Abstract
BACKGROUND
The black-white maternal mortality disparity is the largest disparity among all conventional population perinatal health measures and the mortality gap between black and white women in New York City has nearly doubled in recent years. For every maternal death, 100 women experience severe maternal morbidity, a life threatening diagnosis or undergo a lifesaving procedure during their delivery hospitalization. Like maternal mortality, severe maternal morbidity is more common among black than white women. A significant portion of maternal morbidity and mortality is preventable making quality of care in hospitals a critical lever for improving outcomes. Hospital variation in risk-adjusted severe maternal morbidity rates exists. The extent to which variation in hospital performance on severe maternal morbidity rates contributes to black-white disparities in New York City hospitals has not been studied.
OBJECTIVE
We examined the extent to which black-white differences in severe maternal morbidity rates in New York City hospitals can be explained by differences in the hospitals in which black and white women deliver.
STUDY DESIGN
We conducted a population-based study using linked 2011–2013 New York City discharge and birth certificate datasets (N= 353,773 deliveries) to examine black-white differences in severe maternal morbidity rates in New York City hospitals. Mixed-effects logistic regression with a random hospital-specific intercept was used to generate risk-standardized severe maternal morbidity rates for each hospital (N=40). We then assessed differences in the distributions of black and white deliveries among these hospitals.
RESULTS
Severe maternal morbidity occurred in 8,882 deliveries (2.5%) and was higher among black than white women (4.2% vs. 1.5%, p<.001). After adjustment for patient characteristics and comorbidities the risk remained elevated for black women (odds ratio=2.02; 95% CI 1.89–2.17). Risk-standardized severe maternal morbidity rates among New York City hospitals ranged from 0.8 to 5.7 per 100 deliveries. White deliveries were more likely to be delivered in low morbidity hospitals: 65% of white versus 23% of black deliveries occurred in hospitals in the lowest tertile for morbidity. We estimated that black-white differences in delivery location may contribute as much as 47.7% of the racial disparity in severe maternal morbidity rates in New York City.
CONCLUSION
Black mothers are more likely to deliver at higher risk-standardized severe maternal morbidity hospitals than are white mothers, contributing to black-white disparities. More research is needed to understand the attributes of high performing hospitals and to share best practices among hospitals.
Keywords: disparities, hospital, severe maternal morbidity
Black women are 12 times more likely to suffer a pregnancy-related death than are white women in New York City.1 This disparity is three to four times greater than the US black-white maternal mortality disparity.2 Not only are there striking racial disparities in maternal mortality rates but overall performance on the maternal mortality ratio (MMR) – the number of maternal deaths per 100,000 live births – in the US is poor compared to other countries: we rank 60th among World Health Organization member nations.3 For every maternal death, 100 women experience severe maternal morbidity.4,5 Similar to racial/ethnic disparities in maternal mortality, black women are more likely to suffer from severe maternal morbidity than white women.4
Quality of health care in hospitals is a critical lever for improving outcomes as data suggest over one-third of maternal morbidity and mortality is preventable.6–9 Obstetrical complications are sensitive to the quality of care provided at delivery,10,11 and variations in the quality of maternal care across hospitals exists.12,13 The contribution of hospital quality to racial disparities in obstetrical outcomes has been less studied. The few studies that have examined this topic suggest that racial/ethnic minority women often deliver in lower quality hospitals.14,15 In our previous work investigating quality measures and severe maternal morbidity in New York City,16 we found wide variation in hospital performance. The objective for this study was to examine whether variation in hospital performance on severe maternal morbidity in New York City hospitals contributes to black-white disparities in this outcome. We focus on the black-white severe maternal morbidity disparity, as black-white maternal mortality represents the largest disparity among all the conventional perinatal health measures and the mortality gap between black and white women in NYC has nearly doubled in recent years.1,2
MATERIALS AND METHODS
DATA SOURCE
We used Vital Statistics birth records linked with New York State discharge abstract data - The Statewide Planning and Research Cooperative System (SPARCS) for all delivery hospitalizations in New York City from 2011–2013. Data linkage was conducted by the New York State Department of Health and 98.8% of maternal discharge abstracts were linked with infant live birth certificates. Institutional Review Board approvals were obtained from the New York City Department of Health and Mental Hygiene, the New York State Department of Health, and the Icahn School of Medicine at Mount Sinai. Delivery hospitalizations were identified based on ICD-9-CM diagnosis and procedure codes and DRG delivery codes.17 From linked records, four hospitals with annual delivery volumes less than five births and 1360 deliveries with missing hospital identifiers were excluded. The final sample included 353,773 deliveries at 40 hospitals.
SEVERE MATERNAL MORBIDITY
We used a published algorithm to identify severe maternal morbidity, using diagnoses for life-threatening conditions (e.g. renal failure, eclampsia) and procedure codes for life-saving procedures (e.g. hysterectomy, ventilation, blood transfusion) defined by investigators from the Centers for Disease Prevention and Controls (CDC).5,18 As specified by the algorithm we excluded hospitalizations with a length of stay less than the 90th percentile as calculated separately for vaginal, primary, and repeat cesarean deliveries.5 All severe maternal morbidity hospitalizations associated with in-hospital mortality and transfer as well as severe complications identified by procedure codes were included regardless of the length of stay, as recommended.5 Transfers were defined as discharge disposition after delivery or source of admission for delivery as specified.5
COVARIATES
To risk-adjust hospital-level rates of maternal morbidity we used variables from the vital statistics records, including mothers’ sociodemographic characteristics (maternal age, self-identified race and ethnicity, parity, education), prenatal care visits, and clinical and obstetric factors (multiple pregnancy, history of previous cesarean delivery, body mass index). New York City Vital Statistics collect self-identified race and ethnicity data. We ascertained patient insurance status from SPARCS. We also included diagnoses for patient risk factors that could lead to maternal morbidity but were likely present on admission to the hospital (e.g. diabetes, hypertension, obesity, premature rupture of membranes, disorders of placentation). These conditions have been used to risk-adjust for severe maternal morbidity,19 cesarean deliveries, and other maternal outcomes.16,20,21
We obtained teaching status from the American Hospital Association, ownership and nursery level from the New York State Department of Health, and volume of deliveries in each hospital from SPARCS to assess how other hospital characteristics are correlated with severe maternal morbidity.
ANALYSIS
We compared the sociodemographic characteristics and clinical conditions of black and white women using Chi Square tests. We used mixed-effects logistic regression with a random hospital-specific intercept to generate risk-standardized severe maternal morbidity rates (SSMMR) for each hospital. The models included covariates described above. Hospital risk-standardized rates were computed from these models using methods recommended by Centers for Medicare and Medicaid Services (CMS) Hospital Compare.16,22 These rates were the ratio of predicted to expected severe maternal morbidity rates, multiplied by the New York City average severe maternal morbidity rate. For each hospital, the numerator of the ratio is the number of severe maternal morbidity cases predicted on the bases of the hospital’s performance with its case-mix, and the denominator is the number of severe maternal morbidity cases expected on the bases of the New York City performance with that hospital’s case mix. We ranked hospitals from lowest to highest risk-standardized severe maternal morbidity rates. These analyses did not include hospital-level variables. We conducted a sensitivity analysis using observed to expected rates for hospital ranking and found that rankings differed very little between the CMS model and the standard observed to expected ratio. In addition, because blood transfusions are an important component of severe maternal morbidity, we examined the correlation between hospital rankings based on severe maternal morbidity with and without blood transfusion.
To assess racial disparities in the use of hospitals with the lowest morbidity rates, we calculated the cumulative distributions of births among hospitals ranked from the lowest to the highest standardized morbidity rate for black and white mothers. We used the Kolmogorov-Smirnov test to assess whether the distributions of deliveries among hospitals differed for white and black women.23
To address the effects on black severe maternal morbidity rates of these differences in delivery location, we conducted a thought experiment and asked what would happen if black mothers went to the same hospitals as white mothers? We used the same risk-standardized morbidity model and kept all individual patient characteristics the same. We calculated the predicted probability of morbidity for each black mother at each hospital. For each black mother, we took the weighted average of these probabilities, where weights were the percentage of white mothers who went to each hospital. The difference between the predicted probability at the hospital a black mother went to and the weighted average probability if the black mother delivered at the white mother’s hospital is the decrease or increase in the probability of a morbid event. The sum of the difference in probabilities across all black women is the morbid events avoided if black mothers went to the same hospitals as white mothers, or the morbid events due to “between-hospital” disparities. A recent simulation study tested this approach against the more common approach of identifying “minority serving” facilities based on the percentage of black patients at a hospital and found that it more accurately measured the magnitude of between-hospital disparities, although both were successful at identifying the existence of disparities.24
To investigate the association between hospital characteristics and severe maternal morbidity rates, we estimated the mixed-effects logistic regression that included maternal sociodemographic and clinical factors as well as the hospital characteristics described above.
All statistical analysis was performed using the SAS system software version 9.3 (SAS Institute Inc, Cary, NC).
RESULTS
Black mothers accounted for 21% and white mothers for 32% of the 353,773 deliveries in New York City in 2011–2013. The remainder of the births were to Hispanics (29.9%), Asian/Pacific Islanders (16.7%) and others (1.6%). Table 1 shows the sociodemographic and clinical characteristics of black and white deliveries in our study sample. Severe maternal morbidity rates were higher among black (4.2%) as compared with white (1.5%) mothers. As shown in Table 1, maternal characteristics differed significantly between black and white women.
Table 1.
Socio-demographic, Clinical and Hospital Characteristics of Deliveries by Race and Ethnicity in New York City Hospitals
| Black | White | P value | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Deliveries | 72849 | 100.00 | 110200 | 100.00 | |
| Maternal Age | <.0001 | ||||
| <20 | 5207 | 7.15 | 1341 | 1.22 | |
| 20–29 | 34815 | 47.79 | 37812 | 34.31 | |
| 30–34 | 17859 | 24.52 | 38161 | 34.63 | |
| 35–39 | 11159 | 15.32 | 25135 | 22.81 | |
| 40–44 | 3477 | 4.77 | 7079 | 6.42 | |
| 45+ | 332 | 0.46 | 672 | 0.61 | |
| Ancestry | <.0001 | ||||
| US Born | 42189 | 57.91 | 79935 | 72.54 | |
| Foreign Born | 30660 | 42.09 | 30265 | 27.46 | |
| Pre-pregnancy body mass index | <.0001 | ||||
| Underweight (<18.5) | 2632 | 3.61 | 6549 | 5.94 | |
| Normal weight (18.5–24.9) | 27782 | 38.14 | 73017 | 66.26 | |
| Overweight (25.0–29.9) | 21231 | 29.14 | 20234 | 18.36 | |
| Obese (30.0–39.9) | 17212 | 23.63 | 9006 | 8.17 | |
| Morbid Obesity (≥40) | 3407 | 4.68 | 1120 | 1.02 | |
| Missing BMI | 585 | 0.80 | 274 | 0.25 | |
| Smoked during pregnancy | 2673 | 3.67 | 2573 | 2.33 | <.0001 |
| Alcohol use during pregnancy | 1141 | 1.57 | 1220 | 1.11 | <.0001 |
| Maternal Education | <.0001 | ||||
| Less than HS | 14606 | 20.05 | 8726 | 7.92 | |
| HS | 19614 | 26.92 | 20612 | 18.70 | |
| Greater than HS | 38232 | 52.48 | 80620 | 73.16 | |
| Missing or unknown | 397 | 0.54 | 242 | 0.22 | |
| Insurance | <.0001 | ||||
| Commercial | 18299 | 25.12 | 70105 | 63.62 | |
| Medicaid | 52683 | 72.32 | 38532 | 34.97 | |
| Other | 607 | 0.83 | 815 | 0.74 | |
| Uninsured | 1260 | 1.73 | 748 | 0.68 | |
| Prenatal visits | <.0001 | ||||
| 0–5 | 8623 | 11.84 | 3737 | 3.39 | |
| 6–8 | 11508 | 15.80 | 11052 | 10.03 | |
| ≥9 | 51658 | 70.91 | 94833 | 86.06 | |
| Unknown | 1060 | 1.46 | 578 | 0.52 | |
| Parity | <.0001 | ||||
| Nulliparous | 41033 | 56.33 | 58308 | 52.91 | |
| Multiparous | 31698 | 43.51 | 51746 | 46.96 | |
| Missing | 118 | 0.16 | 146 | 0.13 | |
| Type of Pregnancy | <.0001 | ||||
| Singleton | 71359 | 97.95 | 107165 | 97.25 | |
| Multiple | 1490 | 2.05 | 3035 | 2.75 | |
| Previous Cesarean Comorbidities | 13031 | 17.89 | 15959 | 14.48 | <.0001 |
| Cardiac Disease | 310 | 0.43 | 616 | 0.56 | <.0001 |
| Renal Disease | 68 | 0.09 | 49 | 0.04 | <.0001 |
| Musculoskeletal Disease | 225 | 0.31 | 341 | 0.31 | 0.98 |
| Digestive Disorder | 17 | 0.02 | 269 | 0.24 | <.0001 |
| Blood Disease | 10557 | 14.49 | 9013 | 8.18 | <.0001 |
| Mental Disorders | 3032 | 4.16 | 3364 | 3.05 | <.0001 |
| CNS disease | 905 | 1.24 | 1310 | 1.19 | 0.31 |
| Rheumatic Heart Disease | 57 | 0.08 | 33 | 0.03 | <.0001 |
| Disorder Placentation | 1600 | 2.20 | 1599 | 1.45 | <.0001 |
| Chronic Hypertension | 2222 | 3.05 | 807 | 0.73 | <.0001 |
| Pregnancy Hypertension | 7576 | 10.40 | 4411 | 4.00 | <.0001 |
| Lupus | 147 | 0.20 | 117 | 0.11 | <.0001 |
| Collagen Vascular Disorder | 24 | 0.03 | 72 | 0.07 | 0.003 |
| Rheumatoid Arthritis | 61 | 0.08 | 149 | 0.14 | 0.0015 |
| Diabetes | 1200 | 1.65 | 585 | 0.53 | <.0001 |
| Gestational diabetes | 4455 | 6.12 | 3534 | 3.21 | <.0001 |
| Asthma/Chronic bronchitis | 5671 | 7.78 | 3174 | 2.88 | <.0001 |
| Delivery method | <.0001 | ||||
| Cesarean Delivery | 27671 | 37.98 | 31405 | 28.50 | |
| Vaginal delivery | 45178 | 62.02 | 78795 | 71.50 | |
| Hospital Characteristics | |||||
| Hospital Ownership | <.0001 | ||||
| Public | 19595 | 26.90 | 3574 | 3.24 | |
| Private | 53254 | 73.10 | 106626 | 96.76 | |
| Teaching Status | <.0001 | ||||
| Not Teaching | 1237 | 1.70 | 1200 | 1.09 | |
| Teaching | 71612 | 98.30 | 109000 | 98.91 | |
| Nursery Level | <.0001 | ||||
| Level 2 | 5725 | 7.86 | 7219 | 6.55 | |
| Level 3–4 | 67124 | 92.14 | 102981 | 93.45 | |
| Delivery Volume | <.0001 | ||||
| Low | 12464 | 17.11 | 3143 | 2.85 | |
| Medium | 21473 | 29.48 | 4203 | 3.81 | |
| High | 17228 | 23.65 | 22954 | 20.83 | |
| Very High | 21684 | 29.77 | 79900 | 72.50 | |
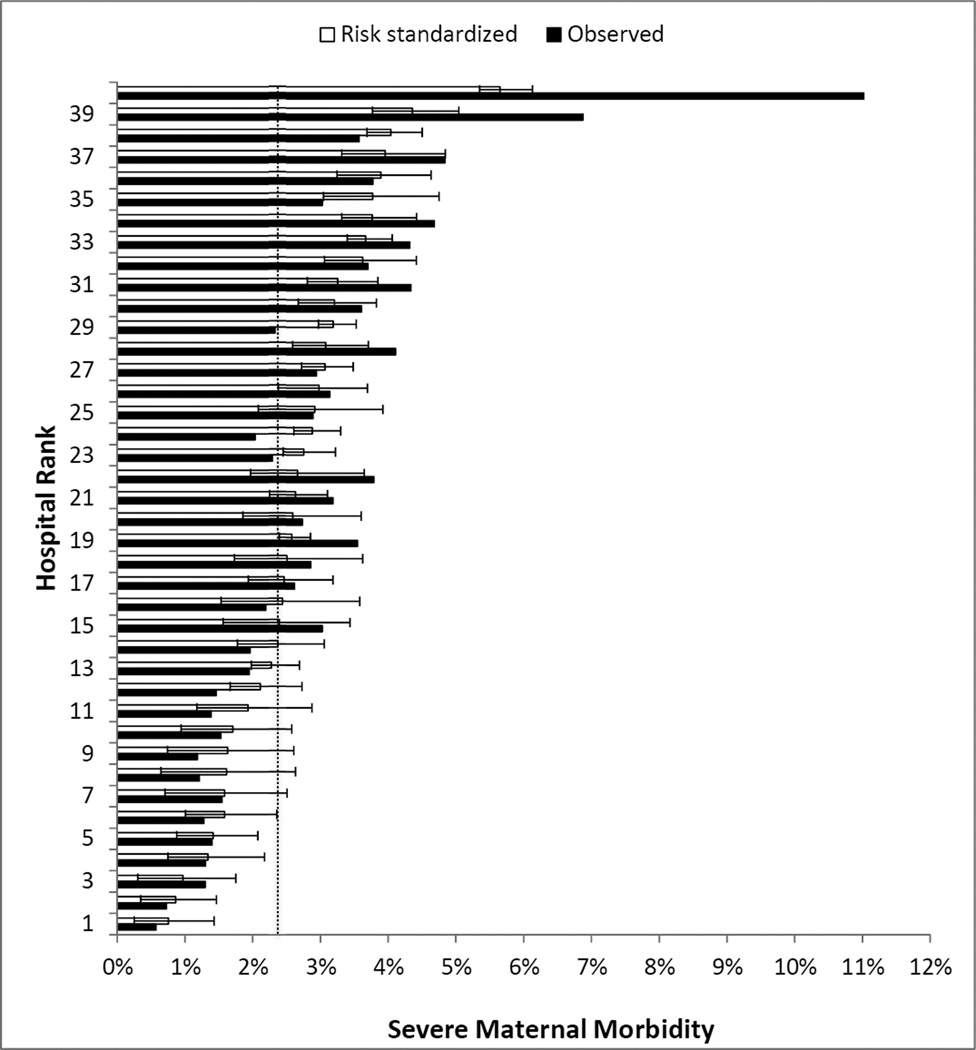
The majority of the 40 hospitals were private, had Level 3/4 nurseries, and were teaching hospitals.16 The median percent of black deliveries was 18.4 (IQR 9.5–35.8%). Hospitals were ranked according to risk-standardized morbidity rates, using a model that included maternal sociodemographic and clinical characteristics associated with severe maternal morbidity (Table 2, model 1). Unadjusted severe morbidity rates ranged from 0.6% to 11.5% and risk standardized rates from 0.8% to 5.7% (Figure 1). The risk standardized morbidity rate for the highest morbidity tertile of hospitals was 3.8% compared with 1.5% for the lowest morbidity tertile (p<0.001). Hospital rankings based on severe maternal morbidity with and without blood transfusion were strongly correlated (p<.0001).
Table 2.
| Model 1: Without
Hospital Characteristics Odds Ratio (95% CI) |
P value |
Model 2:
With Hospital Characteristics Odds Ratio (95% CI) |
P value |
|
|---|---|---|---|---|
| Maternal Age | ||||
| <20 | 1.20 (1.09–1.33) | 1.19 (1.07–1.31) | 0.05 | |
| 20–34 | Reference | Reference | ||
| 35–39 | 1.20 (1.13–1.27) | 0.02 | 1.21 (1.14–1.29) | 0.03 |
| 40–44 | 1.41 (1.29–1.55) | 0.06 | 1.42 (1.30–1.57) | 0.04 |
| >45 | 1.84 (1.45–2.34) | <0.001 | 1.85 (1.46–2.35) | <.001 |
| Maternal race/ethnicity | ||||
| Hispanic | 1.52 (1.42–1.63) | 0.01 | 1.40 (1.31–1.51) | |
| Non-Hispanic black | 2.02 (1.89–2.17) | <0.001 | 1.82 (1.69–1.95) | <.001 |
| Non-Hispanic white | Reference | Reference | ||
| Asian | 1.08 (0.99–1.18) | <0.001 | 1.09 (0.99–1.18) | 0.002 |
| Other | 1.31 (0.85–2.04) | 0.91 | 1.43 (1.31–1.51) | 0.90 |
| Maternal nativity | ||||
| Born in the US | 0.97 (0.92–1.01) | 0.16 | 0.97 (0.93–1.02) | 0.28 |
| Foreign born | Reference | Reference | ||
| Maternal Education | ||||
| Less than HS* | 1.12 (1.05–1.19) | 0.01 | 1.08 (1.008–1.15) | 0.07 |
| HS | 1.02 (0.96–1.09) | <0.001 | 1.00 (0.94–1.06) | <.001 |
| Greater than HS | Reference | Reference | ||
| Insurance | ||||
| Commercial | Reference | Reference | ||
| Uninsured | 1.27 (1.05–1.53) | 0.08 | 1.11 (0.92–1.35) | 0.43 |
| Medicaid | 1.12 (1.05–1.19) | 0.80 | 1.01 (0.95–1.08) | 0.41 |
| Other | 1.06 (0.82–1.37) | 0.65 | 1.07 (0.83–1.38) | 0.84 |
| Prenatal visits | ||||
| 0–5 | 1.42 (1.31–1.52) | <0.001 | 1.34 (1.24–1.45) | 0.004 |
| 6–8 | 1.19 (1.12–1.27) | 0.30 | 1.16 (1.09–1.24) | 0.31 |
| ≥9 | Reference | Reference | ||
| Unknown | 1.38 (1.13–1.69) | 0.14 | 1.35 (1.11–1.65) | |
| Parity | ||||
| Nulliparous | Reference | Reference | ||
| Multiparous | 0.96 (0.94–0.98) | <0.001 | 0.96 (0.94–0.98) | <.001 |
| Type of Pregnancy | ||||
| Singleton | Reference | Reference | ||
| Multiple | 3.04 (2.76–3.34) | <0.001 | 3.06 (2.78–3.37) | <.001 |
| Pre-pregnancy body mass index | ||||
| Underweight (<18.5) | 1.06 (0.95–1.18) | 0.75 | 0.96 (0.94–0.98) | 0.49 |
| Normal weight (18.5–24.9) | Reference | Reference | ||
| Overweight (25.0–29.9) | 0.99 (0.94–1.05) | 0.15 | 0.98 (0.93–1.04) | 0.15 |
| Obese (30.0–39.9) | 0.96 (0.90–1.02) | 0.01 | 0.94 (0.88–1.004) | 0.01 |
| Morbid obese (≥40) | 1.13 (1.001–1.28) | 0.12 | 1.11 (0.98–1.25) | 0.16 |
| Missing | 1.14 (0.87–1.43) | 0.52 | 1.08 (0.84–1.38) | 0.66 |
| Smoked during pregnancy | 0.93 (0.81–1.06) | 0.28 | 0.92 (0.94–0.98) | 0.19 |
| Alcohol use during pregnancy | 1.16 (0.99–1.35) | 0.07 | 1.11 (0.95–1.3) | 0.21 |
| Previous Cesarean | 2.27 (2.16–2.39) | <0.001 | 2.29 (2.18–2.41) | <.001 |
| Comorbidity | ||||
| Cardiac | 2.90 (2.36–3.94) | <0.001 | 2.91 (2.36–3.59) | <.001 |
| Musculoskeletal | 2.72 (0.96–7.72) | 0.06 | 2.58 (0.91–7.28) | 0.07 |
| Digestive | 1.19 (0.57–2.48) | 0.64 | 1.19 (0.57–2.48) | 0.64 |
| Blood disorder | 3.75 (3.56–3.94) | <0.001 | 3.73 (3.55–3.91) | <.001 |
| Mental disorder | 1.40 (1.26–1.55) | <0.001 | 1.38 (1.25–1.53) | <.001 |
| CNS | 1.37 (1.15–1.62) | <0.001 | 1.37 (1.16–1.62) | <.001 |
| Rheumatic heart | 2.97 (1.81–4.86) | <0.001 | 2.88 (1.76–4.73) | <.001 |
| Disorder of placentation | 6.64 (6.13–7.19) | <0.001 | 6.57 (6.07–7.12) | <.001 |
| Chronic Hypertension | 1.34 (1.17–1.54) | <0.001 | 1.32 (1.15–1.51) | <.001 |
| Pregnancy hypertension | 2.95 (2.78–3.13) | <0.001 | 2.9 (2.73–3.08) | <.001 |
| Lupus | 0.92 (0.32–2.64) | 0.88 | 0.97 (0.34–2.76) | 0.96 |
| Collagen/vascular | 0.45 (0.14–1.52) | 0.2 | 0.46 (0.34–2.76) | 0.21 |
| Rheumatoid arthritis | 0.48 (1.16–1.47) | 0.2 | 0.51 (0.17–1.55) | 0.23 |
| Diabetes | 1.27 (1.08–1.49) | 0.004 | 1.26 (1.08–1.48) | 0.004 |
| Pregnancy diabetes | 1.21 (1.11–1.32) | <0.001 | 1.17 (1.08–1.28) | <.001 |
| Asthma/chronic pulmonary | 1.05 (0.96–1.15) | 0.28 | 1.05 (0.96–1.15) | 0.25 |
| Hospital Characteristics1 | ||||
| Hospital Ownership | ||||
| Public | 1.12 (1.06–1.19) | <.001 | ||
| Private | Reference | |||
| Teaching Status | ||||
| Not Teaching | Reference | |||
| Teaching | 0.66 (0.55–0.79) | <.001 | ||
| Nursery Level | ||||
| Level 2 | 1.27 (1.22–1.33) | <.001 | ||
| Level 3–4 | Reference | |||
| Delivery Volume3 | ||||
| Low | 1.69 (1.54–1.85) | <.001 | ||
| Medium | 1.53 (1.42–1.65) | <.001 | ||
| High | 1.32 (1.23–1.41) | 0.16 | ||
| Very High | Reference |
HS – High school
Figure 1.
Observed and Risk-Standardized Severe Maternal Morbidity Rates in New York City Hospitals. Dotted line shows NYC mean observed severe maternal morbidity. 95% CL for risk standardized SMM is shown.
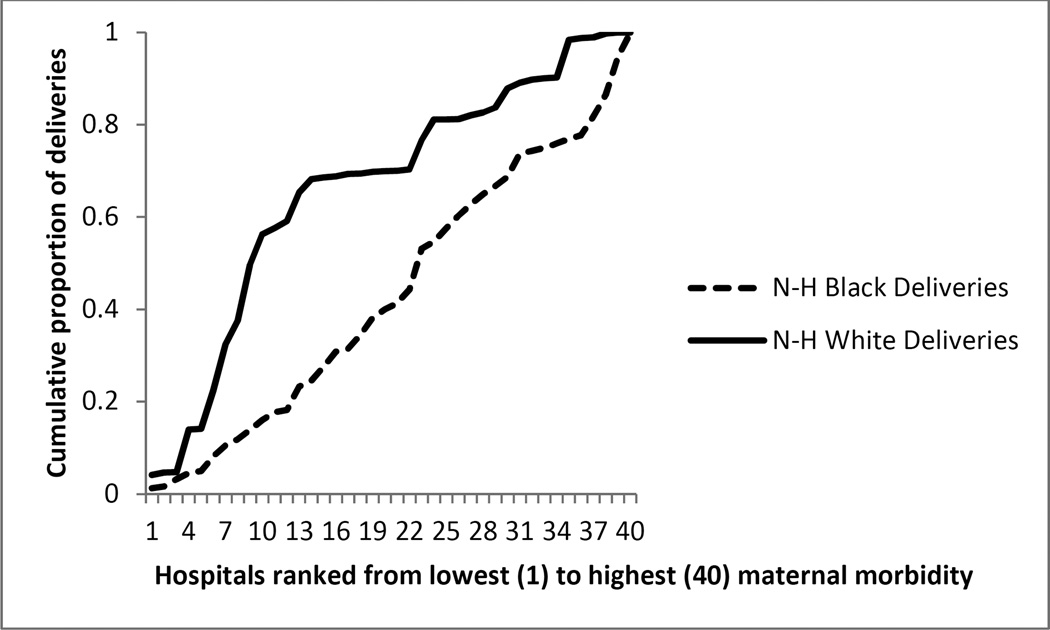
The cumulative distribution of deliveries among hospitals ranked from lowest to highest morbidity rates differed for black and white mothers (p<0.001). The majority of white deliveries (65.3%) occurred in the hospitals in the lowest tertile for severe morbidity compared with 23.3% of all black deliveries. Eighteen percent of white deliveries and 37.3% of black deliveries occurred at hospitals in the highest morbidity tertile (Figure 2).
Figure 2.
Cumulative distributions of deliveries according to hospital, ranked from lowest to highest morbidity ratio, for non-Hispanic (N-H) white mothers and non-Hispanic black mothers.
If black mother mothers delivered in the same hospitals as white women, our simulation model estimated that they would experience 940 fewer severe morbid events, leading to a reduction of black severe maternal morbidity rates by 47.7% from 4.2 to 2.9 (1.3 events per 100 deliveries per year)
Results of our model fitting for severe maternal morbidity rates using maternal and hospital-level variables revealed that teaching status, Level 3/4 nursery, private ownership, and very high volume status were associated with lower severe maternal morbidity rates, but did not fully account for the excess risk among black women.(Table 2, model 2)
COMMENT
Black women are more likely to deliver in New York City hospitals with higher risk-adjusted severe maternal morbidity rates. Severe maternal morbidity rates vary six fold across New York City hospitals. Our data demonstrate that racial differences in the distribution of deliveries may contribute to the black/white disparity in severe maternal morbidity rates in New York City Hospitals. If black women delivered at the same hospitals as white women our results suggest that nearly 1000 black women could avoid a severe morbid event during their delivery hospitalization annually in New York City.
While much of the focus on reducing racial disparities in obstetrics examines social determinants of health, our results highlight the need to address quality of care as an additional means to reduce racial disparities. Data suggest over one-third of maternal deaths and severe events are preventable. 6–9 Current efforts by the American College of Obstetricians and Gynecologists District II, Merck for Mothers, and the New York State Department of Health have made major efforts to standardize care on labor and delivery units and enhance quality.25–28 Data in obstetrics suggest that team building, specific clinical protocols, and improved communication are important targets for quality improvement in the setting of obstetrics and can improve outcomes.27 Our findings suggest quality improvement efforts targeting the lowest performing hospitals may both lower severe maternal morbidity rates for all mothers and narrow the black-white morbidity gap.
Our findings are consistent with a recent study using national data on delivery hospitalizations which found that blacks deliver in a concentrated set of hospitals and these hospitals have higher risk-adjusted severe maternal morbidity rates.14 Unlike this previous study, the current population-based study used a simulation method to quantify the impact of delivery location on the disparity. Others have also found that black-serving hospitals performed worse than other hospitals on delivery-related indicators using data from seven states.15 In pediatrics, investigators have found that black very low birth weight babies are more likely to be delivered in higher risk-adjusted very low birthweight neonatal mortality hospitals and in other areas of medicine including stroke and heart attack care, studies have documented that black and white patients are treated at different sites of care and black patients are often treated at higher mortality hospitals.12,13,29,30 Why hospitals that have a greater proportion of black deliveries experience higher risk-adjusted severe maternal morbidity is not known. Teaching status, level of nursery, volume, and ownership were associated with severe maternal morbidity rates in New York City hospitals but did not fully account for the excess risk among black women.
The reasons why women deliver at specific hospitals is complex and may be related to a number of factors, including where a patient lives, distance to the hospital, patterns of racial segregation, physician referral, risk perception, patient choice, access, insurance, and the management of possible medical emergencies during pregnancy.12,31 Previous studies examining delivery hospital and distance in the setting of very low birth weight births found that distance did not explain why black women were more likely to deliver at higher risk-adjusted neonatal mortality hospitals.31 The extent to which other factors contributed to site of delivery in this study could not be fully evaluated.
Our analysis has some limitations. We used administrative data (ICD-9 procedure and diagnosis codes) that do not contain important clinical data on severity of illness. Both vital statistics and SPARCS have limitations with reliability of specific variables.32,33 We used a published algorithm to identify severe maternal morbidity cases and did not conduct a medical chart review for case ascertainment. Nevertheless we conducted a population-based study and were able to construct a robust risk-adjustment model that included important confounders available in our linked data set (e.g. maternal education, parity, body mass index). We used a simulation model and estimated the extent to which differences in the distribution of deliveries may contribute to disparities. However, similar to others, we were unable to account for unmeasured factors that are associated with both race and severe maternal morbidity. Further, we assumed that unmeasured factors such as social risk are conditionally independent of hospital choice and do not impact choice of hospital after adjusting for a patient’s measured factors, such as race, education, and insurance. If this assumption is false, our simulation results could exaggerate the role of hospital in black-white severe maternal morbidity disparities. In other words, we would attribute higher rates of severe maternal morbidity to the hospital when some of the excess risk should be attributed to the social risk or other characteristics of the patient population. We focused on black-white differences in distribution of deliveries given the significant increase in maternal mortality among black women in New York City.1
We found that differences in the hospitals in which black and white women deliver contribute to the disparity in severe maternal morbidity rates between blacks and whites in New York City hospitals. The increasing excess of maternal deaths and high rate of severe morbid events among black women in New York City are concerning. Our data suggests that efforts to improve care at the lowest performing hospitals may be an important step to reduce these disparities
Acknowledgments
This study was funded by grant number R01MD007651from the National Institute on Minority Health and Health Disparities. The funders of this study had no role in design and conduct of the study, collection, management, analysis, and interpretation of the data, preparation, review, and approval of the manuscript, or the decision to submit the manuscript for publication.
Appendix A. Severe maternal morbidity events and race distribution among hospitals with low (tertile 1) and high (tertile 3) severe maternal morbidity
| Tertile 1, N (%) | Tertile 3, N (%) | P-Value | |
|---|---|---|---|
| Deliveries | 165276 (100) | 87712 (100) | |
| Death1 | <10 (<0.01) | 12 (0.01) | 0.03 |
| Transfers | 345 (0.21) | 457 (0.52) | <0.001 |
| Hysterectomy | 222 (0.13) | 158 (0.18) | 0.005 |
| Ventilation | 118 (0.07) | 147 (0.17) | <0.001 |
| Renal Failure | 103 (0.06) | 141 (0.16) | <0.001 |
| Cardiac Arrest1 | <10 (<0.01) | <10 (<0.01) | 1 |
| Heart Failure Procedure | 333 (0.2) | 452 (0.52) | <0.001 |
| Shock | 72 (0.04) | 73 (0.08) | <0.001 |
| Sepsis | 47 (0.03) | 43 (0.05) | 0.009 |
| Coagulation | 461 (0.28) | 450 (0.51) | <0.001 |
| Amniotic Embolism1 | <10 (0.01) | <10 (<0.01) | 0.07 |
| Thrombotic Embolism | 26 (0.02) | 59 (0.07) | <0.001 |
| Puerperal CVD | 54 (0.03) | 70 (0.08) | <0.001 |
| Anesthesia Complications | 35 (0.02) | 37 (0.04) | 0.003 |
| Pulmonary Edema | 43 (0.03) | 43 (0.05) | 0.003 |
| Respiratory Distress | 85 (0.05) | 101 (0.12) | <0.001 |
| AMI1 | <10 (<0.01) | <10 (<0.01) | 0.42 |
| Eclampsia | 40 (0.02) | 71 (0.08) | <0.001 |
| Blood Transfusion | 1686 (1.02) | 3201 (3.65) | <0.001 |
| Sickle Cell Anemia | 23 (0.01) | 31 (0.04) | <0.001 |
| Intracranial Injury1 | <10 (<0.01) | <10 (<0.01) | 0.35 |
| Injury Thorax/Abdomen/Pelvis1 | <10 (<0.01) | <10 (<0.01) | 0.12 |
| Aneurysm1 | <10 (<0.01) | <10 (<0.01) | 1 |
| Heart Surgery | 86 (0.05) | 95 (0.11) | <0.001 |
| Cardio monitoring1 | <10 (<0.01) | <10 (<0.01) | 1 |
| Tracheostomy1 | <10 (<0.01) | <10 (<0.01)) | 1 |
| Conversion cardiac rhythm | 12 (0.01) | 12 (0.01) | 0.13 |
| Severe Maternal Morbidity | 2253 (1.4) | 3862 (4.4) | <0.001 |
| Race/Ethnicity2 | |||
| Asian | 38640 (23.4) | 8175 (9.3) | <0.001 |
| Black | 16936 (10.3) | 27164 (31.0) | |
| Hispanic | 35004 (21.2) | 30883 (35.2) | <0.001 |
| White | 71993 (43.6) | 19776 (22.6) | |
| Other race | 2703 (1.6) | 1714 (1.9) |
Number of events masked in the compliance with SPARCS regulations
NOTE: differs from percentage given in the manuscript, which measures the percent of black and white women that deliver in each tertile.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This abstract was presented at Academy Health Annual Research Meeting June15, 2015.
The authors report no conflict of interest.
CONDENSATION
Differences in delivery hospital contribute to black-white disparities in severe maternal morbidity rates in New York City hospitals.
REFERENCES
- 1.New York City Department of Health and Mental Hygiene Bureau of Maternal and Child Health. Pregnancy-Associated Mortality New York City, 2006–2010. New York: 2015. [Google Scholar]
- 2.Callaghan WM. Overview of maternal mortality in the United States. Semin Perinatol. 2012 Feb;36(1):2–6. doi: 10.1053/j.semperi.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 3.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 384(9947):980–1004. doi: 10.1016/S0140-6736(14)60696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callaghan WM, Mackay AP, Berg CJ. Identification of severe maternal morbidity during delivery hospitalizations, United States, 1991–2003. Am J Obstet Gynecol. 2008 Aug;199(2) doi: 10.1016/j.ajog.2007.12.020. 133 e131–138. [DOI] [PubMed] [Google Scholar]
- 5.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012 Nov;120(5):1029–1036. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 6.Berg CJ, Atrash HK, Koonin LM, Tucker M. Pregnancy-related mortality in the United States, 1987–1990. Obstet Gynecol. 1996 Aug;88(2):161–167. doi: 10.1016/0029-7844(96)00135-4. [DOI] [PubMed] [Google Scholar]
- 7.Hoyert DL, Danel I, Tully P. Maternal mortality, United States and Canada, 1982–1997. Birth. 2000 Mar;27(1):4–11. doi: 10.1046/j.1523-536x.2000.00004.x. [DOI] [PubMed] [Google Scholar]
- 8.Nannini A, Weiss J, Goldstein R, Fogerty S. Pregnancy-associated mortality at the end of the twentieth century: Massachusetts, 1990–1999. J Am Med Womens Assoc. 2002 Summer;57(3):140–143. [PubMed] [Google Scholar]
- 9.Geller SE, Cox SM, Callaghan WM, Berg CJ. Morbidity and mortality in pregnancy: laying the groundwork for safe motherhood. Womens Health Issues. 2006 Jul-Aug;16(4):176–188. doi: 10.1016/j.whi.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Guendelman S, Thornton D, Gould J, Hosang N. Obstetric complications during labor and delivery: assessing ethnic differences in California. Womens Health Issues. 2006 Jul-Aug;16(4):189–197. doi: 10.1016/j.whi.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Kramer M, Rouleau J, Liu S, Bartholomew S, Joseph K. Amniotic fluid embolism: incidence, risk factors, and impact on perinatal outcome. BJOG. 2012 Jun;119(7):874–879. doi: 10.1111/j.1471-0528.2012.03323.x. [DOI] [PubMed] [Google Scholar]
- 12.Howell EA, Hebert P, Chatterjee S, Kleinman LC, Chassin MR. Black/white differences in very low birth weight neonatal mortality rates among New York City hospitals. Pediatrics. 2008 Mar;121(3):e407–e415. doi: 10.1542/peds.2007-0910. [DOI] [PubMed] [Google Scholar]
- 13.Morales LS, Staiger D, Horbar JD, et al. Mortality among very low-birthweight infants in hospitals serving minority populations. Am J Public Health. 2005 Dec;95(12):2206–2212. doi: 10.2105/AJPH.2004.046730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howell EA, Egorova N, Balbierz A, Zeitlin J, Hebert PL. Black-White Differences in Severe Maternal Morbidity and Site of Care. Am J Obstet Gynecol. 2015 Aug 14; doi: 10.1016/j.ajog.2015.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Creanga AA, Bateman BT, Mhyre JM, Kuklina E, Shilkrut A, Callaghan WM. Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. Am J Obstet Gynecol. 2014 Jun 5; doi: 10.1016/j.ajog.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 16.Howell EA, Zeitlin J, Hebert PL, Balbierz A, Egorova N. Association between hospital-level obstetric quality indicators and maternal and neonatal morbidity. JAMA. 2014 Oct 15;312(15):1531–1541. doi: 10.1001/jama.2014.13381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008 Jul;12(4):469–477. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. [Accessed March 21, 2016];Severe Maternal Morbidity in the United States. http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/SevereMaternalMorbidity.html.
- 19.Gray KE, Wallace ER, Nelson KR, Reed SD, Schiff MA. Population-based study of risk factors for severe maternal morbidity. Paediatr Perinat Epidemiol. 2012 Nov;26(6):506–514. doi: 10.1111/ppe.12011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Srinivas SK, Fager C, Lorch SA. Evaluating risk-adjusted cesarean delivery rate as a measure of obstetric quality. Obstet Gynecol. 2010 May;115(5):1007–1013. doi: 10.1097/AOG.0b013e3181d9f4b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grobman WA, Feinglass J, Murthy S. Are the Agency for Healthcare Research and Quality obstetric trauma indicators valid measures of hospital safety? Am J Obstet Gynecol. 2006 Sep;195(3):868–874. doi: 10.1016/j.ajog.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 22.Ash AS, Normand ST, Stukel TA, Utts J Committee of Presidents of Statistical Societies (COPSS) Statistical Issues in Assessing Hospital Performance. Center for Medicare and Medicaid Services and Yale NewH. 2012 [Google Scholar]
- 23.Hollander M, Wolfe DA. Nonparametric Statistical Methods. Second. New York: John Wiley & Sons; 1999. [Google Scholar]
- 24.Hebert PL, Howell EA, Wong ES, et al. Methods for measuring racial differences in hospitals outcomes attributable to disparities in access to high-quality hospital care. Health Serv Res. doi: 10.1111/1475-6773.12514. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kacica MA. Maternal Mortality Review: New York State Department of Health. 2012
- 26.ACOG Safe Motherhood Initiative. 2015. http://www.acog.org/About-ACOG/ACOG-Districts/District-II/Safe-Motherhood-Initiative-bundles. [Google Scholar]
- 27.Arora KS, Shields LE, Grobman WA, D'Alton ME, Lappen JR, Mercer BM. Triggers, Bundles, Protocols, and Checklists – What Every Maternal Care Provider Needs to Know. Am J Obstet Gynecol. 2015 Oct 15; doi: 10.1016/j.ajog.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 28. [Accessed November 5, 2015];Mothers Mf. 2015 http://www.merckformothers.com/our-work/united-states.html.
- 29.Barnato AE, Lucas FL, Staiger D, Wennberg DE, Chandra A. Hospital-level racial disparities in acute myocardial infarction treatment and outcomes. Med Care. 2005 Apr;43(4):308–319. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005 Feb;36(2):374–386. doi: 10.1161/01.STR.0000153065.39325.fd. [DOI] [PubMed] [Google Scholar]
- 31.Hebert PL, Chassin MR, Howell EA. The contribution of geography to black/white differences in the use of low neonatal mortality hospitals in New York City. Med Care. 2011 Feb;49(2):200–206. doi: 10.1097/MLR.0b013e3182019144. [DOI] [PubMed] [Google Scholar]
- 32.Yasmeen S, Romano PS, Schembri ME, Keyzer JM, Gilbert WM. Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol. 2006 Apr;194(4):992–1001. doi: 10.1016/j.ajog.2005.08.058. [DOI] [PubMed] [Google Scholar]
- 33.DiGiuseppe DL, Aron DC, Ranbom L, Harper DL, Rosenthal GE. Reliability of birth certificate data: a multi-hospital comparison to medical records information. Matern Child Health J. 2002 Sep;6(3):169–179. doi: 10.1023/a:1019726112597. [DOI] [PubMed] [Google Scholar]