Abstract
Background and Objectives
We examined youth recovery outcomes at 6- and 9-months post-participation in an aftercare pilot study called ESQYIR (Educating and Supporting inQuisitive Youth in Recovery) that aimed to investigate the utility of a 12-week mobile texting recovery support intervention.
Methods
A total of 80 youth [Mage 20.4 (SD = 3.5) were randomized to a mobile texting aftercare intervention or an aftercare-as-usual control group. Both groups received identical data collection protocols with psychosocial and behavioral assessments occurring at baseline, during the trial (month 1 & month 2), at discharge from the trial (month 3), and 3-, 6-, and 9-month post-intervention follow-ups.
Results
Mixed modeling showed that youth who participated in the mobile texting aftercare intervention were less likely to test positive for their primary drug compared to youth in the aftercare-as-usual condition during 6- and 9- month follow-ups (p < .01). Additionally, youth in the aftercare intervention reported significantly higher self-efficacy/confidence to abstain during recovery (p < .05) and were more likely to participate in recovery-related behaviors (self-help and goal-directed extracurricular activities) (p < .05) than those in aftercare-as-usual at the 6 and 9 month follow-ups.
Conclusions
Results suggest that delivering a structured, behavioral-based wellness aftercare intervention using mobile texting can be an effective for sustaining recovery outcomes in youth over time compared to youth who receive aftercare-as-usual.
Scientific Significance
This study shows that a mobile-texting aftercare intervention sustained effects at 6- and 9- months post-intervention for young people in substance use recovery.
Keywords: Mobile Texting, Aftercare, Youth, Relapse, Recovery Outcomes
INTRODUCTION
Roughly 7 million people (12 and older) had a substance use disorder in the United States (U.S.) during 2013.1 Research shows that substance use disorders are adolescent onset disorders,2 which support current trends in substance use disorder rates, as they are highest among youth populations (3.5% of youth 12-17 and 7.4% of youth 18-25 years old) compared to older populations (3.1% of 26-44 year olds, 1.1% of 45-64 year olds, and <1% of 65 years or older).1 The suppression of substance use behaviors among young people has been a long-standing problem for the U.S. Despite experiencing acute treatment benefits, substance use relapse post-treatment is a major issue for both young people and adults alike challenged by substance use disorders.2,3 Substance use disorders have been identified as chronic and relapsing,4 similar to other chronic health disorders (e.g., diabetes) that require ongoing care.5 Treatment outcome studies have shown that participation in continued care (also called aftercare) is a critical element to help sustain the benefits of treatment and decrease post-treatment relapse for both adult and youth clinical populations.6
Aftercare approaches commonly used in the treatment field for both young people and adults have traditionally been self-help, such as 12-step Alcoholics Anonymous or Narcotics Anonymous-AA/NA.7 Although literature offers support for such self-help programs producing positive recovery outcomes post-treatment when actively attended (i.e., reduced substance use relapse, improved quality of life, and civility),8 the utility of these programs is less clear for young people.9,10 Limited involvement in aftercare programs, particularly NA/AA, among young people has been linked to a developmental disconnect (i.e., not many age appropriate groups), an inability to connect with the program focus (i.e., disease notions of substance use, total abstinence motto, life-long recovery process), lack of personal motivation, and low perceived benefit.9-13
Alternative aftercare approaches have been supported for young people, including weekly in-home case management, and in-person and brief telephone structured recovery check-up interventions.14,15 Research has shown favorable outcomes resulting from the use of such alternative aftercare approaches with young people, including reduced substance use and improved psychosocial functioning post-treatment;16 however participation in aftercare programs that support recovery for young people continue to pose challenges for the treatment field.6,9,17
Exploring recovery needs among young people in treatment for substance use disorders, Gonzales and colleagues18 found that a majority view recovery as improving one’s behavioral lifestyle, asserting personal control, and engaging in wellness related behavioral changes. The wellness concept has been commonly applied in disease self-management extended care interventions within the healthcare field to help individuals with complex conditions engage in lifestyle change and improve symptoms by promoting self-responsibility for behavior/health.19,20 This model uses the following critical intervention elements for facilitating personal control over behavior change (self-regulation) and reinforcing the adoption of alternative healthy behaviors: monitoring, feedback, reminders, education, and support.21 Another common programmatic element used in disease self-management extended care interventions is the use of mobile technologies for the delivery of such interventions, especially text messaging.22,23 The use of mobile technology in behavior change interventions, in general, have been shown to offer several advantages over traditional based in-person approaches, including expanded access, privacy, real time information/support, ease (i.e., content is pre-programmed on a web-based platform), and standardization of program content.24
A growing body of studies have sought to investigate the feasibility and efficacy of using mobile technology approaches for improving health outcomes among young people, including diabetes, asthma, cigarette smoking, and risky sexual behaviors.25-28 These studies, in particular, found that the texting promoting the intervention features of “monitoring-feedback, reminders, education, and support” helped increase recovery behavioral regiments (i.e., medication use compliance, exercise/diet change, quit/cessation, condom use). Studies found that reasons for these promising effects had to do, in large part, with the increased mobile phone utilization and acceptance among youth populations over the past years. Market segment research identifies youth populations as a “perpetual texting generation.”29
To date, only a few studies have investigated the utility of mobile interventions for substance use prevention among young people (i.e., tobacco cessation30 and alcohol prevention in emergency room settings).31 There are virtually no studies that have used mobile intervention methods for substance use aftercare with young people, with the exception of our previous study.32 Specifically, we found utility and initial efficacy of a 12-week mobile texting aftercare pilot intervention compared to an aftercare-as-usual control group on producing positive recovery outcomes, including reduced primary substance use relapse, less substance use problem severity, and increased participation in self-help and extracurricular recovery-directed behaviors from baseline to discharge, as well as a 3-month follow-up, with effect size for reduced substance use at discharge being .48 and .42 at the 3-month follow-up. This paper is a follow-up extension of this initial study as it focuses on the 6- and 9-month follow-up effects of the mobile texting intervention on substance use and recovery behaviors, and includes other outcomes of abstinence self-efficacy/confidence (compared to aftercare-as-usual).
MATERIALS AND METHODS
Participants
This pilot study recruited 80 youth to participate in an aftercare project called Project ESQYIR (Educating and Supporting inQuisitive Youth in Recovery) between 2012 and 2014 from both outpatient and residential community-based treatment programs located throughout diverse areas of Southern California. Inclusion criteria included being a youth defined broadly as adolescents (12 to 17) or transitional age youth (TAY: 18 to 25); completing treatment, which consisted of relapse prevention/cognitive behavioral groups ranging from 12 to 16 weeks; and owning a mobile phone with SMS texting capabilities. Exclusion criteria included not obtaining parental consent (if adolescents); not willing to comply with the aftercare study procedures; and any psychological/medical conditions that warranted further primary treatment.
Procedures
This pilot study, with an intent-to-treat design and analysis, was conducted under the approval of the Institutional Review Board (IRB) of Azusa Pacific University. A total of six (3 outpatient and 3 residential) community-based treatment programs located throughout diverse areas of Los Angeles County, California were used for study recruitment as they offered substance use services to youth (adolescent and TAY populations). Study recruitment entailed posting IRB-approved fliers conveying eligibility criteria and aftercare project information at participating treatment programs in waiting areas and group rooms as well as in-person announcements during treatment groups by study staff. Interested youth who contacted study research staff were provided an overview of the study prior to obtaining informed consent at participating programs in a private office by which refusal rates were monitored. A total of 90 youth were approached during recruitment efforts for the pilot aftercare study to obtain the sample goal of 80 as approximately 10 refused participation (n = 8 adolescents and 2 TAY), citing not wanting to be in a treatment program any longer.
Informed consent procedures were conducted with youth who agreed to participate. Given the mobile nature of the pilot intervention, youth were informed about taking safety precautions in terms of password protecting their phones or deleting information they received from the program to safeguard their privacy and personal information. Parental consent was obtained for adolescent youth participants (under 18) prior to participating. After consenting procedures, youth completed a battery of self-administered baseline assessments (see measures section for details). Participants were then randomized to one of two study conditions: mobile texting aftercare intervention or aftercare-as-usual using an electronic random generator number method (see http://www.randomizer.org/).
The mobile texting aftercare intervention consisted of 12-weeks of daily text messages guided by a disease management conceptual wellness model for recovery from substance use disorders. The mobile text-messaging intervention platform was developed by EPG Technology Consultant. Specifically, the program used a web-based platform that was pre-programmed to deliver the following disease management intervention components: 1) monitoring, 2) feedback, 3) reminders, and 4) education/support (see Gonzales et al32 for study details). Specifically, one monitoring text message was sent daily in the late afternoon, which consisted of questions that prompted participants about weekly troubles they experienced with regards to critical relapse areas, including confidence, wellbeing (stress/negative mood), recovery behaviors, and substance use. These relapse areas were identified from previous research with substance-abusing youth (see Gonzales et al33). Immediately after the youth responded to the monitoring text, they were sent a feedback text. Feedback texts were automated messages (over 600 messages) grouped into four general text banks: positive appraisal, motivational/inspirational, recovery promotion (stress management tips), and coping advice, as supported by formative work that focused on exploring recovery needs and barriers among substance-abusing youth (see Gonzales et al.34). Feedback texts used pre-determined rules corresponding to levels of “relapse risk” linked to the monitoring areas. The timing of feedback texts followed a randomized 1-30 second window and had user-driven rules to insure no duplication. An example of a monitoring-feedback scenario for recovery behaviors-recovery promotion would be: [Monitoring text] “How many days in the past week did u feel stressed or have negative emotions (Text 0-7)?” Participant texts back a 3. [Feedback text] “Think about 2 good things in ur life right now – write them down and focus on those. Ignore everything else.” Youth were also sent one daily reminder text that provided them with a recovery tip of the day focused on wellness using the following text prompt throughout the 12 weeks: “Today’s a new day in your recovery, think about the change you’re working towards…[wellness tip].” The wellness topics alternated throughout the program weeks between personal health, social health, emotional health, and physical health with a focus in stress management and emotional coping using content from the CDC’s getting healthy program and Kaiser’s wellness program specific to youth populations. An example of a wellness tip text would read: “Stress tip 4 today: write out negative thoughts on a piece of paper, then rip it up!” Education and support texts were sent on the weekends only. Participants received one education text every Saturday, tailored to their primary substance of abuse they reported receiving treatment (i.e., effects/consequences). Content for educational text messages was adapted from the National Institute on Drug Abuse’s educational information, e.g., InfoFacts. Participants were sent one support text on Sundays throughout the 12-week program, providing them with information about recovery support services and resources tailored to their geographic areas using zip-code residence locations.
The aftercare-as-usual control group consisted of the standard protocol that was given at community-based treatment programs once participants completed their current treatment program. Among the participating programs for this study, aftercare-as-usual consisted of promotion to self-help and 12-step recovery support programs in the larger community.
The data collection protocol for this study consisted of repeated in-person assessments at baseline (one week before enrollment in program), discharge (one week after 12-week study intervention), and three follow-ups (3-, 6-, and 9-months post-intervention participation). Due to the longitudinal nature of this study, there could be participants who responded at 9-months and not 6-months (and vice versa); however data reveal that there were only two participants who responded at 9-months but had missing responses at 6-months. Study research team conducted assessments at treatment settings during convenient times for the participants. If participants could not make it back to the recruiting treatment program, staff would meet them at convenient locations in their communities (i.e., local coffee shops or restaurants) to conduct the assessments. Data collection for these time points took approximately 1-1.5 hours to complete. Participants were compensated in gift cards to local retail stores for their time. Follow-up retention rates for this pilot study were 86.2% (n = 68) at 6-months and 82.5% (n = 62) at 9-months. Analyses using chi-square and t-tests revealed no significant differences in participant characteristics (e.g., age, education, gender, and baseline primary substance use) between youth who completed the follow-ups (6 and 9 months) and those who did not.
Measures
The aim of this paper was to examine differences in long-term recovery outcomes at 6- and 9-month follow-ups between participants in the texting intervention vs. aftercare-as-usual control group. The independent measure was study condition (exposure to mobile texting intervention or aftercare-as-usual control). Dependent measures included recovery outcomes defined as the following: (1) relapse, (2) participation in recovery behaviors, and (3) abstinence self-efficacy/confidence (measured at the 6- and 9-month follow-ups). For this paper, relapse was defined by use of one’s primary substance (for which they reported receiving treatment) at the follow-up assessment. Specifically, relapse to primary substance of abuse was coded as 1 (use) if they had a positive urine screen and self-reported any use in the past month or 0 (no use) if they had a negative urine screen and did not self-report any use in the past month, in terms of concordance testing between self-report and urine screens. Recovery behaviors were measured by past month participation in 12-step/self-help meetings and/or goal-directed extracurricular recovery activities assessed by the Brief Addiction Monitor (BAM).35 Specifically, the following questions were used to measure such recovery outcomes: “In the past 30 days, how many days did you attend self-help meetings like AA or NA to support your recovery?” and “In the past 30 days, how many days have you done things to help meet your recovery goals (participated in any extracurricular activities)?” Abstinence self-efficacy/confidence was also assessed with the BAM using the following question “How confident are you in your ability to be completely abstinent (clean) from alcohol and drugs in the next 30 days?” Participants rated their responses using a 5-point likert scale of Not at all, Slightly, Moderately, Considerably, or Extremely.
Statistical Procedures
Mixed modeling using repeated measures regression was used to test the effects of the study condition (intervention vs. control) on the outcome measure of relapse (measured by any use of primary substance they received treatment for – 0 = no use; 1 = use) at the 6- and 9-month follow-ups. We also used mixed modeling to examine differences in recovery behavior outcomes (measured by mean days of participating in self-help meetings in the past month as well as mean days of doing extracurricular/recovery-goal directed activities) collected at follow-ups between study conditions. Lastly, we used mixed modeling to assess for group differences in abstinence self-efficacy/confidence (mean score from Likert scale) across 6- and 9-month follow-ups. For all the multivariate analyses, we controlled for baseline primary drug use, age, gender, and education. The significance level (2-tailed) was set at p < .05 using the Statistical Package for Social Sciences (SPSS), version 22.0, and SAS, version 9.3. Since this is a pilot study, it was principally aimed at providing a descriptive account on the effect size of our primary outcome which is primary drug use. In this case, power calculation shows that our primary outcome has an effect size of .323 in primary drug use, yielding a power of 81.9%.
Results
Participant Characteristics
Table 1 displays differences in baseline characteristics between the mobile texting aftercare intervention and aftercare-as-usual control groups.
Table 1.
Baseline Characteristics of Youth Sample by Study Condition
| Mobile Texting Intervention (N = 40) |
Aftercare as Usual Control Mobile Texting Intervention (N = 40) |
P-value | |
|---|---|---|---|
|
| |||
| Age (sd) | 22.1 (3.1) | 18.9 (3.1) | 0.01 |
|
| |||
| Gender (%) | 0.08 | ||
| Female | 15 (37.5%) | 8 (19.5%) | |
| Male | 25 (62.5%) | 33 (80.5%) | |
|
| |||
| Education (sd) | 14.1 (2.3) | 11.7 (2.9) | 0.001 |
|
| |||
| Ethnicity (%) | 0.14 | ||
| Latino | 10 (25%) | 20 (48.8%) | |
| Non-Latino White | 22 (55%) | 13 (31.7%) | |
| Black | 4 (10%) | 4 (9.8%) | |
| Asian | 3 (7.5%) | 4 (9.8%) | |
| American Indian | 1 (2.5%) | 0 (0%) | |
|
| |||
| Employed (%) | 16 (40%) | 14 (34.1%) | 0.58 |
|
| |||
| Primary Drug* (%) | |||
| Marijuana | 9 (22.5%) | 19 (48.7%) | |
| Heroin | 5 (12.5%) | 4 (9.8%) | 0.17 |
| Methamphetamine | 15 (37.5%) | 8 (19.5%) | |
| Cocaine | 6 (15.0%) | 7 (17.1%) | |
| Alcohol | 2 (5.0%) | 1 (2.4%) | |
| Rx Drugs | 3 (7.5%) | 1 (2.4%) | |
|
| |||
| Current Tobacco Use (%) | 24 (60.0%) | 28 (68.3%) | 0.44 |
Primary drug in treatment for prior to participating in the pilot aftercare project
Relapse to Primary Substance of Abuse Follow-up Outcomes between Study Groups
Controlling for baseline characteristics (baseline primary drug use, age, gender, education), youth participants in the texting aftercare intervention were significantly less likely to relapse to their primary drug over time between the 6- and 9-month follow-ups (OR = 0.72, p = 0.02 & OR = 0.74, p = 0.01, respectively) compared to participants in the aftercare-as-usual control condition. Results showed that fewer texting intervention participants used their primary substance of abuse for which they reported receiving treatment compared to control participants at the 6-month (54.1% vs. 28.6%) and 9-month (42.9% vs. 14.7%) follow-ups (see Figure 1). Given the variation in primary drug type (meth vs. heroin vs marijuana, etc.) among the sample, additional analyses were conducted controlling for baseline primary drug use type using dummy-coded categories (primary heroin, primary meth, primary marijuana, etc.), as well as, primary drug use type combined (combines all clients together as one group). Results did not differ from the overall analyses as there was not any significant effects on the outcomes (i.e., both sets of analyses did not change ORs much from original analyses). We also conducted a sensitivity analysis to see if coefficients in our model (which look different by primary drug type in terms of both coefficients and percentages) were significantly different, however these were also not significantly different.
Figure 1.
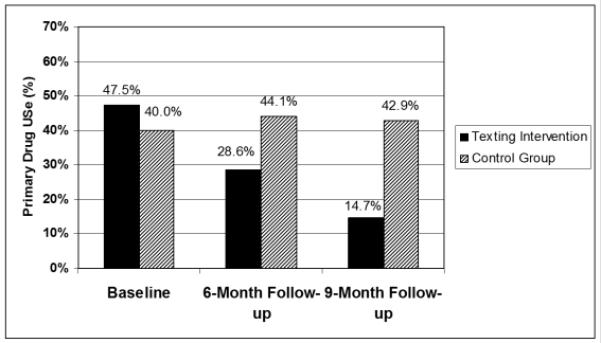
Primary substance use rates at baseline, 6-month and 9-month follow-up
Follow-up Recovery Outcomes between Study Groups
Examining recovery outcomes, results showed that youth who participated in the mobile texting intervention had higher recovery behaviors and higher self-efficacy/confidence to abstain from their primary substance compared to those in the aftercare-as-usual condition during the follow-up period. Specifically, although the number of days youth attended self-help meetings decreased over time at 6- and 9- month follow-ups (β = −0.632, p < .001), youth in the mobile texting aftercare intervention group reported participating in a higher number of days of self-help than youth in the aftercare-as-usual control group at the follow ups (β = 3.2, p = 0.047), 7 days vs 4 days at 6-months and 6 days vs 3 days at 9-months, respectively. Youth in the aftercare mobile texting intervention also reported greater participation in recovery-related extracurricular activities than youth in the aftercare-as-usual control group (β = 0.04, p < .001) at 6-months (15 vs. 11 days) and 9-months (18 vs. 13 days). Abstinence self-efficacy/confidence (measured as an outcome across time) was also found to be higher among the intervention group (OR = 1.36, p = .031) and was related to a lower odds of primary substance use over time (OR = 0.62, p = 0.002).
DISCUSSION
This paper builds on a previous study that found positive behavioral outcomes, including reduced relapse, less substance use problem severity, and increased participation in aftercare recovery behaviors among young people who participated in a 12-week pilot aftercare project comparing a mobile texting intervention to aftercare-as-usual.32 The current paper examined recovery outcomes (primary substance use, aftercare participation behaviors, and abstinence self-efficacy/confidence) at 6- and 9-months post participation in the pilot project.
Results showed promising recovery outcomes among the young people that participated in the mobile-based wellness aftercare intervention as opposed to aftercare-as-usual. Specifically, youth who participated in the mobile texting aftercare intervention were significantly less likely to relapse to their primary drug during the 6- and 9- month follow-up interviews, as well as more likely to report increased participation in 12-step meetings, extracurricular recovery activities and abstinence self-efficacy/confidence compared to those who received aftercare-as-usual. It is extremely difficult to motivate youth to maintain behavioral health changes over time following intervention. Thus, this study is important to the literature as it shows that behavior change can be sustained to 6- and 9- months out following treatment with mobile texting recovery support. Findings from our study add to the limited literature of behavioral studies that have sought out the long-term utility of mobile texting extended care interventions for sustaining behavior change among clinical populations,36 which have shown very limited to modest impact on behavior change over time.30
As with many other clinical disorders, substance use disorders among young people are challenging, and often associated with a complex array of factors that impact the course of recovery behaviors. Hence, there is a growing need for identifying useful and effective aftercare interventions that can assist substance abusing young people with behavior change efforts. Results from this pilot study suggest that using aftercare approaches with young people that are responsive to their recovery needs is ideal for promoting and sustaining treatment gains and recovery outcomes. Specifically, the current pilot aftercare intervention used with substance using youth emphasized wellness lifestyle behavior change as opposed to clinical abstinence and used a novel delivery mechanism - mobile texting. The intervention’s focus on wellness for promoting lifestyle behavior change during aftercare emerged from substance using youth perceptions about the nature of recovery during the early development of the mobile intervention.18 We found that most young people reject the view that recovery comprises lifetime chronic disease processes and total abstinence, and instead view substance use as a behavior that can be changed via lifestyle improvement (i.e., adopting alternative/healthy lifestyle alternatives) and personal control. A behavioral self-management model commonly used in healthcare fits well with the latter view of “personal control” as it promotes taking responsibility for one’s health using components of self-monitoring, feedback, reminders, and education/support.
Limitations
Results reported should be examined with caution given the pilot nature of the study which is associated with several limitations. First, the study included a relatively small sample size, which limits our ability to generalize the effects of the intervention beyond the pilot group. Second, participants in the pilot study were comprised of youth who completed a course of clinical treatment; hence results may not generalize to other youth groups who do not complete treatment. Third, we examined relapse as a function of use of one’s primary substance of abuse for which they reported receiving treatment and did not consider other substance use. This may be a limiting measure of recovery and may be problematic for being able to adequately understand recovery trajectories among young people. Fourth, there were no randomization protocols in place to control for any pre-selected attributes when assigning youth to study conditions (i.e., primary substance type, age) that could differentially affect recovery outcomes. Although results held when controlling for primary drug type, there were age differences found. Hence, our ability to understand the effects of the intervention on age specific groups is limited. Fifth, this pilot study did not examine how initial treatment outcomes may have played a role in affecting or predicting follow-up recovery outcomes. Lastly, the pilot study followed a two-group design of mobile intervention vs. aftercare-as-usual. This generic control group limited our ability to assess for potential differential effects (i.e., dosing) that the mobile texting intervention had such as monitoring or reminders on outcomes over time.
Although the results of the mobile intervention showed to be promising (preventing worsening of substance use relapse among youth over time), this is really a pilot study with several caveats (noted above) that need to be addressed in a larger clinical trial with tighter methodological controls. Overall, this study makes a valuable contribution to the extant literature on the recovery of substance use disorders among young people. Foremost, there is insufficient research on the long-term benefits of structured aftercare interventions that promote wellness/self-management of behavior via mobile technology. Future studies on the long-term utility of mobile interventions on substance use relapse for different sub-groups of users are needed to more accurately provide a comprehensive overview of the unique challenges associated with young people in recovery, such as substance-using youth with other co-occurring disorders (i.e., depression, HIV) and substance-using youth with criminal justice issues. Furthermore, future research is needed to investigate patterns of substance use among youth in recovery beyond “relapse” to one’s primary drug. This is important given that most youth are poly-drug users and continue to use other substances post-treatment that may affect recovery trajectories. Such information is important to understand, especially during the crux of the recovery assessment for better informing the development of effective aftercare strategies.
ACKNOWLEDGMENTS
This study was supported by grant K01 DA027754 from the National Institute on Drug Abuse (NIDA).
The authors acknowledge the contributions of the research team, including Samantha B. Douglas, Kara Lee, Christina Zavalza, Shannon Davidson, Grace Kim, and Andrew McKeown as well as the collaborating treatment program staff.
Footnotes
Declaration of Interests
The authors report no conflicts of interest. The authors alone are responsible for the content of this paper.
REFERENCES
- 1.Substance Abuse Mental Health Service Administration (SAMHSA) Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health 2013.
- 2.Dennis ML, Babor T, Roebuck MC, Donaldson J. Changing the focus: The case for recognizing and treating marijuana use disorders. Addiction. 2002;97:S4–S15. doi: 10.1046/j.1360-0443.97.s01.10.x. [DOI] [PubMed] [Google Scholar]
- 3.Cornelius JR, Maisto SA, Pollock NK, et al. Rapid relapse generally follows treatment for substance use disorders among adolescents. Addict Behav. 2003;28(2):381–6. doi: 10.1016/s0306-4603(01)00247-7. [DOI] [PubMed] [Google Scholar]
- 4.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic mental illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 5.McKay JR. Continuing care in the treatment of addictive disorders. Curr Psychiatry Rep. 2006;8:355–362. doi: 10.1007/s11920-006-0036-9. [DOI] [PubMed] [Google Scholar]
- 6.Kaminer Y, Godley M. From assessment reactivity to aftercare for adolescent substance abuse: Are we there yet? Child Adolesc Psychiatr Clin N Am. 2010;19:577–590. doi: 10.1016/j.chc.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 7.White WL. The mobilization of community resources to support long-term addiction recovery. J Subst Abuse Treat. 2009;36(2):146–58. doi: 10.1016/j.jsat.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Laudet A. What does recovery mean to you? Lessons from the recovery experience for research and practice. J Subst Abuse Treat. 2007;33:243–256. doi: 10.1016/j.jsat.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gonzales R, Anglin MD, Glik DC, Zavalza C. Perceptions about recovery needs and drug-avoidance recovery behaviors among youth in substance abuse treatment. J Psychoactive Drugs. 2013;45:297–303. doi: 10.1080/02791072.2013.825028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sussman S. A review of Alcoholics Anonymous/Narcotics Anonymous programs for teens. Eval Health Prof. 2010;33:26–55. doi: 10.1177/0163278709356186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly JF, Myers MG, Brown SA. The effects of age composition of 12-step groups and adolescent participation and substance use outcome. J Child Adolesc Subst Abuse. 2005;15(1):63–72. doi: 10.1300/J029v15n01_05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelly JF, Myers MG. Adolescents' participation in Alcoholics Anonymous and Narcotics Anonymous: review, implications and future directions. J Psychoactive Drugs. 2007;39(3):259–269. doi: 10.1080/02791072.2007.10400612. [DOI] [PubMed] [Google Scholar]
- 13.Whorley LW. Exploring inpatient expectations of continuing care treatment: Focus groups with substance-dependent veterans. Alcohol Treat Q. 1996;14(2):59–66. [Google Scholar]
- 14.Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of assertive continuing care on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2006;102:81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- 15.Kaminer Y, Burleson JA, Burke RH. The efficacy of aftercare for adolescents with alcohol use disorders: A randomized controlled study. J Am Acad Child Adolesc Psychiatry. 2008;47(12):1405–1412. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Godley SH, Garner BR, Passetti LL, Funk RR, Dennis ML, Godley MD. Adolescent outpatient treatment and continuing care: Main findings from a randomized clinical trial. Drug Alcohol Depend. 2010;110(1-2):44–54. doi: 10.1016/j.drugalcdep.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fisher EA. Recovery supports for young people: What do existing supports reveal about the recovery environment? Peabody J Educ. 2014;89(2):258–270. doi: 10.1080/0161956X.2014.897104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gonzales R, Anglin MD, Beattie R, Ong CA, Glik DC. Perceptions of chronicity and recovery among youth in treatment for substance use problems. J Adolesc Health. 2012;51(2):144–9. doi: 10.1016/j.jadohealth.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dunn HA. High-Level Wellness; a Collection of Twenty-Nine Short Talks on Different Aspects of the Theme "High-Level Wellness for Man and Society.". R.W. Beatty Co; Arlington, Va.: 1961. [Google Scholar]
- 20.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: Translating evidence into action. Health Aff. 2001;20:64–7. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 21.Barr VJ, Robinson S, Marin-Link B, et al. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q. 2003;7(1):73–82. doi: 10.12927/hcq.2003.16763. [DOI] [PubMed] [Google Scholar]
- 22.Banks K. Mobile phones and the digital divide. PC World Communications Inc.; San Francisco, CA: www.pcworld.com/businesscenter/article/149075/mobile_phones_and_the_digital_divide.html. Published July 29, 2008. [Google Scholar]
- 23.De Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Libr. 2012;(12) doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones KR, Lekhak N, Kaewluang N. Using mobile phones and short message service to deliver self-management interventions for chronic conditions: A meta-review. Worldviews Evid Based Nurs. 2014;11(2):81–88. doi: 10.1111/wvn.12030. [DOI] [PubMed] [Google Scholar]
- 25.Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized automated reminder diabetes system (CARDS): e-mail and SMS cell phone text messaging reminders to support. Diabetes Technol Ther. 2009;11:99–106. doi: 10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dowshen N, Kuhns LM, Johnson A, et al. Mobile phone text messaging can help young people manage asthma. BMJ. 2002;325:600. doi: 10.1136/bmj.325.7364.600/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomized trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14(4):255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leach-Lemens C. Using mobile phones in HIV care and prevention. HIV AIDS Treat Pract. 2009;137:2–8. [Google Scholar]
- 29.Fox S, Duggan M. Mobile Health Pew Internet & American Life Project. California Healthcare Center; Washington, DC: 2012. [Google Scholar]
- 30.Whittaker R, Borland R, Bullen C, et al. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2012;11 doi: 10.1002/14651858.CD006611.pub3. [DOI] [PubMed] [Google Scholar]
- 31.Suffoletto B, Callaway C, Kristan J, Monti P, Clark D. Mobile phone text message intervention to reduce binge drinking among young adults: Study protocol for a randomized controlled trial. Trials. 2013;14(96) doi: 10.1186/1745-6215-14-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gonzales R, Ang A, Murphy DA, Glik DC, Anglin MD. Substance use recovery outcomes among a cohort of youth participating in a mobile-based texting aftercare program. J Subst Abuse Treat. 2014;47(1):20–26. doi: 10.1016/j.jsat.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gonzales R, Anglin MD, Beattie R, Ong CA, Glik DC. Understanding recovery barriers: Youth perceptions about substance use relapse. Am J Health Behav. 2012;36(5):602–614. doi: 10.5993/AJHB.36.5.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gonzales R, Anglin MD, Glik DC. Exploring the feasibility of text messaging to support substance abuse recovery among youth in treatment. Health Educ Res. 2014;29:13–22. doi: 10.1093/her/cyt094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cacciola JS, Alterman AI, DePhilippis D, et al. Development and initial evaluation of the Brief Addiction Monitor (BAM) J Subst Abuse Treat. 2013;44(3):256–263. doi: 10.1016/j.jsat.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010;32(1):56–69. doi: 10.1093/epirev/mxq004. [DOI] [PMC free article] [PubMed] [Google Scholar]


