Abstract
Background
Sugar-sweetened beverage (SSB) consumption among children and adolescents is a determinant of childhood obesity. Many programs to reduce consumption across the socio-ecological model report significant positive results; however, the generalizability of the results, including whether reporting differences exist among socio-ecological strategy levels, is unknown.
Objectives
This systematic review aims to (1) examine the extent to which studies reported internal and external validity indicators defined by RE-AIM (reach, effectiveness, adoption, implementation, maintenance) and (2) assess reporting differences by socio-ecological level: intrapersonal/interpersonal (Level 1), environmental/policy (Level 2), multi-level (Combined Level).
Methods
Six major databases (PubMed, Web of Science, Cinahl, CAB Abstracts, ERIC, and Agiricola) systematic literature review was conducted to identify studies from 2004–2015 meeting inclusion criteria (targeting children aged 3–12, adolescents 13–17, and young adults 18 years, experimental/quasi-experimental, substantial SSB component). Interventions were categorized by socio-ecological level, and data were extracted using a validated RE-AIM protocol. A one-way ANOVA assessed differences between levels.
Results
There were 55 eligible studies (N) accepted, including 21 Level 1, 18 Level 2, and 16 Combined Level studies. Thirty-six (65%) were conducted in the USA, 19 (35%) internationally, and 39 (71%) were implemented in schools. Across levels, reporting averages were low for all RE-AIM dimensions (reach=29%, efficacy/effectiveness=45%, adoption=26%, implementation=27%, maintenance=14%). Level 2 studies had significantly lower reporting on reach and effectiveness (10% and 26%, respectively) compared to Level 1 (44%, 57%) or Combined Level studies (31%, 52%) (p<0.001). Adoption, implementation, and maintenance reporting did not vary among levels.
Conclusion
Interventions to reduce SSB in children and adolescents across the socio-ecological spectrum do not provide the necessary information for dissemination and implementation in community nutrition settings. Future interventions should address both internal and external validity to maximize population impact.
Keywords: beverages, youth, children and adolescents, review, systematic
INTRODUCTION
Over the past decade, the consumption of sugar-sweetened beverages (SSBs) has garnered attention as a correlate to childhood obesity.1,2 SSBs, including soft drinks, fruit drinks, and sports and energy drinks, contain few nutrients yet are a top energy source for children and adolescents. Based on a nationally representative sample, children and adolescents in the United States consume an average of 155 calories per day from SSBs, accounting for approximately 8% of their daily caloric intake.3
There is compelling evidence that a link exists between SSB consumption and weight status among children and adolescents and that reducing consumption has favorable effects on weight status.1,4–5 High levels of SSB consumption have also been linked to other adverse health conditions, such as dental decay, headaches, anxiety, and Type 2 diabetes mellitus.6–9 Furthermore, low-income children and adolescents and racial/ethnic minorities consume disproportionate amounts of SSBs and are at higher risk for developing obesity-related diseases, especially Type 2 diabetes.3,10–12
Current interventions to reduce SSB intake use a variety of implementation strategies across levels of the socio-ecological model.13 The model considers the influence of intrapersonal, interpersonal, environmental, and organizational/policy factors on individual and population-level behavior change and is often used to develop childhood obesity initiatives.14–15 The socio-ecological model can be applied to SSB behaviors given that they are ubiquitous, i.e., readily and easily accessible, highly influenced by parental patterns, and pervasively marketed, particularly to Black and Hispanic children.16–24 The Centers for Disease Control specifically recommends using this model when designing strategies to reduce SSB intake, particularly among at-risk populations.25
Many promising studies demonstrate effective interventions to reduce SSB consumption among children and adolescents.1,4,5,26–29 However, all current published and planned systematic reviews of these studies focus almost exclusively on internal validity.1,4,5,26–29 More specifically, these reviews highlight efforts to test interventions under optimal conditions in order to determine the causal relationship between the intervention and participants’ improved SSB outcomes.30 This firmly established evidence regarding the negative impact of SSBs on child and adolescent weight1–2 has led to calls for health and nutrition professionals to promptly and widely facilitate this behavior change, particularly within at-risk groups.2,25 However, translation of research into practice-based recommendations that enhance public health impact requires a better understanding of the external validity across socio-ecological levels. This approach evaluates the degree to which an intervention’s effects are generalizable to contexts outside controlled populations and environments.30–31 This is a gap in the current reporting approach, which provides limited understanding about the external validity. One proposed approach to better understand the potential impact of these interventions is use of Glasgow and colleagues’ RE-AIM (reach, effectiveness, adoption, implementation, maintenance) framework.31
RE-AIM is a tool that assesses both internal and external validity elements of interventions and can be applied to various child and adolescent SSB interventions across socio-ecological levels.32 The framework provides criteria to evaluate the degree to which studies report both internal and external validity. Internal validity components are inclusion/exclusion criteria of participants and delivery agents (reach and adoption), attrition and imputation use (effectiveness, individual-level maintenance), and fidelity (implementation). Examples of external validity components include representativeness of the study sample or setting (reach and adoption), quality of life (effectiveness), and resource costs of implementing and sustaining an intervention in a given setting (implementation and site-level maintenance).31–32
The RE-AIM framework has been frequently used to evaluate the validity of obesity-related interventions that utilize intra- and interpersonal strategies to change behavior and has been recommended TO EVALUATE environmental/policy strategies. However, it has not been used to examine intervention strategies that span the socio-ecological levels.33–42 The body of literature across different levels may differ widely in study design, reporting priorities, and quality. As one example, policy/environmental studies may focus more on setting-level indicators than individual/interpersonal studies. Therefore, assessing overall reporting quality by RE-AIM dimension and evaluating differences among socio-ecological levels will fully inform potential public health impact of available SSB interventions.41
The primary purpose of this systematic review of child and adolescent SSB intervention studies was to (1) examine the extent to which studies reported on RE-AIM indicators and (2) assess differences in reporting on RE-AIM indicators by socio-ecological level (intrapersonal, interpersonal, environmental, policy). Based on previous literature,33–41 our a priori hypotheses were (1) reporting quality would be highest for effectiveness and implementation, followed by reach, adoption, and maintenance and (2) when compared to intrapersonal/interpersonal studies, policy/environmental studies would report reach, efficacy/effectiveness, implementation, and individual-level maintenance indicators to a lower degree and would report adoption and organizational maintenance at a similar or higher degree. A post-hoc exploratory aim was to explore differences in reporting by study design (RCT, quasi-experimental) and setting (school vs. non-school, US vs. non US). Contrary to previous reviews that focus exclusively on internal validity,1,4,5,26–29 findings from this review can identify the gaps in promoting translation of interventions to reduce SSB among children and adolescents into real world practice settings.
METHODS
This systematic review was conducted in June 2015. Eligible articles were those published in English between 2004–2015 and targeting children, adolescents, or young adults (ages 3–18). Study designs included experimental or quasi-experimental designs where pretest-posttest data were presented. Consumption, sales, and/or servings measures were eligible study outcomes across the socio-ecological levels. Articles were excluded if they were not peer-reviewed, were cross-sectional, only reported methods, were published prior to the seminal SSB intervention study in 2004, and did not identify an SSB outcome a priori. Articles that did not include a clear and substantial SSB reduction component (i.e., only assessed SSB as part of a general nutrition intervention or did not explicitly include SSB in policy guidelines) were also excluded.
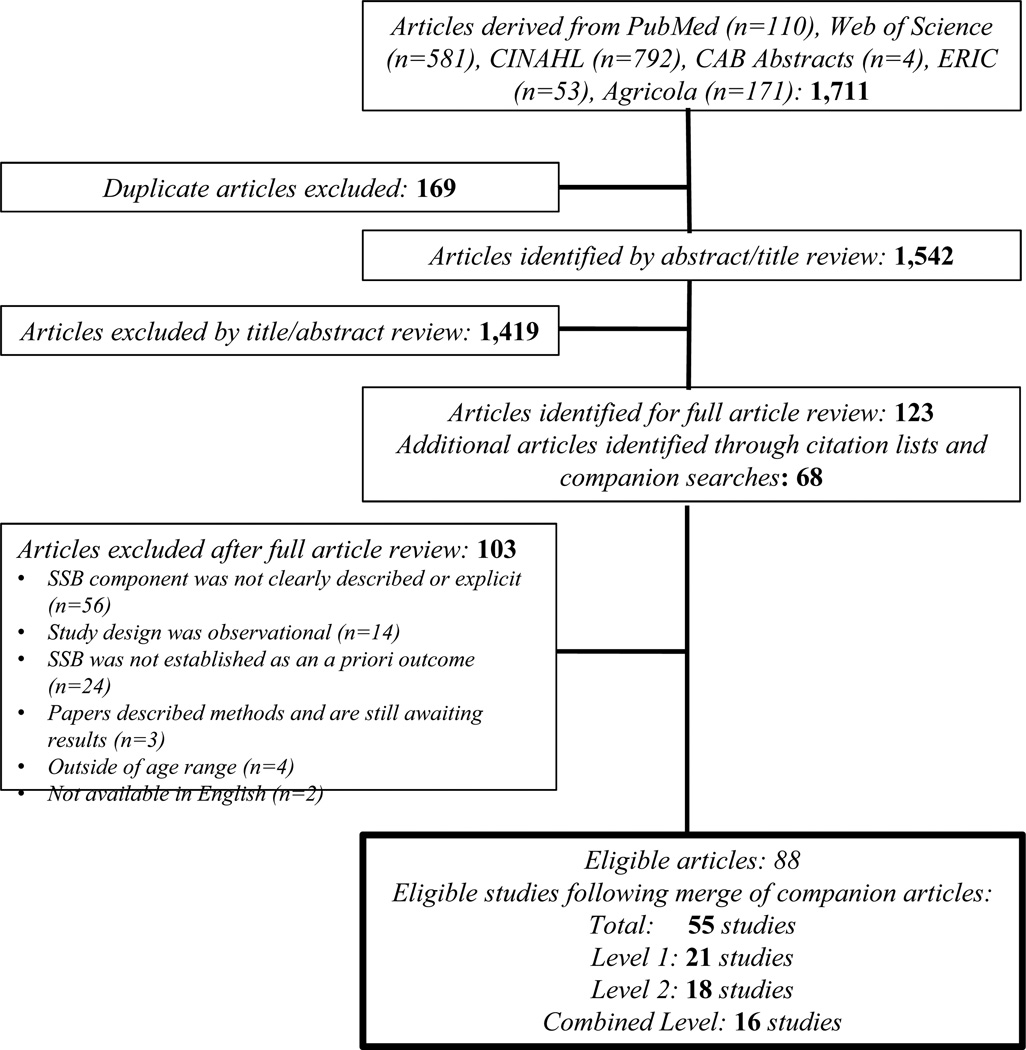
Initial search terms in six databases (Figure 1) included carbonated beverages, energy drinks, sugar sweetened beverage, SSB, sugary drinks, soda, soft drinks, as well as youth, adolescent, child, school and intervention, program, policy, environmental. The search excluded articles pertaining to university or college. This search yielded 1,542 unique citations. Two authors (HL and JZ) reviewed titles and abstracts to determine whether they appeared to meet key inclusion criteria and then met to resolve discrepancies and reach consensus. Subsequent review of citation lists of recent systematic reviews1,4,5,26–29 and eligible studies also yielded 68 unique companion articles, which described additional aspects of eligible interventions. Figure 1 details the systematic process of identification of studies eligible for inclusion in this review.
Figure 1.
Research study selection criteria of experimental, and quasi-experimental SSB studies in children and adolescents.
Eligible articles were reviewed and coded by HL and KP using a previously validated 21-item RE-AIM extraction tool.43,44 The 21 items of the extraction tool represented indicators of the five RE-AIM domains:
Reach: number, proportion, and representativeness of the participants in a study compared to eligible non-participants;
Efficacy/Effectiveness: impact on primary study outcomes, quality of life, and unintended consequences;
Adoption: number, proportion, and representativeness of settings and staff/intervention agents who agree to deliver or implement an intervention compared to non-deliverers;
Implementation: degree to which intervention is delivered as intended and associated costs; and
Maintenance: long-term individual change in primary outcomes and the extent to which intervention delivery or implementation is sustained over time.
Two authors coded five articles together to develop familiarity with the scoring protocol and met with the senior researchers for troubleshooting. All remaining articles were coded independently. Each reviewer coded a 1 (yes) or 0 (no) to indicate the presence or absence of each RE-AIM indicator and, where appropriate, noted specific details for indicators. Cohen’s kappa was calculated for all independently coded articles to determine the tool’s inter-rater reliability (mean=0.85). Coders met to resolve coding disagreements;45 all authors discussed unresolved disagreements to gain consensus.
Proportions of each of the 21 items reported were derived by summing across all studies and dividing by the study total (n=55). The proportion of reporting was also calculated for each RE-AIM dimension. Results were reported as the mean proportion reported across studies by dimensions and specific indicators. Using established protocol, a “comprehensiveness of reporting” score was determined for each study: high quality (15–21 indicators reported), moderate quality (8–14), or low quality (<8).33
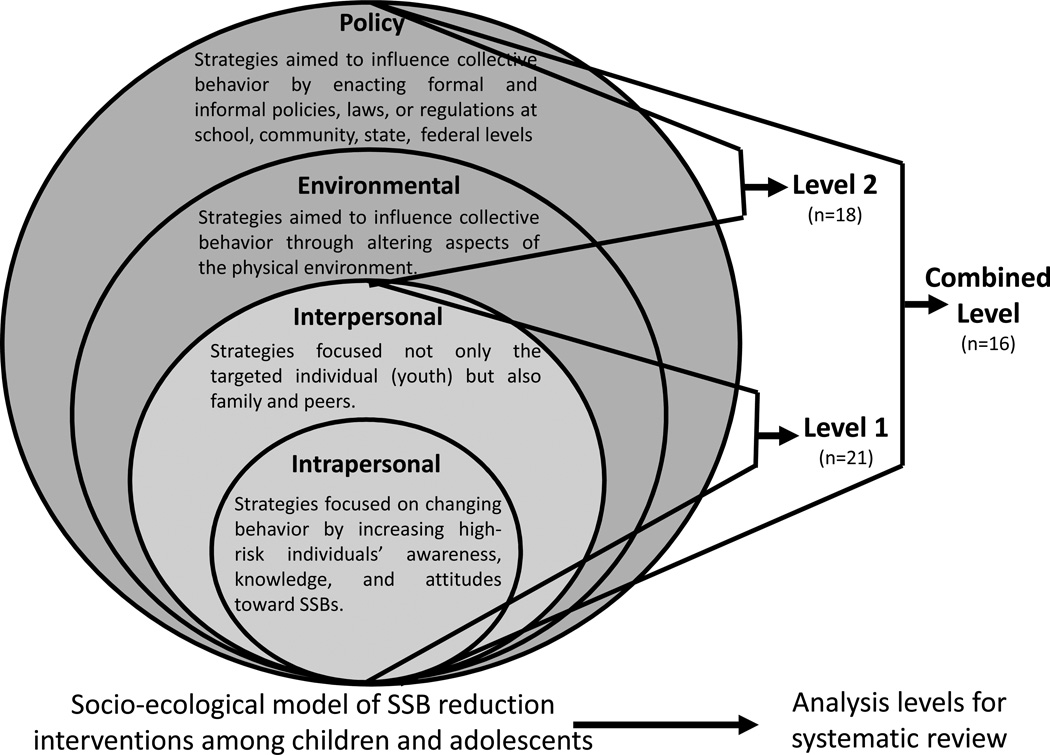
The socio-ecological level of the interventions (i.e., intrapersonal, interpersonal, environmental, or policy) was also documented. The studies were classified into one of three levels derived from the socio-ecological model, as shown in Figure 2:
Level 1: intrapersonal and/or interpersonal strategies;
Level 2: environmental and/or policy strategies;
Combined Level: multi-level strategies, including intrapersonal and/or interpersonal strategies AND environmental and/or policy strategies.
Figure 2.
Evaluating socio-ecological strategy levels that address internal and external validity in child and adolescent (3–18 years) sugar-sweetened beverage consumption studies (n=55)
One-way ANOVAs and Tukey’s post-hoc tests were conducted to examine reporting differences for each RE-AIM dimension among these three levels. Additionally, when data was provided, averages, counts, or proportions were calculated for various RE-AIM indicators (e.g., participation rate, adoption rate) across socio-ecological levels.
RESULTS
Overall Findings
The systematic search identified 88 articles representing 55 studies (Supplemental Table 1). Of these studies, 21 (38%) used intrapersonal and/or interpersonal strategies (Level 1)46–80, 18 (33%) utilized environmental or policy strategies (Level 2)81–107, and 16 (29%) used a combination of intrapersonal and/or interpersonal and environmental and/or policy strategies (Combined Level)108–132. Across all levels, the total proportion of RE-AIM reporting was 29%. Level 1 (35%) and Combined Level studies (34%) had a significantly higher proportion of reporting than Level 2 studies (17%) (p<.001).
Description of Included Studies
About half of the 55 studies were randomized controlled trials46,49–55,57–63,65–71,73–75,77–80, 83–85, 96–98, 109–110, 112–118, 121–124, 127–129, 133 (29; 53%). The remaining studies utilized quasi-experimental designs, with either a two-group64,76,86–90,104,106,111,119–120,125,130–132 (11; 20%), or one-group pretest-posttest47–48,56,72,81–82,91–95,99–103,105,107–108,126 (15; 27%) design. In seven of the one-group designs, the pre- and post-tests were administered to different samples93–95,99–100,105, 107,126. Nearly three-quarters of the interventions and policies (39; 71%) were implemented in schools or multiple settings including schools 46, 49–55, 57–64, 70–72, 76, 80, 86–102, 104–108, 110–111, 114–133. Additional settings included home66–67,109,112–113 (4; 7%), clinic47–48,56,65,68–69,73–75,77–79 (7; 13%), and community-based organizations81–85,103 (5; 9%). Twenty of 55 (36%) studies identified SSB as their sole focus 56, 62–64, 70–72, 84–85, 90, 96, 98–99, 105–106, 109, 112–113, 120–125, 133. Of the 55 studies, a third (19; 35%) were conducted internationally 46, 49–54, 57–60, 62–64, 77–80, 100, 106, 109–110, 115–124, 127–129, 133. Of these, 15 (79%) were conducted in countries similar in economic development to the U.S.46,49–54, 57–60,62–64,77–79,106,115–124,127–129,133. Twenty-two reported using a behavioral theory during development (40%) 46–54, 57–61, 64–68, 77–79, 82–83, 96–98, 110, 114–118, 121–124, 127–129, 133. Finally, 21 (38%) reported focusing their programs or policies toward one or more at-risk groups: those of low socioeconomic status54,108,120–124,133 (5; 9%), racial and/or ethnic minorities47 (1; 2%), those who are overweight or obese 55,65,68,73–75,77–79,109,112,113 (8; 15%), those living in rural areas56,72,98 (3; 5%), or multiple at-risk groups66–67,81,84–85 (4; 19%). Supplemental Table 1 describes characteristics of the 55 individual studies, and Supplemental Table 2 summarizes these characteristics across all studies.
Comprehensiveness of Reporting
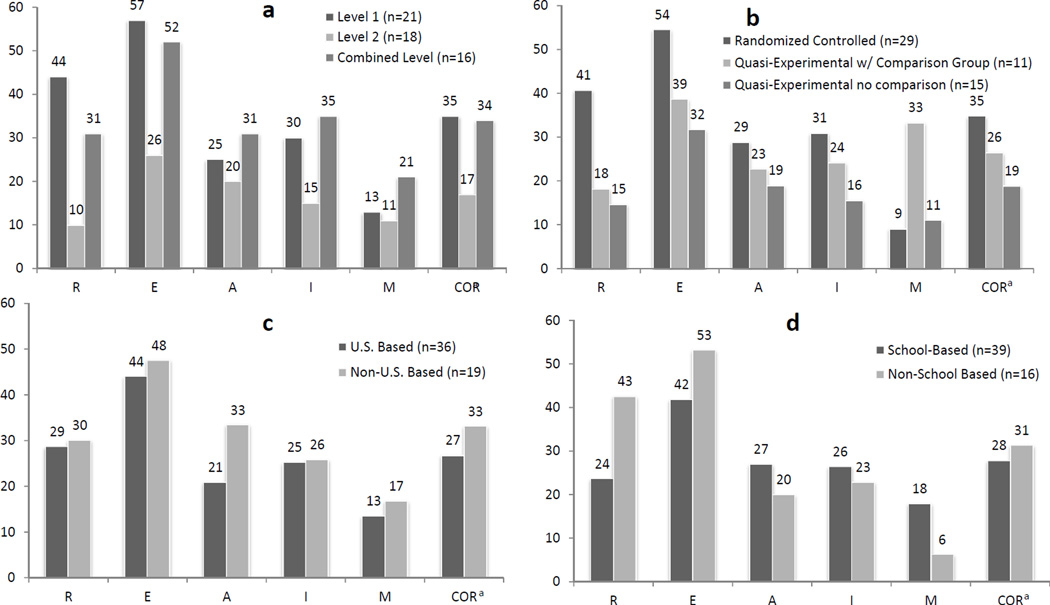
Table 2 details the quality of reporting across the 21 indicators of RE-AIM dimensions by strategy level. Reporting quality was low across studies, with no statistically significant differences by study design or setting (Figure 3). The mean number of indicators reported was 6.0 (SD=3.1), with a range of 1 to 14. Supplemental Table 1 details reporting quality of individual studies. None of the 55 studies were considered high quality, 21 (38%) were moderate quality, and 34 (62%) were low quality. About half of Level 1 and Combined studies (11/21 and 8/16, respectively) were moderate quality, compared to only two of 18 (11%) Level 2 studies.
Figure 3.
Mean proportion reporting of RE-AIM indicators by study characteristics
a. Comprehensiveness of Reporting (COR) score: studies of “low” quality (L) had reported <33% of indicators, studies of “moderate” quality (M) reported between 33% and 67% of indicators, and studies considered “high” quality (H) reported >67%
Figure 3a: Socio-ecological level.; Figure 3b: Study-design; Figure 3c: Country; Figure 3d: Setting
Reach
Across the five reach indicators, the average reporting for all studies was 29%. Level 1 (44%) and Combined Level (31%) studies reported a significantly higher proportion of reach indicators compared to Level 2 (10%) studies (p<.001). Two Level 1 studies reported all reach indicators except representativeness. Reporting averages for each of the five reach indicators are described in Table 2.
Among those reporting participation rate (25 studies), the median number of participants per study was 675±1,331, with an average participation rate of 66%±31%. Across Level 1 (13 studies), Level 2 (4 studies), and Combined Level (8 studies), the median number of participants was 382±497, 705±2,807, and 919±1,075, respectively. Average participation rate ranged widely across Level 1 (63%± 26%), 2 (78%±44%) and C (78%±24%) interventions.
Efficacy/Effectiveness
The average reporting across all studies for the four efficacy/effectiveness indicators was 44%. On average, Level 1 (57%) and Combined Level (52%) studies reported significantly more efficacy/effectiveness indicators than Level 2 (26%) studies (p<.001). One Level 1 study reported all four effectiveness indicators while six Level 1 and five Combined Level studies reported three. Reporting averages for each of the efficacy/effectiveness indicators are described in Table 2.
About half (11/21; 52%) of Level 1 studies reported significant positive results; eight of these had a comparison group. Among Level 2 studies, 14 of 18 (78%) reported positive effects; six of these studies were comparison studies. One of these studies found a positive effect for servings but a null effect for consumption. Finally, over two-thirds of Combined Level studies (11/16; 69%) reported positive effects, including nine of the comparison studies. One of these studies found a positive effect for servings but a null effect for sales while another reported a negative consumption effect (i.e., increased SSB) but found a positive servings effect (i.e., decreased servings). Across all levels, the remaining studies reported either mixed (different within subcategories such as soda and fruit drinks) or null effects (n=5 and n=14, respectively).
Adoption
The average reporting across all studies for the six adoption indicators was 26%. The reporting was not significantly different across levels (25% for Level 1, 20% for Level 2, 31% for Combined Level). While no studies reported all adoption indicators, one Combined Level study reported all but representativeness. Additionally, one Level 1 and one Level 2 study reported four of six indicators. Reporting averages for each of the adoption indicators is described in Table 2.
Of studies reporting participation rate, 21 (38%) reported setting participation rate and two (4%) reported staff participation rate. The average number of settings per study was 40.4±69.0 with an average participation rate of 49%±32%. Across Levels 1 (n=5), 2 (n=7), and Combined (n=9), the respective number of settings was 18.2±13.5, 27.8±36.0, and 67.1±109.5. For the two studies reporting staff participation, the Level 1 study reported participation of 132 staff (38% participation rate) and the Combined Level study reported participation of 140 staff (21% participation rate).
Implementation
The average reporting across all studies for the three implementation indicators was 27%, with differences in reporting across levels approaching significance (p=.052). Level 1, 2, and Combined studies averaged 30%, 15%, and 35% reporting, respectively. Two studies, one Level 1 and one Combined Level reported all three implementation indicators. Reporting averages for each of the implementation indicators is described in Table 2.
Across 12 studies reporting on the degree to which the intervention was implemented as intended, four followed closely with intended protocol, defined as reporting a fidelity <75%, including two of three Level 2 and two of seven Combined Level studies. The remaining eight studies reported fidelity rates between 50 and 75%. No studies reported <50% fidelity. As the few studies that reported implementation costs (n=10) did not use standardized metrics, it was not possible to compare across levels or determine an average implementation cost.
Maintenance
Across the three maintenance indicators, the average reporting among the 55 studies was 14%. There were no statistical differences between levels. The average reporting was 13%, 11%, and 21%, respectively, for Level 1, 2, and Combined studies. No studies reported all three indicators, but five of the 55 studies (representing all levels) reported at least two indicators. Reporting averages for each of the maintenance indicators is described in Table 2.
Of the 11 Level 1 and Combined Level studies reporting maintenance of individual outcomes, seven (64%) reported on maintenance of SSB outcomes as opposed to only weight-related outcomes. Three of these studies, two Level 1 and one Combined Level, reported a positive maintenance outcome, although one had a very brief follow-up period and another only saw maintenance in certain types of SSB. The other four reported either a return to baseline in the intervention group or no significant differences between control and intervention groups at the maintenance time point. Additionally, ten studies reported setting-level maintenance. One was discontinued, seven were sustained with adaptation, and two reported intervention maintenance but did not specify whether adaptation measures were taken.
DISCUSSION
The purpose of this review was to examine the extent to which child and adolescent SSB studies reported on RE-AIM indicators and to determine differences in reporting based on the targeted socio-ecological level. Findings partially support our two hypotheses. First, overall reporting quality was highest for effectiveness and lowest for maintenance, and reporting for reach, implementation, and adoption were relatively similar. Second, studies using environmental/policy strategies reported significantly fewer indicators for reach, efficacy/effectiveness, and individual level maintenance. These studies also were more likely to report on organizational level maintenance but not adoption. Compared to previous RE-AIM reviews, reporting across reach, effectiveness, and implementation dimensions appears to be lower for SSB interventions compared to other behavioral targets, including physical activity, nutrition, or tobacco control.32–35,44 However, SSB studies appear more likely to report adoption rates and setting-level maintenance.
Numerous primary studies and systematic reviews have detailed the promising effects of intervention and policy efforts at achieving reductions in SSB consumption among children and adolescents. However, the true public health impact of these interventions will only be realized if these interventions can be translated beyond research studies and into real-world settings. Simply knowing if an intervention is effective is insufficient. From a public health nutrition perspective, it is important to identify and enact those programs and policies that can reach the most children and adolescents, achieve the best effects, have high likelihood of adoption and implementation by real-world settings, be able to maintain individual-level effects, and be sustained within local systems. Our review highlights that as a whole, key details are missing in these published reports. Without adequate information on all RE-AIM factors, researchers, practitioners, and decision makers lack adequate information to translate the current body of literature into practice and to maximize health impact of available effective interventions and polices to reduce SSB consumption among children and adolescents.
Compared to previous RE-AIM studies, reporting averages for Reach for Levels 1 and Combined appeared lower among SSB interventions than those seen in other behavioral studies.33–35,37,38 However, when compared to reviews of school-based intervention studies (as 39 of the 55 studies were school-based), more similarities emerge. For example, reporting of participation rate in Level 1 and Combined Level studies were similar (∼62% and 50%, respectively) to the proportion of school-based nutrition, physical activity, and tobacco control studies (∼59%).44 The most pronounced difference arises when Level 2 studies are examined— only 22% of these studies reported participation rate. This is similar to the recent review by Brennan and colleagues that found only 10% of 146 obesity, nutrition, and physical activity policy and environmental interventions reported participation rate.42 The lack of reporting of participation rate typically arises due to undefined or unclear denominator, which is defined by the overall target population. Perhaps of even more concern is the lack of reporting of representativeness—only two Level 1 studies reported it—which is also corroborated by Brennan and colleagues, who reported representativeness in two of 32 studies.42 These gaps in reporting indicates a significant lack of understanding of the degree to which a representative population is exposed to interventions to reduce SSB consumption.
When compared to other RE-AIM reviews, our reporting of key efficacy/effectiveness indicators related to changes in quality of life and attrition are lower across SSB intervention studies, particularly Level 2 studies.32–35 However, when compared to other reviews focusing on children and adolescents or school-based interventions, the Level 1 and Combined Level interventions tend to report attrition with similar frequency and also similarly under-report on quality of life indicators.32,35 This suggests that quality of life may not be perceived as important to evaluate in children and adolescents regardless of the targeted behavior. It is promising, however, that most studies showed positive changes to the primary outcome. Furthermore, studies including both individual and environmental components had the highest proportion of effective trials.
Reporting of setting-level adoption and maintenance was considerably higher for SSB reduction studies compared to previous reviews. In particular, maintenance was not reported in any school-based studies of physical activity, nutrition, and tobacco control, or in a systematic review of policy and environmental changes related to childhood obesity.42,44 Studies reporting more on adoption and implementation, particularly adaptations necessary for sustainability, were more likely to include environmental/policy approaches. This suggests that more information is available to promote adoption of these interventions. Similar to reach, there was no data on representativeness of staff or settings where interventions were adopted, making conclusions about generalizability difficult.
Intervention duration, delivery as intended, and cost are key indicators for both internal and external validity. Reporting these factors is critical for replication in both research and practice settings. The lack of reporting on the extent the protocol was implemented as intended limits the internal validity of the findings, particularly among Level 1 and 2 studies. In contrast, the lack of reporting on cost limits the findings’ external validity related to the resources necessary to implement the given intervention in typical practice or community settings. This low implementation reporting is consistent with previous RE-AIM reviews.32–37
Findings also indicate differences in the reporting of specific RE-AIM dimensions between school and non-school studies as well as U.S. and non-U.S. studies. However, the difference in overall comprehensiveness of reporting was negligible (Figure 3cd).
Recommendations for Future Studies
While most of the studies in this review report indicators of internal validity, including SSB outcomes, none comprehensively reported key external validity indicators. This finding is consistent with other reviews that have primarily focused on individual-level behavioral approaches.33,36–38,42,44 Our findings indicate that studies utilizing environmental/policy strategies consistently had lower reporting across individual-level RE-AIM indicators, making it difficult to determine the impact of these intervention strategies at a population level. This finding reinforces the cautionary advice of Jilcott and colleagues, who warn against assuming adopted policies or environmental changes reach everyone within a setting.40 Thus, environmental/policy studies, in particular, could benefit from a balanced reporting of internal and external validity factors across individual and setting level indicators. It is also important to assess any barriers that may prevent the most at-risk members from taking advantage of or being exposed to policy changes.40
The observed gaps in reporting of adoption, implementation, and setting-level maintenance also exist for the individual-level strategies and are not surprising given that this information has been similarly elusive in previous obesity prevention reviews. 134–136 As summarized in this systematic review, the current lack of reporting across RE-AIM dimensions impedes researchers and practitioners’ ability to apply the body of child and adolescent SSB intervention literature to their decisions about appropriate interventions for their own setting and population. Without this information, evidence-based strategies are more difficult to replicate, and are unlikely to reach populations that can benefit most.
Potential challenges
Planning, implementing, and reporting this information may be challenging due to scarce resources, publication word limits, and a lack of knowledge on the importance of reporting both internal and external validity. While these challenges may be particularly prominent for small-scale pilot or feasibility studies, understanding factors beyond effectiveness and internal validity is of paramount importance among these studies. Thus, it is critical to plan, prioritize, and secure resources for a comprehensive evaluation prior to the start of the study. This prioritization needs to be accompanied by more efforts to educate researchers, peer-reviewers, and funding agencies about the importance of moving beyond the “efficacy-based” paradigm and providing opportunities to publish data other than efficacy/effectiveness.31, 137 There is some evidence the paradigm is beginning to shift, such as a recent call to action for nutrition professionals to integrate translational research into their scope of work.137 Based on our review, we have compiled a series of specific recommendations to enable researchers to overcome these challenges, improve reporting of internal and external validity, and subsequently promote the translation of effective intervention strategies into practice.
Recommendation 1
Report reach and representativeness of the study sample to increase transparency of potential generalizability. For strategies at all levels, identify and report characteristics of the study sample (i.e., demographic information), compare them with those of the broader target population, and report the participation rate based on the population. Studies testing environmental/policy approaches should include a measure of target population exposure (i.e., all students in a school district) with a clear description of how exposure is operationalized.
Recommendation 2
Examine the robustness of effects across high-risk groups within the target population and include and report on an indicator of child quality of life as an outcome. Studies at all levels should examine effects across subgroups to emphasize a continued focus on vulnerable children and adolescents. They should also report quality of life to discern whether positive intervention effects are at the expense of child perceptions of quality of life. A number of relatively brief measures of quality of life are available, such as the Peds-QL.138
Additionally, environmental/policy change strategies should provide a logic model highlighting the potential impact on consumption and include brief behavioral assessment of SSB when possible. Although a number of environmental/policy change strategies measure individual-level outcome targets (i.e. sales or servings), these targets are somewhat distal to measurement of consumption.139
Recommendation 3
Provide a description of the study setting and, when applicable, type of staff involved in implementation. For strategies at all levels, identify and report a denominator and characteristics of the target population of settings and staff (i.e., size, location, level of expertise). For studies examining environmental and policy approaches, report any aspects of the decision-making process by which the approach was initially adopted. Further, if the study is in a single setting, provide a detailed description of the setting, including resources available and audiences served.
Recommendation 4
Clearly define and report intervention strategies, content, duration, structure, and costs as well as the degree to which the strategies were implemented as intended. For strategies at all levels, report characteristics of the intervention, including timing and fidelity information, throughout implementation. In addition, include costs related to intervention start-up and ongoing implementation. For policy strategies, include information on the variability in compliance to and enforcement of the policy.40 For environmental change strategies, report on activities related to assessment of any ongoing upkeep.41
Recommendation 5
Assess and report information on the degree to which the intervention is sustained within organizations beyond initial implementation, and whether it leads to sustained behavior change. For strategies at all levels, report outcomes over longer-term periods and include descriptions of adaptations made to ensure sustainability. For policy/environmental changes, include assessments of individual SSB changes for 12 months post-implementation, compliance, and enforcement of policies beyond the scope of research funding.
Limitations
Some limitations to the conclusions and recommendations should be noted. First, the data analyzed and discussed was only that which was reported and does not consider information that may have been collected but not included in the articles. However, companion articles were searched for in order to elicit as much information as possible. Second, the search for articles was limited to peer-reviewed articles, which may have eliminated valuable studies, particularly policy-related, that are published in other outlets. Third, the outcome measures and study designs varied widely and the number of studies per level was modest, which should be considered when interpreting the RE-AIM findings across the levels. Finally, this review focused exclusively on SSB outcomes; therefore, difference in reporting across the socio-ecological strategies may not be generalized to interventions targeting other dietary and health outcomes.
Conclusions
This RE-AIM review across socio-ecological strategy levels systematically documents that child and adolescent-focused SSB intervention studies are not providing enough information to determine best practices for nutrition and dietetics researchers, practitioners, and decision makers. Therefore, despite the quantity of studies as well as the available systematic reviews focused on internal validity,1,4,5,26–29 the potential public health impact of child and adolescent-focused SSB programs and policies remains unclear. To improve translation of evidence-based SSB interventions by nutrition and dietetic professionals in real world settings, future research and reviews should provide more information on all dimensions of the RE-AIM framework, including key elements of both internal and external validity.
Supplementary Material
Table 1.
Proportion of child, adolescent, and young adult-focused sugar-sweetened beverage (SSB) interventions and policies reporting RE-AIM item indicators by socio-ecological level
| Total Trials (%) N=55 Trials; 100% |
Level 1 | Level 2 | Combined Levels | p-value | |
|---|---|---|---|---|---|
| RE-AIM Dimension Total Item Indicators Reported | Individual/ Interpersonal n=21 (% of n) |
Policy/ Environmental n=18 (% of n) |
Individual/ Interpersonal & Policy/ Environmental n=16 (% of n) |
||
| Average % Across all 21 RE-AIM Dimensions | 29 | 35a | 17b | 34a | <0.001 |
| REACH | |||||
| 1) Method to identify target population | 38 | 62 | 11 | 37 | <0.001 |
| 2) Inclusion criteria | 36 | 48 | 17 | 44 | |
| 3) Exclusion criteria | 22 | 38 | 0 | 25 | |
| 4) Participant rate | 45 | 62 | 22 | 50 | |
| 5) Representativeness | 4 | 10 | 0 | 0 | |
| Average % across 5 Item Indicators | 29 | 44a | 10b | 31a | |
| EFFICACY/ EFFECTIVENESS | |||||
| 6) Intent to treat analysis | 20 | 29 | 0 | 31 | <0.001 |
| 7) Quality of life or unintended consequences | 5 | 10 | 0 | 6 | |
| 8) Attrition rate | 56 | 90 | 6 | 69 | |
| 9) Measures/Results from at least one follow-up | 100 | 100 | 100 | 100 | |
| Average % across 4 Item Indicators | 45 | 57a | 26b | 52a | |
| ADOPTION | |||||
| 10) Site and/or staff participation rate | 40 | 24 | 39 | 63 | 0.279 |
| 11) Setting description | 33 | 29 | 39 | 31 | |
| 12) Method to identify staff or delivery agents | 11 | 14 | 6 | 13 | |
| 13) Level of expertise or staff or delivery agents | 40 | 67 | NA | 50 | |
| 14) Inclusion/Exclusion criteria of staff or setting | 29 | 19 | 39 | 31 | |
| 15) Representativeness | 0 | 0 | 0 | 0 | |
| Average % across 6 Item Indicators | 26 | 25 | 20 | 31 | |
| IMPLEMENTATION | |||||
| 16) Intervention duration | 40 | 67 | 6 | 44 | 0.058 |
| 17) Extent protocol delivered as intended | 22 | 10 | 17 | 44 | |
| 18) Measures of implementation costs | 18 | 14 | 22 | 19 | |
| Average % across 3 Item Indicators | 27 | 30 | 15 | 35 | |
| MAINTENANCE | |||||
| 19) Measures/and/or results >6 months post- intervention |
20 | 33 | 0 | 25 | 0.392 |
| 20) Measures of site-level maintenance | 18 | 5 | 22 | 31 | |
| 21) Measures of maintenance costs | 5 | 0 | 11 | 6 | |
| Average % across 3 Item Indicators | 14 | 13 | 11 | 21 | |
Practice Implications.
-
What is the current knowledge on this topic?
Excess consumption of sugar-sweetened beverages (SSBs) among children and adolescents is causal to childhood obesity. Interventions using strategies across the socio-ecological model have reduced consumption among study samples.
-
How does this research add to knowledge on this topic?
This review indicates a lack of reporting of reach, adoption, implementation, and maintenance indicators of these internally effective interventions and policies, limiting their external applicability within different contexts.
-
How might this knowledge impact current dietetics practice?
This review implores SSB researchers to provide more information about external validity of their findings, to enable nutrition practitioners to establish best practices for reducing SSB consumption among children and adolescents.
Acknowledgments
Funding Statement
Support for this research, “Assessing the internal and external validity of sugar-sweetened beverage consumption interventions for children and adolescents: a systematic RE-AIM review using a socio-ecological approach” was provided, in part, by NIH/NCI 1R01CA154364-01 and the Virginia Tech Fralin Translation Obesity Research Center. The views expressed are solely those of the authors and do not reflect the official policy or position of the US government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors of “Assessing the internal and external validity of sugar-sweetened beverage consumption interventions for children and adolescents: a systematic RE-AIM review using a socio-ecological approach” have no conflicts of interest to report.
Contributor Information
Hannah Lane, Virginia Tech, Department of Human Nutrition, Foods and Exercise, 1981 Kraft Drive, Blacksburg, VA 24061, 540-797-3465, hglane07@vt.edu.
Kathleen Porter, Virginia Tech, Department of Human Nutrition, Foods and Exercise, 1981 Kraft Drive, Blacksburg, VA 24061, 540-231-1267, kjporter@vt.edu.
Paul Estabrooks, University of Nebraska Medical Center, Department of Health Promotion, Social & Behavioral Health, Omaha, NE 68198, 402-559-4325, paul.estabrooks@unmc.edu.
Jamie Zoellner, Virginia Tech, Department of Human Nutrition, Foods and Exercise, 1981 Kraft Drive, Blacksburg, VA 24061, 540-231-3670, zoellner@vt.edu.
REFERENCES
- 1.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clinical Nutrition. 2013 doi: 10.3945/ajcn.113.058362. Epub ahead of print August 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related disease. Obesity Reviews. 2013;14:606–619. doi: 10.1111/obr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kit BK, Fakhouri THI, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013;98:180–188. doi: 10.3945/ajcn.112.057943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harrington S. The role of sugar-sweetened beverage consumption in adolescent obesity: a review of the literature. J Sch Nurs. 2008;24(1):3–12. doi: 10.1177/10598405080240010201. [DOI] [PubMed] [Google Scholar]
- 5.Morenga LT, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2013;346:e7492. doi: 10.1136/bmj.e7492. [DOI] [PubMed] [Google Scholar]
- 6.Whiting S, Healey A, Psiuk S, Mirwald R, Kowalski K, Bailey DA. Relationship between carbonated and other low nutrient dense beverages and bone mineral content of adolescents. Nutrition Research. 2001;21(8):1107–1115. [Google Scholar]
- 7.Tahmassebi JF, Duggal MS, Malik-Kotru G, Curzon ME. Soft drinks and dental health: a review of the current literature. J Dent. 2006;34(1):2–11. doi: 10.1016/j.jdent.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Marshall TA, Eichenberger Gilmore JM, Broffitt B, Stumbo PJ, Levy SM. Diet quality in young children is influenced by beverage consumption. J Am Coll of Nutr. 2005;24(1):65–75. doi: 10.1080/07315724.2005.10719445. [DOI] [PubMed] [Google Scholar]
- 9.Wang J, Light K, Henderson M, O’Loughlin J, Mathieu ME, Paradis G, Gray-Donald K. Consumption of added sugars from liquid but not solid sources predicts impaired glucose homeostasis and insulin resistance among youth at risk of obesity. J Nutr. 2014;144(1):81–86. doi: 10.3945/jn.113.182519. [DOI] [PubMed] [Google Scholar]
- 10.Leung CW, Blumenthal SJ, Hoffnagle EE, et al. Associations of food stamp participation with dietary quality and obesity in children. Pediatrics. 2013;131(3):463–472. doi: 10.1542/peds.2012-0889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL. Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics. 2010;125:686–95. doi: 10.1542/peds.2009-2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang YC, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic reviewand meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 13.Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- 14.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 15.Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315:477–480. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haerens L, Craeynest M, Deforche B, Maes L, Cardon G, De Bourdeaudhuij I. The contribution of psychosocial and home environmental factors in explaining eating behaviors in adolescents. Eur J Clin Nutr. 2008;62(1):51–59. doi: 10.1038/sj.ejcn.1602681. [DOI] [PubMed] [Google Scholar]
- 17.Elfhag K, Tholin S, Rasmussen F. Consumption of fruit, vegetables, sweets and soft drinks are associated with psychological dimensions of eating behavior in parents and their 12-year old children. Public Health Nutrition. 2008;11(9):914–923. doi: 10.1017/S1368980008002371. [DOI] [PubMed] [Google Scholar]
- 18.Grimm GC, Harnack L, Story M. Factors associated with soft drink consumption in school-aged children. J Am Diet Assoc. 2004;104(8):1244–1249. doi: 10.1016/j.jada.2004.05.206. [DOI] [PubMed] [Google Scholar]
- 19.Diamant AL, Babey SH, Jones M, Brown ER. Teen dietary habits related to those of parents. Los Angeles, CA: UCLA Center for Health Policy Research; 2009. p. 5. (Health policy research brief) [PubMed] [Google Scholar]
- 20.Robert Wood Johnson Foundation Healthy Eating Research. [Accessed January 31, 2014];Food and beverage marketing to children and adolescents: an environment at odds with good health. http://www.rwjf.org/content/dam/farm/reports/reports/2011/rwjf69944Updated April 2011.
- 21.Harris JL, Schwartz MB, Brownell KD, et al. Sugary Drink FACTS: Evaluating sugary drink nutrition and marketing to youth. New Haven: Rudd Center for Food Policy and Obesity; 2011. [Accessed June 30, 2014]. http://www.sugarydrinkfacts.org/resources/SugaryDrinkFACTS_Report.pdf. Updated October 2011. [Google Scholar]
- 22.Speers SE, Harris JL, Schwartz MB. Child and adolescent exposure to food and beverage brand appearance during prime-time television programming. Am J Prev Med. 2011;41(3):291–296. doi: 10.1016/j.amepre.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 23.Wang YC, Vine SM. Caloric effect of a 16-oz (473-mL) portion-size cap on sugar-sweetened beverages served in restaurants. Am J Clin Nutr. 2013;98(2):430–435. doi: 10.3945/ajcn.112.054833. [DOI] [PubMed] [Google Scholar]
- 24.Robert Wood Johnson Foundation Bridging the Gap Research. [Accessed April 1, 2014];School policies and practice to improve health and prevent obesity: national secondary school survey results. 2 http://www.bridgingthegapresearch.org/_asset/dqzf6p/SS_2012_report.pdf. Updated July 2012. [Google Scholar]
- 25.Centers for Disease Control and Prevention. [Accessed October 1, 2013];The CDC guide to strategies for reducting the consumption of sugar-sweetened beverages. http://www.cdph.ca.gov/SiteCollectionDocuments/StratstoReduce_Sugar_Sweetened_Bev s.pdf. Updated March 2010.
- 26.Clabaugh K, Neuberger GB. Research evidence for reducing sugar sweetened beverages in children. Issues Compr Pediatr Nurs. 2011;34(3):119–130. doi: 10.3109/01460862.2011.593369. [DOI] [PubMed] [Google Scholar]
- 27.Chriqui JF, Pickel M, Story M. Influence of school competitive food and beverage policies on obesity, consumption, and availability: a systematic review. JAMA Pediatr. 2014;168(3):279–286. doi: 10.1001/jamapediatrics.2013.4457. [DOI] [PubMed] [Google Scholar]
- 28.Stevens A, Hamel C, Singh K, et al. Do sugar-sweetened beverages cause adverse health outcomes in children? A systematic review protocol. Systematic Reviews. 2014;3:96. doi: 10.1186/2046-4053-3-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vargas-Garcia E, Evans EL, Cade JE. Impact of interventions to reduce sugar-sweetened beverage intake in children and adults: a protocol for a systematic review and meta-analysis. Systematic Reviews. 2015;4:17. doi: 10.1186/s13643-015-0008-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shadish W, Cook T, Campbell D. Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton Mifflin and Company; 2002. [Google Scholar]
- 31.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999 Sep;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004 Feb;27(1):3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 33.Allen KC, Zoellner JM, Motley M, Estabrooks PA. Understanding the internal and external validity of health literacy interventions: A systematic literature review using the RE-AIM Framework. Journal of Health Communication: International Perspectives. 16:55–72. doi: 10.1080/10810730.2011.604381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harden SM, Burke SM, Haile AM, Estabrooks PA. Generalizing the findings from group dynamic-based physical actviity research to practice settings: what do we know? Eval Health Prof. 2013 doi: 10.1177/0163278713488117. Epub ahead of print May 28. [DOI] [PubMed] [Google Scholar]
- 35.Blackman KCA, Zoellner J, Berrey LM, et al. Assessing the internal and external validity of mobile health physical activity promotion interventions: a systematic literature review using the RE-AIM framework. J Med Internet Res. 2013;15(10):e224. doi: 10.2196/jmir.2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bellicha A, et al. Stair-use interventions in worksites and public settings – a systematic review of effectiveness and external validity. Prev Med. 2015;70C:3–13. doi: 10.1016/j.ypmed.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 37.McGoey T, Root Z, Bruner MW, Law B. Evaluation of physical activity interventions in youth via the Reach, Efficacy/Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework: a systematic review of randomized and non-randomised trials. Prev Med. 2015;76:58–67. doi: 10.1016/j.ypmed.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 38.Klesges LM, Dzewaltowski DA, Glasgow RE. Review of external validity reporting in childhood obesity prevention research. American Journal of Preventive Medicine. 2008;34(3):216–223. doi: 10.1016/j.amepre.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 39.Akers JD, Estabrooks PA, Davy BM. Translational research: bridging the gap between long-term weight loss maintenance research and practice. J Am Diet Assoc. 2010;110(10):1511–1522. doi: 10.1016/j.jada.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jilcott S, Ammerman A, Sommers J. Applying the RE-AIM framework to assess the public health impact of policy change. Ann Behav Med. 2007;34(2):105–114. doi: 10.1007/BF02872666. [DOI] [PubMed] [Google Scholar]
- 41.King DK, Glasgow RE, Leeman-Castillo B. Reaiming RE-AIM: Using the model to plan, implement and evaluation the effects of environmental change approaches to enhancing public health. AJPH. 2010;100:2076–2084. doi: 10.2105/AJPH.2009.190959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brennan LK, Brownson RC, Orleans T. Childhood obesity policy research and practice: evidence for policy and environmental strategies. AJPM. 2014;46(1):e1–e16. doi: 10.1016/j.amepre.2013.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dzewaltowski DA, Estabrooks PA, Klesges LM, Bull S, Glasgow RE. Behavior change intervention research in community settings: how generalizable are the results? Health Promot Int. 2004;19(2):235–245. doi: 10.1093/heapro/dah211. [DOI] [PubMed] [Google Scholar]
- 44.Estabrooks P, Dzewaltowski DA, Glasgow RE, Klesges LM. Reporting of validity from school health promotion studies published in 12 leading journals, 1996–2000. Journal of School Health. 2003;73(1):21–28. doi: 10.1111/j.1746-1561.2003.tb06554.x. [DOI] [PubMed] [Google Scholar]
- 45.Cohen J. A coefficient for agreement for nominal scales. Education and Psychological Measurement. 1960;20:37–46. [Google Scholar]
- 46.Brandstetter S, Klenk J, Berg S, et al. Overweight prevention implemented by primary school teachers: a randomised controlled trial. Obesity Facts. 2012;5(1):1–11. doi: 10.1159/000336255. [DOI] [PubMed] [Google Scholar]
- 47.Bender MS, Clark MJ, Gahagan S. Community engagement approach: developing a culturally appropriate intervention for hispanic mother-child dyads. Journal of Transcultural Nursing. 2014;25(4):373–382. doi: 10.1177/1043659614523473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bender MS, Nader PR, Kennedy C, Gahagan S. A culturally appropriate intervention to improve health behaviors in hispanic mother-child dyads. Childhood Obesity. 2013;9(2):157–163. doi: 10.1089/chi.2012.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bjelland M, Bergh IH, Grydeland M, et al. Changes in adolescents’ intake of sugar-sweetened beverages and sedentary behaviour: results at 8 month mid-way assessment of the HEIA study - a comprehensive, multi-component school-based randomized trial. International Journal of Behavioral Nutrition and Physical Activity. 2011;8(63) doi: 10.1186/1479-5868-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bjelland M, Hausken SES, Bergh IH, et al. Changes in adolescents’ and parents’ intakes of sugar-sweetened beverages, fruit and vegetables after 20 months: results from the HEIA study - a comprehensive, multi-component school-based randomized trial. Food & Nutrition Research. 2015:59. doi: 10.3402/fnr.v59.25932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lien N, Bjelland M, Bergh IH, et al. Design of a 20-month comprehensive, multicomponent school-based randomised trial to promote healthy weight development among 11–13 year olds: the health In Adolescents study. Scandinavian Journal of Public Health. 2010;38(5, Suppl.):38–51. doi: 10.1177/1403494810379894. [DOI] [PubMed] [Google Scholar]
- 52.Grydeland M, Bergh IH, Bjelland M, et al. Correlates of weight status among Norwegian 11-year-olds: the HEIA study. Br J Sports Med. 2013 doi: 10.1186/1471-2458-12-1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gebremariam MK, Andersen LF, Bjelland M, et al. Does the school food environment influence the dietary behaviours of Norwegian 11-year-olds? The HEIA study. Scandinavian Journal of Public Health. 2012;40(5):491–497. doi: 10.1177/1403494812454948. [DOI] [PubMed] [Google Scholar]
- 54.Cunha DB, de Souza BdSN, Pereira RA, Sichieri R. Effectiveness of a randomized school-based intervention involving families and teachers to prevent excessive weight gain among adolescents in Brazil. Plos One. 2013;8(2):e57498. doi: 10.1371/journal.pone.0057498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Davis JN, Ventura EE, Alexander KE, et al. Feasibility of a home-based versus classroom-based nutrition intervention to reduce obesity and type 2 diabetes in Latino youth. International Journal of Obesity. 2007;2:22–30. doi: 10.1080/17477160601133077. [DOI] [PubMed] [Google Scholar]
- 56.Delpier T, Giordana S, Wedin BM. Decreasing sugar-sweetened beverage consumption in the rural adolescent population. J Pediatr Health Care. 2013;27(6):470–478. doi: 10.1016/j.pedhc.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 57.Ezendam NPM, Brug J, Oenema A. Evaluation of the web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized rrial. Archives of Pediatrics & Adolescent Medicine. 2012;166(3):248–255. doi: 10.1001/archpediatrics.2011.204. [DOI] [PubMed] [Google Scholar]
- 58.Ezendam NPM, Oenema A, Van de Looij-Jansen PM, Brug J. Design and evaluation protocol of “FATaintPHAT”, a computer-tailored intervention to prevent excessive weight gain in adolescents. BMC Public Health. 2007;7:324. doi: 10.1186/1471-2458-7-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ezendam NPM, Noordegraaf VSA, Kroeze W, Brug J, Oenema A. Process evaluation of FATaintPHAT, a computer-tailored intervention to prevent excessive weight gain among Dutch adolescents. Health Promotion International. 2012;28(1):26–35. doi: 10.1093/heapro/das021. [DOI] [PubMed] [Google Scholar]
- 60.Ezendam NPM, Burg J, Borsboom G, van Empelen P, Oenema A. Differential effects of the computer-tailored FATaintPHAT programme on dietary behaviours according to sociodemographic, cognitive and home environmental factors. Public Health Nutrition. 2014;17(2):431–439. doi: 10.1017/S1368980012005344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hendy HM, Williams KE, Camise TS. Kid’s Choice Program improves weight management behaviors and weight status in school children. Appetite. 2011;56:484–494. doi: 10.1016/j.appet.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 62.James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ. 2004;328(7450):1237. doi: 10.1136/bmj.38077.458438.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.James J, Thomas P, Kerr D. Preventing childhood obesity: two year follow-up results from the Christchurch obesity prevention programme in schools (CHOPPS) BMJ. 2007;335(7623):762. doi: 10.1136/bmj.39342.571806.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lo E, Coles R, Humbert ML, Polowski J, Henry CJ, Whiting SJ. Beverage intake improvement by high school students in Saskatchewan, Canada. Nutrition Research. 2008;28(3):144–150. doi: 10.1016/j.nutres.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 65.Looney SM, Raynor HA. Examining the effect of three low-intensity pediatric obesity interventions: a pilot randomized controlled trial. Clinical Pediatrics. 2014;53(14):1367–1374. doi: 10.1177/0009922814541803. [DOI] [PubMed] [Google Scholar]
- 66.Nollen NL, Mayo MS, Carlson SE, Rapoff MA, Goggin KJ, Ellerbeck EF. Mobile technology for obesity prevention a randomized pilot study in racial- and ethnic-minority girls. American Journal of Preventive Medicine. 2014;46(4):404–408. doi: 10.1016/j.amepre.2013.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nollen NL, Hutcheson T, Carlson S, Rapoff M, Goggin K, Mayfield C, Ellerbeck E. Development and functionality of a handheld computer program to improve fruit and vegetable intake among low-income youth. Health Education Research. 2013;28(3):249–264. doi: 10.1093/her/cys099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Raynor HA, Osterholt KM, Hart CN, Jelalian E, Vivier P, Wing RR. Efficacy of U.S pediatric obesity primary care guidelines: two randomized trials. Pediatr Obes. 2012;7(1):28–38. doi: 10.1111/j.2047-6310.2011.00005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shapiro JR, Bauer S, Hamer RM, Kordy H, Ward D, Bulik CM. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. Journal of Nutr Educ and Behavior. 2008;40(6):385–391. doi: 10.1016/j.jneb.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sichieri R, Trotte AP, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutrition. 2009;;i(2):197–202. doi: 10.1017/S1368980008002644. [DOI] [PubMed] [Google Scholar]
- 71.Sicheri R, Yokoo EM, Pereira RA, Veiga GV. Water and sugar-sweetened beverage consumption: Changes in BMI among Brazilian fourth graders after 1 year follow-up. Pub Health Nutr. 16(1):73–77. doi: 10.1017/S1368980012001309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Smith LH, Holloman C. Piloting “Sodabriety”: a school-based intervention to impact sugar-sweetened beverage consumption in rural appalachian high schools. Journal of School Health. 2014;84(3):177–184. doi: 10.1111/josh.12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Archives of Pediatrics & Adolescent Medicine. 2011;165(8):714–722. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sonneville KR, Rifas-Shiman SL, Kleinman KP, Gortmaker SL, Gillman MW, Taveras EM. Associations of obesogenic behaviors in mothers and obese children participating in a randomized trial. Pediatric Obesity. 2012;20:1449–1454. doi: 10.1038/oby.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Woo Baidal JA, Price SN, Gonzalez-Suarez E, et al. Parental perceptions of a motivational-interviewing-based pediatric obesity prevention intervention. Clin Pediatr. 2013;52(6):540–548. doi: 10.1177/0009922813483170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tucker S, Lanningham-Foster L, Murphy J, et al. A school based community partnership for promoting healthy habits for life. J Community Health. 2011;36(3):414–422. doi: 10.1007/s10900-010-9323-9. [DOI] [PubMed] [Google Scholar]
- 77.van Grieken A, Renders CM, Veldhuis L, Looman CWN, Hirasing RA, Raat H. Promotion of a healthy lifestyle among 5-year-old overweight children: health behavior outcomes of the ‘Be active, eat right’ study. Bmc Public Health. 2014:14. doi: 10.1186/1471-2458-14-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.van Grieken A, Veldhuis L, Renders CM, et al. Population-based childhood overweight prevention: outcomes of the ‘Be active, eat right’ study. Plos One. 2013;8(5):e65376. doi: 10.1371/journal.pone.0065376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Veldhuis L, Struijk MK, Kroeze W, et al. ‘Be active, eat right,’ evaluation of an overweight prevention protocol among 5 year old children: design of a cluster-randomized controlled trial. BMC Public Health. 2009;9:177. doi: 10.1186/1471-2458-9-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vargas ICD, Sichieri R, Sandre-Pereira G, da Veiga GV. Evaluation of an obesity prevention program in adolescents of public schools. Revista De Saude Publica. 2011;45(1):59–68. doi: 10.1590/s0034-89102011000100007. [DOI] [PubMed] [Google Scholar]
- 81.Wofford L, Froeber D, Clinton B, Ruchman E. Free afterschool program for at-risk African American children: findings and lessons. Family and Community Health. 2013;36(4):299–310. doi: 10.1097/FCH.0b013e31829d2497. [DOI] [PubMed] [Google Scholar]
- 82.Beets MW, Tilley F, Turner-McGrievy G, Weaver RG, Jones S. Community partnership to address snack quality and cost in after-school programs. Journal of School Health. 2014;84(8):543–548. doi: 10.1111/josh.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Beets MW, Tilley F, Weaver RG, Turner-McGrievy G, Moore JB, Webster C. From policy to practice: addressing snack quality, consumption, and price in after-school programs. Journal of Nutrition Education and Behavior. 2014;46(5):384–389. doi: 10.1016/j.jneb.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bleich SN, Herring BJ, Flagg DD, Gary-Webb TL. Reduction in purchases of sugar-sweetened beverages among low-income Black adolescents after exposure to caloric information. Am J Public Health. 2012;102(2):329–335. doi: 10.2105/AJPH.2011.300350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bleich SN, Barry CL, Gary-Webb TL, Herring BJ. Reducing sugar-sweetened beverage consumption by providing caloric information: how Black adolescents alter their purchases and whether the effects persist. Am J Public Health. 2014;104(12):2417–2424. doi: 10.2105/AJPH.2014.302150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Blum JEW, Beaudoin CM, O’Brien LM, Polacsek M, Harris DE, O’Rourke KA. Impact of Maine’s statewide nutrition policy on high school food environments. Preventing Chronic Disease. 2011;8(1):A19. [PMC free article] [PubMed] [Google Scholar]
- 87.Blum JEW, Davee AM, Beaudoin CM, Jenkins PL, Kaley LA, Wigand DA. Reduced availability of sugar-sweetened beverages and diet soda has a limited impact on beverage consumption patterns in Maine high school youth. Journal of Nutrition Education and Behavior. 2008;40(6):341–347. doi: 10.1016/j.jneb.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 88.Blum JEW, Davee AM, Devore RL, et al. Implementation of low-fat, low-sugar and portion-controlled nutrition guidelines in competitive food venues of Main public high schools. Journal of School Health. 2007;77(10):687–693. doi: 10.1111/j.1746-1561.2007.00252.x. [DOI] [PubMed] [Google Scholar]
- 89.Davee AM, Blum JEW, Devore RL, et al. The vending and a la carte policy intervention in Maine Public High Schools. Prev Chronic Dis. 2005 Epub November. [PMC free article] [PubMed] [Google Scholar]
- 90.Cradock AL, McHugh A, Mont-Ferguson H, et al. Effect of schools district policy change on consumption of sugar-sweetened beverages among high school students, Boston, Massachusetts, 2004–2006. Prev Chronic Dis. 2011;8(4):A74. [PMC free article] [PubMed] [Google Scholar]
- 91.Cullen KW, Hartstein J, Reynolds KD, et al. Improving the school food environment; results from a pilot study in middle schools. JADA. 2007;107:484–489. doi: 10.1016/j.jada.2006.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hartstein J, Cullen KW, Reynolds KD, Harrell J, Resnicow K, Kennel P. Impact of portion-size control for school a la carte items: changes in kilocalories and macronutrients purchased by middle school students. J Am Diet Assoc. 2008;108:140–1444. doi: 10.1016/j.jada.2007.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cullen KW, Watson K, Zakeri I. Improvements in middle school student dietary intake after implementation of the Texas Public School Nutrition Policy. Am J Public Health. 2008;98:111–7. doi: 10.2105/AJPH.2007.111765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mendoza J, Watson K, Cullen KW. Change in dietary energy density after implementation of the Texas Public School Nutrition Policy. JADA. 2010;110(3):434–440. doi: 10.1016/j.jada.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fung C, McIsaac JLD, Kuhle S, Kirk SFL, Veugelers PJ. The impact of a population-level school food and nutrition policy on dietary intake and body weights of Canadian children. Preventive Medicine. 2013;57(6):934–940. doi: 10.1016/j.ypmed.2013.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Giles CM, Kenney EL, Gortmaker SL, et al. Increasing water availability during afterschool snack: evidence, strategies, and partnerships from a group randomized trial. American Journal of Preventive Medicine. 2012;43(3):S136–S142. doi: 10.1016/j.amepre.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 97.Kenney EL, Austin SB, Cradock AL, et al. Identifying sources of children’s consumption of junk food in Boston after-school programs, April-May 2011. Prev Chronic Dis. 2014;11:E205. doi: 10.5888/pcd11.140301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Goto K, Waite A, Wolff C, Chan K, Giovanni M. Do environmental interventions impact elementary school students’ lunchtime milk selection? Applied Economic Perspectives and Policy. 2013;35(2):360–376. [Google Scholar]
- 99.Kansagra SM, Kennelly MO, Nonas CA, et al. Reducing sugary drink consumption: New York City’s approach. Am J Public Health. 2015;105(4):e61–e64. doi: 10.2105/AJPH.2014.302497. Epub 302015 Feb 302425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kim K, Park SM, Oh KW. The impact of nutritional policy on socioeconomic disparity in the unhealthy food intake among Korean adolescents. Appetite. 2013:388–395. doi: 10.1016/j.appet.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 101.Kubik MY, Davey C, Nanney MS, MacLehose RF, Nelson TF, Coombes B. Vending and school store snack and beverage trends: Minnesota secondary schools, 2002–2010. American Journal of Preventive Medicine. 2013;44(6):583–588. doi: 10.1016/j.amepre.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Nanney MS, MacLehose R, Kubik MY, Davey CS, Coombes B, Nelson TF. Recommended school policies are associated with student sugary drink and fruit and vegetable intake. Preventive Medicine. 2014;62:179–181. doi: 10.1016/j.ypmed.2014.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of an organizational intervention designed to improve snack and beverage quality in YMCA after-school programs. Am J Public Health. 2010;100(5):925–932. doi: 10.2105/AJPH.2008.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Schwartz MB, Novak SA, Fiore SS. The impact of removing snacks of low nutritional value from middle schools. Health Educ Behav. 2009;36:999–1011. doi: 10.1177/1090198108329998. [DOI] [PubMed] [Google Scholar]
- 105.Simon PA, Lightstone AS, Baldwin S, Kuo T, Shih M, Fielding JE. Declines in sugar-sweetened beverage consumption among children in Los Angeles County, 2007 and 2011. Prev Chronic Disease. 2013;10:E131. doi: 10.5888/pcd10.130049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Visscher TLS, van Hale WCW, Blokdijk L, Seidell JC, Renders CM, Bemelmans WJE. Feasibility and impact of placing water coolers on sales of sugar-sweetened beverages in dutch secondary school canteens. Obesity Facts. 2010;3(2):109–115. doi: 10.1159/000300848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Woodward-Lopez G, Gosliner W, Samuels SE, Craypo L, Kao J, Crawford PB. Lessons learned from evaluations of California’s statewide school nutrition standards. Am J of Public Health. 2010;100(11):2137–2145. doi: 10.2105/AJPH.2010.193490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Samuels SE, Craypo L, Boyle M, Crawford PB, Yancey A, Flores G. The California Endowment’s Healthy Eating, Active Communities program: a midpoint review. Am J of Public Health. 2010;11(11):2114–2123. doi: 10.2105/AJPH.2010.192781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Albala C, Ebbeling CB, Cifuentes M, Lera L, Bustos N, Ludwig DS. Effects of replacing the habitual consumption of sugar-sweetened beverages with milk in Chilean children. American J of Clinical Nutrition. 2008;88(3):605–611. doi: 10.1093/ajcn/88.3.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bacardi-Gascon M, Perez-Morales E, Jimenez-Cruz A. A six-month randomized school intervention and an 18-month follow-up intervention to prevent childhood obesity in Mexican elementary schools. Nutr Hosp. 2012;27(3):755–762. doi: 10.3305/nh.2012.27.3.5756. [DOI] [PubMed] [Google Scholar]
- 111.Bogart LM, Elliott MN, Uyeda K, Hawes-Dawson J, Klein DJ, Schuster MA. Preliminary healthy eating outcomes of SNaX, a pilot community-based intervention for adolescents. Journal of Adolescent Health. 2011;48(2):196–202. doi: 10.1016/j.jadohealth.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, Ludwig DS. A randomized trial of sugar-sweetened beverages and adolescent body weight. N Engl J Med. 2012;367(15):1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ebbeling CB, Feldman HA, Osganian SK, Chomitz VR, Ellenbogen SJ, Ludwig DS. Effects of decreasing sugar-sweetened beverage consumption on body weight in adolescents: a randomized, controlled pilot study. Pediatrics. 2006;117(3):673–680. doi: 10.1542/peds.2005-0983. [DOI] [PubMed] [Google Scholar]
- 114.Goldberg JP, Folta SC, Eliasziw M, et al. Great Taste, Less Waste: A cluster-randomized trial using a communications campaign to improve the quality of foods brought from home to school by elementary school children. Preventive Medicine. 2015;74:103–110. doi: 10.1016/j.ypmed.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Haerens L, De Bourdeaudhuij I, Maes L, Vereecken C, Brug J, Deforche B. The effects of a middle-school healthy eating intervention or adolescents’ fat and fruit intake and soft drinks consumption. Public Health Nutrition. 2007;10(5):443–449. doi: 10.1017/S1368980007219652. [DOI] [PubMed] [Google Scholar]
- 116.Haerens L, Deforche B, Maes L, Cardon G, Stevens V, De Bourdeaudhuij I. Evaluation of a 2-year physical activity and healthy eating intervention in middle school children. Health Education Research. 2006;21(6):911–921. doi: 10.1093/her/cyl115. [DOI] [PubMed] [Google Scholar]
- 117.Kocken PL, van Kesteren NMC, Buijs G, Snel J, Dusseldorg E. Students’ beliefs and behavior regarding low-calorie beverages, sweets or snacks: are they affected by lessons on healthy food and by changes to school vending machines? Public Health Nutrition. 2015;18(9):1545–1553. doi: 10.1017/S1368980014002985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kocken PL, Eeuwijk J, van Kesteren NMC, et al. Promoting the purchase of low-calorie foods from school vending machines: a cluster randomized controlled study. J School Health. 2012;82(3):115–122. doi: 10.1111/j.1746-1561.2011.00674.x. [DOI] [PubMed] [Google Scholar]
- 119.Laurence S, Peterken R, Burns C. Fresh Kids: the efficacy of a health promoting schools approach to increasing consumption of fruit and water in Australia. Health Prom International. 2007;22(3):218–226. doi: 10.1093/heapro/dam016. [DOI] [PubMed] [Google Scholar]
- 120.Loughridge JL, Barratt J. Does the provision of cooled filtered water in secondary school cafeterias increase water drinking and decrease the purchase of soft drinks. J Hum Nutr Dietet. 2005;18:281–286. doi: 10.1111/j.1365-277X.2005.00622.x. [DOI] [PubMed] [Google Scholar]
- 121.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123(4):E661–E667. doi: 10.1542/peds.2008-2186. [DOI] [PubMed] [Google Scholar]
- 122.Muckelbauer R, Libuda L, Clausen K, Kersting M. Long-term process evaluation of a school-based programme for overweight prevention. Child. 2009;35(6):851–857. doi: 10.1111/j.1365-2214.2009.00993.x. [DOI] [PubMed] [Google Scholar]
- 123.Muckelbauer R, Libuda L, Clausen K, Reinehr T, Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obesity Facts. 2009;2:282–285. doi: 10.1159/000229783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Immigrational background affects the effectiveness of a school-based overweight prevention program promoting water consumption. Obesity. 2010;18:528–534. doi: 10.1038/oby.2009.270. [DOI] [PubMed] [Google Scholar]
- 125.Patel AI, Bogart LM, Elliott MN, et al. Increasing the availability and consumption of drinking water in middle schools: a pilot study. Preventing Chronic Disease. 2011;8(3):A60. [PMC free article] [PubMed] [Google Scholar]
- 126.Rogers VW, Hart PH, Motyka E, Rines EN, Vine J, Deatrick DA. Impact of Let’s Go! 5-2-1-0: A Community-Based, Multisetting Childhood Obesity Prevention Program. J Pediatr Psychol. 2013;38(9):1010–1020. doi: 10.1093/jpepsy/jst057. [DOI] [PubMed] [Google Scholar]
- 127.Singh AS, Chin APMJ, Brug J, van Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163(4):309–317. doi: 10.1001/archpediatrics.2009.2. [DOI] [PubMed] [Google Scholar]
- 128.Singh AS, Chinapaw MJ, Brug J, van Mechelen W. Process evaluation of a school-based weight gain prevention program: the Dutch Obesity Intervention in Teenagers (DOiT) Health Educ Res. 2009;24(5):772–777. doi: 10.1093/her/cyp011. [DOI] [PubMed] [Google Scholar]
- 129.Singh AS, Paw MJMCA, Kremers SPJ, Visscher TLS, Brug J, Mechelen W. Design of the Dutch Obesity Intervention in Teenagers (NRG-DOiT): systematic development, implementation and evaluation of a school-based intervention aimed at the prevention of excessive weight gain in adolescents. BMC Public Health. 2006 doi: 10.1186/1471-2458-6-304. Epub ahead of print December 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Taylor RW, McAuley K, Barbezat W, Strong A, Williams SM, Mann JI. APPLE Project: 2-y findings of a community-based obesity prevention prevention program in primary school-age children. Am J Clin Nutr. 2007;86(3):735–742. doi: 10.1093/ajcn/86.3.735. [DOI] [PubMed] [Google Scholar]
- 131.Taylor RW, McAuley KA, Williams SM, Barbezat W, Nielsen G, Mann JI. Reducing weight gain through enhancing physical activity and nutrition: the APPLE project. International J Obesity. 2006;1(3):146–152. doi: 10.1080/17477160600881247. [DOI] [PubMed] [Google Scholar]
- 132.McAuley KA, Taylor RW, Farmer VL, Hansen P, Williams SM, Booker CS, Mann JI. Economic evaluation of a community-based obesity prevention project in children: the APPLE project. Obesity. 2009;18:131–136. doi: 10.1038/oby.2009.148. [DOI] [PubMed] [Google Scholar]
- 133.van de Gaar VMV, Jansen W, van Grieken A, Borsboom G, Kremers S, Raat H. Effects of an intervention aimed at reducing the intake of sugar-sweetened beverages in primary school children: a controlled trial. International Journal of Behavioral Nutrition and Physical Activity. 2014:11. doi: 10.1186/s12966-014-0098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children (Review) Cochrane Database Syst Rev. 2011;12:CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 135.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity. 2008;16:1009–1018. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 136.Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. A synthesis of existing systematic reviews and meta-analyses of school-based behavioral interventions for controlling and preventing obesity. doi: 10.1111/j.1467-789X.2011.00947.x. [DOI] [PubMed] [Google Scholar]
- 137.Zoellner J, Van Horn L, Gleason PM, Boushey CJ. What is translational research? Concepts and applications in nutrition and dietetics. JAND. 2015;115(7):1057–1071. doi: 10.1016/j.jand.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 138.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care. 1999;37(3):126–139. doi: 10.1097/00005650-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 139.Richard L, Potvin L, Kishchuk N, Prlic H, Green LW. Assessment of the integration of the ecological approach in health promotion programs. American Journal of Health Promotion. 1996;10(4):318–328. doi: 10.4278/0890-1171-10.4.318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.