Abstract
BACKGROUND
Currently, the diagnosis of chronic obstructive pulmonary disease (COPD) requires a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) of less than 0.70 as assessed by spirometry after bronchodilator use. However, many smokers who do not meet this definition have respiratory symptoms.
METHODS
We conducted an observational study involving 2736 current or former smokers and controls who had never smoked and measured their respiratory symptoms using the COPD Assessment Test (CAT; scores range from 0 to 40, with higher scores indicating greater severity of symptoms). We examined whether current or former smokers who had preserved pulmonary function as assessed by spirometry (FEV1:FVC ≥0.70 and an FVC above the lower limit of the normal range after bronchodilator use) and had symptoms (CAT score, ≥10) had a higher risk of respiratory exacerbations than current or former smokers with preserved pulmonary function who were asymptomatic (CAT score, <10) and whether those with symptoms had different findings from the asymptomatic group with respect to the 6-minute walk distance, lung function, or high-resolution computed tomographic (HRCT) scan of the chest.
RESULTS
Respiratory symptoms were present in 50% of current or former smokers with preserved pulmonary function. The mean (±SD) rate of respiratory exacerbations among symptomatic current or former smokers was significantly higher than the rates among asymptomatic current or former smokers and among controls who never smoked (0.27± 0.67 vs. 0.08±0.31 and 0.03±0.21 events, respectively, per year; P<0.001 for both comparisons). Symptomatic current or former smokers, regardless of history of asthma, also had greater limitation of activity, slightly lower FEV1, FVC, and inspiratory capacity, and greater airway-wall thickening without emphysema according to HRCT than did asymptomatic current or former smokers. Among symptomatic current or former smokers, 42% used bronchodilators and 23% used inhaled glucocorticoids.
CONCLUSIONS
Although they do not meet the current criteria for COPD, symptomatic current or former smokers with preserved pulmonary function have exacerbations, activity limitation, and evidence of airway disease. They currently use a range of respiratory medications without any evidence base. (Funded by the National Heart, Lung, and Blood Institute and the Foundation for the National Institutes of Health; SPIROMICS ClinicalTrials.gov number, NCT01969344.)
Among the criteria that are needed to make a diagnosis of chronic obstructive pulmonary disease (COPD) are deficits in the rate at which one can forcefully exhale. Most experts consider a low ratio (<0.70) of the forced expiratory volume in 1 second (FEV1) to the forced vital capacity (FVC) after bronchodilator use to be a key diagnostic criterion.1 Once the diagnosis of COPD has been established, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) nomenclature grades severity according to the degree to which the measured FEV1 is lower than the patient's predicted value. GOLD stage 1, indicating mild disease, is defined as an FEV1 that is greater than or equal to 80% of the predicted value; GOLD stage 2, indicating moderate disease, as an FEV1 that is greater than or equal to 50% and less than 80% of the predicted value; GOLD stage 3, indicating severe disease, as an FEV1 that is greater than or equal to 30% and less than 50% of the predicted value; and GOLD stage 4, indicating very severe disease, as an FEV1 that is less than 30% of the predicted value.
However, some smokers who do not have airflow obstruction — those whose FEV1:FVC after bronchodilator use is equal to or greater than the conventionally accepted cutoff of 0.70 — nonetheless report cough, sputum production, and shortness of breath; these symptoms are suggestive of COPD.1-3 Furthermore, the FEV1:FVC ratio can be insensitive to early airway disease.4 A recent task-force document emphasized the need for additional research involving smokers with symptoms and normal lung function.5
In the Subpopulations and Intermediate Outcome Measures in COPD Study (SPIROMICS), we hypothesized that many current or former smokers who have respiratory symptoms despite an FEV1:FVC of at least 0.70 after bronchodilator use have clinical symptoms and findings that are consistent with a chronic lower respiratory disease similar to COPD. To test this hypothesis, we focused on current or former smokers who had respiratory symptoms at baseline despite preserved pulmonary function as assessed by spirometry (FEV1:FVC ≥0.70 and an FVC above the lower limit of the normal range after bronchodilator use). We required an FVC above the lower limit of the normal range in order to minimize the misclassification of participants with restrictive disease as having COPD. We then determined whether these symptomatic current or former smokers with preserved pulmonary function had a higher risk of respiratory exacerbations or abnormalities on a high-resolution computed tomographic (HRCT) scan of the chest or shorter 6-minute walk distances than asymptomatic current or former smokers with preserved pulmonary function.
Methods
Participants and Study Design
In this multicenter observational study funded by the National Heart, Lung, and Blood Institute,6 we enrolled 2736 participants from 2010 through 2015. The study included persons 40 to 80 years of age who were either healthy persons who had never smoked (≤1 pack-year of tobacco-smoking history, FEV1:FVC ≥0.70 before bronchodilator use, an FVC that was equal to or above the lower limit of the predicted normal range,7 and no known current lung disease or unstable cardiovascular disease) or current or former smokers who had a smoking history of more than 20 pack-years, regardless of whether they had a clinical diagnosis of obstructive lung disease.
For this study, we categorized participants for analysis using the GOLD staging system according to the results on spirometry,8 which we performed before and after four inhalations each of albuterol at a dose of 90 μg per inhalation and ipratropium at a dose of 18 μg per inhalation. Current or former smokers who had a concomitant diagnosis of asthma were not excluded; instead, historical data on whether the participant had a diagnosis of asthma were collected. We quantified symptoms during a stable phase of disease (>6 weeks after any exacerbation) using the COPD Assessment Test (CAT), a validated eight-question health-status instrument.9 CAT scores range from 0 to 40, with higher scores indicating greater severity of symptoms. In the context of COPD, GOLD uses a CAT score of 10 or more as a threshold for more severe symptoms in consideration of treatment regimens.8
We obtained an exacerbation history prospectively (every 3 months) with the use of a structured questionnaire, and we defined exacerbations on the basis of the use of antibiotic agents, systemic glucocorticoids, or a combination of both or a health care utilization event (office visit, hospital admission, or emergency department visit for a respiratory flare-up). We defined severe exacerbations as interactions that led to hospitalization or an emergency department visit. Exacerbations were managed by the participants’ usual providers, who were aware of their patient's enrollment in an observational study. The study did not, however, provide guidance on management. Spirometric tracings were independently reviewed.
All the participants underwent testing to determine the distance walked in 6 minutes.10 From computed tomographic scans of the lung, we measured the extent of emphysema and airway-wall thickness with the use of HRCT imaging and VIDA Diagnostics software. A threshold of −950 Hounsfield units was used to define emphysema; Pi10, defined as the square root of the wall area of a theoretical circular cross section of an airway that is 10 mm in the lumenal perimeter, was used to define airway-wall thickening.11
This study was not population-based, so we recruited participants from the population at each center by means of physician referral, advertisement in clinical areas, or self-referral at the study website (www.spiromics.com). The research protocol was approved by the institutional review board at each participating institution, and all the participants provided written informed consent.
Statistical Analysis
The investigators performed the data analysis using SAS software, version 9.3 (SAS Institute). We used one-way analysis of variance, the chi-square test, and the Kruskal–Wallis test, as appropriate, for the comparisons of groups. P values are two-sided, with Bonferroni-corrected pairwise comparisons between individual groups (with adjustment for the 10 comparisons that result from comparisons across five groups). A P value of less than 0.05 was considered to indicate statistical significance.
To control for potential confounders, we used linear regression (for the 6-minute walk distance and lung function) and logistic-regression models (for the bronchodilator response). We fit proportional-means models for recurrent events of exacerbations to accommodate differences in follow-up time across participants.12 We defined annualized exacerbation rates as the total number of events per person, divided by the number of follow-up days for that person, multiplied by 365.
In additional analyses, we stratified the analysis according to smoking status (current or former), participant's report of previous diagnosis of COPD by a health provider (yes or no), and asthma (never, during childhood, or ever). We developed receiver-operating-characteristic curves to determine the value of the CAT, the British modified Medical Research Council (mMRC) dyspnea questionnaire (scores range from 0 to 4, with higher scores indicating more severe dyspnea),13 and the FEV1 to predict the risk of one or more exacerbations versus none in the first year of follow-up. We limited these receiver-operating-characteristic curve analyses to participants with at least 1 year of follow-up.
Results
Characteristics of the Participants
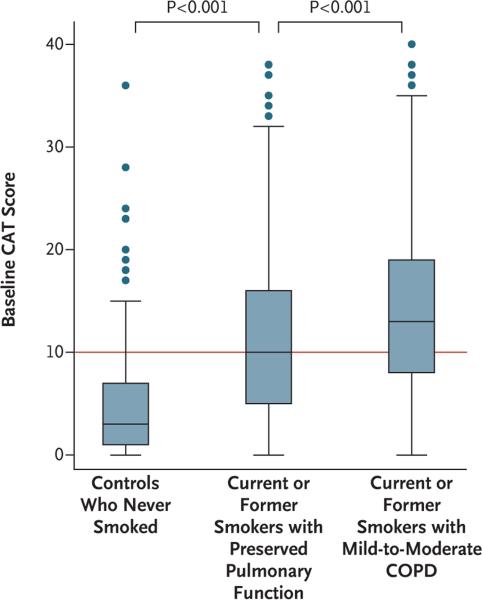
We categorized current or former smokers into four mutually exclusive groups. First, we categorized current or former smokers according to an FEV1:FVC of 0.70 or more after bronchodilator use and an FVC above the lower limit of the normal range (preserved pulmonary function) versus mild-to-moderate COPD (GOLD stage 1 or 2); then we subcategorized the members of each of these two groups into participants with a CAT score of 10 or more (symptomatic) or a CAT score of less than 10 (asymptomatic)8 (Table 1). We found that 50% of current or former smokers with preserved pulmonary function had symptoms (Fig. 1) — a prevalence of symptoms that was slightly less than that among participants with GOLD stage 1 or 2 COPD (65%, P<0.001) but far greater than the prevalence among controls who never smoked (16%, P<0.001).
Table 1.
Characteristics of the Participants at Baseline.*
| Characteristic | Never Smoked | Current or Former Smokers | |||
|---|---|---|---|---|---|
| Group A (N = 199) | Preserved Pulmonary Function | Mild-to-Moderate COPD | |||
| Group B, CAT <10 (N = 424) | Group C, CAT ≥10 (N = 425) | Group D, CAT <10 (N = 337) | Group E, CAT ≥10 (N = 626) | ||
| Percentage of overall study population | 9.9 | 21.1 | 21.1 | 16.8 | 31.1 |
| Age | |||||
| Mean (yr) | 56.4±10.2 | 61.9±9.5 | 59.3±9.9 | 67.9±7.1 | 64.9±8.2 |
| Significant between-group difference† | B, C, D, E | A, C, D, E | A, B, D, E | A, B, C, E | A, B, C, D |
| Male sex | |||||
| No. of participants/total no. (%) | 77/199 (39) | 222/424 (52) | 186/425 (44) | 223/336 (66) | 342/626 (55) |
| Significant between-group difference† | B, D, E | A, D | D, E | A, B, C, E | A, C, D |
| Hispanic ethnic group‡ | |||||
| No. of participants/total no. (%) | 27/199 (14) | 16/423 (4) | 37/425 (9) | 11/336 (3) | 24/626 (4) |
| Significant between-group difference† | B, D, E | A, C | B, D, E | A, C | A, C |
| Race‡ | |||||
| No. of participants (%) | |||||
| White | 137 (69) | 331 (78) | 248 (58) | 292 (87) | 513 (82) |
| Nonwhite | 62 (31) | 93 (22) | 177 (42) | 45 (13) | 113 (18) |
| Significant between-group difference† | D, E | C, D | B, D, E | A, C | A, B, C |
| Body-mass index | |||||
| Mean | 28.5±5.0 | 27.8±4.8 | 29.7±5.3 | 27.1±4.6 | 28.2±5.4 |
| Significant between-group difference† | D | C | B, D, E | A, C, E | C, D |
| Current smoking | |||||
| No. of participants/total no. (%) | 0/196 | 181/422 (43) | 251/419 (60) | 83/331 (25) | 272/617 (44) |
| Significant between-group difference† | — | C, D | B, D, E | B, C, E | C, D |
| Extent of smoking | |||||
| Mean pack-yr | 0 | 41.5±20.9 | 45.8±26.4 | 49.5±23.8 | 54.1±26.7 |
| Significant between-group difference† | B, C, D, E | A, D, E | A, E | A, B, E | A, B, C, D |
| Symptoms of chronic bronchitis | |||||
| No. of participants/total no. (%) | 4/196 (2) | 23/417 (6) | 133/408 (33) | 27/326 (8) | 191/604 (32) |
| Significant between-group difference† | C, E | C, E | A, B, D | C, E | A, B, D |
| Wheezing | |||||
| No. of participants/total no. (%) | 27/198 (14) | 137/422 (32) | 291/421 (69) | 152/334 (46) | 476/623 (76) |
| Significant between-group difference† | B, C, D, E | A, C, D, E | A, B, D | A, B, C, E | A, B, D |
| History of COPD | |||||
| No. of participants/total no. (%) | 0/197 | 45/412 (11) | 173/399 (43) | 168/320 (52) | 485/603 (80) |
| Significant between-group difference† | — | C, D, E | B, E | B, E | B, C, D |
| Any diagnosis of asthma | |||||
| No. of participants/total no. (%) | 10/195 (5) | 30/420 (7) | 114/419 (27) | 50/330 (15) | 161/611 (26) |
| Significant between-group difference† | C, D, E | C, D, E | A, B, D | A, B, C, E | A, B, D |
| Childhood diagnosis of asthma | |||||
| No. of participants/total no. (%) | 4/197 (2) | 15/423 (4) | 41/417 (10) | 25/331 (8) | 69/619 (11) |
| Significant between-group difference† | C, E | C, E | A, B | — | A, B |
| History of congestive heart failure | |||||
| No. of participants/total no. (%) | 1/196 (1) | 3/421 (1) | 8/423 (2) | 4/335 (1) | 25/622 (4) |
| Significant between-group difference† | — | E | — | — | B |
| History of GERD | |||||
| No. of participants/total no. (%) | 35/195 (18) | 112/421 (27) | 142/422 (34) | 89/335 (27) | 221/622 (36) |
| Significant between-group difference† | C, E | E | A | E | A, B, D |
Plus–minus values are means ±SD. Group A included healthy controls who had never smoked, group B current or former smokers with preserved pulmonary function as assessed by spirometry who had a Chronic Obstructive Pulmonary Disease (COPD) Assessment Test (CAT)9 score of less than 10, group C current or former smokers with preserved pulmonary function with a CAT score of 10 or more, group D current or former smokers with COPD symptoms of Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 1 or 2 (indicating mild and moderate disease, respectively) and a CAT score of less than 10, and group E current or former smokers with COPD symptoms of GOLD stage 1 or 2 and a CAT score of 10 or more. Scores on the CAT, a validated eight-question health-status instrument, range from 0 to 40, with higher scores indicating greater severity of symptoms. Data on age and body-mass index (the weight in kilograms divided by the square of the height in meters) were missing for one participant in group D, and data on the extent of smoking were missing for one participant in group A and one in group E. GERD denotes gastroesophageal reflux disease.
P<0.05 for each pairwise comparison (vs. the group indicated) by one-way analysis of variance with Bonferroni correction for multiple comparisons across the five groups (10 comparisons) for continuous variables and by the chi-square test for categorical variables.
Race and ethnic group were self-reported.
Figure 1. Prevalence of Respiratory Symptoms, According to Study Group.
Respiratory symptoms were assessed with the use of the Chronic Obstructive Pulmonary Disease (COPD) Assessment Test (CAT) in controls who had never smoked, in current or former smokers with preserved pulmonary function as assessed by spirometry (a ratio of the forced expiratory volume in 1 second to the forced vital capacity [FVC] of ≥0.70 after bronchodilator use and an FVC above the lower limit of the normal range), and in current or former smokers who had COPD symptoms of Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 1 or 2 (indicating mild and moderate disease, respectively). Scores on the CAT, a validated eight-question health-status instrument, range from 0 to 40, with higher scores indicating a greater severity of symptoms. The red line indicates the cutoff for more severe symptoms that is used by GOLD (CAT score, ≥10). The horizontal line in the boxes represents the median, and the bottom and top of the boxes the 25th and 75th percentiles, respectively. I bars represent the upper adjacent value (75th percentile plus 1.5 times the interquartile range) and the lower adjacent value (corresponding formula below the 25th percentile), and the dots outliers. P values were adjusted with Bonferroni correction for multiple comparisons.
Symptomatic current or former smokers with preserved pulmonary function had elevations in all components of the CAT score (Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org), were younger, were more likely to be nonwhite or Hispanic, had a higher body-mass index (BMI; the weight in kilograms divided by the square of the height in meters), and were more likely to be current smokers, report symptoms of chronic bronchitis, and report a history of wheezing and asthma (during childhood or ever) than those with lesser symptoms (CAT score, <10) (Table 1). Because our definition of symptoms was based on the CAT score and included more than just cough and sputum production, chronic bronchitis was present in only 33% of symptomatic current or former smokers (Table 1).
Current or former smokers with preserved pulmonary function who were symptomatic were also more likely than those who were asymptomatic to report a previous diagnosis of COPD by a health professional (43% vs. 11%, P<0.001), although the prevalence was lower than that among symptomatic participants with GOLD stage 1 or 2 COPD symptoms (80%, P<0.001). Even after the exclusion of participants with an FEV1:FVC of 0.70 or more but who nonetheless had received a health professional's diagnosis of COPD, symptoms remained more prevalent among current or former smokers with preserved pulmonary function than among healthy controls who had never smoked (38% vs. 16%, P<0.001).
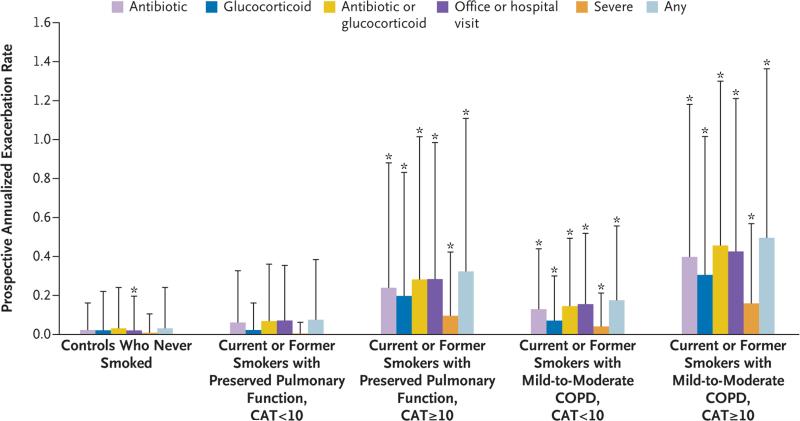
Exacerbations and Activity Limitation
The median prospective follow-up time was 829 days (interquartile range, 494 to 1106). Whether defined on the basis of the use of antibiotics, the use of systemic glucocorticoids, the prescription of either of these medications, any health care utilization, or hospitalization or emergency department visits (severe exacerbations), the prospective rate of exacerbations was higher among symptomatic current or former smokers with preserved pulmonary function than among asymptomatic current or former smokers or among healthy controls who had never smoked (0.27±0.67 vs. 0.08±0.31 and 0.03±0.21 events, respectively, per year; P<0.001 for both comparisons) (Fig. 2, and Fig. S2 and Table S1 in the Supplementary Appendix). The mean distance walked in 6 minutes was also shorter in symptomatic current or former smokers with preserved pulmonary function (79.8±19.2% of the predicted value) than in asymptomatic current or former smokers (89.3± 18.8% of the predicted value) and in participants with GOLD stage 1 or 2 COPD symptoms and a CAT score of less than 10 (89.2±19.3% of the predicted value) (Table S1 in the Supplementary Appendix).
Figure 2. Prevalence of Symptoms and Risk of Respiratory Exacerbations, According to Study Group.
Prospective respiratory exacerbations were defined as respiratory events that were treated with antibiotics or oral glucocorticoids, those associated with health care utilization (office visit, emergency department visit, or hospitalization), those that were considered to be severe exacerbations (i.e., that led to an emergency department visit or hospitalization), or any exacerbation (any of the above). T bars indicate 1 SD. Asterisks indicate a P value of less than 0.05, with Bonferroni correction for multiple comparisons, for the comparison with current or former smokers with preserved pulmonary function and a CAT score of less than 10.
Airway Disease and Emphysema
Symptomatic current or former smokers with preserved pulmonary function differed from asymptomatic current or former smokers in a range of lung-function measures including FEV1 (percentage of predicted FEV1 after bronchodilator use, 94.1±13.1% vs. 98.5±12.6%; P<0.001), FVC, and inspiratory capacity. Current or former smokers with preserved pulmonary function who were symptomatic did not have a higher percentage of lung volume with emphysematous features (hereafter referred to as percent emphysema) than did those who were asymptomatic (1.6±2.2% and 2.0±2.1%, respectively; P = 0.99) but did have a greater Pi10 (3.73±0.09 vs. 3.70±0.09, P = 0.002), a measure of airway-wall thickening on HRCT of the chest. Current or former smokers with preserved pulmonary function who were symptomatic were more likely than those who were asymptomatic to have an increase in FVC after bronchodilator use, according to the combined criteria of an increase of at least 12% and a 200-ml increase in FVC (8% vs. 2%, P = 0.003),14 but not according to the criterion of percentage increase in the FVC alone. For additional details on airway disease and emphysema, see Figures S3 and S4 and Table S1 in the Supplementary Appendix.
Potential Confounders
Given the significant differences in age, race, ethnic group, BMI, current smoking, and asthma between current or former smokers with preserved pulmonary function who were symptomatic and those who were asymptomatic, we developed multivariate models that controlled for these potential confounders of exacerbations as well as for sex, history of congestive heart failure, and history of gastroesophageal reflux disease. We found that even after these potential confounders were controlled for, symptomatic current or former smokers with preserved pulmonary function had more frequent exacerbations than did asymptomatic current or former smokers (Table 2). We also found persistent differences in the 6-minute walk distance and in lung function (Table S2 in the Supplementary Appendix).
Table 2.
Risk of Exacerbations Associated with CAT Score of 10 or More, as Compared with a CAT Score of Less Than 10, among Current or Former Smokers with Preserved Pulmonary Function.*
| Exacerbation | Model 1 |
Model 2 |
Model 3 |
Model 4 |
||||
|---|---|---|---|---|---|---|---|---|
| Relative Risk (95% CI) | P Value | Relative Risk (95% CI) | P Value | Relative Risk (95% CI) | P Value | Relative Risk (95% CI) | P Value | |
| Any | 3.62 (2.17–6.03) | <0.001 | 3.09 (1.82–5.27) | <0.001 | 2.40 (1.46–3.94) | <0.001 | 2.90 (1.71–4.90) | <0.001 |
| While taking antibiotic | 3.19 (1.86–5.49) | <0.001 | 2.72 (1.55–4.77) | <0.001 | 2.07 (1.23–3.49) | 0.006 | 2.56 (1.47–4.47) | <0.001 |
| While taking glucocorticoid | 7.22 (3.49–14.93) | <0.001 | 6.00 (2.87–12.56) | <0.001 | 4.37 (2.16–8.84) | <0.001 | 5.77 (2.77–12.05) | <0.001 |
| While taking antibiotic or glucocorticoid | 3.36 (1.96–5.77) | <0.001 | 2.90 (1.65–5.09) | <0.001 | 2.20 (1.30–3.71) | 0.003 | 2.72 (1.56–4.75) | <0.001 |
| Leading to health care utilization | 3.56 (2.18–5.83) | <0.001 | 3.01 (1.79–5.08) | <0.001 | 2.37 (1.46–3.85) | <0.001 | 2.80 (1.68–4.67) | <0.001 |
| Severe | 18.10 (4.77–68.67) | <0.001 | 11.99 (3.04–47.37) | <0.001 | 9.84 (2.48–39.02) | 0.001 | 11.50 (2.93–45.21) | <0.001 |
Results are from proportional-means models that modeled exacerbations as recurrent events. Model 1 was for the comparison of persons with a CAT score of less than 10 (reference group) with those who had a CAT score of 10 or more. Model 2 included model 1 plus the potential confounders of body-mass index, current smoking status, age, sex, race, and ethnic group. Model 3 included model 2 plus the potential confounders of self-reported coexisting conditions of congestive heart failure, GERD, and diagnosis of asthma at any time. Model 4 included model 2 plus the potential confounders of self-reported coexisting conditions of congestive heart failure, GERD, and diagnosis of asthma during childhood. CI denotes confidence interval.
To assess the effect of active smoking, we performed analyses that were stratified according to current smoking status versus former smoking status and found that symptoms (CAT score, ≥10) were associated with elevations in all components of the CAT score in both current smokers and former smokers with preserved pulmonary function. We also found higher rates of exacerbations among symptomatic current and former smokers with preserved pulmonary function, regardless of current versus former smoking status, than among asymptomatic current or former smokers or persons who had never smoked. For details, see Figures S5 and S6 in the Supplementary Appendix.
Finally, we performed sensitivity analyses in which we excluded participants who reported a history of asthma (during childhood or ever). These analyses showed that exacerbation rates remained higher among current or former smokers with preserved pulmonary function who were symptomatic than among those who were asymptomatic (Tables S3 and S4 in the Supplementary Appendix).
Effect of FEV1:FVC and CAT-Score Cutoffs
We performed receiver-operating-characteristic curve analyses of the association between CAT score and risk of exacerbation in the first year of follow-up. Among current or former smokers with preserved pulmonary function, the area under the curve for the baseline CAT score and the occurrence of any exacerbation in the first year of follow-up was 0.68; the corresponding area under the curve for the FEV1 after bronchodilator use was 0.59 (P = 0.05 for the comparison of CAT score with FEV1 after bronchodilator use). The sensitivity and specificity of the CAT score for at least one exacerbation in the first year of follow-up varied according to CAT-score cutoff. A CAT score of 10 had 75% sensitivity and 54% specificity for any exacerbation.
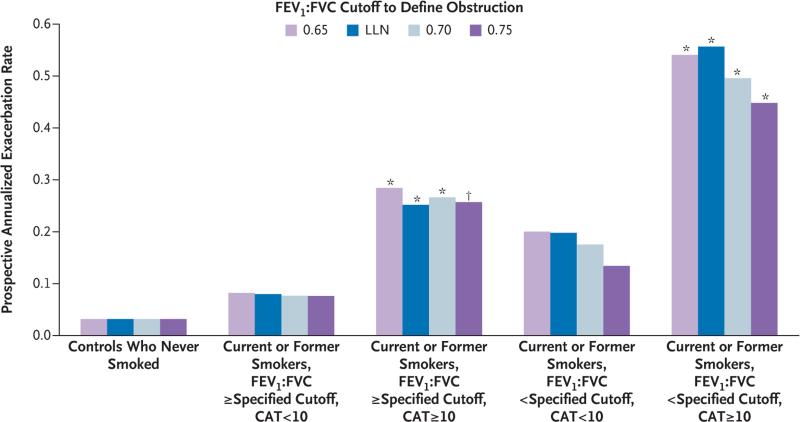
Defining preserved pulmonary function on the basis of each participant's lower limit of the normal range for FEV1:FVC after bronchodilator use or with the use of an FEV1:FVC cutoff of 0.65 did not significantly affect the association between the CAT score and any exacerbation (Fig. 3). However, a definition that was based on a post-bronchodilator FEV1:FVC cutoff of 0.75 led to fewer participants being categorized as having preserved pulmonary function (577 participants with the use of the 0.75 cutoff vs. 849 with the use of the 0.70 cutoff) and weakened the association between the CAT score and exacerbation (Fig. 3). Finally, on receiver-operating-characteristic curve analyses, the mMRC dyspnea score was similar to the CAT score in its association with any exacerbation over the first year of follow-up in current or former smokers with preserved pulmonary function. For details, see Figures S7 and S8 and Table S5 in the Supplementary Appendix.
Figure 3. Effect on Prospective Exacerbation Rates of Different FEV1:FVC Cutoffs to Define Preserved Pulmonary Function.
Shown are the prospective annualized exacerbations rates of any exacerbation, according to different cutoffs of the ratio of the forced expiratory volume in 1 second (FEV1) to the FVC. The definition of preserved pulmonary function that was based on the lower limit of the normal range (LLN) for the FEV1:FVC or that used an FEV1:FVC cutoff of 0.65 did not significantly change the predictive value of the CAT score for any exacerbation. The definition that was based on an FEV1:FVC cutoff of 0.75 weakened the predictive value of the CAT score for any exacerbation, although the sample size was smaller with an FEV1:FVC cutoff of 0.75 than with a cutoff of 0.70 (577 vs. 849 persons). Asterisks indicate a P value of less than 0.05, and the dagger a P value of 0.07, with Bonferroni correction for multiple comparisons, for the comparison with current or former smokers with a FEV1:FVC equal to or greater than the specified cutoff and a CAT score of less than 10.
Use of Respiratory Medication
In the 3 months before enrollment in the study, 42% of symptomatic current or former smokers with preserved pulmonary function had used inhaled bronchodilators, as compared with 8% of asymptomatic current or former smokers (P<0.001), and 23% had used inhaled glucocorticoids (vs. 3%, P<0.001) (Table S1 in the Supplementary Appendix). In sensitivity analyses, we excluded participants with any history of asthma and found that 29% of symptomatic current or former smokers with preserved pulmonary function used inhaled bronchodilators and 22% used inhaled glucocorticoids.
Discussion
In this longitudinal study, we found that respiratory symptoms, as measured by the CAT instrument, were common in current or former smokers, despite FEV1:FVC and FVC values that were in the range that is generally considered to be normal. Current or former smokers with preserved pulmonary function and a CAT score of 10 or more were more likely than those with lower CAT scores to have respiratory exacerbations, a shorter 6-minute walk distance, evidence of occult airway disease characterized by slightly lower lung function (e.g., with regard to FEV1, FVC, and inspiratory capacity), and greater airway-wall thickening. In contrast, the percent emphysema was low and similar among current or former smokers with preserved pulmonary function who were symptomatic and those who were asymptomatic.
Our findings were robust even with adjustment of the analyses for several important potential confounders. Concomitant asthma can confound CAT scores in current or former smokers.15 Although adults with a new diagnosis of COPD can occasionally receive an incorrect diagnosis of asthma, we assessed the effect of asthma by performing sensitivity analyses that controlled for and then excluded persons on the basis of a previous diagnosis of asthma (diagnosed during childhood or ever). Because retrospective data suggest that patients with COPD and coexisting conditions may be at higher risk for symptoms than those without coexisting conditions,16,17 we also controlled for relevant coexisting conditions, including congestive heart failure and gastroesophageal reflux disease.
Obesity can cause abnormal findings on spirometry and accentuate dyspnea.18,19 Extremely obese persons (BMI, >40) were excluded from this study. However, we also controlled for BMI in multivariate analyses, and our findings persisted. Active cigarette smoking can cause cough and sputum without apparent airway obstruction, a condition that has been termed “simple chronic bronchitis”20 or “nonobstructive chronic bronchitis.”2 However, our multivariate and stratified analyses indicate that current smoking does not explain the elevated exacerbation rates that we observed. Nonetheless, despite our efforts, it remains possible that other coexisting conditions, such as undiagnosed cardiovascular and metabolic abnormalities, could contribute to symptoms and some respiratory “exacerbations” in these persons, as they do in persons with COPD.21,22 Clinical trials are needed to determine whether maintenance therapy with bronchodilators or inhaled glucocorticoids will alleviate symptoms and reduce the rate of respiratory exacerbations in this group.
Our findings agree with and extend previously published data, including studies that document exacerbation-like events in smokers without airway obstruction23,24 and an association between an increased percentage of lung that is affected by emphysema and increased mortality among persons without airway obstruction25 and a study that previously challenged the notion of “healthy smokers” by showing the presence of respiratory symptoms, activity limitations, and abnormalities on HRCT in smokers who did not have airway obstruction.26 Our data add to these previous publications by showing that chronic symptoms precede the exacerbations, by showing that a clinically useful tool (the CAT) can identify smokers at risk for exacerbations, and by providing evidence for the type of lung disease these symptomatic persons may have (airway disease rather than emphysema).
Our results also raise the question of whether the clinical definition of COPD should be adjusted or whether a new entity that includes the population of patients with smoking-related chronic pulmonary disease who do not meet the standard criteria for airway obstruction should be considered. Although these current or former smokers with symptoms had spirometric results at enrollment that are generally considered to be normal, we do not know their “best” lung function. Thus, it is possible that had we been able to obtain measurements of lung function in the cohort of symptomatic participants in the years before they were enrolled in the study, we would have been able to compare the lung function at enrollment with the lung function at an earlier time point and show that obstruction had developed in these participants, even though they did not meet spirometric criteria for airway obstruction at enrollment.
This study has an important limitation. We did not enroll a random sample and cannot estimate the population prevalence of symptoms among current or former smokers with preserved pulmonary function. Indeed, some participants may have volunteered for this study because of symptoms. Neither point invalidates the central conclusion that some smokers with symptoms have exacerbations that are suggestive of COPD and that these persons are being treated as if they had COPD even though they do not meet the current criteria for a diagnosis of COPD.
In conclusion, respiratory symptoms and exacerbations are common in current or former smokers who have spirometric values that are generally considered to be within the normal range. Many of these patients are already being treated with respiratory medications despite a lack of data from clinical trials. This finding suggests that the current use of spirometry to define who should receive a diagnosis of COPD may not adequately cover the breadth of symptomatic smoking-related lung disease. Clinical trials that are directed at this large and under-studied population may provide better insight into appropriate treatment strategies for these patients.
Supplementary Material
Acknowledgments
Supported by grants (HHSN2682009000019C, HHSN268200900013C, HHSN268200900013C, HHSN268200900014C, HHSN268200900015C, HHSN268200900016C, HHSN268200900017C, HHSN268200900018C, HHSN268200900019C, and HHSN268200900020C) from the National Heart, Lung, and Blood Institute of the National Institutes of Health and by the Foundation for the National Institutes of Health through contributions made to an external advisory board that includes members from AstraZeneca, Bellerophon Therapeutics, Boehringer-Ingelheim Pharmaceuticals, Chiesi Farmaceutici, Forest Research Institute, GlaxoSmithKline, Grifols Therapeutics, Ikaria, Nycomed, Takeda Pharmaceutical, Novartis Pharmaceuticals, Regeneron Pharmaceuticals, and Sanofi.
We thank Susan Murray, Sc.D., for statistical advice.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 2.Martinez CH, Kim V, Chen Y, et al. The clinical impact of non-obstructive chronic bronchitis in current and former smokers. Respir Med. 2014;108:491–9. doi: 10.1016/j.rmed.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van der Molen T, Willemse BW, Schokker S, ten Hacken NH, Postma DS, Juniper EF. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes. 2003;1:13. doi: 10.1186/1477-7525-1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johns DP, Walters JA, Walters EH. Diagnosis and early detection of COPD using spirometry. J Thorac Dis. 2014;6:1557–69. doi: 10.3978/j.issn.2072-1439.2014.08.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Celli BR, Decramer M, Wedzicha JA, et al. An official American Thoracic Society/European Respiratory Society statement: research questions in COPD. Eur Respir Rev. 2015;24:159–72. doi: 10.1183/16000617.00000315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Couper D, LaVange LM, Han M, et al. Design of the Subpopulations and Intermediate Outcomes in COPD Study (SPIROMICS). Thorax. 2014;69:491–4. doi: 10.1136/thoraxjnl-2013-203897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 8.Global Initiative for Chronic Obstructive Lung Disease Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2015) http://www.goldcopd.org.
- 9.Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–54. doi: 10.1183/09031936.00102509. [DOI] [PubMed] [Google Scholar]
- 10.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 11.Patel BD, Coxson HO, Pillai SG, et al. Airway wall thickening and emphysema show independent familial aggregation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2008;178:500–5. doi: 10.1164/rccm.200801-059OC. [DOI] [PubMed] [Google Scholar]
- 12.Lin DY, Wei LJ, Yang I, Ying Z. Semi-parametric regression for the mean and rate functions of recurrent events. J R Stat Soc B. 2000;62:711–30. [Google Scholar]
- 13.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–6. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–68. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 15.Pinto LM, Gupta N, Tan W, et al. Derivation of normative data for the COPD assessment test (CAT). Respir Res. 2014;15:68. doi: 10.1186/1465-9921-15-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agusti A, Edwards LD, Celli B, et al. Characteristics, stability and outcomes of the 2011 GOLD COPD groups in the ECLIPSE cohort. Eur Respir J. 2013;42:636–46. doi: 10.1183/09031936.00195212. [DOI] [PubMed] [Google Scholar]
- 17.Agusti A, Hurd S, Jones P, et al. FAQs about the GOLD 2011 assessment proposal of COPD: a comparative analysis of four different cohorts. Eur Respir J. 2013;42:1391–401. doi: 10.1183/09031936.00036513. [DOI] [PubMed] [Google Scholar]
- 18.Salome CM, King GG, Berend N. Physiology of obesity and effects on lung function. J Appl Physiol (1985) 2010;108:206–11. doi: 10.1152/japplphysiol.00694.2009. [DOI] [PubMed] [Google Scholar]
- 19.Sin DD, Jones RL, Man SF. Obesity is a risk factor for dyspnea but not for airflow obstruction. Arch Intern Med. 2002;162:1477–81. doi: 10.1001/archinte.162.13.1477. [DOI] [PubMed] [Google Scholar]
- 20.Definition and classification of chronic bronchitis for clinical and epidemiological purposes: a report to the Medical Research Council by their Committee on the Aetiology of Chronic Bronchitis. Lancet. 1965;1:775–9. [PubMed] [Google Scholar]
- 21.Lopez-Campos JL, Agustí A. Heterogeneity of chronic obstructive pulmonary disease exacerbations: a two-axes classification proposal. Lancet Respir Med. 2015;3:729–34. doi: 10.1016/S2213-2600(15)00242-8. [DOI] [PubMed] [Google Scholar]
- 22.Beghé B, Verduri A, Roca M, Fabbri LM. Exacerbation of respiratory symptoms in COPD patients may not be exacerbations of COPD. Eur Respir J. 2013;41:993–5. doi: 10.1183/09031936.00180812. [DOI] [PubMed] [Google Scholar]
- 23.Tan WC, Bourbeau J, Hernandez P, et al. Exacerbation-like respiratory symptoms in individuals without chronic obstructive pulmonary disease: results from a population-based study. Thorax. 2014;69:709–17. doi: 10.1136/thoraxjnl-2013-205048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bowler RP, Kim V, Regan E, et al. Prediction of acute respiratory disease in current and former smokers with and without COPD. Chest. 2014;146:941–50. doi: 10.1378/chest.13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oelsner EC, Hoffman EA, Folsom AR, et al. Association between emphysema-like lung on cardiac computed tomography and mortality in persons without airflow obstruction: a cohort study. Ann Intern Med. 2014;161:863–73. doi: 10.7326/M13-2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Regan EA, Lynch DA, Curran-Everett D, et al. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern Med. 2015;175:1539–49. doi: 10.1001/jamainternmed.2015.2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.