Abstract
New technologies enabling the analysis of various molecules, including DNA, RNA, proteins and small metabolites, can aid in understanding the complex molecular processes in cancer cells. In particular, for the use of novel targeted therapeutics, elucidation of the mechanisms leading to cell death or survival is crucial to eliminate tumor resistance and optimize therapeutic efficacy. While some techniques, such as genomic analysis for identifying specific gene mutations or epigenetic testing of promoter methylation, are already in clinical use, other “omics-based” assays are still evolving. Here, we provide an overview of the current status of molecular profiling methods, including promising research strategies, as well as possible challenges, and their emerging role in radiation oncology.
Keywords: molecular profiling, precision medicine, radiation oncology, targeted therapy
Introduction
During the last decade, the outcome for cancer patients receiving radiotherapy or chemoradiation has continuously improved. This success is not only due to technical and imaging advances and the more accurate delivery of radiation to a tumor, but also to the implementation of molecular therapeutics into radiation oncology treatment regimens, which allows for more specific cancer cell targeting [1,2]. Although very encouraging results have been obtained in a subset of patients with specific molecular-targeted drugs, multiple clinical studies indicate that tumor heterogeneity is a major obstacle resulting in varied tumor responses, including non-response, to targeted therapy [3]. The molecular and phenotypic heterogeneity is present prior to treatment and the treatment itself can select for resistant subpopulations and induce further heterogeneity leading to tumor cell resistance. Thus, elucidation of the complex molecular processes and identification of potential de novo and bypass signaling can contribute to the optimization and individualization of patient therapy [4,5]. Exploiting the tumor phenotype before treatment as well as the adaptation of tumor cells to the changes that result from therapy is a novel approach to effective precision cancer treatment. An interest of our laboratory is understanding how cancer and normal cells adapt to radiation and how these phenotypic changes might be used to enhance the efficacy of radiotherapy [6–8]. With increasing knowledge about molecular mechanisms, it is becoming more evident that the effect of radiotherapy on tumor cell survival is not only dependent on physical beam properties, radiation dose and DNA damage but is also strongly influenced by radiation-induced perturbation of biological processes, a concept named “focused biology” [9]. This implies the potential use of radiation in a novel way in combination with both molecular targeted drugs and also immunotherapy [10,11].
In addition to the targeting of molecules expressed in cancer cells, the therapeutic potential of immune response modulation is currently under intense evaluation in clinical trials [12–14]. This approach is based on the observation that some tumors have the ability to suppress the antigen-induced activation of leukocytes resulting in reduced cancer cell killing and poor patient survival [15–17]. Therefore, immune checkpoint inhibitors such as ipilimumab and nivolumab, which modify the interaction between the tumor cells and T lymphocytes, can be used to abrogate the tumor-mediated immune inhibition [17]. First results in patients with melanoma and advanced non-small cell lung cancer (NSCLC) are very promising [12,13], although a recent randomized phase III trial in patients with metastatic prostate cancer showed no significant survival benefit of ipilimumab treatment after radiotherapy compared with the placebo group [18]. Future studies will clarify the role of these compounds in radiation oncology.
The development of methods facilitating the simultaneous analysis of multiple molecular characteristics in a small tumor sample was a precondition for omics-based assays. With the implementation of DNA microarrays into cancer research, it was possible for the first time to determine the expression of thousands of genes in one assay and detect disease- or resistance-driving mutations in tumor tissue on a large scale [19,20]. Next-generation sequencing enabled the analysis of a complete human genome in one day, a process, which took several years in the past [21,22]. The tremendous technical and methodical advances in the last two decades and the possibility to apply these assays in a high-throughput setting have greatly contributed to the clinical and scientific significance of omics-based methods.
The family of “omics” is growing including analysis of gene mutation status and RNA expression [3,23–26], epigenetic changes such as promotor methylation and histone modifications [27,28], protein expression and phosphorylation [29–31] and metabolite levels [32,33] all of which can affect the radiation and treatment response of tumors (Figure 1). Extensive omics-based analysis of cancer cells before, during and after radio- and chemotherapy could be used to reveal molecular mechanisms, predict therapy efficacy and guide therapy as the tumor adapts to treatment. In this review, we summarize and discuss key findings of genomic, transcriptomic, proteomic, epigenomic and metabolomic studies and the role of the different molecular profiling methods in radiation oncology.
Figure 1. Schematic representation of how genome, epigenome, transcriptome, proteome and metabolome modulate each other and their impact on the cellular phenotype.
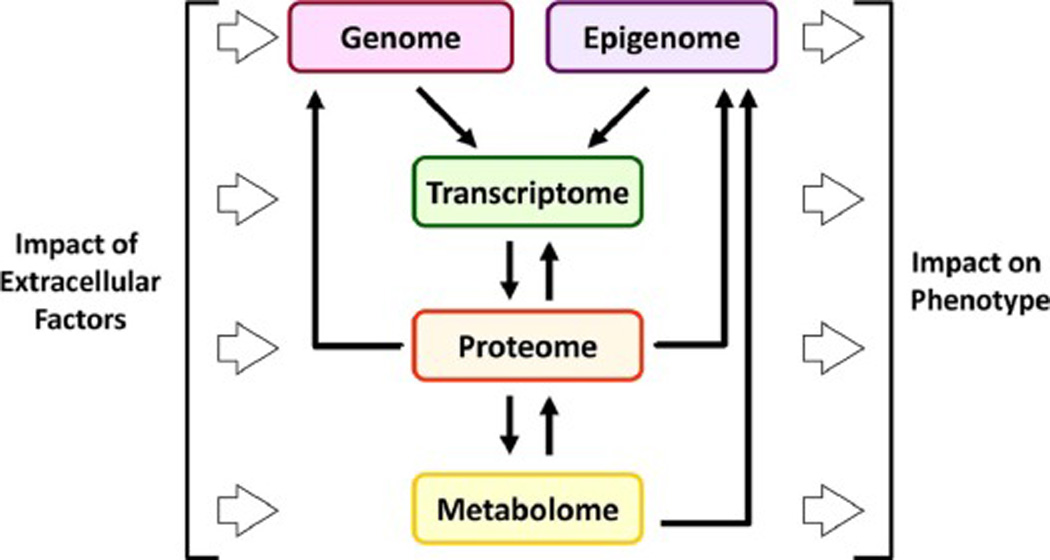
The DNA (genome) and the epigenetic modifications (epigenome) regulate transcription of RNA (transcriptome). The mRNA is translated into proteins (proteome). These proteins including enzymes modulate the expression of metabolites (metabolome), but also transcription, genetic and epigenetic markers. Extracellular factors like irradiation or chemotherapy can affect all molecular processes, with the strongest influence at the metabolic level. The cellular phenotype is substantially determined by all molecules.
Genomic analysis and its potential for patient stratification
Given that both treatment sensitivity to a molecular compound as well as intrinsic or acquired resistance of tumor cells can be caused by gene mutations, genetic analysis is considered to be crucial for choosing the most effective therapy [34,35]. While matching the “right” drug to a mutation is a major area of research, the efficacy of the new molecular therapeutics is very sensitive to structural changes in the target molecule or the functional changes in the downstream signaling pathway and therefore the examination of gene mutation status prior to treatment is essential [36–38].
Inhibitors of the epidermal growth factor receptor (EGFR) were among the first targeted therapeutics whose treatment outcome could be linked to a specific genetic profile including the molecule being targeted as well as downstream pathways, as discussed below. In combination with radiotherapy, clinical studies with the EGFR antibody cetuximab showed promising results in patients with head and neck squamous cell carcinoma (HNSCC), resulting in the approval and implementation of this drug in clinical treatment regimens [39,40]. However, cetuximab failed to improve the overall outcome for patients with colorectal tumors [41,42] and NSCLC [43]. Extensive genomic studies show that one potential factor for the effect of inhibitory EGFR antibodies was the mutation status of the Kirsten rat sarcoma 2 viral oncogene homolog (KRAS) and v-Raf murine sarcoma viral oncogene homolog B (BRAF) genes, coding for two signaling molecules of the EGFR pathway [37,44–47]. Tumors expressing wildtype KRAS and BRAF had a significantly higher control rate when cetuximab therapy was applied, while the presence of specific KRAS or BRAF mutations diminished the tumor response [37,44,45]. In patients with BRAF/KRAS wildtype rectal carcinoma, receiving neoadjuvant radio-chemotherapy, cetuximab increased overall survival and radiologic tumor response rate, while there was no significant effect in the whole patient population (including patients with both wildtype and mutated BRAF/KRAS tumors) [48]. However, factors other than the genetic background may also be important for the therapeutic efficacy of EGFR antibodies, as recent studies show that even in BRAF or KRAS wildtype colorectal carcinoma the response to cetuximab is not invariably present [41,42,49,50].
Similar to EGFR antibodies, EGFR tyrosine kinase inhibitors have been found to be more effective in a specific subset of patients. After the first generation EGFR inhibitor gefitinib was approved for treatment of NSCLC in 2003, two clinical studies showed no significant survival benefit, which led to the use of the drug being restricted to patients who previously benefited from gefitinib without understanding the reasons for the differential clinical responses [51]. Later, sub-analyses revealed that patients with specific activating mutations in the EGFR kinase domain had a much better response rate [3,52]. Similar findings were observed in clinical trials with the EGFR inhibitors erlotinib and afatinib [38,53]. Several recent phase II studies describe promising results for the use of EGFR kinase inhibitors in combination with radiotherapy [54–56]. In these trials, when erlotinib was added to the treatment regimen, the outcome and response in patients with advanced stage NSCLC was better than the results from published studies [54–56]. Interestingly, Komaki and colleagues did not find a correlation between EGFR mutation status and response [54], although this may be due to the relatively small patient numbers or to different molecular mechanisms with the drug used alone or in combination with radiation. Therefore, further studies are needed to clarify the factors modulating the efficacy of EGFR kinase inhibitors combined with radiotherapy and radio-chemotherapy. Within the focused biology concept, the therapeutic effect of drugs that have been developed as mono-therapeutic agents may be improved by using them with radiation, for example, when the target expression is upregulated by radiotherapy.
Genomic analysis can also be used to personalize treatment and enhance the efficacy of drugs on malignant tissue by exploiting existing differences in the structure of target molecules [35]. For example, the BRAF inhibitors vemurafenib and dabrafenib are designed to inhibit only BRAF with a substitution of the amino acid valine at position 600 with glutamic acid (V600E), but not wildtype BRAF [35]. This V600E mutation is frequently found in melanoma and papillary thyroid carcinoma [57]. Inhibition of BRAF results in a significant increase of overall and disease-free survival in patients with BRAF-mutant melanoma [35]. Despite these promising results, the majority of tumors develop resistance over time, leading to disease recurrence and progression [58]. Genomic analysis revealed a variety of underlying mechanisms including changes of the BRAF sequence, itself, and activating mutations of downstream targets [36,58].
To date, there are few clinical studies analyzing the efficacy of BRAF inhibition in combination with radiotherapy. Satzger and colleagues reported several cases of severe radiation dermatitis in patients with metastatic melanoma treated concomitantly with dabrafenib or vemurafenib [59]. Interestingly, all tumors showed no response to the treatment, indicating a radiosensitizing effect on normal tissue with wildtype BRAF, but not on malignant cells harboring BRAF V600E mutations. One possible explanation for this finding is that the effect of radiation on the skin is potentiated by the drug-related cutaneous side effects of BRAF inhibitors including erythema and hand-foot syndrome which are thought to be caused by a paradoxical activation of the mitogen-activated protein kinase (MAPK) pathway in wildtype BRAF cells [59–61]. This further emphasizes how molecular targeted drugs can have different effects when they are used in combination with radiation compared to mono-therapeutic application.
In addition to activating mutations, genetic changes such as gene deletions can be important for the efficacy of targeted therapy. Inhibition of the poly (ADP-ribose) polymerase (PARP), an enzyme involved in repairing DNA single strand breaks (SSBs), has no radiosensitizing effect in normal cells due to an efficient repair of SSBs by homologous recombination (HR). In cells with a defect in HR (e.g. by a frameshift mutation in the breast cancer, early onset [BRCA] 1 or BRCA2 gene), PARP inhibitors strongly reduce cellular radiation survival [62]. As hereditary BRCA mutations promote the development of breast and ovarian cancer, a certain percentage of these tumors are BRCA1 or BRCA2 negative. These tumors have been successfully treated with PARP inhibitors, such as olaparib [63,64]. However, in most clinical trials PARP inhibitors were predominantly combined with cytotoxic drugs and not with radiotherapy, so that the role of PARP inhibition in radiation therapy is not yet clearly defined.
Although these data show that genomic analysis contributes to the optimization of targeted therapy, many resistance mechanisms are based on cellular processes like transcription or protein signaling and not solely on genetic alterations. Therefore, further molecular profiling techniques are required to evaluate the tumor response in more detail.
The use of epigenomics for predicting outcome and drug efficacy
Epigenetic alterations play an important role not only in many physiologic processes including DNA replication and repair, but also in disease development and cancer cell resistance to therapy [65,66]. DNA methylation can regulate promoter activity and therefore affect gene expression and silencing [65]. Additionally, histone modifications at specific residues are involved in gene activation or inactivation and have been shown to modulate radiosensitivity [27,28,66–68].
One example of the use of epigenetic characteristics as a predictive marker for cancer therapy is the promoter methylation status of the O6-methylguanine methyltransferase gene (MGMT) in glioblastoma. Here, a highly methylated and, therefore, silenced promoter correlates with a better outcome for patients after radiation and treatment with temozolomide, an alkylating cytotoxic drug [69,70]. In esophageal cancer, decreased DNA methylation of nine selected genes was found in tumors responding to combined radio- and chemotherapy compared to non-responders [71]. The identified genes included MGMT, cell cycle regulators p16 and p57 and runt-related transcription factor 3 (RUNX-3) [71]. In addition, a recent study demonstrated a significant association between esophageal carcinoma response to definitive chemoradiation and promoter methylation of the zinc finger protein 695 (ZNF695) gene coding for a protein with a not yet well characterized function [72]. Siegel and colleagues examined the DNA methylation status of patients with locally advanced anal carcinoma prior to radiochemotherapy. Patients were stratified into a low risk or a high risk group on the basis of clinical parameters including tumor size and lymph node involvement. The high risk group, which had a significantly reduced overall and disease-free survival, had an increased promotor methylation of seven genes compared to the low risk group [73]. Because most of these studies evaluated the epigenetic modifications only before treatment, changes due to radiation or chemotherapy, which might inform how to adapt treatment based on tumor response, were not taken into account.
Analysis of breast cancer biopsies taken before radiotherapy and after exposure to 10 – 24 Gy showed that the DNA methylation status of genes involved in the immune response could be modulated by irradiation [74]. While DNA methylation in five genes prior to radiotherapy and in six genes after irradiation could be identified as prognostic markers, only two genes were present in both groups, indicating high radiation-induced variability [74]. So, much remains to be done to examine the impact of methylation status on cellular function.
Like promoter methylation, specific histone modifications have also been linked to treatment outcome and tumor response of patients with different cancer types [75–77]. In pancreatic carcinoma, high levels of dimethylated (H3K4me2) or acetylated histone 3 (H3K18ac) are associated with better survival after adjuvant radiochemotherapy, independent of other clinical factors [75]. Similarly, H3K4me2 expression in prostate cancer or NSCLC was low in patients with poor overall and disease-free survival, indicating that histone methylation might be a promising prognostic marker in different tumor entities [76,77].
The use of transcriptomic data to clarify molecular processes and to find suitable drug targets
In contrast to genomic analysis, which is more stable and therefore mainly used to assess the mutational status of cancer cells prior to therapy or when the tumor becomes resistant, gene transcription is a highly dynamic process. To determine the mRNA expression levels of targets at the beginning of the treatment and during therapy is critical for precision medicine. The transcriptome is divided into coding and non-coding RNA. Coding RNA is translated into proteins, while non-coding RNA, including micro RNA (miRNA), long non-coding RNA (lncRNA) and others, is considered to have a regulatory function [78,79]. As non-coding RNA affects the sensitivity to ionizing radiation or chemotherapy, it can also serve as a potential drug target to increase therapy response. [24,80–84].
Both coding and non-coding RNA expression levels have been analyzed in tumors to predict treatment response and clinical outcome [85–87]. Wong and colleagues examined the mRNA expression profiles of patients with cervical cancer prior to radiotherapy to find differences between radiosensitive and radioresistant tumors. Patient stratification into each group was based on clinical outcome and survival time. In radioresistant cancer samples for example, several genes coding for transcription factors, immune modulators or proteins involved in cytoskeletal organization were upregulated [85].
In patients with pancreatic cancer receiving adjuvant chemotherapy or chemoradiation after surgery, low expression of the miRNA, miR-21, was shown to be a negative prognostic marker in tumor tissue [86].
As RNA levels can change upon exposure to ionizing radiation or chemotherapy, analysis of the transcriptome during and after treatment is essential to understand resistance mechanisms and monitor expression of possible therapeutic targets [6,7,10]. A study in patients with rectal carcinoma examining the effects of radio-chemotherapy on mRNA levels in normal and malignant tissue showed a differential expression of genes involved in cell adhesion and leukocyte migration [87]. In line with these results, a specific gene cluster, including cell adhesion proteins and molecules involved in apoptosis is upregulated in cervical cancer after chemoradiation, while expression of cell cycle regulators is reduced [88]. Changes in transcription after treatment can also provide information about the therapeutic efficacy of molecular compounds. The clinical response to cetuximab and chemoradiation on gene expression was evaluated in patients with rectal carcinoma [89]. The authors observed a prolonged disease-free survival when EGFR was upregulated after treatment.
Few studies examined the expression of lncRNA in cancer samples [90,91]. Prensner and colleagues found an increased level of the lncRNA SChLAP1 in metastatic prostate cancer compared to patients with localized disease. Additionally, a high SChLAP1 expression was an independent negative predictive marker and correlated with reduced overall and disease-free survival [90]. In NSCLC, low levels of the lncRNA SPRY4-IT1 are associated with advanced tumor stage, lymph node infiltration and poor prognosis, while overexpression of SPRY4-IT1 in vitro leads to growth arrest and apoptosis [91]. The exact molecular mechanisms of lncRNA in the regulation of cell death and survival, however, are not yet fully understood.
Monitoring the expression of molecular targets during therapy is another important application of transcriptomic analysis. On the one hand, as transcription can be modulated by radiation, downregulation of the target could attenuate the efficacy of molecular drugs. On the other hand, radiotherapy might be used to enhance the expression of specific molecules and enabling in this way innovative molecular targeting approaches. When analyzing the transcriptome in tumor cells and biopsies to identify new promising targets for radiation oncology, both the radiation dose and the fractionation regimen have to be taken into account as these factors can strongly influence RNA expression [6,7,10].
In summary, transcriptomic analysis is an important tool for the examination of molecular processes in cancer cells. The assays can be performed with small tumor samples, for example, biopsies and potentially circulating cancer cells in the blood, and are relatively cost and time efficient. These techniques, therefore, have great potential for optimizing personalized cancer therapy.
Proteome and phosphoproteome analysis in revealing bypass and resistance mechanisms
Expression and functionality of target molecules have a critical impact on the efficacy of molecular therapeutics. In particular, the effect of kinase inhibitors can be modulated by the enzymatic activity status of the target, which is often controlled by post-translational modifications, such as protein phosphorylation. As mRNA levels do not necessarily correlate with protein expression due to other regulatory processes, including translation and protein degradation, proteomic and phosphoproteomic profiling of cancer cells can give valuable information about the complex cellular signaling network [92].
A recent study showed that specific phosphoproteins were upregulated in HNSCC tumors compared to normal mucosa [93]. The activated pathways included checkpoint signaling, regulators of translation and MAPK-associated molecules. Reduced phosphorylation of ErbB3 was found in undifferentiated tumors, while perineural invasion and lymph node metastasis, both negative prognostic markers, significantly correlated with low phosphorylated extracellular signal-regulated kinase (ERK) levels [93].
Rikova and colleagues examined the phosphoproteome in NSCLC patient samples and found different activation clusters of tyrosine kinases [94]. Some tumors expressed only one or two highly active kinases, while other tumors showed activated focal adhesion- or growth factor receptor-related signaling [94]. A correlation analysis with clinical parameters including treatment outcome or therapy resistance was not performed. In rectal carcinoma, phosphorylation of beta-Catenin and Chk2 was shown to be enhanced in tumors with a good response to neoadjuvant chemoradiation, while the GSK3beta phosphorylation level was decreased [95]. The authors only examined phosphorylation before therapy and did not take changes in phosphorylation into account, which occurred during treatment.
Despite the great potential of phosphoproteomic techniques for clarification of molecular processes, several limitations restrain their clinical application, especially in serial examinations. One critical factor is that, in comparison to RNA analysis, many proteomic assays require a relatively large amount of tissue to obtain valid results. Because sample sizes are often limited, as in the case of tumor biopsies, the extended application of proteomic analysis can be very challenging [92]. Moreover, protein phosphorylation is known to be volatile and susceptible to external factors such as temperature or mechanical stress. Therefore, differences in sample processing can compromise the results.
While the aforementioned factors impede the use of phosphoproteomic and proteomic profiling in the clinic, it has undoubtedly an important role in preclinical work. Several studies highlight the importance of the analysis of protein phosphorylation in elucidating the radio- and chemoresistance mechanisms and identifying promising drug combinations [6,30,31,96–103]. For example, a phosphoproteome array in HNSCC cells treated with cetuximab showed activation of the c-Jun N-terminal kinase (JNK) pathway which attenuated the efficacy of cetuximab itself [30]. In line with these findings, combined inhibition of EGFR and JNK significantly reduces radiation survival of HNSCC cells suggesting a promising approach to overcome drug resistance [30]. Similarly, targeting of beta1 integrin leads to enhanced phosphorylation of EGFR/MAPK associated signaling [31]. Dual inhibition of EGFR and beta1 integrin can significantly increase in vitro and in vivo cellular radiosensitivity, indicating the existence of molecular bypass mechanisms in cancer cells to avoid cell death after targeted therapy [31,100]. Phosphoproteomic analysis of human epidermal growth factor receptor 2 (HER2)-positive breast cancer cells showed that trastuzumab resistance could be promoted by activation of different prosurvival pathways including focal adhesion signaling and growth factor receptor-associated pathways. An siRNA-mediated knockdown of these activated proteins restored sensitivity to HER2 inhibition [103].
Although these data are highly interesting for clarifying the underlying resistance mechanisms, further studies in a broad patient population are needed to validate the clinical relevance of these results.
The emerging role of metabolomics in radiation oncology
Metabolism in tumor cells is often different from that in normal tissue. On the one hand this can be caused by intrinsic factors like mutational alterations of important enzymes or differential expression of molecules [33]; on the other hand, also extracellular factors, for example the tumor microenvironment, can have a critical impact on metabolic pathways and metabolite levels. Moreover, drug therapy and systemic diseases, like diabetes or hepatic failure, can affect the results of metabolomics assays. This susceptibility to interference further complicates the use of these techniques in the clinic. Nevertheless, integrative analysis of the tumor metabolome is indispensable for understanding the cellular phenotype and mechanisms of cancer cell resistance (Figure 1).
One example regarding the impact of cellular metabolite levels on tumor formation and progression is the mutation of the isocitrate dehydrogenase (IDH) [104]. IDH mutations found in glioma, chondrosarcoma and hematologic malignancies result in the accumulation of D-2-hydroxyglutarate which inhibits several enzymatic reactions involved in epigenetic modifications and cell signaling [105–108]. As the IDH mutation status is a strong predictor for patient outcome, non-invasive imaging of D-2-hydroxyglutarate with nuclear magnetic resonance spectroscopy could be used for risk stratification when genetic tumor profiling is not feasible [104,109–111]. Additionally, the development of therapeutics targeting only mutated IDH might be a promising approach for treatment of these tumors.
Recent studies have shown that metabolomic profiles can be used as prognostic markers in some cancers and also helps to identify new molecular targets [112–114]. In colorectal cancer patients, a specific expression pattern of 15 metabolites including lactate, cysteine and palmitoleate correlates with overall survival and tumor recurrence after surgery and chemotherapy [115]. In line with these results, the metabolome in breast cancer patients was found to be different in biopsies, based on prognostic criteria, like hormone receptor status, lymph node involvement and tumor stage [116,117]. Wibom and colleagues measured the extracellular level of multiple metabolites in glioblastoma and adjacent brain tissue in patients before and during radiotherapy using microdialysis catheter. While the glucose concentration was lower in the tumor compared with the surrounding normal tissue, the levels of several essential amino acids were increased [32]. After radiation, some metabolites, like alanine and inositol, were upregulated solely in malignant tissue. In contrast, normal brain tissue showed radiation-induced expression of arabitol and pentonic acid.
Although blood samples of cancer patients have also been used to analyze the metabolic changes during cancer therapy, there is a wide variation, even in healthy subjects, making the data interpretation more challenging [118,119]. Despite this variability, an increase in serum octanoylcarnitine and decanoylcarnitine levels during and after radiochemotherapy was observed in patients with esophageal cancer who responded to treatment [118]. Similarly, patients with nasopharyngeal carcinoma were divided into prognostic groups based on the metabolic profile of serum samples during radiotherapy [119].
Overall, evaluation of the metabolome is a novel, promising field. Elucidation of metabolic processes in cancer cells after treatment can help to identify resistance mechanisms and promising targets for molecular therapy.
Conclusion
Omics-based technologies greatly improved our understanding of the complex molecular mechanisms in cancer cells (Figure 2). The discovery of cancer-driving mutations enabled the development of molecular targeted drugs, while the expression profiles of RNA and proteins have already been used to predict treatment outcome and identify patients with high risk for treatment failure. Additionally, understanding the functional abnormalities in the pathways could be used for treatment selection and understanding adaptation and survival of cancer cells during and after therapy.
Figure 2. Omics-based analysis methods and the associated cell processes.
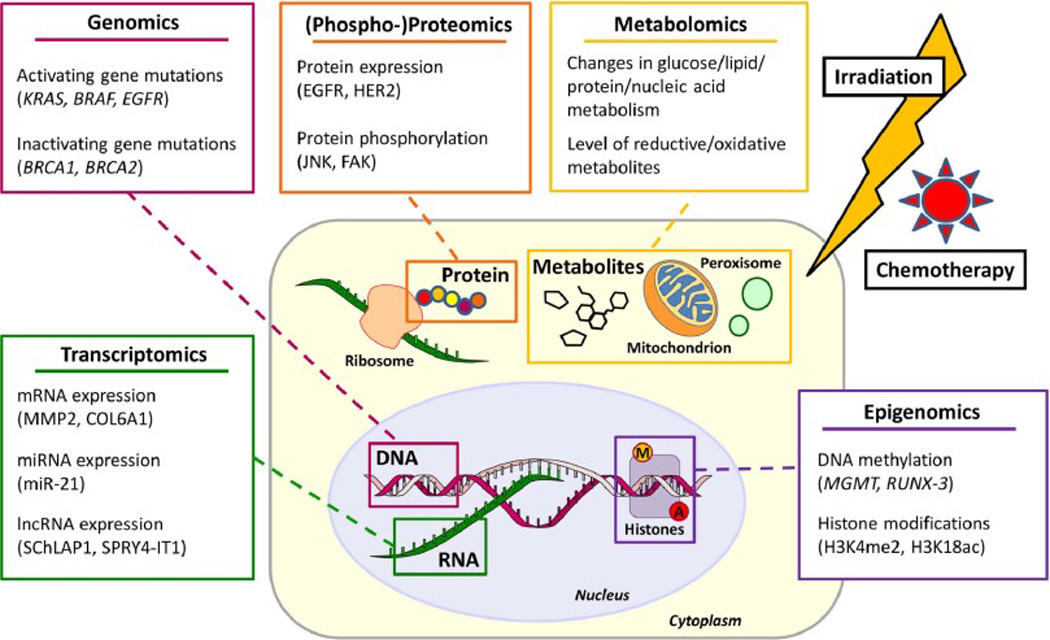
Genomic (activating and inactivating mutations), epigenomic (DNA methylation and histone modifications), transcriptomic (mRNA, miRNA, lncRNA expression), proteomic (protein expression and phosphorylation) and metabolomics (metabolites) analysis is used to clarify resistance mechanisms in tumors. On the one hand, molecular tumor characteristics are used to predict sensitivity to radio-chemotherapy (MGMT promotor methylation, miR-21 or HER2 expression); on the other hand, existing molecular differences between tumor and normal cells are exploited to target malignant cells more specifically (EGFR, BRAF or BRCA mutations).
Some challenges exist, which complicate the clinical use of these new techniques. One major factor is intra-tumoral heterogeneity, with a range of differences in the expression of RNA, proteins and metabolites among sub-populations within the tumor. Consequently, in the evaluation of prognostic molecular profiles, this heterogeneity within one tumor can obscure potential correlations with survival or disease progression. Moreover, because expression patterns can be modulated by multiple external factors, patient comorbidities and the therapy itself, repetitive examinations are required to understand tumor response and adaptation. In recent years, circulating cancer cells or cell-free tumor DNA in the blood have been used for molecular profiling as so-called liquid biopsies [120,121]. These techniques have some advantages compared to conventional tissue biopsies. They are minimal-invasive and allow immediate detection of changes in cancer cells during treatment. Additionally, there is no need for tissue preservation such as formalin fixation, which modifies the DNA structure and therefore can interfere with correct genotyping of cancer cells [122]. Although several studies particularly in patients with advanced disease successfully implemented liquid biopsies for monitoring therapy resistance [123–126], some technical limitations can hinder the broad use in the clinic. To date, there is no standardized procedure for extraction and enrichment of tumor material from the blood. Moreover, the number of circulating cancer cells or DNA fragments can be very low in non-metastatic patients making the molecular analysis challenging [121]. There is also some uncertainty in whether malignant cells from all metastatic or primary sites are equally represented in the circulating fraction [121]. Nevertheless, liquid biopsies have a great potential, especially for cancer genomics and optimization of mutation-based tumor therapy.
Another important challenge for integrating omics-based methods in standard patient care is the large amount of data, demanding sophisticated evaluation techniques and integrative concepts [127]. There are new trial designs from NCI based on targeting particular mutations (Molecular Analysis for Therapy Choice [NCI-MATCH]) although it is likely that there will be confounding factors within the cell and its environment that impact response beyond the presence of a specific mutation. Appropriately sized randomized (or at least stratified) trials with appropriate biomarkers are warranted to show the clinical relevance of the laboratory data.
Given that radiation can induce an adaptive response which potentially modifies heterogeneity and affects drug efficacy, the role of radiation perhaps with new fractionation schedules, along with molecular-targeted and radio-chemotherapy may have an important impact on cancer cure as well as the potential for repurposing drugs already used in the clinical setting. Fortunately, with diagnostic technology and data processing speed increasingly becoming better and more affordable, the goal of precision medicine based on extensive molecular tumor profiling seems to be within reach, employing novel “big-data” analysis techniques, hypothesis-based trials and mechanism-based assessments of the results.
Highlights.
Tumor cell resistance to chemoradiation and targeted drugs affects patient outcome
Novel techniques can be used to stratify patients and predict therapy efficacy
Radiation can modulate target expression and improve efficacy of targeted therapy
Development of personalized treatment strategies enables precision medicine
Acknowledgments
This study was supported by the NIH Intramural Research Program, National Cancer Institute, Center for Cancer Research. The authors thank the NIH Fellows Editorial Board for editorial assistance and Katherine Wilsdon (NCI, NIH) for critical reading and discussion of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors declare no conflicts of interest.
References
- 1.Bernier J, Hall EJ, Giaccia A. Radiation oncology: a century of achievements. Nat. Rev. Cancer. 2004;4:737–747. doi: 10.1038/nrc1451. [DOI] [PubMed] [Google Scholar]
- 2.Morris ZS, Harari PM. Interaction of radiation therapy with molecular targeted agents. J. Clin. Oncol. 2014;32:2886–2893. doi: 10.1200/JCO.2014.55.1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 4.Fraser M, Berlin A, Bristow RG, van der Kwast T. Genomic, pathological, and clinical heterogeneity as drivers of personalized medicine in prostate cancer. Urol. Oncol. 2015;33:85–94. doi: 10.1016/j.urolonc.2013.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Bristow RG, Berlin A, Dal Pra A. An arranged marriage for precision medicine: hypoxia and genomic assays in localized prostate cancer radiotherapy. Br. J. Radiol. 2014;87:20130753. doi: 10.1259/bjr.20130753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makinde AY, John-Aryankalayil M, Palayoor ST, Cerna D, Coleman CN. Radiation survivors: understanding and exploiting the phenotype following fractionated radiation therapy. Mol. Cancer Res. 2013;11:5–12. doi: 10.1158/1541-7786.MCR-12-0492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.John-Aryankalayil M, Palayoor ST, Cerna D, Simone CB, Falduto MT, Magnuson SR, et al. Fractionated radiation therapy can induce a molecular profile for therapeutic targeting. Radiat. Res. 2010;174:446–458. doi: 10.1667/RR2105.1. [DOI] [PubMed] [Google Scholar]
- 8.John-Aryankalayil M, Palayoor ST, Makinde AY, Cerna D, Simone CB, Falduto MT, et al. Fractionated radiation alters oncomir and tumor suppressor miRNAs in human prostate cancer cells. Radiat. Res. 2012;178:105–117. doi: 10.1667/rr2703.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coleman CN. Linking radiation oncology and imaging through molecular biology (or now that therapy and diagnosis have separated, it’s time to get together again!) Radiology. 2003;228:29–35. doi: 10.1148/radiol.2281021567. [DOI] [PubMed] [Google Scholar]
- 10.Aryankalayil MJ, Makinde AY, Gameiro SR, Hodge JW, Rivera-Solis PP, Palayoor ST, et al. Defining molecular signature of pro-immunogenic radiotherapy targets in human prostate cancer cells. Radiat. Res. 2014;182:139–148. doi: 10.1667/RR13731.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palayoor ST, John-Aryankalayil M, Makinde AY, Falduto MT, Magnuson SR, Coleman CN. Differential expression of stress and immune response pathway transcripts and miRNAs in normal human endothelial cells subjected to fractionated or single-dose radiation. Mol. Cancer Res. 2014;12:1002–1015. doi: 10.1158/1541-7786.MCR-13-0623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2015;373:1627–1639. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N. Engl. J. Med. 2015;373:23–34. doi: 10.1056/NEJMoa1504030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crittenden M, Kohrt H, Levy R, Jones J, Camphausen K, Dicker A, et al. Current clinical trials testing combinations of immunotherapy and radiation. Semin. Radiat. Oncol. 2015;25:54–64. doi: 10.1016/j.semradonc.2014.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mellor AL, Keskin DB, Johnson T, Chandler P, Munn DH. Cells expressing indoleamine 2,3-dioxygenase inhibit T cell responses. J. Immunol. 2002;168:3771–3776. doi: 10.4049/jimmunol.168.8.3771. [DOI] [PubMed] [Google Scholar]
- 16.Löb S, Königsrainer A, Zieker D, Brücher BLDM, Rammensee H-G, Opelz G, et al. IDO1 and IDO2 are expressed in human tumors: levo- but not dextro-1-methyl tryptophan inhibits tryptophan catabolism. Cancer Immunol. Immunother. 2009;58:153–157. doi: 10.1007/s00262-008-0513-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer. 2012;12:252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kwon ED, Drake CG, Scher HI, Fizazi K, Bossi A, van den Eertwegh AJM, et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): a multicentre, randomised, double-blind, phase 3 trial. Lancet. Oncol. 2014;15:700–712. doi: 10.1016/S1470-2045(14)70189-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howbrook DN, van der Valk AM, O’Shaughnessy MC, Sarker DK, Baker SC, Lloyd AW. Developments in microarray technologies. Drug Discov. Today. 2003;8:642–651. doi: 10.1016/s1359-6446(03)02773-9. [DOI] [PubMed] [Google Scholar]
- 20.Lockhart DJ, Winzeler EA. Genomics, gene expression and DNA arrays. Nature. 2000;405:827–836. doi: 10.1038/35015701. [DOI] [PubMed] [Google Scholar]
- 21.Grada A, Weinbrecht K. Next-generation sequencing: methodology and application. J. Invest. Dermatol. 2013;133:e11. doi: 10.1038/jid.2013.248. [DOI] [PubMed] [Google Scholar]
- 22.Metzker ML. Sequencing technologies - the next generation. Nat. Rev. Genet. 2010;11:31–46. doi: 10.1038/nrg2626. [DOI] [PubMed] [Google Scholar]
- 23.England B, Huang T, Karsy M. Current understanding of the role and targeting of tumor suppressor p53 in glioblastoma multiforme. Tumour Biol. 2013;34:2063–2074. doi: 10.1007/s13277-013-0871-3. [DOI] [PubMed] [Google Scholar]
- 24.Balça-Silva J, Sousa Neves S, Gonçalves AC, Abrantes AM, Casalta-Lopes J, Botelho MF, et al. Effect of miR-34b overexpression on the radiosensitivity of non-small cell lung cancer cell lines. Anticancer Res. 2012;32:1603–1609. [PubMed] [Google Scholar]
- 25.Lalonde E, Ishkanian AS, Sykes J, Fraser M, Ross-Adams H, Erho N, et al. Tumour genomic and microenvironmental heterogeneity for integrated prediction of 5-year biochemical recurrence of prostate cancer: a retrospective cohort study. Lancet. Oncol. 2014;15:1521–1532. doi: 10.1016/S1470-2045(14)71021-6. [DOI] [PubMed] [Google Scholar]
- 26.de Jong MC, Ten Hoeve JJ, Grénman R, Wessels LF, Kerkhoven R, Te Riele H, et al. Pretreatment microRNA Expression Impacting on Epithelial-to-Mesenchymal Transition Predicts Intrinsic Radiosensitivity in Head and Neck Cancer Cell Lines and Patients. Clin. Cancer Res. 2015 doi: 10.1158/1078-0432.CCR-15-0454. [DOI] [PubMed] [Google Scholar]
- 27.Baschnagel A, Russo A, Burgan WE, Carter D, Beam K, Palmieri D, et al. Vorinostat enhances the radiosensitivity of a breast cancer brain metastatic cell line grown in vitro and as intracranial xenografts. Mol. Cancer Ther. 2009;8:1589–1595. doi: 10.1158/1535-7163.MCT-09-0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krauze AV, Myrehaug SD, Chang MG, Holdford DJ, Smith S, Shih J, et al. A phase II study of concurrent radiation therapy, temozolomide and the histone deacetylase inhibitor Valproic Acid for newly diagnosed patients with Glioblastoma. Int. J. Radiat. Oncol. 2015;92:986–992. doi: 10.1016/j.ijrobp.2015.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bauer JA, Chakravarthy AB, Rosenbluth JM, Mi D, Seeley EH, De Matos Granja-Ingram N, et al. Identification of markers of taxane sensitivity using proteomic and genomic analyses of breast tumors from patients receiving neoadjuvant paclitaxel and radiation. Clin. Cancer Res. 2010;16:681–690. doi: 10.1158/1078-0432.CCR-09-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eke I, Schneider L, Förster C, Zips D, Kunz-Schughart LA, Cordes N. EGFR/JIP-4/JNK2 signaling attenuates cetuximab-mediated radiosensitization of squamous cell carcinoma cells. Cancer Res. 2013;73:297–306. doi: 10.1158/0008-5472.CAN-12-2021. [DOI] [PubMed] [Google Scholar]
- 31.Eke I, Zscheppang K, Dickreuter E, Hickmann L, Mazzeo E, Unger K, et al. Simultaneous β1 integrin-EGFR Targeting and Radiosensitization of Human Head and Neck Cancer. J. Natl. Cancer Inst. 2015;107 doi: 10.1093/jnci/dju419. dju419–. [DOI] [PubMed] [Google Scholar]
- 32.Wibom C, Surowiec I, Mörén L, Bergström P, Johansson M, Antti H, et al. Metabolomic patterns in glioblastoma and changes during radiotherapy: a clinical microdialysis study. J. Proteome Res. 2010;9:2909–2919. doi: 10.1021/pr901088r. [DOI] [PubMed] [Google Scholar]
- 33.Shin S-Y, Fauman EB, Petersen A-K, Krumsiek J, Santos R, Huang J, et al. An atlas of genetic influences on human blood metabolites. Nat. Genet. 2014;46:543–550. doi: 10.1038/ng.2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yun C-H, Mengwasser KE, Toms AV, Woo MS, Greulich H, Wong K-K, et al. The T790M mutation in EGFR kinase causes drug resistance by increasing the affinity for ATP. Proc. Natl. Acad. Sci. U. S. A. 2008;105:2070–2075. doi: 10.1073/pnas.0709662105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chapman PB, Hauschild A, Robert C, Haanen JB, Ascierto P, Larkin J, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 2011;364:2507–2516. doi: 10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poulikakos PI, Persaud Y, Janakiraman M, Kong X, Ng C, Moriceau G, et al. RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E) Nature. 2011;480:387–390. doi: 10.1038/nature10662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lièvre A, Bachet J-B, Le Corre D, Boige V, Landi B, Emile J-F, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006;66:3992–3995. doi: 10.1158/0008-5472.CAN-06-0191. [DOI] [PubMed] [Google Scholar]
- 38.Zhou C, Wu Y-L, Chen G, Feng J, Liu X-Q, Wang C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet. Oncol. 2011;12:735–742. doi: 10.1016/S1470-2045(11)70184-X. [DOI] [PubMed] [Google Scholar]
- 39.Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11:21–28. doi: 10.1016/S1470-2045(09)70311-0. [DOI] [PubMed] [Google Scholar]
- 40.Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, et al. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 2006;354:567–578. doi: 10.1056/NEJMoa053422. [DOI] [PubMed] [Google Scholar]
- 41.Kripp M, Horisberger K, Mai S, Kienle P, Gaiser T, Post S, et al. Does the Addition of Cetuximab to Radiochemotherapy Improve Outcome of Patients with Locally Advanced Rectal Cancer? Long-Term Results from Phase II Trials. Gastroenterol. Res. Pract. 2015;2015:273489. doi: 10.1155/2015/273489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alberts SR, Sargent DJ, Nair S, Mahoney MR, Mooney M, Thibodeau SN, et al. Effect of oxaliplatin, fluorouracil, and leucovorin with or without cetuximab on survival among patients with resected stage III colon cancer: a randomized trial. JAMA. 2012;307:1383–1393. doi: 10.1001/jama.2012.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lynch TJ, Patel T, Dreisbach L, McCleod M, Heim WJ, Hermann RC, et al. Cetuximab and first-line taxane/carboplatin chemotherapy in advanced non-small-cell lung cancer: results of the randomized multicenter phase III trial BMS099. J. Clin. Oncol. 2010;28:911–917. doi: 10.1200/JCO.2009.21.9618. [DOI] [PubMed] [Google Scholar]
- 44.Di Nicolantonio F, Martini M, Molinari F, Sartore-Bianchi A, Arena S, Saletti P, et al. Wildtype BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J. Clin. Oncol. 2008;26:5705–5712. doi: 10.1200/JCO.2008.18.0786. [DOI] [PubMed] [Google Scholar]
- 45.Khambata-Ford S, Garrett CR, Meropol NJ, Basik M, Harbison CT, Wu S, et al. Expression of epiregulin and amphiregulin and K-ras mutation status predict disease control in metastatic colorectal cancer patients treated with cetuximab. J. Clin. Oncol. 2007;25:3230–3237. doi: 10.1200/JCO.2006.10.5437. [DOI] [PubMed] [Google Scholar]
- 46.Garrett C, Sahin I. Predicting cetuximab efficacy in patients with advanced colorectal cancer. Curr. Biomark. Find. 2014;4:61. [Google Scholar]
- 47.Bronte G, Silvestris N, Castiglia M, Galvano A, Passiglia F, Sortino G, et al. New findings on primary and acquired resistance to anti-EGFR therapy in metastatic colorectal cancer: do all roads lead to RAS? Oncotarget. 2015;6:24780–24796. doi: 10.18632/oncotarget.4959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dewdney A, Cunningham D, Tabernero J, Capdevila J, Glimelius B, Cervantes A, et al. Multicenter Randomized Phase II Clinical Trial Comparing Neoadjuvant Oxaliplatin, Capecitabine, and Preoperative Radiotherapy With or Without Cetuximab Followed by Total Mesorectal Excision in Patients With High-Risk Rectal Cancer (EXPERT-C) J. Clin. Oncol. 2012;30:1620–1627. doi: 10.1200/JCO.2011.39.6036. [DOI] [PubMed] [Google Scholar]
- 49.Maughan TS, Adams RA, Smith CG, Meade AM, Seymour MT, Wilson RH, et al. Addition of cetuximab to oxaliplatin-based first-line combination chemotherapy for treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet. 2011;377:2103–2114. doi: 10.1016/S0140-6736(11)60613-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim SY, Shim EK, Yeo HY, Baek JY, Hong YS, Kim DY, et al. KRAS mutation status and clinical outcome of preoperative chemoradiation with cetuximab in locally advanced rectal cancer: a pooled analysis of 2 phase II trials. Int. J. Radiat. Oncol. Biol. Phys. 2013;85:201–207. doi: 10.1016/j.ijrobp.2012.03.048. [DOI] [PubMed] [Google Scholar]
- 51.Giaccone G, Herbst RS, Manegold C, Scagliotti G, Rosell R, Miller V, et al. Gefitinib in combination with gemcitabine and cisplatin in advanced non-small-cell lung cancer: a phase III trial--INTACT 1. J. Clin. Oncol. 2004;22:777–784. doi: 10.1200/JCO.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 52.Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 53.Yang JC-H, Wu Y-L, Schuler M, Sebastian M, Popat S, Yamamoto N, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16:141–151. doi: 10.1016/S1470-2045(14)71173-8. [DOI] [PubMed] [Google Scholar]
- 54.Komaki R, Allen PK, Wei X, Blumenschein GR, Tang X, Lee JJ, et al. Adding Erlotinib to Chemoradiation Improves Overall Survival but Not Progression-Free Survival in Stage III Non-Small Cell Lung Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2015;92:317–324. doi: 10.1016/j.ijrobp.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Iyengar P, Kavanagh BD, Wardak Z, Smith I, Ahn C, Gerber DE, et al. Phase II trial of stereotactic body radiation therapy combined with erlotinib for patients with limited but progressive metastatic non-small-cell lung cancer. J. Clin. Oncol. 2014;32:3824–3830. doi: 10.1200/JCO.2014.56.7412. [DOI] [PubMed] [Google Scholar]
- 56.Lilenbaum R, Samuels M, Wang X, Kong FM, Jänne PA, Masters G, et al. A phase II study of induction chemotherapy followed by thoracic radiotherapy and erlotinib in poor-risk stage III non-small-cell lung cancer: results of CALGB 30605 (Alliance)/RTOG 0972 (NRG) J. Thorac. Oncol. 2015;10:143–147. doi: 10.1097/JTO.0000000000000347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cantwell-Dorris ER, O’Leary JJ, Sheils OM. BRAFV600E: implications for carcinogenesis and molecular therapy. Mol. Cancer Ther. 2011;10:385–394. doi: 10.1158/1535-7163.MCT-10-0799. [DOI] [PubMed] [Google Scholar]
- 58.Wagle N, Emery C, Berger MF, Davis MJ, Sawyer A, Pochanard P, et al. Dissecting therapeutic resistance to RAF inhibition in melanoma by tumor genomic profiling. J. Clin. Oncol. 2011;29:3085–3096. doi: 10.1200/JCO.2010.33.2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Satzger I, Degen A, Asper H, Kapp A, Hauschild A, Gutzmer R. Serious skin toxicity with the combination of BRAF inhibitors and radiotherapy. J. Clin. Oncol. 2013;31:e220–e222. doi: 10.1200/JCO.2012.44.4265. [DOI] [PubMed] [Google Scholar]
- 60.Joseph EW, Pratilas CA, Poulikakos PI, Tadi M, Wang W, Taylor BS, et al. The RAF inhibitor PLX4032 inhibits ERK signaling and tumor cell proliferation in a V600E BRAF-selective manner. Proc. Natl. Acad. Sci. U. S. A. 2010;107:14903–14908. doi: 10.1073/pnas.1008990107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anforth R, Fernandez-Peñas P, Long GV. Cutaneous toxicities of RAF inhibitors. Lancet. Oncol. 2013;14:e11–e18. doi: 10.1016/S1470-2045(12)70413-8. [DOI] [PubMed] [Google Scholar]
- 62.Farmer H, McCabe N, Lord CJ, Tutt ANJ, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–921. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 63.Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, Weitzel JN, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet (London, England) 2010;376:235–244. doi: 10.1016/S0140-6736(10)60892-6. [DOI] [PubMed] [Google Scholar]
- 64.Miki Y, Swensen J, Shattuck-Eidens D, Futreal P, Harshman K, Tavtigian S, et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science. 1994;266:66–71. doi: 10.1126/science.7545954. (80-.) [DOI] [PubMed] [Google Scholar]
- 65.Jones PA, Baylin SB. The epigenomics of cancer. Cell. 2007;128:683–692. doi: 10.1016/j.cell.2007.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smits KM, Melotte V, Niessen HEC, Dubois L, Oberije C, Troost EGC, et al. Epigenetics in radiotherapy: where are we heading? Radiother. Oncol. 2014;111:168–177. doi: 10.1016/j.radonc.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 67.Storch K, Eke I, Borgmann K, Krause M, Richter C, Becker K, et al. Three-dimensional cell growth confers radioresistance by chromatin density modification. Cancer Res. 2010;70:3925–3934. doi: 10.1158/0008-5472.CAN-09-3848. [DOI] [PubMed] [Google Scholar]
- 68.Camphausen K, Tofilon PJ. Inhibition of histone deacetylation: a strategy for tumor radiosensitization. J. Clin. Oncol. 2007;25:4051–4056. doi: 10.1200/JCO.2007.11.6202. [DOI] [PubMed] [Google Scholar]
- 69.Rivera AL, Pelloski CE, Gilbert MR, Colman H, De La Cruz C, Sulman EP, et al. MGMT promoter methylation is predictive of response to radiotherapy and prognostic in the absence of adjuvant alkylating chemotherapy for glioblastoma. Neuro. Oncol. 2010;12:116–121. doi: 10.1093/neuonc/nop020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJB, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet. Oncol. 2009;10:459–466. doi: 10.1016/S1470-2045(09)70025-7. [DOI] [PubMed] [Google Scholar]
- 71.Hamilton JP, Sato F, Greenwald BD, Suntharalingam M, Krasna MJ, Edelman MJ, et al. Promoter methylation and response to chemotherapy and radiation in esophageal cancer. Clin. Gastroenterol. Hepatol. 2006;4:701–708. doi: 10.1016/j.cgh.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 72.Takahashi T, Yamahsita S, Matsuda Y, Kishino T, Nakajima T, Kushima R, et al. ZNF695 methylation predicts a response of esophageal squamous cell carcinoma to definitive chemoradiotherapy. J. Cancer Res. Clin. Oncol. 2015;141:453–463. doi: 10.1007/s00432-014-1841-x. [DOI] [PubMed] [Google Scholar]
- 73.Siegel EM, Eschrich S, Winter K, Riggs B, Berglund A, Ajidahun A, et al. Epigenomic characterization of locally advanced anal cancer: a radiation therapy oncology group 98-11 specimen study. Dis. Colon Rectum. 2014;57:941–957. doi: 10.1097/DCR.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Halvorsen AR, Helland Å, Fleischer T, Haug KM, Grenaker Alnaes GI, Nebdal D, et al. Differential DNA methylation analysis of breast cancer reveals the impact of immune signaling in radiation therapy. Int. J. Cancer. 2014;135:2085–2095. doi: 10.1002/ijc.28862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Manuyakorn A, Paulus R, Farrell J, Dawson NA, Tze S, Cheung-Lau G, et al. Cellular Histone Modification Patterns Predict Prognosis and Treatment Response in Resectable Pancreatic Adenocarcinoma: Results From RTOG 9704. J. Clin. Oncol. 2010;28:1358–1365. doi: 10.1200/JCO.2009.24.5639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Barlési F, Giaccone G, Gallegos-Ruiz MI, Loundou A, Span SW, Lefesvre P, et al. Global histone modifications predict prognosis of resected non small-cell lung cancer. J. Clin. Oncol. 2007;25:4358–4364. doi: 10.1200/JCO.2007.11.2599. [DOI] [PubMed] [Google Scholar]
- 77.Seligson DB, Horvath S, Shi T, Yu H, Tze S, Grunstein M, et al. Global histone modification patterns predict risk of prostate cancer recurrence. Nature. 2005;435:1262–1266. doi: 10.1038/nature03672. [DOI] [PubMed] [Google Scholar]
- 78.Mercer TR, Dinger ME, Mattick JS. Long non-coding RNAs: insights into functions. Nat. Rev. Genet. 2009;10:155–159. doi: 10.1038/nrg2521. [DOI] [PubMed] [Google Scholar]
- 79.He L, Hannon GJ. MicroRNAs: small RNAs with a big role in gene regulation. Nat. Rev. Genet. 2004;5:522–531. doi: 10.1038/nrg1379. [DOI] [PubMed] [Google Scholar]
- 80.Josson S, Sung S-Y, Lao K, Chung LWK, Johnstone PAS. Radiation modulation of microRNA in prostate cancer cell lines. Prostate. 2008;68:1599–1606. doi: 10.1002/pros.20827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Czochor JR, Glazer PM. microRNAs in cancer cell response to ionizing radiation. Antioxid. Redox Signal. 2014;21:293–312. doi: 10.1089/ars.2013.5718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bader AG, Brown D, Stoudemire J, Lammers P. Developing therapeutic microRNAs for cancer. Gene Ther. 2011;18:1121–1126. doi: 10.1038/gt.2011.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pan B, Feng B, Chen Y, Huang G, Wang R, Chen L, et al. MiR-200b regulates autophagy associated with chemoresistance in human lung adenocarcinoma. Oncotarget. 2015 doi: 10.18632/oncotarget.5352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maachani UB, Tandle A, Shankavaram U, Kramp T, Camphausen K. Modulation of miR-21 signaling by MPS1 in human glioblastoma. Oncotarget. 2015 doi: 10.18632/oncotarget.4143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wong YF, Selvanayagam ZE, Wei N, Porter J, Vittal R, Hu R, et al. Expression genomics of cervical cancer: molecular classification and prediction of radiotherapy response by DNA microarray. Clin. Cancer Res. 2003;9:5486–5492. [PubMed] [Google Scholar]
- 86.Hwang J-H, Voortman J, Giovannetti E, Steinberg SM, Leon LG, Kim Y-T, et al. Identification of microRNA-21 as a biomarker for chemoresistance and clinical outcome following adjuvant therapy in resectable pancreatic cancer. PLoS One. 2010;5:e10630. doi: 10.1371/journal.pone.0010630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Snipstad K, Fenton CG, Kjaeve J, Cui G, Anderssen E, Paulssen RH. New specific molecular targets for radio-chemotherapy of rectal cancer. Mol. Oncol. 2010;4:52–64. doi: 10.1016/j.molonc.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zempolich K, Fuhrman C, Milash B, Flinner R, Greven K, Ryu J, et al. Changes in gene expression induced by chemoradiation in advanced cervical carcinoma: a microarray study of RTOG C-0128. Gynecol. Oncol. 2008;109:275–279. doi: 10.1016/j.ygyno.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 89.Debucquoy A, Haustermans K, Daemen A, Aydin S, Libbrecht L, Gevaert O, et al. Molecular response to cetuximab and efficacy of preoperative cetuximab-based chemoradiation in rectal cancer. J. Clin. Oncol. 2009;27:2751–2757. doi: 10.1200/JCO.2008.18.5033. [DOI] [PubMed] [Google Scholar]
- 90.Prensner JR, Zhao S, Erho N, Schipper M, Iyer MK, Dhanasekaran SM, et al. RNA biomarkers associated with metastatic progression in prostate cancer: a multi-institutional high-throughput analysis of SChLAP1. Lancet Oncol. 2014;15:1469–1480. doi: 10.1016/S1470-2045(14)71113-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sun M, Liu X-H, Lu K-H, Nie F-Q, Xia R, Kong R, et al. EZH2-mediated epigenetic suppression of long noncoding RNA SPRY4-IT1 promotes NSCLC cell proliferation and metastasis by affecting the epithelial-mesenchymal transition. Cell Death Dis. 2014;5:e1298. doi: 10.1038/cddis.2014.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wulfkuhle JD, Edmiston KH, Liotta LA, Petricoin EF. Technology insight: pharmacoproteomics for cancer--promises of patient-tailored medicine using protein microarrays. Nat. Clin. Pract. Oncol. 2006;3:256–268. doi: 10.1038/ncponc0485. [DOI] [PubMed] [Google Scholar]
- 93.Frederick MJ, VanMeter AJ, Gadhikar MA, Henderson YC, Yao H, Pickering CC, et al. Phosphoproteomic analysis of signaling pathways in head and neck squamous cell carcinoma patient samples. Am. J. Pathol. 2011;178:548–571. doi: 10.1016/j.ajpath.2010.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rikova K, Guo A, Zeng Q, Possemato A, Yu J, Haack H, et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell. 2007;131:1190–1203. doi: 10.1016/j.cell.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 95.Mammano E, Galdi F, Pierobon M, Tessari E, Deng J, Pucciarelli S, et al. Multiplexed protein signal pathway mapping identifies patients with rectal cancer that responds to neoadjuvant treatment. Clin. Colorectal Cancer. 2012;11:268–274. doi: 10.1016/j.clcc.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zakharchenko O, Cojoc M, Dubrovska A, Souchelnytskyi S. A role of TGFβ1 dependent 14-3-3σ phosphorylation at Ser69 and Ser74 in the regulation of gene transcription, stemness and radioresistance. PLoS One. 2013;8:e65163. doi: 10.1371/journal.pone.0065163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee BY, Hochgräfe F, Lin H-M, Castillo L, Wu J, Raftery MJ, et al. Phosphoproteomic profiling identifies focal adhesion kinase as a mediator of docetaxel resistance in castrate-resistant prostate cancer. Mol. Cancer Ther. 2014;13:190–201. doi: 10.1158/1535-7163.MCT-13-0225-T. [DOI] [PubMed] [Google Scholar]
- 98.Yoshida T, Zhang G, Smith MA, Lopez AS, Bai Y, Li J, et al. Tyrosine phosphoproteomics identifies both codrivers and cotargeting strategies for T790M-related EGFR-TKI resistance in non-small cell lung cancer. Clin. Cancer Res. 2014;20:4059–4074. doi: 10.1158/1078-0432.CCR-13-1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Myllynen L, Kwiatkowski M, Gleißner L, Riepen B, Hoffer K, Wurlitzer M, et al. Quantitative proteomics unveiled: Regulation of DNA double strand break repair by EGFR involves PARP1. Radiother. Oncol. 2015 doi: 10.1016/j.radonc.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 100.Eke I, Storch K, Krause M, Cordes N. Cetuximab attenuates its cytotoxic and radiosensitizing potential by inducing fibronectin biosynthesis. Cancer Res. 2013;73:5869–79. doi: 10.1158/0008-5472.CAN-13-0344. [DOI] [PubMed] [Google Scholar]
- 101.Eke I, Deuse Y, Hehlgans S, Gurtner K, Krause M, Baumann M, et al. β1 Integrin/FAK/cortactin signaling is essential for human head and neck cancer resistance to radiotherapy. J. Clin. Invest. 2012;122:1529–1540. doi: 10.1172/JCI61350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lee D-H, Goodarzi AA, Adelmant GO, Pan Y, Jeggo PA, Marto JA, et al. Phosphoproteomic analysis reveals that PP4 dephosphorylates KAP-1 impacting the DNA damage response. EMBO J. 2012;31:2403–2415. doi: 10.1038/emboj.2012.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Boyer AP, Collier TS, Vidavsky I, Bose R. Quantitative proteomics with siRNA screening identifies novel mechanisms of trastuzumab resistance in HER2 amplified breast cancers. Mol. Cell. Proteomics. 2013;12:180–193. doi: 10.1074/mcp.M112.020115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cairns RA, Mak TW. Oncogenic isocitrate dehydrogenase mutations: mechanisms, models, and clinical opportunities. Cancer Discov. 2013;3:730–741. doi: 10.1158/2159-8290.CD-13-0083. [DOI] [PubMed] [Google Scholar]
- 105.Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, Chen K, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N. Engl. J. Med. 2009;361:1058–1066. doi: 10.1056/NEJMoa0903840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Parsons DW, Jones S, Zhang X, Lin JC-H, Leary RJ, Angenendt P, et al. An integrated genomic analysis of human glioblastoma multiforme. Science. 2008;321:1807–1812. doi: 10.1126/science.1164382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Turcan S, Rohle D, Goenka A, Walsh LA, Fang F, Yilmaz E, et al. IDH1 mutation is sufficient to establish the glioma hypermethylator phenotype. Nature. 2012;483:479–483. doi: 10.1038/nature10866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Chowdhury R, Yeoh KK, Tian Y-M, Hillringhaus L, Bagg EA, Rose NR, et al. The oncometabolite 2-hydroxyglutarate inhibits histone lysine demethylases. EMBO Rep. 2011;12:463–469. doi: 10.1038/embor.2011.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zeng A, Hu Q, Liu Y, Wang Z, Cui X, Li R, et al. IDH1/2 mutation status combined with Ki-67 labeling index defines distinct prognostic groups in glioma. Oncotarget. 2015;6:30232–30238. doi: 10.18632/oncotarget.4920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Choi C, Ganji SK, DeBerardinis RJ, Hatanpaa KJ, Rakheja D, Kovacs Z, et al. 2-hydroxyglutarate detection by magnetic resonance spectroscopy in IDH-mutated patients with gliomas. Nat. Med. 2012;18:624–629. doi: 10.1038/nm.2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.DiNardo CD, Propert KJ, Loren AW, Paietta E, Sun Z, Levine RL, et al. Serum 2-hydroxyglutarate levels predict isocitrate dehydrogenase mutations and clinical outcome in acute myeloid leukemia. Blood. 2013;121:4917–4924. doi: 10.1182/blood-2013-03-493197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Spratlin JL, Serkova NJ, Eckhardt SG. Clinical applications of metabolomics in oncology: a review. Clin. Cancer Res. 2009;15:431–440. doi: 10.1158/1078-0432.CCR-08-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kim K, Yeo S-G, Yoo BC. Identification of hypoxanthine and phosphoenolpyruvic Acid as serum markers of chemoradiotherapy response in locally advanced rectal cancer. Cancer Res. Treat. 2015;47:78–89. doi: 10.4143/crt.2013.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mörén L, Bergenheim AT, Ghasimi S, Brännström T, Johansson M, Antti H. Metabolomic Screening of Tumor Tissue and Serum in Glioma Patients Reveals Diagnostic and Prognostic Information. Metabolites. 2015;5:502–520. doi: 10.3390/metabo5030502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Qiu Y, Cai G, Zhou B, Li D, Zhao A, Xie G, et al. A distinct metabolic signature of human colorectal cancer with prognostic potential. Clin. Cancer Res. 2014;20:2136–2146. doi: 10.1158/1078-0432.CCR-13-1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Giskeødegård GF, Grinde MT, Sitter B, Axelson DE, Lundgren S, Fjøsne HE, et al. Multivariate modeling and prediction of breast cancer prognostic factors using MR metabolomics. J. Proteome Res. 2010;9:972–979. doi: 10.1021/pr9008783. [DOI] [PubMed] [Google Scholar]
- 117.Budczies J, Brockmöller SF, Müller BM, Barupal DK, Richter-Ehrenstein C, Kleine-Tebbe A, et al. Comparative metabolomics of estrogen receptor positive and estrogen receptor negative breast cancer: alterations in glutamine and beta-alanine metabolism. J. Proteomics. 2013;94:279–288. doi: 10.1016/j.jprot.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 118.Xu J, Chen Y, Zhang R, Song Y, Cao J, Bi N, et al. Global and Targeted Metabolomics of Esophageal Squamous Cell Carcinoma Discovers Potential Diagnostic and Therapeutic Biomarkers. Mol. Cell. Proteomics. 2013;12:1306–1318. doi: 10.1074/mcp.M112.022830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yi L, Song C, Hu Z, Yang L, Xiao L, Yi B, et al. A metabolic discrimination model for nasopharyngeal carcinoma and its potential role in the therapeutic evaluation of radiotherapy. Metabolomics. 2013;10:697–708. [Google Scholar]
- 120.Pantel K, Alix-Panabières C. Real-time liquid biopsy in cancer patients: fact or fiction? Cancer Res. 2013;73:6384–6388. doi: 10.1158/0008-5472.CAN-13-2030. [DOI] [PubMed] [Google Scholar]
- 121.Diaz LA, Bardelli A. Liquid biopsies: genotyping circulating tumor DNA. J. Clin. Oncol. 2014;32:579–586. doi: 10.1200/JCO.2012.45.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Quach N, Goodman MF, Shibata D. In vitro mutation artifacts after formalin fixation and error prone translesion synthesis during PCR. BMC Clin. Pathol. 2004;4:1. doi: 10.1186/1472-6890-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Taniguchi K, Uchida J, Nishino K, Kumagai T, Okuyama T, Okami J, et al. Quantitative detection of EGFR mutations in circulating tumor DNA derived from lung adenocarcinomas. Clin. Cancer Res. 2011;17:7808–7815. doi: 10.1158/1078-0432.CCR-11-1712. [DOI] [PubMed] [Google Scholar]
- 124.Murtaza M, Dawson S-J, Tsui DWY, Gale D, Forshew T, Piskorz AM, et al. Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature. 2013;497:108–112. doi: 10.1038/nature12065. [DOI] [PubMed] [Google Scholar]
- 125.Carpinetti P, Donnard E, Bettoni F, Asprino P, Koyama F, Rozanski A, et al. The use of personalized biomarkers and liquid biopsies to monitor treatment response and disease recurrence in locally advanced rectal cancer after neoadjuvant chemoradiation. Oncotarget. 2015;6:38360–38371. doi: 10.18632/oncotarget.5256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mohiuddin M, Ahmed MM, Venkatasubbarao K. c-Ki-ras mutations in peripheral blood of pancreatic cancer patients: A marker for early tumor metastasis. Int. J. Radiat. Oncol. 1996;34:161–166. doi: 10.1016/0360-3016(95)02004-7. [DOI] [PubMed] [Google Scholar]
- 127.Mak TD, Laiakis EC, Goudarzi M, Fornace AJ. Selective Paired Ion Contrast Analysis: A Novel Algorithm for Analyzing Postprocessed LC-MS Metabolomics Data Possessing High Experimental Noise. Anal. Chem. 2015;87:3177–3186. doi: 10.1021/ac504012a. [DOI] [PMC free article] [PubMed] [Google Scholar]


