Abstract
Purpose We aimed to identify and inventory clinical decision support (CDS) tools for helping front-line staff select interventions for patients with musculoskeletal (MSK) disorders. Methods We used Arksey and O’Malley’s scoping review framework which progresses through five stages: (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies for analysis; (4) charting the data; and (5) collating, summarizing and reporting results. We considered computer-based, and other available tools, such as algorithms, care pathways, rules and models. Since this research crosses multiple disciplines, we searched health care, computing science and business databases. Results Our search resulted in 4605 manuscripts. Titles and abstracts were screened for relevance. The reliability of the screening process was high with an average percentage of agreement of 92.3 %. Of the located articles, 123 were considered relevant. Within this literature, there were 43 CDS tools located. These were classified into 3 main areas: computer-based tools/questionnaires (n = 8, 19 %), treatment algorithms/models (n = 14, 33 %), and clinical prediction rules/classification systems (n = 21, 49 %). Each of these areas and the associated evidence are described. The state of evidentiary support for CDS tools is still preliminary and lacks external validation, head-to-head comparisons, or evidence of generalizability across different populations and settings. Conclusions CDS tools, especially those employing rapidly advancing computer technologies, are under development and of potential interest to health care providers, case management organizations and funders of care. Based on the results of this scoping review, we conclude that these tools, models and systems should be subjected to further validation before they can be recommended for large-scale implementation for managing patients with MSK disorders.
Keywords: Decision-making, Decision support techniques, Musculoskeletal, Back pain, Return to work, Sick leave
Introduction
Regional musculoskeletal (MSK) disorders, such as back, neck and shoulder pain, are some of the most common and disabling health conditions internationally, leading to substantial personal, social and economic burden [1, 2]. The high costs of disability and lost productive work time associated with these conditions demand significant improvements in health care strategies, especially in those aimed at helping patients return to work. Systematic reviews of health care interventions, such as physical conditioning or pain management programs, targeted to regional MSK disorders have indicated modest effectiveness [3–6]. Furthermore, the response of individual patients to these interventions is highly variable. Some patients benefit greatly, while others do not improve, or even experience a worsening of problems [7]. Improved methods for selecting the optimal interventions for individual patients (i.e. personalized rehabilitation) would be invaluable.
Clinical decision support (CDS) is a term that has been used to define the myriad of ways in which knowledge is represented in health information and/or management systems to assist health care providers and other stakeholders in patient management decisions [8]. CDS tools are devices, instruments, questionnaires or other diverse resources (including algorithms, continuums of care, and treatment models) that present knowledge to health care decision-makers, and are often designed as point-of-care resources that support decisions regarding optimal treatment choices. Research and development of CDS tools is a rapidly growing field. These tools are attractive options, given the widespread adoption of computer tablets and smart phones. Also, CDS tools can be an efficient and time-saving strategy for busy clinicians if treatment algorithms are evidence-based and present minimal risks. This technology has the potential to augment complex decisions such as those performed for regional MSK disorders. Computerized CDS has the potential to significantly improve human decisions by expediting information retrieval, identifying unique patient needs, triaging care, and matching patients to the most appropriate resources and treatments.
Some promising CDS tools have been developed specifically for use with patients that have regional pain disorders [9–11]. However, the effectiveness, utility and feasibility of CDS resources in the treatment of regional MSK disorders has been under investigated [12]. Previous systematic reviews of CDS tools have focused on the evaluation of medical management and included only randomized controlled trials from the health care literature [12–17]. However, CDS for the treatment of patients with regional MSK disorders is an emerging area that covers multiple disciplines (including health care, computing science, occupational health services and human resource management). The current literature is therefore diverse and fragmented [11, 18, 19] using inconsistent terminologies and methods. However, to date, no thorough synthesis and summary of these methods is available. In addition, the state of the science in terms of effectiveness, utility, and feasibility of CDS resources in the treatment of MSK disorders has not been summarized as a whole. Given the diversity of the literature and emerging nature of the field, a comprehensive scoping review is needed to map the scientific and grey literature on this topic [20].
The purpose of this project was therefore to conduct a scoping review of CDS tools designed to help decision-makers select interventions that are specifically intended to improve function and return to work in patients with pain-related MSK disorders. This review was also open to other patient related outcomes such as pain, and disability. Our study aims were to identify and inventory CDS tools for helping front-line staff select interventions. We considered both computer-based CDS and other available tools such as treatment algorithms, care pathways, prediction rules, and models. In addition, we aimed to summarize key concepts and terminology to provide criteria for future reporting, evaluate and synthesize evidence of the effectiveness and utility of the available tools, and recommend directions for future research and development in this area.
Methods
Design
This study was a scoping review, which is a methodology for rigorously collecting, synthesizing, appraising and presenting findings from existing research on a topic [20–22]. This approach is especially relevant when an area is emerging or diverse because it examines the extent, range and nature of the research activity [23]. Generally scoping reviews are referred to as ‘a mapping process’ since they summarize a range of evidence in order to convey the breadth and depth of a field [24]. Unlike systematic reviews, scoping reviews do not require appraisal of the quality of the included studies. However, the scoping process requires an analytical interpretation and inventory of the available literature. A scoping review is also useful for determining whether enough literature is available on a topic to conduct a formal systematic review or a meta-analysis or to identify gaps in the literature. In addition, scoping reviews can include a range of study designs and address complex and diverse questions that cannot typically be addressed with a systematic review. Our research area is both emerging and diverse. For these reasons, we chose to conduct a scoping review.
We adopted the scoping review framework proposed by Arksey and O’Malley [23]. This framework progresses through five stages: (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies for analysis; (4) charting the data; and (5) collating, summarizing and reporting results. Each stage will be discussed in detail below.
Identifying the Research Question
An iterative process was used in which we reflexively adapted our question, search terms, and strategy to ensure comprehensive coverage of the literature [23]. An initial question provided the scope for the review and contained several key concepts that guided the search terms used. However, the question was refined based on the broad spectrum of articles we obtained in the initial search. Initially we had included CDS tools for selecting interventions as well as making diagnoses and prognoses. However, due to the extensive breadth of the literature obtained and impracticality of reviewing all 3 research domains, we decided to focus on intervention tools only. This decision was made after consultation with all the researchers and knowledge users involved.
Our final research question was the following: “Do validated decision support tools (especially computer-based tools) exist for selecting appropriate interventions for improving function and return to work in patients with pain-related MSK disorders?”
Identifying Relevant Studies
Relevant studies were identified through online searches of health care, computing science and management databases. These searches were performed with the assistance of two experienced research librarians at the University of Alberta who had access to, and a thorough knowledge of all the necessary databases and search engines. Databases searched included Ovid MEDLINE, Ovid EMBASE, Scopus, CINAHL, Business Source Complete, ABI/INFORM Global, Social Science Research Network (SSRN), Web of Science, ACM Digital Library, IEEE Xplore, ACM Computing Reviews, Computing Research Repository (CoRR), NECI ResearchIndex (formerly CiteSeer) and Google Scholar. Our search strategies were adapted to the various databases as required with the assistance of the librarians. The search included all articles in all languages since the inception of the databases.
Keywords included musculoskeletal diseases; musculoskeletal disorders; back pain; neck pain; shoulder pain; disability evaluation; vocational rehabilitation; return to work; decision support techniques; decision support tools; decision making; clinical protocols; computer-assisted. An example of a search strategy performed in Medline is presented in “Appendix 1”.
Grey literature (unpublished documents from outside the peer-reviewed scientific literature) were also searched. We applied the Canadian Agency for Drugs and Technologies in Health’s Grey Matters search tool to search for relevant information and websites [25]. In addition, Google was searched to identify possible unpublished studies. Relevant articles from the study teams’ own research or libraries were also included.
Each CDS tool located was tracked in the Scopus database and Google Scholar to determine whether additional studies investigating the tool had been published.
Selecting Studies for Analysis
The following were the final set of inclusion/exclusion criteria for the review:
Topic of the article A CDS tool for selecting interventions.
Population Patients with any painful MSK disorder (e.g., regional pain disorders of the back, neck, knee, shoulder, etc.). Our review included all MSK conditions available in the literature and all terms referring to MSK conditions were included in the searches. We excluded articles on non-MSK disorders including metabolic/endocrine disorders (i.e. osteoporosis, diabetic ulcers), rheumatic disorders (i.e. ankylosing spondylitis, rheumatoid arthritis, fibromyalgia) and other general medical conditions.
Outcome Functional and work-related outcomes, including return to work, disability, performance, and absenteeism. Functional recovery is a crucial outcome in regional pain disorders. From the perspective of the various stakeholders involved (i.e. workers, insurers, employers and health care providers), recovery from pain is important; however, functional recovery—such that the patient can return to work and participate in normal daily living—is equally important and has important career and quality-of-life implications [26, 27]. Functional recovery is also often easier to measure. For these reasons, we focused primarily on interventions aimed at improving function or facilitating return to work and other activities of daily living.
Study type Any design describing or evaluating a CDS tool. Systematic reviews were excluded but references within those located were searched for further articles.
The titles and abstracts of articles obtained from the online databases were reviewed and appraised for relevance. Two independent researchers from the team read each title/abstract and judged whether they were relevant to the research question. When there were disagreements between reviewers, the principal researcher (DPG) offered additional consultation until a decision could be reached. If the relevance of a study was still unclear, then the full article was obtained. After selecting the relevant abstracts and titles, two independent researchers assessed the corresponding full versions of the studies to determine which articles should be included in the full review. If discipline-specific questions arose, the reviewers consulted with the team member with relevant expertise (i.e. computers, health care, human resource management, etc.) who could answer the question. We used a Microsoft Access (Redmond, Washington) database stored on an internal server at the University of Alberta that was securely accessible by team members for all stages of the review.
Consultation with Knowledge Users
The consultation process for this study incorporated the development of an advisory committee that included knowledge users who were representatives of local rehabilitation clinics in the Edmonton area, national networks of health care clinics that provide rehabilitation to injured workers, and experienced compensation case managers. We held meetings with knowledge users at two key stages of the review: selecting studies for analysis, and summarizing and reporting results. Knowledge users were asked whether they knew of any CDS tools currently in use or relevant articles. Feedback from knowledge users during these consultative meetings highlighted the importance of: (1) including functional and return-to-work outcomes as search terms; (2) considering not only papers describing specific CDS tools, but also theoretical or conceptual papers dealing with models or algorithms describing treatment selection approaches for patients with MSK disorders; (3) having reviewers consider workplace-based interventions (i.e. accommodations, modifications, etc.) and work-related outcomes (i.e. productivity, absenteeism, etc.) during abstract and title screening; and lastly, (4) considering the importance of feasibility, time of tool administration, cost, and ease of interpretation in addition to scientific validation when considering the utility of any CDS tools located. Before charting the data, the knowledge users were consulted to determine whether the number of articles selected was appropriate and whether the search terms should be altered.
Data Analysis
Charting the Data
Reviewers extracted relevant information from the articles and entered it into an electronic data chart created with the Microsoft Access program. This form included data for authors, year of publication, article title, discipline of the lead authors, geographic location of the study, type and brief description of the CDS tool (including a list of factors included in the tool’s algorithm such as age, sex, pain level, etc.), cost of the tool, study population, study design and goals, methods used, outcome measures used, important results and any economic data recorded. For computer-based tools, we extracted additional information using categories taken from a previously published CDS taxonomy [28]. These charting methods provided a standard and systematic approach to summarize the papers and extract all relevant information.
Collating, Summarizing and Reporting Results
During this stage, we created an overview of all research located. Initially, we presented a basic numerical summary of the studies, including the extent, nature and distribution of the articles. Then, we summarized articles according to the types of tools described or evaluated, research methods used, populations studied, and study results/outcomes.
As mentioned earlier, the scoping review methodology was intended to summarize both the breadth and depth of the literature. We reported the number of articles for each CDS tool as well as some descriptive information about the articles. Since this was a scoping review, we did not undertake a critical appraisal of quality. However, we attempted to map the diversity observed and inventory the various study designs and methods used. This procedure allowed us to draw conclusions about the nature of research in this area and provide recommendations for future studies.
Several clinical prediction rules were designed to identify those individuals likely to respond positively to a particular treatment or intervention. These types of tools have been summarized in other reviews [29, 30], but we created an updated table to establish the range of tools in this category and to examine the strengths and limitations of these rules.
The various CDS tools identified in the articles were also categorized, and key concepts and terminology used in the articles were summarized in tables.
Guidelines developed by Terwee et al. [31] were used to define quality of measurement properties of the CDS tools. Briefly, quality of measurement included internal (internal consistency, relevance of items and representativeness of items of the scale-content validity) as well as external components of validity (the relationship with other tests in a manner that is consistent with theoretically derived hypotheses-construct validity). Intra and inter-rater reliability (i.e. repeatability of measurements taken by the same tester at different times and repeatability of measurements taken by different testers, respectively) were also considered. Definitions of psychometric properties for this review are provided in “Appendix 2”.
Results
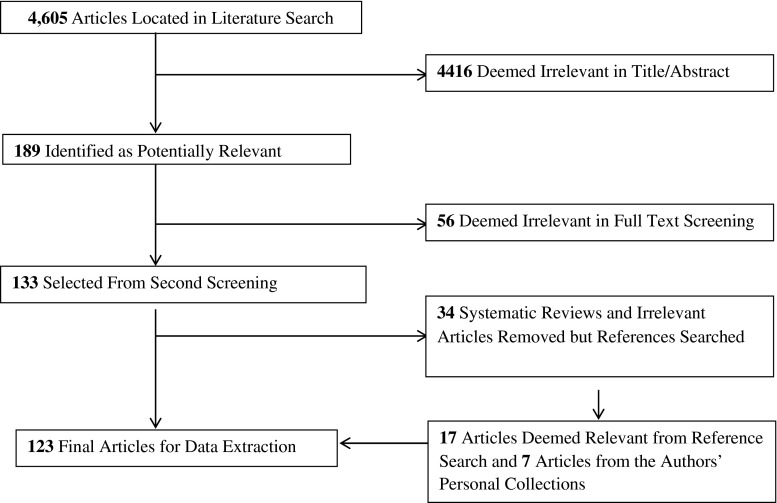
The initial search considering all online databases identified 4605 potentially relevant articles. From these, 189 unique studies were included for the second stage; screening full texts. After screening full texts, 133 articles were selected. From these, 34 articles were removed since they were systematic reviews or considered irrelevant for the purposes of the study. However, their references were searched. From the reference search of these studies and stakeholder meetings, we obtained 24 additional articles. Thus, 123 studies were included for data extraction. The reliability of the screening process of titles and abstracts was high with an average agreement percentage of 92.3 % between reviewers. Figure 1 shows the flow chart of our article search and relevance selection process. A search of the grey literature obtained no new documents or websites specific to MSK disorders.
Fig. 1.
Flow chart of article search and relevance selection process
General Description of Articles
Of the 123 relevant articles located, most originated in North America (n = 70, 57 %), were published between 2006 and 2014 (n = 101, 82 %), and discussed a clinical prediction rule or a classification system (n = 79, 64 %). Twenty-one articles (17 %) discussed treatment algorithms or models, 15 (12 %) discussed questionnaires, while only 8 (7 %) discussed computer-based tools. Most of the articles pertained to low back pain (n = 69, 56 %), followed by neck, shoulder or arm pain (n = 21, 17 %), and general MSK disorders (n = 17, 14 %). When the article described an original study (n = 75), designs of these studies varied greatly from randomized controlled trials (RCTs) to case series and reports. The majority of the original studies were observational in nature, most commonly cohort studies (n = 31, 41 %). Table 1 displays more details about the characteristics of located studies.
Table 1.
Descriptive characteristics of included articles (n = 123)
| Number (%) | |
|---|---|
| Source of evidence | |
| Peer-review journal article | 75 (61) |
| Commentary/editorial/article summary | 19 (15) |
| Conference proceeding | 9 (7) |
| Review | 9 (7) |
| Study protocol | 6 (5) |
| Thesis | 5 (4) |
| Discipline of lead authors | |
| Health care | 121 (98) |
| Computing science | 2 (2) |
| Geographic location of lead authors | |
| North America | 70 (57) |
| Europe | 21 (17) |
| Australasia | 9 (7) |
| Asia | 4 (3) |
| Multiple locations | 19 (15) |
| Year of publication | |
| 2006–2014 | 101 (82) |
| 2000–2005 | 18 (15) |
| Before 2000 | 4 (3) |
| Type of tool discussed in the article | |
| Clinical prediction rule/classification system | 79 (64) |
| Questionnaire | 15 (12) |
| Treatment algorithm | 15 (12) |
| Theoretical/empirical model | 6 (5) |
| Computer-based tool | 8 (7) |
| Condition aimed at by tool | |
| Low back pain | 69 (56) |
| Neck/shoulder/arm pain | 21 (17) |
| General MSK disorders | 17 (14) |
| Knee/ankle pain | 6 (5) |
| Upper extremity pain | 3 (2) |
| Serious pathology (fractures, etc.) | 5 (4) |
| Thoracolumbar injury | 2 (2) |
| Reasoning method | |
| Rule-based | 109 (89) |
| Other (e.g., neural network, decision tree) | 8 (7) |
| Unclear | 6 (5) |
| Study design of peer-review studies located (n = 75) | |
| Experimental | |
| Randomized controlled trial | 12 (16) |
| Quasi-experimental | 4 (5) |
| Observational | |
| Cohort study | 31 (41) |
| Case control/case report/case series | 15 (20) |
| Cross-sectional study | 6 (8) |
| Secondary analysis | 5 (7) |
| Methodological study | 2 (3) |
Overall, there were 43 CDS tools located. After reviewing the tools and identified articles, these were classified into three main areas: (1) specific computer-based tools or questionnaires (n = 8, 19 %); (2) clinical prediction rules/classification systems aimed at categorizing patients into various treatment groups (n = 21, 49 %); and (3) theoretical or algorithmic approaches to selecting treatments (treatment algorithms/models) (n = 14, 33 %). Each of these areas and the tools located will be described.
Computer-Based Tools/Questionnaires
Table 2 provides an inventory of the 8 computer-based devices or questionnaires located for selecting interventions for patients with pain-related MSK disorders. Table 3 provides a summary of the original studies evaluating these tools. Twenty-two manuscripts including three theses [32–53] looked at these 8 tools. Three questionnaire-based tools were included: Keele STarT Back Screening Tool (SBST), the Pain Recovery Inventory of Concerns and Expectations (PRICE) questionnaire, and the Orebro Musculoskeletal Pain Questionnaire (OMPQ). We also located 5 tools incorporating computer technology: Repetitive Strain Injury (RSI) QuickScan intervention program, the Pain Management Advisor (PMA), the Decision Support System (DSS) for helping ergonomists better match workers with the work environment, the Soft Tissue Injury Continuum of Care Model with computerized prompts for case managers, and the Work Assessment Triage Tool (WATT). Three of these tools were aimed at workers with low back pain (SBST, PRICE and OMPQ), 2 were aimed at work-related upper extremity disorders (RSI QuickScan and DSS), 2 were aimed at general work-related MSK injuries (WATT and Soft Tissue Continuum of Care), and 1 aimed at assisting physicians in managing patients with chronic pain (PMA).
Table 2.
Inventory of computer-based tools and questionnaires located
| Name of CDSS | Purpose | Description | Stage of Development | Hardware and Software | Data Input Requirements | Output(s) | TargetRecipient of Output | Limitations |
|---|---|---|---|---|---|---|---|---|
| Keele STarT Back Screening Tool (SBST) [34] | The SBST allocates low back pain patients into three risk groups and is intended to assist clinicians in their decisions about choice of treatment in primary care settings | Questionnaire consisting of nine items covering aspects of fear avoidance beliefs, depression, disability and presence of leg pain and neck/shoulder pain. Patients are allocated into one of three subgroups (low, medium or high risk of chronicity) based on the obtained score. Treatments are targeted based on score | The developers have conducted one RCT to compare treatment informed by the SBST to usual care. Patients managed using the SBST had better functional outcomes at 1-year, but this effect was mainly seen in the medium and high risk groups. Acceptable concurrent validity has been demonstrated with the OMPQ [162–164] The presence of high depression, fear avoidance beliefs, or catastrophizing scores increase significantly from the SBST low risk group, over the medium group to the high-risk group [165] Fair agreement between SBST tool (K = 0.22) and clinicians classification of patients into risk groups [33] StarT Back Tool has been translated and cross culturally validated into Danish [166], Spanish [167],French [168], German [155], Swedish [163], Chinese [156], and Finnish [169] The test–retest reliability of the SBST total score was excellent (intraclass correlation coefficient = 0.78; [169] 0.93 [156]; and 0.90 [164]) and good for the psychosocial subscale (0.68) [169] The StarT Back Tool demonstrated acceptable to outstanding discrimination to determine individuals with different levels of disability as indicated by widely accepted questionnaires such as the Roland Morris Disability Questionnaire, Tampa Scale of Kinesiophobia among others (AUC ranged from 0.79 to 0.91 [155], and 0.75–0.89 [156] |
Not needed | 9 questions are answered with a Likert-scale regarding pain and activities of daily living. The tool has been translated into several languages | Treatments recommendations based on risk categories: low, medium or high risk. The authors suggest that the low risk group only needs a ‘light’ intervention with e.g., analgesics and advice, the medium group requires treatments involving elements such as exercises or manual therapy, and that a combination of physical and cognitive-behavioral approaches should be considered for the high risk groups | Primary care providers | The tool has not been validated via clinical trial outside the United Kingdom There is also a need for a large RCT designed to test whether treatment effects differ across the SBST subgroups |
| Repetitive Strain Injury (RSI) Quick Scan, Now named ‘Compufit Quick Scan’ [40, 52] | To assess the presence or absence of potential risk factors for the establishment of risk profiles related to neck, shoulder and arm symptoms in computer workers and potentially determine targeted treatment | Computer-based survey aimed at identifying workers’ at risk of arm, shoulder and neck symptoms. Based on score results, recommendations are made to the worker to reduce risk of symptoms. In total, the questionnaire consists of 81 items, divided over two categories and 11 subcategories. A description of the actual questions can be found at: www.compufitquickscan.com/ne/quickscan/ | The tool has been tested in a cluster randomized control trial and associated cost-effectiveness evaluation. Use of the tool did not reduce work disability and the tool was not found to be cost-effective The tool does have acceptable internal consistency, reliability and concurrent validity. Cronbach’s alpha was mostly between 0.40 and 0.85. Six scales scored 0.70 or higher. Concurrent validity of the RSI with original questionnaires was acceptable [170] The concurrent validity of the questionnaire symptom items with the observations of 2 physicians was defined as poor to moderate with kappa values between 0.16 and 0.53 [171] Predictive Validity of the RSI QuickScan questionnaire was tested. High scores of the RSI QuickScan on 9 out of 13 scales, including previous symptoms, were significantly related to arm, shoulder and neck symptoms at follow-up [172] |
Internet-based RSI QuickScan survey/questionnaire (https://www.compufitquickscan.com/ne/quickscan) | Items are answered following a web platform | Interventions can be targeted at each of the factors in the RSI QuickScan, with a total of 16 interventions aimed at reducing the associated risk [36, 52]. A score of 30 % or less of the maximum on a scale was classified as a low risk, colour-coded “green”. A score of 31 % to 60 % of the maximum on a scale was classified as a medium risk, colour-coded “amber”. A score of 61 % or more of the maximum on a scale was classified as a high risk, colour-coded “red”. | Primary care providers and ergonomists | The RSI QuickScan appears to have a modest effect and was not cost-effective. However, this might have been due to problems with implementation of expensive ergonomic interventions, which were sold at regular commercial prices during the trial. This was despite commitment from all participating organizations prior to starting the study that they were prepared to invest in the necessary preventive measures |
| Pain Recovery Inventory of Concerns and Expectations (PRICE) [36] | Brief screening questionnaire to triage return-to-work strategies among patients with low back pain | Questionnaire consisting of 46 items measuring, depressive symptoms (12 items), pain catastrophizing (2 items), lack of organizational support (7 items), activity limitation (15 items), fear of movement (4 items), perceiving grave life impacts (3 items) poor expectations for recovery (2 items), and pain intensity (1 item) [36] | A confirmatory cluster analysis replicated previous findings of three risk subgroups: distressed, avoidant, and lacking employer support Validity of the PRICE screening was supported by its prospective association with the 3-month disability outcome measures (return to work, functional limitation, and clinical case rating) [36] |
Not needed | Subjects are asked to respond to each of the 46 items on different Likert-type scales scale (i.e. “strongly disagree” to “strongly agree.”; “not at all” to “all the time”) | PRICE can be used to identify early intervention needs among working adults with low back pain based on the group classifications It provides an indication of whether attention should be focused on workplace coordination, physical activation, or psychological coping, and this may improve the ability to provide more patient-centered strategies for early disability prevention |
Primary care providers | This questionnaire is at an early stage of development. Future trials should be conducted to validate the classification and targeted management approach |
| Orebro Musculoskeletal Pain Questionnaire (OMPQ) [39] | Screening tool aimed at identifying high-risk patients with MSK pain in need of early intervention | Questionnaire consisting of 24-items that allocates patients into three different risk categories related to work absenteeism and guides potential interventions for those with low (reassurance and advice), moderate (physical therapy) or high risk (psychologically-informed care) | The OMPQ was initially developed as a screening tool and has been evaluated in several settings and translated into several languages for this purpose. However, it has recently been evaluated as a potential CDS tool for selecting interventions for patients with MSK pain. One study is underway in Germany that evaluates the OMPQ as a CDS tool [44] | Not needed | 24 items with various response options for different sections of the tool | After OMPQ administration and scoring, the questionnaire categorized patients into one of three risk level categories: low, medium and high risk. Various cut-points have been recommended for the categorization, with the developers stating the cut-off scores are related to the population studied | Primary care providers | Has only been evaluated as a CDS tool in one student thesis, with negative results. The OMPQ was not explicitly developed as a CDS tool, although early risk stratification implies different approaches for different categories |
| Pain Management Advisor (PMA) [35] |
To enhance primary care providers’ management of chronic pain | Computer-based tool that relies on rule-based algorithms derived from expert knowledge of pain specialists User asked a series of questions to refine the diagnosis and determine appropriate therapy Interactive capability (e.g., for explanations, therapeutic rationales, therapy guidelines) |
Working version developed: some field testing conducted | Computer program PMA written in MicroSoft Visual Basic, v. 5.0, run as an expert application in XpertRule Algorithms stored in MicroSoft Access database MicroSoft Help Utility used for explanations and queries |
Patient demographics Diagnosis Pain characteristics Laboratory tests and imaging studies Current medications Prior therapies Concurrent disease conditions Allergies Psychological status |
A prioritized list of recommendations: (1) medical management (pharmacologic and nonpharmacological management, physical, psychosocial modalities); (2) invasive procedures; (3) referrals | Primary care providers. | This software was only tested qualitatively in one study. No further testing has been published |
| Decision Support Software (DSS) [38] | To determine whether the use of software as a decision support system can help with evaluation and control of physical job stresses and prevent re-injury of workers who have experienced or are concerned about work-related musculoskeletal disorders The ergonomists used the database as a decision support tool in the control of work-related MSK disorders (WMSDs) |
Computer-based tool consisting of decision support software is a spreadsheet-based database program written in Microsoft Excel. It has a graphical user interface (GUI) in the WindowsTM environment, and contains video clips of representative cycles of the selected job and in some cases, multiple videos showing multiple views It was designed specifically for the site, but is adaptable to other manufacturing plants with relatively stable work patterns. The software program is a database that stores detailed job information such as standardized work data, videos, and upper-extremity physical stress ratings for over 400 jobs in the plant. Additionally, the database users were able to record comments about the jobs and related control issues |
Testing usability and effectiveness to prevent worker injuries No further testing The database seems to be useful to facilitate the quality of job evaluation. This improvement in quality can lead to better intervention and control of MSK problems [38] |
Pentium-based PCs Ideally a portable computer Windows 95 Excel Program Visual interface For video import, mpg images are needed |
Upper extremity exposure ratings (evaluated by the research team) for repetition, posture, contact stress, and force Standard data: work elements and times for selected job, obtained from the company standard data system -Text box that allows users to store and retrieve comments about selected job -Menu to search for a job by department, section, line position, and by date Videos of the work environment |
Information from database was used to make recommendations for injury prevention and management strategies by the ergonomists | Ergonomists | This software was only tested qualitatively in one study. No further testing has been published [38] |
| Soft Tissue Continuum of Care Model [37] | The model was designed as a high-level, decision-making tool or “roadmap” to promote a consistent, evidence-based approach to manage soft tissue injuries | The model with computer-based tool that involves 3 main components: (1) Staged application of rehabilitation services; (2) Case management protocols and case planning checkpoints; and (3) Contracted services with providers | A population-based, quasi-experimental, before-and-after design with concurrent control groups was used to evaluate the model’s impact and effectiveness | Computer-based prompts were given to workers’ compensation case managers via a custom-built program | Data on type of injury and time since injury is used from within the workers’ compensation administrative database to generate prompts for case managers | Based on type of injury and time of recovery, claimants are referred to different assessment and treatment programs | Workers’ compensation case managers | Further validation of this model is recommended through the implementation of experimental design such as RCT |
| Work Assessment Triage Tool (WATT) [32] | The classification algorithm and accompanying computer-based CDS tool help categorize injured workers toward optimal rehabilitation interventions based on unique worker characteristics | Computer-based tool comprised of 18 variables related to: injury duration, occupation, job attachment and working status at time of RTW assessment, availability of modified work, National Occupational Classification Code, ICD9 diagnostic group, calendar days injury to assessment, the ‘Occupation’ item from the PDI Pain VAS out of 10, and 9 items from the SF36 (items 2, 4, 5, 7, 12, 14, 18, 21, 25) |
The algorithm used by the WATT was developed using machine learning techniques and demonstrated high accuracy for correct classifications during internal validation [32, 41] Concurrent validity of WATT with clinician’s recommendations was tested. Percent agreement between clinician and WATT recommendations was low to moderate. The WATT did not improve upon clinician recommendations, but was more likely to recommend evidence-based interventions [42] | HTML-based computer program that can run on any computer system with access to the Internet | Data entered into WATT involves 18 items related to injury duration, occupation, job attachment and working status at time of RTW assessment, availability of modified work, National Occupational Classification Code, ICD9 diagnostic group, calendar days injury to assessment, the ‘Occupation’ item from the PDI, Pain VAS out of 10, and9 items from the SF36 (items 2, 4, 5, 7, 12, 14, 18, 21, 25) |
The rehabilitation options available to clinicians were: physical therapy, interdisciplinary functional restoration, workplace-based rehabilitation, ‘hybrid’ functional restoration/workplace-based rehabilitation; complex interdisciplinary bio-psychosocial rehabilitation and no further rehabilitation | Primary care providers and case managers | This tool is at the early stages of validation. Findings do not provide evidence of concurrent validity of the WATT against clinician recommendations. WATT appeared more likely than clinicians to recommend treatments supported by current evidence such as workplace-based interventions. Further validation is needed |
Table 3.
Summary table of original studies evaluating computer-based tools or questionnaires for selecting interventions for patients with musculoskeletal disorders
| Authors (ID) | Year | Study design | Population | Body part | Context | Tool mentioned | Properties tested | Methods | Outcome | Results |
|---|---|---|---|---|---|---|---|---|---|---|
| Hill et al. [34] | 2011 | RCT | 851 adults aged ≥18 years with low back pain with or without radiculopathy | Low Back | Ten general practice clinics in England | Questionnaire: Keele STarT Back Screening Tool that stratifies patients into low, medium or high risk, requiring different interventions | Validity of a stratified/classification approach to primary care Sensitivity/specificity for identifying treatments |
Eligible patients were randomly assigned to intervention (use of SBST to inform management) or control group (usual care). Disability, cost and quality of life were evaluated | Results indicate a classification approach using the tool significantly improves patient outcomes and is associated with substantial economic benefits | Positive |
| Hill et al. [33] | 2010 | Methodological study | 12 consecutively consulting patients with primary care back pain | Low Back | 8 General Practices in the United Kingdom | Questionnaire: Keele STarT Back Screening Tool that stratifies patients into low, medium or high risk, requiring different interventions | Agreement between clinicians and STarT Back tool | 12 patients underwent a video-recorded clinical assessment. The SBST was completed on the same day. Clinical experts reviewed the videos and categorized subjects to low, medium or high-risk | Clinicians make inconsistent risk estimations for primary care patients with back pain when using intuition alone, with little agreement with the STarT Back tool | Unclear |
| Spekle et al. [40] | 2010 | Cluster RCT | 741 computer workers from 7 Dutch organisations in various work branches (e.g., health care, local government, nature conservation, engineering, education and regulatory affairs), located throughout the Netherlands The population consisted of office staff, local government officials, engineers, consultants, teachers, health care personnel, nature conservation professionals, researchers and managers |
Arm, shoulder and neck pain | Employees of a large occupational health service in the Netherlands | Questionnaire: RSI QuickScan intervention program | Effectiveness of the intervention program for reducing symptoms and sick leave | The participants were assigned to either an intervention or usual care group by means of cluster randomization. At baseline and after 12 months of follow-up, participants completed the RSI QuickScan questionnaire to determine exposure to the risk factors and prevalence of arm, shoulder and neck symptoms. A tailor-made intervention program was proposed to participants with high-risk profiles at baseline. Examples of implemented interventions are an individual workstation check, a visit to the occupational health physician and an education program on the prevention of arm, shoulder and neck symptoms | There were no significant differences in changes in the prevalence of arm, shoulder and neck symptoms or sick leave between the intervention and usual care group | Negative |
| Spekle et al. [52] | 2010 | Economic evaluation alongside a cluster RCT | 638 computer users with and without shoulder, arm and neck symptoms | Arm, shoulder and neck | Workers from seven Dutch companies | Questionnaire: RSI QuickScan intervention program | Cost–benefit of the RSI QuickScan program | Workers were randomized to either the intervention or usual care group. The intervention consisted of a tailor-made program based on the RSI-QuickScan program. Usual care group did not receive elaborate advice. The participants completed the questionnaire at baseline and 12-month follow-up. Effectiveness and cost were compared | The RSI QuickScan intervention program did not prove to be cost-effective. However, with a relatively small investment, the program increased the number of workers who received information on healthy computer use and improved their work posture and movement | Negative |
| Shaw et al. [36] | 2013 | Cohort study | 496 workers with acute (fewer than 14 days) work-related low back pain | Low Back | A private network of occupational health clinics in the USA with eight participating clinics located in various states | Questionnaire: The Pain Recovery Inventory of Concerns and Expectations (PRICE) measure. Designed to subgroup patients within the first 2 weeks of an episode of back pain to determine needed treatment depending on whether disability is related to pain beliefs, emotional distress, or workplace concerns | Sensitivity analysis conducted to reduce the number of items while maintaining scale reliability, then classification accuracy was tested using a confirmatory cluster analysis | Patients were recruited from the consecutive caseload of patients reporting low back pain, and volunteer patients completed a brief demographic questionnaire and a 10-page psychosocial test battery. Participants were then followed-up at 3-months to determine pain, function, and work status | The reduced PRICE measure is a 46-item screening measure that can be used to identify early intervention needs of working adults with low back pain | Unclear Not testing effectiveness, only development |
| Aravena-Paez [39] | 2014 | Retrospective cohort study | 2046 workers compensation claimants with back disorders | Low Back | Rehabilitation facilities in Alberta, Canada with contracts to treat workers’ compensation claimants | Questionnaire: OMPQ. Screening tool aimed at identifying high-risk patients with MSK pain in need of early intervention | Tested level of agreement between clinician recommendations and OMPQ categories. Also examined whether a match between OMPQ categories and actual programs were associated with better RTW outcomes | Secondary analysis of a dataset used for developing a CDS tool. Examined whether a match between OMPQ categories, clinician recommendations and actual rehab program undertaken was related to a better return to work outcome | The OMPQ had limited agreement with clinician recommendations suggesting other measures or factors are considered when making treatment recommendations. Finally, concordance of OMPQ categorization and actual rehabilitation undertaken did not appear to favorably impact outcomes | Negative |
| Knab et al. [35] | 2001 | Quasi-experimental study | 100 patients with chronic pain referred for treatment at a chronic pain clinic | All | VA San Diego Healthcare System Pain Clinic in the United States |
Computerized: Pain management advisor (PMA) | Validity and acceptability of recommendations made based on a computerized tool | A pain specialist used a decision support system to determine appropriate pain therapy and sent letters to the referring physicians outlining these recommendations. Separately, five board-certified PCPs used a CBDS system to “treat” the 50 cases. Patients were followed up 1-year later | The use of a Computer-Based Decision-Support system may improve the ability of primary care physicians to manage chronic pain and may facilitate screening of consults to optimize specialist utilization | Positive |
| Womack and Armstrong [38] | 2005 | Quasi-experimental study | Workers in an automobile assembly plant conducting over 400 jobs in the plant | Upper extremity | Worksite-based study. The plant built small trucks in a 2.1 million square foot facility. There were over 500 on- and offline assembly jobs and a workforce of ~2580 union employees | Computerized: Decision support system (DSS) for helping ergonomists better match workers with the work environment | Utility of the tool over a 20-month period | Evaluation of qualitative comments regarding utility of the tool as well as 1-on-1 semi-structured interviews with users | Of 197 comments entered by users, 25 % pertained to primary prevention, 75 % pertained to secondary prevention, and 94 comments (47.7 %) described ergonomic interventions. Use of the software tool improved the quality and efficiency of the ergonomic job analysis process | Positive |
| Stephens and Gross [37] | 2007 | Quasi-experimental study | 171,736 workers’ compensation claimants with any type of MSK injury aged 18–65 years | All | Rehabilitation facilities in Alberta, Canada with contracts to treat workers’ compensation claimants | Soft Tissue Injury Continuum of Care Model with computerized prompts for case managers | Effectiveness of the tool compared to usual care | A population-based, quasi-experimental, before-and-after design with concurrent control groups was used to evaluate the model’s impact. Data were extracted from the main WCB-Alberta administrative database from 2 years before model implementation to 5 years after | Implementation of a soft tissue injury continuum of care involving staged application of various types of rehabilitation services appears to have resulted in more rapid and sustained recovery | Positive |
| Gross et al. [32] | 2013 | Cohort study | 8611 injured Canadian workers’ compensation claimants with any type of MSK injury between 18 and 65 years old | All | Rehabilitation facilities in Alberta, Canada with contracts to treat workers’ compensation claimants | Computerized: Work Assessment Triage Tool | Classification accuracy of the tool | Data were extracted from a workers’ compensation database and machine-learning techniques were used to generate and test a tool | A CDS tool was developed for selecting rehabilitation interventions for injured workers. Preliminary validation was also conducted | Not testing effectiveness, only tool development |
| Zhang et al. [41] | 2013 | Methodological study (rule-based classifiers) | 8611 injured Canadian workers’ compensation claimants with any type of MSK injury between 18 and 65 years old | All | Rehabilitation facilities in Alberta, Canada with contracts to treat workers’ compensation claimants | Computerized: Work Assessment Triage Tool | Accuracy of various rule-based classifiers | Data were extracted from a workers’ compensation database and various machine-learning techniques and rule-based classifiers were tested | This paper presents a description of the algorithm development from a computer science/machine learning perspective | Not testing effectiveness, only tool development |
| Qin et al. [42] | 2015 | Cross sectional | 434 injured Canadian workers’ compensation claimants with any type of MSK injury between 18 and 65 years old | All | Workers’ compensation rehabilitation facility in Alberta, Canada | Computerized: Work Assessment Triage Tool (WATT). Designed to categorize injured workers to various programs including functional restoration, workplace-based intervention, or chronic pain programs | Concurrent validity of the tool’s recommendations | Level of agreement was examined between the WATT and clinical recommendations by therapists participating in a clinical trial | Percent agreement between clinician and WATT recommendations was low to moderate. The WATT did not improve upon clinician recommendations | Unclear |
Most of these tools had some psychometric testing in the way of validation of items, concurrent validity, acceptability of the tool, accuracy of the classification as well as testing the effectiveness of the tool compared to standard treatment. Nevertheless, this testing has been preliminary, and a more exhaustive validation process involving randomized controlled trials at multiple sites and settings is needed for all of the tools. Four of the tools [34, 35, 37, 38] showed positive preliminary results regarding the use of the tool to determine appropriate treatments for managing some MSK conditions. However, one tool (RSI QuickScan) did not prove to be effective for reducing work disability or cost-effective [40, 52], and two studies did not have clear positive or negative results regarding the tools evaluated (SBST and WATT) [33, 42]. One student thesis evaluated the utility of the OMPQ as a clinical decision support tool for workers’ compensation claimants, with negative results [39]. However, the OMPQ was initially developed as a screening or prognostic tool, not explicitly as a CDS tool. In addition, one protocol of a cluster RCT that attempts to use the OMPQ as a CDS tool for selecting interventions for patients with LBP was found [44]. The results of this RCT are still unpublished, so it is unknown how well the OMPQ functions as a CDS tool. Three other studies [32, 36, 41] only looked at the development phase of the tools (WATT and PRICE). Thus, evidence is limited regarding validity evidence of these CDS tools. For details of the measurement properties of the CDS tools found, see Table 4.
Table 4.
Summary of the quality of measurement properties of the computer-based tools or questionnaires located
| Tool | Internal consistency | Face validity | Content validity | Criterion validity* | Construct validity | Reproducibility (agreement/reliability) |
|---|---|---|---|---|---|---|
| StarT Back | + | + | + | +* | + | + |
| RSI Quick Scan | + | + | + | – | + | + |
| PRICE | + | + | + | – | + | – |
| PMA | – | + | + | + | + | – |
| DSS | – | + | + | – | – | – |
| Soft Tissue Model | – | + | + | – | + | – |
| WATT | – | + | + | + | + | – |
+Quality of measurements properties were based on guidelines established by Terwee et al. [31]
(+) Criterion accomplished
(−) Criterion not accomplished
* Comparison was performed with reference standards
Treatment Algorithms/Decision-Models
Of the 22 articles [54–75] discussing treatment algorithms/models, there were 15 original studies evaluating 14 different algorithms or decision-models (theoretical or empirical) for selecting interventions for patients with MSK disorders. Details of these algorithms/models and the studies can be found in Table 5. Nine of the studies [54–61, 76] looked at low back pain, 2 discussed knee disorders [62, 63], 2 discussed shoulder disorders [64, 65] and 2 examined other body regions (wrist and neck) [66, 67]. Research designs used in these studies varied greatly, with the observational cohort study being the most common among them. Methodologies and types of algorithms were also wide-ranging, making the analysis of these studies challenging. Most of the algorithms or decision models were developed to determine possible treatment paths. Nevertheless, most testing of these algorithms/decision models was preliminary or exploratory (e.g., small sample size, secondary analyses of previous collected data, lack of replication or validation samples, use of research designs that are prone to bias including case series, cross sectional or cohort studies rather than randomized controlled trials). Nine of these algorithms [54, 58, 62–67, 76] seemed to lead to positive results when deciding on intervention strategies. Nevertheless, one study [56] found that the use of the algorithm would not result in better outcomes for patients with low back pain. Four studies [55, 57, 59, 61] only looked at the development of an algorithm/model without associated testing of it.
Table 5.
Summary table of original studies describing or evaluating algorithms or decision-models (theoretical or empirical) for selecting interventions for patients with musculoskeletal disorders
| Authors (ID) | Year | Study design | Body part | Algorithm/model mentioned | Population | Methods | Outcome/conclusion | Results |
|---|---|---|---|---|---|---|---|---|
| Hurd et al. [63] | 2008 | Cohort study | Knee | Algorithm for managing subacute anterior ligament (ACL) injuries was created using clinical information on: concomitant injury, unresolved impairments, and results of a screening examination | 345 highly active adults (216 men, 129 women) with subacute anterior cruciate ligament injury aged 18–65 years presenting to an orthopedic surgeon | Prospective follow-up study. Patients presenting within 7 months of their injury were treated using a decision-making algorithm. Algorithm was used as criteria to guide management and classify individuals as ‘noncopers’ (poor potential) or potential ‘copers’ (good potential) for non-operative care. Patients were followed up for the duration of care (up to 10 PT sessions over 5 weeks) | 199 subjects classified as ‘noncopers’ and 146 as potential ‘copers’. 63 of 88 potential ‘copers’ successfully returned to pre-injury activities without surgery, with 25 of these not undergoing ACL reconstruction at follow-up. The algorithm should be considered as an alternative to management based on anterior knee laxity, age, and preinjury activity levels | Positive |
| Kodama et al. [66] | 2013 | Review and retrospective study | Wrist | Scoring system for selecting treatment for distal radius fractures. Includes a variety of clinical factors related to the fracture, as well as dominant hand, high occupational or recreational activity, age, and supplemental factors (Table 2 in paper) | 164 patients with distal radius fracture who were 50 years or older presenting to a surgeon. | Development of the decision-making guide was described, and then a retrospective study was used to evaluate the guide in patients. Comparison was made on clinical outcomes (DASH questionnaire scores) between patients where recommendations of the guide were followed and not followed | 164 patients were divided into 4 groups using the tool: conservative care, relative conservative care, relative surgical care, and surgical care. Clinical outcomes of those that followed the recommendation were better than those not following the recommendation. The present scoring system is an easy-to-use decision-making tool for choosing conservative or surgical treatment for distal radius fractures | Positive |
| Murphy et al. [76] | 2007 | Cohort study | Low back | The approach is based on 3 questions: (1) Are the symptoms reflective of a visceral disorder or a serious/potentially life-threatening disease? (2) From where is the patient’s pain arising? (3) What has gone wrong with this person as a whole that would cause the pain experience to develop and persist? | 264 patients with moderate to severe low back pain over 18 years old presenting to a private practice physical therapy clinic | Cross-sectional feasibility study. Demographic, diagnostic and baseline outcome measure data were gathered on a cohort of low back pain patients examined by one of three examiners trained in the application of a diagnosis-based clinical decision rule that guided subsequent treatment | The guide can be applied in a private practice setting It appears that patients with low back pain can be distinguished on the basis of this approach, and treatment plans can be formulated utilizing this strategy |
Development article |
| Sonnabend [64] | 1994 | Case Series | Shoulder | Treatment algorithm was based on presence of fracture location, weeks in a sling, presence of pain and weakness, and arthrogram or ultrasound results | 53 patients with primary traumatic anterior shoulder dislocation older than 40 years of age presenting to an orthopedic surgeon | Patients were classified into 3 groups according to an algorithm based on signs and symptoms. This algorithm was used to determine treatment. Clinical outcomes in the different groups were described after the treatment | The algorithm is suggested as an approach to treatment of primary traumatic dislocation | Development article |
| Spiegl et al. [65] | 2013 | Retrospective case series | Shoulder | Treatment algorithm for acute osseous Bankart lesions consisting of a conservative strategy for small defect sizes and a surgical approach for medium-sized and large defects | 25 patients who sustained acute traumatic osseous Bankart lesions after a first time shoulder dislocation from a ski or snowboard accident without rotator cuff tears | Retrospective case series to describe outcomes. Operative therapy was performed in patients with osseous defects of 5 % or more, otherwise conservative therapy was initiated | Applying the treatment algorithm appears to lead to encouraging mid-term results and a low rate of recurrent instability in active patients | Positive |
| Stanton et al. [55] | 2011 | Cross sectional study and test–retest reliability for a subset | Low back | Treatment-Based Classification Algorithm based on clinical examination findings for selecting treatments for patients with low back pain. This algorithm was summarized into a decision-making flowchart | 250 patients with acute or sub-acute low back pain recruited from teaching hospitals (Sydney, Australia) and private physical therapy clinics (Australia and United States) | Observational study to determine the prevalence of patients meeting the criteria for each subgroup (i.e. responders to the various treatments in the system). Trained physical therapists performed standardized assessments on all participants. These findings were used to classify participants into subgroups. 31 participants were reassessed to determine inter-rater reliability of the algorithm decision | Reliability of the algorithm is sufficient for clinical use. But 25 % of participants met the criteria for more than 1 subgroup and 25 % did not meet the criteria for any subgroup. This has important implications for validity and potential revisions to the algorithm’s section that guides unclear classification | Development article |
| Stanton et al. [56] | 2013 | Cross-sectional secondary analysis from 3 previous studies | Low back | Treatment-Based Classification Algorithm (see above) | 529 patients with low back pain treated at private physical therapy clinics in USA, Australia and the Netherlands, and public hospital physical therapy outpatient departments in Australia | To guide improvements in the algorithm, this study aimed to determine whether people with unclear classifications are different from those with clear classifications. Univariate logistic regression was used to determine which participant variables were related to having an unclear classification | People with unclear classifications appeared to be less affected by low back pain (less disability and fewer fear avoidance beliefs), despite typically having a longer duration of low back pain. Recommendations to the algorithm are suggested, this study provides no evidence that any changes will result in better outcomes | Unclear |
| Strong et al. [57] | 1995 | Cohort study | Low back | The Integrated Psychosocial Assessment Model (IPAM), a multidimensional assessment for use with patients with chronic low back pain | 70 consecutive patients with chronic low back pain presenting at the Auckland Regional Pain Service or private practice pain facility in Auckland, New Zealand | Subjects were assessed on pain intensity, disability, coping strategies, depression and illness behavior. Cluster analysis was used to identify homogenous groups of patients. Clusters were named “In Control”, “Depressed and Disabled”, and “High Denial”. The clustered obtained by this study were used to propose management | The IPAM model may be valuable for identifying low back pain subgroups. Treatments corresponding to each subgroup were proposed | Development article |
| Wang et al. [67] | 2003 | Cohort study | Neck | Clinical reasoning algorithm for treating patients with neck pain. This algorithm was developed before the study by one of the authors. The algorithm consists of 4 categories: (1) radicular arm pain or neck pain; (2) referred arm pain or neck pain; (3) cervicogenic headaches; and (4) neck pain only. There are subcategories formed by different clinical patterns that are used to guide treatment | 57 adults referred from general practitioners for physical therapy treatment of neck pain. All patients had current neck pain with or without radiating pain and no other serious pathology | A quasi-experimental, nonequivalent, pretest-post-test control group design was used to investigate the effects of algorithm-based clinical decision making. Outcomes in a treatment group of 30 patients with neck pain treated based on the algorithm were compared to a control group of convenience formed of 27 subjects who also had neck pain but did not receive treatment for various reasons | After ~4 weeks of physical therapy intervention, patients in the treatment group demonstrated statistically significant increases of cervical range of motion, decreased pain, increases of physical performance measures, and decreases in level of disability. The control group showed no differences in all five outcome variables. Authors conclude that organized and specific physical therapy program was effective in improving the status of patients with neck pain, and the algorithm can help clinicians classify patients with cervical pain into clinical patterns | Positive |
| Widerstrom et al. [58] | 2007 | Multiple case pretest–posttest study | Back | Clinical ‘pain modulating’ treatment classification for patients with low back pain that was formed empirically. It is considered for patients with moderate to high irritability and high pain and/or disability scores, and where judgments on spinal mobility were inconclusive and no segmental level could be determined | 16 consecutive adults patients with low back pain, regardless of duration, with or without radiating pain to the lower extremities. Patients were from the waiting list of a primary care physiotherapy clinic in Sweden. All patients but one had chronic low back pain (>3 months) | The first part of the paper was descriptive, resulting in an individualized clinical decision-making algorithm As an illustration of the utility of the presented algorithm, a multiple subject case study was then conducted, using a pretest–posttest design. The 16 patients were classified based on the algorithm, and treated based on the algorithm, then evaluated at discharge from physiotherapy |
Two patients were excluded from the study (1 pregnancy and 1 with progressive symptoms). All but 1 of the remaining 14 patients showed improvements in pain intensity scores. The authors interpret study findings to suggest that the presented model may be used when clinical decisions on selecting interventions for patients with chronic low back pain are made | Positive |
| Fitzgerald et al. [62] | 2000 | Cohort Study | Knee | Decision-making scheme for returning patients to high-level activity with non-operative treatment after anterior cruciate ligament rupture. The screening exam consists of four 1- legged hop tests, the incidence of knee giving-way, a self-report functional survey, and a self-report global knee function rating | 93 consecutive patients with acute unilateral anterior cruciate ligament rupture | Patients were classified as either candidates (n = 39, 42 %) or non-candidates (n = 54, 58 %) for non-operative management based on the decision-making scheme. Patients were returned to full activity an average of 4 weeks after the screening examination. Successful treatment was defined as the ability to return to preinjury levels of activity without experiencing an episode of giving-way at the knee. Failure was defined as either having at least one episode of givingway at the knee or a reduction in functional status | Of the 39 rehabilitation candidates, 28 chose non-operative management and returned to preinjury activity levels, 22 of whom (79 %) returned to preinjury activity levels without further episodes of instability or a reduction in functional status. The decision-making scheme described in this study shows promise in identifying patients who can safely postpone surgical reconstruction and temporarily return to physically demanding activities | Positive |
| Rundell et al. [54] | 2009 | Case series | Back pain | Management of acute and chronic low back pain using the World Health Organization’s International Classification of Functioning. This model provides a method that considers biological, individual, and social contributions that can be used to classify patients | Two patients, 1 with acute and 1 with chronic pain were treated pragmatically using models of clinical reasoning | Manual therapy, exercise, and education interventions were directed toward relevant body structure and function impairments, activity limitations, and contextual factors based on their hypothesized contribution to functioning and disability. Patients were evaluated after a period of 3 and 10 weeks of intervention, respectively | Both patients demonstrated clinically important improvements in pain, disability, and psychosocial factors after intervention. The WHO-ICF model appears to provide an effective framework for physical therapists to better identify each person’s experience with his or her disablements and assists in prioritizing treatment selection | Positive |
| Shaw et al. [60] | 2007 | Cohort study | Back pain | A model is developed for discriminating patients with acute back pain into subgroups depending on whether disability is related to pain beliefs, emotional distress, or workplace concerns | 528 patients with work-related back pain seeking treatment for acute back pain at one of 8 community-based occupational health clinics in the New England region of the USA | Patients with back pain completed a 16-item questionnaire of potential disability risk factors before their initial medical evaluation. Outcomes of pain, functional limitation, and work disability were assessed 1 and 3 months later | A K-Means cluster analysis of 5 disability risk factors (pain, depressed mood, fear avoidant beliefs, work inflexibility, and poor expectations for recovery) resulted in 4 sub-groups: low risk (n = 182); emotional distress (n = 103); severe pain/fear avoidant (n = 102); and concerns about job accommodation (n = 141). Pain and disability outcomes at follow-up were superior in the low-risk group and poorest in the severe pain/fear avoidant group | Development article |
| Steenstra et al. [61] | 2010 | Secondary analysis of previous cohort study data | Back pain | Evaluation of the Risk Factor-Based Intervention Strategy Model proposed previously by Shaw et al. The model was developed based on a literature review and classifies patients into 1 of 4 groups that require different forms of intervention | 442 workers with a new, accepted or pending, work related injury lost-time claim for low back pain who were absent from work for at least 5 days within the first 14 calendar days post-injury, and were at least 15 years of age | Claimants (n = 259) who had already returned to work, were categorized as low risk. A latent class analysis was performed on 183 workers absent from work. Groups were classified based on: pain, disability, fear avoidance beliefs, physical demands, people-oriented culture and disability management practice at the workplace, and depressive symptoms | Three classes were identified; (1) workers with ‘workplace issues’, (2) workers with a ‘no workplace issues, but back pain’, and (3) workers having ‘multiple issues’ (the most negative values on every scale, notably depressive symptoms). This study confirms an earlier model theorizing that subgroups of patients can be identified who might benefit from different interventions | Positive but exploratory |
| Reme et al. [59] | 2012 | Cohort study | Back pain | Development of a sub-classification of workers with acute back pain. Patterns of early disability risk factors from this study suggest patients have differential needs with respect to overcoming emotional distress, resuming normal activity, and obtaining workplace support | 496 workers seeking treatment for work-related, acute back pain at private occupational medicine clinics in the states of Massachusetts, Rhode Island, or Texas, USA | Workers completed self-report measures comprising 11 possible risk factors for chronicity of pain and disability. Outcomes of pain, function, and return-to-work were assessed at 3-month follow-up. A K-means cluster analysis was used to derive patient subgroups based on risk factor patterns, and then these subgroups were compared with respect to 3-month outcomes | A 4-cluster solution met criteria for cluster separation and interpretability, and the four clusters were labeled: minimal risk (29 %), workplace concerns (26 %); activity limitations (27 %); and emotional distress (19 %). Classifying patients in this manner may improve the cost–benefit of early intervention strategies to prevent long-term sickness absence and disability due to back pain | Development article |
Clinical Prediction Rules/Classification Systems
The remaining 79 articles [76–154] looked at 21 unique clinical prediction rules or classification systems. Four articles described the clinical prediction rules in general. Most of these studies targeted rules for identifying responders to interventions for low back pain (8 rules) followed by neck pain (6 rules), patellofemoral pain (3 rules), lateral epicondylagia (2 rules), ankle sprain (1 rule) and thoracolumbar injury (1 rule). For details on the clinical prediction rules and classification systems found in this scoping review, see Table 6. The rules were developed to determine response to specific treatments that included spinal manipulation, stabilization exercises, McKenzie approach, mechanical traction, Pilates-based exercise, foot orthoses, patellar taping, or general classification models.
Table 6.
Summary of clinical prediction rules and classification systems for painful musculoskeletal conditions
| Condition | Purpose of rule/system | Evaluation status of the rule/system |
|---|---|---|
| Low back pain | Identifying responders to spinal manipulation [77–97, 119, 120] | Rule developed empirically Confirmatory testing in additional samples, including workers, has shown mixed results Unsuccessful evaluation via clinical trial Patients positive for the main factors in the rule (symptom duration <16 days and no symptoms distal to the knee) respond to other interventions such as McKenzie therapy |
| Low back pain | Treatment-based classification system [55, 56, 97–111] | Rule developed theoretically Empirical testing has had mixed results Mixed evaluations via clinical trial Reliability of mobilization and stabilization subgroups has been unacceptable in some studies Questionable utility of the system as 25 % of patients fall into multiple subgroups and 25 % remain unclassified |
| Low back pain | Identifying responders to stabilization exercise [92, 97, 110, 112] | Rule developed empirically Confirmatory testing in additional samples has had mixed results Stabilization and manipulation rules do not represent mutually exclusive subgroups |
| Low back pain | Identifying responders to McKenzie approach [95, 97, 113] | Rule developed empirically No confirmatory testing Prevalence testing of McKenzie classifications shows overlap with other prediction rules |
| Low back pain | Identifying non-responders to spinal manipulation [114] | Rule developed empirically No confirmatory testing |
| Low back pain | Identifying responders to mechanical traction [115, 116] | Two separate rules developed empirically Factors in the rules are not consistent No confirmatory testing |
| Low back pain | CBI health classification system [117] | System developed theoretically Empirically tested by the developers No confirmatory testing |
| Low back pain | Identifying responders to pilates based exercises [118] | Rule developed empirically No confirmatory testing |
| Neck pain | Treatment-based classification system for neck pain [123, 124, 128–131, 135, 137] | System developed theoretically Empirical testing has been promising (case series, pilot and cohort studies) No evaluation via clinical trial |
| Neck pain | Identifying responders to Thoracic manipulation [102, 125–127] | Rule developed empirically Unsuccessful evaluation via clinical trial |
| Neck pain | Identifying responders to cervical traction and exercise [133, 134] | Rule developed empirically No confirmatory testing |
| Neck pain | Identifying responders to home-based cervical traction [122] | Rule developed empirically No confirmatory testing |
| Neck pain | Identifying responders to cervical manipulation [132, 136] | Two separate rules developed empirically Factors in the rules are not consistent No confirmatory testing |
| Neck pain | Identifying responders to cervical manipulation physiotherapy or usual care [138] | Rule developed empirically No confirmatory testing |
| Patellofemoral knee pain | Identifying responders to lumbopelvic manipulation [141, 142] | Rule developed empirically Confirmatory testing in a separate sample was unsuccessful |
| Patellofemoral knee pain | Identifying responders to foot orthosis [140, 146] | Two separate rules developed empirically Factors in the rules are not consistent No confirmatory testing |
| Patellofemoral knee pain | Identifying responders to patellar taping [143] | Rule developed empirically No confirmatory testing |
| Ankle sprain | Identifying responders to manipulation and exercises [148] | Rule developed empirically No confirmatory testing |
| Lateral epicondylalgia | Classification model for tennis elbow [149] | Theoretical model description No empirical testing |
| Lateral epicondylalgia | Identifying responders to manual therapy and exercise [147] | Rule developed empirically No confirmatory testing |
| Thoracolumbar injury | Classification system for Thoracolumbar spine injury [144, 145] | System developed theoretically Successful reliability testing No confirmatory testing |
From the rules looking at back pain (8 rules in total involving 47 articles [77–121, 150, 152]), three rules (rules for manipulation and stabilization exercise, and the treatment-based classification system) have been the most commonly studied. Confirmatory evaluation of these rules has shown mixed or unsuccessful results. The remaining 5 rules (rules for the McKenzie approach, mechanical traction, Pilates, and the CBI Health classification system) have been developed empirically or theoretically but no confirmatory testing has been conducted. Thus, it is unknown if the results from these studies would provide clarification regarding management of patients with back pain.
Six rules discussed in 18 articles targeted neck pain [122–139]. From these rules, only one (treatment-based classification system) showed positive results when tested in case series, pilot and cohort studies. However, this rule has not been tested in a randomized controlled trial. The remaining 5 rules for neck pain were either unsuccessful (rule for thoracic manipulation) or had no confirmatory testing evidence. From the rules developed for patellofemoral pain, 2 rules discussed in 5 articles [140–143, 146] (1 rule for patellar taping and 1 for foot orthoses) were not tested further and 1 rule for lumbopelvic manipulation obtained unsuccessful results when tested in a separate sample. The remaining rules developed for lateral epicondylalgia (2 rules in 2 articles [147, 149]), ankle sprain (1 rule in 1 article [148]) and thoracolumbar injury (1 rule in 2 articles [144, 145]) did not have additional testing. Of note, there were 3 interventions where two separate rules were generated for the same condition (traction for low back pain, manipulation for neck pain, and foot orthoses for patellofemoral pain), but results indicated the rules were not consistent and the rules were formed of different variables.
Discussion
The number of CDS tools relevant to MSK disorders is small but it appears that this field is rapidly expanding. Results of this scoping review identify that although there are several publications around CDS tools, with the majority (82 %) published since 2006, few correspond to formal and validated tools to help with the management of MSK conditions. Furthermore, the tools, models and classification systems we identified are intended for use by health care providers. One tool, the RSI Quickscan, is intended for use by ergonomists for identifying appropriate management strategies for workers with upper extremity disorders, including job or equipment modifications where appropriate. However, we were unable to locate any decision support systems for human resource managers or other employer agents who develop return-to-work processes and identify appropriate job modifications.
There was a wide range of literature including treatment algorithms/decision-models and several publications related to clinical prediction rules applied in the context of MSK disorders, most commonly low back pain. The included articles were rather diverse and most of this information was exploratory or developmental in nature, particularly with regard to use of research designs that are prone to bias including case series, cross sectional or cohort studies rather than randomized controlled trials, secondary analyses of previous collected data, and lack of replication or testing in validation samples. It appears that research in this area is starting to develop and would benefit from an internationally coordinated effort. Consequently, more studies regarding feasibility, usability, and effectiveness of these tools as well as psychometric testing would benefit the area of CDS tools applied to health care specifically to the area of MSK disorders.
Computer-Based Tools or Questionnaires
Our review located 3 questionnaires and 5 computer-based tools that were used to select interventions for patients with MSK disorders. Most of these tools were at initial stages of development or validation. However, we were not able to locate or get further information from the authors of 2 tools (DSS and PMA) indicating the developers likely did not pursue further development. The majority of the studies we reviewed were non-experimental in design, focusing on early stages of questionnaire development and testing or focused mainly on process measures, such as clinician ratings of system acceptability and usability. Of the located tools, six had some validity evidence (WATT, SBST, OMPQ, RSI QuickScan, PMA). The tool that appears to have been most evaluated has been the SBST. This tool has been translated into several languages and has demonstrated good discriminative validity when compared with widely accepted questionnaires such as the Roland Morris Disability Questionnaire and Tampa Scale of Kinesiophobia, among others (AUC ranged from 0.79 to 0.91 [155], and 0.75–0.89 [156]). Although this information is promising, this tool has not been examined through a clinical trial outside the United Kingdom. Thus, the validation studies for these tools overall have not provided strong evidence for use of these tools in clinical or workplace settings. Of note, the OMPQ was not explicitly developed as a CDS tool but as a screening/prognostic tool, which may explain the negative results in a validation study [39]. Thus, none of them are ready for widespread implementation in clinical practice since more testing is necessary.
Since the research obtained regarding CDS tools in MSK disorders is at the early stages, information about user preferences regarding the presentation of computer output, including content, formatting (e.g., color, graphics), and length, have not been conducted to date. Similarly, there are no published data concerning technical difficulties (e.g., type and number of system crashes or touch-screen calibration problems) encountered by computer-based CDS tool users. Both issues have important implications for future system refinements and implementation strategies. In addition, there is a lack of information regarding contextual circumstances or the processes used to integrate the CDS into the existing clinical workflow, as well as testing in different populations and settings. Most of the studies found have tested the CDS tools in one single group of patients. In addition, some limitations of the existing CDS tools for treating MSK conditions were lack of integration with computer and/or mobile devices, the reduced use of web-based interfaces, and infrequent use of data directly entered by patients. Some of the tools were even questionnaires administered by paper and pencil, which was also highlighted by the recent review performed by Pombo et al. [157].
Research of the effectiveness of CDS tools to improve patient outcomes is still fairly sparse. Only 3 of these tools (SBST, RSI QuickScan, Continuum of Care) have tested patient outcomes such as patients’ recovery, disability, cost, and quality of life. Results from these studies are inconsistent, and more replication with variable settings and population sampling strategies is needed. Other major patient outcomes of interest for policy makers have not been examined, such as health care utilization, health care costs, and communication with health care providers. Similar results have been obtained in early systematic reviews of computerized decision-support systems for chronic pain management in primary care and CDS tools targeted to healthcare professionals, especially for medical conditions [158, 159].
Further validation of these tools with larger samples and with stronger designs are needed. It is necessary that larger randomized controlled trials testing the effectiveness of CDS tools against standard care be performed to determine clearly if these systems are worth being implemented in clinical practice.
Clinical Prediction Rules/Classification Systems
Clinical Prediction Rules and classification systems that aim to identify which patients would benefit from a specific treatment have attracted the attention of many researchers regarding their effectiveness and validity. Several narrative and two systematic reviews have been conducted [29, 30]. Our scoping review adds to this literature by attempting to inventory all clinical prediction rules developed for a wide variety of MSK conditions and comment on the status of the research in this area. We located 21 clinical prediction rules that have been developed for MSK disorders, however studies evaluating effectiveness of these rules have been inconsistent. Most of the rules lack external validation in different samples using strong methods such as RCTs, but validation studies that have been conducted by separate research groups have largely been unsuccessful. We also found that rules developed for the same treatment for the same condition by different research groups were inconsistent in terms of the clinical variables in the final rules. These results are not surprising based on the results obtained from different systematic reviews focusing on rules in low back pain and the physical therapy area [29, 30, 160]. According to Beneciuk et al. [29] there are several clinical prediction rules in physical therapy that have not been validated in external samples. In addition, recently Patel et al. [161] examined the quality of the validation studies for clinical prediction rules in subjects with back pain. They found that the evidence from randomized trials validating rules for non-specific back pain is weak. These results were also in agreement with those of May et al. [30] Haskin et al. [160] and Patel et al. [161] Thus, based on the current evidence, more widespread use of clinical prediction rules for identifying responders to various interventions in clinical practice is not recommended at this point.
If clinical prediction rules are well designed and validated in appropriate populations, they could have the potential to identify patients most likely to benefit from a particular treatment. This in turn would help improve clinical decision-making and practice. However, the current evidence, especially the lack of cross-validation and replication, does not support large-scale implementation of clinical prediction rules to improve disability outcomes [160]. At present, it is unknown if the unsatisfactory performance of rules in clinical trials is because inappropriate rules have been tested, the trials have been poorly designed, underpowered, or simply that it is impossible to develop rules that are fit for all conditions, subjects and settings [29]. Thus more research is needed to elucidate all of these questions.
Treatment Algorithms/Decision-Models
The literature around treatment algorithms and models was diverse, which made the analysis of these studies challenging. Most of these algorithms or decision models have been developed for determining an appropriate treatment path without formal and rigorous testing. Sample sizes have been relatively small in most cases. The results from these studies also are inconsistent. Thus, no clear conclusions extracted from these algorithms or models can be made at this point.
Strengths and Limitations
This study represents the first attempt to inventory available CDS tools for MSK disorders, and comment on the status of the research literature. Strengths of our project include the involvement of a large international group or researchers and stakeholders with diverse backgrounds who provided input on the project. Additionally, we conducted a very comprehensive literature search (all languages and years since inception of databases) across health, computer science, and management databases with the assistance of research librarians as well as a search of grey literature using validated methods. The methodology used in this project was that of a scoping review, which summarizes the state of the science in a given area, but does not synthesize evidence on specific outcomes (e.g., patient outcomes, cost-effectiveness) across studies. This represents a limitation of the scoping review methodology, but it was appropriate in this case due to the diversity of methods and literature encompassed by the review. Also, scoping review methods do not require detailed critical appraisal and, therefore, study quality likely varied in the articles we identified. Additionally, while we sought to be as comprehensive as possible in our literature search, it is possible that there are other CDS tools under development that we failed to identify. As the various CDS tools are tested in different settings and using consistent methodology, more definitive conclusions about the impact of these tools on clinicians’ performance or patients outcomes may be drawn.
Conclusions
The potential for CDS tools, especially those employing rapidly advancing computer technologies, has sparked great interest among health care providers, case management organizations and funders of care. Our literature review identified 5 computer-based tools, 3 questionnaires, 14 algorithms or decision-models, as well as 21 clinical prediction rules or classification systems. However, currently none of these tools, models or systems appears ready for widespread use in clinical practice to select interventions for patients with MSK disorders. More research is needed examining more advanced levels of validity of existing tools, including impact on patient outcome, or developing new evidence-based CDS tools to help guide clinical and workplace practice for managing patients with MSK disorders.
Acknowledgments
The Workers’ Compensation Board of Manitoba provided funding for this research.
Appendix 1
See Table 7.
Table 7.
Example search strategy
| Searches | Results |
|---|---|
| Musculoskeletal diseases/or musculoskeletal diseases/or fasciitis, plantar/or foot deformities, acquired/or heel spur/or posterior tibial tendon dysfunction/or hand deformities, acquired/or exp temporomandibular joint disorders/or bursitis/or joint deformities, acquired/or joint instability/or joint loose bodies/or patellofemoral pain syndrome/or shoulder impingement syndrome/or synovitis/or compartment syndromes/or anterior compartment syndrome/or ischemic contracture/or contracture/or dupuytren contracture/or muscle cramp/or myofascial pain syndromes/or exp tendinopathy/or tennis elbow/ | 75,820 |
| musculoskeletal pain/or exp back pain/or chronic pain/or neck pain/or pain, intractable/ | 41,304 |
| exp arm injuries/or exp back injuries/or contusions/or exp dislocations/or exp fractures, bone/or fractures, cartilage/or exp hand injuries/or exp hip injuries/or exp leg injuries/or exp neck injuries/or occupational injuries/or soft tissue injuries/or exp spinal injuries/or exp “sprains and strains”/or exp tendon injuries/ | 237,957 |
| ((Pain* or tear or tears or injur* or sprain* or strain* or dislocation*) adj (musc* or joint or back or spine or spinal or neck or cervical or pelvic or hip or rotator cuff or knee or ankle or elbow or shoulder)).mp. | 8305 |
| (carpal tunnel or frozen shoulder or shoulder impingement or chronic pain or myofascial pain or patellofemoral pain or regional pain disorder* or whiplash).mp. | 39,549 |
| 1 or 2 or 3 or 4 or 5 | 356,444 |
| (osteoporosis or (diabet* and ulcer*) or fibromyalgia or ankylosing spondilytis or RA or arthritis or osteomyelitis).ti. | 113,335 |
| exp *Osteoporosis/ | 32,044 |
| exp *Diabetic Foot/ | 4942 |
| exp *Fibromyalgia/ | 5462 |
| exp *Arthritis/ | 165,770 |
| exp *Osteomyelitis/ | 13,996 |
| or/7–12 | 230,601 |
| 6 not 13 | 330,638 |
| Decision Support Systems, Clinical/ | 5200 |
| decision making, computer-assisted/or decision support techniques/ | 14,671 |
| decision making/and (model or models or classification or subgroup* or sub-group* or algorithm*).mp. | 12,813 |
| decision support.mp. | 22,109 |
| clinical prediction rule*.mp. | 710 |
| decision tree*.mp. | 11,491 |
| decision system*.tw. | 157 |
| treatment based classification.tw. | 35 |
| knowledge-base*.tw. | 9101 |
| treatment rule*.tw. | 72 |
| treatment selection.tw. | 1635 |
| targeted treatment*.tw. | 2353 |
| (treatment algorithm* or management algorithm*).tw. | 4400 |
| (orebro adj4 (musculoskeletal or questionnaire* or pain*)).tw. | 35 |
| STarT Back.tw. | 23 |
| Acute Low Back Pain Screening.tw. | 9 |
| ((support* or guide or aid* or rule* or tool*) adj4 decision).tw. | 20,310 |
| active knowledge system*.tw. | 3 |
| inference engine*.tw. | 148 |
| rule based system*.tw. | 244 |
| artificial intelligence/or expert systems/or “neural networks (computer)”/or support vector machines/or knowledge bases/or medical informatics computing/or exp pattern recognition, automated/ | 49,273 |
| (machine learning or artificial intelligence).tw. | 7145 |
| connectionist expert system*.tw. | 7 |
| careflow system*.tw. | 4 |
| or/15–37 | 119,832 |
| 14 and 39 | 1894 |
| limit 40 to animals | 38 |
| 40 not 41 | 1856 |
| limit 42 to “all child (0–18 years)” | 376 |
| limit 43 to “all adult (19 plus years)” | 263 |
| 42 not (43 not 44) | 1743 |
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Dec 10, 2013
Search History (45 searches) (close)
Appendix 2
See Table 8.
Table 8.
Definitions of psychometric properties
| Psychometric property | Definition | Criteria for scoring the psychometric properties as accomplished (adapted from Terwee et al. [31]) |
|---|---|---|
| Internal consistency | The extent to which items in a (sub)scale are intercorrelated, thus measuring the same construct | Factor analyses performed on adequate sample size AND Cronbach’s alpha(s) calculated per dimension AND Cronbach’s alpha(s) between 0.70 and 0.95; |
| Content validity | The extent to which the domain of interest is comprehensively sampled by the items in the questionnaire | A clear description is provided of the measurement aim, the target population, the concepts that are being measured, and the item selection AND target population and (investigators OR experts) were involved in item selection |
| Criterion validity | The extent to which scores on a particular questionnaire relate to a gold standard | Convincing arguments that gold standard is ‘‘gold’’ AND correlation with gold standard >0.70; |
| Construct validity | The extent to which scores on a particular questionnaire relate to other measures in a manner that is consistent with theoretically derived hypotheses concerning the concepts that are being measured | Specific hypotheses were formulated AND at least 75 % of the results are in accordance with these hypotheses |
| Reproducibility | ||
| a. Agreement | The extent to which the scores on repeated measures are close to each other (absolute measurement error) | Convincing arguments that agreement is acceptable; |
| b. Reliability | ||
| Test–retest reliability | The extent of agreement across two administrations of a test, assuming nothing happened between testings (like treatment or other change-producing event) | ICC or Kappa >0.70 |
| Inter-rater reliability | The extent of agreement among two or more raters at a single testing session. Introduces an additional source of unreliability (the rater) to the test unreliability found in other domains | ICC or Kappa >0.70 |
Compliance with Ethical Standards
Conflict of interest
The authors declare no conflict of interest.
Contributor Information
Douglas P. Gross, Email: dgross@ualberta.ca
Ivan A. Steenstra, Email: ivan.steenstra@ryerson.ca
References
- 1.Power JD, Perruccio AV, Desmeules M, Lagacé C, Badley EM. Ambulatory physician care for musculoskeletal disorders in Canada. J Rheumatol. 2006;33(1):133–139. [PubMed] [Google Scholar]
- 2.Coyte PC, Asche CV, Croxford R, Chan B. The economic cost of musculoskeletal disorders in Canada. Arthritis Care Res. 1998;11(5):315–325. doi: 10.1002/art.1790110503. [DOI] [PubMed] [Google Scholar]
- 3.Gagnon CM, Stanos SP, van der Ende G, Rader LR, Norman Harden R. Treatment outcomes for workers compensation patients in a US-Based Interdisciplinary Pain Management Program. Pain Pract. 2013;13(4):282–288. doi: 10.1111/j.1533-2500.2012.00586.x. [DOI] [PubMed] [Google Scholar]
- 4.Schaafsma F, Schonstein E, Whelan KM, Ulvestad E, Kenny DT, Verbeek JH. Physical conditioning programs for improving work outcomes in workers with back pain. Cochrane Database Syst Rev. 2010; (1):CD001822. [DOI] [PubMed]
- 5.Van Oostrom SH, Driessen MT, De Vet HCW, Franche RL, Schonstein E, Loisel P, Van Mechelen W, Anema JR. Workplace interventions for preventing work disability. Cochrane Database Syst Rev. 2009; (2):CD006955. [DOI] [PubMed]
- 6.Karjalainen K, Malmivaara A, van Tulder M, Roine R, Jauhiainen M, Hurri H, Koes B. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain among working age adults. Cochrane Database Syst Rev. (Online : Update Software) 2003; (2):CD002193. [DOI] [PubMed]
- 7.Gross DP, Haws C, Niemelainen R. What is the rate of functional improvement during occupational rehabilitation in workers’ compensation claimants? J Occup Rehabil. 2012;22(3):292–300. doi: 10.1007/s10926-011-9346-9. [DOI] [PubMed] [Google Scholar]
- 8.Hayward RS, El-Hajj M, Voth TK, Deis K. Patterns of use of decision support tools by clinicians. In: AMIA annual symposium proceedings/AMIA symposium, AMIA symposium; 2006, p. 329–33. [PMC free article] [PubMed]
- 9.Haldorsen EMH. The right treatment to the right patient at the right time. Occup Environ Med. 2003;60(4):235–236. doi: 10.1136/oem.60.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hill JC, Fritz JM. Psychosocial influences on low back pain, disability, and response to treatment. Phys Ther. 2011;91(5):712–721. doi: 10.2522/ptj.20100280. [DOI] [PubMed] [Google Scholar]
- 11.Blackmore CC, Mecklenburg RS, Kaplan GS. Effectiveness of clinical decision support in controlling inappropriate imaging. JACR J Am Coll Radiol. 2011;8(1):19–25. doi: 10.1016/j.jacr.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Hemens BJ, Holbrook A, Tonkin M, Mackay JA, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB. Computerized clinical decision support systems for drug prescribing and management: a decision-maker–researcher partnership systematic review. Implement Sci. 2011;6(1):1–17. doi: 10.1186/1748-5908-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sahota N, Lloyd R, Ramakrishna A, Mackay JA, Prorok JC, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB. Computerized clinical decision support systems for acute care management: A decision-maker–researcher partnership systematic review of effects on process of care and patient outcomes. Implement Sci. 2011;6(1):1–14. doi: 10.1186/1748-5908-6-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Souza NM, Sebaldt RJ, Mackay JA, Prorok JC, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB. Computerized clinical decision support systems for primary preventive care: a decision-maker–researcher partnership systematic review of effects on process of care and patient outcomes. Implement Sci. 2011;6(1):1–14. doi: 10.1186/1748-5908-6-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roshanov PS, Misra S, Gerstein HC, Garg AX, Sebaldt RJ, Mackay JA, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB. Computerized clinical decision support systems for chronic disease management: a decision-maker–researcher partnership systematic review. Implement Sci. 2011;6(1):1–16. doi: 10.1186/1748-5908-6-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haynes RB, Wilczynski NL. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: methods of a decision-maker–researcher partnership systematic review. Implement Sci. 2010;5(1):1–8. doi: 10.1186/1748-5908-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nieuwlaat R, Connolly SJ, Mackay JA, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB. Computerized clinical decision support systems for therapeutic drug monitoring and dosing: a decision-maker–researcher partnership systematic review. Implement Sci. 2011;6(1):1–14. doi: 10.1186/1748-5908-6-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel S, Brown S, Friede T, Griffiths F, Lord J, Ngunjiri A, Thistlethwaite J, Tysall C, Woolvine M, Underwood M. Study protocol: improving patient choice in treating low back pain (IMPACT–LBP): a randomised controlled trial of a decision support package for use in physical therapy. BMC Musculoskel Disord. 2011;12:1–7. doi: 10.1186/1471-2474-12-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trafton J, Martins S, Michel M, Lewis E, Wang D, Combs A, Scates N, Tu S, Goldstein MK. Evaluation of the acceptability and usability of a decision support system to encourage safe and effective use of opioid therapy for chronic, noncancer pain by primary care providers. Pain Medicine. 2010;11(4):575–585. doi: 10.1111/j.1526-4637.2010.00818.x. [DOI] [PubMed] [Google Scholar]
- 20.Grimshaw J. A knowledge synthesis chapter. Published Online: Canadian Institute of Health Research (Online). http://www.cih-rirsc.gc.ca/e/documents/knowledge_synthesis_chapter_e.pdf.
- 21.Davis K, Drey N, Gould D. What are scoping studies? A review of the nursing literature. Int J Nurs Stud. 2009;46:1386–1400. doi: 10.1016/j.ijnurstu.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 22.Poth C, Ross S. Meta-analysis, systematic review, or scoping review? Comparing methodologies in educational research. In: The Canadian Society for the Study of Education Annual Congress; 2009.
- 23.Arskey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 24.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):1–9. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grey Matters: a practical search tool for evidence-based medicine. Canadian Agency for Drugs and Technologies in Health. https://www.cadth.ca/resources/finding-evidence/grey-matters-practical-search-tool-evidence-based-medicine.
- 26.Young AE, Roessler RT, Wasiak R, McPherson KM, van Poppel MN, Anema JR. A developmental conceptualization of return to work. J Occup Rehabil. 2005;15(4):557–568. doi: 10.1007/s10926-005-8034-z. [DOI] [PubMed] [Google Scholar]
- 27.International Classification of Function, Disability and Health: ICF. In. Geneva, Switzerland: World Health Organization; 2001.
- 28.Berlin A, Sorani M, Sim I. A taxonomic description of computer-based clinical decision support systems. J Biomed Inform. 2006;39(6):656–667. doi: 10.1016/j.jbi.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 29.Beneciuk JM, Bishop MD, George SZ. Clinical prediction rules for physical therapy interventions: a systematic review. Phys Ther. 2009;89(2):114–124. doi: 10.2522/ptj.20080239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.May S, Rosedale R. Prescriptive clinical prediction rules in back pain research: a systematic review. J Man Manip Ther. 2009;17(1):36–45. doi: 10.1179/106698109790818214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, Bouter LM, de Vet HCW. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 32.Gross DP, Zhang J, Steenstra I, Barnsley S, Haws C, Amell T, McIntosh G, Cooper J, Zaiane O. Development of a computer-based clinical decision support tool for selecting appropriate rehabilitation interventions for injured workers. J Occup Rehabil. 2013;23(4):597–609. doi: 10.1007/s10926-013-9430-4. [DOI] [PubMed] [Google Scholar]
- 33.Hill JC, Vohora K, Dunn KM, Main CJ, Hay EM. Comparing the STarT back screening tool’s subgroup allocation of individual patients with that of independent clinical experts. Clin J Pain. 2010;26(9):783–787. doi: 10.1097/AJP.0b013e3181f18aac. [DOI] [PubMed] [Google Scholar]
- 34.Hill JC, Whitehurst DG, Lewis M, Bryan S, Dunn KM, Foster NE, Konstantinou K, Main CJ, Mason E, Somerville S. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378(9802):1560–1571. doi: 10.1016/S0140-6736(11)60937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knab JH, Wallace MS, Wagner RL, Tsoukatos J, Weinger MB. The use of a computer-based decision support system facilitates primary care physicians’ management of chronic pain. Anesth Analg. 2001;93(3):712–720. doi: 10.1097/00000539-200109000-00035. [DOI] [PubMed] [Google Scholar]
- 36.Shaw WS, Reme SE, Pransky G, Woiszwillo MJ, Steenstra IA, Linton SJ. The pain recovery inventory of concerns and expectations: a psychosocial screening instrument to identify intervention needs among patients at elevated risk of back disability. J Occup Environ Med. 2013;55(8):885–894. doi: 10.1097/JOM.0b013e318289ee6c. [DOI] [PubMed] [Google Scholar]
- 37.Stephens B, Gross DP. The influence of a continuum of care model on the rehabilitation of compensation claimants with soft tissue disorders. Spine. 2007;32(25):2898–2904. doi: 10.1097/BRS.0b013e31815b64b6. [DOI] [PubMed] [Google Scholar]
- 38.Womack SK, Armstrong TJ. Use of a computerized decision support system for primary and secondary prevention of work-related MSD disability. J Occup Rehabil. 2005;15(3):313–328. doi: 10.1007/s10926-005-5939-5. [DOI] [PubMed] [Google Scholar]
- 39.Aravena HI. Utility of the Orebro Musculoskeletal Questionnaire as a Screening and Clinical Decision Support tool in Workers’s Compensation Claims Edmonton. Canada: University of Alberta; 2014. [Google Scholar]
- 40.Speklé EM, Hoozemans MJ, Blatter BM, Heinrich J, van der Beek AJ, Knol DL, Bongers PM, van Dieën JH. Effectiveness of a questionnaire based intervention programme on the prevalence of arm, shoulder and neck symptoms, risk factors and sick leave in computer workers: a cluster randomised controlled trial in an occupational setting. BMC Musculoskel Disord. 2010;11(1):99. doi: 10.1186/1471-2474-11-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang J, Cao P, Gross D, Zaiane OR. On the application of multi-class classification in physical therapy recommendation. Health Inf Sci Syst Health Inf Sci Syst. 2013;1(1):1–15. [Google Scholar]
- 42.Qin Z, Armijo-Olivo S, Woodhouse LJ, Gross DP. An investigation of the validity of the Work Assessment Triage Tool clinical decision support tool for selecting optimal rehabilitation interventions for workers with musculoskeletal injuries. Clin Rehabil. (Epub ahead of print) 2015:0269215515578696. [DOI] [PubMed]
- 43.Qin Z, Armijo-Olivo S, Woodhouse L, Gross D. Evaluation of A Clinical Decision Support Tool for Selecting Optimal Rehabilitation Intervention for Injured Workers. Calgary: Education & Research Archive: University of Alberta; 2014. [Google Scholar]
- 44.Schmidt CO, Pfingsten M, Fahland RA, Lindena G, Marnitz U, Pfeifer K, Kohlmann T, Chenot JF. Assessing a risk tailored intervention to prevent disabling low back pain—protocol of a cluster randomized controlled trial. BMC Musculoskel Disord. 2010;11:1–7. doi: 10.1186/1471-2474-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J, Cao P, Gross D, Zaiane OR. On the application of multi-class classification in physical therapy recommendation. Edmonton: University of Alberta; 2012. [Google Scholar]
- 46.Zhang J, Gross D, Zaïane OR. On the application of multi-class classification in physical therapy recommendation. In: 17th Pacific-Asia conference on knowledge discovery and data mining, PAKDD 2013. vol. 7867 LNAI. Gold Coast, QLD; 2013, p. 143–54.
- 47.Hay EM, Dunn KM, Hill JC, Lewis M, Mason EE, Konstantinou K, Sowden G, Somerville S, Vohora K, Whitehurst D. A randomised clinical trial of subgrouping and targeted treatment for low back pain compared with best current care. The STarT Back Trial Study Protocol. BMC Musculoskel Disord. 2008;9(1):58. doi: 10.1186/1471-2474-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Main C, Sowden G, Hill J, Watson P, Hay E. Integrating physical and psychological approaches to treatment in low back pain: the development and content of the STarT Back trial’s ‘high-risk’intervention (StarT Back; ISRCTN 37113406) Physiotherapy. 2012;98(2):110–116. doi: 10.1016/j.physio.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 49.Robinson ME, George SZ. Screening for problematic low back pain: STarT. Pain. 2012;153(11):2159–2160. doi: 10.1016/j.pain.2012.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Storheim K. Targeted physiotherapy treatment for low back pain based on clinical risk can improve clinical and economic outcomes when compared with current best practice. J Physiother. 2012;58(1):57. doi: 10.1016/S1836-9553(12)70073-5. [DOI] [PubMed] [Google Scholar]
- 51.Traeger A, McAuley JH. STarT Back Screening Tool. J Physiother. 2013;59(2):131. doi: 10.1016/S1836-9553(13)70170-X. [DOI] [PubMed] [Google Scholar]
- 52.Speklé EM, Heinrich J, Hoozemans MJ, Blatter BM, van der Beek AJ, van Dieën JH, van Tulder MW. The cost-effectiveness of the RSI QuickScan intervention programme for computer workers: results of an economic evaluation alongside a randomised controlled trial. BMC Musculoskel Disord. 2010;11(1):259. doi: 10.1186/1471-2474-11-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sowden G, Hill JC, Konstantinou K, Khanna M, Main CJ, Salmon P, Somerville S, Wathall S, Foster NE. Targeted treatment in primary care for low back pain: the treatment system and clinical training programmes used in the IMPaCT Back study (ISRCTN 55174281) Fam Pract. 2012;29:50–62. doi: 10.1093/fampra/cmr037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rundell SD, Davenport TE, Wagner T. Physical therapist management of acute and chronic low back pain using the World Health Organization’s International Classification of Functioning, Disability and Health. Phys Ther. 2009;89(1):82–90. doi: 10.2522/ptj.20080113. [DOI] [PubMed] [Google Scholar]
- 55.Stanton TR, Fritz JM, Hancock MJ, Latimer J, Maher CG, Wand BM, Parent EC. Evaluation of a treatment-based classification algorithm for low back pain: a cross-sectional study. Phys Ther. 2011;91(4):496–509. doi: 10.2522/ptj.20100272. [DOI] [PubMed] [Google Scholar]
- 56.Stanton TR, Hancock MJ, Apeldoorn AT, Wand BM, Fritz JM. What characterizes people who have an unclear classification using a treatment-based classification algorithm for low back pain? A cross-sectional study. Phys Ther. 2013;93(3):345–355. doi: 10.2522/ptj.20120263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Strong J, Large RG, Ashton R, Stewart A. A New Zealand Replication of the IPAM Clustering Model for alow back Patients. Clin J Pain. 1995;11(4):296–306. doi: 10.1097/00002508-199512000-00007. [DOI] [PubMed] [Google Scholar]
- 58.Widerstrom B, Olofson N, Arvidsson I. Manual therapy and a suggested treatment based classification algorithm in patients with low back pain: a pilot study. J Back Musculoskel Rehabil. 2007;20(2):61–70. [Google Scholar]
- 59.Reme SE, Shaw WS, Steenstra IA, Woiszwillo MJ, Pransky G, Linton SJ. Distressed, immobilized, or lacking employer support? A sub-classification of acute work-related low back pain. J Occup Rehabil. 2012;22(4):541–552. doi: 10.1007/s10926-012-9370-4. [DOI] [PubMed] [Google Scholar]
- 60.Shaw WS, Pransky G, Patterson W, Linton SJ, Winters T. Patient clusters in acute, work-related back pain based on patterns of disability risk factors. J Occup Environ Med. 2007;49(2):185–193. doi: 10.1097/01.jom.0000254205.47334.c3. [DOI] [PubMed] [Google Scholar]
- 61.Steenstra IA, Ibrahim SA, Franche R-L, Hogg-Johnson S, Shaw WS, Pransky GS. Validation of a risk factor-based intervention strategy model using data from the readiness for return to work cohort study. J Occup Rehabil. 2010;20(3):394–405. doi: 10.1007/s10926-009-9218-8. [DOI] [PubMed] [Google Scholar]
- 62.Fitzgerald G, Axe M, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 63.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: Part 1, outcomes. Am J Sp Med. 2008;36(1):40–47. doi: 10.1177/0363546507308190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sonnabend DH. Treatment of primary anterior shoulder dislocation in patients older than 40 years of age: conservative versus operative. Clin Orthop Relat Res. 1994;304:74–77. [PubMed] [Google Scholar]
- 65.Spiegl UJ, Ryf C, Hepp P, Rillmann P. Evaluation of a treatment algorithm for acute traumatic osseous Bankart lesions resulting from first time dislocation of the shoulder with a two year follow-up. BMC Musculoskel Disord. 2013;14(1):305. doi: 10.1186/1471-2474-14-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kodama N, Imai S, Matsusue Y. A simple method for choosing treatment of distal radius fractures. J Hand Surg. 2013;38(10):1896–1905. doi: 10.1016/j.jhsa.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 67.Wang WT, Olson SL, Campbell AH, Hanten WP, Gleeson PB. Effectiveness of physical therapy for patients with neck pain: an individualized approach using a clinical decision-making algorithm. Am J Phys Med Rehabil. 2003;82(3):203–218. doi: 10.1097/01.PHM.0000052700.48757.CF. [DOI] [PubMed] [Google Scholar]
- 68.Björklund M, Djupsjöbacka M, Svedmark Å, Häger C. Effects of tailored neck-shoulder pain treatment based on a decision model guided by clinical assessments and standardized functional tests. A study protocol of a randomized controlled trial. BMC Musculoskel Disord. 2012;13(1):75. doi: 10.1186/1471-2474-13-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Study will use hybrid model to create decision support package for conservative treatment of nonspecific low back pain. Lippincott’s Bone Joint Newsl. 2011; 17(6):67–8.
- 70.Shaw WS, Linton SJ, Pransky G. Reducing sickness absence from work due to low back pain: How well do intervention strategies match modifiable risk factors? J Occup Rehabil. 2006;16(4):591–605. doi: 10.1007/s10926-006-9061-0. [DOI] [PubMed] [Google Scholar]
- 71.Sueoka SS, LaStayo PC. Zone II flexor tendon rehabilitation: a proposed algorithm. J Hand Ther. 2008;21(4):410–413. doi: 10.1197/j.jht.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 72.Tuttle N. Is it reasonable to use an individual patient’s progress after treatment as a guide to ongoing clinical reasoning? J Manipulative Physiol Ther. 2009;32(5):396–403. doi: 10.1016/j.jmpt.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 73.Van Zundert J, Van Kleef M. Low back pain: From algorithm to cost-effectiveness? Pain Pract. 2005;5(3):179–189. doi: 10.1111/j.1533-2500.2005.05303.x. [DOI] [PubMed] [Google Scholar]
- 74.Wisneski RJRR. The Pennsylvania Plan II: an algorithm for the management of lumbar degenerative disc disease. Instr Course Lect. 1985;34:17–36. [PubMed] [Google Scholar]
- 75.Forseen SE, Corey AS. Clinical decision support and acute low back pain: evidence-based order sets. J Am Coll Radiol. 2012; 9(10):704–12.e704. [DOI] [PubMed]
- 76.Murphy DR, Hurwitz EL. A theoretical model for the development of a diagnosis-based clinical decision rule for the management of patients with spinal pain. BMC Musculoskel Disord. 2007;8(1):75. doi: 10.1186/1471-2474-8-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fritz JM, Brennan GP, Leaman H. Does the evidence for spinal manipulation translate into better outcomes in routine clinical care for patients with occupational low back pain? A case–control study. Spine J. 2006;6(3):289–295. doi: 10.1016/j.spinee.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 78.Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, Butler B, Garber M, Allison S. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27(24):2835–2843. doi: 10.1097/00007632-200212150-00021. [DOI] [PubMed] [Google Scholar]
- 79.Brence J. Should a prescriptive clinical prediction rule drive our decision process in patients with low back pain? SportEX Med. 2013;58:7–8. [Google Scholar]
- 80.Chen J, Phillips A, Ramsey M, Schenk R. A case study examining the effectiveness of mechanical diagnosis and therapy in a patient who met the clinical prediction rule for spinal manipulation. J Man Manip Ther. 2009;17(4):216–220. doi: 10.1179/106698109791352111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Childs JD. Validation of a clinical prediction rule to identify patients likely to benefit from spinal manipulation: a randomized clinical trial. Pittsburgh: University of Pittsburgh; 2003. [Google Scholar]
- 82.Childs JD, Flynn TW, Fritz JM. A perspective for considering the risks and benefits of spinal manipulation in patients with low back pain. Man Ther. 2006;11(4):316–320. doi: 10.1016/j.math.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 83.Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, Delitto A. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141(12):920–928. doi: 10.7326/0003-4819-141-12-200412210-00008. [DOI] [PubMed] [Google Scholar]
- 84.Childs JD, Fritz JM, Piva SR, Erhard RE. Clinical decision making in the identification of patients likely to benefit from spinal manipulation: a traditional versus an evidence-based approach. J Orthop Sports Phys Ther. 2003;33(5):259–272. doi: 10.2519/jospt.2003.33.5.259. [DOI] [PubMed] [Google Scholar]
- 85.Cleland J, Fritz J, Childs JD, Kulig K, Eberhart S, Davenport T, Magel J, Landel RF. Generalizability of a clinical prediction rule for identifying patients with low back pain who are likely to respond rapidly and dramatically to thrust manipulation. In: 14th annual meeting of the American Academy of Orthopaedic Manual Physical Therapists: 2008; Seattle, Washington; 2008, p. 161–81.
- 86.Cleland JA, Fritz JM, Kulig K, Davenport TE, Eberhart S, Magel J, Childs JD. Comparison of the effectiveness of three manual physical therapy techniques in a subgroup of patients with low back pain who satisfy a clinical prediction rule: a randomized clinical trial. Spine. 2009;34(25):2720–2729. doi: 10.1097/BRS.0b013e3181b48809. [DOI] [PubMed] [Google Scholar]
- 87.Cleland JA, Fritz JM, Whitman JM, Childs JD, Palmer JA. The use of a lumbar spine manipulation technique by physical therapists in patients who satisfy a clinical prediction rule: a case series. J Orthop Sports Phys Ther. 2006;36(4):209–214. doi: 10.2519/jospt.2006.36.4.209. [DOI] [PubMed] [Google Scholar]
- 88.Fritz JM, Childs JD, Flynn TW. Pragmatic application of a clinical prediction rule in primary care to identify patients with low back pain with a good prognosis following a brief spinal manipulation intervention. BMC Fam Pract. 2005;6(1):29. doi: 10.1186/1471-2296-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hallegraeff HJM, Winters JC, de Greef M, Lucas C. Manipulative therapy and clinical prediction criteria in treatment of acute nonspecific low back pain. Percept Mot Skills. 2009;108(1):196–208. doi: 10.2466/PMS.108.1.196-208. [DOI] [PubMed] [Google Scholar]
- 90.Hancock MJ, Maher CG, Latimer J, Herbert RD, McAuley JH. Independent evaluation of a clinical prediction rule for spinal manipulative therapy: a randomised controlled trial. Eur Spine J. 2008;17(7):936–943. doi: 10.1007/s00586-008-0679-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Learman K, Showalter C, Cook C. Does the use of a prescriptive clinical prediction rule increase the likelihood of applying inappropriate treatments? A survey using clinical vignettes. Man Ther. 2012;17(6):538–543. doi: 10.1016/j.math.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 92.Maher C, Childs JD, Cleland JA, Vreeman DJ. Clinical prediction rules. Virginia: American Physical Therapy Association Inc.; 2006. p. 759. [Google Scholar]
- 93.May S, Rosedale R. A case of a potential manipulation responder whose back pain resolved with flexion exercises. J Manipulative Physiol Ther. 2007;30(7):539–542. doi: 10.1016/j.jmpt.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 94.Resch K. Can a spinal manipulation clinical prediction rule improve decision making for patients with low back pain? Focus Altern Complement Ther. 2005;10(4):309–310. [Google Scholar]
- 95.Schenk R, Dionne C, Simon C, Johnson R. Effectiveness of mechanical diagnosis and therapy in patients with back pain who meet a clinical prediction rule for spinal manipulation. J Man Manip Ther. 2012;20(1):43–49. doi: 10.1179/2042618611Y.0000000017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Underwood M. A clinical prediction rule predicted outcome in patients with low back pain having spinal manipulation and exercise treatment. Evid Based Med. 2005;10(4):125–125. [Google Scholar]
- 97.Werneke MW, Hart D, Oliver D, McGill T, Grigsby D, Ward J, Weinberg J, Oswald W, Cutrone G. Prevalence of classification methods for patients with lumbar impairments using the McKenzie syndromes, pain pattern, manipulation, and stabilization clinical prediction rules. J Man Manip Ther. 2010;18(4):197–204. doi: 10.1179/106698110X12804993426965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Apeldoorn AT, Ostelo RW, van Helvoirt H, Fritz JM, de Vet HC, van Tulder MW. The cost-effectiveness of a treatment-based classification system for low back pain: design of a randomised controlled trial and economic evaluation. BMC Musculoskel Disord. 2010;11(1):58. doi: 10.1186/1471-2474-11-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Apeldoorn AT, Ostelo RW, van Helvoirt H, Fritz JM, Knol DL, van Tulder MW, de Vet HC. A randomized controlled trial on the effectiveness of a classification-based system for subacute and chronic low back pain. Spine. 2012;37(16):1347–1356. doi: 10.1097/BRS.0b013e31824d9f2b. [DOI] [PubMed] [Google Scholar]
- 100.Beneciuk JM, George S, Fritz J. Treatment-based classification subgroups among STarT Back Screening Tool risk categories in patients seeking outpatient physical therapy. In: CSM 2011 Orthopaedic and Sports Physical Therapy Section Programming: 2011; New Orleans, LA; 2011.
- 101.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute “nonspecific” low back pain: results of a randomized clinical trial. Spine. 2006;31(6):623–631. doi: 10.1097/01.brs.0000202807.72292.a8. [DOI] [PubMed] [Google Scholar]
- 102.Carpenter K, Mintken P. Examination, intervention, and outcomes for 3 patients treated with mechanical traction per the treatment-based classification: a retrospective case series. In: CSM 2009 Orthopaedic and Sports Physical Therapy Section Programming: 2009; Las Vegas, NV; 2009.
- 103.Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75(6):470–485. doi: 10.1093/ptj/75.6.470. [DOI] [PubMed] [Google Scholar]
- 104.Fritz JM, Cleland JA, Childs JD. Subgrouping patients with low back pain: evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37(6):290–302. doi: 10.2519/jospt.2007.2498. [DOI] [PubMed] [Google Scholar]
- 105.George SZ. Characteristics of patients with lower extremity symptoms treated with slump stretching: a case series. J Orthop Sports Phys Ther. 2002;32(8):391–398. doi: 10.2519/jospt.2002.32.8.391. [DOI] [PubMed] [Google Scholar]
- 106.Hebert JJ, Koppenhaver SL, Walker BF. Subgrouping patients with low back pain a treatment-based approach to classification. Sports Health Multidiscip Approach. 2011;3(6):534–542. doi: 10.1177/1941738111415044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Henry SM, Fritz JM, Trombley AR, Bunn JY. Reliability of a treatment-based classification system for subgrouping people with low back pain. J Orthop Sports Phys Ther. 2012;42(9):797–805. doi: 10.2519/jospt.2012.4078. [DOI] [PubMed] [Google Scholar]
- 108.Parent EC, FJ, Brennan GP, Hunter SJ, Long A. The effect of a workshop on using specific exercises on the outcomes of patients with low back pain and treatment-based classification. In: CSM 2009 Orthopaedic and Sports Physical Therapy Section Programming: 2009; Las Vegas, NV; 2009.
- 109.Scott DR, MA, Walters J: Use of treatment-based classification groups produces significant outcomes in patients with LBP. In: CSM 2008 Orthopaedic and Sports Physical Therapy Section Programming: 2008; Mashville, Tennessee; 2008.
- 110.Sions J. Combining mobilization and stabilization clinical prediction rules provide relief for patient with acute exacerbation of chronic low back pain. In: CSM 2009 Orthopaedic and Sports Physical Therapy Section Programming: 2009; Las Vegas; 2009.
- 111.Widerström B, Olofsson N, Arvidsson I, Harms-Ringdahl K, Larsson UE. Inter-examiner reliability of a proposed decision-making treatment based classification system for low back pain patients. Man Ther. 2012;17(2):164–171. doi: 10.1016/j.math.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 112.Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005;86(9):1753–1762. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 113.May S, Gardiner E, Young S, Klaber-Moffett J. Predictor variables for a positive long-term functional outcome in patients with acute and chronic neck and back pain treated with a McKenzie approach: a secondary analysis. J Man Manip Ther. 2008;16(3):155–160. doi: 10.1179/jmt.2008.16.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Fritz JM, Whitman JM, Flynn TW, Wainner RS, Childs JD. Factors related to the inability of individuals with low back pain to improve with a spinal manipulation. Phys Ther. 2004;84(2):173–190. [PubMed] [Google Scholar]
- 115.Cai C, Pua YH, Lim KC. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with mechanical lumbar traction. Eur Spine J. 2009;18(4):554–561. doi: 10.1007/s00586-009-0909-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Fritz JM, Lindsay W, Matheson JW, Brennan GP, Hunter SJ, Moffit SD, Swalberg A, Rodriquez B. Is there a subgroup of patients with low back pain likely to benefit from mechanical traction? Results of a randomized clinical trial and subgrouping analysis. Spine. 2007;32(26):E793–E800. doi: 10.1097/BRS.0b013e31815d001a. [DOI] [PubMed] [Google Scholar]
- 117.Hall H, McIntosh G, Boyle C. Effectiveness of a low back pain classification system. Spine J. 2009;9(8):648–657. doi: 10.1016/j.spinee.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 118.Stolze LR, Allison SC, Childs JD. Derivation of a preliminary clinical prediction rule for identifying a subgroup of patients with low back pain likely to benefit from Pilates-based exercise. J Orthop Sports Phys Ther. 2012;42(5):425–436. doi: 10.2519/jospt.2012.3826. [DOI] [PubMed] [Google Scholar]
- 119.Laslett M: Clinical prediction rule for rapid pain relief of low back pain following manipulation. NZ J Physiother. 2006; 34(2).
- 120.Vela LI, Haladay DE, Denegar C. Clinical assessment of low-back-pain treatment outcomes in athletes. J Sport Rehabil. 2011;20(1):74–88. doi: 10.1123/jsr.20.1.74. [DOI] [PubMed] [Google Scholar]
- 121.Chaitow L. Clinical prediction rules. J Bodyw Mov Ther. 2010;14(3):207–208. doi: 10.1016/j.jbmt.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 122.Cai C, Ming G, Ng LY. Development of a clinical prediction rule to identify patients with neck pain who are likely to benefit from home-based mechanical cervical traction. Eur Spine J. 2011;20(6):912–922. doi: 10.1007/s00586-010-1673-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Carpenter K, Mintken P, Cleland JA. Evaluation of outcomes in patients with neck pain treated with thoracic spine manipulation and exercise: a case series. NZ J Physiother. 2009;37(2):76. [Google Scholar]
- 124.Childs MJD, Fritz JM, Piva SR, Whitman JM. Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther. 2004;34(11):686–700. doi: 10.2519/jospt.2004.34.11.686. [DOI] [PubMed] [Google Scholar]
- 125.Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87(1):9–23. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 126.Cleland JA, Mintken PE, Carpenter K, Fritz JM, Glynn P, Whitman J, Childs JD. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010;90(9):1239–1250. doi: 10.2522/ptj.20100123. [DOI] [PubMed] [Google Scholar]
- 127.Cleland JA, CJ, Fritz JM, Whitman JM, Eberhart SL, A clinical prediction rule for classifying patients with neck pain who demonstrate short-term improvement with thoracic spine manipulation. In: 12th annual meeting of the American Academy of Orthopaedic Manual Physical Therapists: 2006; Charlotte, NC; 2006, p. 168–87.
- 128.Farrell KPL, Katherine E. Implementation of a treatment based classification system for neck pain: a pilot study. Orthop Phys Ther Pract. 2011;23(2):91–96. [Google Scholar]
- 129.Fritz JM, Brennan GP. Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain. Phys Ther. 2007;87(5):513–524. doi: 10.2522/ptj.20060192. [DOI] [PubMed] [Google Scholar]
- 130.Heintz MM, Hegedus EJ. Multimodal management of mechanical neck pain using a treatment based classification system. J Man Manip Ther. 2008;16(4):217–224. doi: 10.1179/106698108790818260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.O’Hearn M, ML, Gillespie C. Physical therapy outcomes of a treatment-based classification scheme for individuals with neck pain. In: CSM 2009 Orthopaedic and Sports Physical Therapy Section Programming: 2009; Las Vegas, NV; 2009.
- 132.Puentedura EJ, Cleland JA, Landers MR, Mintken P, Louw A, Fernández-de-las-Peñas C. Development of a clinical prediction rule to identify patients with neck pain likely to benefit from thrust joint manipulation to the cervical spine. J Orthop Sports Phys Ther. 2012;42(7):577–592. doi: 10.2519/jospt.2012.4243. [DOI] [PubMed] [Google Scholar]
- 133.Raney NH, Petersen EJ, Smith TA, Cowan JE, Rendeiro DG, Deyle GD, Childs JD. Development of a clinical prediction rule to identify patients with neck pain likely to benefit from cervical traction and exercise. Eur Spine J. 2009;18(3):382–391. doi: 10.1007/s00586-008-0859-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Raney NH, PE, Smith TA, Cowan JE, Rendeiro DG, Deyle GD, Childs JD. A clinical prediction rule for classifying patients with neck pain who demonstrate short-term improvement with cervical traction and exercise. In: CSM 2008 Orthopaedic and Sports Physical Therapy Section Programming: 2008; Mashville, Tennessee; 2008.
- 135.Tamayo A. The use of a clinical prediction rule for diagnosis and treatment based classification system for the treatment of a cervical radiculopathy patient: a case report. Orthop Phys Ther Pract. 2009;21(1):24–30. [Google Scholar]
- 136.Tseng Y-L, Wang WT, Chen W-Y, Hou T-J, Chen T-C, Lieu F-K. Predictors for the immediate responders to cervical manipulation in patients with neck pain. Man Ther. 2006;11(4):306–315. doi: 10.1016/j.math.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 137.Wyatt LH. Commentary on Cleland JA et. al_2007. J Am Chiropract Assoc. 2007; 27.
- 138.Schellingerhout JM, Verhagen AP. Letter to the Editor concerning “Development of a clinical prediction rule to identify patients with neck pain likely to benefit from cervical traction and exercise” by Raney N et al.(2009) Eur Spine J 18: 382–391. Eur Spine J. 2010;19(5):833–833. doi: 10.1007/s00586-010-1322-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Schellingerhout JM, Verhagen AP, Heymans MW, Pool JJM, Vonk F, Koes BW, de Vet HCW. Which subgroups of patients with non-specific neck pain are more likely to benefit from spinal manipulation therapy, physiotherapy, or usual care? Pain. 2008;139(3):670–680. doi: 10.1016/j.pain.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 140.Barton CJ, Menz HB, Crossley KM. Clinical predictors of foot orthoses efficacy in individuals with patellofemoral pain. Med Sci Sports Exerc. 2011;43(9):1603–1610. doi: 10.1249/MSS.0b013e318211c45d. [DOI] [PubMed] [Google Scholar]
- 141.Crowell MS, Wofford NH. Lumbopelvic manipulation in patients with patellofemoral pain syndrome. J Man Manip Ther. 2012;20(3):113–120. doi: 10.1179/2042618612Y.0000000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Iverson CA, Sutlive TG, Crowell MS, Morrell RL, Perkins MW, Garber MB, Moore JH, Wainner RS. Lumbopelvic manipulation for the treatment of patients with patellofemoral pain syndrome: development of a clinical prediction rule. J Orthop Sports Phys Ther. 2008;38(6):297–312. doi: 10.2519/jospt.2008.2669. [DOI] [PubMed] [Google Scholar]
- 143.Lesher JD, Sutlive TG, Miller GA, Chine NJ, Garber MB, Wainner RS. Development of a clinical prediction rule for classifying patients with patellofemoral pain syndrome who respond to patellar taping. J Orthop Sports Phys Ther. 2006;36(11):854–866. doi: 10.2519/jospt.2006.2208. [DOI] [PubMed] [Google Scholar]
- 144.Vaccaro AR, Lehman RA, Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30(20):2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 145.Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, Reinhold M, Aarabi B, Kandziora F, Chapman J. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine. 2013;38(23):2028–2037. doi: 10.1097/BRS.0b013e3182a8a381. [DOI] [PubMed] [Google Scholar]
- 146.Vicenzino B, Collins N, Cleland J, McPoil T. A clinical prediction rule for identifying patients with patellofemoral pain who are likely to benefit from foot orthoses: a preliminary determination. Br J Sports Med. 2010;44(12):862–866. doi: 10.1136/bjsm.2008.052613. [DOI] [PubMed] [Google Scholar]
- 147.Vicenzino B, Smith D, Cleland J, Bisset L. Development of a clinical prediction rule to identify initial responders to mobilisation with movement and exercise for lateral epicondylalgia. Man Ther. 2009;14(5):550–554. doi: 10.1016/j.math.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 148.Whitman JM, Cleland JA, Mintken P, Keirns M, Bieniek ML, Albin SR, Magel J, McPoil TG. Predicting short-term response to thrust and nonthrust manipulation and exercise in patients post inversion ankle sprain. J Orthop Sports Phys Ther. 2009;39(3):188–200. doi: 10.2519/jospt.2009.2940. [DOI] [PubMed] [Google Scholar]
- 149.Wixom SM, LaStayo P. A potential classification model for individuals with tennis elbow. J Hand Ther. 2012;25(4):418–421. doi: 10.1016/j.jht.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 150.Flynn T. Clinical prediction rules for the lumbar spine. N Z J Physiother. 2009;37(3):145–145. [Google Scholar]
- 151.Miller J. Clinical prediction rules: Time to sacrifice the holy cow of specificity? J Man Manip Ther. 2007;15(2):123–124. doi: 10.1179/106698107791090141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Murphy DR, Hurwitz EL. Application of a diagnosis-based clinical decision guide in patients with low back pain. Chiropr Man Ther. 2011;19(1):1–10. doi: 10.1186/2045-709X-19-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Nee RJ, Coppieters MW. Interpreting research on clinical prediction rules for physiotherapy treatments. Man Ther. 2011;16(2):105–108. doi: 10.1016/j.math.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 154.Yealy DM, Auble TE. Choosing between clinical prediction rules. New Engl J Med. 2003;349(26):2553. doi: 10.1056/NEJMe038184. [DOI] [PubMed] [Google Scholar]
- 155.Aebischer B, Hill JC, Hilfiker R, Karstens S. German translation and cross-cultural adaptation of the STarT back screening tool. PLoS ONE. 2015;10(7):1–14. doi: 10.1371/journal.pone.0132068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Luan S, Min Y, Li G, Lin C, Li X, Wu S, Ma C, Hill JC. Cross-cultural adaptation, reliability, and validity of the chinese version of the STarT back screening tool in patients with low back pain. Spine. 2014;39(16):E974–E979. doi: 10.1097/BRS.0000000000000413. [DOI] [PubMed] [Google Scholar]
- 157.Pombo N, Araújo P, Viana J. Knowledge discovery in clinical decision support systems for pain management: a systematic review. Artif Intell Med. 2014;60(1):1–11. doi: 10.1016/j.artmed.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 158.Smith MY, Depue JD, Rini C. Computerized decision-support systems for chronic pain management in primary care. Pain Med. 2007;8(Suppl 3):S155–S166. [Google Scholar]
- 159.Cresswell K, Majeed A, Bates DW, Sheikh A. Computerised decision support systems for healthcare professionals: an interpretative review. Inform Prim Care. 2012;20(2):115–128. doi: 10.14236/jhi.v20i2.32. [DOI] [PubMed] [Google Scholar]
- 160.Haskins R, Rivett DA, Osmotherly PG. Clinical prediction rules in the physiotherapy management of low back pain: a systematic review. Man Ther. 2012;17(1):9–21. doi: 10.1016/j.math.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 161.Patel S, Friede T, Froud R, Evans DW, Underwood M. Systematic review of randomized controlled trials of clinical prediction rules for physical therapy in low back pain. Spine. 2013;38(9):762–769. doi: 10.1097/BRS.0b013e31827b158f. [DOI] [PubMed] [Google Scholar]
- 162.Hill JC, Dunn KM, Main CJ, Hay EM. Subgrouping low back pain: a comparison of the STarT Back Tool with the Örebro Musculoskeletal Pain Screening Questionnaire. Eur J Pain. 2010;14(1):83–89. doi: 10.1016/j.ejpain.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Betten C, Sandell C, Hill JC, Gutke A. Cross-cultural adaptation and validation of the Swedish STarT Back Screening Tool. Eur J Physiother. 2015;17(1):29–36. [Google Scholar]
- 164.Bruyère O, Demoulin M, Beaudart C, Hill JC, Maquet D, Genevay S, Mahieu G, Reginster JY, Crielaard JM, Demoulin C. Validity and reliability of the French version of the start back screening tool for patients with low back pain. Spine. 2014;39(2):E123–E128. doi: 10.1097/BRS.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 165.Kongsted A, Johannesen E, Leboeuf-Yde C. Feasibility of the STarT back screening tool in chiropractic clinics: a cross-sectional study of patients with low back pain. Chiropr Man Ther. 2011;19(1):1–10. doi: 10.1186/2045-709X-19-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Morsø L, Albert H, Kent P, Manniche C, Hill J. Translation and discriminative validation of the STarT Back Screening Tool into Danish. Eur Spine J. 2011;20(12):2166–2173. doi: 10.1007/s00586-011-1911-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gusi N, Del Pozo-Cruz B, Olivares PR, Hernández-Mocholi M, Hill JC. The Spanish version of the “sTarT back screening tool” (SBST) in different subgroups. Aten Prim. 2011;43(7):356–361. doi: 10.1016/j.aprim.2010.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bruyère O, Demoulin M, Brereton C, Humblet F, Flynn D, Hill JC, Maquet D, Van Beveren J, Reginster JY, Crielaard JM, et al. Translation validation of a new back pain screening questionnaire (the STarT Back Screening Tool) in French. Arch Public Health. 2012;70(1):1–12. doi: 10.1186/0778-7367-70-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Piironen S, Paananen M, Haapea M, Hupli M, Zitting P, Ryynänen K, Takala EP, Korniloff K, Hill JC, Häkkinen A et al: Transcultural adaption and psychometric properties of the STarT Back Screening Tool among Finnish low back pain patients. Eur Spine J. 2015; 1–9. [DOI] [PubMed]
- 170.Speklé EM, Hoozemans MJM, van der Beek AJ, Blatter BM, Bongers PM, van Dieën JH. Internal consistency, test–retest reliability and concurrent validity of a questionnaire on work-related exposure related to arm, shoulder and neck symptoms in computer workers. Ergonomics. 2009;52(9):1087–1103. doi: 10.1080/00140130902915939. [DOI] [PubMed] [Google Scholar]
- 171.Hoozemans MJM, Speklé EM, Van Dieën JH. Concurrent validity of questions on arm, shoulder and neck symptoms of the RSI QuickScan. Int Arch Occup Environ Health. 2013;86(7):789–798. doi: 10.1007/s00420-012-0809-x. [DOI] [PubMed] [Google Scholar]
- 172.Speklé EM, Hoozemans MJM, van der Beek AJ, Blatter BM, van Dieën JH. The predictive validity of the RSI QuickScan questionnaire with respect to arm, shoulder and neck symptoms in computer workers. Ergonomics. 2012;55(12):1559–1570. doi: 10.1080/00140139.2012.718365. [DOI] [PubMed] [Google Scholar]