Abstract
Aim:
To study all the elderly patients (≥75 years) who were admitted in an Intensive Care Unit (ICU) of a Spanish hospital and identify factors associated with mortality.
Patients and Methods:
A retrospective, observational data collected prospectively in patients ≥75 years recruited from the ICU in the period of January 2004 to December 2010.
Results:
During the study period, 1661 patients were admitted to our unit, of whom 553 (33.3%) were older than 75 years. The mean age was 79.9 years, 317 (57.3%) were male, and the overall in-hospital mortality was 94 patients (17% confidence interval 14–20.3%). When comparing patients who survived to those who died, we found significant differences in mean age (P = 0.001), Acute Physiologic Assessment and Chronic Health Evaluation II and Simplified Acute Physiology Scoring II (SAPS II) on admission (P < 0.0001, postoperative patients (P = 0.001), and need for mechanical ventilation (P < 0.0001). Comparing age groups, we found statistically significant differences in SAPS II (P = 0.007), diagnosis of non-ST-segment elevation myocardial infarction (P = 0.014), complicated postoperative period (P = 0.001), and pacemaker (P = 0.034). Mortality between the groups was statistically significant (P = 0.004). The survival between the group of 65 and 74 years and patients >75 years was not significant (P = 0.1390).
Conclusions:
The percentage of elderly patients in our unit is high, with low mortality rates. The age itself is not the sole determinant for admission to the ICU and other factors should be taken into account.
Keywords: Elderly, in-hospital mortality, outcome
Introduction
The increase in life expectancy observed in Spain over recent years (recently second after Japan), along with a significant decrease in fertility means that the average age of patients being admitted to an Intensive Care Unit (ICU) has increased considerably. Furthermore, elderly patients above the age of 75 years now represent the largest group of patients admitted to the ICU setting.[1,2,3] However, this is not a new phenomenon, it has been appreciated for several decades already and has prompted a change in attitudes around the subject.[4,5]
The care of elderly patients admitted to ICU can be complicated for several reasons. This cohort of patients has an associated poor life expectancy, high mortality rates, and high health-care costs, which increases proportionally with age. Furthermore, the use of new technologies is increasingly expensive and admission to ICU unit is associated with functional impairment which results in a decreased quality of life. This encompasses the underlying diagnosis, procedures undertaken, complications encountered, and the general aging process including malnutrition, loss of bone and muscle mass, and therefore decreased pulmonary ventilation.[6,7,8]
Therefore, this has led to several questions being asked prior to admitting elderly patients to ICU, such as: Which patient is best suited to admission? What is the maximum level of care? Along with other related ethical considerations.[9] Several studies have shown that a number of factors are related to hospital survival rates and that age alone should not be used in determining an elderly patient's eligibility for admission to ICU.[1,10,11]
In this article, we studied elderly patients (≥75 years) who were admitted to the ICU of a county hospital with a rapidly aging population and identified factors associated with mortality during the hospital stay.
Patients and Methods
This was a retrospective observational study, following hospital Ethics Committee approval of patients ≥75 years consecutively admitted to the medical ICU at the Hospital Valle de los Pedroches, between January 2004 and December 2010. During the 6-year study period study, 1661 were admitted to the ICU. All older persons 75 years and over (n = 553) consecutively admitted to the ICU were assessed for eligibility. The ICU receives patients with both medical and surgical diagnoses and provides regular treatment such as assisted ventilation, dialysis, hemodynamic surveillance, and treatment. The emergency department provides cover for more than 30,000 patient visits per year with an eight bed observational medical unit of that permits short-term patient monitoring and/or treatment over an initial 24–48 h period.
Data were collected via computerized medical records. We collected the following variables: Age, sex, primary reason for the ICU admission (surgical or medical), comorbidities, patient's conditions on admission (coronary, medical, elective surgery, emergency surgery, and trauma), referral source (emergency department, observation unit, internal medicine, general surgery, operating room, etc.), length of stay, mechanical ventilation, primary diagnoses, and according to International Classification of Diseases, 10th Revision. To assess illness severity, the Simplified Acute Physiology Scoring II (SAPS II) system was used. Calculation of the individual SAPS II scores was based on the most deranged physiological values recorded within the first 24 h of ICU admission. The SAPS II score consists of the combined total value achieved across 17 domains (12 physiological variables, age, type of admission, and three underlying diseases). The weight assigned to these variables can range from 0 to a maximum of 26 points. The total SAPS II score ranges from 0 to a maximum of 158 points, with higher scores representing more severe illness. Furthermore, Acute Physiologic Assessment and Chronic Health Evaluation (APACHE) scores and invasive parameters were also recorded, along with continuous venovenous hemofiltration, central venous catheter (CVC), pacemakers, and mortality.
Statistical analyses were performed using the Statistics Package for Social Scientists 18.0 (SPSS Inc. Released 2009. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc.). Descriptive statistics included frequency analysis (percentages) for nominal variables and mean ± standard deviations or medians and interquartile ranges for continuous variables according to their distribution. Independent t-test (continuous variables) and Chi-square test (categorical variables) were used for a univariate analysis when comparing age groups and survivors/nonsurvivors. P ≤ 0.05 was considered significant for all tests. The total sample was divided into three groups according to age (<80 years, 80–85 years, and >85 years) and we compared the different groups using analysis of variance for continuous variables and Chi-square test to compare percentages, considering P ≤ 0.05 as significant. Finally, we studied the influence of several factors on mortality by multivariate logistic regression analysis. Odds ratios and 95% confidence intervals (CIs) were used to estimate the association between the independent determinants of hospital mortality
Results
During the study period, 1661 patients were admitted to our unit, 553 (33.3%) were older than 75 years of age. Of these participants, the mean age was 79.9 years, 317 (57.3%) were male, and a total of 94 deaths were observed (17% CI 14–20.3%). The demographic and clinical characteristics are summarized in Table 1.
Table 1.
Clinical and demographic characteristics of patients ≥75 years admitted to the Intensive Care Unit and differences between patients according to mortality
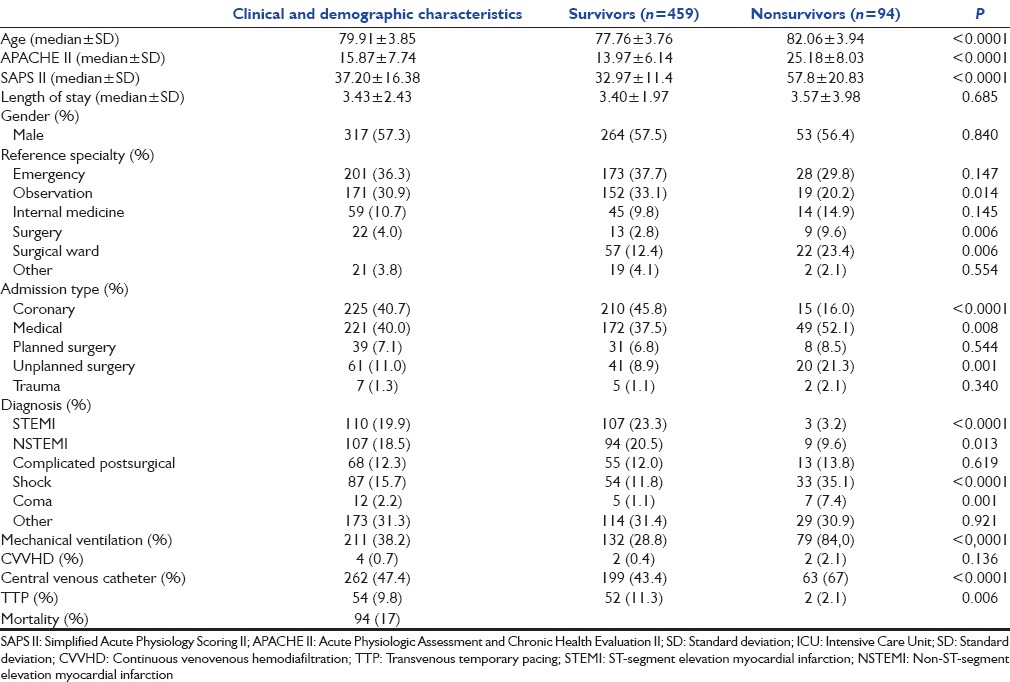
When comparing patients who survived to those who died, we found significant differences in mean age (P < 0.0001), APACHE II and SAPS II scores on admission (P < 0.0001), being transferred from observation unit (P = 0.01), being transferred from a surgical ward (P = 0.006), coronary patients (P < 0.0001), physician (P = 0.008), postoperative patients (P = 0.001), need for mechanical ventilation (P < 0.0001), CVC (P = 0.0001), pacemaker (P = 0.006), and certain specific diagnoses [Table 1].
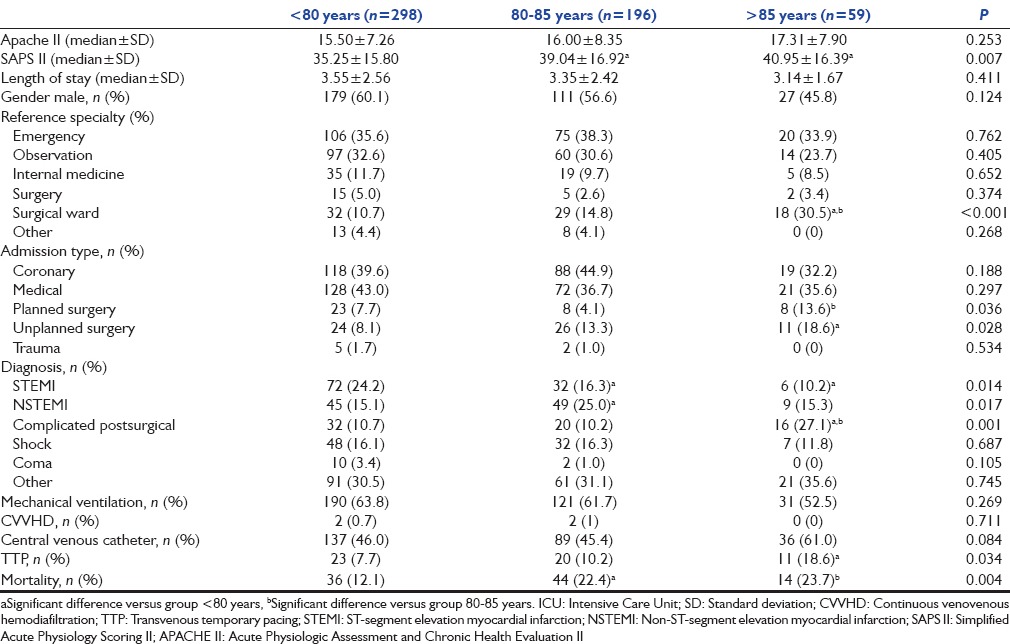
We divided the entire sample by age group (<80 years, 80–85 years, and > 85 years) finding statistically significant differences in SAPS II score (P = 0.007), being transferred from surgery (P ≤ 0.0001), scheduled and urgent postoperative (P = 0.036 and P = 0.028, respectively), diagnosis of non-ST-segment elevation myocardial infarction (P = 0.014), complicated postoperative period (P = 0.001), and pacemaker (P = 0.034). Mortality between the groups was statistically significant (P = 0.004) [Table 2].
Table 2.
Differences between patients according to age group
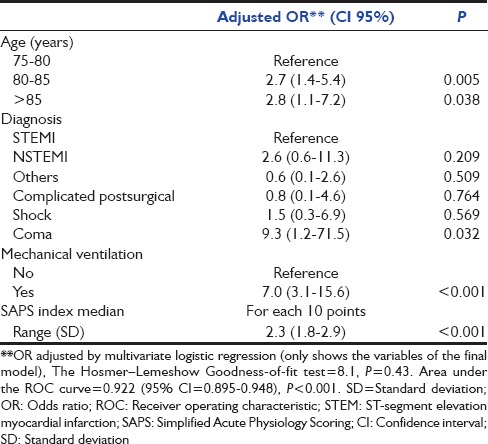
Multivariate analysis, without including APACHE II and (CVVHD) Venovenous Hemodiafiltration, was performed because of the low causality which showed the independent variables associated with mortality in elderly patients ≥75 years in ICU setting are age, diagnosis at admission, SAPS II, and the need of mechanical ventilation [Table 3].
Table 3.
Risk factors for Intensive Care Unit mortality in elderly patients
Finally, when compared the survival between the group of 65 and 74 years and patients >75 years showed a nonsignificant P value of 0.1390.
Discussion
First, one the most notable and relevant findings from our work was that patients ≥75 years of age represented over 30% of the total patients admitted to our ICU department. According to a recent study by Blot et al.,[12] there has been an increase of 33% of patients ≥75 years admitted to the ICU between 1992–1996 and 2002–2006. During the same year, a French group of Daubin et al.[13] carried out a study of the predictors of short-term mortality, physical and mental dependence in patients over 75 years following admission to ICU, with this cohort of patients representing 19% of the total admissions to the department. The slightly higher observed figure in our series is likely due to the larger proportion elderly population residing in our region.
Within our sample, the mortality rate was 17%, significantly lower than 42% overall mortality rate observed in the study undertaken by Daubin et al. This is also true when comparing our series with the study by Vosylius et al. where mortality was studied in a group of patients over 75 years, with an overall result of 39%. The same group found severity index at admission (measured by SAPS II), impaired level of consciousness, and the presence of infection during their stay were identified as independent risk factors of mortality.[14] It is well known that elderly adults are at an increased risk of developing complications during their hospital stay along with having a higher inpatient hospital mortality rate. The risk factors associated with mortality in the oldest patients admitted to the ICU include age >85 years, being transferred from the emergency department, observation unit or surgical wards, shock, undergoing emergency surgery, and hyperglycemia, this is similar to the findings by the recent study of Hwang el al.[15]
The influence of mechanical ventilation on mortality in patients over 75 years has been studied elsewhere, with a 38% mortality rate.[16] If we compare our results with Spanish groups, Obón et al. in 2009 published a study obtaining a mortality rate of 21.25%; however, these patients were older than 84 years of age.[17] The study of Santana et al. in Gran Canaria obtained mortality rate of 18.7%; however, the patients were older than 70 years of age and had an ICU admission exceeding 30 days.[17] In our study, the overall incidence of failed extubation represented 11.6% of the deaths in ICU. Mortality rates within ICU were 4.7% and 11.6% in successfully extubated patients and in those with failed extubation, respectively (P = 0.001). Age remained a risk factor for inpatient hospital mortality after adjusting for failed extubation, a finding that is consistent with previous studies.[18]
When comparing patients according to their age group, we found statistically significant differences in terms of mortality with increasing age. However, we cannot consider it as the only determinant factor as there was also an observed increase in the SAPS II severity index and the percentage of postoperative complications. There are many studies which have compared the mortality of elderly patients based on their respective age group. The group of Obón et al. found a variation in mortality of patients depending if they were ≥84 or <84 years.[3] Recently, other studies have also found that mortality rates increase proportionally with age although it is not clear if the observed differences were significant.[9,19] Finally, Yu et al. have also compared the mortality of patients according to age group showing a global increase. They also observed that mortality was greater in patients admitted to the ICU compared to those not admitted.[20]
There is a wealth of studies that have identified factors associated with the mortality of elderly patients in the ICU.[7,8,11,13,14,17] Roch et al. studied the mortality of 299 patients in an ICU for a period of 6 consecutive years. The hospital mortality was found to be 55% and they identified that the independent factors associated with mortality are high severity index SAPS II on admission to ICU and the presence of a fatal disease according to McCabe score and cardiac diagnosis during admission.[21] In another study of a Brazilian ICU, Collyer et al. examined 84 patients over 60 years of age who were admitted to ICU department. They found a high mortality rate (62.8%) and identified age, coma, hypotension, respiratory failure, and acute renal failure on admission as the risk factors for mortality.[22]
The APACHE II score that has been the gold standard in ICUs and is the sum of 12 physiological parameters is widely used to quantify the severity of illness in the ICU and has been validated in many clinical trials, and it has been demonstrated that it can be applied in elderly patients.[23] As in other studies,[24,25,26,27] the APACHE II score was sufficiently accurate in the present study to be able to predict mortality in elderly patients. However, the APACHE score emphasizes the measurement of physiological derangement, and there is small consideration of preexisting disease and may not adequately account for the quantitative or qualitative contribution of comorbid illness (e.g., the APACHE II system assigns 0, 2, or 5 chronic health points for preexisting comorbidity out of a possible 73 total points), thus limiting the ability of these model to accurately predict mortality. Although the APACHE II score was not included in the multivariate analysis, the univariate analysis was significant with a median APACHE of 13.97 ± 6.14 in the survival group and 25.18 ± 8.03, P < 0.0001 in the nonsurvival group. The entire APACHE II may not be necessary for determining patients’ prognosis of the components of the APACHE II score, the age component seems to be the most strongly associated with long-term mortality. In a study of predictors of long-term survival in chronic obstructive pulmonary disease patients admitted to a general medical ward,[28] Cox regression was used to determine the relative importance of individual components; of the three components, age was the variable most strongly associated with long-term mortality in a multivariate model.
Elderly patients are commonly categorized in three classes: “Young old” or “young elderly” for patients between 65 and 70 or 75 years, “old-old” or “older elderly” for patients aged between 70 or 75 and 80 or 85, and “oldest-old” or “very elderly” for patients aged more than 80 or 85 years.[29,30,31,32] The study compared the mortality in the group of patients >75 years old (“older elderly” and “very elderly”) with the group of patients between 65 and 74 years (“young old” or “young elderly”) that was the largest group of patients admitted to the ICU, there were no significant differences in the mortality in both groups. Very advanced age only represents a minor risk factor for early mortality. Among relevant factors with an impact on later mortality at 6 months, 1 year, or more after ICU are the number and the type of comorbidities, the functional status, and the quality of life before or just after the ICU stay. A systematic review concerning the prognostication of the mortality of elderly ICU patients reported that there are only seven studies of a sufficient quality. The paper showed that there is no acceptable, credible, or clinically useful model able to predict the mortality in the elderly.[33] A number of studies tried to identify the risk factors of mortality for a number of specific ICU diseases with variable success.
The Eldicus study in 2012[34] was conducted with the goal to determine the effect of ICU triage decisions on mortality and ICU benefit, specifically for elderly patients in seven European ICUs, it concluded that the mortality benefit appears greater for the elderly patients despite the fact that of a higher mortality and more rejections. Recently, Fassier et al.[35] studied ICU admissions for patients aged ≥80 years in 2009 in France with an in-hospital mortality of 33.9%. The median time spent in the ICU was 3 days. Medical and surgical diagnosis-related group hospitalizations were characterized by significant differences in volume, mortality, ICU days and costs with a marked clinical heterogeneity in the population of elderly patients hospitalized in the ICU. These data provide baseline information and prompt further studies comparing intensive care utilization across age groups, between countries and over time.
Possible limitations to our study include lack of data regarding mortality outside of our unit as well as the quality of life of patients successfully discharged from ICU. Similarly, there is no data reflecting the cases in which there was a limited therapeutic effort.
Conclusions
We can confirm that a considerable number of elderly patients are admitted to our unit and form a large proportion of the total number of patients. The overall mortality rate in this cohort of patients in our unit is relatively less than in comparative studies and age itself is not the only determining factor for prognosis. In our unit diagnosis SAPS II and the need of mechanical ventilation were associated with mortality in patients ≥75 years in ICU. Thus, it is imperative that eligibility for admission to an ICU should not be based only on age but take into account baseline patient status and possible subsequent recovery, other factors including the comorbidities, reason for admission and critical conditions. Furthermore, every effort should be made to consider the patient's wishes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.López-Messa JB. Age and Intensive Medicine. Med Intensiva. 2005;29:469–74. [Google Scholar]
- 2.McDermid RC, Bagshaw SM. ICU and critical care outreach for the elderly. Best Pract Res Clin Anaesthesiol. 2011;25:439–49. doi: 10.1016/j.bpa.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Obón B, Gutiérrez I, Sánchez C. Appropriateness of admissions to the intensive care unit in the oldest-old. Rev Esp Geriatr Gerontol. 2006;41:193–5. [Google Scholar]
- 4.Lerolle N, Trinquart L, Bornstain C, Tadié JM, Imbert A, Diehl JL, et al. Increased intensity of treatment and decreased mortality in elderly patients in an intensive care unit over a decade. Crit Care Med. 2010;38:59–64. doi: 10.1097/CCM.0b013e3181b088ec. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen YL, Angus DC, Boumendil A, Guidet B. The challenge of admitting the very elderly to intensive care. Ann Intensive Care. 2011;1:29. doi: 10.1186/2110-5820-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santana Cabrera L, Sánchez-Palacios M, Hernández Medina E, Eugenio Robaina P, Villanueva-Hernández A. Characteristics and prognosis of patients with very long stay in an intensive care unit. Med Intensiva. 2008;32:157–62. doi: 10.1016/s0210-5691(08)70931-8. [DOI] [PubMed] [Google Scholar]
- 7.García Lizana F, Manzano Alonso JL, Saavedra Santana P. Mortality and quality of life of patients beyond 65 years one year after ICU discharge. Med Clin (Barc) 2001;116:521–5. doi: 10.1016/s0025-7753(01)71893-3. [DOI] [PubMed] [Google Scholar]
- 8.López-Soto A, Sacanella E, Pérez JM. Elderly patient in an intensive critical unit. Rev Esp Geriatr Gerontol. 2009;44:27–33. doi: 10.1016/j.regg.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Galzerano A, Sabatini E, Durì D, Rossi C, Silvestri L, Mazzon D, et al. Old patients in intensive care unit (ICU): What decisions to make? Arch Gerontol Geriatr. 2009;49:294–7. doi: 10.1016/j.archger.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Nathanson BH, Higgins TL, Brennan MJ, Kramer AA, Stark M, Teres D. Do elderly patients fare well in the ICU? Chest. 2011;139:825–31. doi: 10.1378/chest.10-1233. [DOI] [PubMed] [Google Scholar]
- 11.López-Soto A. Geriatric assessment in the frail elderly hospitalized in the intensive care unit. Rev Multidiscip Gerontol. 2005;15:50–3. [Google Scholar]
- 12.Blot S, Cankurtaran M, Petrovic M, Vandijck D, Lizy C, Decruyenaere J, et al. Epidemiology and outcome of nosocomial bloodstream infection in elderly critically ill patients: A comparison between middle-aged, old, and very old patients. Crit Care Med. 2009;37:1634–41. doi: 10.1097/CCM.0b013e31819da98e. [DOI] [PubMed] [Google Scholar]
- 13.Daubin C, Chevalier S, Séguin A, Gaillard C, Valette X, Prévost F, et al. Predictors of mortality and short-term physical and cognitive dependence in critically ill persons 75 years and older: A prospective cohort study. Health Qual Life Outcomes. 2011;9:35. doi: 10.1186/1477-7525-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vosylius S, Sipylaite J, Ivaskevicius J. Determinants of outcome in elderly patients admitted to the intensive care unit. Age Ageing. 2005;34:157–62. doi: 10.1093/ageing/afi037. [DOI] [PubMed] [Google Scholar]
- 15.Hwang LC, Hsu CP, Tjung JJ, Shih SC, Lin CH, Huang TH. Predictors of in-hospital mortality in oldest-old patients in Taiwan. Int J Gerontol. 2013;7:22–6. [Google Scholar]
- 16.Ely EW, Evans GW, Haponik EF. Mechanical ventilation in a cohort of elderly patients admitted to an intensive care unit. Ann Intern Med. 1999;131:96–104. doi: 10.7326/0003-4819-131-2-199907200-00004. [DOI] [PubMed] [Google Scholar]
- 17.Obón B, Gutiérrez I, Sánchez C. Patients over 80 years in intensive medicine. Med Intensiva. 2009;33:461. doi: 10.1016/j.medin.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Cheng AC, Cheng KC, Chen CM, Hsing SC, Sung MY. The outcome and predictors of failed extubation in intensive care patients - The elderly is an important predictor. Int J Gerontol. 2011;5:206–11. [Google Scholar]
- 19.Grace RF, Gosley M, Smith P. Mortality and outcomes of elderly patients admitted to the intensive care unit at Cairns Base Hospital, Australia. Crit Care Resusc. 2007;9:334–7. [PubMed] [Google Scholar]
- 20.Yu W, Ash AS, Levinsky NG, Moskowitz MA. Intensive care unit use and mortality in the elderly. J Gen Intern Med. 2000;15:97–102. doi: 10.1046/j.1525-1497.2000.02349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roch A, Wiramus S, Pauly V, Forel JM, Guervilly C, Gainnier M, et al. Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care. 2011;15:R36. doi: 10.1186/cc9984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alves GC, Silva Júnior GB, Lima RS, Sobral JB, Mota RM, Abreu KL, et al. Risk factors for death among critically ill elderly patients. Rev Bras Ter Intensiva. 2010;22:138–43. [PubMed] [Google Scholar]
- 23.Zhou GP, Song YX, Zhao ZJ. Efficiency of APACHE II and III scoring system in the prognostication of patients older than 75 years. Zhonghua Nei Ke Za Zhi. 2005;44:251–3. [PubMed] [Google Scholar]
- 24.Quach S, Hennessy DA, Faris P, Fong A, Quan H, Doig C. A comparison between the APACHE II and Charlson index score for predicting hospital mortality in critically ill patients. BMC Health Serv Res. 2009;9:129. doi: 10.1186/1472-6963-9-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schönhofer B, Guo JJ, Suchi S, Köhler D, Lefering R. The use of APACHE II prognostic system in difficult-to-wean patients after long-term mechanical ventilation. Eur J Anaesthesiol. 2004;21:558–65. doi: 10.1017/s0265021504007100. [DOI] [PubMed] [Google Scholar]
- 26.Sakr Y, Krauss C, Amaral AC, Réa-Neto A, Specht M, Reinhart K, et al. Comparison of the performance of SAPS II, SAPS 3, APACHE II, and their customized prognostic models in a surgical intensive care unit. Br J Anaesth. 2008;101:798–803. doi: 10.1093/bja/aen291. [DOI] [PubMed] [Google Scholar]
- 27.Mbongo CL, Monedero P, Guillen-Grima F, Yepes MJ, Vives M, Echarri G. Performance of SAPS3, compared with APACHE II and SOFA, to predict hospital mortality in a general ICU in Southern Europe. Eur J Anaesthesiol. 2009;26:940–5. doi: 10.1097/EJA.0b013e32832edadf. [DOI] [PubMed] [Google Scholar]
- 28.Goel A, Pinckney RG, Littenberg B. APACHE II predicts long-term survival in COPD patients admitted to a general medical ward. J Gen Intern Med. 2003;18:824–30. doi: 10.1046/j.1525-1497.2003.20615.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hennessy D, Juzwishin K, Yergens D, Noseworthy T, Doig C. Outcomes of elderly survivors of intensive care: A review of the literature. Chest. 2005;127:1764–74. doi: 10.1378/chest.127.5.1764. [DOI] [PubMed] [Google Scholar]
- 30.Chelluri L, Pinsky MR, Grenvik AN. Outcome of intensive care of the “oldest-old” critically ill patients. Crit Care Med. 1992;20:757–61. doi: 10.1097/00003246-199206000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Djaiani G, Ridley S. Outcome of intensive care in the elderly. Anaesthesia. 1997;52:1130–6. doi: 10.1111/j.1365-2044.1997.237-az0369.x. [DOI] [PubMed] [Google Scholar]
- 32.Kaarlola A, Tallgren M, Pettilä V. Long-term survival, quality of life, and quality-adjusted life-years among critically ill elderly patients. Crit Care Med. 2006;34:2120–6. doi: 10.1097/01.CCM.0000227656.31911.2E. [DOI] [PubMed] [Google Scholar]
- 33.Minne L, Ludikhuize J, de Jonge E, de Rooij S, Abu-Hanna A. Prognostic models for predicting mortality in elderly ICU patients: A systematic review. Intensive Care Med. 2011;37:1258–68. doi: 10.1007/s00134-011-2265-6. [DOI] [PubMed] [Google Scholar]
- 34.Sprung CL, Artigas A, Kesecioglu J, Pezzi A, Wiis J, Pirracchio R, et al. The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: Intensive care benefit for the elderly. Crit Care Med. 2012;40:132–8. doi: 10.1097/CCM.0b013e318232d6b0. [DOI] [PubMed] [Google Scholar]
- 35.Fassier T, Duclos A, Abbas-Chorfa F, Couray-Targe S, West TE, Argaud L, et al. Elderly patients hospitalized in the ICU in France: A population-based study using secondary data from the national hospital discharge database. J Eval Clin Pract. 2016;22:378–86. doi: 10.1111/jep.12497. [DOI] [PubMed] [Google Scholar]


