Abstract
Objective
To better understand the impact of age at injury, severity of injury, and time since injury on long-term school outcomes of children with traumatic brain injury (TBI).
Participants
Four groups of children: complicated mild/moderate TBI (n=23), severe TBI (n=56), orthopedic injury (n=35), and healthy controls (n=42). Children with TBI were either two years post injury or six years post injury.
Design
Cross-sectional design
Measures
School records as well as parental ratings of functional academic skills and school competency.
Results
Children with severe TBI had consistently high usage of school services and low school competency ratings than children with orthopedic injuries and healthy controls. In contrast, children with complicated-mild/moderate TBI were significantly more likely to receive school support services and have lower competence ratings at six years than at two years post injury. Students injured at younger ages had lower functional academic skill ratings than those injured at older ages.
Conclusions
These findings highlight the increasing academic challenges faced over time by students with complicated-mild/moderate TBI and the vulnerability of younger children to poorer development of functional academic skills.
Keywords: traumatic brain injury, children, school outcomes, special education
Traumatic brain injury (TBI) is a leading cause of death and disability in childhood. Each year in the United States, approximately 475,000 children under the age of 14 years sustain a TBI1 and approximately 30,000 have long-term disabilities2. TBI is viewed as a chronic disease process that initiates ongoing and possibly lifelong changes that affect multiple organ systems3. Common consequences of moderate to severe pediatric TBI include chronic, often lifelong, impairments in cognition, psychological health, adaptive behavior, and academic functioning. Academic functioning is particularly important to health related quality of life because mastering the school curriculum is one of the major developmental tasks of childhood. Functional academic deficits often emerge long-term following significant TBI and are characterized by poor school performance, high rates of grade retention, and receipt of special academic support services4, 5. In this paper, we examine long-term academic outcomes in children with a range of TBI severity using a prospective, multidimensional approach.
Time Since Injury, Severity of TBI, and Age at Injury
Academic deficits, which are among the most significant and pervasive areas of difficulty after pediatric TBI, are influenced by injury-related variables such as the time since injury, severity of injury, and age at injury. During the initial six months after TBI, core academic skills are commonly reduced in children with a wide range of injury severity. Difficulties have been reported in virtually all academic areas evaluated, including reading, mathematics, and written language in children with TBI as compared to children with orthopedic injuries or healthy children6–8. Although some initial improvement in core academic skills typically occurs during the first 6 to 12 months after injury, longitudinal studies indicate a persistent deficit in academic skills from one to five years post-injury4, 5, 9. Although children with TBI develop new skills, these skills develop more slowly and often do not catch up to skills of healthy children. Parent and teacher ratings of academic competence also indicate significant long-term reduction in everyday academic performance4, 10–12.
In addition to disruption of core academic skills, greater injury severity is associated with increased initiation of school support services10. Ewing-Cobbs and colleagues4 found that only 21% of severely injured school-aged children and adolescents received a regular education curriculum and were promoted each year despite most having generally average achievement scores. In a recent one year follow-up study, 45% of children with moderate and severe TBI and 6% of children with mild TBI group received new school support services under federal statutes13. Glang and colleagues14 found 25% of school-aged students with mild-moderate and severe TBI received formal special education services upon return to school and that another 41% received informal school supports. At an extended follow-up four years after injury, special education services were received in 50% of children with severe TBI, 14% of children with moderate TBI and 10% of children with orthopedic injuries12. Informal academic accommodations were provided for an additional 31 to 62 percent of the same groups12. These rates of new educational support services are very high, particularly in light of the view in the educational community that TBI is a low-incidence disability.15, 16
Very little is known about the impact of age at injury on academic outcomes. Young age at injury does not appear to confer any advantage relative to older age at injury for either academic skill development or functional academic performance. Infants and toddlers who sustained moderate to severe TBI and were followed for 5 to 8 years after injury showed significantly lower reading and math scores relative to a healthy comparison group. Nearly 50% of the injured children had been retained and/or required placement in self-contained special education classrooms. The odds of unfavorable academic performance were 18 times higher for young children with TBI than for healthy comparison children6. In children ages 3 to 6 years at injury, severe TBI was associated with lower scores than moderate TBI and orthopedic injury groups on measures of applied mathematical reasoning and school readiness at both post-acute and 1 year follow-up evaluations7, 8.
Academic Support Services after TBI
Two different laws regulate receipt of academic services. In 1990, reauthorization of the Individuals with Disabilities Education Act specifically mandated TBI as a qualifying condition for receipt of a free and appropriate public education. Despite this federal mandate, relatively few students are served under this qualifying condition. The majority who do receive services had relatively severe injuries and received hospital-school transition supports14. The second law, Section 504 of the Rehabilitation Act of 1973, is civil rights legislation requiring schools to eliminate barriers that prevent students from full participation in the general curriculum. Section 504 protects students who have a disability, have a record of disability, or are treated as having a disability from discrimination. Section 504 does not require either assessment of suspected areas of disability or a structured educational plan and there are fewer protections and procedural safeguards. Despite the provision of formal and informal educational supports, many children with TBI have serious functional deficits in everyday performance that limit educational attainment, psychological adjustment, and eventual vocational opportunities.
Rationale and Hypotheses
Although it appears that long-term school outcome for children with complicated-mild, moderate and severe TBI is unfavorable, it is unclear whether children injured in infancy or early childhood fare worse than those injured during school age or adolescence. This study sought to better understand the impact of age at injury, severity of injury, and time since injury on long-term school outcomes by including children injured in infancy and early childhood as well as those injured in later childhood and adolescence. This study is the first to compare school outcome of children injured in early childhood to those injured in later childhood and adolescence. Because of this wide span of age at injury (from 2 months to 15 years), children from two different age at injury cohorts were recruited for this study. To better delineate school outcomes, academic records were obtained directly from the children’s school. In addition to school records, academic functioning was assessed through parental ratings of functional academic skills and school competency. School outcomes for children with TBI were compared to school outcomes for children with orthopedic injuries as well as healthy children from the community. We hypothesized that children with severe TBI, injured at young ages would have higher rates of school support services and lower academic competencies.
METHODS
Participants
Participants in this study included four groups of children: complicated -mild/moderate TBI, severe TBI, orthopedic injuries, and healthy children from the community. All participants were recruited from one of two cohorts: a longitudinal study from 1994 to 1998 and a prospective study from 2004 to 2007. Children in the first cohort ranged in age from 2 months to 6 years at time of injury. Participants in the second cohort ranged in age from 8 years to 15 years at time of injury. Participants with orthopedic injuries were recruited only in the second cohort (2004–2007). Participants with TBI or orthopedic injuries were hospitalized at Children’s Memorial Hermann Hospital or Texas Children’s Hospital in Houston, Texas. Inclusionary criteria for children with TBI were the same for both cohorts: 1) complicated-mild, moderate or severe TBI, 2) no known premorbid neurologic, metabolic, or major psychiatric disorder, 3) no history of prior TBI, and 4) gestational age ≥ 32 weeks. A total of 99 children with TBI participated in the long-term outcome components of both cohorts. Of that sample, four were lost to follow-up, one was ineligible to participate in the study because of severe cognitive limitations, and one withdrew. Of the remaining 93 children with TBI, school records and parent ratings of academic functioning were obtained on 79. The participants with TBI in this study did not significantly differ in age at injury, gender, socioeconomic status, or injury severity from the 14 children who were not included in this study (ps >.20). Within the TBI group, two participants were diagnosed with Attention-Deficit/Hyperactivity Disorder prior to the injury and were receiving medication. No participant was receiving special education services prior to the TBI.
The severity of TBI was determined using the lowest post-resuscitation Glasgow Coma Scale (GCS) score17. The motor and verbal scales were modified to be developmentally appropriate for children from birth through 35 months of age6. Injury severity was further classified using acute computed tomography (CT) or brain magnetic resonance imaging (MRI) findings as follows18. Complicated mild was defined as lowest post-resuscitation GCS scores from 13–15 with neuroimaging evidence of parenchymal injury. Moderate and severe TBI consisted of lowest post-resuscitation GCS scores from 9–12 and 3–8, respectively, regardless of imaging findings. Because of the small number of children with complicated-mild TBI and the similarity in outcomes following complicated-mild and moderate TBI18, data from these three children were combined with data for children with moderate TBI creating a combined complicated-mild/moderate TBI group.
The orthopedic comparison group was recruited during their hospitalization (2004–2007) and their school records were obtained two years after their enrollment in the study. Children with orthopedic injuries were excluded from the study if they sustained injuries suggestive of head injury such as facial bruising or facial fractures or exhibited any alteration in consciousness or symptoms of concussion. Of the thirty-five children with orthopedic injuries enrolled in the study, twenty-eight children participated in the current school outcomes study. Children with orthopedic injuries were included to account for possible preinjury demographic factors, as well as the stresses associated with injury and hospitalization, that may influence outcomes.
Healthy children were recruited in both cohorts (1994–1998 and 2004–2007). Age at enrollment ranged from 2 months to 16 years (n=42). These children were recruited from advertisements at local libraries, daycares, and well child programs in the community. Children in both the orthopedic and healthy comparison groups met inclusionary criteria 2–4 as described above for the TBI samples. Socioeconomic status (SES) was assessed using the Hollingshead Four Factor Scale19. Demographic and injury variables for the four groups are presented in Table 1.
Table 1.
Comparison of Demographic Variables by Group
| Traumatic Brain Injury Groups | Comparison Groups | |||
|---|---|---|---|---|
| Complicated- mild/moderate (n=23) |
Severe (n=56) |
Orthopedic (n=28) |
Healthy (n=42) |
|
| Months of age at injury M (SD) | 106.78 (56.58) | 109.94 (48.35) | 124.18 (34.85) | N/A |
| Months of age at follow-up M (SD) | 158.64 (37.68) | 156.34 (40.10) | 149.55 (35.14) | 142.80 (49.98) |
| Glasgow Coma Scale-lowest M (SD) | 10.83 (3.02) | 4.05 (1.92) | N/A | N/A |
| Gender F/M | 10/13* | 9/47* | 12/16 | 19/23 |
| Ethnicity (n) | ||||
| African-American | 0 | 6 | 7 | 9 |
| Asian | 1 | 1 | 2 | 1 |
| Latina/o | 3 | 15 | 7 | 4 |
| White | 17 | 33 | 11 | 25 |
| Other/multiethnic | 2 | 1 | 1 | 3 |
| Socioeconomic Background M (SD) | 36.65 (12.33)** | 38.05 (13.15)** | 42.32 (14.21) | 48.00 (13.02)** |
Note: TBI=traumatic brain injury, C-M=complicated-mild, M=mean, SD=standard deviation;
p < .01 Severe TBI vs. C-M/Moderate;
p<.01 Healthy Comparison Group vs. Complicated-mild/moderate TBI and Severe TBI;
Written informed consent to participate was obtained from the children’s guardians. The protocol was approved by the Institutional Review Board at each medical school and affiliated hospital. Information regarding the child’s school functioning was obtained from parental report and school records. Child oral assent was obtained for participants ages 6 years and older. Written assent was obtained for children 8 years and older.
Measures
School Services
School records were released directly from the schools to the study by parental consent. School records were obtained for children in the first cohort six years after their enrollment in the study and for the second cohort at approximately two years post enrollment. Schools records were coded to reflect the presence or absence of the following variables: formal placement in special education (I.E.P.); self-contained classroom (child is removed from the general education curriculum and placed in a classroom with remedial assistance); pull-out services, sometimes referred to as content mastery (small classroom setting with additional instruction); classroom accommodations (i.e. extended time for examinations, reduced work); tutorial assistance at school, reading intervention (Tier II/small group instruction) and grade repetition. If the child received any of these support services or repeated a grade, then the dichotomous school services outcome variable was coded as present or “1”. Participants who did not receive any services, accommodations, and who did not repeat a grade were coded as “0”.
Parent Ratings
Child Behavior Checklist-20 School Competence
This subscale is composed of parental ratings of the child’s performance on several academic subjects and also includes whether the child is in a special class, repeated one or more grades, and has other academic problems. This scale yields a T-score with a mean of 50 and a standard deviation of 10; higher scores indicate better academic competence.
Adaptive Behavior Assessment System-II-21 Functional Academics Subscale
This twenty-three item scale is completed by the parent and assesses use of basic reading, writing, and mathematics skills in everyday settings such as telling time, writing letters, measuring, and using money correctly. It yields a scaled score with a mean of 10 and standard deviation of 3; higher scores indicate better functional academic skills.
Statistical Approach
We first assessed the bivariate relations among group (complicated-mild/moderate TBI, severe TBI, orthopedic controls, and healthy comparison) and school support services. Chi-square analyses were conducted to assess significant differences across the four groups for the dichotomous school support variable and for each of the support services individually.
For children with TBI, the bivariate relations between injury variables and school support services were subsequently analyzed. The relation of injury severity, age at injury, time since injury, and their interactions with the dichotomous support services was examined using a generalized linear model (GLM) using logit link function. Gender and socioeconomic status (SES) were examined as covariates. Pearson product moment correlations were also conducted.
To evaluate school competency and functional academic skill outcomes across the four groups, a GLM was used to examine the effect of group with gender and SES as covariates. To evaluate these outcomes in relation to injury variables in children with TBI, a GLM was used to examine the relation of age at injury, injury severity (complicated-mild/moderate versus severe), time since injury, and their interactions on school competency and functional academic skills. Multicollinearity was assessed using variance inflation factors (VIF). VIF was less than 2 for all predictors indicating multicollinearity is not a significant factor in these models.
RESULTS
Demographic and Injury Variables
The four groups (complicated-mild /moderate TBI, severe TBI, orthopedic controls, and healthy controls) did not differ in age at time of assessment of school outcomes (F [3,145] = 1.21, p = .31) nor were there significant group differences for ethnicity (χ2[12, N = 149] = 18.80, p = .09). Although the groups did not significantly differ in ethnicity, there are a high number of children of Latino descent in the severe TBI group. The groups differed in gender with the severe TBI group having significantly fewer females than males (χ2 [3, N = 149] = 12.35, p = .0063. Significant group differences were noted on SES; the healthy comparison group had significantly higher status than the two TBI groups (F [3, 147] = 5.66, p = .001).
Within the TBI group, children with complicated-mild/moderate TBI and children with severe TBI did not differ significantly in age at injury, time since injury, ethnicity, age at assessment, and SES, see Table 1. There was a significant gender difference with the severe group having a higher number of males than the complicated-mild/moderate group (χ2 [1, N= 79] = 4.80, p = .02). Children with TBI in the first cohort (1994–1998) did not differ from those in the second (2004–2007) in injury severity or age that school records were assessed. Comparing children with TBI whose records were assessed at the 2 year time point versus the 6 year time point revealed that children assessed at the 6 year time point were significantly younger at age at injury than those assessed at the 2 year time point (F [1, 81] = 45.08, p < .0001). This difference in age at injury occurred because school outcomes of children injured at very young ages (three years and under) cannot be assessed until several years after their injury when they are in school.
School Support Services
Children with TBI and Comparison Groups
The dichotomous outcome variable reflecting receipt of any school support services differed significantly across groups, (χ2 [3, N = 149] = 37.48, p < .0001; φc=.50). The children with severe TBI received significantly more services than those in the orthopedic and healthy comparison groups. The number of children receiving different types of services and findings of significant cell type chi-square comparing rates across the groups as well as odds ratios are provided in Table 2. Healthy children from the community and children with orthopedic injuries had very low rates of school support services.
Table 2.
Number of Children Receiving School Services and Parent Ratings by Group
| Traumatic Brain Injury Groups | Comparison Groups | Severe TBI vs Healthy Comparison |
|||
|---|---|---|---|---|---|
| Complicated- mild/Moderate |
Severe | Orthopedic | Healthy | ||
| Odds Ratio 95% Confidence Interval |
|||||
| School Support Services n (%) | n=23 | n=56 | n=28 | n=42 | |
| Any Support Service* | 15 (65) | 40 (71) | 7 (25) | 7 (17) | 12.50 |
| 4.61–33.89 | |||||
| Special Education Plan* | 5 (22) | 20 (35) | 1 (3) | 0 | 47.74 |
| 2.79–817.19 | |||||
| Self-contained Classroom | 0 | 4 (7) | 0 | 0 | 7.28 |
| 0.38–139.15 | |||||
| Classroom Accommodations* | 7 (30) | 24 (43) | 3 (11) | 0 | 64.08 |
| 3.75–1093.44 | |||||
| Pull-Out Services* | 3 (13) | 10 (18) | 1 (4) | 0 | 19.19 |
| 1.09–337.64 | |||||
| Tutoring at School* | 6 (26) | 21 (38) | 4 (14) | 2 (5) | 12.60 |
| 2.76–57.50 | |||||
| Reading Intervention* | 5 (22) | 13 (23) | 1 (4) | 0 | 26.38 |
| 1.52–457.96 | |||||
| Grade Repetition* | 6 (26) | 11 (20) | 1 (4) | 1 (2) | 10.02 |
| 1.24–81.06 | |||||
| Parent Ratings M (SD) | Effect Sizes | ||||
| Cohens d | |||||
| Functional Academicsa | 9.7 (3.4) | 8.8 (3.8) | 9.5 (3.0) | 11.8 (1.9) | −.99 |
| School Competence b, c | 42.2 (10.8) | 41.8 (9.1) | 47.3 (7.3) | 50.6 (6.2) | −.99 |
Cell type chi-square p<.01 for Severe TBI versus Healthy Comparison Group.
Tukey’s HSD Test:
Healthy Comparison Group > Orthopedic and Severe TBI,
Healthy Comparison Group> both TBI groups,
Orthopedic > Severe TBI.
Chi square analyses were also run for each of the school support services. Significant group differences were found for the following variables: special education plan (χ2 [3, N = 149] = 25.88, p < .0001; φc=.42); classroom accommodations/modifications (χ2 [3, N = 149] = 28.27, p < .0001; φc=51); pull-out services (χ2 [3, N = 149] = 10.54, p = .01; ; φc=.27); tutoring at school (χ2 [3, N = 149] = 16.22, p = .001; φc=.33); reading intervention (χ2 [3, N = 149] = 15.43, p = .0015; φc=.32); and grade repetition (χ2 [3, N = 149] = 12.24, p = .007; φc=.29). As indicated in Table 2, children with severe TBI had higher rates of school services than children from the healthy comparison group; rates of school services did not differ significantly for the complicated-mild/moderate and severe TBI groups. Significant group differences were not found for self-contained placement; only four children with severe TBI were educated in self-contained classrooms. It should be noted that no participant in this study had a Section 504 plan at the time of the study as most received formal services through an IEP plan or had informal accommodations.
Children with TBI
Pearson product moment correlations examined the relation of time since injury and at age at injury with school supports. Time since injury was positively correlated with reading intervention (r = .22, p = .049) for children with TBI. That is, the further out from injury, the greater the number of students with TBI who received reading intervention services. Placement in a self-contained classroom half-time was also positively correlated with time since injury (r = .23, p = .0437) and negatively correlated with age at injury (r = −.26, p = .0187). Therefore, greater time since injury and younger age at injury were associated with being in self-contained classroom for half-time.
GLM analyses were initially performed co-varying for gender and SES. Neither covariate was significantly related to the dichotomous school support services outcome and their inclusion did not alter the results. Therefore, we report the results without gender and SES as covariates (final models are presented in supplemental digital content 1). The GLM with logit link function did not find a significant three way interaction for age at injury, time since injury, and injury severity for students with TBI and this interaction was dropped from the model. However, a significant two way interaction was found for time since injury by injury severity (χ2 [1, N = 79] = 4.13, p=.0421) after controlling for age at injury. Plotting the interaction (see Figure 1) revealed that the percentage of children with severe TBI who received school services did not vary by time since injury. However, children with complicated-mild/moderate injuries were less likely to receive school support services when they were closer in time to the injury than children who were further in time from the injury. Students with complicated-mild/moderate TBI who were further in time from the injury had comparable rates of school support services as those with severe TBI.
Figure 1.
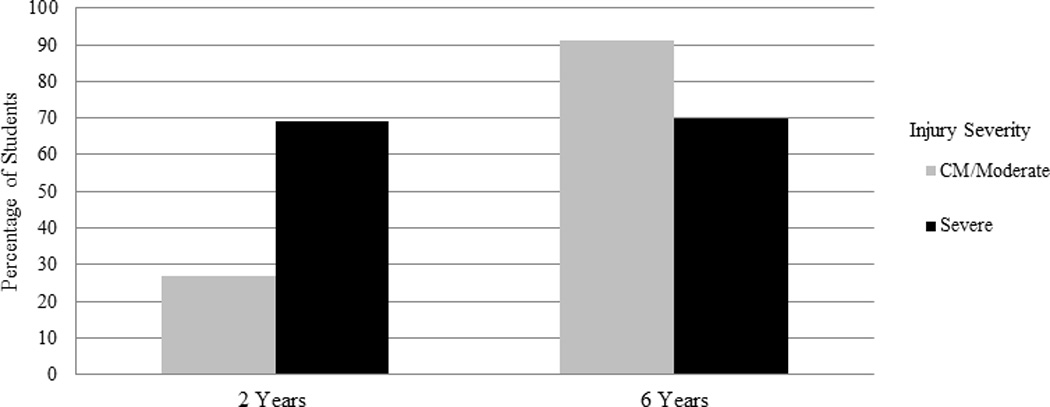
Likelihood of School Services and Time Since Injury
Parent Ratings of Academic Competence
Children with TBI and Comparison Groups
Significant group differences were found on both the ABAS functional academic scale (F [3, 136] = 6.93, p = .0002; R2 =.13) and the CBCL school competency scale (F [3, 141] = 10.14, p = .0001; R2=.18). Follow-up Tukey pairwise comparisons revealed that children with severe TBI were rated as having lower functional academic scores on the ABAS than children in the healthy comparison group (p < .05 corrected). For school competency on the CBCL, follow-up Tukey pairwise comparisons revealed that the healthy comparison group significantly differed from children with moderate TBI as well as children with severe TBI. The orthopedic injury group also differed from children with severe TBI (p < .05 corrected).
Children with TBI
For GLM analyses examining the parent ratings for children with TBI, neither gender nor SES were significantly related to outcomes and they were trimmed from each model. The three-way interaction among age at injury, time since injury, and injury severity was not significant and was also trimmed from each model.
For the ABAS functional academic scale, none of the two-way interactions was significant and they were also dropped (all ps > .15). The main effect for age at injury was significant; children injured at younger ages had lower scores (F [1, 69] = 6.04, p = .02; ηp2 =.08). For ratings of school competency (CBCL), only the interaction of time since injury and injury severity was significant (F [1,68] = 4.41, p = .04; ηp2 =.06) after controlling for age at injury. Plotting the interaction indicated that students with less time since injury who had complicated-mild/moderate TBI had higher school competency ratings than students with more time since injury (see Figure 2). Time since injury was not significantly related to school competency for those with severe TBI.
Figure 2.
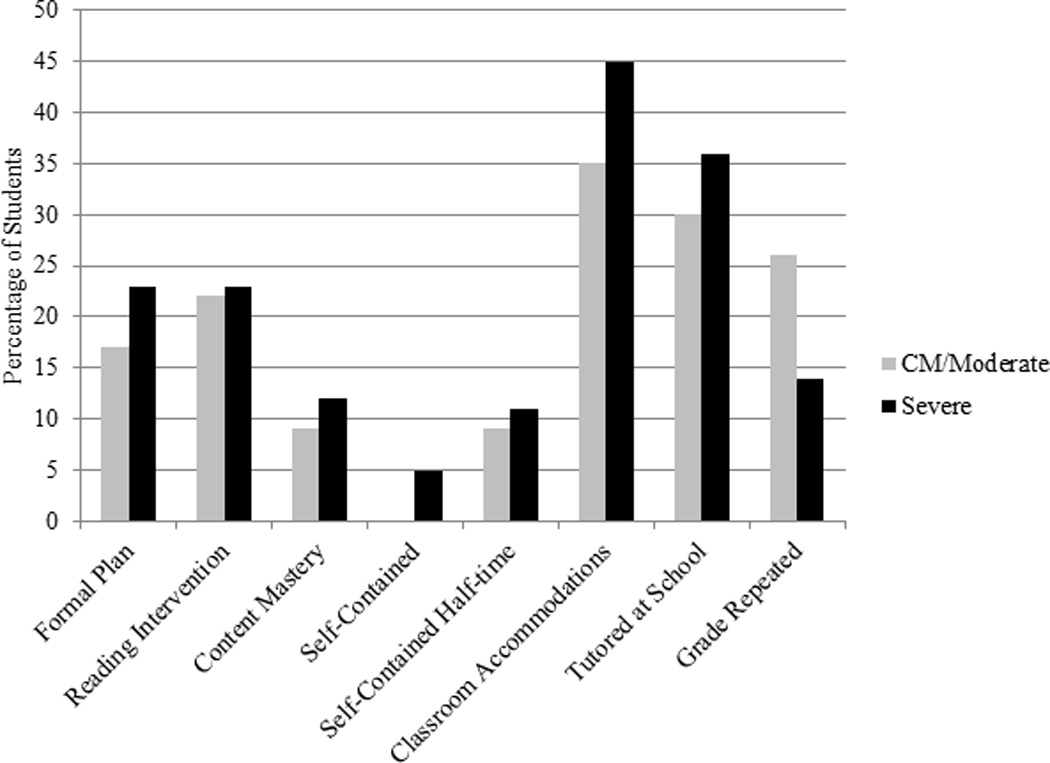
School Services by Injury Severity
DISCUSSION
The results of this cross-sectional study highlight the long-term educational challenges facing children with TBI. As predicted, we found that children with TBI have higher rates of school support services than students with orthopedic injuries and healthy comparison children. Students with severe TBI had high rates of educational support services, regardless of age at injury or time since injury. An unexpected finding was the disparity in the provision of educational services between students with complicated-mild/moderate and severe TBI. Children with complicated-mild/moderate TBI were less likely to receive educational services at two years post injury than children with severe TBI; however, those assessed at an average of six years post injury had comparable levels of educational services to students with severe TBI at the same time point. That is, the complicated-mild/moderate TBI group who was further from injury had much higher rates of school based services than those who were two years post injury. Data regarding school services mirrors parental ratings of school competency and academic performance metrics such as grades and retention. Parental ratings of school competency were significantly related to time since injury for children with complicated-mild/moderate TBI; the cohort that was assessed at the later time point had lower competency than those assessed at two years post injury.
For children with complicated-mild/moderate TBI, educational issues may be increasingly evident as they age and more demands are placed upon them. These findings are consistent with previous studies which have found that children with TBI are at high risk for falling further behind their peers as they age5, 9, 22, 23. The lower rates of educational support services for children with complicated-mild/moderate TBI at two years post injury raises concerns about under identification of educational needs for students with less severe TBI.
Based on previous research indicating younger children are more vulnerable to the deleterious effects of TBI6, 24, we predicted that children injured at younger ages would have greater educational services than children injured at older ages. We found that younger age at injury was associated with placement in a self-contained classroom, which is an educational setting for children with significant disabilities who cannot be appropriately educated in a less restrictive regular classroom setting. Younger age at injury was associated with lower functional academic skills based on parental ratings of basic reading, writing, and math skills.
Previous studies have found generally favorable recovery of basic academic skills on standardized tests but poor school outcomes, such as grade retention and poor grades4, 9, 25. Even though academic performance may decline over time, de novo placements in special education occur infrequently after the first year post-injury12. Therefore, inadequate monitoring of children’s academic progress during the first several years after injury represents a barrier to accessing appropriate supports. The longer the interval between the injury and identification of academic problems, the less likely that educational and medical providers will connect the TBI to the academic difficulties and initiate services to which the child may be eligible under federal statutes.
In studies, such as this one and those by Taylor26, Glang14, and Rivara13 the high rates of school support services for students with TBI is contrary to the view that TBI is a low incidence disability in school settings14. Participants in this study were enrolled in longitudinal studies of outcome from TBI in children. As part of their participation in those studies, the parents received interval reports about their child’s functioning and recommendations for services or accommodations at school. These reports may have aided parents in identifying their child’s educational needs and provided a means by which they could advocate for educational services. Therefore, it is likely that this study may overestimate educational services typically provided to students with TBI. Most families do not have the benefit of ongoing contact with healthcare professionals who are knowledgeable about TBI. Schools rely primarily on parental information regarding TBI and often do not receive information from health care providers about the long-term effects of TBI on the child’s cognitive, social, and academic functioning11. Most parents are not well informed about the possible long-term sequelae of TBI and as such, do not advocate for services for their children until the child experiences academic failure or social rejection27. Educating parents about the long-term impairments experienced by children with TBI often falls to health care professionals, such as pediatricians11. The low rates of special education services for students with TBI relative to the fairly high incidence14 suggests that health-care providers may be unfamiliar with the long-term sequelae of TBI and the educational rights of students with TBI.
Limitations of the current study include its cross sectional design. A longitudinal study of school outcomes would allow for examination of changes in educational services overtime. Although it appears that children with complicated-mild/moderate TBI have an increase in school services by six years post injury, without following their school trajectory overtime, no conclusions can be drawn about change in services overtime. In order to assess the impact of early age at injury on school outcomes, children injured in early childhood had much longer time since injury than those injured in later childhood. It is not possible to assess school functioning in children who are not yet school age, therefore there follow-up period was much longer than their older counterparts. In order to address the question of age at injury on school outcome, children who participate in this study hailed from two different ongoing research studies or two cohorts. It would be ideal to be able to follow children injured in infancy through late adolescence; however, the reality of research funding makes it improbable to do so. Although there may be unknown cohort differences, these cohort differences are not likely to have influenced findings related to injury severity. An additional issue for this study is that school records from students without TBI were obtained at the two year time point. Long term follow-up of school outcomes of typically developing children and children with orthopedic injuries is needed to better understand how school outcomes for students with TBI differ. Although school records were obtained, we were not able to acquire ratings from teachers regarding the students’ school competences. Teachers may differ from parents in how they view the academic capabilities of their students. Similar to other studies of children with TBI, this study has a small sample size which reduces statistical power to identify significant findings. The small sample size likely reduced the ability to detect the interaction among age at injury, injury severity, and time since injury.
Conclusion
This study highlights the increasing vulnerability of children with complicated-mild/moderate TBI to poor long-term academic outcomes. Long-term monitoring of educational performance and service delivery is essential for children across the spectrum of TBI severity. Future studies addressing barriers to educational services and efficacy of educational supports are needed.
Supplementary Material
Acknowledgments
This manuscript was supported by Grant Number R01NS046308 from the National Institute of Neurological Disorders and Stroke to Dr. Linda Ewing-Cobbs. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health.
Funding Source: All phases of this study were supported by the following NIH grant: R01NS046308
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflict of interests to disclose.
References
- 1.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehab. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention NCfIPaC. Traumatic brain injury. Washington, DC: Centers for Disease Control and Prevention; 2004. National Information Center for Children and Youth with Disabilities. [Google Scholar]
- 3.Masel BE, DeWitt DS. Traumatic brain injury: a disease process, not an event. J Neurotrauma. 2010;27(8):1529–1540. doi: 10.1089/neu.2010.1358. [DOI] [PubMed] [Google Scholar]
- 4.Ewing-Cobbs L, Fletcher JM, Levin HS, Iovino I, Miner ME. Academic achievement and academic placement following traumatic brain injury in children and adolescents: A two-year longitudinal study. J Clin Exp Neuropsyc. 1998;20:769–781. doi: 10.1076/jcen.20.6.769.1109. [DOI] [PubMed] [Google Scholar]
- 5.Jaffe KM, Polissar NL, Fay GC, Liao S. Recovery trends over three years following pediatric traumatic brain injury. Arch Phys Med Rehabi. 1995;76:17–26. doi: 10.1016/s0003-9993(95)80037-9. [DOI] [PubMed] [Google Scholar]
- 6.Ewing-Cobbs L, Prasad M, Kramer L, Cox C, Baumgartner J, Fletcher S, et al. Late intellectual and academic outcomes following traumatic brain injury sustained during early childhood. J Neurosurg. 2006;105(Suppl 4):287–296. doi: 10.3171/ped.2006.105.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor HG, Swartwout MD, Yeates KO, Walz NC, Stancin T, Wade SL. Traumatic brain injury in young children: postacute effects on cognitive and school readiness skills. J Int Neuropsychol Soc. 2008;14(5):734–745. doi: 10.1017/S1355617708081150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fulton JB, Yeates KO, Taylor HG, Walz NC, Wade SL. Cognitive predictors of academic achievement in young children 1 year after traumatic brain injury. Neuropsychology. 2012;26(3):314–322. doi: 10.1037/a0027973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fay GC, Jaffe KM, Polissar NL, Liao S, Rivara JB, Martin KM. Outcome of pediatric traumatic brain injury at three years: A cohort study. Arch Phys Med Rehabil. 1994;75:733–741. [PubMed] [Google Scholar]
- 10.Arnett AB, Peterson RL, Kirkwood ML, Taylor HG, Stancin T, Brown TM, Wade SL. Behavioral and cognitive predictors of educational outcomes in pediatric traumatic brain injury. J Int Neuropsych Soc. 2013;19(8):881–889. doi: 10.1017/S1355617713000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hawley CA. Behaviour and school performance after brain injury. Brain Inj. 2004;18(7):645–659. doi: 10.1080/02699050310001646189. [DOI] [PubMed] [Google Scholar]
- 12.Taylor HG, Yeates K, Wade S, Drotar D, Stancin T, Montpetite M. Long-term educational interventions after traumatic brain injury in children. Rehabil Psychol. 2003;48(4):227–236. [Google Scholar]
- 13.Rivara FP, Koepsell TD, Wang J, Temkin N, Dorsch A, Vavilala MS, et al. Incidence of disability among children 12 months after traumatic brain injury. Am J Public Health. 2012;102(11):2074–2079. doi: 10.2105/AJPH.2012.300696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glang A, Todis B, Thomas CW, Hood D, Bedell G, Cockrell J. Return to school following childhood TBI: who gets services? NeuroRehabilitation. 2008;23(6):477–486. [PubMed] [Google Scholar]
- 15.Dettmer J, Ettel D, Glang A, McAvoy K. Building statewide infrastructure for effective educational services for students with TBI: promising practices and recommendations. J Head Trauma Rehabil. 2014;29(3):224–232. doi: 10.1097/HTR.0b013e3182a1cd68. [DOI] [PubMed] [Google Scholar]
- 16.Ylvisaker M, Todis B, Glang A, Urbanczyk B, Franklin C, DePompei R, et al. Educating students with TBI: themes and recommendations. J Head Trauma Rehabil. 2001;16(1):76–93. doi: 10.1097/00001199-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 18.Levin HS, Hanten G, Roberson G, Li X, Ewing-Cobbs L, Dennis M, et al. Prediction of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. J Neurosurg Pediatr. 2008;1(6):461–470. doi: 10.3171/PED/2008/1/6/461. [DOI] [PubMed] [Google Scholar]
- 19.Hollingshead A. Four factor index of social status. New Haven: Yale University Press; 1975. [Google Scholar]
- 20.Achenbach T. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. urlington, VT: University of Vermont College of Medicine; 1991. [Google Scholar]
- 21.Harrison PL, Oakland T. Adaptive behavior assessment system - II. San Antonio: The Psychological Corporation; 2003. [Google Scholar]
- 22.Hawley CA. Reported problems and their resolution following mild, moderate and severe traumatic brain injury amongst children and adolescents in the UK. Brain Inj. 2003;17(2):105–129. doi: 10.1080/0269905021000010131. [DOI] [PubMed] [Google Scholar]
- 23.Taylor HG, Yeates KO, Wade SL, Drotar D, Klein S. Influences on first-year recovery from traumatic brain injury in children. Neuropsychology. 1999;13:76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- 24.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116(6):1374–1382. doi: 10.1542/peds.2004-1728. [DOI] [PubMed] [Google Scholar]
- 25.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16(1):15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 26.Taylor HGY, K O, Wade SL, Drotar D, Stancin T, Montpetite M. Long-term educational interventions after traumatic brain injury in children. Rehabil Psychol. 2003;48(4):227–236. [Google Scholar]
- 27.Gfroerer SD, Wade SL, Wu M. Parent perceptions of school-based support for students with traumatic brain injuries. Brain Inj. 2008;22(9):649–656. doi: 10.1080/02699050802227162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


