Abstract
Context
Blunt abdominal trauma often presents a substantial diagnostic challenge. Well-informed clinical examination can identify patients who require further diagnostic evaluation for intra-abdominal injuries after blunt abdominal trauma.
Objective
To systematically assess the precision and accuracy of symptoms, signs, laboratory tests, and bedside imaging studies to identify intra-abdominal injuries in patients with blunt abdominal trauma.
Data Sources
We conducted a structured search of MEDLINE (1950–January 2012) and EMBASE (1980–January 2012) to identify English-language studies examining the identification of intra-abdominal injuries. A separate, structured search was conducted for studies evaluating bedside ultrasonography.
Study Selection
We included studies of diagnostic accuracy for intra-abdominal injury that compared at least 1 finding with a reference standard of abdominal computed tomography, diagnostic peritoneal lavage, laparotomy, autopsy, and/or clinical course for intra-abdominal injury. Twelve studies on clinical findings and 22 studies on bedside ultrasonography met inclusion criteria for data extraction.
Data Extraction
Critical appraisal and data extraction were independently performed by 2 authors.
Data Synthesis
The prevalence of intra-abdominal injury in adult emergency department patients with blunt abdominal trauma among all evidence level 1 and 2 studies was 13% (95% CI, 10%–17%), with 4.7% (95% CI, 2.5%–8.6%) requiring therapeutic surgery or angiographic embolization of injuries. The presence of a seat belt sign (likelihood ratio [LR] range, 5.6–9.9), rebound tenderness (LR, 6.5; 95% CI, 1.8–24), hypotension (LR, 5.2; 95% CI, 3.5–7.5), abdominal distention (LR, 3.8; 95% CI, 1.9–7.6), or guarding (LR, 3.7; 95% CI, 2.3–5.9) suggest an intra-abdominal injury. The absence of abdominal tenderness to palpation does not rule out an intra-abdominal injury (summary LR, 0.61; 95% CI, 0.46–0.80). The presence of intraperitoneal fluid or organ injury on bedside ultrasound assessment is more accurate than any history and physical examination findings (adjusted summary LR, 30; 95% CI, 20–46); conversely, a normal ultrasound result decreases the chance of injury detection (adjusted summary LR, 0.26; 95% CI, 0.19–0.34). Test results increasing the likelihood of intra-abdominal injury include a base deficit less than −6 mEq/L (LR, 18; 95% CI, 11–30), elevated liver transaminases (LR range, 2.5–5.2), hematuria (LR range, 3.7–4.1), anemia (LR range, 2.2–3.3), and abnormal chest radiograph (LR range, 2.5–3.8). Symptoms and signs may be most useful in combination, particularly in identification of patients who do not need further diagnostic workup.
Conclusions
Bedside ultrasonography has the highest accuracy of all individual findings, but a normal result does not rule out an intra-abdominal injury. Combinations of clinical findings may be most useful to determine which patients do not require further evaluation, but the ideal combination of variables for identifying patients without intra-abdominal injury requires further study.
CLINICAL SCENARIOS
Case 1
A 25-year-old man was a restrained passenger in a high-speed motor vehicle collision. He reports abdominal pain, which he attributes to his lap restraint belt. He is hemodynamically stable with a blood pressure of 120/75 mm Hg and a pulse of 88/min. Physical examination reveals a transverse area of erythema and ecchymosis consistent with the lap restraint belt, and the patient has mild suprapubic tenderness on abdominal palpation (Figure 1).
Figure 1. Seat Belt Sign.

Linear abrasion and ecchymosis across abdominal wall from lap portion of safety restraint.
Case 2
A 55-year-old man fell 8 ft from a ladder onto the ground. He is hemodynamically stable with a blood pressure of 132/72 mm Hg and a pulse of 76/min. Physical examination reveals bruising and tenderness to the right costal margin and abrasions along the right flank but no tenderness with palpation over his abdomen. Laboratory testing demonstrates normal hematocrit, white blood cell (WBC) count, and liver transaminases and absence of hematuria.
WHY IS THIS QUESTION IMPORTANT?
Trauma is the leading cause of death in those younger than 45 years in the United States.1 Intra-abdominal injuries (any injury to intraperitoneal and retroperitoneal organs including the presence of hemoperitoneum) following blunt (80%) or penetrating (20%) trauma cause a substantial proportion of traumatic deaths.2 Motor vehicle collisions and falls are the most common causes of blunt trauma, whereas gunshot and stab wounds are the most common causes of penetrating trauma.2 Penetrating abdominal trauma has a relatively straightforward diagnostic evaluation, but blunt abdominal trauma often presents a substantial diagnostic challenge. Patients with severe injuries and ongoing hemorrhage require immediate recognition and treatment (laparotomy or angiographic embolization). Patients with seemingly less severe trauma or no apparent injury on initial examination may still have clinically significant intra-abdominal injuries, and delayed diagnosis of such injuries is an important cause of preventable morbidity and mortality.3–5 The anatomical features of the abdominal organs and the physiological events following abdominal injuries produce the signs and symptoms that direct the initial examination (eAppendix; available at http://www.jama.com) and allow categorization of patients into those who are hemodynamically unstable (persistent hypotension despite crystalloid resuscitation) or hemodynamically stable.
Hemodynamically Unstable Patients
Although all trauma patients undergo a primary and secondary survey (a trauma-focused history and physical examination; see eAppendix),6 the abdominal examination for detecting intra-abdominal injury in unstable patients is often unreliable because of the frequency of concomitant factors including distracting injuries, endotracheal intubation, and altered level of consciousness from neurological injuries or intoxication.7,8 Because these patients are often too unstable for transportation from the trauma resuscitation area to obtain computed tomography (CT) imaging, conventional algorithms for hemodynamically unstable patients make use of bedside diagnostic testing such as ultrasonography or diagnostic peritoneal lavage (DPL) to rapidly determine the need for exploratory laparotomy.9
Hemodynamically Stable Patients
In hemodynamically stable patients, abdominal CT is the reference standard diagnostic imaging test to identify abdominal injuries.9–12 Helical abdominal CT is both sensitive (97%–98%) and specific (97%–99%) for abdominal injuries.13,14 Current trauma guidelines recommend abdominal CT imaging in patients with unreliable physical examinations; physical examination findings including abdominal tenderness, abdominal wall contusions, or multiple rib fractures; or intraperitoneal fluid on ultrasound.9 However, less than 20% of abdominal CT scans obtained in patients with blunt trauma are positive for intra-abdominal injury,15,16 while less than 3% have injuries that require surgical intervention.17 When overused, abdominal CT scans contribute to increased health care costs and prolonged emergency department (ED) stays and add to the risk of contrast-induced nephropathy and lifetime risk of radiation-induced malignancy.18–20 A 20-year-old patient undergoing abdominal CT imaging has an estimated 1 in 500 lifetime risk of developing a radiation-induced cancer.20
We reviewed the evidence for clinical history, physical examination, laboratory studies, and bedside imaging to assess the likelihood of intra-abdominal injury in adults who had blunt abdominal trauma. We included bedside abdominal ultrasonography (Focused Assessment With Sonography for Trauma [FAST] examination) (Figure 2; see videos of all 4 FAST ultrasound views at http://www.jama.com) because when performed by an ED physician, it may be part of the initial clinical evaluation for an intra-abdominal injury.
Figure 2. Focused Assessment With Sonography for Trauma (FAST) Examination Positions for Assessment of Intra-abdominal Injuries.
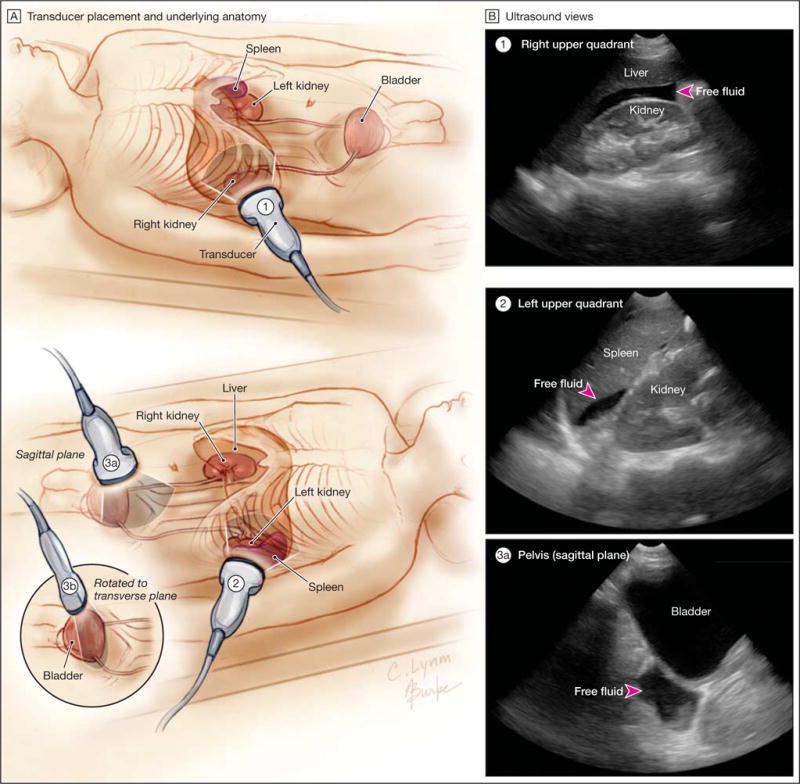
The FAST examination uses bedside ultrasonography for the rapid identification of intra-abdominal and intrapericardial hemorrhage in trauma patients. A, Locations of transducer placement for the evaluation of intra-abdominal injury and B, corresponding ultrasound views demonstrating intra-abdominal free fluid (arrowheads). Transducer planes shown are approximate. The examiner tilts the transducer as necessary to detect free fluid around tissues. A complete FAST examination also includes a pericardial ultrasound view (not shown) to assess pericardial effusion. See videos of all 4 FAST ultrasound views at http://www.jama.com.
METHODS
Literature Search Strategy
A structured search of MEDLINE (1950–January 2012) and EMBASE (1980–January 2012) was conducted by a librarian to identify English-language studies that examine the identification of intra-abdominal injuries (eAppendix). Key words in the search included physical examination, medical history taking, palpation, diagnosis, laboratory testing, imaging studies, sensitivity, specificity, observer variation, reproducibility, decision support, abdomen, non-penetrating wounds, and blunt abdominal trauma. Additional articles were identified from searching the bibliographies of relevant studies.
Because the FAST examination has been evaluated in a large number of studies, we searched for high-quality systematic reviews (search terms in Pubmed: ultrasound abdominal trauma AND systematic [sb]) to serve as a filter for primary studies that evaluated the sensitivity, specificity, and likelihood ratios of this diagnostic test.21 We retrieved the original articles included in these systematic reviews, then sought newer studies published since the most recent high-quality systematic review published.
Selection Strategy
We sought articles that evaluated the test characteristics of history and physical examination findings in adult patients with suspected intra-abdominal injury (eAppendix). Additionally, we sought articles evaluating readily available and noninvasive diagnostic studies used in the workup of suspected intra-abdominal injury. For all symptoms, signs, and noninvasive tests, we included only studies with a reference standard of abdominal CT, DPL, laparotomy, autopsy, or clinical course to detect intra-abdominal injury or hemoperitoneum. Not all intra-abdominal injuries have important clinical consequences, so we also reviewed each article for clinically significant intra-abdominal injury. We accepted the classification of the investigators of each study, though clinically significant intra-abdominal injuries almost always implied that the patient required an invasive therapeutic procedure (therapeutic surgery or angiographic embolization to stop hemorrhage). All retrieved studies underwent a review of methodological quality.
Statistical Analysis
We abstracted the published data from all studies meeting the selection criteria. Sensitivity, specificity, and likelihood ratios (LRs) were calculated with confidence intervals for each symptom, sign, or laboratory or imaging test. The summary prevalence (pretest probability) was calculated with random-effects measures and risk factors were assessed with odds ratios (ORs).22 Tests with higher specificity have higher LRs and positive results are most useful for identifying patients with an intra-abdominal injury, while tests with higher sensitivity have lower LRs and negative results are most useful for identifying patients without an intra-abdominal injury. For findings evaluated in only 1 study, we provide the point estimate with its confidence interval. We used ranges to summarize results for findings evaluated in only 2 studies and univariate random-effects summary measures with confidence intervals for findings evaluated in 3 studies (Comprehensive Meta-analysis, version 2, Biostat Inc). When 4 or more studies suitable for meta-analysis were identified, a bivariate random-effects model was used to create summary measures (SAS, version 9.2, TS Level 2M3, SAS Institute Inc), though the univariate estimates were used if the model did not converge on a reliable solution.23 Evidence level 4 studies were not included in any summary measures (see eAppendix for evidence level definitions). We assessed findings for statistical heterogeneity that were evaluated in more than 3 studies. The large number of ultrasound studies allowed us to evaluate publication bias by inspecting the funnel plot, Egger test of the intercept, and the trim-and-fill procedure to impute the effect of missing studies (Comprehensive Meta-analysis, version 2).24
RESULTS
Study Characteristics
The initial search identified 2704 studies that were systematically reviewed (eFigure 1), with 12 articles retained for inclusion (Table 1). The majority of included studies were performed at American College of Surgeons–designated level I trauma centers (highest level of trauma surgical care, with 24-hour availability of all specialists). Sample sizes ranged from 117 to 3435 patients. All studies defined inclusion criteria as adult patients with any blunt abdominal trauma except for 2 studies that included only adult patients in motor vehicle collisions.27,32
Table 1.
Studies Assessing the Clinical Examination to Identify Intra-abdominal Injury
| Source | Setting | Year | Patients, No. | Injuries, No. (%) | Inclusion Criteria | Reference Standard |
|---|---|---|---|---|---|---|
| Evidence Level 1 | ||||||
| Holmes et al,17 2009 | US level I trauma center, university hospital | 2002–2004 | 3435 | 311 (9.1) | Blunt torso trauma with CT of abdomen, DPL, or laparoscopy/laparotomy | CT of abdomen for stable patients or DPL/laparotomy for unstable patients |
|
| ||||||
| Poletti et al,25 2004 | US level I trauma center, university hospital | NA | 714 | 85 (12) | Blunt abdominal trauma with CT of abdomen | CT of abdomen |
|
| ||||||
| Evidence Level 3 | ||||||
| Beck et al,26 2004 | US level I trauma center, university hospital | NA | 213 | 56 (26) | Blunt trauma with CT of abdomen | CT of abdomen |
|
| ||||||
| Chandler et al,27 1997 | US level I trauma center, university hospital | 1993–1994 | 117 | 18 (15) | Adult patients in motor vehicle collision | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Ferrera et al,28 1998 | US level I trauma center, university hospital | 1995–1996 | 350 | 54 (15) | Blunt trauma and normal mental status with CT of abdomen and/or DPL | CT of abdomen or DPL |
|
| ||||||
| Mofidi et al,29 2010 | University hospital in Iran | 2007–2008 | 400 | 68 (17) | Blunt abdominal trauma | CT of abdomen or laparotomy |
|
| ||||||
| Richards and Derlet,30 1998 | US level I trauma center, university hospital | 1995 | 196 | 22 (11) | Blunt abdominal trauma with CT of abdomen | CT of abdomen |
|
| ||||||
| Sahdev et al,31 1991 | US level I trauma center, university hospital | 1988–1989 | 309 | 51 (17) | Blunt multisystem trauma patients | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Velmahos et al,32 1999 | US level I trauma center, university hospital | 1984–1985 | 400 | 20 (5.0) | Restrained patients in motor vehicle collision | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Evidence Level 4 | ||||||
| Grieshop et al,33 1995a | US level I trauma center, university hospital | 1991–1992 | 956 | 44 (4.6) | Blunt abdominal trauma with CT of abdomen | CT of abdomen, DPL, or clinical course |
|
| ||||||
| Mackersie et al,34 1989b | US level I trauma center, university hospital | 1985–1988 | 3223 | 265 (8.2) | Blunt abdominal trauma | Laparotomy or clinical course |
|
| ||||||
| Richards et al,35 1997c | US level I trauma center, university hospital | 1993–1994 | 444 | 49 (11) | Blunt abdominal trauma with CT of abdomen within 24 h of arrival | CT of abdomen |
Abbreviations: CT, computed tomography; DPL, diagnostic peritoneal lavage; NA, not available.
Outcome was intra-abdominal injury that influenced patient management or outcome.
Outcome was intra-abdominal injury with operative repair.
Outcome was intra-abdominal injury defined as any potentially serious or life-threatening injury on CT or laparotomy.
Analysis of the systematic reviews and updated literature search (eFigure 2 and eFigure 3) evaluating the FAST examination identified 22 studies meeting selection criteria (Table 2).25,36–56 All studies were prospective, with consecutive enrollment and blinding, and included a reference standard (CT, DPL, laparotomy, autopsy, and/or clinical course).
Table 2.
Studies Assessing the FAST Examination to Identify Intra-abdominal Injury
| Source | Setting | Years | Patients, No. | Injuries, No. (%) | Inclusion Criteria | Reference Standard |
|---|---|---|---|---|---|---|
| Evidence Level 1 | ||||||
| Bode et al,36 1999 | US level I trauma center, university hospital | 1993–1998 | 1671 | 97 (5.8) | Blunt abdominal trauma | CT of abdomen, laparotomy, autopsy, or clinical course |
|
| ||||||
| Healey et al,37 1996 | US level I trauma center, university hospital | NA | 796 | 51 (6.4) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Kern et al,38 1997 | US level I trauma center, university hospital | 1995–1996 | 518 | 30 (5.8) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Richards et al,39 2002 | US level I trauma center, university hospital | 1995–1998 | 3264 | 396 (12) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Rozycki et al,40 1998 | US level I trauma center, university hospital | NA | 1227 | 74 (6.0) | Torso trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Evidence Level 2 | ||||||
| Boulanger et al,41 1996 | Regional Canadian trauma center | 1993–1995 | 400 | 63 (16) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy |
|
| ||||||
| Boulanger et al,42 1999 | Regional Canadian trauma center | 1995–1997 | 460 | 82 (18) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy |
|
| ||||||
| Brenchley et al,43 2006 | UK teaching hospital | NA | 153 | 8 (5.2) | Blunt trauma | CT of abdomen, DPL, laparotomy, autopsy, or clinical course |
|
| ||||||
| Brooks et al,44 2004 | UK teaching hospital | NA | 100 | 9 (9.0) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Goletti et al,45 1994 | Italian university hospital | 1994–1995 | 250 | 52 (21) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy |
|
| ||||||
| Ma et al,46 2005 | US level I trauma center, university hospital | 1999–2000 | 252 | 35 (14) | Blunt trauma with trauma team activation | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| McGahan et al,47 1997 | US level I trauma center, university hospital | NA | 121 | 38 (31) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy |
|
| ||||||
| McKenney et al,48 1994 | US level I trauma center, university hospital | 1992–1993 | 200 | 30 (18) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy |
|
| ||||||
| Miller et al,49 2003 | US level I trauma center, university hospital | 2001–2002 | 359 | 38 (11) | Blunt abdominal trauma | CT of abdomen |
|
| ||||||
| Poletti et al,50 2003 | US level I trauma center, university hospital | 2000–2001 | 204 | 83 (41) | Blunt abdominal trauma | CT of abdomen or laparotomy |
|
| ||||||
| Poletti et al,25 2004 | US level I trauma center, university hospital | NA | 488 | 60 (12) | Blunt abdominal trauma with CT of abdomen | CT of abdomen |
|
| ||||||
| Rose et al,51 2001 | US level I trauma center, university hospital | 1997–1998 | 104 | 15 (14) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Röthlin et al,52 1993 | US level I trauma center, university hospital | 1992–1993 | 312 | 126 (40) | Blunt abdominal or thoracic trauma | CT of abdomen, laparotomy, or clinical course |
|
| ||||||
| Rozycki et al,53 1995 | US level I trauma center, university hospital | NA | 371 | 65 (18) | Blunt abdominal or thoracic trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Shackford et al,54 1999 | University hospital | NA | 234 | 51 (22) | Blunt abdominal trauma | CT of abdomen, DPL, laparotomy, or clinical course |
|
| ||||||
| Soyuncu et al,55 2007 | Turkish university hospital | 2001–2002 | 442 | 35 (7.9) | Blunt abdominal trauma | CT of abdomen, laparotomy, or autopsy |
|
| ||||||
| Tso et al,56 1992 | US level I trauma center, university hospital | 1990 | 163 | 16 (9.8) | Blunt abdominal trauma with CT or DPL | CT of abdomen, DPL,or laparotomy |
Abbreviations: CT, computed tomography; DPL, diagnostic peritoneal lavage; FAST, Focused Assessment With Sonography for Trauma; NA, not available.
Prevalence of Intra-abdominal Injury in Patients Presenting With Abdominal Trauma
The prevalence of intra-abdominal injury in adult ED patients with blunt abdominal trauma among all evidence level 1 and 2 studies (n=23 studies with 15 750 patients; eAppendix) was 13%, with clinically narrow confidence limits despite heterogeneity (95% CI, 10%–17%; I2 = 96%; P <.001 for heterogeneity).17,25,36–56 Among the evidence level 1 and 2 studies that reported the prevalence of clinically significant injuries as defined by the original investigators (n=4 studies with 4908 patients), the prevalence was 4.7% (95%CI, 2.5%–8.6%; I2 = 96%; P <.001 for heterogeneity).17,25,41,49
Accuracy of Individual Findings From the Clinical History and Physical Examination
Risk Factors
The type of trauma mechanism (fall, pedestrian hit by a vehicle, motor vehicle collision, motorcycle collision, or other causes) did not identify patients more or less likely to have an intra-abdominal injury ( ; P=.60).26 In the same study, the presence of alcohol intoxication did not identify patients at higher risk (OR, 0.46; 95% CI, 0.24–0.89; P=.02).26 Patients who required intubation in the field or in the ED were more likely to have an intra-abdominal injury (OR, 2.5; 95% CI, 1.1–5.9).26
Abdominal Symptoms and Examination
Only 1 study assessed interrater reliability of physical examination findings (eTable 1).17 In patients who had blunt abdominal trauma, abdominal pain as a symptom (LR, 1.6; 95% CI, 1.3–2.0)28 and abdominal tenderness with palpation (summary LR, 1.4; 95% CI, 1.3–1.5; I2=0%; P=.62 for heterogeneity)17,25,28,30 were less predictive in identifying intra-abdominal injury compared with other findings (Table 3). The presence of rebound tenderness was infrequent (1.2% in a single large study), but its presence had a high LR (6.5; 95% CI, 1.8–24).25 The presence of abdominal distention (LR, 3.8; 95% CI, 1.9–7.6) or abdominal guarding (LR, 3.7; 95% CI, 2.3–5.9) appears more reliable than rebound tenderness because of narrower confidence intervals.25 In patients involved in motor vehicle collisions, the seat belt sign (a continuous abrasion or ecchymosis secondary to an overlying lap belt) (Figure 1) is also useful (LR range, 5.6–9.9).27,32 The absence of abdominal pain after trauma (LR, 0.52; 95% CI, 0.34–0.79)28 and abdominal tenderness to palpation (summary LR, 0.61; 95% CI, 0.46–0.80; I2 = 54%; P = .09 for heterogeneity)17,25,28,30 does not rule out intra-abdominal injury. The absence of rebound tenderness, abdominal distention, or guarding is not useful because the LR for each of these approaches 1.0.25
Table 3.
Accuracy of Symptoms and Signs to Identify Intra-abdominal Injury From Evidence Level 1 to 3 Studiesa
| Finding/Source | Sensitivity, % (95% CI) | Specificity, % (95% CI) | Positive Likelihood Ratio (95% CI) | Negative Likelihood Ratio (95% CI) |
|---|---|---|---|---|
| Seat belt sign27,32b,c | 50 (35–65) | 91–95 | 5.6–9.9 | 0.53–0.55 |
| Rebound tenderness25 | 5 (0–10) | 99 (99–100) | 6.5 (1.8–24) | 0.96 (0.91–1.0) |
| Hypotension (systolic blood pressure <90 mm Hg)17 | 12 (9–16) | 98 (97–98) | 5.2 (3.5–7.5) | 0.90 (0.87–0.94) |
| Abdominal distention25 | 13 (6–20) | 97 (95–98) | 3.8 (1.9–7.6) | 0.90 (0.83–0.98) |
| Guarding25 | 26 (16–35) | 93 (91–95) | 3.7 (2.3–5.9) | 0.80 (0.70–0.91) |
| Concomitant femur fracture17 | 12 (9–16) | 96 (95–97) | 2.9 (2.1–4.1) | 0.92 (0.88–0.96) |
| Glasgow Coma Scale score <1417,25b | 23–27 | 85–88 | 1.8–2.0 | 0.86–0.87 |
| Abdominal pain as a symptom28 | 70 (57–81) | 57 (51–63) | 1.6 (1.3–2.0) | 0.52 (0.34–0.79) |
| Costal margin tenderness17 | 52 (46–57) | 65 (63–66) | 1.5 (1.3–1.7) | 0.74 (0.66–0.84) |
| Abdominal tenderness to palpation17,25,28,30d | 71 (57–82) | 50 (44–57) | 1.4 (1.3–1.5) | 0.61 (0.46–0.80) |
See eTable 1 for results from individual studies.
Finding reported in only 2 studies, so summary measures are reported as a range.
A single value with 95% CI is provided for sensitivity since the result was identical for both studies.
Random-effects univariate summary measures are reported because the data did not converge on a reliable bivariate solution.
Extra-abdominal Findings
Hypotension on arrival to the ED (systolic blood pressure <90 mm Hg; LR, 5.2; 95% CI, 3.5–7.5) is among the most useful signs applicable to all patients with abdominal trauma.17 Patients with an altered mental status (Glasgow Coma Scale score <14; LR range, 1.8–2.0) have an increased likelihood of intra-abdominal injury.17,25 The presence of a femoral fracture occurring concomitantly with abdominal trauma also increases the likelihood of an abdominal injury (LR, 2.9; 95% CI, 2.1–4.1).17
Laboratory Testing and Plain Film Radiographs
Following abdominal trauma, several abnormal laboratory test results studied in evidence level 1 through 3 studies suggest intra-abdominal injury (Table 4). A base deficit (< −6 mEq/L) is predictive of an intra-abdominal injury (LR, 18; 95% CI, 11–30).29 Hematuria (defined as >25–50 red blood cells [RBCs] per high-power field) carries a 4-fold increased risk of intra-abdominal injury (LR range, 3.7–4.1).17,30 A hematocrit level of less than 30% (LR, 3.3; 95% CI, 2.4–4.5)17 increases the likelihood of intra-abdominal injury more than less-severe anemia (hematocrit <36%; LR, 2.2; 95% CI, 1.6–3.1).25 Other laboratory markers including elevated WBC count (LR, 1.7; 95% CI, 1.5–2.0)25 and elevated lactate (LR, 1.3; 95% CI, 1.1–1.5)25 are less useful to identify patients with intra-abdominal injury. Elevated liver transaminases (aspartate aminotransferase or alanine aminotransferase) are markers for liver injury (LR range, 2.5–5.2),25,31 with higher levels increasing the likelihood.31
Table 4.
Accuracy of Diagnostic Testing to Identify Intra-abdominal Injury From Evidence Level 1 to 3 Studiesa
| Test and Threshold | Sensitivity, % (95% CI) | Specificity, % (95% CI) | Positive Likelihood Ratio (95% CI) | Negative Likelihood Ratio (95% CI) |
|---|---|---|---|---|
| Laboratory | ||||
| Base deficit <−6 mEq/L29 | 88 (78–95) | 95 (92–97) | 18 (11–30) | 0.12 (0.06–0.24) |
|
| ||||
| Liver transaminases, U/L | ||||
| AST or ALT >13031 | 59 (45–71) | 89 (84–92) | 5.2 (3.5–7.9) | 0.46 (0.33–0.65) |
|
| ||||
| AST >5025 | 73 (62–82) | 70 (66–74) | 2.5 (2.0–3.0) | 0.38 (0.26–0.56) |
|
| ||||
| Hematuria, red blood cells per high-power field | ||||
| >2517 | 41 (35–46) | 90 (89–91) | 4.1 (3.4–4.9) | 0.66 (0.60–0.72) |
|
| ||||
| >5030 | 64 (43–80) | 83 (77–88) | 3.7 (2.4–5.8) | 0.44 (0.25–0.77) |
|
| ||||
| Hematocrit, % | ||||
| <3017 | 27 (9–16) | 92 (96–98) | 3.3 (2.4–4.5) | 0.79 (0.71–0.88) |
|
| ||||
| <3625 | 37 (27–48) | 83 (80–86) | 2.2 (1.6–3.1) | 0.76 (0.64–0.90) |
|
| ||||
| Change >530 | 27 (13–48) | 70 (63–76) | 0.91 (0.44–1.9) | 1.0 (0.79–1.4) |
|
| ||||
| White blood cell count >10 000 cells/μL25 | 81 (72–88) | 54 (50–58) | 1.7 (1.5–2.0) | 0.35 (0.23–0.55) |
|
| ||||
| Serum lactate >2.2 mmol/L25 | 73 (62–82) | 44 (40–48) | 1.3 (1.1–1.5) | 0.61 (0.41–0.90) |
|
| ||||
| Imaging | ||||
| Abnormal FAST examination result, bedside (all US references) | ||||
| Unadjustedb | 82 (75–89) | 99 (98–99) | 69 (38–101) | 0.18 (0.11–0.25) |
|
| ||||
| Adjusted for publication biasc | 74 (66–80) | 96 (91–98) | 30 (20–46) | 0.26 (0.19–0.34) |
|
| ||||
| Abnormal chest radiograph17,25d | 28–42 | 83–93 | 2.5–3.8 | 0.70–0.78 |
|
| ||||
| Abnormal pelvic radiograph25e | 10 (5–18) | 94 (92–96) | 1.6 (0.78–3.4) | 0.96 (0.90–1.0) |
Abbreviations: AST, aspartate aminotransferase; ALT, alanine transaminase; FAST, Focused Assessment With Sonography for Trauma.
Random-effects bivariate summary measures unadjusted for publication bias.
Random-effects univariate summary measures adjusted for publication bias.
Finding reported in only 2 studies, so summary measures are reported as a range. Abnormalities include fracture, pleural effusion, pneumothorax, pneumomediastinum, or parenchymal opacity consistent with contusion.
Acute fracture.
Abnormal chest radiograph findings (LR range, 2.5–3.8) increase the likelihood of concomitant intra-abdominal injury.17,25 Normal plain chest or pelvic radiograph findings do not have a sufficiently low LR to rule out abdominal injury (LR range, 0.70–0.96).17,25
A few normal laboratory test results had lower LRs than the findings from physical examination. The presence of a base deficit of −6 mEq/L or greater (LR, 0.12; 95% CI, 0.06–0.24), WBC count of less than 10 000 cells/μL (LR, 0.35; 95% CI, 0.23–0.55), aspartate aminotransferase of less than 50 U/L (LR, 0.38; 95% CI, 0.26–0.56), and urinalysis with 50 or fewer RBCs per high-power field (LR, 0.44; 95% CI, 0.25–0.77) had LR point estimates lower than the findings for abdominal pain as a symptom or sign.17,25,28–30
Bedside Ultrasound (FAST Examination)
The FAST examination is by far the most accurate single bedside test in the evaluation of patients with suspected intra-abdominal injury (Table 4). A positive FAST examination finding makes an intra-abdominal injury likely with a summary LR of 69 (95% CI, 38–101; I2=75%; P<.001 for heterogeneity). A normal FAST examination finding decreases the likelihood of an intra-abdominal injury (summary LR, 0.18; 95% CI, 0.11–0.25; I2= 89%; P<.001 for heterogeneity). Despite the statistical heterogeneity, the confidence intervals suggest clinical utility. Inspection of the funnel plot and Egger test of the intercept (P=.001) reveals possible publication bias with missing studies of lower accuracy (eFigure 4, A and B). The trim-and-fill procedure to impute the missing values yields an adjusted univariate summary LR of 30 (95% CI, 20–46) for a positive FAST examination result. After adding the imputed studies, the negative result becomes slightly less useful, with an adjusted univariate summary LR of 0.26 (95% CI, 0.19–0.34).
Because 5 studies excluded patients with hemodynamic instability, we assessed this criterion as a contributor to heterogeneity.25,49,50,53,56 Patients with hemodynamic instability might be more likely to have obvious FAST examination findings identifying an intra-abdominal injury. A positive FAST examination result had a summary LR of 82 (95% CI, 39–125) for studies that included hemodynamically unstable patients, while those that excluded such patients had a summary LR of 36 (95% CI, 3.8–69), a difference that approached statistical significance (P=.06). A negative FAST examination finding had a summary LR of 0.16 (95% CI, 0.10–0.21) for studies that included hemodynamically unstable patients, while those that excluded such patients had a summary LR of 0.33 (95% CI, 0.08–0.58), a difference that was not statistically significant (P=.10).
Accuracy of Physician Impression of Intra-abdominal Injury and Clinical Decision Rules
Physicians’ overall clinical impressions of intra-abdominal injury (surveyed prior to abdominal CT imaging) were compared with clinical decision rules in 2 evidence level 1 studies (Table 5 and Table 6).17,25 In one study, physicians recorded their overall impression of intra-abdominal injury (>50%, >10%–50%, >5%–10%, 1%–5%, or <1% probability) (complete data set provided by J.F.H.) before the FAST examination results were known.17 A second study had physicians rank their clinical impression into 5 ordinal categories that described their impression of the likelihood of an intra-abdominal injury from “most likely” to “no suspicion,” taking into consideration the clinical examination, basic laboratory results, plain film radiography, and the FAST examination.25 Both studies showed an appropriately increasing LR for an intra-abdominal injury as clinicians’ impression of the probability of an injury increased (χ2=185; P<.001 for the correlation between level of suspicion and LR). When patients were rated as most likely to have an intra-abdominal injury (probability >50% or level 5), the LR was 11 to 19. When physicians’ impression was that patients did not have an intra-abdominal injury (no suspicion or <1% probability; 24%–46% of patients), the LR range was 0.21 to 0.38.
Table 5.
Accuracy of Physician Clinical Impression to Identify Intra-abdominal Injury From Evidence Level 1 to 3 Studies
| Clinical Impression | Serial Likelihood Ratio (95% CI) |
|---|---|
| Probability estimate of injury based on overall clinical impression, %17a | |
| >50 | 11 (4.1–30) |
|
| |
| >10 to 50 | 8.9 (5.2–16) |
|
| |
| >5 to 10 | 2.5 (2.0–3.0) |
|
| |
| 1 to 5 | 0.46 (0.33–0.62) |
|
| |
| <1 | 0.21 (0.11–0.42) |
|
| |
| Overall clinical impression, ordinal ranking from no suspicion (1) to most likely to have an injury (5)25b | |
| 5 | 19 (7.7–48) |
|
| |
| 4 | 3.2 (1.6–6.5) |
|
| |
| 3 | 1.6 (1.1–2.3) |
|
| |
| 2 | 0.57 (0.32–1.0) |
|
| |
| 1 | 0.38 (0.24–0.61) |
Clinical impression established before Focused Assessment With Sonography for Trauma (FAST) examination was performed. When dichotomized into injury unlikely (<1%) vs injury possible (≥1%), injury possible has a likelihood ratio of 1.3 (95% CI, 1.2–1.4) and injury unlikely has a likelihood ratio of 0.21 (95% CI, 0.11–0.42).
Clinical impression established after FAST examination performed. When dichotomized into no suspicion (1) vs injury possible (>1), injury possible has a likelihood ratio of 1.6 (95% CI, 1.4–1.8) and no suspicion has a likelihood ratio of 0.38 (95% CI, 0.24–0.61).
Table 6.
Accuracy of Combinations of Findings to Identify Intra-abdominal Injury From Evidence Level 1 to 3 Studies
| Combination | Sensitivity, % (95% CI) | Specificity, % (95% CI) | Positive Likelihood Ratio (95% CI) | Negative Likelihood Ratio (95% CI) |
|---|---|---|---|---|
| Abnormal mental status, abdominal guarding, or abdominal tenderness25 | 65 (53–75) | 75 (71–79) | 2.6 (2.0–3.2) | 0.47 (0.34–0.65) |
| Abnormal mental status, abdominal guarding, abdominal tenderness, abnormal FAST examination result, or abnormal chest radiograph25 | 89 (80–94) | 36 (32–40) | 1.4 (1.3–1.5) | 0.31 (0.17–0.58) |
| Hematuria (≥25 RBCs/high-power field), abnormal chest radiograph, abdominal tenderness, GCS score <14, costal margin tenderness, femur fracture, or hematocrit <30%17 | 97 (95–99) | 28 (26–29) | 1.3 (1.3–1.4) | 0.10 (0.06–0.17) |
| Abnormal mental status, abdominal guarding, abdominal tenderness, AST >50 U/L, WBC count >10 000 cells/μL, or hematocrit <36%25 | 99 (94–100) | 19 (16–22) | 1.2 (1.2–1.3) | 0.06 (0.01–0.45) |
| Abnormal mental status, abdominal guarding, abdominal tenderness, AST >50 U/L, WBC count >10 000 cells/μL, hematocrit <36%, abnormal FAST examination result, or abnormal chest radiograph25a | 100 (95–100) | 12 (9–15) | 1.1 (1.1–1.2) | 0.05 (0.00–0.80) |
Abbreviations: AST, aspartate aminotransferase; FAST, Focused Assessment with Sonography for Trauma; GCS, Glasgow Coma Scale; RBC, red blood cell; WBC, white blood cell.
0.5 was added to each cell of the 2 × 2 table to obtain the upper 95% CI for the 100% sensitivity result.
Explicit combinations of findings have been studied because individual findings and the clinical impression do not accurately identify patients without an intra-abdominal injury following abdominal trauma. Poletti et al25 used multivariate modeling to select increasingly useful combinations of findings to identify patients at low risk of injuries. A normal physical examination (normal mental status and no abdominal guarding or tenderness) in addition to normal laboratory test results (aspartate aminotransferase, WBC count, and hematocrit) together suggested a very low likelihood of intra-abdominal injury (LR, 0.06; 95% CI, 0.01–0.45).25 The addition of a normal chest radiograph and normal FAST examination result could rule out an intra-abdominal injury (LR, 0.05; 95% CI, 0–0.80) were it not for the broad confidence intervals.25 Similarly the lack of hematuria, abdominal tenderness, costal margin tenderness, abnormal chest x-ray, and femur fracture together with a normal mental status and initial hematocrit of 30% or higher made injury unlikely and had the narrowest confidence intervals of the varying combinations of findings (LR, 0.10; 95% CI, 0.06–0.17).17
Accuracy of Findings to Detect Clinically Significant Intra-abdominal Injuries
In one evidence level 1 study, test characteristics for individual symptoms, signs, laboratory studies, and plain film radiographs for identifying patients with clinically significant intra-abdominal injuries (therapeutic surgery or angiographic embolization) did not differ substantially vs when the outcome was any intra-abdominal injury (eTable 4).25 However, when physicians recorded their overall impression of any injury after incorporating the results of their clinical findings, laboratory, and radiographic results (ordinal scale from least likely [1] to most likely [5]), the investigators found a stepwise increased prevalence of these clinically significant intra-abdominal injuries (0.34%, 0%, 2.0%, 21%, and 52%, respectively, for increasing suspicion).
Two evidence level 1 studies evaluated combinations of explicit findings to identify patients with clinically significant injuries.17,25 The absence of abdominal tenderness, costal margin tenderness, hypotension (systolic blood pressure <90 mm Hg), hematuria (≥25 RBCs/high-power field), and anemia (hematocrit <30%), together with a normal mental status, is the best combination of findings to rule out clinically significant intra-abdominal injury (LR, 0.02; 95% CI, 0–0.29).17
Three evidence level 1 and 2 studies presented data that allowed us to extract performance of the FAST examination in detecting clinically significant injuries.25,41,49 One of these studies defined clinically significant as an injury that required a therapeutic laparotomy (as opposed to a diagnostic laparotomy) within 24 hours of the trauma.41 Two other studies defined clinically significant as an injury that required therapeutic laparotomy or angiographic embolization.25,49 For identifying these patients, a positive FAST examination result had a summary LR of 16 (95% CI, 12–21) while a negative FAST examination result decreased the likelihood of a significant injury (summary LR, 0.26; 95% CI, 0.10–0.67).
LIMITATIONS
Our primary objective was to assess test characteristics of clinical findings to identify intra-abdominal injury, counting all injuries as important. An alternative and more complex outcome considers only clinically significant abdominal injuries requiring acute intervention or altering management. Such an outcome was reported in only 7 studies (eTable 4).17,25,33–35,41,49 While we did not review studies of clinical outcomes, a Cochrane systematic review found that ultrasound-based patient management algorithms reduced CT ordering by 50%.57
Physicians’ overall clinical impression regarding the risk of intra-abdominal injury was reported in only 2 studies, with neither strictly specifying the clinical experience of the physicians, so the generalizability of the results cannot be assessed.17,25 However, in both studies an appropriate increase in the LR occurred as patients were categorized into 5 strata from least likely to most likely to have an intra-abdominal injury. Potentially, no explicit combination of clinical findings will improve the accuracy for identifying intra-abdominal injury compared with clinical impression. Future studies are needed to determine the impact of the clinical impression before and after the FAST examination such that the role of the FAST examination with or without explicit combinations of findings can be better defined.
Differences in inclusion/exclusion criteria may have affected the probability of intra-abdominal injury and test characteristics of clinical findings. Studies excluding hemodynamically unstable patients likely have a different baseline population than studies including these patients. Ultrasound studies including hemodynamically unstable patients have higher positive LRs and lower negative LRs compared with studies constrained to hemodynamically stable patients. However, with only 5 studies of hemodynamically stable patients, we may not have had enough statistical power to detect a difference. A single study directly compared the results of the FAST examination between normotensive and hypotensive patients, but it was similarly underpowered to detect important differences.40
Many of the included studies were conducted more than 10 years ago. Standards of care and technology have changed over this period. Studies using earlier-generation CT scanners may have different outcome rates if more accurate, later-generation scanners were used. Additionally, DPL was included as a reference standard in many studies because it was commonly used to direct management in patients with blunt abdominal trauma at the time of the studies. However, while DPL was still included as an option by trauma guidelines in 2002, it is used infrequently now as it is more invasive and less accurate compared with other diagnostic tests such as ultrasound and CT.9 Although 22 of 32 studies included DPL as one of the reference standards, no study used DPL as the sole reference standard.
SCENARIO RESOLUTION
Case 1
This patient’s physical examination is highly concerning for intra-abdominal injury. The presence of a seat belt sign has the highest LR of all physical examination findings (LR range, 5.6–9.9). Even with a pretest probability as low as 5% (the lower bound of 95% confidence interval for prevalence),17,25,36–56 the posttest probability with the presence of a seat belt sign is at least 23% for intra-abdominal injury. This patient should undergo further evaluation to detect any clinically significant intra-abdominal injuries.
Case 2
Based on the literature, this patient’s pretest probability for intra-abdominal injury is approximately 13%.17,25,36–56 The absence of abdominal tenderness to palpation (LR, 0.61) in this patient does not rule out intra-abdominal injury. The presence of right costal margin tenderness might alert the clinician to the possibility of liver injury (LR, 1.5). Performance of a bedside FAST examination would further risk-stratify this patient. A negative FAST examination result (adjusted LR, 0.26) decreases the posttest probability of an intra-abdominal injury. After a period of observation and serial negative abdominal examination results, the patient is discharged home with instructions and close follow-up with his primary care physician.
CLINICAL BOTTOM LINE
The presence or absence of abdominal tenderness does not reliably include or exclude intra-abdominal injury. Rebound tenderness, abdominal distention, guarding, seat belt sign, and hypotension (defined as systolic blood pressure <90 mm Hg) have LRs indicating the need for rapid evaluation. Although most laboratory tests lack specificity, a base deficit, hematuria, elevated liver transaminases, and anemia should alert the clinician to the possibility of intra-abdominal injury.
The data for the FAST examination are most reliable and have been studied in multiple high-quality studies. A positive FAST examination result indicates a high likelihood of intra-abdominal injury and this single test may perform better than the physician’s overall clinical impression. In patients with high clinical probability, a positive FAST examination result essentially confirms an intra-abdominal injury. A negative FAST examination in moderate- to high-risk patients does not sufficiently exclude intra-abdominal injury. While a negative FAST examination result in low-risk patients lowers the posttest probability, it does not necessarily rule out an intra-abdominal injury. Nonetheless, 2 randomized controlled trials demonstrate a safe reduction in abdominal CT use with a protocol including the FAST examination.51,58
A few cautions exist regarding a normal FAST examination result. First, accuracy of the FAST examination requires an experienced operator.46,54 Physicians who perform the test must have prior training, since proficiency requires 20 to 50 examinations (eAppendix), and physicians should be aware of their own accuracy. Second, publication bias suggests that a normal FAST examination result may not have as favorable an LR as suggested in published studies. The impact of this bias is inferred when comparing the 2 studies in which the overall clinical impression was established before17 vs after25 the FAST examination. When the FAST examination was included as part of the clinical impression, the overall impression of no abdominal injury was less accurate, suggesting that physicians underestimate the possibility of a false-negative FAST examination result. Because of publication bias, using the adjusted LR for a positive study (LR, 30; 95% CI, 20–46) would be more conservative. The FAST examination may be best used as one of several explicit findings (combinations of clinical examination findings and laboratory data). Unfortunately, no combination of findings has been validated independently and prospectively for widespread use.59,60 Validation of previously derived clinical decision rules would be an important step to limiting radiation exposure from unnecessary abdominal CT scans.
Supplementary Material
Acknowledgments
Funding/Support: The study did not receive any direct funding. Dr Nishijima was supported through a Mentored Clinical Research Training Program Award (K30 and KL2), grant UL1 RR024146 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and the NIH Roadmap for Medical Research.
Role of the Sponsors: The NCRR and NIH had no role in design or conduct of the study; in the analysis or interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
The Rational Clinical Examination Section Editors: David L. Simel, MD, MHS, Durham Veterans Affairs Medical Center and Duke University Medical Center, Durham, NC; Drummond Rennie, MD, Deputy Editor.
Author Contributions: Dr Nishijima had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Nishijima, Simel, Wisner, Holmes.
Acquisition of data: Nishijima, Holmes.
Analysis and interpretation of data: Nishijima, Simel, Holmes.
Drafting of the manuscript: Nishijima, Simel, Holmes.
Critical revision of the manuscript for important intellectual content: Nishijima, Simel, Wisner, Holmes.
Statistical analysis: Nishijima, Simel, Holmes.
Administrative, technical, or material support: Nishijima, Simel, Holmes.
Study supervision: Nishijima, Simel, Wisner, Holmes.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential conflicts of Interest. Dr Simel receives honoraria for contributions to JAMAEvidence.com.
Disclaimer: The views expressed in this article are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH. Information on the NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://commonfund.nih.gov/clinicalresearch/overview-translational.aspx. Dr Simel did not participate in the editorial decision for this article. No other disclosures were reported.
Online-Only Material: The eAppendix, eTables 1 through 4, eFigures 1 through 4, and the interactive videos of the FAST examination are available at http://www.jama.com.
Additional Contributions: We appreciate the assistance of Andrea Markinson, MLS, DPM, State University of New York, Downstate Medical Center, for her support with the database searches. We also appreciate the critical commentary on previous versions of this article provided by Charles Gerardo, MD, Mark L. Shapiro, MD, and Fletcher D. Srygley IV, MD, Duke University Medical Center. We appreciate the assistance of Kenneth Kelley, MD, and Zachary Soucy, MD, University of California Davis Medical Center, with ultrasound images. These individuals received no compensation for their assistance.
References
- 1.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57(14):1–134. [PubMed] [Google Scholar]
- 2.Isenhour JL, Marx J. Advances in abdominal trauma. Emerg Med Clin North Am. 2007;25(3):713–733. doi: 10.1016/j.emc.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 3.Fakhry SM, Brownstein M, Watts DD, Baker CC, Oller D. Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma. 2000;48(3):408–414. doi: 10.1097/00005373-200003000-00007. discussion 414–415. [DOI] [PubMed] [Google Scholar]
- 4.Jansen JO, Yule SR, Loudon MA. Investigation of blunt abdominal trauma. BMJ. 2008;336(7650):938–942. doi: 10.1136/bmj.39534.686192.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Niederee MJ, Byrnes MC, Helmer SD, Smith RS. Delay in diagnosis of hollow viscus injuries: effect on outcome. Am Surg. 2003;69(4):293–298. [PubMed] [Google Scholar]
- 6.Committee on Trauma ACoS. ATLS: Advanced Trauma Life Support Program for Doctors. 8th. Chicago, IL: American College of Surgeons; 2008. [Google Scholar]
- 7.Rodriguez A, DuPriest RW, Jr, Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims: a prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457–459. [PubMed] [Google Scholar]
- 8.Schurink GW, Bode PJ, van Luijt PA, van Vugt AB. The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury. 1997;28(4):261–265. doi: 10.1016/s0020-1383(97)00007-7. [DOI] [PubMed] [Google Scholar]
- 9.Hoff WS, Holevar M, Nagy KK, et al. Eastern Association for the Surgery of Trauma. Practice management guidelines for the evaluation of blunt abdominal trauma: the EAST practice management guidelines work group. J Trauma. 2002;53(3):602–615. doi: 10.1097/00005373-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 10.Linsenmaier U, Krötz M, Häuser H, et al. Whole-body computed tomography in polytrauma: techniques and management. Eur Radiol. 2002;12(7):1728–1740. doi: 10.1007/s00330-001-1225-x. [DOI] [PubMed] [Google Scholar]
- 11.Jhirad R, Boone D. Computed tomography for evaluating blunt abdominal trauma in the low-volume nondesignated trauma center: the procedure of choice? J Trauma. 1998;45(1):64–68. doi: 10.1097/00005373-199807000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Shuman WP, Ralls PW, Balfe DM, et al. Imaging of blunt abdominal trauma: American College of Radiology: ACR appropriateness criteria. Radiology. 2000;215(suppl):143–151. [PubMed] [Google Scholar]
- 13.Peitzman AB, Makaroun MS, Slasky BS, Ritter P. Prospective study of computed tomography in initial management of blunt abdominal trauma. J Trauma. 1986;26(7):585–592. doi: 10.1097/00005373-198607000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Holmes JF, McGahan JP, Wisner DH. Rate of intra-abdominal injury after a normal abdominal computed tomographic scan in adults with blunt trauma [published online ahead of print June 3, 2011] Am J Emerg Med. doi: 10.1016/j.ajem.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Heilbrun ME, Chew FS, Tansavatdi KR, Tooze JA. The role of negative CT of the abdomen and pelvis in the decision to admit adults from the emergency department after blunt trauma. J Am Coll Radiol. 2005;2(11):889–895. doi: 10.1016/j.jacr.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Jindal A, Velmahos GC, Rofougaran R. Computed tomography for evaluation of mild to moderate pediatric trauma: are we overusing it? World J Surg. 2002;26(1):13–16. doi: 10.1007/s00268-001-0174-5. [DOI] [PubMed] [Google Scholar]
- 17.Holmes JF, Wisner DH, McGahan JP, Mower WR, Kuppermann N. Clinical prediction rules for identifying adults at very low risk for intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2009;54(4):575–584. doi: 10.1016/j.annemergmed.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 18.Gardner RL, Sarkar U, Maselli JH, Gonzales R. Factors associated with longer ED lengths of stay. Am J Emerg Med. 2007;25(6):643–650. doi: 10.1016/j.ajem.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 19.Pannu N, Wiebe N, Tonelli M, Alberta Kidney Disease Network Prophylaxis strategies for contrast-induced nephropathy. JAMA. 2006;295(23):2765–2779. doi: 10.1001/jama.295.23.2765. [DOI] [PubMed] [Google Scholar]
- 20.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169(22):2078–2086. doi: 10.1001/archinternmed.2009.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 22.Eddy DM, Hasselblad V, Shachter RD. Meta-analysis by the Confidence Profile Method. Boston, MA: Academic Press; 1992. [Google Scholar]
- 23.Simel DL, Bossuyt PM. Differences between univariate and bivariate models for summarizing diagnostic accuracy may not be large. J Clin Epidemiol. 2009;62(12):1292–1300. doi: 10.1016/j.jclinepi.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 24.Borenstein MHL, Higgins JPT, Rothstein HR. Introduction to Meta-analysis. West Sussex, England: John Wiley & Sons; 2009. [Google Scholar]
- 25.Poletti PA, Mirvis SE, Shanmuganathan K, et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma. 2004;57(5):1072–1081. doi: 10.1097/01.ta.0000092680.73274.e1. [DOI] [PubMed] [Google Scholar]
- 26.Beck D, Marley R, Salvator A, Muakkassa F. Prospective study of the clinical predictors of a positive abdominal computed tomography in blunt trauma patients. J Trauma. 2004;57(2):296–300. doi: 10.1097/01.ta.0000130612.60661.c3. [DOI] [PubMed] [Google Scholar]
- 27.Chandler CF, Lane JS, Waxman KS. Seatbelt sign following blunt trauma is associated with increased incidence of abdominal injury. Am Surg. 1997;63(10):885–888. [PubMed] [Google Scholar]
- 28.Ferrera PC, Verdile VP, Bartfield JM, Snyder HS, Salluzzo RF. Injuries distracting from intra-abdominal injuries after blunt trauma. Am J Emerg Med. 1998;16(2):145–149. doi: 10.1016/s0735-6757(98)90032-8. [DOI] [PubMed] [Google Scholar]
- 29.Mofidi M, Hasani A, Kianmehr N. Determining the accuracy of base deficit in diagnosis of intra-abdominal injury in patients with blunt abdominal trauma. Am J Emerg Med. 2010;28(8):933–936. doi: 10.1016/j.ajem.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Richards JR, Derlet RW. Computed tomography for blunt abdominal trauma in the ED: a prospective study. Am J Emerg Med. 1998;16(4):338–342. doi: 10.1016/s0735-6757(98)90122-x. [DOI] [PubMed] [Google Scholar]
- 31.Sahdev P, Garramone RR, Jr, Schwartz RJ, Steelman SR, Jacobs LM. Evaluation of liver function tests in screening for intra-abdominal injuries. Ann Emerg Med. 1991;20(8):838–841. doi: 10.1016/s0196-0644(05)81422-2. [DOI] [PubMed] [Google Scholar]
- 32.Velmahos GC, Tatevossian R, Demetriades D. The “seat belt mark” sign: a call for increased vigilance among physicians treating victims of motor vehicle accidents. Am Surg. 1999;65(2):181–185. [PubMed] [Google Scholar]
- 33.Grieshop NA, Jacobson LE, Gomez GA, Thompson CT, Solotkin KC. Selective use of computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma. 1995;38(5):727–731. doi: 10.1097/00005373-199505000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Mackersie RC, Tiwary AD, Shackford SR, Hoyt DB. Intra-abdominal injury following blunt trauma: identifying the high-risk patient using objective risk factors. Arch Surg. 1989;124(7):809–813. doi: 10.1001/archsurg.1989.01410070063013. [DOI] [PubMed] [Google Scholar]
- 35.Richards JR, Derlet RW. Computed tomography and blunt abdominal injury: patient selection based on examination, haematocrit and haematuria. Injury. 1997;28(3):181–185. doi: 10.1016/s0020-1383(96)00187-8. [DOI] [PubMed] [Google Scholar]
- 36.Bode PJ, Edwards MJ, Kruit MC, van Vugt AB. Sonography in a clinical algorithm for early evaluation of 1671 patients with blunt abdominal trauma. AJR Am J Roentgenol. 1999;172(4):905–911. doi: 10.2214/ajr.172.4.10587119. [DOI] [PubMed] [Google Scholar]
- 37.Healey MA, Simons RK, Winchell RJ, et al. A prospective evaluation of abdominal ultrasound in blunt trauma: is it useful? J Trauma. 1996;40(6):875–883. doi: 10.1097/00005373-199606000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Kern SJ, Smith RS, Fry WR, Helmer SD, Reed JA, Chang FC. Sonographic examination of abdominal trauma by senior surgical residents. Am Surg. 1997;63(8):669–674. [PubMed] [Google Scholar]
- 39.Richards JR, Schleper NH, Woo BD, Bohnen PA, McGahan JP. Sonographic assessment of blunt abdominal trauma: a 4-year prospective study. J Clin Ultrasound. 2002;30(2):59–67. doi: 10.1002/jcu.10033. [DOI] [PubMed] [Google Scholar]
- 40.Rozycki GS, Ballard RB, Feliciano DV, Schmidt JA, Pennington SD. Surgeon-performed ultrasound for the assessment of truncal injuries: lessons learned from 1540 patients. Ann Surg. 1998;228(4):557–567. doi: 10.1097/00000658-199810000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boulanger BR, McLellan BA, Brenneman FD, et al. Emergent abdominal sonography as a screening test in a new diagnostic algorithm for blunt trauma. J Trauma. 1996;40(6):867–874. doi: 10.1097/00005373-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Boulanger BR, McLellan BA, Brenneman FD, Ochoa J, Kirkpatrick AW. Prospective evidence of the superiority of a sonography-based algorithm in the assessment of blunt abdominal injury. J Trauma. 1999;47(4):632–637. doi: 10.1097/00005373-199910000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Brenchley J, Walker A, Sloan JP, Hassan TB, Venables H. Evaluation of focussed assessment with sonography in trauma (FAST) by UK emergency physicians. Emerg Med J. 2006;23(6):446–448. doi: 10.1136/emj.2005.026864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brooks A, Davies B, Smethhurst M, Connolly J. Prospective evaluation of non-radiologist performed emergency abdominal ultrasound for haemoperitoneum. Emerg Med J. 2004;21(5):e5. doi: 10.1136/emj.2003.006932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goletti O, Ghiselli G, Lippolis PV, et al. The role of ultrasonography in blunt abdominal trauma: results in 250 consecutive cases. J Trauma. 1994;36(2):178–181. doi: 10.1097/00005373-199402000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Ma OJ, Gaddis G, Steele MT, Cowan D, Kaltenbronn K. Prospective analysis of the effect of physician experience with the FAST examination in reducing the use of CT scans. Emerg Med Australas. 2005;17(1):24–30. doi: 10.1111/j.1742-6723.2005.00681.x. [DOI] [PubMed] [Google Scholar]
- 47.McGahan JP, Rose J, Coates TL, Wisner DH, Newberry P. Use of ultrasonography in the patient with acute abdominal trauma. J Ultrasound Med. 1997;16(10):653–662. doi: 10.7863/jum.1997.16.10.653. [DOI] [PubMed] [Google Scholar]
- 48.McKenney M, Lentz K, Nunez D, et al. Can ultrasound replace diagnostic peritoneal lavage in the assessment of blunt trauma? J Trauma. 1994;37(3):439–441. doi: 10.1097/00005373-199409000-00018. [DOI] [PubMed] [Google Scholar]
- 49.Miller MT, Pasquale MD, Bromberg WJ, Wasser TE, Cox J. Not so FAST. J Trauma. 2003;54(1):52–59. doi: 10.1097/00005373-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 50.Poletti PA, Kinkel K, Vermeulen B, Irmay F, Unger P-F, Terrier F. Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology. 2003;227(1):95–103. doi: 10.1148/radiol.2271020139. [DOI] [PubMed] [Google Scholar]
- 51.Rose JS, Levitt MA, Porter J, et al. Does the presence of ultrasound really affect computed tomographic scan use? a prospective randomized trial of ultrasound in trauma. J Trauma. 2001;51(3):545–550. doi: 10.1097/00005373-200109000-00022. [DOI] [PubMed] [Google Scholar]
- 52.Röthlin MA, Näf R, Amgwerd M, Candinas D, Frick T, Trentz O. Ultrasound in blunt abdominal and thoracic trauma. J Trauma. 1993;34(4):488–495. doi: 10.1097/00005373-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 53.Rozycki GS, Ochsner MG, Schmidt JA, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma. 1995;39(3):492–498. doi: 10.1097/00005373-199509000-00016. [DOI] [PubMed] [Google Scholar]
- 54.Shackford SR, Rogers FB, Osler TM, Trabulsy ME, Clauss DW, Vane DW. Focused abdominal sonogram for trauma: the learning curve of nonradiologist clinicians in detecting hemoperitoneum. J Trauma. 1999;46(4):553–562. doi: 10.1097/00005373-199904000-00003. [DOI] [PubMed] [Google Scholar]
- 55.Soyuncu S, Cete Y, Bozan H, Kartal M, Akyol AJ. Accuracy of physical and ultrasonographic examinations by emergency physicians for the early diagnosis of intraabdominal haemorrhage in blunt abdominal trauma. Injury. 2007;38(5):564–569. doi: 10.1016/j.injury.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 56.Tso P, Rodriguez A, Cooper C, et al. Sonography in blunt abdominal trauma: a preliminary progress report. J Trauma. 1992;33(1):39–43. doi: 10.1097/00005373-199207000-00009. [DOI] [PubMed] [Google Scholar]
- 57.Stengel D, Bauwens K, Sehouli J, et al. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev. 2005;2:CD004446. doi: 10.1002/14651858.CD004446.pub2. [DOI] [PubMed] [Google Scholar]
- 58.Melniker LA, Leibner E, McKenney MG, Lopez P, Briggs WM, Mancuso CA. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: the first sonography outcomes assessment program trial. Ann Emerg Med. 2006;48(3):227–235. doi: 10.1016/j.annemergmed.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 59.Laupacis A, Sekar N, Stiell IG. Clinical prediction rules: a review and suggested modifications of methodological standards. JAMA. 1997;277(6):488–494. [PubMed] [Google Scholar]
- 60.McGinn TG, Guyatt GH, Wyer PC, Naylor CD, Stiell IG, Richardson WS, Evidence-based Medicine Working Group Users’ Guides to the Medical Literature, XXII: how to use articles about clinical decision rules. JAMA. 2000;284(1):79–84. doi: 10.1001/jama.284.1.79. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


