Abstract
Child maltreatment is a reliable predictor of post-traumatic stress disorder (PTSD) symptoms. However, not all maltreated children develop PTSD symptoms, suggesting that additional mediating variables explain how certain maltreated children develop PTSD symptoms when others do not. The current study tested three potential mediators of the relationship between child maltreatment and subsequent PTSD symptoms: 1) respiratory sinus arrhythmia reactivity, 2) cortisol reactivity, and 3) experiential avoidance, or the unwillingness to experience painful private events such as thoughts and memories. Maltreated (n = 51) and non-maltreated groups (n = 59) completed a stressor paradigm, a measure of experiential avoidance, and a semi-structured interview of PTSD symptoms. One year later, participants were re-administered the PTSD symptoms interview. Results of a multiple mediator model showed the set of potential mediators mediated the relationship between child maltreatment and subsequent PTSD symptoms. However, experiential avoidance was the only significant specific indirect effect, demonstrating that maltreated children avoiding painful private events after the abuse were more likely to develop a range of PTSD symptoms one year later. These results highlight the importance of experiential avoidance in the development of PTSD symptoms for maltreated children and implications for secondary prevention and clinical intervention models are discussed.
Keywords: Child maltreatment, Respiratory sinus arrhythmia, Cortisol, Experiential avoidance, Posttraumatic stress disorder
Posttraumatic stress disorder (PTSD) is a debilitating condition that can result after a child is exposed to an environmental event involving actual or threatened death, injury or harm to one’s physical integrity (American Psychiatric Association, 2000). Up to 82% of children will experience at least one such event before adulthood (Breslau, Wilcox, Storr, Lucia, & Anthony, 2004; Cuffe et al., 1998; Giaconia et al., 1995), resulting in a PTSD prevalence rate of 5% in the general child population (Merikangas et al., 2010). Rates of PTSD vary however depending on the type of event to which children are exposed. Child maltreatment, including physical abuse, sexual abuse and neglect, affects 700,000 children under the age of eighteen each year in the United States (U.S. Department of Health and Human Services, 2010) and increases the risk for a number of adverse developmental outcomes, including low educational achievement (Lansford et al., 2002; Perez & Widom, 1994), sexually transmitted infections (Hillis, Anda, Felitti, Nordenberg, & Marchbanks, 2000), teenage pregnancy (Noll, Shenk, & Putnam, 2009), and obesity (Bentley & Widom, 2009). Child maltreatment is also one of the most reliable predictors of PTSD symptoms (Copeland, Keeler, Angold, & Costello, 2007; De Bellis, Hooper, Woolley, & Shenk, 2010; Tolin & Foa, 2006) with maltreated children 5–10 times more likely to meet full PTSD diagnostic criteria as young adults than non-maltreated, psychiatric controls (Scott, Smith, & Ellis, 2010). PTSD prevalence estimates range between 30–37% in adults with a documented history of child maltreatment (Widom, 1999), considerably higher than the 7% estimate found in the general adult population (Kessler et al., 2005). Thus, child maltreatment poses an increased risk for PTSD and PTSD symptoms throughout the lifespan, resulting in significantly higher medical costs even when compared to more prevalent psychiatric conditions, including all other anxiety disorders (Marciniak et al., 2005) and major depressive disorder (Ivanova et al., 2011).
While the risk that child maltreatment poses for subsequent PTSD symptoms is clear, not all maltreated children develop PTSD symptoms (Collishaw et al., 2007), suggesting that additional, mediating variables explain how some maltreated children go on to develop PTSD symptoms when others do not. Researchers have examined both psychological and neurobiological processes related to child maltreatment and PTSD symptoms to identify such mediating variables. Psychological processes are mediational pathways explaining how an event, such as child maltreatment, leads to an increased risk for a particular outcome, such as PTSD symptoms. Experiential avoidance is one such process and has gained considerable attention recently as it is related to a number of adverse psychological outcomes (Aldao, Nolen-Hoeksema, & Schweizer, 2010). Experiential avoidance is an unwillingness to experience painful or aversive private events, such as unwanted thoughts, emotions, memories, and physiology, with attempts to control, suppress or inhibit the form or frequency of these private events and the contexts that occasion them (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996). Child maltreatment, like other forms of trauma, can prompt painful private events, such as reoccurring images or recollections of the event, heightened physiological reactivity, and increased fear and anxiety. These events may generate attempts to alter, suppress or otherwise control specific private events so that the aversiveness of the experience can be reduced. This can establish the use of avoidance strategies, a key symptom cluster of PTSD, while actually maintaining or increasing other PTSD symptoms (Cameron, Palm, & Follette, 2010; Rosenthal, Cheavens, Lynch, & Follette, 2006).
Previous research has demonstrated that child maltreatment is related to higher levels of experiential avoidance (Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007; Sullivan, Meese, Swan, Mazure, & Snow, 2005) with higher levels of experiential avoidance predicting the development of PTSD symptoms above and beyond initial symptom severity (Plumb, Orsillo, & Luterek, 2004). Experiential avoidance has also demonstrated mediation of child maltreatment and several global measures of adult psychiatric distress (Marx & Sloan, 2002; Polusny, Rosenthal, Aban, & Follette, 2004). Experiential avoidance may even play a mediational role in PTSD symptom development for maltreated children (Shenk, Putnam, & Noll, 2012) and explain how some of these individuals develop subsequent PTSD symptoms when others do not. Such research would guide prevention and intervention strategies toward more effective targeting of psychological processes influencing PTSD symptom development.
Child maltreatment also affects multiple neurobiological processes that recent theory outlines as potential mediators of the relationship between child maltreatment and subsequent PTSD symptoms. For instance, allostatic load (McEwen & Wingfield, 2003) specifies that severe or chronic stress, such as child maltreatment, affects multiple, inter-related stress mediating systems, such as the endocrine and autonomic systems, that increase the probability of adverse psychological development (Juster et al., 2011). The respiratory sinus arrhythmia (RSA) is an estimate of parasympathetic control over cardiac activity and is an example of one such stress-mediating pathway, as it responsible for facilitating and regulating sympathetic activity during and after environmental challenge (Porges, 2003). Child maltreatment can limit the protective effects of RSA by reducing estimates observed in adolescent females at rest (Miskovic, Schmidt, Georgiades, Boyle, & MacMillan, 2009) as well as in adult females during challenge (Dale et al., 2009). Reduced RSA estimates at rest and greater reductions during challenge are predictive of poor psychological outcomes in children due to an under-regulation of sympathetic activity (Beauchaine, Gatzke-Kopp, & Mead, 2007). Reduced RSA can therefore promote hyper-aroused physiological states, a key symptom cluster of PTSD, and research with adults has found reduced RSA estimates at rest for those with PTSD (Blechert, Michael, Grossman, Lajtman, & Wilhelm, 2007; Hopper, Spinazzola, Simpson, & van der Kolk, 2006). Similar research with adults has found that stress paradigms elicit stronger reductions in RSA estimates for those with PTSD symptoms (Keary, Hughes, & Palmieri, 2009; Sack, Hopper, & Lamprecht, 2004). Thus, existing theory and research posit that disruptions in RSA, specifically reduced influence over sympathetic activity, may serve as a potential biological pathway explaining how child maltreatment promotes the risk of subsequent PTSD symptom development.
The hypothalamus-pituitary-adrenal (HPA) axis is another stress-mediating system responsible for promoting and resolving the biological response to environmental challenges (Chrousos & Gold, 1992). Disruptions in cortisol profiles, an index of HPA axis activity, are linked to several subsequent psychological and health outcomes (Miller, Chen, & Zhou, 2007). Both hyper- and hypocortisolism profiles have been observed in maltreated samples at rest (Cicchetti & Rogosch, 2001; King, Mandansky, King, Fletcher, & Brewer, 2001) and during chemical or laboratory stress paradigms (Carpenter et al., 2007; Hart, Gunnar, & Cicchetti, 1995; Heim et al., 2000). Each of these cortisol profiles observed during rest and challenge are related to current and subsequent PTSD symptoms (Bremner, Vermetten, & Kelley, 2007; Carrion et al., 2002; Lemieux & Coe, 1995; Santa Ana et al., 2006; Yehuda, 2001). Although identifying a specific cortisol profile related to PTSD in maltreated samples has been difficult, due in part to changes in HPA axis activity observed across development (Trickett, Noll, Susman, Shenk, & Putnam, 2010), atypical cortisol profiles such as hyper- and hypocortisol responses are consistently linked to both child maltreatment and PTSD symptoms. Such research suggests that cortisol may serve as a potential mediating pathway between exposure to child maltreatment and subsequent PTSD symptom development. However, cortisol concentrations vary according to a diurnal pattern (Kiess et al., 1995), and recent maltreatment is more strongly associated with PTSD symptoms (Kendall-Tackett, Williams, & Finkelhor, 1993). Accounting for these factors can strengthen inferences made about the role of cortisol as a potential mediator of PTSD symptoms in maltreated children (Shea, Walsh, Macmillan, & Steiner, 2005).
Formal mediational tests of the specific indirect effects of RSA and cortisol activity are lacking and represent an important area for future research. Moreover, a multiple levels of analysis approach (Cicchetti & Blender, 2004; Cicchetti & Dawson, 2002), where researchers incorporate knowledge from various sub-disciplines and examine several psychological and neurobiological processes simultaneously, is needed to truly advance a developmental psychopathology perspective on the identification of potential mediators of the relationship between child maltreatment and PTSD symptoms. Child maltreatment is an environmental event that affects multiple risk processes that also co-occur (Dale et al., 2009; Gordis, Granger, Susman, & Trickett, 2008). This co-occurrence can exert an additive risk impact where multiple processes affected by child maltreatment each contribute to the increased probability of adverse development, such as PTSD symptoms. Testing several potential mediators simultaneously within a multiple levels of analysis framework can therefore assess the cumulative effect of child maltreatment on several risk processes while minimizing the risk of attributing mediational status to a single process when other relevant processes are omitted from the analysis. A simultaneous test of multiple risk processes also allows each individual mediator to compete for variance in a specified outcome, leading to more rapid and effective identification of the putative mediational processes responsible for the development of PTSD symptoms in maltreated populations. A final important advantage of this approach is that results have direct clinical utility for prevention and intervention programs. Identifying one or more mediators prioritizes clinical resources toward those processes most influential in increasing the risk of subsequent PTSD symptoms. Clinical interventions that directly alter risk processes can then be delivered following an instance of maltreatment or after PTSD symptoms emerge.
Adopting a multiple levels of analysis approach, the current study simultaneously tested the indirect effects of experiential avoidance, RSA, and cortisol in mediating the relationship between child maltreatment and subsequent PTSD symptoms using a sample of maltreated and non-maltreated adolescents. Two primary hypotheses were tested. One, the set of potential mediators would mediate the relationship between child maltreatment and subsequent PTSD symptoms after controlling for relevant covariates and baseline estimates. This hypothesis tests the additive risk impact of experiential avoidance, RSA, and cortisol when testing mediation of the relationship between child maltreatment and PTSD symptoms. Two, experiential avoidance, RSA reactivity, and cortisol reactivity would each constitute a significant indirect effect of the relationship between child maltreatment and PTSD symptoms when simultaneously estimating the other risk processes. This hypothesis will identify the most potent specific indirect effects contributing to PTSD symptoms, thereby informing prevention and intervention programs serving children who have been maltreated.
Method
Sample
One hundred ten adolescent females between the ages of 14–19 years of age participated in this study. A sample of adolescent females was selected as older children experiencing trauma are most likely to develop PTSD symptoms (Copeland et al., 2007) with females more likely to experience different forms of child abuse (U.S. Department of Health and Human Services, 2010) and more likely to develop PTSD symptoms (Breslau et al., 2004). Two distinct groups of adolescent females participated. A child maltreatment group (n = 51) was recruited from Child Protective Service (CPS) agencies investigating allegations of physical neglect or contact physical or sexual abuse. With the assistance of CPS caseworkers, a consecutive referral process identified families who had a child with a substantiated case of maltreatment and who were willing to be contacted by research staff about participation in the study. A non-maltreated, comparison group (n = 59) was recruited using posted flyers in a primary care outpatient clinic servicing the general medical complaints of at-risk, adolescent females. This outpatient clinic was chosen as a recruitment site over alternative venues as it serves a population with a similar demographic profile as those in the maltreated group. At the time of entry into the study, the mean age of the total sample was 17.00 years (SD=1.17; Age range = 14–19 years), 58% of the adolescents were from single-caregiver homes, the median family income level was $40,000–$49,000, and the sample was 42% Caucasian, 51% African-American, 1% Hispanic and 6% Multi-racial. Demographic information is presented by group membership in Table 1.
Table 1.
Demographic information for maltreated and comparison groups at study entry.
| Variable | Maltreated M (SD) or n |
Comparison M (SD) or n |
|---|---|---|
| Age | 16.78 (1.12) | 17.19 (1.20) |
| Race | ||
| African-American | 24 | 32 |
| Caucasian | 24 | 22 |
| Hispanic | 0 | 1 |
| Multi-racial | 3 | 3 |
| Income | ||
| Under $10,000 | 14 | 14 |
| $10,000 – $19,999 | 8 | 6 |
| $20,000 – $29,999 | 9 | 9 |
| $30,000 – $39,999 | 5 | 10 |
| $40,000 – $49,999 | 4 | 6 |
| $50,000 – $59,999 | 1 | 3 |
| $60,000 – $69,999 | 3 | 3 |
| $70,000 – $79,999 | 4 | 2 |
| $80,000 – $89,999 | 2 | 2 |
| $90,000 – $99,999 | 0 | 1 |
| >$100,000 | 0 | 2 |
| Family Environment | ||
| Single-caregiver home | 26 | 33 |
| Dual-caregiver home | 20 | 23 |
Procedure
All study procedures were approved by the local Institutional Review Board prior to data collection. Causal inferences about the effects of potential mediators assessed in observational research are strengthened when there is proper temporal ordering of events that follow a logical or theoretical pathway (Maxwell & Cole, 2007; Preacher & Hayes, 2008). As such, adolescent females who experienced substantiated child maltreatment prior to study entry and a non-maltreated comparison group were recruited to participate in an assessment of potential mediators of PTSD symptoms. This same cohort was then followed one-year later to re-assess PTSD symptoms and determine whether the set of potential mediators, as well as individual mediators, exerted a significant indirect effect on subsequent PTSD symptoms. To illustrate the actual temporal relationships among the predictor, the set of potential mediators, and outcome variable assessed in this study, child maltreatment is presented as Time 1, the assessment of mediators as Time 2, and the subsequent PTSD assessment as Time 3.
Determination of Child Maltreatment (Time 1)
Child maltreatment was determined by a CPS investigation that resulted in a substantiated/indicated designation of child maltreatment. All substantiated/indicated designations of child maltreatment were made prior to the onset of this study and individual case records were reviewed and screened for eligibility and recruitment purposes. Participants in the maltreated group were required to have had a substantiated/indicated designation of maltreatment within the twelve months prior to study participation. Of the 51 participants in the maltreatment group, 49% experienced sexual abuse, 45% experienced physical abuse, and 16% experienced physical neglect with 10% experiencing more than one form of abuse. Comparison females were screened and excluded if they had a substantiated case of child maltreatment within the twelve months prior to study participation.
Assessment of Potential Mediators (Time 2)
All appointments were scheduled between 11 a.m. and 5 p.m. Participants completed a general interview about current health habits, self-report questionnaires, a semi-structured interview assessing PTSD symptoms, and a stressor paradigm measuring physiological reactivity. The stressor paradigm involved participants first completing a five-minute resting condition where each participant sat comfortably in a chair while listening to soft music and watching slow-moving images on a computer screen. Participants then completed a combined stressor task to elicit reactivity across different physiological systems. A combined performance and interpersonal stressor was chosen given varying autonomic and HPA axis responses to different stressor types (Stroud et al., 2009). The performance aspect of the stressor paradigm involved each participant completing a series of affect recognition tasks (Porges, Cohn, Bal, & Lamb, 2007). Participant responses were timed and each participant was asked to identify the emotion as quickly as they could while not making any mistakes before the time elapsed. The average length of time to complete the affect recognition tasks was 7.45 minutes (SD = 1.19). The interpersonal stressor involved participants viewing a series of video-clips of parent-adolescent conflict. The time required to view all videos was 8 minutes.
Assessment of Subsequent PTSD Symptoms (Time 3)
Study participants were re-contacted one-year later to complete the same semi-structured interview assessing PTSD symptoms completed at Time 2. Five percent (n = 6) of the original sample was unable to complete the subsequent PTSD symptoms assessment, indicating a 95% retention rate throughout the course of the study.
Measures
General demographics and health habits form
Demographic information was assessed via self- and caregiver-report and included age, race, family income and family constellation (single-caregiver vs. dual-caregiver homes). Health habits were assessed at Time 2 to determine their potential influence on RSA and HPA axis reactivity. Specific health habits assessed were: pregnancy status, use of steroids (topical, oral and inhaled), cigarettes, over-the counter (aspirin, ibuprofen) and prescription drugs (psychotropic, seasonal allergies, oral contraceptive), whether participants ate anything one hour prior to their appointment, and whether participants exercised or drank caffeine on the day of their appointment.
RSA
Inter-beat intervals (IBI’s), the time measured in milliseconds between heart contractions, were recorded via electrocardiogram (ECG) using disposable Ag/AgCl electrodes placed on the chest and abdomen of each participant. IBI’s were detected in real-time using a QRS peak detection algorithm applied to the ECG data and stored on the Biolog 3991x/2-EIR system manufactured by UFI Inc. IBI’s were subsequently transferred to a computer via USB for later inspection. CardioEdit and CardioBatch software (Brain-Body Center, University of Illinois at Chicago) were used to visually inspect and edit IBI streams for artifacts. Editing consisted of integer arithmetic such as dividing intervals when detections are missed or adding intervals when spuriously invalid detections occur. After editing of IBI data streams, the amplitude of RSA was calculated by summing the variances of heart rate activity across the band of frequencies associated with spontaneous respiration during adolescence and young adulthood. The natural logarithm of the extracted variance for each successive 30-second epoch was calculated as the measure of the amplitude of RSA. The average across epochs within the resting, RSARest, and stressor conditions, RSAStress was used to characterize individual differences in RSA. These procedures are statistically equivalent to frequency domain methods (e.g. spectral analysis) for the calculation of the amplitude of RSA when heart period data are stationary (Porges & Byrne, 1992). Reliable ECG recordings were not obtained on three participants and therefore could not be used in data analysis. A manipulation check was performed to assess if the stressor paradigm significantly changed values of RSA from resting to stressor conditions. A paired samples t-test indicated that RSA estimates declined significantly from the resting to stressor condition, t(105) = −3.52, p < .001.
Cortisol
Cortisol reactivity was assessed across five samples collected at strategic times to detect resting and stress responses. Each participant was instructed not to eat or drink one hour prior to participation. Upon arrival, each participant was asked to swish their mouth with water prior to beginning their appointment. The first sample, CortisolRest, was collected approximately 25 minutes (M = 25.30, SD = .24) after participants began their study appointment to give them time to acclimate to the research environment and procedures. Samples two through five were collected 5-, 10-, 20- and 30-minutes post stressor to detect the maximum cortisol response to the combined stressor, CortisolStress. Saliva was obtained through passive drooling into 20 mL polypropylene vials and stored at −80°C until assayed. Samples were assayed in duplicate using a highly-sensitive enzyme immunoassay from Salimetrics. The test has a lower limit sensitivity of <.003 μg/dl and average intra-and inter-assay coefficients of variation 3.35% – 3.65% and 3.75% – 6.41%, respectively. A manipulation check was performed to assess if cortisol concentrations changed significantly from resting to stressor conditions. A paired samples t-test indicated that cortisol concentrations, on average, did not change significantly from the resting to the stressor condition for the total sample, t(108) = .71, p = .48.
Acceptance and Action Questionnaire (AAQ; Hayes et al., 2004)
Experiential avoidance was measured using the 22-item version of the AAQ. Items are rated on a 7-point Likert scale ranging from “Never True” to “Always True” with higher scores representing higher levels of experiential avoidance. Example items include, “Anxiety is bad”, “I try hard to suppress thoughts and feelings that I don’t like by just not thinking about them” and “I’m not afraid of my feelings” (reverse scored). The AAQ has demonstrated reliability (α = .70 – .79) and convergent validity with measures of anxiety (r = .59, p < .01), depression (r = .75, p < .01) and child trauma (r = .18, p < .01). The reliability of the AAQ at Time 2 was α = .72.
PTSD symptoms
The Comprehensive Trauma Interview (CTI; Barnes, Noll, Putnam, & Trickett, 2009) is a semi-structured interview assessing a wide variety of information following an instance of child maltreatment. The CTI has demonstrated good inter-rater reliability with information collected from CPS investigations (κ =.70 – .87). The CTI has a specific section devoted to the assessment of PTSD symptoms across each symptom domain (re-experiencing, avoidance and hyperarousal) outlined in the Diagnostic and Statistical Manual of Mental Disorders-IV-Text Revision (American Psychiatric Association, 2000). Examples of questions are: “Have you ever had painful images, memories or thoughts of what happened?”, “Have you ever avoided doing things or getting into situations that reminded you of what happened?”, and “Have you ever been jumpy, on edge, or easily startled because of what happened?” Responses to questions are coded (0= No, 1=Yes) with composite scores generated for each PTSD symptom domain as well as total PTSD symptoms. Reliability of the total PTSD symptoms composite score used in statistical analysis was α = .89 at Time 2 and α = .91 at Time 3.
Data Analytic Strategy
A multiple mediator model was employed to identify the total and specific indirect effects of RSAStress, CortisolStress and AAQ scores when explaining the relationship between child maltreatment and subsequent PTSD symptoms. The multiple mediator model was performed with Mplus v.6 (Muthén & Muthén, 1998–2010) using the maximum likelihood estimator to account for missing data. This method of testing mediation is particularly useful in the current study because it tests the indirect effects of each mediator simultaneously and through its use of bootstrapping. Bootstrapping is a non-parametric, re-sampling procedure for estimating the standard errors of indirect effects and their corresponding confidence intervals with optimal accuracy (MacKinnon, Lockwood, & Williams, 2004). By randomly sampling from n observations and estimating indirect effects k times with replacement of observations, estimates of the total and specific indirect effects, their standard errors and confidence intervals can be obtained. There is also the opportunity to enter variables into the multiple mediator model as statistical covariates. Results of the current multiple mediator model are based on k = 5000 bootstrap samples with bias-corrected, 95% confidence intervals (BC 95% CI).
Results
Data Screening
Participants who reported being pregnant (n = 6) were excluded from statistical analyses. Chi-square and serial analysis of variance (ANOVA) tests were used to evaluate differences between maltreatment and comparison groups on demographic, health and study-related variables at Time 2. Results indicated significant between-group differences on the use of prescribed steroid medication (Steroid use = 1; No steroid use = 0), χ2(1) = 5.27, p = .02, OR = 5.64, 95% CI: 1.14 – 28.02, and cigarette use (Cigarette use = 1; No cigarette use = 0), χ2(1) = 7.81, p = .01, OR = 5.07, 95% CI: 1.53 – 16.82, with the maltreated group using steroid medication and cigarettes more often than the comparison group. There were no significant differences between groups on race, income, family constellation, medication use (prescription, over-the-counter), the use of caffeine prior to the study, whether participants exercised on the day of their appointment or ate in the hour prior to the study (p’s = .11 – .81). The ANOVAs indicated that the maltreated group was marginally younger, F(1, 102) = 3.37, p = .07, η2 = .03, had significantly higher AAQ scores, F(1, 102) = 5.99, p = .02, η2 = .06, and had more PTSD symptoms at both the Time 2, F(1, 102) = 15.19, p < .001, η2 = .13, and Time 3 assessment, F(1, 96) = 16.06, p < .001, η2 = .14. There were no significant group differences on the time of day the first cortisol sample was collected, RSARest, RSAStress, CortisolRest, or CortisolStress, (p’s = .12 – .41).
Cortisol concentrations continue to decline throughout the afternoon and into the evening hours (Kiess et al., 1995). As such, the relationship between the time the first cortisol sample was collected and the observed cortisol concentrations was examined. Although there was no significant difference between the maltreated and comparison groups as to the time of day when the first cortisol sample was obtained, the time of day when cortisol was first collected was systematically related to observed cortisol concentrations, r = −.22, p = .02. This result indicated that samples collected later in the day had cortisol concentrations that were lower than samples collected earlier in the day. Because age, steroid use, and cigarette use were either marginally or significantly different between groups at Time 2, and because the time of day in which the first cortisol sample was collected was systematically related to observed cortisol concentrations, each of these variables were used as covariates in subsequent statistical analyses.
A partial correlation matrix, controlling for age, steroid use, cigarette use and the time of day that the first cortisol sample was collected, was then estimated to assess the relationships among variables to be included in the multiple mediator model (see Table 2). While the manipulation check for cortisol indicated that cortisol values did not change significantly from resting to stressor conditions for the entire sample, the partial correlation matrix revealed that the maltreated group exhibited significantly lower concentrations of cortisol, or a hypocortisol profile, during the stressor condition once age, steroid use, cigarette use and time of day that the first cortisol sample was collected were controlled. The relationships between experiential avoidance and each PTSD symptom domain at Time 3 were then estimated to ensure that experiential avoidance was not highly correlated with any one domain, specifically the avoidance domain. Results indicated that AAQ scores were moderately correlated with all three PTSD symptom domains: re-experiencing, r = .25, p = .01; avoidance, r = .34, p < .001, and hyperarousal, r = .34, p < .001; however, there were no significant differences in the strengths of the relationships among symptom domains.
Table 2.
Partial correlation matrix for variables used in the multiple mediator analysis.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Maltreatment | - | ||||||
| 2. RSARest | .17 | - | |||||
| 3. RSAStress | .15 | .88*** | - | ||||
| 4. CortisolRest | −.14 | −.07 | −.05 | - | |||
| 5. CortisolStress | −.21* | −.08 | −.11 | .70*** | - | ||
| 6. AAQ | .29** | −.02 | .03 | −.12 | −.10 | - | |
| 7. PTSD | .39*** | −.03 | .01 | −.07 | −.05 | .34*** | - |
Note:
p ≤ .001;
p ≤ .01;
p ≤ .05.
Age, steroid use, cigarette use and sampling time were controlled in matrix. Maltreatment coded as: 0 = Comparison, 1 = Maltreated; RSARest = RSA assessed during rest; RSAStress = RSA assessed during stressor; CortisolRest = Cortisol assessed during rest; CortisolStress = Cortisol assessed during stress; AAQ = Acceptance and Action Questionnaire; PTSD = Post-traumatic stress disorder symptoms at Time 3.
Multiple Mediator Analysis1
Hypothesis 1: The set of potential mediators would mediate the relationship between child maltreatment and subsequent PTSD symptoms
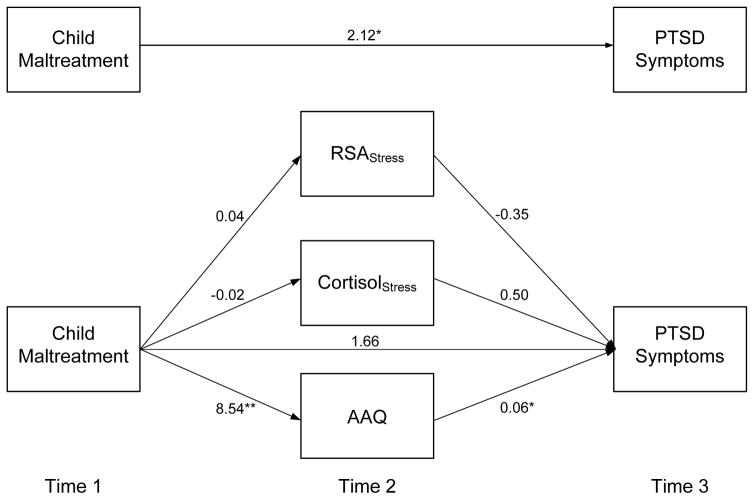
CortisolRest, RSARest, and Time 2 PTSD symptoms were added to the list of covariates that included age, steroid use, cigarette use, and the time of day when the first cortisol sample was collected. All directional and non-directional relationships between the predictor, list of covariates, set of mediators and the outcome were estimated and freely correlated in the model. Model fit indices indicated that the overall multiple mediator model provided a good fit to the observed data, χ2(9) = 11.75, p = .23; Comparative Fit Index = .99; Root Mean Square Error of Approximation = .05; Standardized Root Mean Square Residual = .03. The total indirect effect, or the sum of each specific indirect effect tested in the multiple mediator model, was significantly different from zero, Point Estimate = .46, BC 95% CI = .06–1.21, indicating that the set of proposed variables mediated the relationship between child maltreatment and PTSD symptoms. As seen in Figure 1, the total effect for child maltreatment on PTSD symptoms was significant, b = 2.12, p = .03; however the direct effect, when the set of mediators were estimated in the model, was non-significant, b = 1.66, p = .09, providing further evidence of a mediation effect.
Figure 1.
Results of the multiple mediator model.
Note: ** = p ≤ .001; * = p ≤ .05.
Hypothesis 2: Experiential avoidance, RSA reactivity, and cortisol reactivity would each constitute a significant indirect effect of the relationship between child maltreatment and PTSD symptoms
The specific indirect effects of each proposed mediator were then examined to determine which proposed mediator or mediators contributed to the overall mediation effect. Results demonstrated that the confidence interval around the point estimate for the specific indirect effect of the AAQ did not include zero, indicating that the AAQ contributed significantly to the mediation effect when simultaneously estimating the contributions of RSAStress and CortisolStress, Point Estimate = .49, BC 95% CI = .11–1.20. The proportion of the total effect accounted for by the AAQ is .49/2.12 = .23, indicating that the AAQ accounted for 23% of the total effect of child maltreatment on subsequent PTSD symptoms (MacKinnon, 2008). The unstandardized parameter estimates reported in Figure 1 indicated that child maltreatment was significantly related to higher levels of experiential avoidance with higher levels of experiential avoidance significantly related to more, subsequent PTSD symptoms. The specific indirect effects for RSAStress or CortisolStress, as well as the unstandardized parameter estimates for each path, were not significantly different from zero and therefore did not contribute significantly to the mediation effect.
Pairwise contrasts comparing the strength of each specific indirect effect relative to another indirect effect in the model were estimated for each proposed mediator. Results demonstrated that the BC 95% CI around the contrast comparing the indirect effects for AAQ vs. RSAStress did not contain zero, Point Estimate = .50, BC 95% CI = .09–1.23, indicating that the indirect effect for AAQ was significantly stronger in comparison to RSAStress. The indirect effect for AAQ was also significantly stronger when compared to the indirect effect of CortisolStress, Point Estimate = .49, BC 95% CI = .08–1.21. There was no significant difference between the indirect effects of RSAStress and CortisolStress.
Discussion
Several limitations should be considered before interpreting the results of this study. First, mediational modeling was used to examine the contributions of several variables in a single statistical model to identify pathways to PTSD symptom development for maltreated children. While these variables have both theoretical and empirical relevance for child maltreatment and PTSD symptom development, additional mediators almost certainly exist yet were not tested in this study. Experiential avoidance accounted for a significant proportion of the variance in subsequent PTSD symptoms yet a large amount of variance remains unexplained. Alternative models testing experiential avoidance with other potential mediators, such as quality of parenting and interpersonal relationships (Collishaw et al., 2007), hold considerable promise in future research. Second, the effects of child maltreatment in this sample are limited to those with a substantiated case of maltreatment. Substantiated cases of maltreatment can exert stronger effects on PTSD symptoms when compared to self-report measures of child maltreatment (Scott et al., 2010). Thus, results cannot necessarily generalize to other methods assessing child maltreatment. Similarly, the comparison group was screened for substantiated maltreatment occurring in the twelve months prior to study entry. It is possible that the comparison condition experienced maltreatment at some point in their lifetime prior to the year before study entry, thereby potentially limiting the fidelity of the comparison group. Third, the sample for this study consists entirely of females with the maltreated group experiencing higher rates of sexual abuse than the general maltreatment population. This study targeted females specifically to identify mediators of PTSD symptom development in the subpopulation of maltreated children at greatest risk for PTSD. Thus, it is not unusual that a higher rate of sexual abuse was observed in this study, as females are more likely to be sexually abused when compared to males (Sedlak et al., 2010). It is important to emphasize that the findings of this study therefore only generalize to the adolescent female subpopulation and the extent to which the current results generalize to maltreated males or the larger maltreatment population can only be determined by future research. Fourth, severity of maltreatment was not assessed in this study. More severe types or cases of maltreatment may increase active attempts to avoid painful private experiences. Examining the relationship between maltreatment severity and varying levels of experiential avoidance is an important area of future research. Finally, timing within the menstrual cycle was not assessed yet can influence hormone concentrations, particularly cortisol. Future research should assess and control the effect of menstrual cycle timing on cortisol concentrations.
Despite these limitations, the results of this study are based on a strong, longitudinal test of several potential mediators of the relationship between child maltreatment and PTSD symptoms. The set of mediators was identified using a multiple levels of analysis approach that integrated prior theoretical and empirical findings from several scientific sub-disciplines (e.g. autonomic, endocrine, psychological) to advance a more complete developmental psychopathology perspective of the relationship between child maltreatment and PTSD symptoms. The results supported the mediational effect of experiential avoidance when simultaneously estimating the indirect effects of two neurobiological processes responsible for managing environmental demands. This suggests that the more maltreated participants avoided painful thoughts, emotions, memories, and physiology, the more PTSD symptoms they reported one year later. In addition, these results were estimated while accounting for the effects of several important covariates, including prior levels of PTSD symptoms. The effect for experiential avoidance was uniform across PTSD symptom clusters, demonstrating that it is related to moderate increases in re-experiencing, hyperarousal, and avoidance symptoms. These results suggest that experiential avoidance following child maltreatment plays an important role in the development of PTSD symptoms. These results also suggest that maltreated children who did not use strategies to avoid painful private events, or who engaged in experiencing private events with awareness and acceptance, were more resilient to abuse and less likely to develop PTSD symptoms. Together, these findings offer an alternative interpretation of the role private events play in the development of PTSD symptoms. For instance, etiological models of PTSD (Ehlers & Clark, 2000) assign a primary role to the presence and influence of negative cognitions or appraisals following a traumatic event. However, the presence of these private events may be a less important aspect to consider when explaining how PTSD symptoms develop. It may be more useful to assess and understand how maltreated children are relating to such private events, including but not limited to negative cognitions and appraisals, as opposed to their mere presence. This study provides evidence that relating to private events with either acceptance or avoidance, not simply the presence of these events, can have a significant, differential impact on the development of PTSD symptoms.
Contrary to expectations, cortisol and RSA reactivity did not exert significant indirect effects. One explanation for this may come from longitudinal research showing that women who were sexually abused have higher resting cortisol concentrations during childhood, comparable estimates to non-sexually abused peers during adolescence, and significantly lower concentrations in adulthood (Trickett et al., 2010). Thus, an adjustment of the HPA axis may be occurring in maltreated samples across development with profiles assessed in younger and older developmental stages tied more strongly to PTSD symptoms. Like cortisol, there is variation in findings reported across studies examining the relationship between RSA and PTSD using adult (Sahar, Shalev, & Porges, 2001) and child samples (Scheeringa, Zeanah, Myers, & Putnam, 2004). Thus, there may be a similar adjustment in RSA control during adolescence that prevents detection of a relationship between child maltreatment and PTSD symptoms.
Another explanation may be that the stressor used in this study had mixed effects in achieving levels of reactivity, particularly for cortisol. RSA reactivity did change significantly from resting to stressor conditions while cortisol reactivity did not. However, the maltreated group did display a hypocortisol reaction during the stressor condition once relevant demographic variables and health-related behaviors were controlled. This finding is consistent with previous research showing a relationship between child maltreatment and hypocortisol reactions during stress paradigms (Hart et al., 1995). Thus, the stressor did elicit a cortisol stress profile consistent with prior research, thereby providing an adequate test of its relationship with subsequent PTSD symptoms. While there is support for a relationship between hypocortisolism in adults with PTSD (Yehuda, 2001), this relationship is not always found in samples of adolescent females exposed to child maltreatment (MacMillan et al., 2009). This study adds to this literature with adolescents and suggests that RSA and cortisol reactivity may not be as strong as other indicators for maltreated adolescents when evaluating the putative mediators for subsequent PTSD symptoms. Several studies have shown that RSA and cortisol moderate several psychological outcomes in children experiencing maltreatment (Gordis, Feres, Olezeski, Rabkin, & Trickett, 2010; Gordis, Granger, Susman, & Trickett, 2006) or inter-parental conflict (El-Sheikh, Harger, & Whitson, 2001; El-Sheikh & Whitson, 2006). Thus, it may be more appropriate for future research to consider RSA and cortisol reactivity as moderators of the relationship between child maltreatment and subsequent psychological outcomes and not as mediators of this relationship.
There are specific, clinically-relevant implications for prevention and intervention of PTSD symptoms within maltreated populations based on these results. For instance, secondary prevention programs can incorporate a focus on disrupting experiential avoidance as part of an overall program assisting adolescents recovering from child maltreatment. This method of prevention could disrupt the pathway from maltreatment to PTSD symptoms and thereby prevent the development of subsequent PTSD symptoms. Such implications however illustrate the need for future research on clinical methods that directly and effectively target experiential avoidance. Several existing, well-established interventions for children (Cohen, Mannarino, & Deblinger, 2006) and adults (Foa & Rothbaum, 1998) with PTSD target avoidance using various adaptations of exposure (imaginal, written exercises, in-vivo). Exposure, although typically used to counteract overt behaviors generated to avoid places or situations that prompt reminders of the trauma, may be one tool for targeting experiential avoidance of painful private events. Future research on the effects of exposure on experiential avoidance seems worthy and could result in more innovative applications of exposure that more directly target relevant psychological processes in maltreated patients and improve treatment response rates. However, experiential avoidance is a global approach to all painful private events, not just overt behaviors or private events specific to child maltreatment or PTSD, and there are several interventions available using novel methods to target experiential avoidance directly and broadly. Interventions promoting acceptance of private events in conjunction with behavioral change strategies (Hayes, Strosahl, & Wilson, 1999; Linehan, 1993; Segal, Williams, & Teasdale, 2002) have a growing empirical base. These interventions use methods such as mindfulness, acceptance and cognitive defusion to disrupt experiential avoidance and improve clinical outcomes (Forman, Herbert, Moitra, Yeomans, & Geller, 2007). The efficacy of these interventions and their methods for targeting experiential avoidance may be an avenue to explore in future clinical research examining mechanisms of change and improvements in PTSD outcomes. By promoting a willingness to experience difficult thoughts, emotions and memories children who have been maltreated may be able to counteract patterns of experiential avoidance and promote the experiencing of abuse needed to achieve optimal recovery.
Acknowledgments
This project was supported by a University Research Council Award (Shenk: University of Cincinnati), Institutional Clinical and Translational Science Award (NIH/NCRR Grant #: 1UL1RR026314) and an award from the National Institute on Child Health and Human Development (Noll: R01HD052533).
Footnotes
Area under the curve with respect to increase (AUC; Pruessner, Kirschbaum, Meinlschmid, & Hellhammer, 2003) was calculated using all available cortisol samples and estimated in a separate multiple mediator model to determine whether this method of assessing cortisol reactivity provided different results than the model examining CortisolStress. Though point estimates changed slightly, the supplementary model with AUC replicated findings from the original model with CortisolStress and yielded a total indirect effect for the three mediators, Point Estimate = .48, BC 95% CI = .07–1.24, as well as a lone, specific indirect effect for experiential avoidance, Point Estimate = .48, BC 95% CI = .08–1.18.
References
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statisical Manual of Mental Disorders - IV - Text Revision (DSM-IV-TR) Washington, D.C: American Psychiatric Press; 2000. [Google Scholar]
- Barnes JE, Noll JG, Putnam FW, Trickett PK. Sexual and physical revictimization among victims of severe childhood sexual abuse. Child Abuse & Neglect. 2009;33:412–420. doi: 10.1016/j.chiabu.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal Theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology. 2007;74:174–184. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley T, Widom CS. A 30-year follow-up of the effects of child abuse and neglect on obesity in adulthood. Obesity. 2009;17:1900–1905. doi: 10.1038/oby.2009.160. [DOI] [PubMed] [Google Scholar]
- Blechert J, Michael T, Grossman P, Lajtman M, Wilhelm FH. Autonomic and respiratory characteristics of posttraumatic stress disorder and panic disorder. Psychosomatic Medicine. 2007;69:935–943. doi: 10.1097/PSY.0b013e31815a8f6b. [DOI] [PubMed] [Google Scholar]
- Bremner D, Vermetten E, Kelley ME. Cortisol, dehydroepiandrosterone, and estradiol measured over 24 hours in women with childhood sexual abuse-related posttraumatic stress disorder. Journal of Nervous and Mental Disease. 2007;195:919–927. doi: 10.1097/NMD.0b013e3181594ca0. [DOI] [PubMed] [Google Scholar]
- Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: A study of youths in urban America. Journal of Urban Health. 2004;81:530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron A, Palm K, Follette V. Reaction to stressful life events: What predicts symptom severity? Journal of Anxiety Disorders. 2010;24:645–649. doi: 10.1016/j.janxdis.2010.04.008. [DOI] [PubMed] [Google Scholar]
- Carpenter LL, Carvalho JP, Tyrka AR, Wier LM, Mello AF, Mello MF, Anderson GM, Wilkinson CW, Price LH. Decreased adrenocorticotropic hormone and cortisol responses to stress in healthy adults reporting significant childhood maltreatment. Biological Psychiatry. 2007;62:1080–1087. doi: 10.1016/j.biopsych.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrion VG, Weems CF, Ray RD, Glaser B, Hessl D, Reiss AL. Diurnal salivary cortisol in pediatric posttraumatic stress disorder. Biological Psychiatry. 2002;51:575–582. doi: 10.1016/s0006-3223(01)01310-5. [DOI] [PubMed] [Google Scholar]
- Chrousos GP, Gold PW. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA. 1992;267:1244–1252. [PubMed] [Google Scholar]
- Cicchetti D, Blender JA. A multiple-levels-of-analysis approach to the study of developmental processes in maltreated children. Proceedings of the National Academy of Sciences (USA) 2004;101:17325–17326. doi: 10.1073/pnas.0408033101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Dawson G. Multiple levels of analysis. Development and Psychopathology. 2002;14:417–420. doi: 10.1017/s0954579402003012. doi:10.1017.S0954579402003012. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Diverse patterns of neuroendocrine activity in maltreated children. Development and Psychopathology. 2001;13:677–693. doi: 10.1017/s0954579401003145. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. New York, NY: Guilford Press; 2006. [Google Scholar]
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse & Neglect. 2007;31:211–229. doi: 10.1016/j.chiabu.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Cuffe SP, Addy CL, Garrison CZ, Waller JL, Jackson KL, McKeown RE, Chilappagari S. Prevalence of PTSD in a community sample of older adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:147–154. doi: 10.1097/00004583-199802000-00006. [DOI] [PubMed] [Google Scholar]
- Dale LP, Carroll LE, Galen G, Hayes JA, Webb KW, Porges SW. Abuse history is related to autonomic regulation to mild exercise and psychological wellbeing. Applied Psychophysiology Biofeedback. 2009;34:299–308. doi: 10.1007/s10484-009-9111-4. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Hooper SR, Woolley DP, Shenk CE. Demographic, maltreatment, and neurobiological correlates of PTSD symptoms in children and adolescents. Journal of Pediatric Psychology. 2010;35:570–577. doi: 10.1093/jpepsy/jsp116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Harger J, Whitson SM. Exposure to interparental conflict and children’s adjustment and physical health: The moderating role of vagal tone. Child Development. 2001;72:1617–1636. doi: 10.1111/1467-8624.00369. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Whitson SA. Longitudinal relations between marital conflict and child adjustment: Vagal regulation as a protective factor. Journal of Family Psychology. 2006;20:30–39. doi: 10.1037/0893-3200.20.1.30. [DOI] [PubMed] [Google Scholar]
- Foa E, Rothbaum B. Treating the trauma of rape: Cognitive-behavioral therapy for PTSD. New York, NY: Guilford Press; 1998. [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification. 2007;31:772–799. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B, Frost AK, Cohen E. Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:1369–1380. doi: 10.1097/00004583-199510000-00023. [DOI] [PubMed] [Google Scholar]
- Gordis EB, Feres N, Olezeski CL, Rabkin AN, Trickett PK. Skin conductance reactivity and respiratory sinus arrhythmia among maltreated and comparison youth: Relations with aggressive behavior. Journal of Pediatric Psychology. 2010;35:547–558. doi: 10.1093/jpepsy/jsp113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordis EB, Granger DA, Susman EJ, Trickett PK. Asymmetry between salivary cortisol and alpha-amylase reactivity to stress: Relation to aggressive behavior in adolescents. Psychoneuroendocrinology. 2006;31:976–987. doi: 10.1016/j.psyneuen.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Gordis EB, Granger DA, Susman EJ, Trickett PK. Salivary alpha amylase-cortisol asymmetry in maltreated youth. Hormones and Behavior. 2008;53:96–103. doi: 10.1016/j.yhbeh.2007.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, Lejuez CW. A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behavior Therapy. 2007;38:256–268. doi: 10.1016/j.beth.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Hart J, Gunnar M, Cicchetti D. Salivary cortisol in maltreated children: Evidence of relations between neuroendocrine activity and social competence. Development and Psychopathology. 1995;7:11–26. [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, Polusny MA, Dykstra TA, Batten SV, Bergan J, Stewart SH, Zvolensky MJ, Eifert GH, Bond FW, Forsyth JP, Karekla M, McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54:553–578. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experiental avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Felitti VJ, Nordenberg D, Marchbanks PA. Adverse childhood experiences and sexually transmitted diseases in men and women: A retrospective study. Pediatrics. 2000;106:E11. doi: 10.1542/peds.106.1.e11. [DOI] [PubMed] [Google Scholar]
- Hopper JW, Spinazzola J, Simpson WB, van der Kolk BA. Preliminary evidence of parasympathetic influence on basal heart rate in posttraumatic stress disorder. Journal of Psychosomatic Research. 2006;60:83–90. doi: 10.1016/j.jpsychores.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Ivanova JI, Birnbaum HG, Chen L, Duhig AM, Dayoub EJ, Kantor ES, Schiller MB, Phillips GA. Cost of post-traumatic stress disorder vs major depressive disorder among patients covered by medicaid or private insurance. American Journal of Managed Care. 2011;17:e314–323. [PubMed] [Google Scholar]
- Juster RP, Bizik G, Picard M, Arsenault-Lapierre G, Sindi S, Trepanier L, Marin MF, Wan N, Sekerovic Z, Lord C, Fiocco AJ, Plusquellec P, McEwen BS, Lupien SJ. A transdisciplinary perspective of chronic stress in relation to psychopathology throughout life span development. Development and Psychopathology. 2011;23:725–776. doi: 10.1017/s0954579411000289. [DOI] [PubMed] [Google Scholar]
- Keary TA, Hughes JW, Palmieri PA. Women with posttraumatic stress disorder have larger decreases in heart rate variability during stress tasks. International Journal of Psychophysiology. 2009;73:257–264. doi: 10.1016/j.ijpsycho.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin. 1993;113:164–180. doi: 10.1037/0033-2909.113.1.164. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kiess W, Meidert A, Dressendorfer RA, Schriever K, Kessler U, Konig A, Schwarz HP, Strasburger CJ. Salivary cortisol levels throughout childhood and adolescence: Relation with age, pubertal stage, and weight. Pediatric Research. 1995;37:502–506. doi: 10.1203/00006450-199504000-00020. [DOI] [PubMed] [Google Scholar]
- King JA, Mandansky D, King S, Fletcher KE, Brewer J. Early sexual abuse and low cortisol. Psychiatry and Clinical Neurosciences. 2001;55:71–74. doi: 10.1046/j.1440-1819.2001.00787.x. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Archives of Pediatrica and Adolescent Medicine. 2002;156:824–830. doi: 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemieux AM, Coe CL. Abuse-related posttraumatic stress disorder: Evidence for chronic neuroendocrine activation in women. Psychosomatic Medicine. 1995;57:105–115. doi: 10.1097/00006842-199503000-00002. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Earlbaum Associates; 2008. [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMillan HL, Georgiades K, Duku EK, Shea A, Steiner M, Niec A, Tanaka M, Gensey S, Spree S, Vella E, Walsh CA, De Bellis MD, Van der Meulen J, Boyle MH, Schmidt LA. Cortisol response to stress in female youths exposed to childhood maltreatment: Results of the youth mood project. Biological Psychiatry. 2009;66:62–68. doi: 10.1016/j.biopsych.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marciniak MD, Lage MJ, Dunayevich E, Russell JM, Bowman L, Landbloom RP, Levine LR. The cost of treating anxiety: The medical and demographic correlates that impact total medical costs. Depression & Anxiety. 2005;21:178–184. doi: 10.1002/da.20074. [DOI] [PubMed] [Google Scholar]
- Marx BP, Sloan DM. The role of emotion in the psychological functioning of adult survivors of childhood sexual abuse. Behavior Therapy. 2002;33:563–577. doi: 10.1016/s0005-7894(02)80017-x. [DOI] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12:23–44. doi: 10.1037/1082-989x.12.1.23. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Hormones and Behavior. 2003;43:2–15. doi: 10.1016/s0018-506x(02)00024-7. S0018506X02000247. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bulletin. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Miskovic V, Schmidt LA, Georgiades K, Boyle M, MacMillan HL. Stability of resting frontal electroencephalogram (EEG) asymmetry and cardiac vagal tone in adolescent females exposed to child maltreatment. Developmental Psychobiology. 2009;51:474–487. doi: 10.1002/dev.20387. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Noll JG, Shenk CE, Putnam KT. Childhood sexual abuse and adolescent pregnancy: A meta-analytic update. Journal of Pediatric Psychology. 2009;34:366–378. doi: 10.1093/jpepsy/jsn098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez CM, Widom CS. Childhood victimization and long-term intellectual and academic outcomes. Child Abuse & Neglect. 1994;18:617–633. doi: 10.1016/0145-2134(94)90012-4. [DOI] [PubMed] [Google Scholar]
- Plumb JC, Orsillo SM, Luterek JA. A preliminary test of the role of experiential avoidance in post-event functioning. Journal of Behavior Therapy and Experimental Psychiatry. 2004;35:245–257. doi: 10.1016/j.jbtep.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Rosenthal MZ, Aban I, Follette VM. Experimental avoidance as a mediator of the effects of adolescent sexual victimization on negative adult outcomes. Violence & Victims. 2004;19:109–120. doi: 10.1891/vivi.19.1.109.33238. [DOI] [PubMed] [Google Scholar]
- Porges SW. The Polyvagal Theory: Phylogenetic contributions to social behavior. Physiology & Behavior. 2003;79:503–513. doi: 10.1016/s0031-9384(03)00156-2. [DOI] [PubMed] [Google Scholar]
- Porges SW, Byrne EA. Research methods for measurement of heart rate and respiration. Biological Psychology. 1992;34:93–130. doi: 10.1016/0301-0511(92)90012-j. [DOI] [PubMed] [Google Scholar]
- Porges SW, Cohn JF, Bal E, Lamb D. The Dynamic Affect Recognition Evaluation (DARE) software. University of Illinois-Chicago; Chicago, IL: 2007. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–931. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Rosenthal MZ, Cheavens JS, Lynch TR, Follette V. Thought suppression mediates the relationship between negative mood and PTSD in sexually assaulted women. Journal of Traumatic Stress. 2006;19:741–745. doi: 10.1002/jts.20162. [DOI] [PubMed] [Google Scholar]
- Sack M, Hopper JW, Lamprecht F. Low respiratory sinus arrhythmia and prolonged psychophysiological arousal in posttraumatic stress disorder: Heart rate dynamics and individual differences in arousal regulation. Biological Psychiatry. 2004;55:284–290. doi: 10.1016/s0006-3223(03)00677-2. [DOI] [PubMed] [Google Scholar]
- Sahar T, Shalev AY, Porges SW. Vagal modulation of responses to mental challenge in posttraumatic stress disorder. Biological Psychiatry. 2001;49:637–643. doi: 10.1016/s0006-3223(00)01045-3. [DOI] [PubMed] [Google Scholar]
- Santa Ana EJ, Saladin ME, Back SE, Waldrop AE, Spratt EG, McRae AL, LaRowe SD, Timmerman MA, Upadhyaya H, Brady KT. PTSD and the HPA axis: Differences in response to the cold pressor task among individuals with child vs. adult trauma. Psychoneuroendocrinology. 2006;31:501–509. doi: 10.1016/j.psyneuen.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Myers L, Putnam F. Heart period and variability findings in preschool children with posttraumatic stress symptoms. Biological Psychiatry. 2004;55:685–691. doi: 10.1016/j.biopsych.2004.01.006. [DOI] [PubMed] [Google Scholar]
- Scott KM, Smith DR, Ellis PM. Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults. Archives of General Psychiatry. 2010;67:712–719. doi: 10.1001/archgenpsychiatry.2010.71. [DOI] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, Greene A. Fourth National Incidence Study of Child Abuse and Neglect (NIS-4): Report to Congress. Washington, DC: US Dept. of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, National Center on Child Abuse and Neglect; 2010. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse 2002 [Google Scholar]
- Shea A, Walsh C, Macmillan H, Steiner M. Child maltreatment and HPA axis dysregulation: Relationship to major depressive disorder and post traumatic stress disorder in females. Psychoneuroendocrinology. 2005;30:162–178. doi: 10.1016/j.psyneuen.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Shenk CE, Putnam FW, Noll JG. Experiential avoidance and the relationship between child maltreatment and PTSD symptoms: Preliminary evidence. Child Abuse & Neglect. 2012;36:118–126. doi: 10.1016/j.chiabu.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud LR, Foster E, Papandonatos GD, Handwerger K, Granger DA, Kivlighan KT, Niaura R. Stress response and the adolescent transition: Performance versus peer rejection stressors. Development and Psychopathology. 2009;21:47–68. doi: 10.1017/s0954579409000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan TP, Meese KJ, Swan SC, Mazure CM, Snow DL. Precursors and correlates of women’s violence: Child abuse traumatization victimization of women, avoidance coping, and psychological symptoms. Psychology of Women Quarterly. 2005;29:290–301. doi: 10.1111/j.1471-6402.2005.00223.x. [DOI] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Trickett PK, Noll JG, Susman EJ, Shenk CE, Putnam FW. Attenuation of cortisol across development for victims of sexual abuse. Development and Psychopathology. 2010;22:165–175. doi: 10.1017/s0954579409990332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Child Maltreatment, 2009. 2010. [Google Scholar]
- Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. American Journal of Psychiatry. 1999;156:1223–1229. doi: 10.1176/ajp.156.8.1223. [DOI] [PubMed] [Google Scholar]
- Yehuda R. Biology of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62(Suppl 17):41–46. [PubMed] [Google Scholar]