Abstract
Periodontitis, a chronic infection by periodontopathic bacteria, induces uncontrolled inflammation, which leads to periodontal tissue destruction. 2,3,5,4′-Tetrahydroxystilbene-2-O-beta-glucoside (THSG), a polyphenol extracted from Polygoni Multiflori, reportedly has anti-inflammatory properties. In this study, we investigated the mechanisms of THSG on the Porphyromonas gingivalis-induced inflammatory responses in human gingival fibroblasts and animal modeling of ligature-induced periodontitis. Human gingival fibroblast cells were treated with lipopolysaccharide (LPS) extracted from P. gingivalis in the presence of resveratrol or THSG to analyze the expression of TNF-α, IL-1β, and IL-6 genes. Increased AMP-activated protein kinase (AMPK) activation and SirT1 expression were induced by THSG. Treatment of THSG decreased the expression of LPS-induced inflammatory cytokines, enhanced AMPK activation, and increased the expression of SirT1. In addition, it suppressed the activation of NF-κB when cells were stimulated with P. gingivalis LPS. The anti-inflammatory effect of THSG and P. Multiflori crude extracts was reproduced in ligature-induced periodontitis animal modeling. In conclusion, THSG inhibited the inflammatory responses of P. gingivalis-stimulated human gingival fibroblasts and ameliorated ligature-induced periodontitis in animal model.
1. Introduction
Periodontitis is an immune-associated inflammatory disease of the periodontium characterized by progressive destruction of the supporting tissues of teeth [1]. It can destroy the surrounding connective tissue and adjacent alveolar bone and eventually causes tooth loss [2, 3]. The immune and inflammatory responses that are critical to the pathogenesis of periodontitis are modified by a number of host-related factors [4]. Therefore, while microbial plaque is the primary etiology and initiates the host immune response, which induces the signs of periodontitis [5], the major component of the outer membrane of Gram-negative bacteria, Porphyromonas gingivalis, lipopolysaccharide (LPS), initiates the production of various cytokines such as interleukin-8 (IL-8) and TNF-α [6] which infiltrate gingival connective tissue and elicit a local inflammatory response. It further causes an increase in number and activity of polymorphonucleocytes (PMN) along with these cytokines. PMNs also produce reactive oxygen species (ROS) superoxide via the respiratory burst mechanism as part of the defense response to infection [7]. The neutrophil-produced high levels of ROS are associated with the local and systemic destructive phenotype found in the chronic inflammatory disease periodontitis [8]. The ROS has the capacity to activate macrophages to synthesize and secrete inflammatory cytokines and hydrolytic enzymes, which manifest potent proinflammatory and catabolic activities and play key roles in periodontal tissue breakdown [9]. Periodontitis has been shown to link other chronic diseases such as diabetes, cardiovascular diseases, and rheumatoid arthritis. Studies indicate that treatment of rheumatoid arthritis may improve the associated periodontal disease and vice versa [8].
Lately natural compounds capable of modulating the host inflammatory response have received considerable attention [10]. Naturally occurring orally related antibacterial and anti-inflammatory actions of polyphenols are capable of modulating the host inflammatory response. Of these, certain flavonoids appear to stand out because of their beneficial profile and clinical evidence [10]. Resveratrol (trans-3,4′,-5-trihydroxystilbene) is a widely existing stilbenoid in grape skin [11] and in other plants such as berries and peanuts [12, 13]. It exhibits antioxidant activity and contributes to a reduction in inflammation [14]. Resveratrol has been shown to neutralize free radicals and other oxidizing molecules [13]. Its supplementation directly suppresses the release of proinflammatory cytokines such as TNF-α, IL-1β, IL-6, IL-10, MCP-1, IFNα, and IFNβ in a wide range of tissues [15–19], including the brain in rodents [20]. It has been shown to significantly inhibit NF-κB-dependent cell adhesion molecules in monocyte adhesion to the endothelium induced by P. gingivalis LPS suggesting that resveratrol has therapeutic effect in periodontal pathogen-induced vascular inflammation [21]. Resveratrol has been shown to effectively delay osteoblastogenesis and subsidize new bone formation [22]. These properties are very essential for the treatment of periodontitis.
The stilbene glucoside 2,3,5,4′-tetrahydroxystilbene-2-O-β-D-glucoside (THSG) is one of the major bioactive components of Polygonum multiflorum Thunb. (He Shou Wu), which has been shown to exert antiaging activities [23]. It also has protective effects on experimental colitis by reducing the level of oxygen and nitrogen free radicals [24]. Mechanism involved in P. multiflorum-induced antiatherosclerosis may be caused by THSG-induced antagonistic effects on oxidation of lipoprotein, proliferation, and decrease of NO content of coronary arterial smooth muscle cells [25]. It also has been shown to exert protective effect on cardiotoxicity induced by doxorubicin in vitro and in vivo [26]. In addition, THSG can diminish peroxidation levels in the brain in a mouse model of Alzheimer's disease or cerebral ischemia-reperfusion. The protective effects of THSG are mediated by modulation of JNK, SirT1, and NF-κB pathways [27].
In animals, experimental periodontitis can be induced by dietary manipulation [28], bacterial toxin injection [29], laying of peridental silk ligatures or orthodontic elastics for bacterial colonization [29, 30], and surgical removal of alveolar bone [31, 32]. In the present study, we investigate the role of ethanol extract of P. Multifloriand pure 2,3,5,4′-tetrahydroxystilbene-2-O-beta-glucoside on the degree of alveolar bone loss associated with periodontitis in rats and its signal transduction pathways involved in the preventative and inhibitory effects in the development of periodontitis.
2. Materials and Methods
2.1. Reagents
2,3,5,4′-Tetrahydroxystilbene-2-O-beta-glucoside (THSG, purity: 95%, dissolved in 50% ethanol for animal feeding; dissolved in DMSO for cell treatment) was kindly provided by Dr. Ching-Chiung Wang. Resveratrol (Sigma-Aldrich, Inc., St. Louis, Mo, USA) was dissolved in 50% ethanol for animal feeding and dissolved in DMSO for cell treatment.
2.2. Plant Materials
P. multiflora Thunb was purchased from a traditional Chinese medicine market in China and identified by Industrial Technology Research Institute, Taiwan. Moreover, voucher specimens (He Shou Wu 01) of dried rhizoma were deposited in the Graduate Institute of Pharmacognosy, College of Pharmacy, Taipei Medical University, Taipei, Taiwan.
2.3. Extraction
The rhizome of P. multiflora was cut into small pieces, immersed in a 10-fold amount of 50% ethanol, and refluxed for 2 hour at 65°C, twice. And then the twice filtrate was combined and concentrated under a vacuum using a rotary evaporator to remove the ethanol. The ethanolic extract was freeze-dried to yield the powder (PM-E). The yield of PM-E was about 27.82% (w/w) and 2,3,5,4′-tetrahydroxystilbene-2-O-beta-glucoside (THSG) amount is 8.0% in PM-E by HPLC analysis. The substance marker, THSG (purity: 95%), was kindly provided by Dr. Ching-Chiung Wang.
2.4. Isolation and Culture of Human Gingival Fibroblasts
Human gingival fibroblasts (HGFs) were obtained from five patients (males aged 22 to 32 years; mean age: 24 years), and all experiments were repeated three times as described in our previous study [33]. Briefly, gingival specimens were taken from gingivectomy, crown lengthening, or distal wedge procedure of noninflamed periodontal tissues. Specimens were directly submerged in Leibovitz L-15 medium (Invitrogen, Grand Island, NY, USA) containing 2 mg/mL Dispase II (Roche Diagnostics, Indianapolis, IN, USA) and 10% fetal bovine serum (FBS) (Invitrogen) at 4°C for 2 days. After separating and removing the outer epithelial layer, the connective tissue was minced and digested in Leibovitz L-15 medium containing 10% FBS and 2 mg/mL collagenase (Sigma-Aldrich, Inc.) for 24 hours. Tissue was then placed in flasks containing 10% FBS in Dulbecco modified Eagle medium/F12 (DMEM/F12) (Invitrogen) to allow the cells to migrate from the explants. HGFs of five to seven passages were used for these experiments. When HGFs reached 80% confluence, cells were starved in serum-free DMEM/F12 for 24 hours before experiments. Similar patterns were examined in different cell origins, and one of them was selected to report. Approval of all procedures was granted by the Ethics Committee of the Faculty of Medicine, Tri-Service General Hospital, Taipei, Taiwan (TSGHIRB number 2-103-05-067). All participants included in the study signed a written consent form before the procedure.
2.5. Cell Viability Test
To evaluate the toxic effects of resveratrol and THSG on HGFs, HGFs were placed at a density of 1 × 103 cell/well in the wells of 96-well plates containing DMEM/F12 and 10% FBS and cultured until 80% confluence. The cells were washed once with phosphate-buffered saline, and the medium was replaced with serum-free medium for 24 hours' starvation. THSG and resveratrol were solubilized in DMSO at different concentrations in all experiments below. The cell viability of HGFs was tested after treatment of THSG (0, 10, 25, 100, or 200 μM) or resveratrol (0, 10, 25, 100, or 200 μM) in 0.25% stripped FBS medium for 72 h with reflashed medium with agents daily. The cell viability was performed with CellTiter 96® AQueous One Solution (Promega, Madison, WI, USA) according to the manufacturer's protocol.
2.6. Quantitative Real-Time PCR
To examine the effects of resveratrol and THSG on the mRNA expression of proinflammatory cytokines, we treated HGFs with vehicle, 1 μg/mL P. gingivalis LPS (Porphyromonas gingivalis lipopolysaccharide) (InvivoGen, San Diego, CA, USA), 1 and 10 μM resveratrol, and 1 and 10 μM THSG or combined treatments for 6 h. Furthermore, in order to investigate the impacts of THSG on proinflammatory cytokines and inflammatory markers in ligature-induced experimental periodontitis of rats, silk-surrounded gingival tissues were removed and homogenized by a high-throughput tissue (Precellys® 24, Bertin Corp., Rockville, MD, USA). Total RNA was extracted and genomic DNA was also eliminated with illustra RNAspin Mini RNA Isolation Kit (GE Healthcare Life Sciences, Buckinghamshire, United Kingdom). 1 μg of DNase I-treated total RNA was reverse-transcribed with RevertAid H Minus First Strand cDNA Synthesis Kit (Life Technologies Corporation, Carlsbad, California, USA) into cDNA and used as the template for real-time PCR reactions and analysis. The real-time PCR reactions were performed using QuantiNova™ SYBR® Green PCR Kit (QIAGEN) on CFX Connect™ Real-Time PCR Detection System (Bio-Rad Laboratories, Inc., Hercules, CA, USA). This involved an initial denaturation at 95°C for 5 min, followed by 45 cycles of denaturing at 95°C for 5 sec and combined annealing/extension at 60°C for 10 sec, as described in the manufacturer's instructions. The primer sequences were shown as follows: Homo sapiens tumor necrosis factor-alpha (TNF-α), forward 5′-GCCCATGTTGTAGCAAACCC-3′ and reverse 5′-TATCTCTCAGCTCCACGCCA-3′ (accession number NM_000594.3); Homo sapiens interleukin-1 beta (IL-1β), forward 5′-CTTCGAGGCACAAGGCACA-3′ and reverse 5′-GCTTCAGACACTTGAGCAATGA-3′ (accession number NM_000576.2); Homo sapiens interleukin-6 (IL-6), forward 5′-AATCATCACTGGTCTTTTGGAG-3′ and reverse 5′-GCATTTGTGGTTGGGTCA-3′ (accession number NM_000600.3); Homo sapiens sirtuin 1 (SirT1), forward 5′-TTGGGTACCGAGATAACCTTCT-3′ and reverse 5′-TTGCATGTGAGGCTCTATCC-3′ (accession number NM_012238.4); Homo sapiens 18S ribosomal RNA (18S), forward 5′-GTAACCCGTTGAACCCCATT-3′ and reverse 5′-CCATCCAATCGGTAGTAGCG-3′ (accession number NR_003286); Rattus norvegicus tumor necrosis factor-alpha (TNF-α), forward 5′-TTCTCATTCCTGCTCGTGGC-3′ and reverse 5′-GCCCATTTGGGAACTTCTCCT-3′ (accession number NM_012675.3); Rattus norvegicus interleukin-1 beta (IL-1β), forward 5′-AGCTTTCGACAGTGAGGAGAA-3′ and reverse 5′-TCATCTGGACAGCCCAAGTC-3′ (accession number NM_031512.2); Rattus norvegicus inducible nitric oxide synthase (iNOS), forward 5′-AAAACCCCAGGTGCTATTCCC-3′ and reverse 5′-TCCAGGGATTCTGGAACATTCTGT-3′ (accession number NM_012611.3); Rattus norvegicus cyclooxygenase-2 (COX-2), forward 5′-TTCCAAACCAGCAGGCTCAT-3′ and reverse 5′-AAAAGCAGCTCTGGGTCGAA-3′ (accession number L20085.1); Rattus norvegicus sirtuin 1 (SirT1), forward 5′-AGGCCACGGATAGGTCCATA-3′ and reverse 5′-GAATTGTTCGAGGATCGGTGC-3′ (accession number XM_006223877.2); Rattus norvegicus 18S ribosomal RNA (Rn18S), forward 5′-CCTGGTTGATCCTGCCAGTAG-3′ and reverse 5′-GGCCGTGCGTACTTAGACAT-3′ (accession number NR_046237.1). Calculations of relative gene expression (normalized to 18S reference gene) were performed according to the ΔΔCT method. Fidelity of the PCR reaction was determined by melting temperature analysis.
2.7. Nuclear and Cytoplasmic Protein Extraction
To examine the effects of THSG in P. gingivalis LPS-induced NF-κB activation, nuclear and cytoplasm proteins were extracted and isolated from HGFs by using of the Thermo Scientific NE-PER® Nuclear and Cytoplasmic Extraction Kit protocol (Thermo Scientific, Rockford, IL, USA). Briefly, HGFs were lysed in cytoplasm extraction reagent and were centrifuged at 16,000 ×g for extraction of the nuclear material. Proteins from the nuclear material were further extracted by the addition of nuclear extraction reagent to the nuclei and centrifuged at 16,000 ×g. Nuclear and cytoplasmic extracts were stored at −80°C until use. The protein concentration of the nuclear and cytoplasmic extracts was determined with the BCA™ Protein Assay kit (Thermo Scientific).
2.8. Western Blot Analysis
To examine the effects of THSG in P. gingivalis LPS-induced NF-κB activation in nucleus, we performed Western blot analysis to quantify the protein expression levels of NF-κB in the nuclear extracts of HGFs which had been pretreated with 25 μM THSG and followed by the treatment with 1 μg/mL P. gingivalis LPS for 3 h. Nuclear protein samples were resolved on a 10% sodium dodecyl sulfate polyacrylamide gel (SDS-PAGE). A 20-μg quantity of protein was loaded in each well with 5x sample buffer, and the protein samples were resolved by electrophoresis at 100 V for 2 hrs. The resolved proteins were transferred from the polyacrylamide gel to Millipore Immobilon-PSQ Transfer PVDF membranes (Millipore, Billerica, MA, USA) with the Mini Trans-Blot® Cell (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The membranes were blocked with a solution of 2% fetal bovine serum in Tris-buffered saline. The membranes were incubated with primary antibodies to NF-κB, phospho-p44/42 MAPK (pERK1/2), ERK2, glyceraldehyde 3-phosphate dehydrogenase (GAPDH) (GeneTex International Corporation, Hsinchu City, Taiwan), phospho-AMPKα, AMPKα (Cell Signaling Technology, Inc., Beverly, MA, USA), and Lamin B1 (Abcam, Cambridge, MA, USA), at 4°C overnight and washed, and the proteins were detected with HRP-conjugated secondary antibodies and Immobilon™ Western HRP Substrate Luminol Reagent (Millipore). Images of the Western blots were visualized and recorded by BioSpectrum® Imaging System (UVP, LLC, Upland, CA, USA).
2.9. Ligature-Induced Experimental Periodontitis in Rats
All rats were housed in a reserved, pathogen-free facility and were handled in accordance with protocols approved by the Institutional Animal Care and Use Committee, National Defense Medical Center, Taipei, Taiwan (IACUC-15-361). A group of 8-week-old male Sprague-Dawley rats weighing between 200 and 250 g (n = 50) were randomly divided into eleven treatment groups defined as follows: nonligature (control, n = 10); ligature (n = 10); ligature + 0.1 mg/kg/d of THSG (n = 5); ligature + 10 mg/kg/d of THSG (n = 5); ligature + 25 mg/kg/d of resveratrol (n = 5); ligature + 12.5 mg/kg/d of ethanol extracts (n = 5); ligature + 25 mg/kg/d of ethanol extracts (n = 5); ligature + 50 mg/kg/d of ethanol extracts (n = 5). For the ligation, THSG, and ethanol extracts groups, experimental periodontitis was induced by placing 3-0 silk sutures around mandibular first molars at the gingival level (two molars in each rat), as described in our previous study [34]. The rats in the THSG and ethanol extracts groups also received these extracts by gavage feeding, starting 1 d before ligation. The rats in the control and ligature groups received sterile water daily. On day 8, all rats were sacrificed by CO2 inhalation, and the mandibles were excised and silk-surrounded gingiva was also collected for further mRNA examination, and then the mandibles were fixed in 4% paraformaldehyde. The mandibular specimens were prepared for dental radiography.
2.10. Radiographic Examination
To verify the level of bone loss for these treatment groups, the mandibular molars were examined by digital radiography using a computerized imaging system (Asahi Xspot; Asahi Roentgen Ind. Co., Ltd., Kyoto, Japan). The X-ray tube was operated at 70 kV, with a current of 6 mA, for 0.64 s, and the source-to-sensor distance was 50 cm. The images were processed using an image management system (INFINITT Dental PACS image system; INFINITT North America Inc., Phillipsburg, NJ, USA). We determined the dental alveolar bone level, defined as the distance from the cementoenamel junction (CEJ) to the most coronal level of the alveolar bone crest (CEJ-bone distance), using IMAGE J processing software (Image J software, National Institutes of Health, Bethesda, MD, USA). We also measured the radiographic periodontal bone-supporting ratio. The two parameters of the first mandibular molar were recorded along the mesial or distal root surfaces, respectively [34].
2.11. Statistical Analyses
In this study, all of the collected data of immunoblot and nucleotide densities were analyzed by IBM® SPSS® Statistics software version 19.0 (SPSS Inc., Chicago, IL, USA). Two-tail Student's t-test was conducted and considered significant at p values < 0.05 (∗ or #), 0.005 (∗∗ or ##), and 0.001 (∗∗∗ or ###).
3. Results
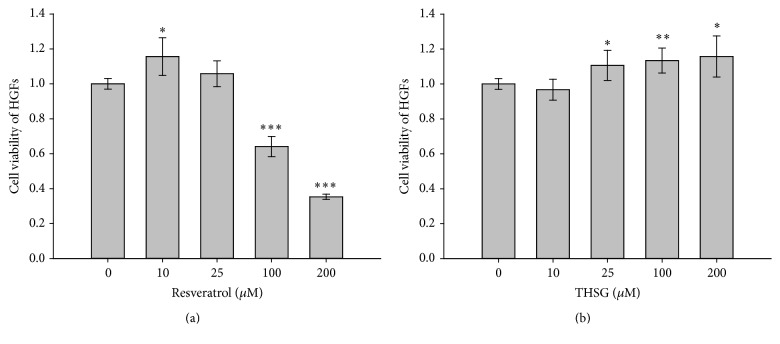
3.1. Resveratrol and THSG Stimulate Cell Proliferation in HGFs
HGFs (1 × 104 cells/well) were cultured in 96-well plate for 24 h and then starved with serum-free DMEM/F12 medium for 24 h. After starvation, HGFs were refed with medium containing 0.25% stripped FBS with different concentrations of resveratrol (0, 10, 25, 100, or 200 μM) or THSG (0, 10, 25, 100, or 200 μM) reflashed daily for 72 h. Resveratrol significantly enhanced cell proliferation of HGFs at low concentration (10 μM) but inhibited cell proliferation at high concentrations (100 and 200 μM) significantly (Figure 1(a)). On the other hand, THSG significantly enhanced HGFs cell proliferation when the concentration was over 25 μM and did not show any cytotoxic effect in HGFs (Figure 1(b)).
Figure 1.
The cytotoxic effects of resveratrol and THSG in HGFs. HGFs (1 × 104 cells/well) were cultured in 96-well plate and then were starved with serum-free DMEM/F12 medium for 24 h. After starvation, HGFs were treated with (a) resveratrol (0, 10, 25, 100, or 200 μM) or (b) THSG (0, 10, 25, 100, or 200 μM) in 0.25% stripped FBS medium for 72 h with reflashed medium with agents daily. (Numbers of experiments are 5, N = 5; ∗ p < 0.05; ∗∗ p < 0.01; ∗∗∗ p < 0.001 were compared with solvent/DMSO group.)
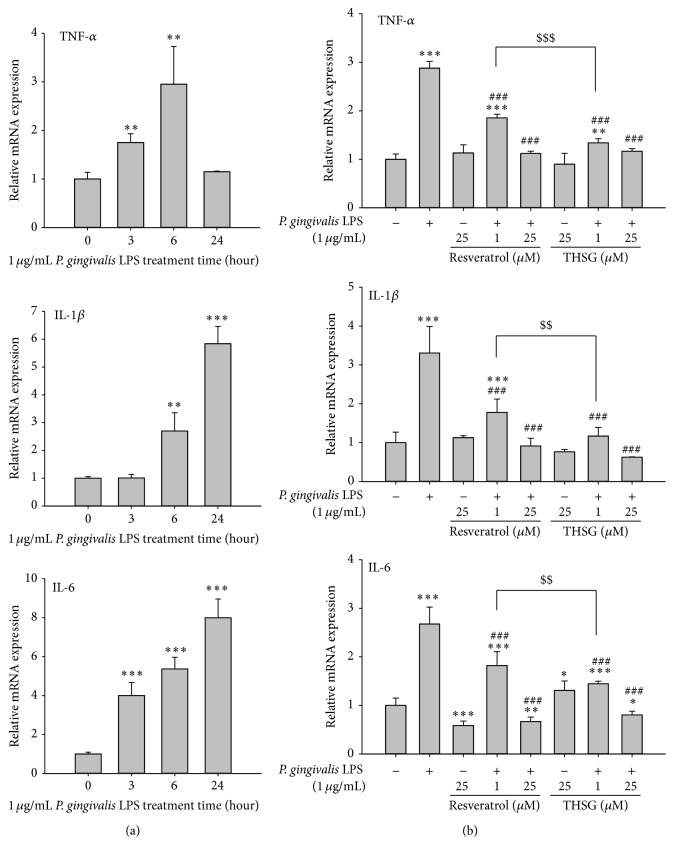
3.2. Resveratrol and THSG Induce Anti-Inflammatory Effects in P. gingivalis LPS-Treated HGFs
HGFs were cultured in 6-well plate. After starvation, cells were treated with 1 μg/mL of LPS extracted from P. gingivalis for 0, 3, 6, and 24 h prior to harvest. Total RNA was extracted and quantitative PCR was performed. LPS induced the expression of TNF-α at 3 h and maximum expression at 6 h (Figure 2(a), upper panel). LPS stimulated the expression of IL-1β at 6 h and expressed more at 24 h. LPS stimulated the expression of IL-6 at 3 h, 6 h, and 24 h (Figure 2(a), middle and lower panel).
Figure 2.
The anti-inflammatory effects of resveratrol and THSG in P. gingivalis LPS-treated HGFs. HGFs were cultured in 6-well plate and were starved with serum-free DMEM/F12 medium for 24 h when the cell confluence reached 80%. (a) HGFs were treated with 1 μg/mL P. gingivalis LPS for 0, 3, 6, and 24 h. (b) HGFs were pretreated with resveratrol and THSG (1 and 25 μM) for 30 min and then were treated with 1 μg/mL P. gingivalis LPS for 6 h. Total RNA was extracted and reverse transcripted to cDNA, and then the quantitative PCR was performed. (N = 3; ∗ p < 0.05; ∗∗ p < 0.01; ∗∗∗ p < 0.001 were compared with control group. ### p < 0.001 were compared with LPS group. $$ p < 0.01; $$$ p < 0.001 were compared with 1 μM resveratrol group with LPS treatment.)
HGFs were cultured in 100 mm Petri dish and starved with serum-free DMEM/F12 medium for 24 h before studies. HGFs were pretreated with resveratrol or THSG (1 and 25 μM) for 30 min and then treated with 1 μg/mL P. gingivalis LPS for another 6 h. Resveratrol and THSG significantly attenuated LPS-induced expression of proinflammatory cytokines such as TNF-α, IL-1β, and IL-6 (Figure 2(b)). The inhibitory effect on the expression of proinflammatory cytokines by low concentration of THSG (1 μM) was more than that of resveratrol.
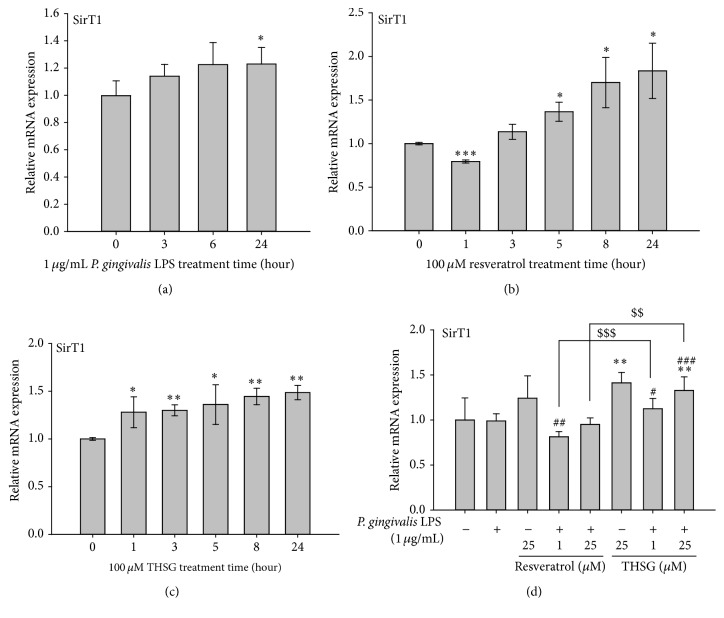
3.3. THSG Attenuate P. gingivalis LPS-Induced Proinflammatory Cytokines Expression via Induced SirT1 Expression in HGFs
Activation of SirT1 is involved in anti-inflammatory process [16, 35]. It is of interest to investigate if activation of SirT1 also plays a role in THSG-inhibited proinflammatory cytokines expression. HGFs were cultured in 6-well plate and were starved with serum-free DMEM/F12 medium for 24 h when the cell confluence was reached to 80%. HGFs were treated with 1 μg/mL of LPS extracted from P. gingivalis, 100 μM resveratrol, or THSG, and then RNA was extracted. QPCR of SirT1 was conducted. Results shown in Figure 3(a) indicate that LPS significantly induced SirT1 expression at 24 h. However, resveratrol significantly reduced the mRNA expression of SirT1 at 1 h but enhanced it at 5 h to 24 h dramatically (Figure 3(b)). On the other hand, THSG constantly enhanced the mRNA expression of SirT1 significantly from 1 h to 24 h (Figure 3(c)). HGFs were pretreated with resveratrol or THSG (1 and 25 μM) for 30 min and then treated with 1 μg/mL P. gingivalis LPS for another 6 h. The mRNA expression of SirT1 was significantly enhanced by 25 μM THSG but significantly reduced by 1 μM resveratrol when treated with P. gingivalis LPS (Figure 3(d)). The enhanced effect on the expression of SirT1 by THSG was more than that of resveratrol when cells were treated with P. gingivalis LPS.
Figure 3.
THSG attenuated P. gingivalis LPS-induced proinflammatory cytokines expression via inducing SirT1 expression in HGFs. HGFs were cultured in 6-well plate and were starved with serum-free DMEM/F12 medium for 24 h when the cell confluence reached 80%. (a) HGFs were treated with 1 μg/mL P. gingivalis LPS, (b) 100 μM resveratrol, and (c) 100 μM THSG for 24 h. (d) HGFs were pretreated with resveratrol and THSG (1 and 25 μM) for 30 min and then were treated with 1 μg/mL P. gingivalis LPS for 6 h. The mRNA expression of SirT1 was examined by quantitative PCR. (N = 3; ∗ p < 0.05; ∗∗ p < 0.01; ∗∗∗ p < 0.001 were compared with control group. # p < 0.05; ## p < 0.01; ### p < 0.001 were compared with LPS group. $$ p < 0.01; $$$ p < 0.001 were compared with 1 μM or 25 μM resveratrol group with LPS treatment.)
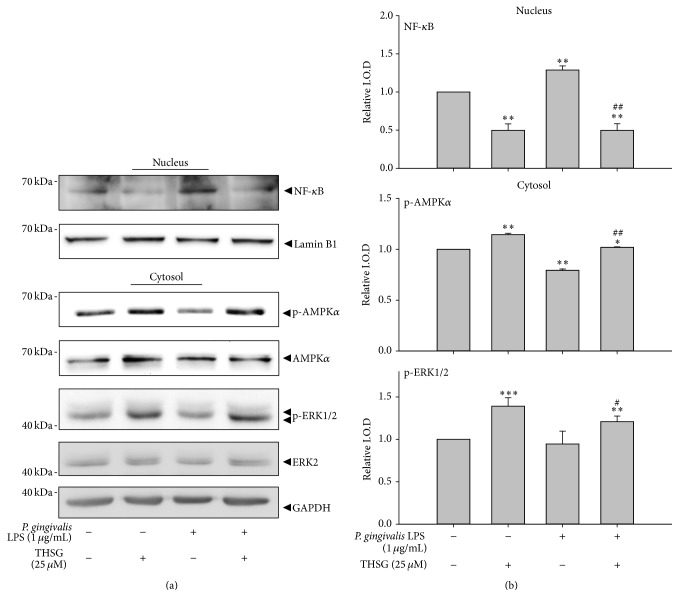
3.4. Signal Transduction Is Involved in THSG-Induced Anti-Inflammation
Signal transductions involved in the inhibitory effect of THSG on LPS-induced inflammation were also studied. HGFs were pretreated with resveratrol or THSG (25 μM) for 30 min and then treated with 1 μg/mL P. gingivalis LPS for another 3 h. The cytosolic and nuclear proteins of HGFs were extracted. In nuclear protein, the nuclear translocation of NF-κB was significantly augmented by LPS in HGFs. However, THSG did not only significantly reduce LPS-augmented nuclear translocation of NF-κB but also decrease that when THSG was presented alone in HGFs (Figures 4(a) and 4(b), upper panel). In cytosolic protein of HGFs, the activation of AMPK and ERK1/2 was significantly enhanced by THSG. On the other hand, treatment of LPS significantly reduced AMPK activation. Pretreatment of THSG significantly enhanced LPS-reduced AMPK activation and increased ERK1/2 activation even in the presence of LPS (Figures 4(a) and 4(b), middle and lower panel).
Figure 4.
THSG attenuated P. gingivalis LPS-induced proinflammatory cytokines expression via reducing NF-κB activation and activating AMPK and ERK1/2 in HGFs. HGFs were cultured in 10-cm dishes and starved for 24 h when the cell confluence reached 80%. HGFs were pretreated with 100 μM resveratrol and THSG for 30 min and then treated with 1 μg/mL P. gingivalis LPS for another 3 h. (a) The cytosolic and nuclear proteins of HGFs were extracted and Western blot was performed. (b) The relative intensity of nuclear translocation of NF-κB and activation of AMPK and ERK1/2 were evaluated. (N = 3; ∗ p < 0.05; ∗∗ p < 0.01; ∗∗∗ p < 0.001 were compared with control group. # p < 0.05; ## p < 0.01 were compared with LPS group.)
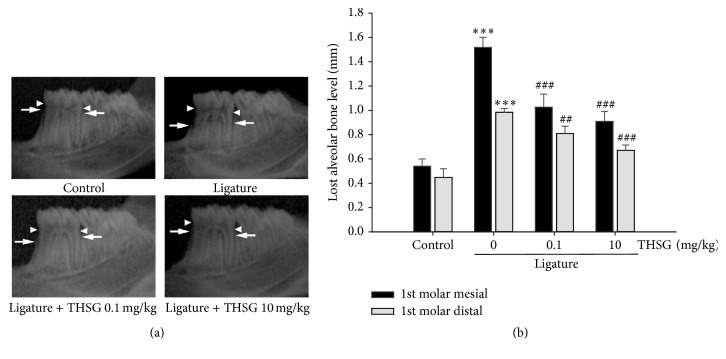
3.5. THSG Attenuates Ligature-Induced Experimental Periodontitis
Ligature-induced experimental periodontitis was performed in rats (8-week-old) at their first molar. Rats were fed with THSG (0.1 or 10 mg/kg/day dissolved in sterile water) or sterile water by gavage for 7 days. Radiographic films were taken and the lost alveolar bone level was evaluated (Figure 5(a)). The lost alveolar bone level was significantly increased in ligature group at first molar. However, administration of THSG significantly attenuated ligature-induced alveolar bone level lost (Figure 5(b)).
Figure 5.
THSG attenuated ligature-induced experimental periodontitis. Rats were performed ligature-induced experimental periodontitis at first molar and fed with THSG (0.1 or 10 mg/kg/day dissolved in sterile water) or sterile water by gavage for 7 days. (a) The alveolar bone crest (white arrow) and the cementoenamel junction (CEJ, white arrowhead) were shown on radiographic images of the mandible from these treatments. (b) The radiographic lost alveolar bone level was measured along the mesial/distal root surface and was defined as the distance from the CEJ to the most coronal level of the alveolar bone crest. (∗∗∗ p < 0.001 was compared with control group. ## p < 0.01; ### p < 0.001 were compared with 0 mg/kg THSG group.)
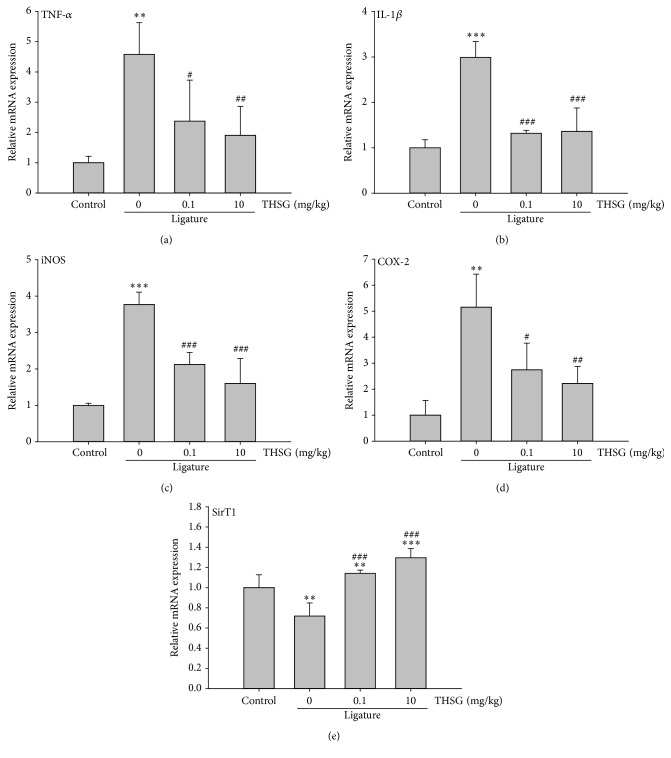
3.6. THSG Attenuates Proinflammatory Cytokines and Mediators mRNA Expression in the Gingival Tissues of Rats
The mRNA expression of proinflammatory cytokines and mediators, including TNF-α, IL-1β, iNOS, COX-2, and SirT1, in rat gingival tissues was evaluated by QPCR. THSG significantly attenuated ligature-induced TNF-α, IL-1β, iNOS, and COX-2 mRNA expressions, even in low concentration (0.1 mg/kg) (Figures 6(a)–6(d)). In addition, administration of THSG significantly enhanced the mRNA expression of SirT1 in rat gingival tissues (Figure 6(e)).
Figure 6.
THSG attenuated the mRNA expression of proinflammatory cytokines and mediators in the gingival tissues of rats. Rat gingival tissues were collected from the first molars of mandible and homogenized. Their RNAs were extracted and reverse transcripted to cDNA. QPCR was performed to examine the mRNA expression of TNF-α (a), IL-1β (b), iNOS (c), COX-2 (d), and SirT1 (e). (∗∗ p < 0.01; ∗∗∗ p < 0.001 were compared with control group. # p < 0.05; ## p < 0.01; ### p < 0.001 were compared with 0 mg/kg THSG group.)
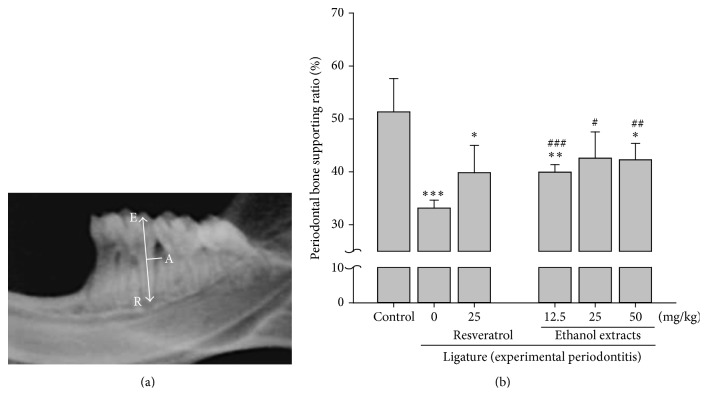
3.7. P. Multiflori Ethanol Extract and THSG Have Similar Effect on the Amelioration of Ligature-Induced Experimental Periodontitis
To evaluate whether the crude extracts of P. Multiflori would also have ameliorated effect on periodontitis, ligature-induced experimental periodontitis was performed in rats at their first molar and rats were fed with resveratrol (25 mg/kg/day), ethanol extracts (12.5, 25, or 50 mg/kg/day), or 50% ethanol by gavage for 7 days. According to our previous reports [29, 34], the periodontal bone-supporting ratio was measured. The radiographic image demonstrated the mandible from a ligatured rat and the measurements used to measure the periodontal bone-supporting ratio (Figure 7(a)). The periodontal bone-supporting ratio was significantly reduced in ligature group at first molar. Ethanol extracts of P. Multiflori significantly ameliorated ligature-induced periodontal bone-supporting ratio in all concentrations (Figure 7(b)). Damage of periodontal bone in rats receiving 25 mg/kg resveratrol was also reduced but there was no significant difference between resveratrol-treated group and control.
Figure 7.
P. Multiflori ethanol extracts attenuated ligature-induced experimental periodontitis. Rats were performed ligature-induced experimental periodontitis at first molar and then fed with resveratrol (25 mg/kg/day dissolved in 50% ethanol), ethanol extracts (12.5, 25, or 50 mg/kg/day dissolved in 50% ethanol), or 50% ethanol by gavage for 7 days. (a) The periodontal bone-supporting ratio was measured along the distal root surface and was labeled (based on measurements spanning the cusp tip, E, the deepest bony defect, A, and the root apex, R) as the A-R distance divided by the E-R distance × 100%. (b) The periodontal bone-supporting ratio was measured and shown. (∗ p < 0.05; ∗∗ p < 0.01; ∗∗∗ p < 0.001 were compared with control group. # p < 0.05; ## p < 0.01; ### p < 0.001 were compared with ligature group.)
4. Discussion
Among all herb medicines, resveratrol contributes the most in terms of health benefits due to its antioxidant properties. It has been described as a scavenger of superoxides, hydroxyl radicals, and peroxynitrites [12]. Furthermore, resveratrol has been shown to induce activation of antioxidant enzymes [36, 37] and activates the nuclear factor E2-related factor (Nrf2) antioxidant defense pathway [38]. Activated Nrf2 translocates to the nucleus and mediates the transcription of target genes such as heme oxygenase 1 (HO-1) and NAD(P)H:quinine oxidoreductase 1 (NQO-1) which are involved in cellular resistance to oxidative stress which confers protection against inflammation [39].
When human gingival fibroblasts were treated with different concentrations of resveratrol or THSG, resveratrol only stimulated cell proliferation at low concentration (Figure 1) but THSG stimulated cell proliferation at all concentrations (1 to 250 μM) examined (Figure 1). These results suggest that there is less cytotoxic of THSG than of resveratrol. Resveratrol suppressed P. gingivalis LPS-stimulated IκBα phosphorylation and nuclear translocation of the p65 subunit of NFκB in HMECs [21]. The concentration of IL-17 in the resveratrol group is lower than that in control group gingival tissue (p < 0.05); however, there is no difference in the IL-1β and IL-4 levels of the groups (p > 0.05) [40]. THSG activated AMPK and ERK1/2 as resveratrol (Figure 2). In addition, both resveratrol and THSG inhibited NFκB activation which is essential for the expression of inflammatory cytokines.
Resveratrol is also able to downregulate the cell adhesion molecules, ICAM-1 and VCAM-1, and significantly inhibits the P. gingivalis LPS-induced adhesion of leukocytes to endothelial cells and to the aortic endothelium [21]. In addition, resveratrol is able to reduce the inducible NO synthase (iNOS) expression [20] and further prevents NO production. This characteristic contributes to oxidative stress reduction to decrease the systemic levels of some proinflammatory cytokines and result in resveratrol's immunomodulatory effect [40, 41].
In addition, resveratrol can stimulate mitochondrial biogenesis by increasing the expression of NAD-dependent nuclear class III histone deacetylase, sirtuin 1 (SirT1) via the activated AMP-activated protein kinase (AMPK) [42, 43]. Our studies also indicate that THSG and resveratrol were able to activate SirT1 and showed a role in the inhibitory effect on LPS-induced expression of inflammatory cytokines (Figure 3(b)).
Both ethanol extract THSG and pure compound did inhibit ligature-induced periodontitis (Figures 5 and 7). On the other hand, the treatment of resveratrol did not attenuate ligature-induced periodontitis of rats (p = 0.054) in our studies (Figure 7). Studies conducted by Casati et al. using 10 mg/kg resveratrol per day for 19 days pretreatment indicated that there were higher bone loss values in ligated molars and unligated teeth in the control group than in the resveratrol-fed group (p < 0.05) [40]. Resveratrol added in drinking water has been shown to lead to relieve ligature placement associated alveolar bone resorption [41]. Further, systemic administration of resveratrol continuously also decreased ligature-induced periodontal breakdown [40]. Those studies and our results confirm the positive effects of resveratrol on ligature-induced periodontitis animal model. Studies have also found a powerful effect of resveratrol in preventing lipid peroxidation, specifically low density lipoprotein (LDL) [44]. Improved endothelial function and enhanced cardioprotective effects have been observed with resveratrol through its anti-inflammatory and antioxidant properties in various animal models of myocardial injury, hypertension, and type 2 diabetes [39, 45, 46].
In summary, THSG and resveratrol prevented the development of ligature-induced rat modeling periodontitis. Similar to resveratrol, THSG activated the expression of SirT1 during the process. Although both resveratrol and THSG activated ERK1/2 and AMPK and inhibited NFκB activation in human gingival fibroblasts, regenerating capacity of THSG is better than that of resveratrol. THSG and resveratrol both inhibited the expression of proinflammatory cytokines such as IL-1β and TNF-α, which are involved in pathogenesis of periodontitis. Yet again, the efficiency of THSG on the prevention of periodontitis is better than that of resveratrol. From all those evidences, it suggests that THSG either in crude extract or as pure compound may be used in the prevention and treatment of periodontitis in the future.
Acknowledgments
This work was supported in part by the grant from Taipei Medical University for featured team (TMU-T103-01) and the Department of Health (DOH) to Taipei Medical University-Center of Excellence for Cancer Research (TMU-CECR, MOHW103-TD-B-111-01) and grants from Ministry of Science and Technology, Taiwan (MOST-102-2311-B-038-00; MOST103-2320-B-038-050).
Competing Interests
The authors declare no competing interests.
References
- 1.Listgarten M. A. Pathogenesis of periodontitis. Journal of Clinical Periodontology. 1986;13(5):418–430. doi: 10.1111/j.1600-051x.1986.tb01485.x. [DOI] [PubMed] [Google Scholar]
- 2.Lindhe J., Nyman S. Clinical trials in periodontal therapy. Journal of Periodontal Research. 1987;22(3):217–221. doi: 10.1111/j.1600-0765.1987.tb01572.x. [DOI] [PubMed] [Google Scholar]
- 3.Listgarten M. A. Nature of periodontal diseases: pathogenic mechanisms. Journal of Periodontal Research. 1987;22(3):172–178. doi: 10.1111/j.1600-0765.1987.tb01560.x. [DOI] [PubMed] [Google Scholar]
- 4.Cochran D. L. Inflammation and bone loss in periodontal disease. Journal of Periodontology. 2008;79(8, supplement):1569–1576. doi: 10.1902/jop.2008.080233. [DOI] [PubMed] [Google Scholar]
- 5.Listgarten M. A. The role of dental plaque in gingivitis and periodontitis. Journal of Clinical Periodontology. 1988;15(8):485–487. doi: 10.1111/j.1600-051x.1988.tb01019.x. [DOI] [PubMed] [Google Scholar]
- 6.Zhou Q., Desta T., Fenton M., Graves D. T., Amar S. Cytokine profiling of macrophages exposed to Porphyromonas gingivalis, its lipopolysaccharide, or its FimA protein. Infection and Immunity. 2005;73(2):935–943. doi: 10.1128/iai.73.2.935-943.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dahiya P., Kamal R., Gupta R., Bhardwaj R., Chaudhary K., Kaur S. Reactive oxygen species in periodontitis. Journal of Indian Society of Periodontology. 2013;17(4):411–416. doi: 10.4103/0972-124X.118306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dias I. H. K., Chapple I. L. C., Milward M., et al. Sulforaphane restores cellular glutathione levels and reduces chronic periodontitis neutrophil hyperactivity in vitro. PLoS ONE. 2013;8(6) doi: 10.1371/journal.pone.0066407.e66407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Page R. C. The role of inflammatory mediators in the pathogenesis of periodontal disease. Journal of Periodontal Research. 1991;26(3, part 2):230–242. doi: 10.1111/j.1600-0765.1991.tb01649.x. [DOI] [PubMed] [Google Scholar]
- 10.Palaska I., Papathanasiou E., Theoharides T. C. Use of polyphenols in periodontal inflammation. European Journal of Pharmacology. 2013;720(1–3):77–83. doi: 10.1016/j.ejphar.2013.10.047. [DOI] [PubMed] [Google Scholar]
- 11.Chin Y.-T., Hsieh M.-T., Yang S.-H., et al. Anti-proliferative and gene expression actions of resveratrol in breast cancer cells in vitro. Oncotarget. 2014;5(24):12891–12907. doi: 10.18632/oncotarget.2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pervaiz S. Resveratrol: from grapevines to mammalian biology. The FASEB Journal. 2003;17(14):1975–1985. doi: 10.1096/fj.03-0168rev. [DOI] [PubMed] [Google Scholar]
- 13.Bhat K. P. L., Pezzuto J. M. Cancer chemopreventive activity of resveratrol. Annals of the New York Academy of Sciences. 2002;957:210–229. doi: 10.1111/j.1749-6632.2002.tb02918.x. [DOI] [PubMed] [Google Scholar]
- 14.Udenigwe C. C., Ramprasath V. R., Aluko R. E., Jones P. J. H. Potential of resveratrol in anticancer and anti-inflammatory therapy. Nutrition Reviews. 2008;66(8):445–454. doi: 10.1111/j.1753-4887.2008.00076.x. [DOI] [PubMed] [Google Scholar]
- 15.Knobloch J., Hag H., Jungck D., Urban K., Koch A. Resveratrol impairs the release of steroid-resistant cytokines from bacterial endotoxin-exposed alveolar macrophages in chronic obstructive pulmonary disease. Basic and Clinical Pharmacology and Toxicology. 2011;109(2):138–143. doi: 10.1111/j.1742-7843.2011.00707.x. [DOI] [PubMed] [Google Scholar]
- 16.Zhu X., Liu Q., Wang M., et al. Activation of Sirt1 by resveratrol inhibits TNF-α induced inflammation in fibroblasts. PloS ONE. 2011;6(11) doi: 10.1371/journal.pone.0027081.e27081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang F., Wang H., Wu Q., et al. Resveratrol protects cortical neurons against microglia-mediated neuroinflammation. Phytotherapy Research. 2013;27(3):344–349. doi: 10.1002/ptr.4734. [DOI] [PubMed] [Google Scholar]
- 18.Mbimba T., Awale P., Bhatia D., et al. Alteration of hepatic proinflammatory cytokines is involved in the resveratrol- mediated chemoprevention of chemically-induced hepatocarcinogenesis. Current Pharmaceutical Biotechnology. 2012;13(1):229–234. doi: 10.2174/138920112798868575. [DOI] [PubMed] [Google Scholar]
- 19.Yen G.-C., Chen Y.-C., Chang W.-T., Hsu C.-L. Effects of polyphenolic compounds on tumor necrosis factor-α (TNF-α)-induced changes of adipokines and oxidative stress in 3T3-L1 adipocytes. Journal of Agricultural and Food Chemistry. 2011;59(2):546–551. doi: 10.1021/jf1036992. [DOI] [PubMed] [Google Scholar]
- 20.Bi X. L., Yang J. Y., Dong Y. X., et al. Resveratrol inhibits nitric oxide and TNF-α production by lipopolysaccharide-activated microglia. International Immunopharmacology. 2005;5(1):185–193. doi: 10.1016/j.intimp.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 21.Park H.-J., Jeong S.-K., Kim S.-R., et al. Resveratrol inhibits Porphyromonas gingivalis lipopolysaccharide-induced endothelial adhesion molecule expression by suppressing NF-κB activation. Archives of Pharmacal Research. 2009;32(4):583–591. doi: 10.1007/s12272-009-1415-7. [DOI] [PubMed] [Google Scholar]
- 22.Tseng P.-C., Hou S.-M., Chen R.-J., et al. Resveratrol promotes osteogenesis of human mesenchymal stem cells by upregulating RUNX2 gene expression via the SIRT1/FOXO3A axis. Journal of Bone and Mineral Research. 2011;26(10):2552–2563. doi: 10.1002/jbmr.460. [DOI] [PubMed] [Google Scholar]
- 23.Büchter C., Zhao L., Havermann S., et al. TSG (2,3,5,4′-tetrahydroxystilbene-2-O-β-D-glucoside) from the Chinese herb Polygonum multiflorum increases life span and stress resistance of caenorhabditis elegans. Oxidative Medicine and Cellular Longevity. 2015;2015:12. doi: 10.1155/2015/124357.124357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang X., Zhao L., Han T., Chen S., Wang J. Protective effects of 2,3,5,4′-tetrahydroxystilbene-2-O-beta-d-glucoside, an active component of Polygonum multiflorum Thunb, on experimental colitis in mice. European Journal of Pharmacology. 2008;578(2-3):339–348. doi: 10.1016/j.ejphar.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 25.Liu Q.-L., Xiao J.-H., Ma R., Ban Y., Wang J.-L. Effect of 2,3,5,4′-tetrahydroxystilbene-2-O-beta-D-glucoside on lipoprotein oxidation and proliferation of coronary arterial smooth cells. Journal of Asian Natural Products Research. 2007;9(8):689–697. doi: 10.1080/17415990500209064. [DOI] [PubMed] [Google Scholar]
- 26.Zhang S.-H., Wang W.-Q., Wang J.-L. Protective effect of tetrahydroxystilbene glucoside on cardiotoxicity induced by doxorubicin in vitro and in vivo. Acta Pharmacologica Sinica. 2009;30(11):1479–1487. doi: 10.1038/aps.2009.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang T., Gu J., Wu P.-F., et al. Protection by tetrahydroxystilbene glucoside against cerebral ischemia: involvement of JNK, SIRT1, and NF-κB pathways and inhibition of intracellular ROS/RNS generation. Free Radical Biology and Medicine. 2009;47(3):229–240. doi: 10.1016/j.freeradbiomed.2009.02.027. [DOI] [PubMed] [Google Scholar]
- 28.Robinson M., Hart D., Pigott G. H. The effects of diet on the incidence of periodontitis in rats. Laboratory Animals. 1991;25(3):247–253. doi: 10.1258/002367791780808374. [DOI] [PubMed] [Google Scholar]
- 29.Cheng W.-C., Huang R.-Y., Chiang C.-Y., et al. Ameliorative effect of quercetin on the destruction caused by experimental periodontitis in rats. Journal of Periodontal Research. 2010;45(6):788–795. doi: 10.1111/j.1600-0765.2010.01301.x. [DOI] [PubMed] [Google Scholar]
- 30.Shoji K., Ohtsuka-Isoya M., Shimauchi H., Shinoda H. Effects of lactation on alveolar bone loss in experimental periodontitis. Journal of Periodontology. 2007;78(1):152–156. doi: 10.1902/jop.2007.060037. [DOI] [PubMed] [Google Scholar]
- 31.Ericsson I., Lindhe J. Lack of effect of trauma from occlusion on the recurrence of experimental periodontitis. Journal of Clinical Periodontology. 1977;4(2):115–127. doi: 10.1111/j.1600-051x.1977.tb01891.x. [DOI] [PubMed] [Google Scholar]
- 32.Chiu H.-C., Chiang C.-Y., Tu H.-P., Wikesjö U. M. E., Susin C., Fu E. Effects of bone morphogenetic protein-6 on periodontal wound healing/regeneration in supraalveolar periodontal defects in dogs. Journal of Clinical Periodontology. 2013;40(6):624–630. doi: 10.1111/jcpe.12075. [DOI] [PubMed] [Google Scholar]
- 33.Kuo P.-J., Tu H.-P., Chin Y.-T., et al. Cyclosporine-A inhibits MMP-2 and -9 activities in the presence of Porphyromonas gingivalis lipopolysaccharide: an experiment in human gingival fibroblast and U937 macrophage co-culture. Journal of Periodontal Research. 2012;47(4):431–438. doi: 10.1111/j.1600-0765.2011.01450.x. [DOI] [PubMed] [Google Scholar]
- 34.Chiang C.-Y., Tsai H.-T., Chang W.-L., et al. A Salvia miltiorrhiza ethanol extract ameliorates tissue destruction caused by experimental periodontitis in rats. Journal of Periodontal Research. 2016;51(1):133–139. doi: 10.1111/jre.12292. [DOI] [PubMed] [Google Scholar]
- 35.Kuroyanagi G., Otsuka T., Yamamoto N., Matsushima-Nishiwaki R., Kozawa O., Tokuda H. Resveratrol suppresses TGF-β-induced VEGF synthesis in osteoblasts: inhibition of the p44/p42 MAPKs and SAPK/JNK pathways. Experimental and Therapeutic Medicine. 2015;9(6):2303–2310. doi: 10.3892/etm.2015.2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Soufi F. G., Sheervalilou R., Vardiani M., Khalili M., Alipour M. R. Chronic resveratrol administration has beneficial effects in experimental model of type 2 diabetic rats. Endocrine Regulations. 2012;46(2):83–90. doi: 10.4149/endo_2012_02_83. [DOI] [PubMed] [Google Scholar]
- 37.Bhatt S. R., Lokhandwala M. F., Banday A. A. Resveratrol prevents endothelial nitric oxide synthase uncoupling and attenuates development of hypertension in spontaneously hypertensive rats. European Journal of Pharmacology. 2011;667(1–3):258–264. doi: 10.1016/j.ejphar.2011.05.026. [DOI] [PubMed] [Google Scholar]
- 38.Wang X., de Rivero Vaccari J. P., Wang H., et al. Activation of the nuclear factor E2-related factor 2/antioxidant response element pathway is neuroprotective after spinal cord injury. Journal of Neurotrauma. 2012;29(5):936–945. doi: 10.1089/neu.2011.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vang O., Ahmad N., Baile C. A., et al. What is new for an old molecule? Systematic review and recommendations on the use of resveratrol. PLoS ONE. 2011;6(6) doi: 10.1371/journal.pone.0019881.e19881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Casati M. Z., Algayer C., Da Cruz G. C., et al. Resveratrol decreases periodontal breakdown and modulates local levels of cytokines during periodontitis in rats. Journal of Periodontology. 2013;84(10):e58–e64. doi: 10.1902/jop.2013.120746. [DOI] [PubMed] [Google Scholar]
- 41.Tamaki N., Cristina Orihuela-Campos R., Inagaki Y., Fukui M., Nagata T., Ito H.-O. Resveratrol improves oxidative stress and prevents the progression of periodontitis via the activation of the Sirt1/AMPK and the Nrf2/antioxidant defense pathways in a rat periodontitis model. Free Radical Biology and Medicine. 2014;75:222–229. doi: 10.1016/j.freeradbiomed.2014.07.034. [DOI] [PubMed] [Google Scholar]
- 42.Howitz K. T., Bitterman K. J., Cohen H. Y., et al. Small molecule activators of sirtuins extend Saccharomyces cerevisiae lifespan. Nature. 2003;425(6954):191–196. doi: 10.1038/nature01960. [DOI] [PubMed] [Google Scholar]
- 43.Zong Y., Sun L., Liu B., et al. Resveratrol inhibits LPS-induced MAPKs activation via activation of the phosphatidylinositol 3-kinase pathway in murine RAW 264.7 macrophage cells. PLoS ONE. 2012;7(8, article e44107) doi: 10.1371/journal.pone.0044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brito P., Almeida L. M., Dinis T. C. P. The interaction of resveratrol with ferrylmyoglobin and peroxynitrite; protection against LDL oxidation. Free Radical Research. 2002;36(6):621–631. doi: 10.1080/10715760290029083. [DOI] [PubMed] [Google Scholar]
- 45.Raj P., Zieroth S., Netticadan T. An overview of the efficacy of resveratrol in the management of ischemic heart disease. Annals of the New York Academy of Sciences. 2015;1348(1):55–67. doi: 10.1111/nyas.12828. [DOI] [PubMed] [Google Scholar]
- 46.Natalin H. M., Garcia A. F. E., Ramalho L. N. Z., Restini C. B. A. Resveratrol improves vasoprotective effects of captopril on aortic remodeling and fibrosis triggered by renovascular hypertension. Cardiovascular Pathology. 2016;25(2):116–119. doi: 10.1016/j.carpath.2015.11.003. [DOI] [PubMed] [Google Scholar]