Abstract
Aim
The aim of this study was to investigate lifestyle habits and lifestyle adjustments among subfertile women trying to conceive.
Materials and methods
Women (n = 747) were recruited consecutively at their first visit to fertility clinics in mid-Sweden. Participants completed a questionnaire. Data were analyzed using logistic regression, t tests, and chi-square tests.
Results
The response rate was 62% (n = 466). Mean duration of infertility was 1.9 years. During this time 13.2% used tobacco daily, 13.6% drank more than three cups of coffee per day, and 11.6% consumed more than two glasses of alcohol weekly. In this sample, 23.9% of the women were overweight (body mass index, BMI 25–29.9 kg/m2), and 12.5% were obese (BMI ≥30 kg/m2). Obese women exercised more and changed to healthy diets more frequently than normal-weight women (odds ratio 7.43; 95% confidence interval 3.7–14.9). Six out of ten women (n = 266) took folic acid when they started trying to conceive, but 11% stopped taking folic acid after some time. Taking folic acid was associated with a higher level of education (p < 0.001).
Conclusions
Among subfertile women, one-third were overweight or obese, and some had other lifestyle factors with known adverse effects on fertility such as use of tobacco. Overweight and obese women adjusted their habits but did not reduce their body mass index. Women of fertile age would benefit from preconception counseling, and the treatment of infertility should routinely offer interventions for lifestyle changes.
Keywords: Alcohol consumption, assisted reproduction, diet, infertility, lifestyle, obesity, pregnancy, tobacco use
Introduction
A healthy lifestyle is known to be of importance for women, especially when they are planning to get pregnant, since negative lifestyle factors may contribute to impaired reproduction and a lower chance of having a healthy child. Such negative factors include smoking, drinking alcohol and over-use of other drugs, underweight or overweight, unhealthy diet, harmful infections, exposure to environmental hazards, and an adverse medical history. These issues might be particularly important for women seeking treatment for infertility (1–3). Another important factor affecting female fertility is age. Women in Europe have delayed their childbearing considerably during the past decades, and the mean age for childbearing is currently 30 years or more in almost half of the member states of the European Union (4,5). In Sweden, the mean age for having the first child was 28.5 years in 2013 compared with 24 years in 1973.
The postponement of the birth of the first child is due to different reasons throughout Europe. Interviews with Swedish men and women who had an academic education showed that a majority of them wanted children, but postponed their parenthood as a rational adaptation to changes in society such as having a sound personal economy. Participants believed that fertility could be restored by assisted reproductive technologies (ART) (6). A consequence of this demographic trend seems to be associated with an increase in the incidence of female subfertility (7).
Major advances have been achieved in the field of infertility treatment and assisted reproductive technology (ART) during the past 25 years, leading to increased pregnancy rates. However, researchers and clinicians are still trying to identify additional factors that might impact on live birth rates. Also in ART, factors such as nutrition and diet, exercise, and the use of tobacco and alcohol, as well as being overweight or underweight, might have an impact on outcomes (2,8).
The effectiveness of preconception care and counseling (PCC) in general, and for couples with a fertility problem in particular, has been demonstrated (9,10). Studies have shown that PCC reduces costs, improves reproductive outcomes, promotes healthy pregnancies, and reduces pregnancy complications and poor neonatal birth outcomes.
There is a lack of homogeneous guidelines, recommendations, and services for preconception health care in European countries (11,12). The European Society of Human Reproduction and Embryology (ESHRE) Guideline Development Group recommends that fertility staff should consider providing women with information about the impact of lifestyle habits and supporting them in making necessary changes (13). Some counseling about lifestyle is generally included in initial consultations in fertility clinics. Brochures and hand-outs about lifestyle are generally available at fertility clinics in Sweden, but this information is usually not handed out or explained to the patients actively. Effective strategies and support for making healthy changes are not routinely offered.
Despite the existing knowledge about the association of risk of fertility problems and adverse pregnancy outcomes with unhealthy lifestyles (14,15), it is largely unknown to what extent subfertile women adjust their habits during the time they are trying to conceive. Effective individual counseling to subfertile women demands an understanding about what measures women take to increase the chances of conception.
The aim of this study was therefore to investigate lifestyle habits among subfertile women trying to conceive in relation to their background characteristics. It was hypothesized that age, duration of infertility, BMI (body mass index), immigration status, education, occupation, income, and information searching were associated with lifestyle habits and lifestyle adjustments among subfertile women trying to conceive.
Material and methods
Design
This was a cross-sectional study constituting baseline measurements for a planned longitudinal cohort study. The follow-up is scheduled to take place 2 years after the return of the questionnaire.
Participants and recruitment
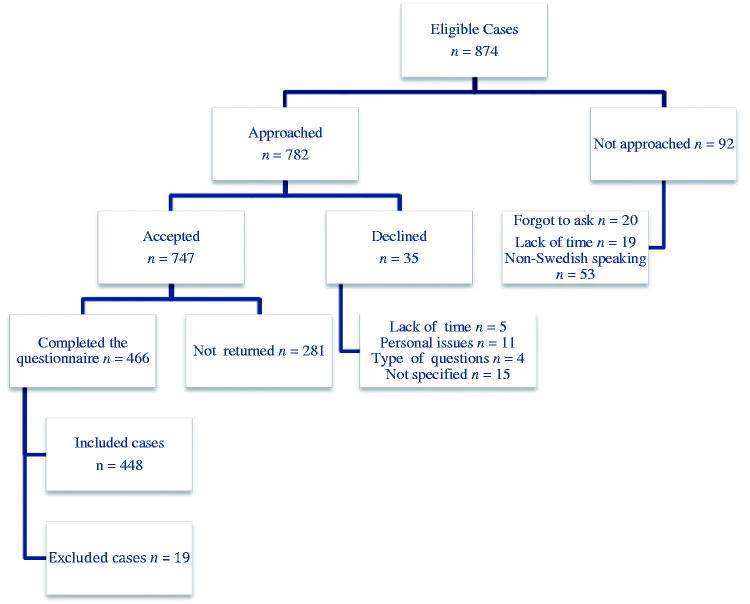
Women attending 10 fertility clinics in mid-Sweden participated. Eligible women (n = 782) were asked to participate in the study at their first visit to the clinic. The time of this first visit to the clinic is defined as ‘Baseline year’. Data collection started in May 2013 and ended in March 2015 with a planned follow-up 2 years later. Being able to read and write Swedish and having no previous infertility diagnosis were inclusion criteria for the study. Midwives gave oral and written information about the study to eligible women who fulfilled the inclusion criteria. In 19 cases, women were excluded from the study either because they reported having a female partner or did not answer the question about lifestyle changes while they tried to conceive. Thirty-five women declined to participate in the study. Those who agreed to participate received a questionnaire to complete at the clinic or at home and return it by mail in a prepaid envelope. The midwife registered a telephone number or an email address for participating women, and a reminder was sent by text message or email to those who had not returned the questionnaire within 2 weeks. The completed questionnaires were returned including the signed informed consent, which immediately upon receipt was separated to be archived securely and safely. During the study period, the midwives listed all registrations, numbers of women approached, and their response (accepted/declined). Of the 782 eligible women, 747 (95.5%) agreed to participate in the study, and 466 of these (62.4%) completed the study. A flow chart of the procedure is presented in Figure 1.
Figure 1.
Flow chart of the study procedure.
Of the group of women (n = 281) who had agreed to participate in the study but did not return the questionnaire, 14% (n = 39) were analyzed using information from patient records with regard to age, infertility duration, BMI (weight/height2 in kg/m2), tobacco use, and alcohol consumption. The results showed no significant differences between this group and the group of women who completed the study.
Questionnaire
The questionnaire (available online) consisted of 71 items and included validated instruments for pregnancy planning, stress, anxiety, postpartum depression, sexual satisfaction, exercise habits, alcohol consumption, tobacco use, and diet (16–22). Researchers and clinicians reviewed the questions and conducted a pilot study with 30 women, after which some items were adjusted. The following themes were covered: demographic characteristics, immigrant background, medical and reproductive history, and methods for seeking information about infertility. The questionnaire also included specific questions on the type of lifestyle factors at baseline year and number of lifestyle changes made while the women had been trying to conceive. In the following sections we present items relevant to the aim of the study.
Background characteristics
Questions were asked about background characteristics: age; partner’s age; height and self-reported weight at baseline year as well as 1 year earlier; marital status; duration of current relationship; country of birth; parents’ country of birth; level of education; occupation and household income/month; understanding of Swedish language; and duration of infertility.
Background lifestyle and lifestyle changes
Questions regarding lifestyle covered health-promoting lifestyle changes: intake of folic acid and/or multivitamin supplements; daily tobacco use; weekly alcohol consumption; daily coffee consumption; type of diet; and weekly physical activity graded in number of hours. The participants were also asked to describe any changes to a healthier diet in free text. Access to sites for information-seeking and type of professional counseling were also included. Questions covered baseline year as well as the time from when they started to plan for pregnancy.
Ethical considerations
The study was approved by the Regional Ethical Review Board in Uppsala (2012/278).
Statistical analysis
Data were analyzed using IBM SPSS Statistics (version 20; IBM Corp., Armonk, NY). Data regarding age, household income, duration of infertility, and current BMI in kg/m2 were treated as continuous variables and are presented as the mean and standard deviation (SD), while the duration of the relationship and frequency of physical activity were treated as ordinal variables and are presented as the median and interquartile range (Q1, Q3). Differences in background characteristics between women with and without lifestyle changes during the time when they were trying to conceive were analyzed using the Mann–Whitney non-parametric U test for ordinal variables, Student’s t test for continuous variables, and Pearson’s chi-square test for categorical variables. For all statistical analyses, a two-sided p value <0.05 was considered significant (Table 3). Logistic regression was used to analyze the effect of background variables (independent variables) on lifestyle changes (dependent variable). Results are reported as the odds ratio (OR) with 95% confidence interval (CI) (Table 4). The variables with significant values in Table 3 were included as covariates in the multivariate logistic regression described in Table 4.
Table 3.
Results for univariate tests with type of health-promoting lifestyle change as outcome in relation to background characteristics.
| Started to take folic acid |
Changes in tobacco use (decrease/stop) |
Change to more physical activity/healthier diet |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes n = 266 (59.4) | No n = 182 (4.6) | P value | Yes n = 105 (23.4) | No n = 343 (76.6) | P value | Yes n = 186 (41.5) | No n = 262 (58.5) | P value | |
| Age (years), mean (SD) | 30.6 (4.8) | 29.9 (4.9) | 0.142 | 28.9 (4.8) | 30.7 (4.8) | 0.001 | 29.9 (5) | 30.5 (4.7) | 0.204 |
| Duration of infertility (years), mean (SD) | 1.5 (3.4) | 2.1 (1.9) | 0.028 | 1.74 (4.5) | 1.76 (2.3) | 0.958 | 2.0 (3.6) | 1.6 (2.3) | 0.192 |
| Household income/month (SEK), mean (SD) | 48,596 (21,466) | 41,321 (20,974) | 0.001 | 38,978 (20,749) | 47,719 (21,394) | <0.001 | 43,193 (22,706) | 47,434 (20,532) | 0.047 |
| Level of education, n (%) | <0.001 | <0.001 | 0.08 | ||||||
| College/university | 165 (68.2) | 77 (31.8) | 36 (14.9) | 206 (85.1) | 92 (38.0) | 150 (62.0) | |||
| Non-college/non-university | 98 (48.8) | 103 (51.2) | 68 (33.8) | 133 (66.2) | 93 (46.3) | 108 (53.7) | |||
| Occupation, n (%) | 0.21 | 0.005 | 0.29 | ||||||
| Working >50% | 220 (60.8) | 142 (39.2) | 75 (20.7) | 287 (79.3) | 146 (40.3) | 216 (59.7) | |||
| Not working | 46 (53.5) | 40 (46.5) | 30 (34.9) | 56 (65.1) | 40 (46.5) | 46 (53.5) | |||
| Current BMI (kg/m2), mean (SD) | 24.2 (4.2) | 25.3 (5.8) | 0.036 | 24.4 (4.3) | 24.8 (5.0) | 0.531 | 26.4 (5.7) | 23.4 (3.8) | <0.001 |
| BMI (three categories), n (%) | 0.049 | 0.83 | <0.001 | ||||||
| Normal | 166 (60.8) | 107 (39.2) | 66 (24.2) | 207 (75.8) | 81 (29.7) | 192 (70.3) | |||
| Overweight | 68 (63.6) | 39 (36.4) | 23 (21.5) | 84 (78.5) | 59 (55.1) | 48 (44.9) | |||
| Obese | 25 (44.6) | 31 (55.4) | 14 (25.0) | 42 (75.0) | 42 (75.0) | 14 (25.0) | |||
| Country of birth, n (%) | 0.001 | 0.899 | 0.74 | ||||||
| Sweden | 237 (62.9) | 140 (37.1) | 87 (23.1) | 290 (76.9) | 158 (41.9) | 219 (58.1) | |||
| Born outside Sweden | 26 (41.3) | 37 (58.7) | 15 (23.8) | 48 (76.2) | 25 (39.7) | 38 (60.3) | |||
| Parents’ country of birth (one or both), n (%) | 0.008 | 0.31 | 0.48 | ||||||
| Born in Sweden | 225 (62.5) | 135 (37.5) | 86 (23.9) | 274 (76.1) | 154 (42.8) | 206 (57.2) | |||
| Born outside Sweden (one or both) | 36 (46.2) | 42 (53.8) | 16 (20.5) | 62 (79.5) | 30 (38.5) | 48 (61.5) | |||
| Understanding Swedish, n (%) | 0.07 | 0.58 | 0.31 | ||||||
| Very good | 249 (61.0) | 159 (39.0) | 94 (23.0) | 314 (77.0) | 173(42.4) | 235 (57.6) | |||
| Quite good/neither good nor bad | 15 (45.5) | 18 (54.5) | 9 (27.3) | 24 (72.7) | 11 (33.3) | 22 (66.7) | |||
| Information searching | <0.001 | 0.82 | 0.038 | ||||||
| 0–1 sites | 53 (19.9) | 62 (34.3) | 29 (27.6) | 86 (25.1) | 39 (21.0) | 76 (29.1) | |||
| 2 sites | 73 (27.4) | 61 (33.7) | 32 (30.5) | 102 (29.8) | 52 (28.0) | 82 (31.4) | |||
| ≥ 3 sites | 140 (52.6) | 58 (32.0) | 44 (41.9) | 154 (45.0) | 95 (51.1) | 103 (39.5) | |||
P values (bold information indicates significant values) are from chi-square and Student’s t tests.
BMI: body mass index; SD: standard deviation.
Table 4.
Results for multivariate logistic regression model with type of health-promoting lifestyle changes as outcome, given as the odds ratio (OR) with 95% confidence interval (CI).
| OR | 95% CI | P | |
|---|---|---|---|
| Started taking folic acid supplements (cases included in analysis: 377 (84%)): | |||
| Duration of infertility in years (mean) | 0.921 | (0.840–1.009) | 0.078 |
| Household income/month (1,000 SEK) | 1.012 | (1.001–1.024) | 0.040 |
| Level of education | |||
| College/university | 1.853 | (1.151–2.983) | 0.011 |
| Non-college/non-university | (Ref.) | ||
| BMI | |||
| Normal | (Ref.) | ||
| Overweight | 1.287 | (0.752–2.203) | 0.357 |
| Obese | 0.568 | (0.293–1.102) | 0.094 |
| Country of birth | |||
| Sweden | 1.828 | (0.659–5.074) | 0.247 |
| Born outside Sweden | (Ref.) | ||
| Parents’ country of birth | |||
| Born in Sweden | 1.618 | (0.664–3.941) | 0.289 |
| Born outside Sweden (one or both) | (Ref.) | ||
| Information searching | |||
| 0–1 sites | (Ref.) | ||
| 2 sites | 1.143 | (0.631–2.067) | 0.660 |
| ≥3 sites | 2.172 | (1.241–3.801) | 0.007 |
| Decrease or stop in tobacco use (cases included in analysis: 412 (92%): | |||
| Age (years) | 0.950 | (0.900–1.002) | 0.060 |
| Household income/month (1,000 SEK) | 0.991 | (0.978–1.005) | 0.223 |
| Level of education | |||
| College/university | (Ref.) | ||
| Non-college/non-university | 2.256 | (1.352–3.765) | 0.002 |
| Occupation | |||
| Working >50% of the time | (Ref.) | ||
| Not working | 1.314 | (0.705–2.448) | 0.390 |
| Increase in physical activity and/or change to more healthy diet (cases included in analysis: 407 (91%)): | |||
| Household income/month (1,000 SEK) | 0.996 | (0.985–1.007) | 0.451 |
| Level of education | |||
| College/university | (Ref.) | ||
| Non-college/non-university | 1.057 | (0.673–1.661) | 0.810 |
| BMI | |||
| Normal | (Ref.) | ||
| Overweight | 2.931 | (1.789–4.800) | <0.001 |
| Obese | 7.431 | (3.700–14.923) | <0.001 |
| Information searching | |||
| 0–1 sites | (Ref.) | ||
| 2 sites | 1.114 | (0.614–2.023) | 0.722 |
| ≥3 sites | 2.032 | (1.184–3.487) | 0.010 |
Results
The mean age of the studied women was 30.2 years (range 19–42 years), and they had a mean duration of infertility of 1.9 years. About half of the women (54.7%, n = 245) reported that they had been in a stable relationship for more than 4 years. In 71.4% of the women (n = 320), the partners jointly took the decision to start trying to conceive; in 25% (n = 112) the woman decided by herself; and in 3% (n = 14) the partner had taken the initiative. The couples had vaginal intercourse on average twice a week, and 67% (n = 300) used ovulation tests with a mean of 18 tests (SD 26.6, range 1–200) per woman. One out of three women (n = 132) had set a time frame for becoming pregnant of 1 year, and 19% (n = 85) had considered the possibility of adoption. Fourteen percent (n = 63) were born outside Sweden, and 91% stated that their understanding of the Swedish language was very good (Table 1).
Table 1.
Background characteristics and lifestyles of the 448 women included in the study.
| Characteristic | n (%) |
|---|---|
| Age (years), mean (SD)a | 30.2 (4.8) |
| Partner’s age (years), mean (SD) | 33.4 (6.8) |
| Duration of current relationship (years), median (Q1, Q3) | 5 (3, 8) |
| Household income/month (SEK) | |
| Mean (SD) | 45,664 (21,541) |
| Median (Q1, Q3) | 47,000 (30,000, 59,000) |
| Currently working (>50%), n (%) | 362 (80.8) |
| Level of education, n (%) | |
| College/university | 242 (54.0) |
| Non-college/non-university | 201 (44.9) |
| Body mass index (BMI) in kg/m2, mean (SD) | 24.6 (4.9) |
| Normal, ≤25, n (%) | 273 (60.9) |
| Overweight, 25–29.9, n (%) | 107 (23.9) |
| Obese, ≥30, n (%) | 56 (12.5) |
| Country of birth, n (%) | |
| Born in Sweden | 377 (84.2) |
| Born outside Sweden | 63 (14.1) |
| Parent (one or two) born outside Sweden, n (%) | 78 (17.4) |
| Understanding of Swedish language, n (%) | |
| Very good | 408 (91.1) |
| Quite good/neither good nor bad | 33 (7.4) |
| Duration of infertility (years) | |
| Mean (SD) | 1.9 (1.7) |
| Median (Q1, Q3) | 1.4 (1.2, 2.0) |
| Taking folic acid supplementation, n (%) | 216 (48.2) |
| Taking vitamin supplementation, n (%) | 119 (26.6) |
| Weekly alcohol consumption, n (%) | 60 (13.4) |
| Amount of alcohol consumption/week, n (%) | |
| >1 glass/week | 98 (21.9) |
| >2 glasses/week | 52 (11.6) |
| Using tobacco, n (%) | 78 (17.4) |
| Using tobacco daily, n (%) | 59 (13.2) |
| Eating a balanced diet, n (%) | 325 (72.5) |
| Vegetarian | 20 (4.4) |
| GI diet | 15 (3.3) |
| LCHF | 15 (3.3) |
| Coffee >1 cup/day, n (%) | 225 (50.2) |
| Coffee >3 cups/day, n (%) | 61 (13.6) |
| Weekly physical activity in hours, median (Q1, Q3) | 3 (2, 4) |
| Women who sought information about fertility, n (%) | 442 (98.7) |
| Number of information sites consulted, n (%) | |
| 0–1 | 115 (25.7) |
| 2 | 134 (29.9) |
| 3–9 | 198 (44.2) |
| Type of information site, n (%)a | |
| Mother care unit | 158 (35.3) |
| Blogs | 293 (65.4) |
| Health care guide (1177)b | 245 (54.7) |
| Women who obtained professional counseling, n (%) | 316 (70.5) |
| Type of professional counselor, n (%) | |
| Midwife | 161 (35.9) |
| Specialist | 138 (30.8) |
| Other | 30 (6.7) |
| Number of negative lifestylesc | |
| 0 | 102 (22.8) |
| 1 | 176 (39.3) |
| 2 | 110 (24.6) |
| ≥3 | 60 (13.4) |
Multiple answer possible.
1177: telephone number for health care guide.
Not taking folic acid; using tobacco; consuming alcohol or coffee; BMI ≥25 kg/m2.
GI: glycemic index; LCHF: low-carb high-fat diet; SD: standard deviation; SEK: Swedish krona.
Lifestyle during the pregnancy planning period
Almost half of the women (48.2%, n = 216) were taking folic acid supplements at their first visit to the clinics. However, 59.4% (n = 266) had started to take folic acid by the time they started to plan for pregnancy (Table 2).
Table 2.
Reported health-promoting lifestyle changes during the time when the women were trying to conceive.
| Reported health-promoting lifestyle changes | n (%) |
|---|---|
| Started taking folic acid supplement | |
| Yes | 266 (59.4) |
| No | 182 (40.6) |
| Change in coffee-drinking habits | |
| Quit drinking | 17 (3.8) |
| Cut down | 93 (20.8) |
| No change | 338 (75.4) |
| Change in alcohol-drinking habits | |
| Stopped drinking | 59 (13.2) |
| Reduced drinking | 105 (23.4) |
| No change | 284 (63.4) |
| Change in tobacco usea | |
| Quit tobacco | 60 (13.4) |
| Reduced tobacco use | 49 (10.9) |
| No change | 339 (75.7) |
| Change to more healthy diet | |
| Yes | 92 (20.5) |
| No change in diet | 356 (79.5) |
| Physical activity | |
| More | 143 (31.9) |
| Less | 16 (3.6) |
| No change | 289 (64.5) |
| Number of reported health-promoting lifestyle changes | |
| Few (0–1) | 146 (32.6) |
| Medium (2) | 128 (28.6) |
| Many (3–6) | 174 (38.8) |
Tobacco use = smoking and/or taking snuff.
Daily tobacco use was reported by 13% of the women (n = 59) and was more common among younger women (OR 0.93; 95% CI 0.88–0.99) and women with a lower level of education (OR 2.98; 95% CI 1.6–5.5), as well as among women with lower household income (OR 0.98; 95% CI 0.96–0.99).
Six out of ten women (61.6%) consumed 0–1 standard glasses of alcohol per week. Being older was the only background characteristic of the women who were consuming alcohol weekly (p = 0.001).
Lifestyle modifications
One-third of the women in our study made few (i.e. 0–1) health-promoting lifestyle modifications during the time they were trying to conceive. One out of four reduced their consumption of tobacco, and 37% changed their alcohol-drinking habits (Table 2).
Associations between background characteristics and health-promoting actions/lifestyle changes
The univariate analyses (Table 3) showed association between household income, level of education, duration of infertility, country of birth, parents’ country of birth, BMI, the intensity level of information searching, and taking folic acid supplements (p < 0.05). However, the multivariate logistic regression model (Table 4) showed that women with a higher education level and higher level of searching for information about fertility took folic acid more often (OR 1.8; 95% CI 1.1–2.9 and OR 2.1; 95% CI 1.2–3.8, respectively). The multivariate logistic regression model did not show any significant associations with other variables.
Age, household income, education level, and occupation in our analysis associated with decrease or stop in tobacco use in the univariate test. The only background characteristic remaining in the multivariate logistic regression model was that change in tobacco use was more common among women with a lower education level (OR 2.2; 95% CI 1.3–3.7).
The women were divided into three groups according to their BMI (in kg/m2): underweight to normal with BMI <24.9 in 60.9% (n = 273); overweight with BMI 25–29.9 in 23.9% (n = 107); and obese with BMI ≥30 in 12.5% (n = 56). There was an association between the level of physical activity/changing to a more healthy diet and BMI, with an overrepresentation among overweight and obese women (p < 0.001). The obese women exercised more and changed to healthy diets more frequently (OR 7.43; 95% CI 3.7–14.9), but despite their efforts they showed no significant decrease in weight compared to their reported weight 1 year earlier.
The reported level of understanding of the Swedish language was the only factor in our analysis that could be associated with a decrease in alcohol consumption (p = 0.019). Age, country of birth, parents’ country of birth, understanding of Swedish, information-searching intensity, and higher BMI were associated with the number of health-promoting actions taken by the women during the time they were trying to conceive (p < 0.05).
Discussion
This is the first large-scale Swedish study focusing on lifestyle behaviors among women with infertility problems. One interesting finding was that approximately 50% of the women in the study retained habits with negative effects on fertility, although a majority made initially one or more health-promoting lifestyle changes. One would assume that women not succeeding to conceive would be motivated to learn more about this and try to avoid less favorable habits. Screening for lifestyle factors and correcting those negatively affecting reproductive health should be emphasized in the initial stage of infertility treatment and preferably when women start their planning to become pregnant.
Obese women have an increased risk of subfecundity and infertility (23), and miscarriage rates and pregnancy complications are higher in this group (24,25). In our sample, as many as one-fourth were classified as overweight and 12.5% as obese, which is similar to the distribution of weight found among women in early pregnancy in antenatal care in Sweden (26). A recent study has shown that using motivational interviewing in a weight control program for pregnant women resulted in a significant weight loss in treated women compared to a control group (27). This indicates that a meaningful weight loss can be achieved with effective interventions.
In our study, women with a low level of education had changed their tobacco use habits more, probably because they were the ones using more tobacco in the first place. They also tended to be younger and having a lower household income than women who made no changes in tobacco-use habits. This is worrying because the negative consequences of tobacco use, such as an increased risk of infertility, pregnancy loss, preterm delivery, and fetal growth retardation, are well established (28–30).
The use of tests for predicting the time of ovulation was extensive among women in our study, possibly because many women have a poor understanding of their menstrual cycle and of the timing of ovulation. It has been suggested that timing intercourse to coincide with ovulation by using ovulation tests might lead to emotional distress; however, the evidence to support this hypothesis is limited (31).
Another interesting result in our study was that six out of ten women started to take folic acid supplements when they started their attempts to become pregnant, but 11% stopped after some time. Other studies have shown that only three out of ten women, regardless of whether the pregnancy was being well planned, complied with the recommendation from public health authorities of an intake of 400 μg/day of folic acid via supplements for women planning a pregnancy in order to prevent neural tube defects (32–34). Obviously more information to all women planning a pregnancy is needed.
Our results indicate that greater efforts are needed to improve compliance with the recommendations for subfertile women, as, surprisingly, more than half of the women seeking help for infertility do not comply with these recommendations and do not adjust their lifestyle accordingly. A study from the United Kingdom showed that only 2.9% complied fully with the recommendations for alcohol and folic acid intake during the 3 months before becoming pregnant (35). Low compliance with nutrition and lifestyle recommendations when planning a pregnancy has also been reported in studies from the USA (36) and Iran (37). The FAST Study by Homan et al. (38) showed that an individualized assessment of current lifestyle behaviors for couples attending a fertility clinic, followed by continuous support, is likely to achieve healthy lifestyle changes. An individually tailored plan was developed, including strategies to achieve realistic goals in terms of lifestyle changes, as well as referrals to allied health professionals, e.g. dieticians, physiotherapists, and counselors. Results from a study in the Netherlands suggest that tailored preconceptional dietary and lifestyle counseling is effective among subfertile couples to change unhealthy behaviors within a period of 3 months (39).
This indicates that it is possible to change unhealthy lifestyle factors to reduce or even eliminate them in order to enhance the chances of conception.
The response rate (62%) was satisfactory compared to other similar studies in Sweden (40). It may be worth considering whether the response rate could have been increased if respondents had been offered a free choice between a paper-based and a web-based questionnaire (41). The relatively high proportion of women of non-Swedish origin (14%) is considered to be a strength of this study. However, we used a retrospective measure for estimating the incidences of health-promoting actions and lifestyle changes, which could be either overestimated or underestimated. It is well known that people underreport alcohol intake and smoking, and this might have resulted in an overestimation of the women’s positive health behaviors.
Conclusions
Detecting and changing unfavorable lifestyles is essential for improving spontaneous fertility and ART results. One-third of the studied women were overweight or obese, and some had other lifestyle factors with adverse effects on fertility. Obese women adjusted their habits, but there was no adequate change in their weight. Women of a fertile age would benefit from preconception counseling. Infertility treatment should routinely offer interventions for lifestyle changes.
Supplementary Material
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Funding information
Grants were received from the Foundation Family Planning Fund in Uppsala, the Uppsala County Council, the College of Medicine at Uppsala University, Sweden, Västmanland County Council, Sweden, and the Uppsala-Örebro Regional Research Council, Sweden (LTV-218591, RFR-387811).
References
- 1.Homan GF, Davies M, Norman R.. The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Hum Reprod Update. 2007;13:209–23. [DOI] [PubMed] [Google Scholar]
- 2.Anderson K, Nisenblat V, Norman R.. Lifestyle factors in people seeking infertility treatment—a review: Invited Review. Aust New Zeal J Obstet Gynaecol. 2010;50:8–20. [DOI] [PubMed] [Google Scholar]
- 3.Anderson K, Norman R, Middleton P.. Preconception lifestyle advice for people with subfertility. Cochrane Database Syst Rev. 2010;(4):CD008189. [DOI] [PubMed] [Google Scholar]
- 4.European Commission. Directorate-General for Employment SA and EO . Demography Report 2010: Older, more numerous and diverse European. ISSN 1831-9440, Demography. Luxembourg; 2011. [Google Scholar]
- 5.European Commission. Fertility statistics. Eurostat [Internet]. Population structure and ageing - Statistics Explained. 2015; (June 2015):1–10. Available from: http://ec.europa.eu/eurostat/statistics-explained/index.php/Population_structure_and_ageing. [Google Scholar]
- 6.Eriksson C, Larsson M, Tydén T.. Reflections on having children in the future—interviews with highly educated women and men without children. Ups J Med Sci. 2012;117:328–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson J-A, Tough S.. Delayed child-bearing. J Obstet Gynaecol Can. 2012;34:80–93. [DOI] [PubMed] [Google Scholar]
- 8.Sharma R, Biedenharn KR, Fedor JM, Agarwal A.. Lifestyle factors and reproductive health: taking control of your fertility. Reprod Biol Endocrinol. 2013;11:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kelly-Weeder S, O’Connor A.. Modifiable risk factors for impaired fertility in women: what nurse practitioners need to know. J Am Acad Nurse Pract. 2006;18:268–76. [DOI] [PubMed] [Google Scholar]
- 10.Vause TDR, Jones L, Evans M, Wilkie V, Leader A.. Pre-conception health awareness in infertility patients. J Obstet Gynaecol Can. 2009;31:717–20. [DOI] [PubMed] [Google Scholar]
- 11.Stephenson J, Patel D, Barrett G, Howden B, Copas A, Ojukwu O, et al. How do women prepare for pregnancy? Preconception experiences of women attending antenatal services and views of health professionals. PLoS One. 2014;9:e103085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Backhausen MG, Ekstrand M, Tydén T, Magnussen BK, Shawe J, Stern J, et al. Pregnancy planning and lifestyle prior to conception and during early pregnancy among Danish women. Eur J Contracept Reprod Heal Care. 2014;19:57–65. [DOI] [PubMed] [Google Scholar]
- 13.ESHRE. Routine psychosocial care in infertility and medically assisted reproduction – A guide for fertility staff. 2015;(March):1–162. Available from: http://www.eshre.eu/~/media/Files/Guidelines/Psychology/ESHRE psychology guideline_2015_final_version 1_2.pdf [DOI] [PubMed] [Google Scholar]
- 14.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC.. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol. 2007;110:1050–8. [DOI] [PubMed] [Google Scholar]
- 15.Gardiner PM, Nelson L, Shellhaas CS, Dunlop AL, Long R, Andrist S, et al. The clinical content of preconception care: nutrition and dietary supplements. Am J Obstet Gynecol. 2008;199(6 Suppl 2):S345–S56. [DOI] [PubMed] [Google Scholar]
- 16.Bell M, Billington R, Becker B.. A scale for the assessment of object relations: reliability, validity, and factorial invariance. J Clin Psychol. 1986;42:733–41. [DOI] [PubMed] [Google Scholar]
- 17.Zigmond AS, Snaith RP.. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- 18.Cox JL, Holden JM, Sagovsky R.. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. [DOI] [PubMed] [Google Scholar]
- 19.Rubertsson C, Wickberg B, Gustavsson P, Rådestad I.. Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Arch Womens Ment Health. 2005;8:97–104. [DOI] [PubMed] [Google Scholar]
- 20.McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, et al. The Arizona Sexual Experience Scale (ASEX): reliability and validity. J Sex Marital Ther. 2000;26:25–40. [DOI] [PubMed] [Google Scholar]
- 21.Bergman H, Kallmen H, Rydberg U, Sandahl C.. [Ten questions about alcohol as identifier of addiction problems. Psychometric tests at an emergency psychiatric department]. Lakartidningen. 1998;95:4731–5. [PubMed] [Google Scholar]
- 22.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. [DOI] [PubMed] [Google Scholar]
- 23.Van Der Steeg JW, Steures P, Eijkemans MJC, Habbema JDF, Hompes PG, Burggraaff JM, et al. Obesity affects spontaneous pregnancy chances in subfertile, ovulatory women. Hum Reprod. 2008;23:324–8. [DOI] [PubMed] [Google Scholar]
- 24.Boots C, Stephenson MD.. Does obesity increase the risk of miscarriage in spontaneous conception: a systematic review. Semin Reprod Med. 2011;29:507–13. [DOI] [PubMed] [Google Scholar]
- 25.Johansson S, Villamor E, Altman M, Bonamy A-KE, Granath F, Cnattingius S.. Maternal overweight and obesity in early pregnancy and risk of infant mortality: a population based cohort study in Sweden. BMJ. 2014;349:g6572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sweden Statistics . Pregnancies, births and newborns - Medical Birth Register 1973–2013 - Assisted fertilization 1991–2012. 2015;2014–15. [Google Scholar]
- 27.West DS, Gorin AA, Subak LL, Foster G, Bragg C, Hecht J, et al. A motivation-focused weight loss maintenance program is an effective alternative to a skill-based approach. Int J Obes (Lond). 2011;35:259–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Augood C, Duckitt K, Templeton AA.. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod. 1998;13:1532–9. [DOI] [PubMed] [Google Scholar]
- 29.Kharrazi M, DeLorenze GN, Kaufman FL, Eskenazi B, Bernert JT, Graham S, et al. Environmental tobacco smoke and pregnancy outcome. Epidemiology. 2004;15:660–70. [DOI] [PubMed] [Google Scholar]
- 30.Zaren B, Lindmark G, Wibell L, Folling I.. The effect of smoking on glucose homeostasis and fetal growth in pregnant women. Ups J Med Sci. 2000;105:41–56. [DOI] [PubMed] [Google Scholar]
- 31.Severy LJ, Robinson J, Findley-Klein C, McNulty J.. Acceptability of a home monitor used to aid in conception: psychosocial factors and couple dynamics. Contraception. 2006;73:65–71. [DOI] [PubMed] [Google Scholar]
- 32.Wilson RD, Johnson J-A, Wyatt P, Allen V, Gagnon A, Langlois S, et al. Pre-conceptional vitamin/folic acid supplementation 2007: the use of folic acid in combination with a multivitamin supplement for the prevention of neural tube defects and other congenital anomalies. J Obstet Gynaecol Can. 2007;29:1003–26. [DOI] [PubMed] [Google Scholar]
- 33.Stern J, Salih Joelsson L, Tydén T, Berglund A, Ekstrand M, Hegaard H, et al. Is pregnancy planning associated with background characteristics and pregnancy planning behavior? Acta Obstet Gynecol Scand. 2016;95:182–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tyden T, Stern J, Nydahl M, Berglund A, Larsson M, Rosenblad A, et al. Pregnancy planning in Sweden – a pilot study among 270 women attending antenatal clinics. Acta Obstet Gynecol Scand. 2011;90:408–12. [DOI] [PubMed] [Google Scholar]
- 35.Inskip HM, Crozier SR, Godfrey KM, Borland SE, Cooper C, Robinson SM.. Women’s compliance with nutrition and lifestyle recommendations before pregnancy: general population cohort study. BMJ. 2009;338:b481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Domar AD, Conboy L, Denardo-Roney J, Rooney KL.. Lifestyle behaviors in women undergoing in vitro fertilization: a prospective study. Fertil Steril. 2012;97:697–701.e1. [DOI] [PubMed] [Google Scholar]
- 37.Mirghafourvand M, Sehhati F, Rahimi M.. Health-promoting lifestyle and its demographic predictors in infertile couples referred to infertility clinic of Tabriz Al-Zahra Hospital, 2013. J Caring Sci. 2014;3:175–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Homan G, Litt J, Norman RJ.. The FAST study: Fertility Assessment and advice Targeting lifestyle choices and behaviours: a pilot study. Hum Reprod. 2012;27:2396–404. [DOI] [PubMed] [Google Scholar]
- 39.Hammiche F, Laven JSE, Van Mil N, De Cock M, De Vries JH, Lindemans J, et al. Tailored preconceptional dietary and lifestyle counselling in a tertiary outpatient clinic in the Netherlands. Hum Reprod. 2011;26:2432–41. [DOI] [PubMed] [Google Scholar]
- 40.Wenemark M. The respondent's perspective in health-related surveys: the role of motivation [Dissertation]. Linköping University: Department of Medical and Health Sciences; 2010. [Google Scholar]
- 41.Christensen AI, Ekholm O, Glümer C, Juel K.. Effect of survey mode on response patterns: comparison of face-to-face and self-administered modes in health surveys. Eur J Public Health. 2014;24:327–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.