp 39-57. [Google Scholar]
- 32. Stroebe MS, Hansson RO, Schut H, et al: Bereavement research: 21st century prospects, in Stroebe MS, Hansson RO, Schut H, Stroebe W (eds): Handbook of Bereavement Research and Practice: Advances in Theory and Practice. Washington, DC, American Psychological Association, 2008, pp 577-603. [Google Scholar]
- 33. Carr D, Jeffreys JS: Spousal bereavement in later life, in Neimeyer RA, Harris DL, Winokuer HR, Thornton GF (eds): Grief and Bereavement in Contemporary Society: Bridging Research and Practice. New York, NY, Routledge, 2011, pp 81-92. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.