Abstract
Aims:
This study was conducted retrospectively to define early demographic and clinical predictors for acute kidney injury (AKI) among snake bite patients at the time of hospital admission.
Materials and Methods:
We analyzed 138 cases with a poisonous snake bite. Patients were classified into two groups according to the presence and absence of AKI. The data regarding clinical features and demographic profile of these patients were collected from the hospital records in a prestructured pro forma and statistically compared.
Results:
Of the 138 patients of venomous snake bite, 62 developed AKI (44.92%). Patients who developed AKI were older in age. Moreover, prolonged bite to anti-snake venom (ASV) time had a significant relationship in developing AKI (P < 0.05). Among the clinical features, there was an independent positive association of AKI with abdomen pain, tenderness and vomiting, cellulitis, bleeding tendencies, myalgia, and black or brown urine (P < 0.05). Neurological features were inversely associated with renal involvement.
Conclusion:
We found that marked abdominal pain, tenderness and vomiting, myalgia, black or brown urine, bite site cellulitis, bleeding tendencies, and prolonged (>2 h) bite to ASV time were significantly associated with the development of AKI in snake bite patients.
Keywords: Acute kidney injury, clinical predictors, snake bite
Introduction
Snake bite is a serious occupational hazard for the rural population. Every year, about 40,000–50,000 people die of snake bite in India.[1] Snake venom causes neurotoxicity, coagulopathy, and renal failure. Who will develop which organopathy depends on the snake species in a particular geographical region? As it is not always possible to identify the snake, need of clinical predictors for organ involvement is crucial in management.
Patients at high risk of developing acute renal failure should be identified earlier and referred to the higher center for proper treatment to prevent serious consequences of uremia. With this objective in mind, we did this retrospective record-based controlled study of 138 patients who presented to our institute with venomous snake bite between July 2014 and December 2015 to identify early predictors of renal involvement in snake bite.
Materials and Methods
The present study was conducted at a tertiary care hospital in the North Eastern region of Uttar Pradesh, India, which is an important referral center for the rural population of the district.
We had 280 snake bite patients presenting to our institute between July 2014 and December 2015. Records of these were retrospectively analyzed. Ethical approval was taken for the study from the Institute's Ethical Committee. Patient data regarding age, gender, time elapsed between snake bite and administration of anti-snake venom (ASV), clinical features, and laboratory investigations and outcome were collected in prestructured pro forma.
Of the 280 cases, only 138 had a venomous bite while rest 142 who had nonvenomous bites were excluded from the study. We further analyzed the 138 cases with venomous bite. Of these 138 cases with snake bite, 62 developed renal injury while 76 did not. Of these 76 patients who did not develop renal injury, 48 developed neurotoxicity, while 28 had mild symptoms such as isolated cellulitis or perioral paresthesia or giddiness but no life-threatening systemic toxicity.
Venomous bites were given polyvalent ASV at admission followed by continuous infusion till 48 h or till correction of abnormal clotting time.
Inclusion criteria[2,3]
Definitive history of snake bite
Clinical picture of snake bite like two close set puncture marks denoting fang marks or local tissue reaction or cellulitis or abnormal 20 min whole blood clotting time >20 min within 12 h of snake bite or later; bleeding tendencies or acute kidney injury (AKI) or neuroparalysis
Development of AKI defined as absolute increase in serum creatinine ≥0.3 mg/dl from baseline or a percentage increase in the serum creatinine of ≥50% above baseline within 48 h or oliguria of <0.5 ml/kg per hour for more than 6 h or urine output 400 ml/day
Development of neurotoxicity was considered when there was documented ptosis, weakness of neck and bulbar muscles, difficulty in breathing, and need for neostigmine or ventilatory support.
Exclusion criteria[2,3]
Nonvenomous bites, i.e., those who had ragged bite marks and did not manifest any clinical or laboratory features of envenoming during their hospital stay of at least 12 h and did not re-present to the hospital with delayed envenoming
Patients with preexistent renal diseases, i.e., serum creatinine >1.5 mg/dl prior to snake bite
Known case of diabetes or hypertension
Patients who had exposure to nephrotoxic drugs/agents
Patients with malaria diagnosed on peripheral smear examination
Patients whose ultrasound abdomen showed bilateral small kidneys/loss of corticomedullary differentiation/any obstructive uropathy or previous renal pathology.
Statistical analysis
Patients were classified into two groups according to the presence and absence of AKI. Difference between the two groups was compared using the Chi-square test. Risk factors for the development of AKI were statistically analyzed. P < 0.05 was considered statistically significant.
Results
Of 138 patients who had venomous snake bites, 62 patients developed acute renal injury, putting the incidence of 44.92% for nephrotoxic bites. Renal toxicity due to snake bite occurred within 48 h to 10 days of envenomation. Most of the patients (94%) developed symptoms and signs of acute renal failure within 48–72 h, while 6% of patients developed renal manifestations from 5 to 10 days after the snake bite.
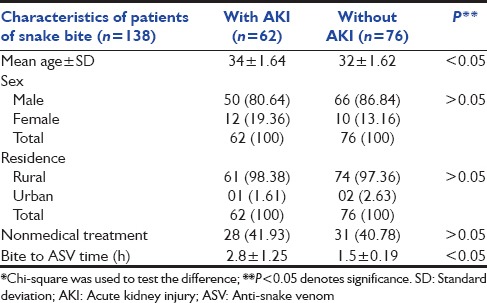
Most of the snake bite patients were males (84.05%). Patients who developed AKI were mostly older than those who did not develop AKI (34 ± 1.64 vs. 32 ± 1.62) (P < 0.05). In our study, snake bite patients hailed predominantly from the rural population (97.87%). Furthermore, 59 out of 138 venomous bite patients (42.75%) took nonmedical treatment before coming to the health facility. Prolonged bite to ASV time had a significant relationship in developing AKI (P < 0.05) [Table 1].
Table 1.
Demographic features of snake bite patients with and without acute kidney injury*
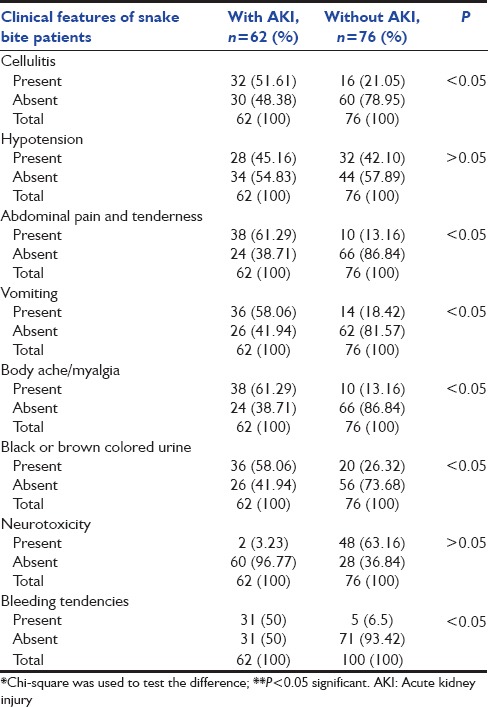
Among the clinical features [Table 2], there was an independent positive association of AKI with abdominal pain, tenderness and vomiting, cellulitis, myalgia, and black or brown urine (P < 0.05), as well as and bleeding tendencies, while neurological features had an inverse relation for the development of AKI. Hypotension on initial presentation did not show a positive association with AKI in our study.
Table 2.
Clinical features of snake bite patients with and without acute kidney injury*
Discussion
In our study, we studied the demographic and clinical predictors of developing AKI in snake bite victims. Males were more commonly the victims of snake bites, probably due to their more outdoor activities in the field. However, there was no significant association of gender of the patient and development of AKI after snake bite (P > 0.05). Patients who developed AKI were mostly older than those who did not develop AKI (34 ± 1.64 vs. 32 ± 1.62) (P < 0.05). Athappan et al.[4] also found an increased incidence of AKI in older age group. This could be due to declining renal reserve with age.
Our snake bite patients hailed predominantly from the rural population as Barabanki is predominantly an agricultural district and people working in the fields are more exposed to snakes. However, the development of AKI was not significantly related to residence of the patient independently as compared to other factors.
An important observation was that significant number of patients (42.75%) took nonmedical treatment before coming to the hospital demonstrating the prevalent customs in the population. This is an important contributing factor for the development of various complications of snake bite including renal failure because of prolongation of bite to ASV time.
Increased time interval between bite to the administration of ASV (bite to needle time) had a direct correlation with the development of AKI (P < 0.05). Delay in administration of ASV increases the risk of developing AKI. The venom continues to produce damage until it is neutralized. Athappan et al.[4] and Reid[5] found that early administration of anti-venom could reverse all clinical manifestations of snake bite. Causes of delay in seeking proper medical treatment could be due to lack of awareness of importance of early medical treatment of snake bite patients and consulting local healers using charms and other nonmedical treatment in snake bite as well poor transportation facilities in rural areas. The majority of snake bite victims in villages are initially treated by professional snake bite healers, snake charmers, and religious men, who use herbal remedies, chant divine mantras, and apply snake stone causing delay in seeking medical aid.[4] Hence, early transfer of the patient to a health-care facility where ASV can be given is important.
Snakes that cause renal failure are either myotoxic or hemotoxic but venom may have direct nephrotoxicity.[6] Among land snakes, there are five important venomous species in India.[4] They are neurotoxic Elapidae, including common Cobra (Naja naja), King Cobra (Ophiophagus hannah), and Krait (Bungarus caeruleus, Bungarus fasciatus); and vasculotoxic Viperidae, Russell's viper (Daboia russelii), and saw-scaled viper (Echis carinatus).[3] Acute renal failure is an important complication of Russell's viper and saw-scaled viper species of snakes in India.[7] Up to 70% of the protein content of viper venom is phospholipase A2, present in the form of at least seven isoenzymes.[8] Possible clinical effects of the enzyme include hemolysis, rhabdomyolysis, presynaptic neurotoxicity, vasodilatation and shock, release of endogenous autacoids, and interaction with monoamine receptors.[8] Interestingly, Warrell[8] found geographical variation in the clinical manifestations, reflecting differences in venom composition.
In our study, we noticed that those patients who subsequently developed acute renal injury had predominant complaints of GIT symptoms such as abdominal pain, tenderness, and vomiting. Abdominal pain, thought to be caused by submucosal hemorrhages in the stomach, has long been recognized as an important and early symptom of venomous snake bite.[9,10,11] Abdominal pain and vomiting may denote severity of envenomation.[12] Vomiting can be a part of autonomic symptoms of snake bite. Jorge et al. 1997[13] report severe envenomation is associated with several autonomic symptoms such as vomiting, nausea, sweating, and abdominal colic. Kalantri et al.[11] found that risk of death was six times higher for those snake bite patients with a history of vomiting.
Why venom causes autonomic symptoms of vomiting and abdominal colic? It seems possible that snake venom which causes nephrotoxicity affects the autonomic system due to the fact that postganglionic parasympathetic neurons are unmyelinated. Hence, toxin may directly affect these neurons leading to parasympathetic stimulation resulting in vomiting and abdominal colic. Similarly, it is quite possible that stimulation of postganglionic sympathetic neurons may give rise to ischemic nephropathy leading to acute renal shutdown.
Cellulitis was another important symptom associated with the development of AKI (P < 0.05). Local cellulitis is an important finding in most of the venomous bites except krait, which causes neurotoxicity.[11] In fact, in viper bites, it is the earliest symptom and viper is known to cause renal failure.
We also observed that severe body ache and myalgia had a significant relationship in developing renal failure (P < 0.05). Myotoxicity due to snake venom can be responsible for generalized myalgias. Similarly, black/brown colored urine (coca cola colored urine) was present in 36 out of 62 (58.06%) cases who developed renal failure. Paul and Dasgupta[14] and Vanholder et al.[15] also observed that dark black or brown urine was strongly related to AKI. These symptoms can be attributed to muscle damage (rhabdomyolysis) due to snake venom and are important predictors of developing renal injury as a result of myoglobin accumulation in the renal tubule. Black/coca cola colored urine is a sign of myoglobinuria indicative of muscle breakdown.
In our study, 31 out of 62 (50%) patients who developed ARF had bleeding tendencies in the form of epistaxis, hemoptysis, and malena. This is indicative of venom-induced coagulopathy or thrombocytopenia. Intravascular hemolysis due to phospholipase A2 is a significant factor in the pathogenesis of snake bite-induced AKI.[3] The most common coagulopathy in snake bite is venom-induced consumption coagulopathy (VICC) which results from activation of the coagulation pathway by snake toxins.[16] In a proportion of patients with VICC, a clinical syndrome consistent with thrombotic microangiopathy has been reported, and it is characterized by acute renal failure, thrombocytopenia, and microangiopathic hemolytic anemia.[16]
Hypotension is also an important risk factor for the development of renal failure. Russell's viper can cause hypotension by releasing bradykinin.[4] This leads to prerenal insult. However, in our study hypotension on presentation did not have statistically significant predictive value for the development of AKI (P > 0.05), probably because we were aggressive in correcting it.
We also observed that in our study, neurological toxicity was inversely related with the development of AKI. This could be due to low prevalence in our region of snakes which cause both neurotoxicity and kidney injury (e.g., sea snakes),[17] and also pure neurotoxic snakes do not cause renal injury.
Conclusion
We found that early clinical predictors for the development of AKI in snake bite patients are marked abdominal pain, tenderness and vomiting, myalgias and black or brown urine, as well as prolonged(>2 h) bite to ASV time, cellulitis, bleeding tendencies. More research is needed to validate these findings, especially to find correlation of these symptoms with the development of AKI so that early identification of prognostic risk factors and proper timely management may reduce patient's morbidity and mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank Dr. Prashant Kumar Bajpai, Department of SPM, KGMU, Lucknow for helping us with the statistical analysis of the data.
References
- 1.Mohapatra B, Warrell DA, Suraweera W, Bhatia P, Dhingra N, Jotkar RM, et al. Snakebite mortality in India: A nationally representative mortality survey. PLoS Negl Trop Dis. 2011;5:e1018. doi: 10.1371/journal.pntd.0001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patil TB, Bansod YV, Patil MB. Snake bite induced acute renal failure: A study of clinical profile and predictors of poor outcome. World J Nephrol Urol. 2012;1:59–65. [Google Scholar]
- 3.Dharod MV, Patil TB, Deshpande AS, Gulhane RV, Patil MB, Bansod YV. Clinical predictors of acute kidney injury following snake bite envenomation. N Am J Med Sci. 2013;5:594–9. doi: 10.4103/1947-2714.120795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Athappan G, Balaji MV, Navaneethan U, Thirumalikolundusubramanian P. Acute renal failure in snake envenomation: A large prospective study. Saudi J Kidney Dis Transpl. 2008;19:404–10. [PubMed] [Google Scholar]
- 5.Reid HA. Myoglobinuria and sea-snake-bite poisoning. Br Med J. 1961;1:1284–9. doi: 10.1136/bmj.1.5235.1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chugh KS, Aikat BK, Sharma BK, Dash SC, Mathew MT, Das KC. Acute renal failure following snakebite. Am J Trop Med Hyg. 1975;24:692–7. doi: 10.4269/ajtmh.1975.24.692. [DOI] [PubMed] [Google Scholar]
- 7.Chugh KS. Snake-bite-induced acute renal failure in India. Kidney Int. 1989;35:891–907. doi: 10.1038/ki.1989.70. [DOI] [PubMed] [Google Scholar]
- 8.Warrell DA. Snake venoms in science and clinical medicine 1.Russell's viper: Biology, venom and treatment of bites. Trans R Soc Trop Med Hyg. 1989;83:732–40. doi: 10.1016/0035-9203(89)90311-8. [DOI] [PubMed] [Google Scholar]
- 9.Theakston RD, Phillips RE, Warrell DA, Galagedera Y, Abeysekera DT, Dissanayaka P, et al. Envenoming by the common krait (Bungarus caeruleus) and Sri Lankan cobra (Naja naja): Efficacy and complications of therapy with Haffkine antivenom. Trans R Soc Trop Med Hyg. 1990;84:301–8. doi: 10.1016/0035-9203(90)90297-r. [DOI] [PubMed] [Google Scholar]
- 10.Kularatne SA. Common krait (Bungarus caeruleus) bite in Anuradhapura, Sri Lanka: A prospective clinical study, 1996-98. Postgrad Med J. 2002;78:276–80. doi: 10.1136/pmj.78.919.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalantri S, Singh A, Joshi R, Malamba S, Ho C, Ezoua J, et al. Clinical predictors of in-hospital mortality in patients with snake bite: A retrospective study from a rural hospital in central India. Trop Med Int Health. 2006;11:22–30. doi: 10.1111/j.1365-3156.2005.01535.x. [DOI] [PubMed] [Google Scholar]
- 12.Warrell DA. Guidelines for the clinical management of snakebites in the South East Asian regions. Southeast Asian J Trop Med Public Health. 1999;30:1–84. [Google Scholar]
- 13.Jorge MT, Sano-Martins IS, Tomy SC, Castro SC, Ferrari RA, Ribeiro LA, et al. Snakebite by the bushmaster (Lachesis muta) in Brazil: Case report and review of the literature. Toxicon. 1997;35:545–54. doi: 10.1016/s0041-0101(96)00142-0. [DOI] [PubMed] [Google Scholar]
- 14.Paul J, Dasgupta S. Early prediction of acute kidney injury by clinical features of snakebite patients at the time of hospital admission. N Am J Med Sci. 2012;4:216–20. doi: 10.4103/1947-2714.95903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vanholder R, Sever MS, Erek E, Lameire N. Rhabdomyolysis. J Am Soc Nephrol. 2000;11:1553–61. doi: 10.1681/ASN.V1181553. [DOI] [PubMed] [Google Scholar]
- 16.Isbister GK. Snakebite doesn’t cause disseminated intravascular coagulation: Coagulopathy and thrombotic microangiopathy in snake envenoming. Semin Thromb Hemost. 2010;36:444–51. doi: 10.1055/s-0030-1254053. [DOI] [PubMed] [Google Scholar]
- 17.Sitprija V, Boonpucknavig V. Snake venoms and nephrotoxicity. In: Lee CV, editor. Snake Venoms. New York: Springer-Verlag Berlin Heidelberg; 1979. pp. 997–1018. [Google Scholar]


