Abstract
The intra- and inter-hospital patient transfer is an important aspect of patient care which is often undertaken to improve upon the existing management of the patient. It may involve transfer of patient within the same facility for any diagnostic procedure or transfer to another facility with more advanced care. The main aim in all such transfers is maintaining the continuity of medical care. As the transfer of sick patient may induce various physiological alterations which may adversely affect the prognosis of the patient, it should be initiated systematically and according to the evidence-based guidelines. The key elements of safe transfer involve decision to transfer and communication, pre-transfer stabilisation and preparation, choosing the appropriate mode of transfer, i.e., land transport or air transport, personnel accompanying the patient, equipment and monitoring required during the transfer, and finally, the documentation and handover of the patient at the receiving facility. These key elements should be followed in each transfer to prevent any adverse events which may severely affect the patient prognosis. The existing international guidelines are evidence based from various professional bodies in developed countries. However, in developing countries like India, with limited infrastructure, these guidelines can be modified accordingly. The most important aspect is implementation of these guidelines in Indian scenario with periodical quality assessments to improve the standard of care.
Keywords: Air transport, complications of patient transfer, intra-hospital, inter-hospital transfer, intra-hospital transfer guidelines, patient transfer
INTRODUCTION
The transfer of a patient to another facility or hospital or to another department in the same hospital is least known but an equally important topic. The decision to transfer the patient is based on the benefits of care available at another facility against the potential risks involved. The need to transfer a patient should take into account the benefit of providing extra care on the management or outcome. The risk of transferring a critically ill patient is manifold.[1] The various contributors of need to transfer the patient include the presence of few centres which provide super-speciality care, non-availability of speciality beds and funding of medical treatment.[2,3,4] Any intra- or inter-hospital patient transfer should aim at maintaining optimal health of the patient which is carried out by transferring the patient to the nearest facility providing highest specialised care.[5] Both the transferring and the receiving facility should aim at continuity of medical care of the patient. A poorly organised and hastily done patient transfer can significantly contribute to morbidity and mortality.[6] This article reviews the various guidelines for an effective intra- or inter-hospital transfer and current scenario of patient transfer in developing countries like India.
SEARCH OF LITERATURE
We conducted a systematic literature search using search engines such as PubMed, Google and Google Scholar with the use of following single text words and combinations: Inter-hospital transfer, inter-facility transfer, aeromedical transfer and guidelines for patient transfer. The search was performed from the year 1970 till date. The references of relevant articles were cross-checked, and articles on inter- and intra-hospital patient transfer were included.
EXISTING GUIDELINES
Different guidelines have been proposed to safely execute the patient transfer. The various professional bodies have formulated guidelines for safe patient transfer which includes American College of Critical Care Medicine, Society of Critical Care Medicine, Intensive Care Society, Association of Anaesthetist of Great Britain and Ireland and Paediatric Intensive Care Society.[7,8] All guidelines have stressed upon some key elements of safe patient transfer which will be described in detail. These key elements are same for inter- or intra-hospital transfer of patient.
KEY ELEMENTS OF PATIENT TRANSFER
Decision to transfer and communication
The decision to transfer the patient is important because of exposure of the patient and the staff to additional risk and additional expense for the relatives and the hospital. The decision to transfer the patient is taken by a senior consultant level doctor after thorough discussion with patient's relatives about the benefits and risks involved. A written and informed consent of patient's relatives along with the reason to transfer is mandatory before the transfer. In some countries, dedicated critical care transfer groups have been established to coordinate and facilitate the patient transfer. These groups also arrange appropriate facilities at the receiving hospital or facility.[9,10] A direct communication between the transferring and receiving facility should be undertaken with sharing of complete information on patient's clinical condition, treatment being given, reasons for transfer, mode of transfer and timeline of transfer, in a written document.
Pre-transfer stabilisation and preparation
A proper and meticulous preparation and stabilisation of patient should be done before transfer to prevent any adverse events or deterioration in patient's clinical condition. The patient should be adequately resuscitated and stabilised to the maximum extent possible without wasting undue time. During the preparation, patient's A, B, C and D, i.e., airway, breathing, circulation and disability, should be checked, and any associated preventable problems should be corrected. The use of pre-transfer checklist is useful in this context:[11,12]
Airway
The patients with possibility of airway compromise during transfer should be electively intubated with endotracheal tube (ETT) with a cuff which should be secured properly after confirming its correct position. A properly placed nasogastric tube is required in some patients to prevent aspiration of gastric contents during transfer. The cervical spine stabilisation may be required in some trauma patients.
Breathing
The ventilation should be adequately controlled with optimisation of the arterial blood gas values. In the suspected pneumothorax, chest drain should be inserted before transfer, especially before air transport.
Circulation
The patient should have at least two wide bore intravenous working cannulas in place before transfer. External haemorrhage, if any, should be adequately controlled, and any shock should be treated with intravenous fluids and/or vasopressors. The availability of crossed-matched blood may be required during the transport.
Disability or neurological status
Patients with head injury should have their Glasgow coma scale (GCS) adequately monitored and documented before and during transfer and before administration of any sedative or paralytic agent.
Apart from the above pre-transfer checklist, the patient should be protected from cold by provision of suitable blankets. All the baseline investigations should be done on the day of transfer to reflect the present condition of the patient.
Mode of transfer
The two most commonly employed modes of transfer of patients are ground transport, with the inclusion of ambulances and Mobile Intensive Care Units (MICUs), and air transport which includes helicopter or aeroplane ambulances.
Ground transport
This is accomplished by the use of different types of ambulances:
Basic life-support ambulance: These ambulances are equipped with appropriate staff and monitoring devices to transport patients with non-life-threatening conditions as these can only provide basic life-support services
Advanced life-support ambulance: These ambulances can provide advanced life-support services such as endotracheal intubation, cardiac monitoring, defibrillation, administration of intravenous fluids or vasopressors. These are adequately staffed and equipped for transporting patients with life-threatening conditions
MICU: These are specialised vehicles with all the equipment and staff to transfer critically ill patients and are usually used in conjunction with specialist retrieval teams in few developed countries. The literature also supports the use of MICUs with reduced incidences of major adverse events during transfer and improved survival rates with reduced mortality.[13,14,15]
Air transport
The use of air transport has been on the rise in developed countries because of advantages of rapid transport with inclusion of specialised medical care. There has been an improved prognosis of patients with major trauma, acute myocardial infarction and acute stroke due to rapid provision of appropriate medical care by use of air transport.[16,17,18] The air transport is of two types:
Fixed wing or aeroplane type air ambulance: It is usually used for long distances inter-hospital patient transfer for approximately more than 240 km. It is more rapid mode of transport with the provision of pressurised cabin and less noise and vibration. It is used for travel across countries or continents. The main disadvantage is requirement of additional ground transport between the hospital and the air facility
Rotor wing or helicopter ambulance: It can be used for shorter travel distances of about 80 km. It can be used to transfer the patient directly to the receiving hospital with the facility of helipad. There is no requirement of additional ground transport. However, space is more compact with interference of noise and vibration during patient transfer.
According to the guidelines of Air Medical Dispatch by American College of Emergency Physician, the air transport is indicated when the ground transport is not feasible due to the factors such as time of transfer, distance to be travelled and the level of care needed during the transfer.[19] The patients more likely to benefit from air transport are:
Severe trauma patients with penetrating chest injuries, multisystem injuries, crush injuries, age less than 12 years or more than 55 years or patients with unstable vital signs
Patients with acute coronary syndrome in urgent need of revascularisation procedure, cardiac tamponade with haemodynamic compromise, cardiogenic shock in need of intra-aortic balloon pump or other assist devices
Patients due to receive organ transplant
Critically ill high-risk medical or surgical patients, for example, those on high vasopressors, special modes of ventilation, requiring hyperbaric oxygen therapy or with surgical emergencies such as aortic dissection with haemodynamic compromise.[20,21,22]
Air transport may not be feasible in the presence of dangerous environmental conditions for flying, uncooperative patients, untreated pneumothorax or penetrating eye injury, patients with recent abdominal surgery, potentially obstructed airway, respiratory distress, significant facial injury and reduced level of consciousness, as these patients can undergo sudden decompensation during the air transfer.[23]
Accompanying the patient
It is usually recommended to have at least two competent personnel accompanying the patient to be transferred. The care required by each patient during transfer depends on the level of patient's critical care dependency and accordingly are divided into:
Level 0: It includes the patients who can be managed at the level of ward in a hospital and are usually not required to be accompanied by any specialised personnel
Level 1: It includes those patients who are at risk of deterioration in their condition during the transfer but can be managed in an acute ward setting with support from critical care team. These usually have to be accompanied by a paramedic or a trained nurse
Level 2: It includes patients who require observation or intervention for failure of single organ system and must be accompanied by trained and competent personnel
Level 3: It includes patients with requirement of advanced respiratory care during the transport with support of at least two failing organ systems. These patients have to be accompanied by a competent doctor along with a nurse and a paramedic.
The accompanying person should be suitably trained, competent and experienced and preferably should have done training in patient transfer and should have sufficient training in advanced cardiac life support, airway management and critical care. If the physician is not available to transfer unstable patients, then the provision of contacting the concerned physician by the transport team should definitely be available.
Equipment, drugs, and monitoring
A proper monitoring with the provision of all lifesaving drugs is mandatory for transfer of all patients with level 1, 2 and 3 critical care needs. The transfer ambulance must be equipped with all the drugs and instruments required for airway management, oxygenation, ventilation, haemodynamic monitoring and resuscitation. All the monitoring needs to be established before the commencement of transfer along with the starting of infusion drugs. The drugs needed for patient transfer include muscle relaxants, sedatives, analgesics, inotropes and resuscitation drugs. The person in charge of patient transfer should ensure proper supplies of these emergency drugs. Some of these drugs may be required to be prepared in pre-filled syringes before the transfer. The minimum standard of monitoring recommended for patient transfer includes continuous electrocardiogram monitoring, non-invasive blood pressure, oxygen saturation, end-tidal carbon dioxide (in ventilated patients) and temperature. The non-invasive blood pressure may be significantly affected by the motion artefacts, so it may be prudent to use invasive blood pressure monitoring in selected subset of patients. All the monitoring equipment should be secured properly and should be placed at or below the level of the patient for uninterrupted monitoring. The electrical equipment must be functional on battery power with the provision of extra batteries during the transfer. Patients on ventilator must be transferred on portable transport ventilators with the provision of display of alarms related to tidal volume, airway pressure, inspiratory: expiratory ratio, inspired oxygen fraction and respiratory rate.
Documentation
The documentation of patient transfer is most important but often missed as part of transfer. The documentation should always be clear at all stages of transfer. As it was the only legal document that the patient was transferred, so it must include the patient's condition, reason to transfer, names and designation of referring and receiving clinicians, details and status of vital signs before the transfer, clinical events during the transfer and the treatment given. A standardised document should be used and maintained both for intra- and inter-hospital transfer. These documents should be used for audit purposes for investigating the flaws in the patient transfer. There should be a formal handing over at the receiving facility between the transferring team and the receiving team including the doctors and nurses. The various reports of clinical investigations and diagnostic studies should be handed over to the receiving team. In spite of existing recommendations and guidelines for safe patient transfer, these are often not followed or are not met.
PHYSIOLOGICAL ALTERATIONS DURING TRANSPORT
The transfer of patient, whether via ground or air, imposes various physiological alterations in both the patient and the transport team, seriously affecting a safe patient transfer. These include:
Noise
The various sources of noise during the patient transfer are external wind, rotors of helicopter, propellers of aircraft, engine and monitoring equipment. The noise created can hinder the auscultation of patient and also can interfere in conversation between the doctor and the transferring patient.
Vibration
The various sources of vibration depend on the mode of transfer. The uneven roads and vehicular suspension create vibration in ground transport, whereas engine, rotors, propellers and air turbulence create vibration during air transport. The vibration can cause nausea, discomfort, headache, impaired visual performance, pain at fractured site, aggravation of spinal injuries and internal brain haemorrhage with interference in intravenous cannulation, endotracheal intubation, etc. There can be malfunction of motion sensing pacemakers or gravity linked infusion pumps and motion artefacts in the monitoring equipment. These effects of vibration can be minimised by use of holding restraints for the accompanying persons, vibration absorbing mattresses and padding of contact points between the vehicle and the patient.
Acceleration and gravitational forces
The patients are subjected to both radial and linear acceleration and deceleration forces during transfer and the physiological effects produced may be more profound in critically ill patients due to their hypovolaemic and vasodilated nature. The patient can have transient hypertension and dysrhythmias due to sudden acceleration or deceleration. These effects can be minimised by positioning the patient's trolley at a right angle to the long axis of aircraft and by keeping the legend of the patient towards the cockpit to avoid venous pooling.
Temperature and humidity
The environment inside the ambulance is kept at lower temperature by use of air conditioning which can cause hypothermia in susceptible patients, especially neonates. These patients should be covered with warming blankets during transfer. The humidity decreases with altitude in air transport and thus can lead to drying of secretions of respiratory tract and mucous membranes. These patients will require the use of humidified oxygen and lubrication of eyes by use of artificial tears or drops.
Altitude
The effect of increasing the altitude is mainly related to decrease in inspired oxygen levels. The rotor wing ambulances usually fly at 2000–5000 feet above sea levels, whereas fixed wing ambulances fly at 15,000–40,000 feet above sea levels. It is recommended to have pressurised air cabins at an altitude of 10,000 feet above sea level. The physiological effects of increasing the altitude are:
Hypobaric hypoxia
As mentioned earlier, the partial pressure of oxygen decreases with increase in altitude which can in turn aggravate hypoxia in patients with cardiorespiratory problems.
Expansion of gas in body spaces and in medical equipment
This is due to reduction in the atmospheric pressure and can lead to ear pain, gastric distension or ileus. The cuff pressure in the ETT cuff or tracheostomy cuff can increase considerably causing pressure necrosis. The high altitude flights are thus contraindicated in patients with trapped gas in body cavities such as untreated pneumothorax, pneumocephalus, recent abdominal surgery and gas gangrene.
Third space fluid loss
The pressure changes associated with altitude changes cause increased vascular permeability thus causing fluid shifts from intravascular to extravascular compartment leading to oedema and hypovolaemia.
Motion sickness
The difference between the visual and vestibular inputs to brain produces nausea, vomiting or retching. There should be provision of a mechanical or electrical suction apparatus during the transfer to prevent from any aspiration.
COMPLICATIONS DURING TRANSPORT AND PREVENTION STRATEGIES
Pulmonary and airway complications
Literature shows that oxygen desaturation, atelectasis, bronchospasm, pneumothorax, accidental extubation and airway loss may occur during patient transport.[24,25,26] These can be prevented by providing optimal sedation and analgesia with provision of suctioning of ETT, confirmation of correct position of ETT and provision of full oxygen cylinder before transport. There should be provision of a properly functioning pulse oximeter.
Cardiovascular complications
Tachycardia, hypotension, hypertension, arrhythmia and even cardiac arrest (0.34–1.6%) may occur during transport.[27,28,29] These can be prevented by having adequate resuscitation before transport with provision of invasive and non-invasive haemodynamic monitoring can prevent these complications.
Infectious complications
Risk of infection both to transported patient and others who might be exposed to that patient have been reported.[30] These can be prevented by good communication between transport team and receiving team.
Endocrine complications
Hyperglycaemia and hypoglycaemia may develop during transport due to discontinuation of insulin pumps and altered fluid therapy. These can be prevented by paying close attention to glucose regulation during all phases of transport.
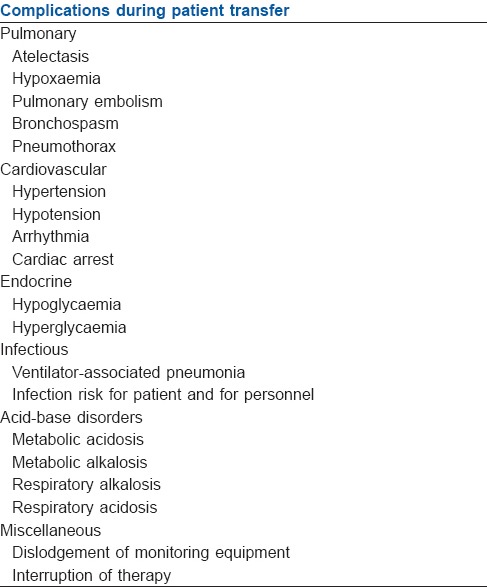
Acid-base derangement, equipment dislodgement and interruption in vital infusions such as vasopressor, inotrope, analgesia and sedation may occur.[31] These complications may be prevented by provision of blood gas analysis before transport which can be repeated during the transport if the facilities are available and ensuring the running and patent lines to continue infusions and transfer them to transport bed. Table 1 shows a complete list of complications during patient transfer.
Table 1.
Complications that may occur during patient transfer
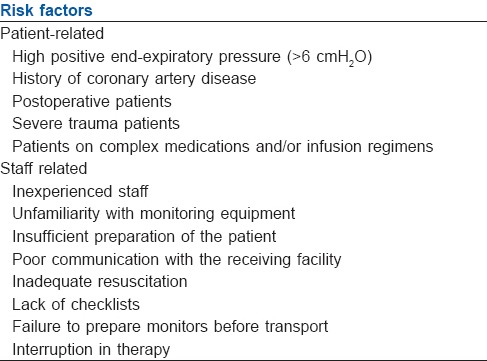
RISK FACTORS FOR COMPLICATIONS[32]
Certain factors add to the risk for development of complications during transport [Table 2]. Attention to identification and possible optimisation may reduce morbidity and mortality during transport.
Table 2.
Risk factors for the development of complications during transport
INDIAN SCENARIO
The International guidelines as described may not be possible in developing countries like India due to the diversity of Intensive Care Units which may be state of the art or may be just basic units capable of giving initial resuscitative measures. In a study by Verma et al. comparing the transfer characteristics of trauma patients transferred to a tertiary trauma centre from peripheral centres, they found a significant lower GCS, higher injury severity score and a longer duration of hospital stay in the transferred patients. Only 3.66% of the patients were accompanied by a paramedic or trained nurse, whereas only 2.9% of the patients had cervical spine stabilised.[33] The variation in the infrastructure of each hospital in India, thus, establishes the need to modify the International guidelines according to the local needs. There is a need for proper documentation at all stages of patient transfer with continuous quality assessments to improve upon the existing protocols. The existing guidelines from Indian Society of Critical Care Medicine for intra- and inter-hospital transport of patient is an evidence-based guideline developed for Indian scenario to help standardise the equipment, the personnel and monitoring during these transfers. These guidelines are similar to other international guidelines with minor changes according to Indian settings. These guidelines need to be implemented on an urgent basis in India to improve the level of safe transport of critically ill patients.
SUMMARY
Transfer is an important but often neglected phase of continuing care of a patient who may also need additional care. Transfer should be initiated after carefully balancing the benefits obtained versus the risks involved. The patient transfer should be based on the concept of ‘stabilise and shift’ by initiating stabilisation of patient at the transferring facility and continuing such care till the receiving facility. The transport personnel, an important factor in the safe transport, should be well qualified to anticipate and manage any complications that may arise during the transport process. The guidelines should be modified according to the infrastructure available in developing countries like India with periodical quality assessments.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Waydhas C. Intrahospital transport of critically ill patients. Crit Care. 1999;3:R83–9. doi: 10.1186/cc362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wagner J, Iwashyna TJ, Kahn JM. Reasons underlying interhospital transfers to an academic medical intensive care unit. J Crit Care. 2013;28:202–8. doi: 10.1016/j.jcrc.2012.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ivanusa M. Reducing mortality in myocardial infarction: Goal should be interhospital transfer for primary angioplasty. BMJ. 2005;330:1271. doi: 10.1136/bmj.330.7502.1271-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aguirre FV, Varghese JJ, Kelley MP, Lam W, Lucore CL, Gill JB, et al. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: The Stat Heart Program. Circulation. 2008;117:1145–52. doi: 10.1161/CIRCULATIONAHA.107.728519. [DOI] [PubMed] [Google Scholar]
- 5.Iwashyna TJ, Courey AJ. Guided transfer of critically ill patients: Where patients are transferred can be an informed choice. Curr Opin Crit Care. 2011;17:641–7. doi: 10.1097/MCC.0b013e32834b3e55. [DOI] [PubMed] [Google Scholar]
- 6.Joosse P, Saltzherr TP, van Lieshout WA, van Exter P, Ponsen KJ, Vandertop WP, et al. Impact of secondary transfer on patients with severe traumatic brain injury. J Trauma Acute Care Surg. 2012;72:487–90. doi: 10.1097/TA.0b013e318226ed59. [DOI] [PubMed] [Google Scholar]
- 7.Warren J, Fromm RE, Jr, Orr RA, Rotello LC, Horst HM. American College of Critical Care Medicine. Guidelines for the inter-and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256–62. doi: 10.1097/01.CCM.0000104917.39204.0A. [DOI] [PubMed] [Google Scholar]
- 8.American College of Emergency Physicians. Principles of appropriate patient transfer. Ann Emerg Med. 1990;19:337–8. [PubMed] [Google Scholar]
- 9.Duke GJ, Green JV. Outcome of critically ill patients undergoing interhospital transfer. Med J Aust. 2001;174:122–5. doi: 10.5694/j.1326-5377.2001.tb143182.x. [DOI] [PubMed] [Google Scholar]
- 10.Vos GD, Nissen AC, Nieman FH, Meurs MM, van Waardenburg DA, Ramsay G, et al. Comparison of interhospital pediatric intensive care transport accompanied by a referring specialist or a specialist retrieval team. Intensive Care Med. 2004;30:302–8. doi: 10.1007/s00134-003-2066-7. [DOI] [PubMed] [Google Scholar]
- 11.Dunn MJ, Gwinnutt CL, Gray AJ. Critical care in the emergency department: Patient transfer. Emerg Med J. 2007;24:40–4. doi: 10.1136/emj.2006.042044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin TE, editor. 1st ed. London: Cambridge University Press; 2001. Stabilization prior to transportation. Handbook of Patient Transportation; pp. 45–54. [Google Scholar]
- 13.Uusaro A, Parviainen I, Takala J, Ruokonen E. Safe long-distance interhospital ground transfer of critically ill patients with acute severe unstable respiratory and circulatory failure. Intensive Care Med. 2002;28:1122–5. doi: 10.1007/s00134-002-1348-9. [DOI] [PubMed] [Google Scholar]
- 14.Gebremichael M, Borg U, Habashi NM, Cottingham C, Cunsolo L, McCunn M, et al. Interhospital transport of the extremely ill patient: The Mobile Intensive Care Unit. Crit Care Med. 2000;28:79–85. doi: 10.1097/00003246-200001000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Wiegersma JS, Droogh JM, Zijlstra JG, Fokkema J, Ligtenberg JJ. Quality of interhospital transport of the critically ill: Impact of a Mobile Intensive Care Unit with a specialized retrieval team. Crit Care. 2011;15:R75. doi: 10.1186/cc10064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Essebag V, Halabi AR, Churchill-Smith M, Lutchmedial S. Air medical transport of cardiac patients. Chest. 2003;124:1937–45. doi: 10.1378/chest.124.5.1937. [DOI] [PubMed] [Google Scholar]
- 17.Imaizumi T, Hata N, Kobayashi N, Yokoyama S, Shinada T, Tokuyama K, et al. Early access to patients with life-threatening cardiovascular disease by an air ambulance service. J Nippon Med Sch. 2004;71:352–6. doi: 10.1272/jnms.71.352. [DOI] [PubMed] [Google Scholar]
- 18.Isakov A. Urgent air-medical transport: Right patient, place and time. CMAJ. 2009;181:569–70. doi: 10.1503/cmaj.091258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomson DP, Thomas SH. Air Medical Services Committee of the National Association of EMS Physicians. Guidelines for air medical dispatch. Prehosp Emerg Care. 2003;7:265–71. [Google Scholar]
- 20.Hatlestad DC, Van Horn J. Air transport of the IABP patient. Intra-Aortic Balloon Pump. Air Med J. 2002;21:42–8. [PubMed] [Google Scholar]
- 21.Berset A, Albrecht R, Ummenhofer W, Erne JJ, Zuercher M. Air transfer of patients with intraaortic balloon pump support: Swiss experience and recommendations. Swiss Med Wkly. 2012;142:w13552. doi: 10.4414/smw.2012.13552. [DOI] [PubMed] [Google Scholar]
- 22.Fang R, Allan PF, Womble SG, Porter MT, Sierra-Nunez J, Russ RS, et al. Closing the “care in the air” capability gap for severe lung injury: The Landstuhl Acute Lung Rescue Team and extracorporeal lung support. J Trauma. 2011;71:S91–7. doi: 10.1097/TA.0b013e3182218f97. [DOI] [PubMed] [Google Scholar]
- 23.Martin TE, editor. 1st ed. London: Cambridge University Press; 2001. Inter-ITU transfers. Handbook of Patient Transportation; pp. 83–92. [Google Scholar]
- 24.Parmentier-Decrucq E, Poissy J, Favory R, Nseir S, Onimus T, Guerry MJ, et al. Adverse events during intrahospital transport of critically ill patients: Incidence and risk factors. Ann Intensive Care. 2013;3:10. doi: 10.1186/2110-5820-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Lassence A, Timsit JF, Tafflet M, Azoulay E, Jamali S, Vincent F, et al. Pneumothorax in the intensive care unit: Incidence, risk factors, and outcome. Anesthesiology. 2006;104:5–13. doi: 10.1097/00000542-200601000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Mazza BF, Amaral JL, Rosseti H, Carvalho RB, Senna AP, Guimarães HP, et al. Safety in intrahospital transportation: Evaluation of respiratory and hemodynamic parameters. A prospective cohort study. Sao Paulo Med J. 2008;126:319–22. doi: 10.1590/S1516-31802008000600005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor JO, Chulay JD, Landers CF, Hood W, Jr, Abelman WH. Monitoring high-risk cardiac patients during transportation in hospital. Lancet. 1970;2:1205–8. doi: 10.1016/s0140-6736(70)92176-8. [DOI] [PubMed] [Google Scholar]
- 28.Damm C, Vandelet P, Petit J, Richard JC, Veber B, Bonmarchand G, et al. Complications during the intrahospital transport in critically ill patients. Ann Fr Anesth Reanim. 2005;24:24–30. doi: 10.1016/j.annfar.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 29.Schmidt JM. Stopping the chain of infection in the radiology suite. Radiol Technol. 2012;84:31–48. [PubMed] [Google Scholar]
- 30.Choi HK, Shin SD, Ro YS, Kim DK, Shin SH, Kwak YH. A before- and after-intervention trial for reducing unexpected events during the intrahospital transport of emergency patients. Am J Emerg Med. 2012;30:1433–40. doi: 10.1016/j.ajem.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 31.Conrad BP, Rossi GD, Horodyski MB, Prasarn ML, Alemi Y, Rechtine GR. Eliminating log rolling as a spine trauma order. Surg Neurol Int. 2012;3(Suppl 3):S188–97. doi: 10.4103/2152-7806.98584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knight PH, Maheshwari N, Hussain J, Scholl M, Hughes M, Papadimos TJ, et al. Complications during intrahospital transport of critically ill patients: Focus on risk identification and prevention. Int J Crit Illn Inj Sci. 2015;5:256–64. doi: 10.4103/2229-5151.170840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Verma V, Singh GK, Carvello EJ, Kumar S, Singh CM, Harjai M. Inter-hospital transfer of trauma patients in a developing country: A prospective descriptive study. Indian J Community Health. 2013;25:309–15. [Google Scholar]


