Abstract
A 60-year-old male with a huge prostate cyst presented with obstruction symptom of urethra and intestinal tract. Complete excision of the cystic prostate failed as a result of the strong adherence and twice operations history, but we confirmed prostate adenocarcinoma and relieved his obstruction symptom. Case 2 was a 77-year-old male with an 8 cm cyst of which biopsy showed prostate cancer in local hospital. He was admitted 18 months later because of intestinal obstruction. Radical resection had a satisfied result of obstruction symptom and PSA. Here we summarized malignant characteristics of cystic lesions in prostate or surrounding structures and management.
Keywords: Prostatic neoplasm, Prostatic cysts, Hemorrhage
Introduction
Cysts in prostate or surrounding structures are common, but cystic prostatic neoplasm is a rare entity. Although prostatic carcinoma presenting as a cystic rather than a solid lesion is infrequent, it may be prone to underdiagnosis. Here we detail two cases of gigantic prostatic cyst, one of which prostatic cancer was confirmed in the fourth operation.
Case presentation
Case 1
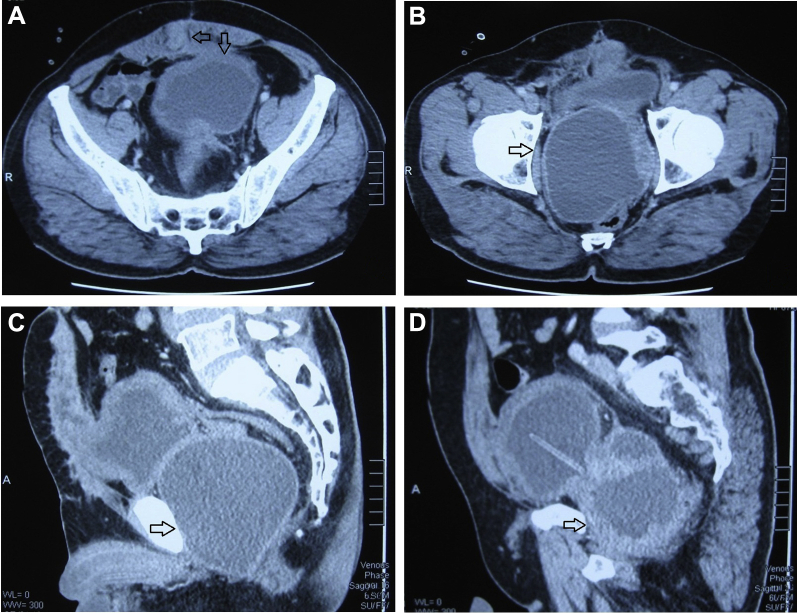
A 60-year-old male presented with a history of dysuria, pollakisuria and dyschesia for 6 years. Before visited our hospital, he was indwelled catheter because of urinary retention. This patient had a history of twice pelvic operations in local hospital, but could not provide any medical record except computerized tomography (CT). On physical examination, a 15 cm scar could be found at hypogastric region. Digital rectal examination revealed a large, smooth mass without boundary. Serum prostate-specific antigen (PSA) was 172.70 μg/L and carcinoembryonic antigen was 32.21 ng/mL. CT showed a cystic mass measuring approximately 12 cm in diameter (Fig. 1). Even though prostate cancer was suspected, he refused prostate biopsy.
Figure 1.
CT scan before the first operation in our hospital showing a huge pelvic cyst: (A) thickened bladder wall and nodules at rectus abdominis (arrow). (B) the huge cyst (arrow) was in the posterior of bladder. (C, D) sagittal CT shows the cyst (arrow) was beneath the bladder.
Complete excision of the cyst and prostate failed because of strong adherence. Approximately 450 mL of brown fluid was drained in the operation. Silver Nitrate and alcohol was used in operation and post-operation separately, to cauterize the cystic wall. The pathology of partial cystic wall was fibrous tissue. After operation, obstruction symptom of urethra and intestinal tract disappeared.
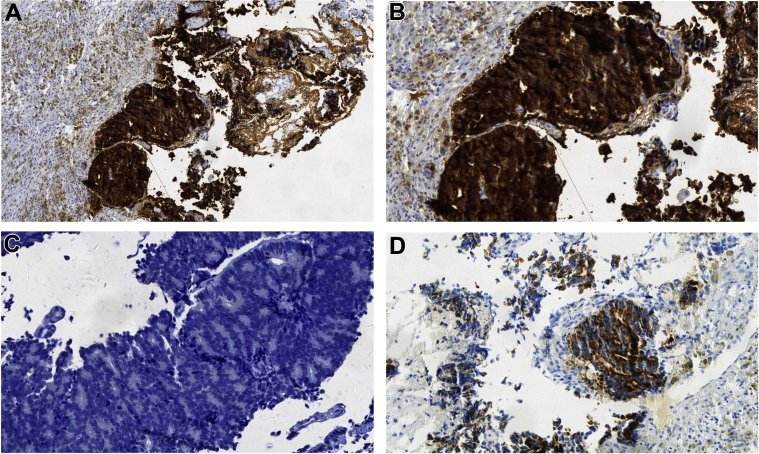
Five months later, obstruction symptom recurred and CT found a cyst in the same position. PSA rose to 192.00 μg/L. Bone scan revealed metastasis at sacrum. We explored by abdominoperineal incision. Some part of cystic wall adhered tightly to the pelvic. After partial cystic wall and bladder wall were excised by two approaches, a 1.5 cm channel between bladder and cyst was formed. A Malecot catheter was implanted into the cyst through bladder approach, which turned the cyst into a bladder diverticulum. Prostate adenocarcinoma was determined by immunohistochemical stain (Fig. 2). Bicalutamide and goserelin was given and external beam radiotherapy was performed. Little brown precipitate could be found in urine in the first several months. Follow-up for 36 months, obstruction symptom of urethra and intestinal tract hadn't recurred. PSA was 5.61 μg/L 35 months after operation. After bicalutamide and goserelin was given, PSA was 0.34 μg/L in the next month.
Figure 2.
Histopathological findings: (A) Immunohistochemical analysis with PSA stain (×100). (B) Immunohistochemical analysis with PSA stain (×200). (C) Immunohistochemical analysis with P504s stain (×200). (D) Immunohistochemical analysis with CK5/6 stain (×200).
Case 2
A 77-year-old male was admitted with the chief complaint of weak stream. Weak stream, frequency, macroscopic hematuria and flat stool started 2 years ago. After admitted in local hospital, CT showed a prostate cyst measuring approximately 6 cm in diameter. Serum PSA is more than 100 ng/mL and bone scan was negative. Prostate biopsy showed prostate cancer with Gleason Score of 2 + 2. Orchiectomy was performed and flutamide was given. Serum PSA was 0.39 μg/L at 18 months later.
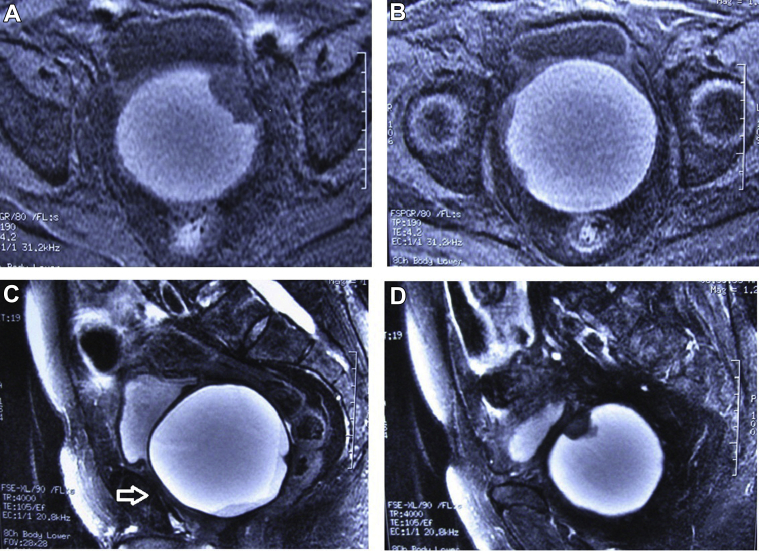
The patient was admitted in local hospital again with the complaint of recurred failure of stool and gas pass for 2 months. X-ray showed intestinal obstruction. After recovered from septic shock in local hospital, CT and MRI showed a 8.3 cm prostatic cyst with multiple nodules on cystic wall and reinforcement of partial cystic wall (Fig. 3). The patient was transferred to our hospital at that time and PSA rose to 28.15 ng/mL. Digital rectal examination revealed a huge mass at the position of prostate, of which the boundary can't be touched. His bone scan was negative.
Figure 3.
MRI showed a cystic mass measuring approximately 8.3 cm in diameter in The posterior region of the bladder. (A, B) some nodules on the cyst wall. (C, D) sagittal image of the cyst (arrow).
At surgery, approximate 300 mL brown fluid content was extracted from the cyst. After radical prostatectomy, pathology of specimen showed cyst wall was muscle and fiber tissue with hemorrhage and cystic change, the nodules on cyst wall were cholesterol crystal and inflammatory foreign body granuloma. Cystic fluid cytology revealed a little erythrocytoma and inflammatory cells microscopically. Serum PSA was 0.19 μg/L 3 weeks later. Follow-up for 24 months, he is free of obstruction symptom and PSA was 0.01 μg/L.
Discussion
Differential diagnosis of cystic lesions in prostate or surrounding structures includes Müllerian duct cyst, prostatic utricle cyst, ejaculatory duct cyst, prostatic retention cyst, abscess and so on. Some cysts may be secondary to malignant lesion, others may be primary, such as prostate cystadenocarcinoma. It was reported the incidence of neoplasia arising in Müllerian duct cyst was 3%.1 Malignant cystic lesions are not common, but could be falsely diagnosed as benign disease. It is difficult to distinguish in some cases similar to our case since elevating PSA only suggested a prostate original and hemorrhaging, not benign or malignant.2
In case 1, rapidly growth of cyst, hemorrhaging, elevating PSA increased the possibility of malignance. From above cases and literature gathered, we summarized some characteristics should be pay attention to: (1) Inhomogeneous or enhanced cystic density indicates hemorrhaging or protein component. More than 80% of cystic prostate cancer accompanied with hemorrhaging was reported.3 (2) Cyst with irregular margin, nodule, thickness of wall and enhanced of these solid elements.4, 5 (3) Multiple cysts, enhancing septa, and cystic-solid mixed mass.6 (4) Rapidly growing cyst or recurrent cyst.2, 5 (5) Elevated PSA.
Biopsy is necessary when malignance could not be ruled out. The positive rate of prostate biopsy is relative with the ratio of puncture numbers/prostate volume. This ratio of huge prostate cysts is lower. It's hard to puncture the nodule because of depth and angle without CT or ultrasound-MRI combined guide. Through the second pathology of case 2 was benign, radical resection had a lasting satisfied result of symptom and PSA. Usually, minimally invasive surgery such as transurethral surgery or puncture can be chosen preferentially to relieve obstruction symptom. As reported, cystic prostate cancer was confirmed in several cases with negative result of malignancy after transurethral operation or biopsy.2, 5 Transurethral surgery could not obtain complete specimens and some cysts may be underdiagnosis. We prefer laparoscopic radical prostatectomy or open operation for complete resection when multiple malignant characteristics above exist. When complete resection is difficult, it's necessary to relieve the obstruction of urethra and intestinal tract by surgery.
Conclusion
For the cases with several malignant characteristics summarized above, we prefer complete resection surgery even though biopsy is negative.
Conflict of interest
Authors declare that they have no conflict of interests.
Acknowledgment
We would like to acknowledge Yuhua Huang and Gang Li, Department of Urology, The First Affiliated Hospital of Soochow University. Weina Zhu and Shuqin Han, Department of Pathology, Suzhou Kowloon Hospital, Shanghai Jiaotong University School of Medical.
Footnotes
This work was conducted in Department of Urology, Suzhou Kowloon Hospital, Shanghai Jiaotong University School of Medical.
References
- 1.Schunhrke T.D., Kaplan G.W. Prostatic utricle cyst (müllerian duct cysts) J Urol. 1978;119:765–767. doi: 10.1016/s0022-5347(17)57627-2. [DOI] [PubMed] [Google Scholar]
- 2.Chang Y.H., Chuang C.K., Ng K.F., Liao S.K. Coexistence of a hemorrhagic cyst and carcinoma in the prostate gland. Chang Gung Med J. 2005;28:264–267. [PubMed] [Google Scholar]
- 3.Ishida K., Kubota Y., Takada T. A case of prostate cancer with cyst formation. Hinyokika Kiyo. 2003;49:235–237. [PubMed] [Google Scholar]
- 4.Henderson-Jackson E., Sexton W., Zhang J. Cystic prostatic ductal adenocarcinoma: an unusual presentation and cytological diagnosis. Ann Clin Lab Sci. 2012;42:81–88. [PubMed] [Google Scholar]
- 5.Pariente J.L., Hostyn B., Grenier N. Diagnosis and follow-up of a prostatic cystic carcinoma. Br J Urol. 1998;81:177. doi: 10.1046/j.1464-410x.1998.00352.x. http://dx.doi.org/10.1046/j.1464-410x.1998.00352.x [DOI] [PubMed] [Google Scholar]
- 6.Seong B.M., Cheon J., Lee J.G. A case of multilocular prostatic cystadenoma. J Korean Med Sci. 1998;13:554–558. doi: 10.3346/jkms.1998.13.5.554. http://dx.doi.org/10.3346/jkms.1998.13.5.554 [DOI] [PMC free article] [PubMed] [Google Scholar]