Abstract
Objective:
Translation of evidence into practice by health systems can be slow and incomplete and may disproportionately impact disadvantaged populations. Coronary heart disease is the leading cause of death among Aboriginal Australians. Timely access to effective medical care for acute coronary syndrome substantially improves survival. A quality-of-care audit conducted at a regional Western Australian hospital in 2011–2012 compared the Emergency Department management of Aboriginal and non-Aboriginal acute coronary syndrome patients. This audit is used as a case study of translating knowledge processes in order to identify the factors that support equity-oriented knowledge translation.
Methods:
In-depth interviews were conducted with a purposive sample of the audit team and further key stakeholders with interest/experience in knowledge translation in the context of Aboriginal health. Interviews were analysed for alignment of the knowledge translation process with the thematic steps outlined in Tugwell’s cascade for equity-oriented knowledge translation framework.
Results:
In preparing the audit, groundwork helped shape management support to ensure receptivity to targeting Aboriginal cardiovascular outcomes. Reporting of audit findings and resulting advocacy were undertaken by the audit team with awareness of the institutional hierarchy, appropriate timing, personal relationships and recognising the importance of tailoring messages to specific audiences. These strategies were also acknowledged as important in the key stakeholder interviews. A follow-up audit documented a general improvement in treatment guideline adherence and a reduction in treatment inequalities for Aboriginal presentations.
Conclusion:
As well as identifying outcomes such as practice changes, a useful evaluation increases understanding of why and how an intervention worked. Case studies such as this enrich our understanding of the complex human factors, including individual attributes, experiences and relationships and systemic factors that shape equity-oriented knowledge translation. Given the potential that improving knowledge translation has to close the gap in Aboriginal health disparities, we must choose strategies that adequately take into account the unique contingencies of context across institutions and cultures.
Keywords: Knowledge translation, implementation science, Aboriginal Australians, indigenous, Aboriginal and Torres Strait Islanders, health equity, coronary heart disease, acute coronary syndrome, case studies
Background
Many Aboriginal and Torres Strait Islander Australians (hereafter, the term ‘Aboriginal’ is used to refer to the Aboriginal and Torres Strait Islanders peoples of Australia) experience worse health outcomes than non-Aboriginal Australians.1 Coronary heart disease (CHD) is currently the leading cause of death among Aboriginal Australians, with disproportionately high rates across all age groups (most marked in younger people) contributing to reduced life expectancy and the destructive flow-on effects of debilitating disease.2–4
Evidence highlights the substantial impact of timely access to effective medical care on the survival of individuals experiencing acute coronary syndrome (ACS).5,6 Early and appropriate treatment is important to reduce mortality,7 permanent myocardial damage8 and complications after discharge.9 Failure to implement this evidence into practice is particularly pertinent in the context of Aboriginal health. Failure to ensure timely or effective medical care to Aboriginal ACS patients can usefully be examined as a knowledge-to-action gap, that is, one contributor to a broad range of determinants of Aboriginal health disparities. This gap may well be a manifestation of institutionalised racism within the Australian health system10,11 that works in conjunction with Aboriginal disadvantage shaped by a historical legacy of dispossession and discrimination which continues to impact on Aboriginal health.1 Therefore, developing, evaluating and sharing knowledge translation (KT) strategies that benefit disadvantaged populations are essential to address health inequity.
The Bettering Aboriginal heart health in Western Australia (BAHHWA) project investigates the ways in which the health system, multiple comorbidities, socio-economic factors and cultural differences interact to perpetuate poor health outcomes for Aboriginal Western Australians. Different aspects of the research have investigated frequency and outcomes of cardiovascular disease (CVD), the kind of care Aboriginal patients receive compared with non-Aboriginal patients, the experiences of Aboriginal people receiving care for CVD3,12–15 and enablers and barriers in health system change.16 Investigation of strategies that facilitate or impede KT is a core component of the project.
Knowledge Translation (KT)
The gap between evidence and practice in healthcare is a problem globally, with a diverse range of services failing to deliver evidence-based care.17,18 It has also been recognised that the impact of suboptimal care disproportionately affects disadvantaged populations.19,20 The field of KT has provided an important focus to understanding how evidence can be successfully and universally implemented into practice.21
KT has been defined by the Canadian Institutes of Health Research as
the exchange, synthesis and ethically sound application of knowledge – within a complex system of interactions among researchers and users – to accelerate the capture of benefits of research … through improved health, more effective services and products, and a strengthened health care system.22
The term KT has become widely used in the last 20 years (for discussion of the history and development of KT theory, as well as debates around differing models, see Davison23), with a range of frameworks developed and general principles formulated.24 Initially concerned with improving the incorporation of research discoveries into day-to-day clinical care,25 the field has more recently broadened to include an additional translational step from health practice to population health outcomes.26
There is no consensus regarding the best methods of implementing new knowledge across varied health service contexts. As a consequence, KT theory is inherently interdisciplinary as it attempts to account for the diverse and often unpredictable factors involved in implementing changes to health service delivery.27 As interventions often involve context-specific elements, the potential for generalised extrapolation of methods and principles can be limited. Implementation of new initiatives can be inhibited by structural, geographical, organisational and professional barriers and by professional–patient interactions.27
Within the continuum of research evaluating the effectiveness of KT approaches, this article explores the enablers and barriers in implementing interventions in real-world settings.28 This type of health policy and systems research investigates clinical and public health policies, programmes and practices, in order ‘to understand not only what is and isn’t working, but how and why implementation is going right or wrong, and testing approaches to improve it’ (p. 27).29 The translation of audit data into practice change, supplemented with information reflecting perspectives from practitioners experienced in these processes, is examined here as a case study, with the aim of contributing to knowledge of the factors involved in the implementation of evidence, particularly in areas of health inequity.
Clinical guidelines audits
There is evidence across many clinical contexts that adherence to clinical guidelines is a determinant of patient outcomes. That is, when adherence improves, so do morbidity and mortality outcomes.6,30–33 Clinical guidelines help service providers to be aware of current recommendations for practice and can be used as the basis for specifying benchmarks and measuring performance. Audits can encourage and assist the use of guidelines thereby relating evidence to practice, and as such are ‘potentially invaluable in assisting both clinicians and administrators … in meeting both quality and business objectives through cost-effective, integrated care’ (p. 203).34 Guideline-based audit processes demonstrably prompt fidelity to evidence,35 by providing the feedback necessary to implement and maintain small but potentially important improvements in care.36,37 Audit and feedback processes are likely to be particularly valuable for assessing the circumstances of disadvantaged patients who may be less likely and able to recognise suboptimal care or to utilise complaint mechanisms to ensure deficiencies are addressed. Information from audits is therefore important in supporting advocacy on behalf of these populations.
This article presents a case study to support learnings regarding how evidence can be used to produce change, with a particular focus on the process by which an Emergency Department (ED) audit at a regional (non-metropolitan) Western Australian hospital was translated to change practice. Western Australia (WA) is a geographically vast state, covering a third of the landmass of Australia; yet, only 11% of the population reside there. More than three quarters of the Western Australian population reside in metropolitan Perth with the rest of state having very low population density. This has a significant impact on the health system and patterns of care, presenting many challenges in healthcare delivery. Regional hospitals receive patients from all over their particular region, including referrals from smaller district hospitals. Specialist services in rural areas are limited, with patients often requiring transfer by aeroplane to tertiary hospitals in distant Perth. Treatment and referral pathways appropriate for each region are thus central to the appropriate treatment of patients. In the study hospital, a regional emergency chest pain pathway existed for the investigation and treatment of patients presenting with chest pain. This pathway closely follows the recommendations of Australian national guidelines.38
The details of the audit process which form the basis of this case study are reported elsewhere39 and reflect typical hospital medical audit approaches, whereby the management of a series of cases is compared to a current clinical management pathway. As audits are undertaken as a quality improvement activity, feedback to relevant clinicians involved is an expected component of the undertaking. The audit had arisen in the context of a supervised specialist public health physician training placement and was designed in collaboration with a local university centre with an interest in Aboriginal disparities and CVD and a regional public health physician. In developing the audit protocol, members of the regional health service staff were consulted, including the Medical and ED Directors. The audit data collection and analysis were undertaken in 2011–2012 by the public health medicine registrar (the principal investigator (PI)) employed by the Western Australian Country Health Service (WACHS).40 As with all quality improvement, a follow-up audit using the same protocol was completed 2 years later (in 2014) to assess changes, and a report summarising the results was submitted to the Western Australian Department of Health in the same year.41
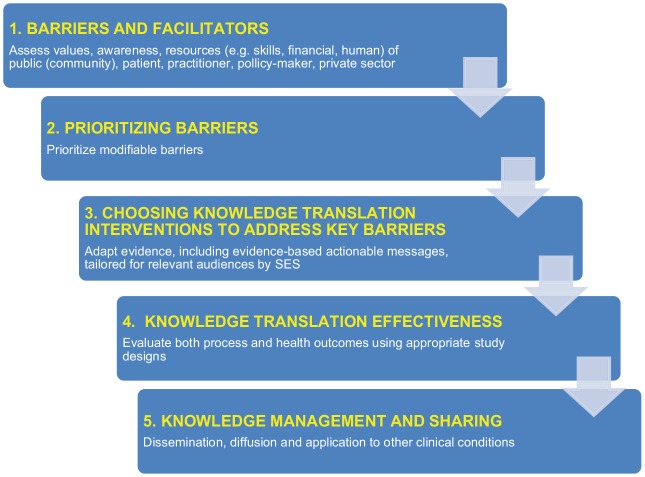
Both audits measured quality of care and outcomes for patients who presented to the hospital with symptoms of ACS, in order to assess the following: (1) adherence to ACS management guidelines and (2) differences in management of Aboriginal and non-Aboriginal people with regard to adherence to the guidelines.40 The first audit (2011–2012) identified systemic deficiencies in the way ACS was managed in the hospital for both Aboriginal and non-Aboriginal patients and provided evidence that Aboriginal people were less likely to receive recommended interventions. The second audit (2013–2014) documented a general improvement in adherence to the pathway and a reduction in the gap in care of Aboriginal presentations. In this case study, we analyse the process of undertaking these audits and translating results of the original audit into intervention, using the lens of a relevant KT framework, the cascade for equity-oriented KT proposed by Tugwell et al.20 (Figure 1).
Figure 1.
Tugwell et al.’s20 cascade for equity knowledge translation.
Source: Adapted from original.
Method
Equity-oriented KT is concerned with disparities in provision of care between different groups and thus the ‘ethically sound application of knowledge’.22 While Tugwell et al.’s20 framework was originally designed to support the translation of evidence from randomised controlled studies to community settings, it was useful for this case study because of its focus on inequity in health outcomes. This framework emphasises the following: (1) the importance of locating barriers and facilitators to equity in KT, (2) prioritising key barriers, (3) choosing KT interventions to address those barriers, (4) evaluating KT effectiveness and (5) documenting and sharing what was found to be effective.20
A case study approach is appropriate here42 as KT is a largely context-dependent process where ‘interventions cannot be taken on their own without considering the characteristics of the knowledge that was being transferred, providers, participants and organizations’.43 Case studies are a well-established social research method,44,45 effective in generating ‘an in-depth, multi-faceted understanding of a complex issue in its real-life context’.46
Data were collected using semi-structured, face-to-face or telephone interviews, conducted by the first author (E.H.) with a purposive sample of four members of the team associated with the conception, development and conduct of the audit. The restriction of the sample to people closely associated with the audit reflects a research focus on the enablers and barriers to organisational- and/or system-level support for practice changes.47 The interviews were conducted after the first audit and lasted between 45 and 60 min and were transcribed from notes or audio recordings. They were then analysed thematically and coded for alignment with the themes outlined in the steps of Tugwell et al.’s20 theoretical framework (Figure 1). The interviewees comprised the PI, the Regional Director of Medical Services, the regional public health physician and an academic public health physician who co-supervised the PI’s research project. Two other hospital staff with some involvement in the audit declined to participate because of time constraints. Interviews explored participants’ experience of the knowledge exchange and translation processes involved in the audit and how the results were acted upon.
Interviewee data were triangulated with the findings from semi-structured interviews with key informants (n = 7) who had identified themselves as having interest/experience in KT in Aboriginal health at an Aboriginal heart health forum. Additional information was drawn from informal discussions with other stakeholders, including from the cardiovascular policy area of the Department of Health and from professionals closely associated with clinical service delivery. Interviewees were given opportunities to correct and comment on both interviews and the analysis presented in this case study. The research team also documented evidence of changes to ACS management in the study hospital occurring after the results of the first audit were reported back to policymakers and management. Representative quotes are reported below with a unique number and coding to reflect the sample, that is, either audit team (AT) or key stakeholder (KS). In total, there were seven women and four men. All were health professionals, most in managerial or policy positions. Four were located in the regional area.
This study was undertaken in the context of a large cardiovascular health services research project that focussed on disparities in Aboriginal CVD. The research received ethics approval from the Western Australian Aboriginal Health Ethics Committee (381-01/2011), WACHS and The University of Western Australian Human Research Ethics Committee (Reference number: 2011/89).
Results
Interview findings are presented in accordance with the steps described by Tugwell et al.20 (Figure 1), summarised in Table 1.
Table 1.
Summary of areas of key correspondence between the Tugwell cascade and KT processes following the Aboriginal ACS patients’ treatment audit.
| Cascade for equity knowledge translation20 | Case study of knowledge translation following audit of treatment of Aboriginal ACS patients at a regional hospital |
|---|---|
| 1. Assess barriers and facilitators | ● Existing partnerships establish rationale and guide planning ● Engagement of stakeholders at multiple levels of organisation, using multiple approaches ● Build confidence in a research team that is skilled in addressing barriers ● Alignment of the PI’s clinical and technical knowledge with the task |
| 2. Prioritise barriers to address | ● Priority given to engaging key stakeholders ● Prioritising based on awareness of hierarchies, timing and personal relationships ● Use of a local, small-scale audit. Findings were actionable at local level but revealed wider system issues to be addressed ● Recommendations presented to highlight actions that were essential and achievable |
| 3. Choose knowledge translation (KT) interventions to address key barriers | ● Findings tailored for presentation to appropriate stakeholders ● Hospital management was advised of audit results and recommended changes prior to wider dissemination ● Management invited to respond with strategies to address the issue ● Develop and build on partnerships ● Recognise significance of KT facilitator role |
| 4. Assess KT effectiveness | ● A collaborative process has been established ● Follow-up concluded that there had been a general improvement in adherence to the pathway and a reduction in inequalities in the treatment of Aboriginal presentations, but emphasised the continuing need for improvement to optimise the management of ACS in this setting ● Analysis needed to better understand why/how this process worked as an intervention |
| 5. Knowledge management and sharing | ● Study findings provided to WACHS and hospital management ● Process, findings and recommended actions presented at conferences ● Journal publication after completion of a follow-up audit ● Follow-up audit shows institutional commitment to ongoing collaboration |
ACS: acute coronary syndrome; PI: principal investigator; WACHS: Western Australian Country Health Service.
Barriers and facilitators
Institutional factors were considered the most significant source of potential barriers or facilitators to conducting the audit and implementing recommendations. Prior to commencement of the research, the research team recognised a range of potential responses to the proposed audit. While these included positive attitudes, potentially significant barriers were recognised, including institutional apathy and concern for possible consequences of findings, particularly in the context of a regional health service with high workforce turnover and long-term staff lacking clear incentives to alter behaviour.
One participant observed that while ‘decision-makers get that they have to do something differently’, it was considered a logistical challenge to ‘fit the important stuff into bureaucratic constraints’ (KS2). Consequently, interviewees spoke of the importance of identifying more than one area for action, recognising that ‘opportunities for change might not arise for a while’ (KS2). A KS described how after ‘five or six years’ of advocacy for system-level improvements ‘suddenly this thing just swung into action’ and everything changed (KS3).
A number of key facilitators were used by the AT to moderate potential institutional barriers. Prior to the audit being developed, groundwork had been done to make the managerial environment more conducive to targeting Aboriginal cardiovascular health outcomes. One strategy was the engagement of the Cardiovascular Health Network (CHN), a state-funded collaborative policy group located within the health department aimed at improving patient-centred care and clinical interventions for CVD. The importance of the CHN role was described by a member as strategic, pulling ideas together, providing support and facilitation to ‘make sure actions happen … support is what makes all the difference’ (KS2). As a result of collaboration in the BAHHWA project, the CHN, WACHS and the BAHHWA investigators had an established partnership that had supported an ongoing dialogue about the policy environment and disparities in outcomes and care, identifying potential opportunities for overcoming deficiencies. The experiences of group members involved in similar processes of using audits to prompt change, including the challenge associated with getting hospital agreement to conduct an audit in the first place, were drawn on. Additionally, this supportive collaboration meant that by participating in the audit, the hospital could be seen as contributing to a statewide understanding of factors contributing to Aboriginal heart health disparities, as well as disparities between rural and metropolitan qualities of cardiovascular care.
While permissions had been obtained at multiple levels within the hierarchy of hospital management and local Health Department Executive prior to beginning the audit, it was critical for administrators to have confidence in both the personnel and processes involved in the audit. Importantly, the hospital administrators had sufficient confidence in the expertise of the AT, ensuring a broad acceptance among stakeholders of the audit process. It was recognised that having a team may be critical, as ‘you can’t do it on your own, you need a group of people … a motivated team’ (KS2) and change requires ‘the right people to pick up and run with [it] to make things happen’ (KS3). The medically qualified PI had recent tertiary clinical experience in emergency care and treatment of ACS presentations, with sound technical knowledge and experience of treatment pathways that members of the Regional Executive (RE) lacked. Several members of the team were experienced with development and use of clinical management guidelines, ensuring that there was awareness of the challenges involved in sustaining system change at the point of service.
In addition, interpersonal skills were an important factor in reducing potential barriers when engaging stakeholders. Several interviewees commented on the PI’s conscientious approach and moderate manner, reflecting the importance of his careful deliberation and consultation. Similarly, the presentation of relevant data to stakeholders in a manner that was appropriate, concise and unthreatening helped as it reflected a professional and familiar mode of communication.
Prioritising barriers
In the context of the ‘wicked’ longstanding challenge of improving care for Aboriginal patients,48–50 it was recognised that institutional-level changes that were long-term and multifaceted were needed. ‘You certainly need priorities … [to] decide what are the most important issues to tackle and then what are the best ways to tackle that’ (KS2). Particularly, for system-level problems to be addressed, ‘working out workable solutions’ for potentially ‘defensive’ staff was regarded as important (KS3). Additionally, prioritising particular parts of the system was important, ‘the thing I would really like to see is more executive level engagement … really, to get widespread change we do need people at the top to be passionate’ (KS2). This requires being strategic in identifying and working with those who ‘get it’, as opposed to those might ‘sound quite plausible’ in their talk but have limited real understanding (KS2). Despite successful actions, often arising from the efforts of committed ‘champions’, the perception was that change requires ‘a bit of clout’ at an organisational level, with ‘key players at the same level around the table’ (KS3). As described by one KS, ‘there is more power in a group’ … ‘everybody was there, it was everybody’s problem … so you [individuals] couldn’t wriggle out of it’ (KS3).
Restricting the audit to one hospital was a practical decision based on resource availability. While this has implications for the generalisability of the audit results, it is an important finding of the case study.This focus was perceived as beneficial in lessening the possibility of the hospital resiling from making recommended changes. That is, the team was aware from the start that localised, small-scale research identifying local, practical and targeted correctives may be more likely to give rise to change than statewide research recommending broader health system reform. Additionally, stakeholders’ awareness of the fact that other audits51,52 and the statewide administrative data analysed by BAHHWA researchers had found similar disparities in treatment15 gave the audit results increased legitimacy, and in raising a wider, systemic problem for which solutions were evident, enabled the hospital to be a leader of reform. Having strong data to prompt change within hospital settings was also identified as important in the supplementary interviews:
the sort of thing you can really almost shock people with, because they do realise it’s an issue, but they might not realise the magnitude of the problem … we certainly have to drive them with the data [until they] have an interest in their health service performing better. (KS2)
In the case of the audit, the sample size (across a full year and including all Aboriginal chest pain presentations to the ED, more than 300 ACS presentations) was sufficiently large to provide meaningful results that required an institutional response.
Choosing KT interventions to address key barriers
In this case study, the AT used two key strategies to address identified barriers: the selection of modifiable problems and carefully crafted communication. From the start, the AT concentrated on how best to maximise uptake of their findings, rather than simply exposing institutional failure. A diplomatic process was considered to be as necessary to improving performance as the clear presentation of findings. Provision of results and advocacy had to be undertaken with awareness of the institutional hierarchy, appropriate timing and emphasising the importance of personal relationships. It was important to tailor messages to the relevant audience, promoting the importance of using the information to improve the quality of patient care and prioritising action to address modifiable barriers.
The PI described the need to be sensitive to context when presenting findings to appropriate stakeholders; he was respectful of seeking permission to present the findings to outside agencies and of not naming the regional health service in any presentations. As a result, the PI chose to present early findings from the audit to the hospital’s Director of the ED for feedback on what recommendations might be included with the results and to clarify any issues to ensure accuracy. A week before the results were presented to the RE of the State Health Department, two of the investigators, including the PI, met with the two key directors on the Executive, in order to forewarn them of the audit findings and potential recommended changes. When subsequently presenting the data to the whole committee, the PI highlighted only the recommendations that they could influence directly as too many recommendations can dilute the incentive to initiate change. Having been prepared, the Medical Director was able to respond immediately by outlining strategies to address the issue.
This refining of the message, or effective communication, was a common theme. Other respondents also discussed the importance of prioritising key findings by limiting communication to three major recommendations from their research, ‘collect, collate and summarise what is most important in your thinking’ (KS1).
KT effectiveness
The follow-up audit allowed comparison of changes between 2011-2012 and 2013-2014 in the quality of care provided for patients presenting with ACS and differences between Aboriginal and non-Aboriginal patients. It identified that there had been a general improvement in adherence to the pathway and a reduction in inequalities in the treatment of Aboriginal presentations. However, the findings underscored the continuing need for improvement to optimise the management of ACS in this setting.41 The detailed findings from the audit process are reported elsewhere.39
These changes can be assumed to at least in part be the result of recommendations and feedback to the RE from the first audit. These resulted in specific practical outcomes which have been and continued to be implemented:
Access to timely exercise stress tests improved, with publicly funded tests now provided regularly by a visiting cardiology team. This occurred in response to the need to improve stress test referrals for diagnostic assessment; at the time of the first audit, there had been nowhere for patients without private health insurance to have publicly funded stress tests conducted within the recommended time frame (within 72 h). Patients who could not access a private stress test faced an extended wait or did not receive this assessment. As Aboriginal patients are overwhelmingly without private health insurance and often have low incomes they had less access to guideline-directed diagnostic testing, which is essential in for optimal ongoing management.
There was more rigorous implementation of the latest best-practice pathway. The hospital employed ED specialists to improve the quality of management for all ED patients, including those with ACS. Even with ongoing turnover of staff, guideline-adherent management of ACS presentations is likely to be applied more consistently, particularly as these changes have been supported by small, regular internal audits to review performance and provide feedback and education to staff utilising the pathway. Additionally, the increase in number of Senior Medical Officers employed will improve the stability of rostering.
The current ACS pathway was modified for WACHS services by the CHN to allow clinicians to stratify risk more accurately and thereby determine appropriate investigations and treatment. The audit was referred to in this process. The current pathway plan was also to be adjusted to improve information flow and clarity with a new Director of the ED at the hospital planning to provide input into this review and ensure implementation of the new and improved pathway when available.
A specialist general physician (internist) highly experienced in providing health services for Aboriginal communities was employed by the hospital to visit four times per year to train the staff. This training was to improve the confidence and abilities of clinicians in their treatment and management of Aboriginal patients.
Knowledge management and sharing
The final step of the cascade describes the iterative nature of the KT/exchange process. A written report on the findings was provided to WACHS and presented to hospital management.40 Audit findings were also presented at conferences and at research translation forums organised by the BAHHWA team and prepared for publication in a peer-reviewed journal. Consequently, the approach has garnered attention beyond the local health service, also prompting the WA Health Department review of the rural chest pain pathway statewide. Finally, this article itself represents a key part of this step: reflecting on lessons learnt from this case study can inform future KT practices in suitable contexts. As observed by a Health Department interviewee, there is not a lot of intervention study available, so being able to demonstrate ‘what works’ is likely to be influential. And hope was expressed that the case study of the audit would be used to prompt other hospitals to ask ‘Do we do that too?’ (KS2). The challenge of attribution (knowing which of many factors contributed to changes) was also recognised.
Discussion
This case study used the framework created by Tugwell and colleagues to examine why and how a quality-of-care audit conducted at a regional Western Australian hospital worked to implement change in ACS management at the study hospital. Using a health equity perspective to focus on disparities in the ED management of Aboriginal and non-Aboriginal ACS patients, the most important steps within the framework were found to be as follows:
The collaborative work undertaken prior to the audit being developed that helped shape a managerial environment conducive to targeting Aboriginal cardiovascular health outcomes;
The tailoring of messages to the relevant audience, including the need to be aware of the institutional hierarchy, appropriate timing and personal relationships needed in provision of results and advocacy for change;
The identification and prioritisation of practices that were modifiable.
These strategies resulted in acknowledgement at both personal and institutional levels of responsibility for reducing identified health inequalities. This is particularly important in a health system where, despite the rhetoric of cultural competency and policies requiring healthcare services to meet the needs of Aboriginal patients, the combination of structural racism and outright failure to recognise the legitimacy of these needs ensures ‘business as usual’ is not questioned.61 The finding from the second audit showed a general improvement in adherence to the pathway and a reduction in disparities between Aboriginal and non-Aboriginal presentations, suggesting that the process of feeding back the first audit results was successful in generating change.
Although frameworks for knowledge exchange and translation are emerging, there is a dearth of case studies that explore the operation of such frameworks in practice. The BAHHWA research had an explicit focus from its inception on KT, and given our interest in achieving greater health equity, we have utilised the framework of Tugwell and colleagues to examine its application. As well as identifying outcomes, such as practice changes, a useful evaluation also attempts to understand why and how an intervention worked.23 As Table 1 demonstrates, there is good alignment between the processes surrounding the audit and the steps outlined in Tugwell et al.’s20 framework. Steps delineated by means of this framework in the process of developing and implementing the audit may be instructive for future similar KT interventions.
In addition to factors identified through the ‘lens’ of an equity-oriented KT framework,20 the case study demonstrates the importance of collaborative partnerships between researchers and health services. Also, particularly significant in this case, as reflected in the KS interviews, is the role of a KT champion, in this case, the PI. This corresponds with Greenhalgh et al.’s34 systematic review of the literature on innovation diffusion, which found individual champions were a key determinant of organisational innovation. These two elements are discussed in more detail.
Partnerships for change
The audit described here arose in the context of a supervised placement and was designed in collaboration with a University Department of Rural Health and a regional public health physician. In developing the proposal, members of the regional health service staff were consulted, including the Medical and ED Directors. The approval by hospital management of the second, follow-up audit can be seen as an indicator that the established collaborative process between the researchers and stakeholders was developed and strengthened. These collaborative processes accord with the experiences of others undertaking similar KT initiatives and reflect the relational or partnership factors identified by Davison23 as indicators to use in evaluating the success of a KT intervention: (1) improved communication channels and processes, (2) working relationships among stakeholders, (3) an ongoing forum for sharing among stakeholders, (4) opportunities for collaboration and (5) the creation of a shared vocabulary among stakeholders.
The iterative nature of audit and feedback processes means that partnerships between researchers and health services need to be ongoing. It is therefore important to understand the factors that can strengthen or derail the effectiveness of partnerships. In particular, understanding partnerships as activities between people and organisations that are complex, dynamic and subject to changes in power relations and essentially dependent on relationships.53 Masuda et al.54 argue that KT aimed at promoting health equity requires a focus on the relational aspects of knowledge construction, acknowledging ‘the relationship between knowledge and power … in knowledge production’ (p. 458). In the context of the ongoing discourse of institutional racism, it is important to form ‘collaborative knowledge relationships’ committed to ‘critical inquiry and reflexive practice’ (p. 463) that can inform actions at the institutional and political levels.54
Role of champions/facilitators/leaders
This case study highlights the importance of the role variously termed champion, facilitator or leader. While the role of the PI in this case was crucial during the audit itself, other people championed the project at different points in the planning, implementation and dissemination of the audit. This role was similarly identified as important in the KS interviews. Aarons et al.47 identify empirical evidence supporting the importance of the role of leaders in fostering change and innovation in the implementation process, including evidence that ‘relations-oriented’ leadership and organisational management processes, such as auditing and feedback/reminders, support guideline use. Similarly, Tsou et al.55 argue that in the context of partnerships for change, champions or facilitators with the skills and preparedness to cross traditional boundaries (referred to as ‘boundary spanners’ in a number of partnership discourses56–58), need to be nurtured and motivated. This is particularly important given a context where barriers to implementation are known to operate at multiple levels, and change agents are therefore required to work with a cross section of stakeholders at multiple levels in an institution.23 This role is also important in the context of health inequity as the champion is in effect an advocate for the disadvantaged population.
Evaluating KT strategies
This case study of an audit process as a KT strategy has demonstrated that the approach of the research team was effective because it was based on an understanding of the contextual factors and a careful, competent and respectful response to them. However, in different contexts, for example, where the institutional hierarchy is less inclined to develop collaborative relationships, aspects of the strategy may need to be different. This need to be responsive to context is an ongoing challenge in evaluating KT strategies; for example, LaRocca et al.’s43 systematic review concluded that no single KT strategy was effective across all contexts. Similarly, Scott et al.59 argue that shortcomings of research – such as equivocal results, poor methodological quality and outcome reporting bias – mean it is not possible to identify any one KT strategy as being more effective than any other. Despite these difficulties, developing, evaluating and sharing KT strategies that benefit disadvantaged populations, including the need for flexibility in different contexts, are essential components of achieving health equity.20
Given the substantial gap in knowledge and practice that could help overcome health disparities, identifying the themes and elements common to effective KT could help in better delivery of practical and systematic interventions. Although Tugwell et al.’s20 framework suggests that lessons from this case study can to some extent be extrapolated, differences in hospital size and culture, personalities and current practices will have distinctive influence over other contexts. The approach of the research team as described in this case study demonstrated a strategy that was effective, although this may not be possible to replicate in contexts where the institutional hierarchy is less inclined to develop collaborative relationships. Accurate evaluation of KT needs to account for the subjective experiences of participants. The unique contingencies of context cannot always be accounted for.
Study limitations
We did not interview all of the stakeholders involved in the audit and KT process. While this decision was in line with our focus on the key drivers of KT, it limits the article’s scope. We were unable to fulfil certain points of the consolidated criteria for reporting qualitative research (COREQ) checklist.60 The limitations of this investigation are also bound up with those of the audit: data were collected retrospectively, with findings reflecting routine documentation in medical records. Factors that were not well-documented could not be considered. The level of documentation improved in the period between the two audits, making difficult a comparative analysis over time, which is most dependent on detailed documentation. Finally, while Tugwell’s framework is useful for categorising and analysing data, it is a linear, mechanistic tool that is not necessarily very effective at explaining the lengthy and iterative nature of KT.
Conclusion
Evidence supporting the use of standardised KT interventions remains incomplete. However, case study analyses such as used in this article are valuable in not just describing outcomes such as practice changes but in developing understandings of why and how an intervention works. Reflection of lessons learnt to inform future KT practices is an important part of the iterative KT process.
Only recently have large Australian hospitals been attentive, and often in a limited way, to the needs of Aboriginal people.11 Given that disparities in treatment of individuals are at least in part due to lack of adherence to current guidelines, audit and feedback processes must consistently give consideration to potential inequalities in patient profiles and outcomes, combined with careful reflection and actions based on findings.
In particular, KT evaluation needs to account for context and the complex human factors (including both individual attributes and relationships) which inevitably shape equity-oriented KT. Case studies can enrich our understanding of the real-life contexts46 that shape the translation of evidence by clinicians, policymakers and health service managers. Given the potential that improving KT has to close the gap in Aboriginal health disparities, while general principles encoded in frameworks can guide KT processes, we must choose strategies that adequately take into account the unique contingencies of context across institutions and cultures. That is, analysis of the context-dependent components of individual cases should go hand in hand with attempts to formulate general principles for implementing change. We recommend additional qualitative studies that seek to account for the complex human interactions between barriers, facilitators and change agents – particularly important in settings where health equity is a concern. Given that no single KT strategy is likely to work across all contexts, the way forward is therefore to encourage both implementations and evaluations that promote flexibility, common sense and reflective approaches to KT.
Acknowledgments
The authors gratefully acknowledge the contribution of Marisa Gilles to this work and for comments on the manuscript. E.H. conceptualised and designed this study. She conducted interviews, wrote the paper and oversaw revisions. S.C.T. facilitated contact with the relevant participants and provided editorial advice. J.M.K. and S.C.T. contributed to the study design and editing of the final paper. B.D.S. conducted the audit that is the subject of this case study. H.H. assisted E.H. at the writing and reviewing stages. All authors critically reviewed the manuscript for important intellectual content and approved the final draft.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: The University of Western Australian Human Research Ethics Committee reference number: 2011/89.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Health and Medical Research Council of Australia (grant number 1031057). J.M.K. is funded by an NHMRC Early Career Fellowship (number 037429). The Western Australian Centre for Rural Health received funding from the Department of Health and Ageing.
Informed consent: Written informed consent was obtained from all subjects before the study.
References
- 1. Overview of Australian Indigenous health status, 2012, http://health.act.gov.au/sites/default/files/Overview%20of%20Aboriginal%20and%20Torres%20Strait%20Islander%20Health%20Status,%20HealthInfoNet,%202012.pdf
- 2. Australian Institute of Health and Welfare (AIHW). Contribution of chronic disease to the gap in adult mortality between Aboriginal and Torres Strait Islander and other Australians (Cat. no. IHW 48). Canberra, ACT, Australia: AIHW, 2010. [Google Scholar]
- 3. Katzenellenbogen JM, Sanfilippo FM, Hobbs MS, et al. Incidence of and case fatality following acute myocardial infarction in Aboriginal and non-Aboriginal Western Australians (2000–2004): a linked data study. Heart Lung Circ 2010; 19(12): 717–725. [DOI] [PubMed] [Google Scholar]
- 4. Vos T, Barker B, Begg S, et al. Burden of disease and injury in Aboriginal and Torres Strait Islander Peoples: the Indigenous health gap. Int J Epidemiol 2009; 38(2): 470–477. [DOI] [PubMed] [Google Scholar]
- 5. Lambert L, Brown K, Segal E, et al. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. JAMA 2010; 303(21): 2148–2155. [DOI] [PubMed] [Google Scholar]
- 6. Peterson ED, Roe MT, Mulgund J, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA 2006; 295(16): 1912–1920. [DOI] [PubMed] [Google Scholar]
- 7. Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324: 71–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Serruys PW, Simoons ML, Suryapranata H, et al. Preservation of global and regional left ventricular function after early thrombolysis in acute myocardial infarction. J Am Coll Cardiol 1986; 7(4): 729–742. [DOI] [PubMed] [Google Scholar]
- 9. The CAPRICORN Investigators. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet 2001; 357(9266): 1385–1390. [DOI] [PubMed] [Google Scholar]
- 10. Kelaher MA, Ferdinand AS, Paradies Y. Experiencing racism in health care: the mental health impacts for Victorian Aboriginal communities. Med J Aust 2014; 201(1): 44–47. [DOI] [PubMed] [Google Scholar]
- 11. Durey A, Thompson SC, Wood M. Time to bring down the twin towers in poor Aboriginal hospital care: addressing institutional racism and misunderstandings in communication. Intern Med J 2012; 42(1): 17–22. [DOI] [PubMed] [Google Scholar]
- 12. Katzenellenbogen JM, Sanfilippo FM, Hobbs MST, et al. Voting with their feet – predictors of discharge against medical advice in Aboriginal and non-Aboriginal ischaemic heart disease inpatients in Western Australia: an analytic study using data linkage. BMC Health Serv Res 2013; 13: 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Teng TH, Katzenellenbogen JM, Hung JM, et al. Rural-urban differentials in 30-day and 1-year mortality following first-ever heart failure hospitalisation in Western Australia: a population-based study using data linkage. BMJ Open 2014; 4(5): e004724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Teng TH, Katzenellenbogen JM, Thompson SC, et al. Incidence of first heart failure hospitalisation and mortality in Aboriginal and non-Aboriginal patients in Western Australia, 2000–2009. Int J Cardiol 2014; 173(1): 110–117. [DOI] [PubMed] [Google Scholar]
- 15. Lopez D, Katzenellenbogen JM, Sanfilippo FM, et al. Transfers to metropolitan hospitals and coronary angiography for rural Aboriginal and non-Aboriginal patients with acute ischaemic heart disease in Western Australia. BMC Cardiovasc Disord 2014; 14: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Haynes E, Katzenellenbogen JM, Woods JA, et al. Information for action: improving the heart health story for Aboriginal people in Western Australia (BAHHWA report). Perth, WA, Australia: Western Australian Centre for Rural Health, University of Western Australia, 2015. [Google Scholar]
- 17. Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care 2001; 39(8 Suppl. 2): 46–54. [DOI] [PubMed] [Google Scholar]
- 18. McGlynn E, Asch S, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003; 348: 2635–2645. [DOI] [PubMed] [Google Scholar]
- 19. Cunningham J, Cass A, Arnold PC. Bridging the treatment gap for Indigenous Australians. Med J Aust 2005; 182: 505–506. [DOI] [PubMed] [Google Scholar]
- 20. Tugwell P, Robinson V, Grimshaw J, et al. Systematic reviews and knowledge translation. Bull World Health Organ 2006; 84(8): 643–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Greenhalgh T, Robert G, Bate P, et al. How to spread good ideas: a systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation. London: National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO), 2004. [Google Scholar]
- 22. More about knowledge translation at CIHR, http://www.cihr-irsc.gc.ca/e/30739.html
- 23. Davison CM. Knowledge translation: implications for evaluation. In: Ottoson JM, Hawe P. (eds) Knowledge utilization, diffusion, implementation, transfer, and translation: implications for evaluation. Hoboken, NJ: Wiley, 2009, pp. 75–87. [Google Scholar]
- 24. Lavis J, Robertson D, Woodside J, et al. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q 2003; 81(2): 221–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Westfall JM, Mold J, Fagnan L. Practice-based research – ‘Blue Highways’ on the NIH roadmap. JAMA 2007; 297(4): 403–406. [DOI] [PubMed] [Google Scholar]
- 26. Australian Government Department of Health and Ageing. Strategic review of health and medical research in Australia – better health through research. Canberra, ACT, Australia: Commonwealth of Australia, 2013. [Google Scholar]
- 27. Grimshaw JM, Eccles MP, Lavis JN, et al. Knowledge translation of research findings. Implement Sci 2012; 7: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Woolf S. The meaning of translational research and why it matters. JAMA 2008; 299(2): 211–213. [DOI] [PubMed] [Google Scholar]
- 29. Peters DH, Tran NT, Adam T. Implementation research in health: a practical guide. Geneva: Alliance for Health Policy and Systems Research, World Health Organization, 2013. [Google Scholar]
- 30. Mandelzweig L, Battler A, Boyko V, et al. The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J 2006; 27(19): 2285–2293. [DOI] [PubMed] [Google Scholar]
- 31. Lesho EP, Myers CP, Ott M, et al. Do clinical practice guidelines improve processes or outcomes in primary care? Mil Med 2005; 170(3): 243–246. [DOI] [PubMed] [Google Scholar]
- 32. Smith TJ, Hillner BE. Ensuring quality cancer care by the use of clinical practice guidelines and critical pathways. J Clin Oncol 2001; 19: 2886–2897. [DOI] [PubMed] [Google Scholar]
- 33. Hubbard IJ, Harris D, Kilkenny MF, et al. Adherence to clinical guidelines improves patient outcomes in Australian audit of stroke rehabilitation practice. Arch Phys Med Rehabil 2012; 93: 965–971. [DOI] [PubMed] [Google Scholar]
- 34. Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004; 82(4): 581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Connell LA, McMahon NE, Harris JE, et al. A formative evaluation of the implementation of an upper limb stroke rehabilitation intervention in clinical practice: a qualitative interview study. Implement Sci 2014; 9: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012; 6: CD000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Olivari Z, Steffenino G, Savonitto S, et al. The management of acute myocardial infarction in the cardiological intensive care units in Italy: the ‘BLITZ 4 Qualità’ campaign for performance measurement and quality improvement. Eur Heart J Acute Cardiovasc Care 2012; 1(2): 143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Aroney C, Aylward P, Kelly A, et al. ; National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand. Guidelines for the management of acute coronary syndromes. Med J Aust 2006; 184(8 Suppl.): S9–S29. [DOI] [PubMed] [Google Scholar]
- 39. Scalley B, Gee A, Katzenellenbogen JM, et al. Improving the management of acute coronary syndrome in a regional hospital. Aust N Z J Public Health, in press. [DOI] [PubMed] [Google Scholar]
- 40. Scalley B, Katzenellenbogen JM, Gilles M, et al. Management of acute coronary syndrome in a regional hospital 2011–2012: unpublished report to WACHS. Perth, WA, Australia: WA Department of Health, 2013. [Google Scholar]
- 41. Scalley B, Katzenellenbogen JM, Gilles M, et al. Management of acute coronary syndrome in a regional hospital: follow-up audit 2013–2014: unpublished report to WACHS. Perth, WA, Australia: WA Department of Health, 2014. [Google Scholar]
- 42. Peters DH, Adam T, Alonge O, et al. Implementation research: what it is and how to do it. BMJ 2013; 347: f6753. [DOI] [PubMed] [Google Scholar]
- 43. LaRocca R, Yost J, Dobbins M, et al. The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health 2012; 12: 751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yin RK. Case study research: design and methods. 5th ed. Thousand Oaks, CA: SAGE, 2014. [Google Scholar]
- 45. Stake R. The art of case study research. Thousand Oaks, CA: SAGE, 1995. [Google Scholar]
- 46. Crowe S, Cresswell K, Robertson A, et al. The case study approach. BMC Med Res Methodol 2011; 11: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Aarons GA, Ehrhart MG, Farahnak LR, et al. Leadership and organizational change for implementation (LOCI): a randomized mixed method pilot study of a leadership and organization development intervention for evidence-based practice implementation. Implement Sci 2015; 10(1): 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hutchinson M, Daly J, Usher K, et al. Editorial: leadership when there are no easy answers: applying leader moral courage to wicked problems. J Clin Nurs 2015; 24(21–22): 3021–3023. [DOI] [PubMed] [Google Scholar]
- 49. Gray J, Beresford QA. ‘Formidable challenge’: Australia’s quest for equity in Indigenous education. Aust J Educ 2008; 52(2): 197–223. [Google Scholar]
- 50. Johns G. The Northern Territory Intervention in Aboriginal affairs: wicked problem or wicked Policy? Agenda 2008; 15(2): 65–84. [Google Scholar]
- 51. Coory MD, Walsh WF. Rates of percutaneous coronary interventions and bypass surgery after acute myocardial infarction in Indigenous patients. Med J Aust 2005; 182(10): 507–512. [DOI] [PubMed] [Google Scholar]
- 52. Cunningham J. Diagnostic and therapeutic procedures among Australian hospital patients identified as indigenous. Med J Aust 2002; 176: 58–62. [DOI] [PubMed] [Google Scholar]
- 53. Haynes E, Taylor KP, Durey A, et al. Examining the potential contribution of social theory to developing and supporting Australian Indigenous-mainstream health service partnerships. Int J Equity Health 2014; 13(1): 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Masuda JR, Zupancic T, Crighton E, et al. Equity-focused knowledge translation: a framework for ‘reasonable action’ on health inequities. Int J Public Health 2014; 59(3): 457–464. [DOI] [PubMed] [Google Scholar]
- 55. Tsou C, Haynes E, Warner W, et al. An exploration of inter-organisational partnership assessment tools in the context of Australian Aboriginal-Mainstream Partnerships: a scoping review of the literature. BMC Public Health 2015; 15: 416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cross R, Prusak L. The people who make organizations go – or stop. Harv Bus Rev 2002; 80(6): 104–112. [PubMed] [Google Scholar]
- 57. Fuller JD, Hermeston W, Passey M, et al. Acceptability of participatory social network analysis for problem-solving in Australian Aboriginal health service partnerships. BMC Health Serv Res 2012; 12(1): 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Williams P. The competent boundary spanner. Public Admin 2002; 80(1): 103–124. [Google Scholar]
- 59. Scott SD, Albrecht L, O’Leary K, et al. Systematic review of knowledge translation strategies in the allied health professions. Implement Science 2012; 7: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19(6): 349–357. [DOI] [PubMed] [Google Scholar]
- 61. Ivers NM, Sales A, Colquhoun H, et al. No more ‘business as usual’ with audit and feedback interventions: towards an agenda for a reinvigorated intervention. Implement Sci 2014; 9: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]