Abstract
Parental depression is a significant risk factor for adolescents’ engagement in risk taking. Yet the neural processes that mediate the link between parental depression and adolescents’ functioning remain unknown. Using a longitudinal functional magnetic resonance imaging design, we investigated how parental depression is associated with changes in adolescents’ neural reactivity to rewards during a risk-taking task, and how such changes in neural reactivity are associated with changes in risk-taking behavior. Greater parental depressive symptoms were associated with increases in their adolescent child’s risk taking and self-reported externalizing behavior over time. At the neural level, adolescents of parents with greater depressive symptoms showed longitudinal increases in the ventral striatum and dorsolateral prefrontal cortex to rewards during risk taking. Longitudinal increases in adolescents’ ventral striatum activation mediates the link between greater parental depression and increases in adolescents’ risk taking and externalizing behavior. These findings provide novel evidence that parental depression may contribute to changes in adolescents’ neural reactivity to rewards over time, which is associated with greater increases in their risk taking and externalizing behavior.
Keywords: adolescence, parental depression, risk taking, longitudinal, fMRI
Introduction
Parental depression is a major risk factor for children’s successful development. For example, adolescents of depressed parents are at heightened risk for engaging in a variety of externalizing behaviors, such as aggression, substance use and unprotected sexual activity (Downey and Coyne, 1990; Weissman et al., 2006; Campbell et al., 2009; Allen et al., 2010; Lamis et al., 2012; Pugh and Farrell, 2012). However, we know little about the neural processes through which parental depression contributes to their child’s risk-taking behavior. Although a few neuroimaging studies have examined how parental depression is concurrently associated with adolescents’ neural reactivity to rewards (Monk et al., 2008; Gotlib et al., 2010; Olino et al., 2014; Sharp et al., 2014), this research has been limited in four important ways: prior research has not (i) examined neural reactivity in a risk-taking context, (ii) examined how neural reactivity relates to adolescents’ risk-taking behavior in real life, (iii) used longitudinal neuroimaging techniques to examine how parental depression contributes to changes in adolescents’ neural reactivity or (iv) moved beyond focusing on parental depression in clinical samples and examined these issues in community samples.
In the absence of longitudinal neuroimaging studies as well as tasks that directly assess reward sensitivity during risk taking, the link between parental depression, adolescent neural sensitivity to rewards, and adolescent risk taking is still unclear. Longitudinal approaches enable us to examine how parental depression affects trajectories of adolescents’ neural reactivity over time, which can provide more clear evidence on patterns of change during adolescence. Although attention has been devoted to how parental depression during early childhood contributes to adolescents’ neural reactivity (Morgan et al., 2014), parental depression during adolescence may continue to play an important role in affecting adolescents’ brain development over time. Given that adolescence is a developmental period marked by steep increases in risk-taking behavior coupled with significant neural changes (Dahl, 2004; Casey et al., 2008), it is essential to unpack how parental depression during adolescence is associated with adolescent children’s risk-taking behavior via changes in neural sensitivity to rewards.
Adolescence is a time of dramatic brain, behavioral and psychological changes, contributing to an increase in risk taking. Significant attention has been paid to understanding the neural processes underlying adolescent risk taking. Two key brain systems—affective and cognitive control systems—have been consistently associated with adolescent risk taking. First, as a key region in the human affective system, the ventral striatum (VS) is involved in the anticipation and receipt of rewards (Delgado et al., 2000; Knutson et al., 2000). Moreover, the VS shows greater reactivity in adolescents than children or adults when receiving rewards (Ernst et al., 2005; Galvan et al., 2006), with greater VS activation linked to increased risk-taking behavior in real life (e.g. Braams et al., 2015; Qu et al., 2015). In addition, the lateral prefrontal cortex (PFC), a key brain region in the cognitive control system (Miller and Cohen, 2001), is involved in adolescent risk taking (Fecteau et al., 2007; Schonberg et al., 2012). Given that adolescence is a sensitive period for sociocultural processing (Blakemore and Mills, 2014) and a time when the brain is highly flexible and sensitive to environmental input (Crone and Dahl, 2012), greater parent depression may elicit maladaptive changes in adolescents’ neural development, both in terms of the affective and cognitive control systems, resulting in increased risk taking and externalizing behaviors.
Developmental research has consistently shown that parents with depressive symptoms tend to have lower positive affect, use less positive parenting behavior and expose their children to more negative parent–child interactions (Goodman and Gotlib, 1999; Lovejoy et al., 2000; Pugh and Farrell, 2012). Such negative family environments resulting from parental depression are predictive of increases in children’s risk taking and externalizing problems during adolescence (e.g. Foster et al., 2008; Cummings et al., 2013). Given that recent empirical evidence has consistently found that increases in VS activation are associated with increases in risk taking and sensation seeking (Braams et al., 2015; Qu et al., 2015), parental depression may be associated with longitudinal increases in adolescents’ neural reactivity to rewards over time. Moreover, recent research suggests that parental depression impairs adolescents’ cognitive control (Clasen et al., 2014). Similarly, negative family contexts during adolescence, such as high family conflict and low family cohesion, contribute to longitudinal increases in adolescents’ PFC activity, which are associated with longitudinal increases in risk-taking behavior (McCormick et al., 2016). Therefore, adolescents of depressed parents may exhibit less effective cognitive control via increases in PFC activity over time. Together, parental depression may contribute to adolescents’ risk taking behavior via changes in the affective and cognitive control system.
In this study, we sought to examine how parental depression is associated with changes in adolescents’ neural sensitivity to rewards as well as their risk taking and externalizing behavior over time. To this end, we used a longitudinal design in which adolescents completed a functional magnetic resonance imaging (fMRI) scan twice, approximately 1.5 years apart. Recent evidence suggests there is significant variability of risk taking and neural activation among adolescents over time (e.g. Steinberg, 2010; van den Bulk et al., 2013; Braams et al., 2015). For example, recent research examining changes in adolescents’ neural reactivity has revealed substantial variability in individual changes of adolescent brain activation, both over a short period of time (e.g. 3-month interval, van den Bulk et al., 2013) and over a longer period of time (e.g. 2-year interval, Braams et al., 2015). These studies provide strong evidence that adolescence is characterized by significant changes and variability in terms of their neural activation over time. Thus, we expected to detect important individual differences in neural and behavioral changes across 1.5 years. We first tested whether parental depression is related to increases in adolescent’s risk-taking behavior. Second, we investigated whether parental depression is associated with longitudinal changes in adolescents’ neural reactivity to rewards during risk-taking and whether changes in neural activation are associated with increases in adolescents’ risk taking and externalizing behavior. To this end, we conducted mediation analyses to test whether changes in neural activation explain, in part, why parental depression is associated with increased risk taking and externalizing behavior.
Methods
Participants
Participants were a community sample of 23 adolescents (mean age at T1 = 15.78 years, range = 15.34–17.13 years, s.d. = 0.60, 15 girls) and their parent who self-identified as the adolescents’ primary caregiver (defined as the parent who spent the most time with and knew the adolescent the best; caregiver mean age = 42.26 years, s.d. = 5.43; 17 mothers and 6 fathers).1 Most participants were from low-SES families with the majority of fathers (87%) and mothers (91%) receiving a high school diploma or less. The average annual family income was $26 000, ranging from $10 000 to $53 200. The primary caregiver of the participating adolescents reported on their depressive symptoms at T1. At T1, adolescents completed a risk-taking task during an fMRI scan. Approximately 1.5 years following the first scan (mean age at T2 = 17.13 years, range = 16.43–18.42 years, s.d. = 0.70), adolescent participants completed a second fMRI scan. At both time points, adolescents completed self-report measures of their externalizing behaviors. Adolescents were not diagnosed with depressive disorder at either T1 or T2. Participants completed written consent and assent in accordance with UCLA’s Institutional Review Board.
Measures
Depression. Parents’ depressive symptoms were assessed using the Center for Epidemiologic Studies Depression (CES-D) Scale at T1 (Radloff, 1977). The CES-D Scale is a 20-item self-report scale designed to measure depressive symptoms in the general population. Parents reported on how often they had depressive feelings during the last week on a 4-point scale (0 = ‘Rarely or none of the time’, 3 = ‘Most or all of the time’). Their responses were summed, with higher scores indicating greater depressive symptoms (α = 0.82). The mean score in our sample for parents was 14.51, ranging from 3 to 29, indicating a wide range of depressive symptoms. Following established cut-offs of this measure, scores >16 indicate moderate levels of depression and scores >27 indicate high levels of depression (Radloff, 1977; Zich et al., 1990). In our sample, 15 parents had scores lower than 16, 6 parents had scores greater than 16 and less than 27, and 2 parents had scores greater than 27. Parental report on the CES-D scale was only collected at T1, but not at T2.
In addition, adolescents completed the CES-D at T1 (α = 0.91), and we controlled for adolescents’ depressive symptoms in all analyses in order to examine the independent and unique role that parental depression plays on adolescents’ neural trajectories. For adolescents, the mean score of depression was 20.18, ranging from 3 to 45. The mean score was consistent with prior studies on adolescents in community samples (Garrison et al., 1991). In our sample, 52.2% of adolescents had scores lower than 16, 26.1% of adolescents had scores greater than 16 and less than 27, and 21.7% of adolescents had scores greater than 27. Adolescent and parent depression were not correlated (r = 0.05, P = 0.83). Importantly, the behavioral and neuroimaging results remained the same without controlling for adolescents’ depressive symptoms.
Adolescents’ self-reported externalizing behavior.At both T1 and T2, adolescents reported on their externalizing behavior using the externalizing subscale from the Youth Self Report (YSR) of the Child Behavior Checklist (Achenbach, 1991). The YSR is a well-validated measure for adolescents’ problem behaviors. The externalizing subscale captures a wide range of adolescent problem behavior, such as aggression and rule-breaking behavior (32 items; e.g. ‘I drink alcohol without my parents’ approval’ and ‘I break rules at home, school or elsewhere’). Adolescents rated how true (0 = ‘not true of me’, 2 = ‘true or often true of me’) each statement was (α = 0.73 at T1 and 0.77 at T2). To examine longitudinal changes in externalizing behavior, we computed difference scores (i.e. T2 minus T1 scores), which ranged from −6 (reflecting declines in externalizing behavior) to 5.5 (reflecting increases in externalizing behavior).
Adolescents’ risk-taking behavior. At both T1 and T2, adolescents completed the Balloon Analogue Risk Task (BART) during an fMRI scan. The BART is a well-validated task used in neuroimaging studies to examine adolescents’ neural responses to risk taking (Chiu et al., 2012; Galvan et al., 2013; Telzer et al., 2014). Importantly, behavioral performance on the BART is associated with actual risk behaviors such as adolescent smoking, addiction and drug use (Lejuez et al., 2003; Aklin et al., 2005; Lejuez et al., 2007). Behavioral performance on the BART, as described below, was used as the index of adolescent risk-taking behavior at each time point.
fMRI task
To examine neural sensitivity to rewards during risk taking, adolescents underwent an fMRI scan while completing the BART at both T1 and T2. The BART is completed during one 9-min self-paced run. At the beginning of each trial, adolescents are presented with a virtual red-colored balloon. By pressing one of two buttons, adolescents can choose either a risky option (i.e. pump the balloon), which results in bigger monetary rewards but a greater probability of getting no rewards (i.e. explosion of the balloon), or a safe option (cash out current rewards). For each successful pump without explosion, adolescents receive 25 cents. However, if the balloon explodes before cashing out, adolescents receive no payoff for that trial. As number of pumps increases during a trial, explosion probability increases exponentially. The explosion point of each balloon was drawn from a uniform distribution from 1 to 12 pumps. After each pump, the balloon image disappeared for a jittered interval of 1–3 s before the outcome, either a larger balloon or an exploded one. There was an interstimulus interval of variable (jittered) length ranging from 1 to 12 s (M = 4 s) after the end of each balloon (i.e. after explosion or cash-out). The payoff for each trial is accumulated, and participants receive the total payoff at the end of the task. Adolescents completed 24 balloons on average (s.d. = 3.89), ranging from 14 to 40 balloons. They cashed out 17 balloons on average (s.d. = 4.02), ranging from 7 to 33 balloons.
To assess risk-taking behavior on the BART, following previous studies (Lejuez et al., 2003), we examined the number of pumps before cash-outs (excluding balloons that exploded), with a greater number of pumps before cash-outs indicating greater risk-taking behavior. As reported previously (Qu et al., 2015a), the change in behavioral performance on the BART (i.e. change in average number of pumps from T1 to T2) was correlated with the change in self-reported externalizing behavior (i.e. change in YSR from T1 to T2; r = 0.44, P < 0.05), highlighting the ecological validity of the BART.
fMRI data acquisition
Imaging data were collected using a 3.0 Tesla Siemens Trio MRI scanner. The BART consisted of T2*-weighted echoplanar images (EPI) (slice thickness, 4 mm; 34 slices; TR = 2000 ms; TE = 30 ms; flip angle = 90°; matrix = 64 × 64; FOV = 200 mm; voxel size 3 × 3 × 4 mm3). A T2*weighted, matched-bandwidth (MBW), high-resolution, anatomical scan and magnetization-prepared rapid-acquisition gradient echo (MPRAGE) scan were acquired for registration purposes (TR: 2.3; TE: 2.1; FOV: 256; matrix: 192 × 192; sagittal plane; slice thickness: 1 mm; 160 slices). The orientation for the MBW and EPI scans was oblique axial to maximize brain coverage.
fMRI data Preprocessing and Analysis
Analyses were performed using Statistical Parametric Mapping (SPM8; Wellcome Department of Cognitive Neurology, Institute of Neurology, London, UK). Preprocessing for each participant’s images included spatial realignment to correct for head motion (no participant exceeded 2 mm of maximum image-to-image motion in any direction). For each participant, the realigned functional data at T1 and T2 were coregistered to the corresponding T1 and T2 high resolution MPRAGE, which was then segmented into cerebrospinal fluid, gray matter and white matter. The normalization transformation matrix from the segmentation step was then applied to the functional and T2 structural images, thus transforming them into standard stereotactic space as defined by the Montreal Neurological Institute and the International Consortium for Brain Mapping. The normalized functional data were smoothed using an 8 mm Gaussian kernel, full-width-at-half maximum, to increase the signal-to-noise ratio.
Statistical analyses were performed using the general linear model in SPM8. Each trial was convolved with the canonical hemodynamic response function. High-pass temporal filtering with a cut-off of 128 s was applied to remove low-frequency drift in the time series. Serial autocorrelations were estimated with a restricted maximum likelihood algorithm with an autoregressive model order of 1. In each person’s first level model, multiple regressors were applied to separate different events: risk-taking (i.e. pumps for red balloons), receipt of rewards (i.e. cash outs) and receipt of negative outcomes (i.e. explosions) for T1 and T2. The duration of the events was the response time (time taken to press a button). Following prior studies, we only analysed pumps on balloons that did not explode (i.e. pumps on each balloon prior to cash-out), because pumps on the explosion trials were necessarily constrained (Lejuez et al., 2002). For instance, the balloon may pop after just one or two pumps, but the adolescent may have continued to eight or nine pumps. By including the pumps from the exploded trials, we would likely be bringing down their mean scores. Thus, we used the pumps on the cash-out trials as the index of risk taking, because that is when adolescents actively end their risk-taking behavior during the trials. Null events, consisting of the jittered intertrial intervals, were not explicitly modeled and therefore constituted an implicit baseline.
Given that our key interest was adolescents’ neural reactivity to rewards during risk taking, we focus our analyses on cash-out trials (i.e. adolescents’ decision to keep monetary rewards). Following previous studies, cash outs were modeled with a parametric regressor to test the linear relationship between brain activation and the magnitude of reward. The parametric regressor was the total number of pumps prior to cash out, with pump number mean centered within the individual in order to avoid confounding the parameter estimates. Thus, brain activation reflects adolescents’ neural reactivity when they receive increasing monetary rewards. To examine longitudinal changes in such neural reactivity, contrasts between T1 and T2 were computed at the individual level (e.g. T2 cash out –T1 cash out). These individual contrast images were then used in all group-level analyses. To test how parental depression is associated with changes in neural reactivity, we conducted whole-brain regression analyses, in which we examined how parental depression at T1 is related to the difference in neural activity to rewards (i.e. cash-outs) from T1 to T2. Thus, findings from these whole-brain regressions reflect the regions of the brain showing significant association between parental depression at T1 and changes in neural activity during T2–T1.
To correct for multiple comparisons, we conducted a Monte Carlo simulation implemented using 3dClustSim in the software package AFNI (http://afni.nimh.nih.gov/afni/). We used our group-level brain mask combined with the gray mask in SPM, therefore representing neural coverage in our sample that corresponded to gray matter. Results of the simulation indicated a voxel-wise threshold of P < 0.005 combined with a minimum cluster size of 34 voxels. This joint voxelwise and cluster-size threshold corresponds to a false-positive discovery rate of 5% across gray matter. We used the MarsBaR toolbox to extract parameter estimates for significant clusters in the group-level analyses. Parameter estimates of signal intensity were extracted from the entire cluster of activation. For visualization, statistical maps of all analyses were projected onto a T2 template.
Results
Descriptive statistics of all variables at T1 and T2
We first investigated adolescent risk taking and self-reported externalizing behavior at each time point. The mean and standard deviation for adolescent risk taking and externalizing behavior are presented in Table 1. We examined mean difference in adolescent risk taking and externalizing behavior from T1 to T2 using repeated-measures t-test. The correlation between all study variables are shown in Table 2.
Table 1.
Mean and standard deviation for adolescent risk taking and externalizing behavior at T1 and T2
| T1 mean (s.d.) | T2 mean (s.d.) | Difference between T1 and T2 | |
|---|---|---|---|
| Mean pumps on BART | 3.44 (0.97) | 3.15 (0.90) | t = 1.76, p = 0.09 |
| Self-reported externalizing behavior | 12.39 (5.94) | 12.52 (7.42) | t = 0.12, p = 0.91 |
Table 2.
Correlations between all variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Parental depression at T1 | ||||||||||
| 2. | Teen’s depression at T1 | 0.05 | |||||||||
| 3. | Risk taking at T1 | −0.26 | 0.01 | ||||||||
| 4. | Risk taking at T2 | 0.23 | −0.03 | 0.64*** | |||||||
| 5. | Risk taking T2-T1 | 0.58** | −0.04 | −0.50* | 0.35 | ||||||
| 6. | Externalizing behavior at T1 | −0.34 | 0.12 | −0.03 | 0.22 | 0.28 | |||||
| 7. | Externalizing behavior at T2 | 0.10 | 0.30 | −0.25 | 0.22 | 0.55** | 0.70*** | ||||
| 8. | Externalizing behavior T2-T1 | 0.51* | 0.29 | −0.31 | 0.07 | 0.46* | −0.14 | 0.61** | |||
| 9. | Parents’ education | 0.03 | −0.44* | 0.45* | 0.34 | −0.14 | −0.54** | −0.50* | −0.08 | ||
| 10. | Age at T1 | 0.16 | 0.46* | 0.21 | 0.34 | 0.13 | 0.00 | 0.20 | 0.28 | −0.13 | |
| 11. | Years between T1 and T2 | 0.35 | 0.00 | −0.13 | −0.04 | 0.11 | −0.17 | 0.03 | 0.24 | −0.16 | −0.16 |
Note. Risk taking was measured as number of pumps on the BART task. The values are Pearson’s correlation coefficients.
*P < 0.05;
**P < 0.01;
***P < 0.001.
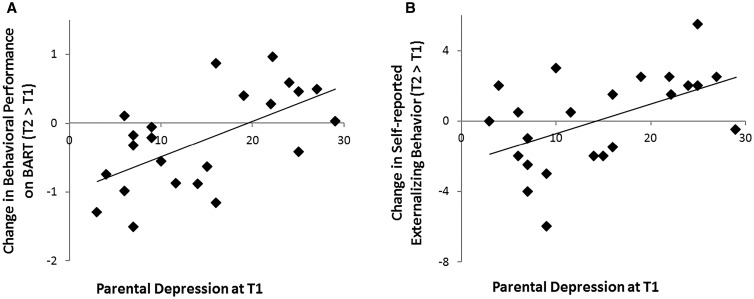
Parental depression and change in adolescents’ risk taking and externalizing behavior
Our first set of analyses tested whether parental depression is associated with increases in adolescents’ risk taking and externalizing behavior over time. Consistent with previous research, our results confirmed that parents with greater depressive symptoms had adolescents who showed longitudinal increases in risk-taking behavior over time as demonstrated by riskier behavior on the BART (i.e. increases in the average number of pumps across time; r = 0.58, P < 0.01), as well as increased self-reported externalizing behavior (r = 0.51, P = 0.01; Figure 1A and B). These associations remain significant after controlling for risk taking and externalizing behavior at T1, suggesting that parents’ depression is associated with changes in adolescents’ risk taking, above and beyond adolescents’ baseline levels of risk taking. Moreover, controlling for socioeconomic status (i.e. parents’ education), parental depression was still associated with increases in adolescent risk taking (r = 0.63, P < 0.01) and externalizing behavior (r = 0.50, P = 0.02). As shown in Table 2, teens’ depressive symptoms at T1 were not associated with changes in either performance on the BART or self-reported externalizing behavior.
Fig. 1.
Parents with greater depressive symptoms had adolescents who showed (A) riskier behavior on the BART and (B) increased self-reported externalizing behavior over time.
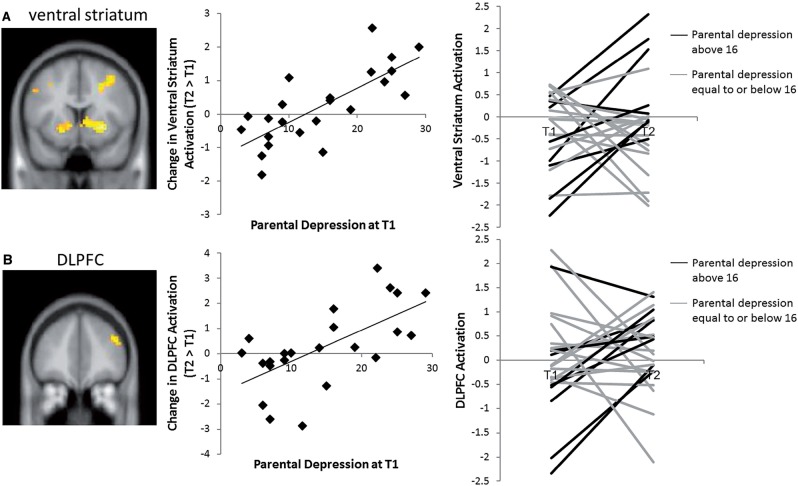
Parental depression and change in adolescents’ neural reactivity to rewards
Next, we conducted whole-brain regression analysis to examine how parental depression was associated with adolescents’ neural sensitivity to rewards at T1. Parental depression was not associated with any neural region in the VS or PFC, and only associated with right insula (x = 27, y = 23, z = −2, t = 4.04). We next investigated how parental depression was associated with changes in adolescents’ neural sensitivity to rewards. To this end, we ran whole-brain regression analyses to test the association between parental depression at T1 and changes in adolescents’ neural reactivity to rewards (T2-T1) over time. As shown in Figure 2A, greater parental depressive symptoms at T1 were associated with adolescents’ longitudinal increases in VS activation to rewards over time (Table 3). To test whether this association holds after accounting for baseline VS activation, we extracted parameter estimates of signal intensity from the same VS region at T1. After controlling for T1 VS activation, greater parental depression at T1 was still associated with greater increases in VS activation over time (r = 0.72, P < 0.001), suggesting that parents’ depression is associated with increases in adolescents’ VS activation, above and beyond adolescents’ baseline levels of VS activation. For descriptive purposes, we extracted VS activation at T1 and T2 and plotted each adolescent’s neural trajectory, separating the data by those with high parental depression (i.e. scores > 16 on the CESD) vs low parental depression (scores ≤ 16). As shown in the right panel of Figure 2A, adolescents of parents with high depression tended to show increases in VS activation to rewards over time, whereas adolescents of parents with low depression tended to show the opposite pattern.
Fig. 2.
Parents with greater depressive symptoms had adolescents who showed longitudinal increases in (A) the VS and (B) the DLPFC.
Table 3.
Whole brain regression between Parental Depression at T1 and Longitudinal Change in Brain Activity
| Anatomical Region | BA | x | y | z | t | k |
|---|---|---|---|---|---|---|
| Right DLPFC | 9/46 | 39 | 38 | 31 | 4.26 | 97 |
| Left VS | −9 | 11 | −2 | 3.29 | 46 | |
| Right VS | 6 | 5 | −2 | 4.40 | 58 | |
| ACC | 32 | 12 | 23 | 43 | 4.18 | 81 |
| Precuneus | 7 | 15 | −70 | 40 | 4.62 | 123 |
| Cuneus | 7 | 18 | −70 | 28 | 3.91 | 92 |
| Calcarine | 31 | 21 | −73 | 16 | 4.22 | 74 |
| Inferior parietal lobule | 40 | 57 | −46 | 43 | 4.21 | 154 |
Note. BA refers to putative Brodmann’s areas. x, y and z refer to MNI coordinates; t refers to the t-score at those coordinates (local maxima); k refers to the number of voxels in each significant cluster. DLPFC, dorsolateral prefrontal cortex; VS, ventral striatum; ACC, anterior cingulate cortex.
In addition to the VS, parents with greater depressive symptoms at T1 had children who showed longitudinal increases in the dorsolateral prefrontal cortex (DLPFC) to rewards over time (Figure 2B and Table 3). As shown in the right panel of the Figure 2B, adolescents of parents with high depression tended to show increases in DLPFC activation over time, whereas adolescents of parents with low depression tended to show the opposite pattern. For additional regions which correlated with parental depressive symptoms, see Table 3.
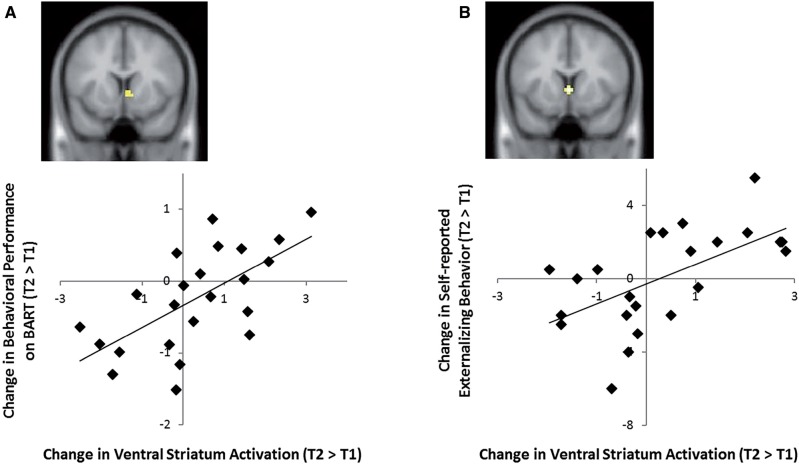
Fig. 3.
Adolescents who showed greater longitudinal increase in the VS also showed (A) riskier behavior on the BART and (B) increased self-reported externalizing behavior over time.
Finally, for exploratory purposes, we ran whole-brain regression analyses with adolescent depression. Adolescent depression at T1 was not associated with neural changes from T1 to T2 in any brain region. In addition, all our results remain the same after taking into account adolescents’ age at T1. For example, parental depression at T1 is still associated with changes in risk-taking behavior (performance on at the BART, r = 0.56, P = 0.01) and self-reported externalizing problems (r = 0.48, P = 0.03), as well as longitudinal changes in the VS (r = 0.73, P < 0.001) and DLPFC (r = 0.61, P = 0.003).
Change in adolescents’ neural reactivity is associated with change in adolescents’ risk taking
Next, we examined how changes in neural reactivity were related to changes in adolescents’ risk-taking behavior and externalizing symptoms. We conducted whole-brain regression analyses to test the association between risk taking (i.e. changes in behavioral performance on the BART) and changes in externalizing symptoms and changes in adolescents’ neural reactivity to rewards (T2–T1) over time. In separate whole-brain regression analyses, we found that adolescents who showed greater increases in risk taking on the BART (Figure 3A) and greater increases in externalizing behavior (Figure 3B) also showed greater increases in VS activation (x = 6, y = 8, z = −2, t = 3.21, and x = 0, y = 8, z = −1, t = 3.40, respectively). No other brain regions were associated with changes in adolescent risk taking and externalizing behavior. The results remained the same after controlling for adolescents’ age at T1.
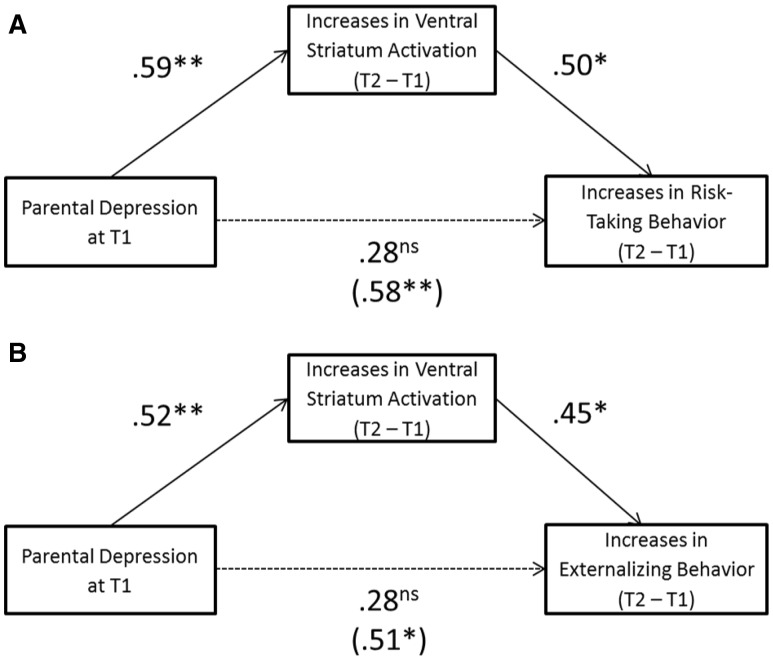
Change in adolescents’ neural reactivity mediates the link between parental depression and change in adolescents’ risk taking
Finally, we tested the relationships among parental depression, changes in VS activation, and changes in risk taking in the context of mediation using bias-corrected bootstrapping resampling techniques (Preacher and Hayes, 2008). To this end, we took the shared VS cluster that showed an association with both parental depression and changes in risk taking. As shown in Figure 4A, greater parental depression at T1 was associated with longitudinal increases in adolescents’ risk taking over time, which was mediated by increases in VS activation to rewards over time. Based on 1000 bootstrap resamples, the indirect path from greater parental depression to increases in VS activation to increases in adolescent risk-taking behavior was significant (indirect effect = 0.29, 95% CI: [0.05, 0.64]). The link between parental depression at T1 and changes in adolescent risk taking was no longer significant after taking into account changes in adolescent VS activation, with a 52% reduction in the total effect. Analyses on changes in externalizing problems yielded identical findings (indirect effect = 0.24, 95% CI: [0.07, 0.56]; Figure 4B).
Fig. 4.
Greater parental depression at T1 was associated with longitudinal increases in (A) risk taking and (B) externalizing behavior, which were mediated by increases in VS activation.
As we demonstrated earlier, adolescents who showed greater increases in risk taking on the BART (Figure 3A) and greater increases in externalizing behavior (Figure 3B) only showed greater increases in VS activation. No other brain regions were associated with changes in adolescent risk taking and externalizing behavior. Therefore, it is not possible for other neural regions (e.g. DLPFC, precuneus, or inferior parietal lobule) to serve as a mediator in the link between parental depression and increases in risk taking or externalizing behavior, since these regions were not significantly associated in path b (i.e. brain → risk taking).
Discussion
In this study, we used a longitudinal fMRI approach to investigate how parental depression is associated with adolescents’ risk taking and externalizing behavior via changes in neural activation. Consistent with theoretical and empirical work (Downey and Coyne, 1990; Weissman et al., 2006; Campbell et al., 2009; Allen et al., 2010; Lamis et al., 2012; Pugh and Farrell, 2012), parents with greater depressive symptoms had adolescents who showed longitudinal increases in risk-taking behavior and self-reported externalizing behavior over time. Our findings provide the first longitudinal fMRI data to demonstrate that parental depressive symptoms are associated with increased reward-related activation and PFC activation in their adolescent children, suggesting that adolescents become increasingly sensitive to rewards during risk taking. Such changes in their neural processing contributed to increases in their risk taking and externalizing behavior.
We found that greater parental depressive symptoms were associated with increased VS activation over time, with such activation predicting increases in risk-taking behavior. These findings are consistent with prior studies showing that heightened VS activation in the context of risk taking is associated with adolescent maladjustment, such as greater risk taking and depression (Galvan et al., 2007; Telzer et al., 2014). Due to low positive affect and social rewards at home (Goodman and Gotlib, 1999; Foster et al., 2008), adolescents of parents with greater depressive symptoms may seek out greater rewards in their external environment. Given the key role of the VS in sensitivity to rewards (Delgado et al., 2000; Knutson et al., 2000), our findings highlight that adolescents of depressed parents may show an increased orientation towards rewards in their environment, which ultimately contributes to more risk-taking behavior in real life.
Despite evidence suggesting that parental depression affects adolescents’ sensitivity to rewards concurrently (Monk et al., 2008; Gotlib et al., 2010; Olino et al., 2014; Sharp et al., 2014), prior neuroimaging research has not examined reward sensitivity in a risk-taking context or tested longitudinal trajectories of neural reactivity, making it unclear how parental depression leads to increases specifically in relation to adolescent risk taking. By using a longitudinal neuroimaging approach, we focused on how parental depression was related to changes in adolescents’ neural reactivity over time. Importantly, we found that parental depression was associated with longitudinal increases in adolescents’ VS activation to rewards, above and beyond baseline levels of VS reactivity, suggesting that the negative impact of parental depression on adolescent brain development may occur gradually during adolescence. Therefore, our findings are not driven by cross-sectional associations and underscore the value of using a longitudinal approach. Our findings highlight the detrimental role of parental depression over the course of adolescent development, underscoring how parent depression contributes to the developmental trajectory by which their adolescent child’s neural activation changed. Bjork and Pardini (2015) suggest that risk-taking behavior more likely occurs in adolescents with a history of risk-related individual differences. Therefore, adolescents likely show greater increases in risk taking and externalizing behavior due to a history of problem behavior and exposure to greater risk factors. Consistent with this argument (Bjork and Pardini, 2015), we found that adolescents who are exposed to greater parental depression, a familial risk factor, show greater increases in problem behavior during adolescence.
In addition to the VS, we also found that greater parental depressive symptoms were associated with increased activation in the DLPFC. The DLPFC is a relatively late developing brain region and is involved in cognitive regulation (Gogtay et al., 2004). Prior research has shown that the DLPFC is associated with executive functioning, impulse control, goal-directed inhibition and risk-taking behavior (Fecteau et al., 2007; Knoch and Fehr, 2007; Steinbeis et al., 2012). Moreover, our findings are consistent with prior research showing that adolescents in negative family contexts, such as high conflict and low cohesion, show longitudinal increases in PFC activation during cognitive control (McCormick et al., 2016). Thus, parental depression may contribute to poor cognitive control over time, coupled with heightened reward sensitivity, thereby increases adolescents’ likelihood to take risks.
Our participants were recruited form a low-income community sample. By using a community sample rather than a clinical sample, the current study was able to examine variability in parental depression ranging from very low levels to clinically relevant levels. While prior research has examined clinically depressed parents (Monk et al., 2008; Gotlib et al., 2010; Olino et al., 2014; Sharp et al., 2014), our findings suggest that normative variation in parental depression can greatly impact adolescents’ functioning. Our findings therefore may be representative of the larger population, and suggest that adolescents whose parents are not clinically depressed are still at high risk for negative outcomes. This is a key finding and underscores the importance of reducing subclinical depressive symptoms in parents with adolescent children. While this study targeted a community sample, future studies should further investigate at-risk or clinical samples.
Our findings build upon a significant body of literature highlighting the importance of social relationships in adolescents’ neural processing and risk taking. For example, we have previously shown in the same sample using cross-sectional fMRI data that positive aspects of family and peer relationships buffer adolescent risk-taking behavior via neural reactivity. For example, family obligation is associated with decreased VS activation, thereby reducing their risk-taking behaviors (Telzer et al., 2013a). Moreover, high levels of peer support buffer the negative impact of peer conflict on adolescents’ reward sensitivity and risk-taking behavior, by decreasing VS activation (Telzer et al., 2015). Moreover, we have previously shown in the same sample using longitudinal fMRI that positive parent–child relationships serve as a protective factor by dampening adolescents’ VS activation over time, thereby buffering their risk taking (Qu et al., 2015a). The present study makes a new contribution to the growing literature and elucidates the role of parental depression—a risk factor in the family context—in adolescent risk taking and externalizing behavior. Together, these studies highlight the important role of social relationships in buffering or exacerbating VS activation in the context of risk taking.
Several limitations and future directions should be acknowledged. The present study provides correlational evidence that parental depression is associated with changes in adolescents’ neural processing of rewards and future research should attempt to identify a causal mechanistic understanding of the neural substrates involved in this association. Moreover, given the small sample size in this study, future studies are needed to examine this neurodevelopmental process in a larger sample size. In addition, we did not collect information on parental depression at T2, making it impossible to examine how changes in parental depression influence changes in adolescents’ neural reactivity and behavior. Future longitudinal studies can measure parental depression over multiple times and examine how trajectories of parental depression impact adolescents’ functioning. Another limitation in this study is that we did not measure other variables that may potentially explain the link between parental depression and adolescents’ risk taking. For example, the causes of parental depression may also cause increases in adolescent risk taking (e.g. severe economic strain, parental substance use). Therefore, future studies are needed to capture more aspects of parents’ attributes to better understand the link between parental depression and adolescents’ problem behavior. Finally, it is interesting to note that adolescent’s and parent’s depression were not correlated. It is possible that this is due to the non-clinical nature of our sample. Although a body of literature indicates that parental depression may be transmitted to adolescents (e.g. Williamson et al., 1995; Goodman et al., 2011), this transmission may occur only in more clinical samples. Moreover, researchers suggest that several factors, such as the timing of the parent’s depression and characteristics of the child, may moderate this process (Goodman and Gotlib, 1999).
This study provides novel evidence that parental depression is associated with changes in adolescent brain function over time. By using a unique longitudinal fMRI approach, we demonstrated the neural correlates through which parental depression is associated with increases in adolescent risk taking and externalizing behavior. Our findings underscore how normative variation in parental depression can greatly impact adolescents’ neural and behavioral sensitivity to risk taking over time.
Funding
Support for this study was provided by the NICHD (R01HD057164-S and R01HD057164; A.J.F.), NIDA (1R01DA039923; E.H.T), and the NSF (SES 1023293; A.J.F. and E.H.T.).
Conflict of interest. None declared.
Footnotes
This sample is a subsample of a larger study of 48 adolescents who completed a scan at T1. Prior data from the full sample at T1with the BART data have been published (e.g., Telzer et al., 2013a,b, 2014, 2015). Published work from this longitudinal data using the BART task and the same sample focuses on the main effect of longitudinal changes in neural reactivity during risk taking (Qu et al., 2015a), and changes in adolescents’ self-reported family relationship quality (Qu et al., 2015b).
References
- Achenbach T.M. (1991). Manual for the Youth Self-Report and 1991 Profiles. Burlington: Department of Psychiatry, University of Vermont. [Google Scholar]
- Aklin W.M., Lejuez C.W., Zvolensky M.J., Kahler C.W., Gwadz M. (2005). Evaluation of behavioral measures of risk taking propensity with inner city adolescents. Behavior Research and Therapy, 43, 215–28. [DOI] [PubMed] [Google Scholar]
- Allen J.P., Manning N., Meyer J. (2010). Tightly linked systems: reciprocal relations between maternal depressive symptoms and maternal reports of adolescent externalizing behavior. Journal of Abnormal Psychology, 119, 825–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjork J. M., Pardini D. A. (2015). Who are those risk-taking adolescents”? Individual differences in developmental neuroimaging research Developmental Cognitive Neuroscience, 11, 56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore S., Mills K.L. (2014). Is adolescence a sensitive period for sociocultural processing? Annual Review of Psychology, 65, 187–207. [DOI] [PubMed] [Google Scholar]
- Braams B.R., van Duijvenvoorde, Anna C.K., Peper J.S, Crone E.A. (2015). Longitudinal changes in adolescent risk-taking: a comprehensive study of neural responses to rewards, pubertal development, and risk-taking behavior. Journal of Neuroscience, 35, 7226–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell S.B., Morgan-Lopez A.A., Cox M.J., McLoyd V.C. (2009). A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. Journal of Abnormal Psychology, 118, 479–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey B.J., Getz S., Galvan A. (2008). The adolescent brain. Developmental Review, 28, 62–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu C.-P., Tlustos S.J., Walz N.C., et al. (2012). Neural correlates of risky decision making in adolescents with and without traumatic brain injury using the balloon analog risk task. Developmental Neuropsychology 37, 176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clasen P.C., Beevers C.G., Mumford J.A., Schnyer D.M. (2014). Cognitive control network connectivity in adolescent women with and without a parental history of depression. Developmental Cognitive Neuroscience, 7, 13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crone E.A., Dahl R.E. (2012). Understanding adolescence as a period of social–affective engagement and goal flexibility. Nature Reviews Neuroscience, 13, 636–50. [DOI] [PubMed] [Google Scholar]
- Cummings E.M., George R.W., Koss K.J., Davies P.T. (2013). Parental depressive symptoms and adolescent adjustment: responses to children’s distress and representations of attachment as explanatory mechanisms. Parenting: Science and Practice, 13(4), 213–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl R.E. (2004). Adolescent brain development: a period of vulnerabilities and opportunities. Annals of the New York Academy of Sciences, 1021, 1–22. [DOI] [PubMed] [Google Scholar]
- Delgado M., Nystrom L., Fissell C., Noll D., Fiez J. (2000). Tracking the hemodynamic responses to reward and punishment in the striatum. Journal of Neurophysiology, 84, 3072–7. [DOI] [PubMed] [Google Scholar]
- Downey G., Coyne J.C. (1990). Children of depressed parents: an integrative review. Psychological Bulletin, 108, 50–76. [DOI] [PubMed] [Google Scholar]
- Ernst M., Nelson E.E., Jazbec S.P., McClure E.B., Monk C.S., Leibenluft E, et al. (2005). Amygdala and nucleus accumbens in responses to receipt and omission of gains in adults and adolescents. NeuroImage, 25, 1279–91. [DOI] [PubMed] [Google Scholar]
- Fecteau S., Knoch D., Fregni F., Sultani N., Boggio P., Pascual-Leone A. (2007). Diminishing risk-taking behavior by modulating activity in the prefrontal cortex: a direct current stimulation study. Journal of Neuroscience, 27, 12500–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster C.J.E., Garber J., Durlak J.A. (2008). Current and past maternal depression, maternal interaction behaviors, and children’s externalizing and internalizing symptoms. Journal of Abnormal Child Psychology, 36, 527–37. [DOI] [PubMed] [Google Scholar]
- Galván A., Hare T.A., Parra C.E., Penn J., Voss H., Glover G, et al. (2006). Earlier development of the accumbens relative to oribitofrontal cortex might underlie risk-taking behavior in adolescents. Journal of Neuroscience, 26, 6885–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galván A., Hare T., Voss H., Glover G., Casey B.J. (2007). Risk-taking and the adolescent brain: who is at risk? Developmental Science, 10, F8–14. [DOI] [PubMed] [Google Scholar]
- Galván A., Schonberg T., Mumford J., Kohno M., Poldrack R.A., London E.D. (2013). Greater risk sensitivity of dorsolateral prefrontal cortex in young smokers than in nonsmokers. Psychopharmacology, 229, 345–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrison C.Z., Addy C.L., Jackson K.L., McKeown R.E., Waller J.L. (1991). The CES-D as a screen for depression and other psychiatric disorders in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 636–41. [DOI] [PubMed] [Google Scholar]
- Gogtay N., Giedd J.N., Lusk L., Hayashi K.M., Greenstein D., Vaituzis A.C, et al. (2004). Dynamic mapping of human cortical development during childhood through early adulthood. Proceedings of the National Academy of Sciences United States of America, 101, 8174–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S.H., Gotlib I.H. (1999). Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–90. [DOI] [PubMed] [Google Scholar]
- Goodman S.H., Rouse M.H., Connell A.M., Broth M.R., Hall C.M., Heyward D. (2011). Maternal depression and child psychopathology: a meta-analytic review. Clinical Child and Family Psychology Review, 14, 1–27. [DOI] [PubMed] [Google Scholar]
- Gotlib I.H., Hamilton J.P., Cooney R.E., Singh M.K., Henry M.L., Joormann J. (2010). Neural processing of reward and loss in girls at risk for major depression. Archives of General Psychiatry, 67, 380–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knoch D., Fehr E. (2007). Resisting the power of temptations: the right prefrontal cortex and self-control. Annals of the New York Academy of Sciences, 1104, 123–34. [DOI] [PubMed] [Google Scholar]
- Knutson B., Westdorp A., Kaiser E., Hommer D. (2000). fMRI visualization of brain activity during a monetary incentive delay task. NeuroImage, 12, 20–7. [DOI] [PubMed] [Google Scholar]
- Lamis D.A., Malone P.S., Lansford J.E., Lochman J.E. (2012). Maternal depressive symptoms as a predictor of alcohol use onset and heavy episodic drinking in youths. Journal of Consulting and Clinical Psychology, 80, 887–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez C.W., Aklin W.M., Zvolensky M.J., Pedulla C.M. (2003). Evaluation of the balloon analogue risk task (BART) as a predictor of adolescent real-world risk-taking behaviors. Journal of Adolescence, 26, 475–9. [DOI] [PubMed] [Google Scholar]
- Lejuez C.W., Aklin W., Daughters S., Zvolensky M., Kahler C., Gwadz M. (2007). Reliability and validity of the youth version of the balloon analogue risk task (BART-Y) in the assessment of risk-taking behavior among inner-city adolescents. Journal of Clinical Child & Adolescent Psychology, 36, 106–11. [DOI] [PubMed] [Google Scholar]
- Lejuez C.W., Read J.P., Kahler C.W., Richards J.B., Ramsey S.E., Stuart G.L, et al. (2002). Evaluation of a behavioral measure of risk taking: the balloon analogue risk task (BART). Journal of Experimental Psychology: Applied, 8, 75–84. [DOI] [PubMed] [Google Scholar]
- Lovejoy M.C., Graczyk P.A., O’Hare E., Neuman G. (2000). Maternal depression and parenting behavior: a meta–analytic review. Clinical Psychology Review, 20, 561–92. [DOI] [PubMed] [Google Scholar]
- McCormick E.M., Qu Y., Telzer E.H. (2016). Adolescent neurodevelopment of cognitive control and risk taking in negative family contexts. NeuroImage, 124, 989–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E.K., Cohen J.D. (2001). An integrative theory of prefrontal cortex function. Annual Review of Neuroscience, 24, 167–202. [DOI] [PubMed] [Google Scholar]
- Monk C.S., Klein R.G., Telzer E.H., Schroth E.A., Mannuzza S., Moulton J.L.I.I.I, et al. (2008). Amygdala and nucleus accumbens activation to emotional facial expressions in children and adolescents at risk for major depression. American Journal of Psychiatry, 165, 90–8. [DOI] [PubMed] [Google Scholar]
- Morgan J.K., Shaw D.S., Forbes E.E. (2014). Maternal depression and warmth during childhood predict age 20 neural response to reward. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 108–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino T.M., McMakin D.L., Morgan J.K., Silk J.S., Birmaher B., Axelson D.A, et al. (2014). Reduced reward anticipation in youth at high-risk for unipolar depression: a preliminary study. Developmental Cognitive Neuroscience, 8, 55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K. J., Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–91. [DOI] [PubMed] [Google Scholar]
- Pugh K.L., Farrell A.D. (2012). The impact of maternal depressive symptoms on adolescents’ aggression: role of parenting and family mediators. Journal of Child and Family Studies, 21, 589–602. [Google Scholar]
- Qu Y., Galván A., Fuligni A.J., Lieberman M.D., Telzer E.H. (2015a). Longitudinal changes in prefrontal cortex activation underlie declines in adolescent risk taking. Journal of Neuroscience, 35, 11308–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu Y., Fuligni A.J., Galván A., Telzer E.H. (2015b). Buffering effect of positive parent-child relationships on adolescent risk taking: a longitudinal neuroimaging investigation. Developmental Cognitive Neuroscience, 15, 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. (1977). The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Schonberg T., Fox C.R., Mumford J.A., Congdon E., Trepel C., Poldrack R.A. (2012). Decreasing ventromedial prefrontal cortex activity during sequential risk-taking: an FMRI investigation of the balloon analog risk task. Frontiers in Neuroscience, 6, 80.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp C., Kim S., Herman L., Pane H., Reuter T., Strathearn L. (2014). Major depression in mothers predicts reduced ventral striatum activation in adolescent female offspring with and without depression. Journal of Abnormal Psychology, 123, 298–309. [DOI] [PubMed] [Google Scholar]
- Steinbeis N., Bernhardt B.C., Singer T. (2012). Impulse control and underlying functions of the left DLPFC mediate age-related and age-independent individual differences in strategic social behavior. Neuron, 73, 1040–51. [DOI] [PubMed] [Google Scholar]
- Steinberg L. (2010). A dual systems model of adolescent risk-taking. Developmental Psychobiology, 52, 216–24. [DOI] [PubMed] [Google Scholar]
- Telzer E.H., Fuligni A.J., Lieberman M.D., Galvan A. (2013a). Meaningful family relationships: neurocognitive buffers of adolescent risk taking. Journal of Cognitive Neuroscience, 25, 374–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telzer E.H., Fuligni A.J., Lieberman M.D., Galvan A. (2013b). The effects of poor quality sleep on brain function during risk taking in adolescence. NeuroImage, 71, 275–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telzer E.H., Fuligni A.J., Lieberman M.D., Galvan A. (2014). Neural sensitivity to eudaimonic and hedonic rewards differentially predict adolescent depressive symptoms over time. Proceedings of the National Academy of Sciences of the United States of America, 111, 6600–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telzer E.H., Fuligni A.J., Lieberman M.D., Miernicki M., Gálvan A. (2015). The quality of adolescents’ peer relationships modulates neural sensitivity to risk taking. Social Cognitive Affective Neuroscience, 10, 389–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Bulk B.G., Koolschijn P.C.M.P., Meens P.H.F., et al. (2013). How stable is activation in the amygdala and prefrontal cortex in adolescence? A study of emotional face processing across three measurements. Developmental Cognitive Neuroscience, 4, 65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M.M., Wickramaratne P., Nomura Y., Warner V., Pilowsky D., Verdeli H. (2006). Offspring of depressed parents: 20 years later. American Journal of Psychiatry, 163, 1001–8. [DOI] [PubMed] [Google Scholar]
- Williamson D.E., Ryan N.D., Birmaher B., et al. (1995). A case-control family history study of depression in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 34, 1596–607. [DOI] [PubMed] [Google Scholar]
- Zich J.M., Attkisson C.C., Greenfield T.K. (1990). Screening for depression in primary care clinics: the CES-D and the BDI. International Journal of Psychiatry in Medicine, 20, 259–77. [DOI] [PubMed] [Google Scholar]