Abstract
Parathyroid adenoma is a benign tumor of the parathyroid glands. The cause of most parathyroid adenomas is unknown. Parathyroid adenoma increases the secretion of parathyroid hormone and results in primary hyperparathyroidism. High amounts of parathyroid hormone in the blood cause the imbalance of calcium, which leads to various complications such as kidney stones, depression, lethargy, nausea, vomiting, abdominal pain, myalgia, bone and joint pain, hoarseness, etc. Oropharyngeal dysphagia is defined as having problem in swallowing due to abnormalities in the structure and function of oropharynx and other related organs. The exact prevalence of dysphagia caused by parathyroid adenoma is unknown, but since this complication can lead to increased mortality and morbidity, its diagnosis is important. It is difficult to distinguish parathyroid malignancies from parathyroid adenoma even after surgery. Therefore, the final diagnosis is possible through surgery and histopathological evaluation. Here, a case of parathyroid adenoma with first presentation of generalized weakness and dysphagia has been reported.
Keywords: Parathyroid neoplasms, Dysphagia, Weakness, Iran
What’s Known
Parathyroid adenoma is a benign tumor of parathyroid glands.
Exact prevalence of dysphagia caused by parathyroid adenoma is unknown; however, since this complication can lead to increased mortality and morbidity, its diagnosis is important.
What’s New
Our patient with parathyroid adenoma initially presented with generalized weakness and dysphagia, which is a rare manifestation for this disease.
Introduction
Primary hyperparathyroidism is the most common cause of hypercalcaemia. A single parathyroid adenoma is usually its cause. Parathyroid adenoma is removed surgically when the patient has symptoms of hypercalcaemia.1
Adenoma causes the parathyroid glands to secrete more parathyroid hormone, which is called primary hyperparathyroidism. Too much parathyroid hormone disturbs body’s normal calcium balance and increases the amount of calcium in the blood stream. This is more frequent among women than men. Primary hyperparathyroidism may be caused by one adenoma, enlargement of all four parathyroid glands (hyperplasia), or cancer (which is very rare).2
A patient with parathyroid adenoma may also experience kidney stones and/or excessive urination. Moreover, there may be more general or nonspecific symptoms such as mental changes like depression, lethargy or confusion, nausea, vomiting, myalgia, abdominal pain, bone and joint pain, hoarseness, palpable neck mass, and unexplained pain.2
Asymptomatic parathyroid adenomas are usually diagnosed when a higher than normal calcium level is found in a routine blood test. The diagnosis of primary hyperparathyroidism is confirmed by using a test that shows parathyroid hormone levels in the blood.3
Sometimes the diagnosis of cancer is difficult even after surgery due to the similarity between parathyroid cancer cells and noncancerous adenoma cells. However, parathyroid cancer is so rare that many of otolaryngologist surgeons never encounter such a patient.2
In the current study, a case of parathyroid adenoma with generalized weakness and dysphagia as his first symptoms is presented.
Case Presentation
A 68-year-old man who was a known case of parathyroid hyperplasia since four years ago and underwent subtotal parathyroidectomy operation, referred with chief complaint of generalized weakness and dysphagia to solid foods since two months ago without a history of weight loss. He has had a positive history of renal stone due to hypercalcemia without surgical intervention. He did not have hypertension and other medical diseases that related to hypercalcemia. On physical examination, vital signs were stable.
During assessment by sestamibi scan, there was an uptake in upper of right mediastinum. Neck and upper chest CT-Scan with IV contrast was performed that showed an enhanced mass (8×3×3 cm) in upper of right mediastinum. His laboratory data were; serum calcium 14 mg/dl, serum phosphorus 2 mg/dl, and parathyroid hormone (PTH) 385.8 pg/ml. Due to hypercalcemia, the hydration was done by normal saline and then 60 mg starting dose of Lasix was administered.
The patient underwent neck collar incision, mid-sternotomy, and exploration of the neck. The mediastinal lymphadenectomy, resection of all lymphatic fats and glands in the anterior mediastinum, and dissection of visceral mediastinum were also done. There was a huge parathyroid adenoma in the form of a capsulated mass with the size of 8×3×3 cm behind the aortic arc and right innominate artery adjacent to esophagus, which was resected and sent for frozen section (figure 1). This mass was found in the anterior mediastinum and the result of frozen section was in favor of adenoma. Then, adenoma was confirmed by pathology (figure 2). At the end of the operation, one chest tube and vacuum drainage were inserted.
Figure 1.

Huge capsulated mass with the size of 8×3×3 cm behind the aortic arc and right innominate artery adjacent to esophagus.
Figure 2.
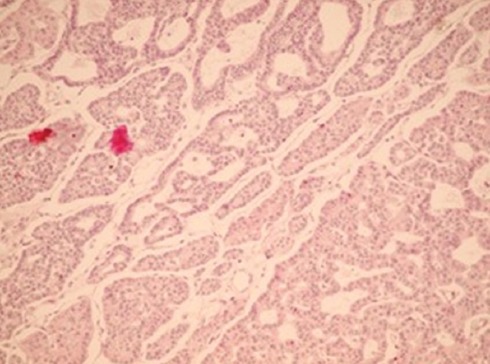
High power view of the parathyroid adenoma pattern.
During postoperative days, his serum calcium ranges were 12.5, 10.9, 10.4, 9.9, 8.2, 8.7, and 9.1 mg/dl, respectively, and serum PTH was 19.75 pg/ml.
The patient was discharged in good condition and normal serum calcium level. He was referred to a clinic for postoperative visits. Since his serum calcium level was 7.5 mg/dL, calcium carbonate was started, which increased his calcium level up to 9.2 mg/dL. His dysphagia and weakness were resolved during work up completely.
Patient’s anonymity has been respected, and consent has been taken for publication.
Discussion
Parathyroid adenoma is an unusual phenomenon, which can cause the resolution of primary hyperparathyroidism.4 In about 6-16% of cases, one or more hyperfunctioning parathyroid gland(s) are found in an ectopic location.5 Dysphagia, neck discomfort and sore throat are among common symptoms of parathyroid adenoma.4 Reports reveal that pain, swelling, tenderness in anterior neck, dysphagia, hoarseness, and ecchymosis are among the usual presentations of parathyroid adenoma.6 Many patients with primary hyperparathyroidism have a series of non-specific symptoms including fatigue, irritability, cognitive impairment, and dysphagia. Parathyroid disease is often associated with symptoms related to hypercalcemia such as osteopenia, depression, bone pain, weakness, and nephrolithiasis. Moreover, in patients with parathyroid disease, oropharyngeal dysphagia can be unusually developed due to a direct pressure on the relevant organs by a large adenoma and ectopic. This may also occur in cases of carcinoma and parathyroid adenoma hemorrhage. The exact prevalence of dysphagia is unknown, but in different studies, it has been mentioned to be 22 percent in people over 50 years of age. This complication causes problems in swallowing and consequently can increase mortality and morbidity. Many patients have the perception of dysphagia with parathyroid disease. Parathyroid surgery leads to significant improvements in this group in many aspects of swallowing-related quality of life measured by the SWAL-QOL instrument. Techniques such as cinefluouroscopy, modified barium swallow, manometry, and upper endoscopy are valuable in evaluating dysphagia. These can help to understand the extent of mechanical disability, but it is important to note that they will not help to treat the complication.7
Liu and colleagues conducted a study in which the clinical features of parathyroid space-occupying lesions were examined in 42 patients. Among 42 cases, 29 patients had parathyroid adenoma in which 3 patients were with dyspnea and dysphagia.8
In a study by Pinchot and colleagues 83 out of 102 patients had parathyroid adenoma among which cases with dysphagia had a significantly lower quality of life than other patients.7
In another study by Yang and colleagues during 1995-2005, 48 cases were examined where 46 out of 48 patients had parathyroid adenoma and the remaining two had parathyroid carcinoma. Serum calcium level and parathyroid hormone had been increased in all 48 cases. Unilateral neck exploration was done in 18 cases with no tumor remnants and bilateral exploration was done in 13 other cases. The study notes that evaluating the level of calcium and parathyroid hormone are both reliable methods for diagnosing parathyroid adenoma and parathyroid carcinoma. It was also shown that the combined use of ultrasonography and 99mTc-MIBI scintigraphy methods is suitable in determining the place of adenomas.9
The sestamibi scan is now the best method for detecting a diseased parathyroid gland before an operation. No other tests come close to it in terms of accuracy. The sestamibi scan has 90% sensitivity and 98-100% specificity.10
At least a one-year follow up period of both clinical and laboratorial investigation is recommended for the diagnosis of parathyroid adenomas.11 Another point worth mentioning is that techniques such as sestamibi scanning, perhaps cannot exactly locate the neoplasm. Therefore, surgery is preferred in order to reach the optimal treatment.12
Conclusion
Although dysphasia is not a common presentation of parathyroid adenoma, we should consider it as a symptom in our differential diagnosis. In the present case, the chief complaint of the patient was dysphagia and the final diagnosis was a huge parathyroid adenoma.
Acknowledgement
We hereby wish to thank Miss Ghasemi for her great help in typesetting and grammatical editing.
Conflict of Interest: None declared.
References
- 1.Gujral JS, El-Choufi L. Spontaneous Haemorrhagic Infarction of Parathyroid Adenoma. Journal, Indian Academy of Clinical Medicine. 2007;8:352–4. [Google Scholar]
- 2.Hyperparathyroidism AATFoP. The American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49–54. doi: 10.4158/EP.11.1.49. [DOI] [PubMed] [Google Scholar]
- 3.Hyperparathyroidism [Internet] Bethesda: Medline Plus; [cited 2010 August 31]. Available from: https://www.nlm.nih.gov/medlineplus/ency/article/001215.htm . [Google Scholar]
- 4.Micale SJ, Kane MP, Busch RS. Spontaneous resolution of primary hyperparathyroidism in parathyroid adenoma. Case Rep Endocrinol. 2012;2012:793753. doi: 10.1155/2012/793753. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roy M, Mazeh H, Chen H, Sippel RS. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg. 2013;37:102–6. doi: 10.1007/s00268-012-1773-z. [DOI] [PubMed] [Google Scholar]
- 6.Cetani F, Ambrogini E, Faviana P, Vitti P, Berti P, Pinchera A, et al. Spontaneous short-term remission of primary hyperparathyroidism from infarction of a parathyroid adenoma. J Endocrinol Invest. 2004;27:687–90. doi: 10.1007/BF03347505. [DOI] [PubMed] [Google Scholar]
- 7.Pinchot SN, Youngwirth L, Rajamanickam V, Schaefer S, Sippel R, Chen H. Changes in swallowing-related quality of life after parathyroidectomy for hyperparathyroidism: a prospective cohort study. Oncologist. 2012;17:1271–6. doi: 10.1634/theoncologist.2012-0203. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu FZ, Dong MM, Zhu Y, Zhang Y, Fan QH. [Clinical features of parathyroid space-occupying lesions] Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2009;44:282–6. [PubMed] [Google Scholar]
- 9.Yang ZQ, Zhu LW, Wang PZ. [Diagnosis and surgical treatment of 48 cases of parathyroid adenoma and parathyroid carcinoma] Zhonghua Zhong Liu Za Zhi. 2006;28:625–7. [PubMed] [Google Scholar]
- 10.Preoperative Localization of Parathyroid Tumors [Internet] Montclair: Endocrin web; [cited 2010 Oct 12]. Available from: http://www.endocrineweb.com . [Google Scholar]
- 11.Kataoka K, Taguchi M, Takeshita A, Miyakawa M, Takeuchi Y. Recurrence of primary hyperparathyroidism following spontaneous remission with intracapsular hemorrhage of a parathyroid adenoma. J Bone Miner Metab. 2008;26:295–7. doi: 10.1007/s00774-007-0816-2. [DOI] [PubMed] [Google Scholar]
- 12.Foppiani L, Del Monte P, Sartini G, Arlandini A, Quilici P, Bandelloni R, et al. Intrathyroidal parathyroid carcinoma as cause of hypercalcemia and pitfall of localization techniques: clinical and biologic features. Endocr Pract. 2007;13:176–81. doi: 10.4158/EP.13.2.176. [DOI] [PubMed] [Google Scholar]


