Abstract
Background
Alcohol use, especially at binge levels, is associated with sexual HIV risk behavior, but the mechanisms through which alcohol increases sexual risk taking are not well examined. Delay discounting, that is, devaluation of future consequences as a function of delay to their occurrence, has been implicated in a variety of problem behaviors, including risky sexual behavior. Probability discounting is studied with a similar framework as delay discounting, but is a distinct process in which a consequence is devalued because it is uncertain or probabilistic.
Methods
Twenty-three, non-dependent alcohol users (13 male, 10 female; mean age = 25.3 years old) orally consumed alcohol (1 g/kg) or placebo in two separate experimental sessions. During sessions, participants completed tasks examining delay and probability discounting of hypothetical condom-protected sex (Sexual Delay Discounting Task, Sexual Probability Discounting Task) and of hypothetical and real money.
Results
Alcohol decreased the likelihood that participants would wait to have condom-protected sex versus having immediate, unprotected sex. Alcohol also decreased the likelihood that participants would use an immediately available condom given a specified level of STI risk. Alcohol did not affect delay discounting of money, but it did increase participants’ preferences for larger, probabilistic monetary rewards over smaller, certain rewards.
Conclusions
Acute, binge-level alcohol intoxication may increase sexual HIV risk by decreasing willingness to delay sex in order to acquire a condom in situations where one is not immediately available, and by decreasing sensitivity to perceived risk of STI contraction. These findings suggest that delay and probability discounting are critical, but heretofore unrecognized, processes that may mediate the relations between alcohol use and HIV risk.
Keywords: alcohol, delay discounting, condom use, sexual HIV risk, probability discounting
Introduction
Alcohol use is strongly associated with sexual HIV risk behavior, including failing to use condoms (Baliunas et al., 2010; Cooper, 2002, 2006; Scott-Sheldon et al., 2013). Specifically, event-level analyses identify a strong link between binge-level alcohol use (i.e., resulting in ≥0.08 g/dL blood alcohol concentration; or 4 [women] or 5 [men] drinks over the course of 2 hours; NIAAA, 2004) and unprotected sex (e.g., Vosburgh et al., 2012; Wray et al., 2015a). Moreover, experimental studies report lower condom use intentions following acute high-dose alcohol administration (Rehm et al., 2012). Collectively, these data suggest alcohol intoxication increases sexual HIV risk behavior.
Despite data linking alcohol intoxication to sexual HIV risk behavior, there is little consensus on how alcohol intoxication influences decisions about condom use (George and Stoner, 2000). One candidate mechanism involves delay discounting, a behavioral process describing the devaluation of consequences when they are delayed (Rachlin et al., 1991). Delay discounting studies have shown that preference for small, immediate rewards over larger, delayed rewards is associated with a wide variety of problematic behaviors (e.g., Bickel et al., 2012). Delay discounting may be particularly relevant in sexual situations if a condom is not available and an individual is faced with a choice between having unprotected sex immediately or waiting to obtain a condom for sex later. Although the individual's preference may be to use a condom if available, a delay to condom availability may decrease the value of condom-protected sex, and increase the likelihood of having unprotected sex. Alcohol may exaggerate delay discounting, such that the value of condom-protected sex is more severely discounted when intoxicated. In other words, alcohol may elevate sexual HIV risk by acutely increasing preference for immediate, unprotected sex over delayed condom-protected sex.
Delay discounting of condom-protected sex has been examined in previous studies using the Sexual Delay Discounting Task (Dariotis and Johnson, 2015; Herrmann et al., 2014; Herrmann et al., 2015; Johnson and Bruner, 2012, 2013; Johnson et al., 2015a). In these studies, reported likelihood of engaging in condom-protected sex reliably decreased as a function of increasing delays to condom availability. Greater sexual delay discounting was significantly correlated with self-reported sexual HIV risk behavior (Dariotis and Johnson, 2015; Herrmann et al., 2015; Johnson and Bruner, 2012) and drug use (Dariotis and Johnson, 2015), and differs between individuals with substance use disorders and matched controls (Herrmann et al., 2014; Johnson et al., 2015a). Despite its relation to substance use, no study has used the Sexual Delay Discounting task to examine how acute effects of drugs (e.g., alcohol) may contribute to sexual HIV risk behavior.
Although alcohol effects on delay discounting of condom-protected sex have yet to be examined, research supports the conclusion that alcohol does not affect delay discounting of money, the most common commodity examined in human discounting studies. Several studies show no statistically significant alcohol effect on delay discounting of money (Bidwell et al., 2013; Ortner et al., 2003; Reynolds et al, 2006; Richards et al., 1999). Two studies have claimed alcohol to increase money discounting, but their results have important limitations. One study found the effect using a delay discounting task involving real monetary rewards that confounded the effect of delay with the effect of probability (Reynolds et al., 2006). Moreover, participants may have maximized local rates of reinforcement by choosing small, immediate rewards to the exclusion of larger, delayed rewards, thereby confounding the effect of reward delay on choice (Madden and Johnson, 2010). Another study claiming alcohol administration increased delay discounting of money appears to have applied parametric statistics to a discounting metric (k value) that typically shows a strongly skewed distribution, calling test validity into question (Reed et al., 2012).
The present within-subjects, double-blind, placebo-controlled study examined the effects of an acute alcohol dose (1 g/kg) on discounting of condom-protected sex in the Sexual Delay Discounting Task. We also examined alcohol effects on the Sexual Probability Discounting Task (Johnson et al., 2015a). Probability discounting is studied with a similar framework as delay discounting, but is a distinct process in which a consequence is devalued because it is uncertain (Rachlin et al., 1991). In addition, we administered delay and probability discounting tasks involving both hypothetical and real monetary rewards, to replicate previous studies suggesting no effect of alcohol on delay discounting of money. The inclusion of the monetary tasks allowed us to test whether alcohol has domain-specific effects on discounting. In other words, alcohol may show a detrimental effect on the discounting of sexual but not monetary outcomes (see Johnson and Bruner, 2012; Lawyer and Schoepflin, 2013).
Materials and Methods
Participants
Participants (n = 23) were recruited using flyers, Internet, and newspaper advertisements. Eligible participants were 21-65 years of age, were literate as evidenced by reading aloud the consent form, and reported drinking 4-5 drinks per episode at least occasionally. Participants were excluded if they were physically dependent on any substance (excluding nicotine and caffeine), were seeking treatment for substance use, reported a current major psychiatric disorder or psychiatric hospitalization in the past 6 months, had medical contraindications to alcohol administration, or had never had sexual intercourse (i.e., vaginal or anal sex). Female participants were excluded if pregnant, nursing, or not using effective contraception. Demographic information is shown in Table 1. Participants received $40 for completing an in-person screening session and an additional $160 for completing both experimental sessions. The Johns Hopkins University Institutional Review Board approved the study.
Table 1.
Demographic information.
| Characteristic | n (%) | Mean (SD) |
|---|---|---|
| Gender | ||
| Male | 13 (57) | |
| Female | 10 (43) | |
| Race | ||
| Caucasian/white | 15 (65) | |
| More than 1 race | 5 (22) | |
| African American/black | 2 (9) | |
| Asian | 1 (4) | |
| Sexual orientation | ||
| Heterosexual | 18 (78) | |
| Bisexual | 5 (22) | |
| Marital status | ||
| Single | 22 (96) | |
| Divorced | 1 (4) | |
| Smoking status | ||
| Non-smoker | 17 (74) | |
| Smoker† | 6 (26) | |
| Age (years) | 25.3 (3.7) | |
| Education (years completed) | 15.3 (1.5) | |
| Monthly income (U.S. dollars) | 1,169.6 (1,021.4) | |
| Alcoholic drinks (per week) | 14.6 (12.9) | |
| HRBS Sexual Risk Subscale Score | 5.2 (4.2) |
All participants identified as non-Hispanic.
HRBS, HIV Risk-Taking Behavior Scale.
Volunteers who identified as smokers smoked an average of 7.4 cigarettes/day (SD= 6.8).
Procedure
Participants meeting preliminary criteria via telephone attended a 2-hour in-person screening session. Participants completed demographic information, medical history, and a verbal intelligence assessment (Quick Test; Ammons and Ammons, 1962). We assessed drug use history and used a checklist to assess DSM-IV-TR criteria for drug abuse and dependence (Hudziak et al., 1993). In preparation for the sexual discounting tasks, participants viewed a set of 60 pictures (30 men and 30 women) and selected photographs of individuals they would be interested in having sex with in a hypothetical casual sex scenario and assigned photographs to four partner conditions: (i) the person they would most want to have sex with, (ii) the person they would least want to have sex with, (iii) the person they judged most likely to have a sexually transmitted infection (STI), and (iv) the person they judged least likely to have an STI. Although the same photograph could be assigned to more than 1 partner condition, it could not be assigned to both the “most” and “least” partner within the same dimension (e.g., the same photograph could not be both “most want to have sex with” and “least want to have sex with”). Participants were disqualified from the study if they selected < 2 photographs or, if the participant was female, selected only hypothetical female sexual partners (given the extremely low risk of female-to-female HIV transmission; CDC, 2014).
Participants also completed the HIV Risk-Taking Behavior Scale (Darke et al., 1991), an 11-item questionnaire assessing injection drug use (6 items) and sexual risk behavior (5 items). Given the focus of the present research, we present only data from the sexual risk subscale, which asked participants to report, for example, number of past-month sexual partners and frequency of condom use with regular and casual partners. Additional personality inventories were also administered during screening, but are not reported here as they are beyond the scope of the present analyses. Three qualified individuals indicated they were no longer interested in participating upon being contacted after the in-person screening.
Drug Administration
Participants completed two experimental sessions lasting 8 hours each. Participants were told to refrain from using alcohol 12 hours before a session, but to otherwise maintain their normal routine (e.g., sleep, caffeine consumption). Participants provided a zero breath alcohol concentration (BrAC) reading upon arrival or the session was rescheduled. Participants ate a standardized low-fat breakfast (two toast slices or 1 bagel; single-serving jelly or butter; juice) approximately 30 minutes before drug administration.
Placebo and alcohol-containing solutions were prepared in an onsite pharmacy. A weight-based administration procedure was used to determine the volume of a 1 g/kg alcohol dose (USP 95% ethanol; Letco Medical, Decatur, AL) or water to be mixed in grapefruit juice. Total solution volume was determined per bodyweight so that alcohol (or added water) was 8% of solution by volume. This was divided equally across three cups. Participants experienced placebo and alcohol sessions in a pseudo-random order. Each cup was fitted with a lid and a straw with a 95% alcohol-soaked elastic hairband wrapped around it to obscure olfactory discrimination of alcohol and placebo sessions. Drinks were served promptly after being refrigerated at ~4 °C. Participants were instructed to drink 1 cup at a regular pace over the course of a 20-minute interval, resulting in a 1-hour administration period for all three cups. The approximate timing of experimental events is shown in Table 2. Primary sexual and money discounting tasks were scheduled to occur near peak drug effects. Additional discounting tasks were administered after these time points, but are not immediately relevant to the present analyses.
Table 2.
Timing of relevant experimental events.
| Approximate time | Time point (min post administration) | Experimental event |
|---|---|---|
| 9:00 a.m. – 10:00 a.m. | 0-60 min | Beverage administration |
| 10:30 a.m. – 11:00 a.m. | 90-120 min | SEQ and vital signs |
| Task Block 1 | ||
| QDOT-2 | ||
| or | ||
| Hypothetical Money Delay Discounting Task | ||
| Hypothetical Money Probability Discounting Task | ||
| Sexual Probability Discounting Task | ||
| 11:00 a.m. – 11:30 a.m. | 120-150 min | SEQ and vital signs |
| BrAC reading | ||
| Task Block 2 | ||
| Sexual fantasy period | ||
| SADI | ||
| Sexual Delay Discounting Task | ||
| Sexual Desire Task | ||
| 11:30 a.m. – 12:00 p.m. | 150-180 min | SEQ and vital signs |
| Task Block 3 | ||
| QDOT-2 | ||
| or | ||
| Hypothetical Money Delay Discounting Task | ||
| Hypothetical Money Probability Discounting Task | ||
| Sexual Probability Discounting Task |
SEQ = Subjective Effects Questionnaire; QDOT-2 = Quick Discounting Operant Task-2; BrAC = breath alcohol concentration; SADI = Sexual Arousal and Desire Inventory. The assignment order of tasks to Task Blocks 1 and 3 (i.e., QDOT-2 in Task Block 1 and other discounting tasks in Task Block 3, or vice versa) was randomized to control for potential differences in performance as a function of time since drug administration.
After the session, participants were discharged if their BrAC reading was ≤ .04 g/dL and they showed no behavioral impairment. Participants were not permitted to drive to or from experimental sessions.
Materials
Breath alcohol concentration
Before drug administration and at 1-hour intervals post administration, a second, unblinded research assistant used a breathalyzer (Alco-Sensor IV, Intoximeters, Inc., St. Louis, MO) to measure BrAC.
Subjective effects and vital signs
Before drug administration and at every 30-minute interval post administration, participants completed the 38-item Subjective Effects Questionnaire (SEQ). Participants were asked to rate the degree to which each drug effect was currently being experienced as a result of the drink consumed earlier. Blood pressure and heart rate were also monitored.
Sexual arousal measures
Sexual fantasy and the Sexual Arousal and Desire Inventory
Participants wore eyeshades and headphones, sat in a comfortable chair, and were instructed to fantasize about a sexual experience for 3 minutes. The participant then completed the Sexual Arousal and Desire Inventory (SADI; Toledano and Pfaus, 2006). Participants were presented with 54 descriptors corresponding to positive or negative subjective aspects of sexual arousal and desire and were asked to indicate to what extent particular phrases described how the volunteer felt while fantasizing. Four factors (Evaluative, Physiological, Motivational, and Negative/Aversive) were scored as the sum of the scores of factor-specific descriptors.
Sexual Desire Task
While viewing a set of 60 printed (21.59 cm × 27.94 cm) color photographs of diverse, clothed individuals (30 men, 30 women; different photographs than those used in the Sexual Delay and Probability Discounting Tasks), participants selected individuals they would consider having sex with in the right environment and if they liked the individual's personality. The dependent measure was the number of photographs selected.
Sexual discounting tasks
Sexual Delay Discounting Task
We administered a computerized version of the Sexual Delay Discounting Task (Herrmann et al., 2014; Johnson et al., 2015a). The partner conditions were presented in a pseudo-random order that was fixed across sessions. On the first trial of each partner condition, the participant was instructed to pretend that they were not in a committed relationship, that the hypothetical partner was interested in having sex now, that there was no chance of pregnancy, and that a condom was immediately available. Using a visual analog scale ranging from “I will definitely have sex with this person without a condom” (0%) to “I will definitely have sex with this person with a condom” (100%), the participant indicated her/his likelihood of using an immediately available condom. Subsequent trials involved the same scenario except condom access was delayed (1 h, 3 h, 6 h, 1 day, 1 week, 1 month, and 3 months). Participants used a visual analog scale ranging from “I will definitely have sex with this person now without a condom” (0%) to “I will definitely wait [delay] to have sex with this person with a condom” (100%) to indicate their likelihood of waiting to have condom-protected sex.
Sexual Probability Discounting Task
The Sexual Probability Discounting Task assessed a participant's likelihood of using an immediately available condom given a specified risk of contracting an STI if a condom was not used. Only most and least “want to have sex with” partner conditions were assessed. Instructions regarding the hypothetical sexual scenario were similar to the Sexual Delay Discounting Task (for further details, see Johnson et al., 2015a). Participants indicated their likelihood of using a condom via a visual analog scale ranging from “I will definitely have sex with this person without a condom” to “I will definitely have sex with this person with a condom.” Odds in favor (with corresponding percent chance) of contracting an STI were 1 in 1 (100%), 1 in 3 (33%), 1 in 13 (8%), 1 in 100 (1%), 1 in 400 (0.25%), 1 in 700 (0.14%), 1 in 2,000 (0.05%), and 1 in 10,000 (0.01%).
Monetary discounting tasks
Real Money Delay Discounting (Quick Discounting Operant Task-2)
The Quick Discounting Operant Task-2 (QDOT-2) is a real-reward discounting task based on the QDOT (Johnson, 2012) that involved repeated choices between a small, immediate amount of money and a large, delayed (5, 10, 20, 40, and 80 s) amount of money (80¢). Like the QDOT, the QDOT-2 featured 5 blocks of 4 choice trials. Based on a participant's choices, the smaller amount available immediately (40¢ on the first trial in each block) was adjusted between trials to determine an indifference point (i.e., an immediate amount of money deemed subjectively equivalent to the 80¢ delayed reward) for that particular delay block (for details, see Johnson, 2012).
The difference between the QDOT and the QDOT-2 is that in the QDOT, participants can complete the decision-making component of the task sooner if they select the smaller-sooner reward than if they select the larger-later reward. Although the QDOT contains a programmed post-session waiting period designed to discourage exploitation of this contingency, it is possible that participants’ choices for the smaller-sooner reward are made in an effort to maximize local reinforcement rate. The QDOT-2 eliminated this confound by beginning trials after a fixed amount of time had elapsed from the beginning of the previous trial, regardless of which reward option was selected.
Hypothetical Money Delay Discounting Task
A computerized task used previously (e.g., Johnson and Bickel, 2002) assessed delay discounting of hypothetical money ($100) using delays to receiving $100 of 1 day, 1 week, 1 month, 6 months, 1 year, 5 years, and 25 years. Indifference points were determined at each delay using a procedure in which a smaller, immediate amount of money was titrated over the course of repeated trials based on a participant's choices (Richards et al., 1999).
Hypothetical Money Probability Discounting Task
A computerized task used previously (e.g., Yi et al., 2005) assessed probability discounting of hypothetical money ($100) using probabilities of receiving $100 of 99%, 90%, 75%, 50%, 25%, 10%, and 1%. Indifference points were determined at each probability using an adjusting-amount procedure.
Data Analysis
Nonsystematic discounting data
Criteria were used to identify nonsystematic discounting data (Johnson and Bickel, 2008; Johnson et al., 2015b). The first criterion was that, starting with the second-shortest delay (or odds against), no data point could be greater than the data point from the immediately preceding delay (or odds against) by more than .20. Second, the data point from the longest delay or highest odds against could not be greater than the data point from the 0-delay or 0-odds-against trial by more than .10. A third criterion was also applied to data from the hypothetical money discounting tasks: The indifference point at the longest delay (25 years) or highest odds against (99) could not be greater than .90. This last criterion was applied to monetary but not sexual tasks because it seems plausible that some individuals would use condoms in casual sex situations regardless of delay or STI probability. In contrast, we judge it implausible that individuals would wait 25 years to receive $100 rather than receive $92 now, or would prefer a 1% chance of receiving $100 rather than a certain $92. In the event that a participant's discounting data violated 1 or more of these criteria, both sessions’ data from that task were excluded for that particular analysis.
Standardized values in sexual discounting tasks
Because individuals differed in their reported likelihood of using a condom at the shortest delay (or lowest odds against), individual likelihood values were standardized by dividing each value by its respective 0-delay trial (or 0-odds-against trial) likelihood in order to isolate the effect of delay (or probability) on condom use. Individuals who indicated a zero likelihood of condom use in the 0-delay or 0-odds-against trial were excluded from these analyses. In the event that a standardized likelihood value exceeded 1, it was assigned a value of 1. Instances of standardized values exceeding 1 occurred infrequently in both sexual discounting tasks (4.2% of all non-0-delay standardized values in the Sexual Delay Discounting Task; 1.9% of all non-0-odds-against standardized values in the Sexual Probability Discounting Task). Statistical conclusions based on standardized values capped at 1 did not differ in any case from conclusions based on uncapped values; we therefore report the results of analyses conducted with capped standardized likelihood values.
Statistical comparison of discounting functions
Discounting data from placebo and alcohol sessions were compared using extra sums-of-squares F-tests (GraphPad Prism, La Jolla, CA; Johnson et al., 2015a) to evaluate best-fit two-parameter hyperboloid discounting curves (Myerson and Green, 1995). Extra sums-of-squares F-tests assessed whether there was significantly less model error using separate best-fit curves for each session relative to 1 best-fit curve for both sessions. If p < .05, then separate curves best characterize data from the two sessions (i.e., discounting differs between placebo and alcohol sessions).
Results
Breath alcohol concentration
BrAC was examined using a mixed-model analysis of variance with the between-subjects factor of Gender (male/female) and the within-subjects factor of Time (60, 120, and 180 minutes post administration). Neither the Gender x Time interaction (p = .08) nor the main effect of Gender (p = .59) were significant for BrAC. Data presented in Table 3 are therefore collapsed across male and female participants. Peak BrAC (p = .32) and time to peak BrAC (p = .11) were also not significantly different between male and female participants (data not shown).
Table 3.
Mean (±SEM) breath alcohol concentration, subjective effects ratings, sexual arousal and desire measures, and vital signs from relevant time points in placebo and alcohol sessions.
| Measure | Time point (min post administration) | Placebo | Alcohol |
|---|---|---|---|
| BrAC | 60 | 0.000 (0.000) | 0.093 (0.005) |
| 120 | 0.000 (0.000) | 0.087 (0.003) | |
| 180 | 0.000 (0.000) | 0.074 (0.003) | |
| SEQa | |||
| Feel a drug effect | 90 | 0.39 (0.20) | 2.91 (0.23)**** |
| 120 | 0.35 (0.18) | 2.65 (0.21)**** | |
| 150 | 0.30 (0.16) | 2.48 (0.23)**** | |
| 180 | 0.23 (0.13) | 2.26 (0.25)**** | |
| Like drug effect | 90 | 0.43 (0.24) | 2.91 (0.23)**** |
| 120 | 0.39 (0.24) | 2.57 (0.23)**** | |
| 150 | 0.48 (0.24) | 2.43 (0.25)*** | |
| 180 | 0.32 (0.20) | 2.26 (0.30)*** | |
| Dislike drug effect | 90 | 0.09 (0.06) | 0.30 (0.12) |
| 120 | 0.09 (0.06) | 0.30 (0.10) | |
| 150 | 0.09 (0.06) | 0.52 (0.16)** | |
| 180 | 0.05 (0.04) | 0.70 (0.21)**** | |
| Feel stimulant effect | 90 | 0.30 (0.15) | 1.78 (0.25)*** |
| 120 | 0.35 (0.18) | 1.48 (0.23)** | |
| 150 | 0.30 (0.16) | 1.17 (0.24)** | |
| 180 | 0.23 (0.13) | 1.17 (0.26)** | |
| Feel sedative effect | 90 | 0.17 (0.08) | 1.39 (0.24)**** |
| 120 | 0.17 (0.10) | 1.48 (0.23)**** | |
| 150 | 0.13 (0.10) | 1.52 (0.23)**** | |
| 180 | 0.14 (0.07) | 1.48 (0.25)**** | |
| Feel sexually aroused | 90 | 0.13 (0.07) | 0.57 (0.22)**** |
| 120 | 0.13 (0.07) | 0.70 (0.21)**** | |
| 150 | 0.13 (0.07) | 0.78 (0.27)**** | |
| 180 | 0.09 (0.06) | 0.74 (0.27)**** | |
| SADI | 120 | ||
| Evaluative factor | 58.91 (6.00) | 54.43 (8.44) | |
| Physiological factor | 32.35 (4.13) | 33.22 (5.29) | |
| Motivational factor | 21.22 (2.32) | 21.74 (3.18) | |
| Negative/Aversive factor | 9.74 (1.88) | 15.65 (2.67)** | |
| Sexual Desire Task | 120 | ||
| Number of pictures | 7.91 (1.10) | 9.39 (1.08)* | |
| Vital signs | |||
| Systolic BP | BL | 114.04 (3.05) | 114.13 (2.92) |
| 90 | 117.87 (2.57) | 114.22 (2.97) | |
| 120 | 113.65 (2.46) | 110.52 (3.18) | |
| 150 | 111.22 (3.23) | 108.17 (2.97) | |
| 180 | 112.22 (2.72) | 110.70 (2.33) | |
| Diastolic BP | BL | 64.30 (2.38) | 62.04 (2.15) |
| 90 | 62.74 (2.48) | 59.43 (2.18) | |
| 120 | 63.35 (2.16) | 59.61 (1.95) | |
| 150 | 60.04 (2.60) | 59.17 (1.98) | |
| 180 | 61.09 (2.28) | 57.91 (2.08) | |
| Heart rate | BL | 70.39 (2.68) | 68.50 (2.18)† |
| 90 | 73.87 (2.36) | 88.65 (3.29)**** | |
| 120 | 75.17 (2.76) | 89.30 (3.76)**** | |
| 150 | 70.78 (2.85) | 84.96 (3.76)**** | |
| 180 | 69.87 (2.52) | 80.91 (3.49)**** |
BrAC = breath alcohol concentration; SEQ = Subjective Effects Questionnaire; SADI = Sexual Arousal and Desire Inventory; BP = blood pressure; BL = baseline. SEQ items were rated on a 5-point scale where 0 = “not at all,” 1 = “possibly mild, but not sure,” 2 = “definitely mild,” 3 = “moderately,” and 4 = “strongly.” SADI scores were calculated as the sum of all descriptor scores for Evaluative (e.g., “enthusiastic,” “wet/hard,” “hot”), Physiological (e.g., “tingly all over,” “sensitive to touch,” “lustful”), Motivational (e.g., “anticipatory,” “driven,” “urge to satisfy”), and Negative/Aversive (e.g., “restrained,” “anxious,” “frigid”) factors. SADI items were rated on a 0-5 scale, where 0 is “does not describe it at all” and 5 is “describes it perfectly”. Bonferonni-corrected pairwise comparisons were conducted to examine the drug effect at each time point for the SEQ. Scores for each of the SADI factors and number of pictures selected in the Sexual Desire Task were compared using paired-samples t-tests.
Due to experimenter error, ratings were not conducted at the 180 post administration time-point in the placebo session for one participant. All ratings from time points immediately preceding and following the 180 time point were 0, and so this value was substituted.
Baseline heart rate was 1 missing for one participant before the alcohol session; baseline heart rate before the placebo session was substituted for this missing value.
p < .05.
p < .01.
p < .001.
p < .0001.
Subjective effects and vital signs
Table 3 displays mean subjective effects ratings and vital signs as a function of post-administration time point and session. Alcohol significantly increased all subjective effects ratings and heart rate for at least 1 time point, but did not affect blood pressure.
SADI and Sexual Desire Task
Only scores on the Negative/Aversive factor of the SADI were significantly increased by alcohol relative to placebo (p < .01; Table 3). Participants also chose a significantly greater number of pictures in the Sexual Desire Task in alcohol versus placebo sessions (p = .04).
Likelihood of condom use in 0-delay/0-odds-against trials
Likelihood of condom use in 0-delay and 0-odds-against trials of the sexual discounting tasks was compared between placebo and alcohol sessions using Wilcoxon signed-ranks tests because data were nonnormally distributed. There was no effect of alcohol on likelihood of using an immediately available condom in the Sexual Delay Discounting Task (all p values ≥ .19), or on likelihood of using a condom when the odds against STI contraction were 0 (i.e., 100% chance of STI contraction) in the Sexual Probability Discounting Task (“most want to have sex with,” p = .50; “least want to have sex with,” p = .09).
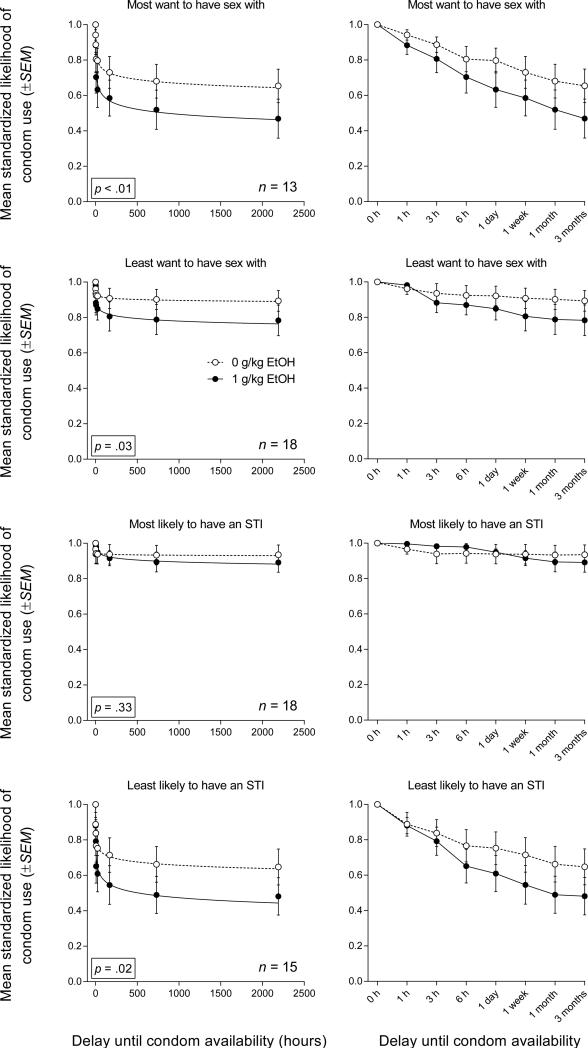
Sexual Delay Discounting
Figure 1 (left column) shows best-fit discounting curves to mean standardized likelihoods of condom use from each partner condition in placebo and alcohol sessions. The right column displays these same data equidistantly on an ordinal x-axis. The left column is optimized to visually assess these data as discounting functions, whereas the right column (ordinal display) is optimized for visually comparing alcohol and placebo conditions, especially at shorter delays. Alcohol increased the rate at which condom-protected sex was discounted as a function of delay to condom availability in 3 of 4 partner conditions: the “most want to have sex with” partner, F(2, 204) = 5.31, p < .01, the “least want to have sex with” partner, F(2, 284) = 3.56, p = .03, and the “least likely to have an STI” partner, F(2, 236) = 4.17, p = .02. Delay discounting of condom-protected sex with the “most likely to have an STI” partner was not significantly affected by alcohol (p = .33).
Fig. 1.
Left column: Best-fit curves to mean standardized likelihood of condom use (proportion of visual analog scale) in each of the Sexual Delay Discounting Task partner conditions in placebo (open symbols) and alcohol (closed symbols) sessions. Right column: Data from left column with delay to condom availability expressed ordinally on the x-axis. Error bars represent ±SEM.
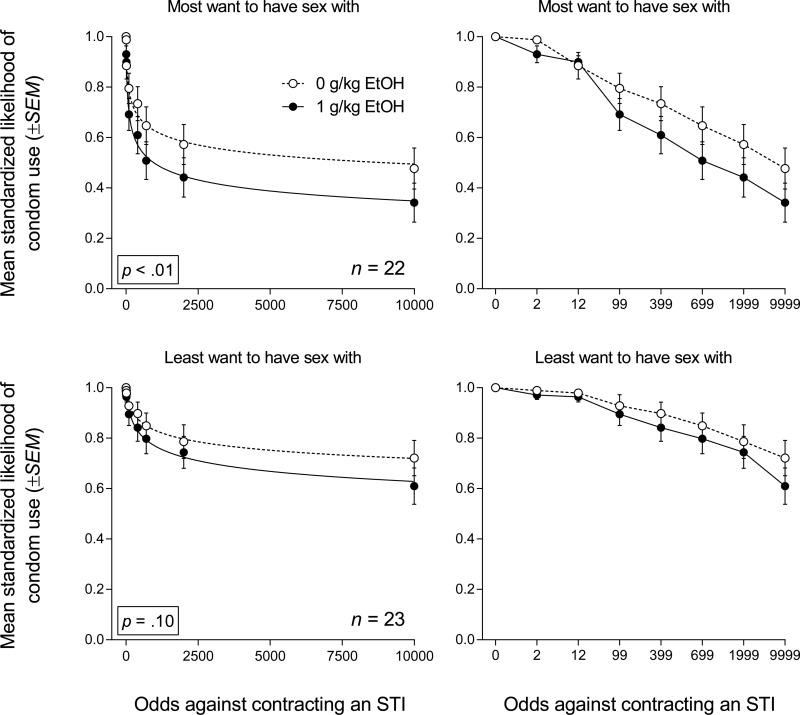
Sexual Probability Discounting
Figure 2 (left column) shows best-fit discounting curves to mean standardized likelihood values from each partner condition in placebo and alcohol sessions. The right column displays these same data equidistantly on an ordinal x-axis to more clearly display low-odds-against likelihood values. Alcohol significantly increased discounting of condom-protected sex as a function of odds against STI contraction in the “most want to have sex with” partner, F(2, 348) = 5.51, p < .01, but not in the “least want to have sex with” partner condition (p = .10).
Fig. 2.
Left column: Best-fit curves to mean standardized likelihood of condom use (proportion of visual analog scale) in each of the Sexual Probability Discounting Task partner conditions in placebo (open symbols) and alcohol (closed symbols) sessions. Right column: Data from left column with odds against STI contraction expressed ordinally on the x-axis. Error bars represent ±SEM.
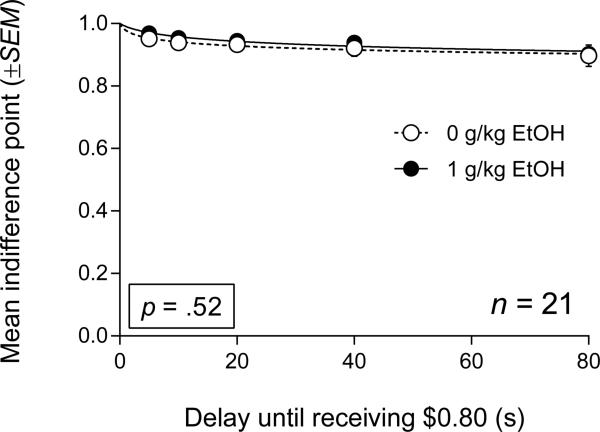
Real Money Delay Discounting (QDOT-2)
QDOT-2 data and best-fit curves are shown in Figure 3. Discounting did not differ significantly between placebo and alcohol sessions (p = .52).
Fig. 3.
Best-fit curves to mean indifference points (proportion of 80¢) from the QDOT-2. Data from placebo and alcohol sessions are designated by open and closed symbols, respectively. Error bars represent ±SEM.
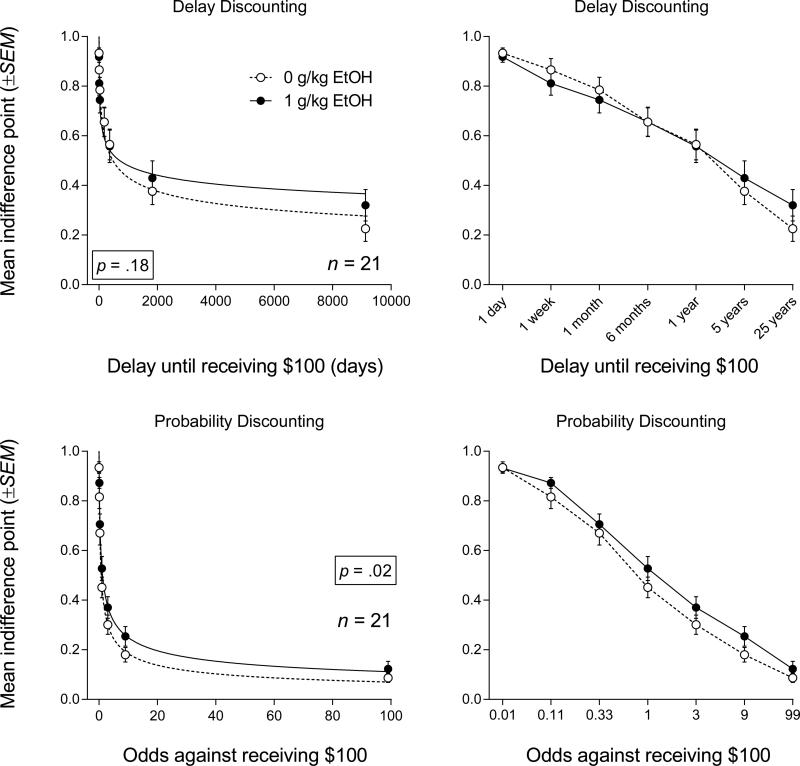
Hypothetical Money Delay Discounting
Figure 4 (top row) displays best-fit discounting curves to mean indifference points from the Hypothetical Money Delay Discounting Task in placebo and alcohol sessions (left graph; right graph shows ordinal plot). Alcohol did not significantly affect discounting of $100 (p = .18).
Fig. 4.
Top row: Best-fit curves to mean indifference points (proportion of $100) from the Hypothetical Money Delay Discounting Task (left graph; right graph shows data with delay expressed ordinally). Bottom row: Best-fit curves to mean indifference points (proportion of $100) from the Hypothetical Money Probability Discounting Task (left graph; right graph shows data with odds against expressed ordinally). Data from placebo and alcohol sessions are designated by open and closed symbols, respectively. Error bars represent ±SEM.
Hypothetical Money Probability Discounting
The bottom row of Figure 4 displays best-fit discounting curves to mean indifference points from the Hypothetical Money Probability Discounting Task in placebo and alcohol sessions (left graph; right graph shows ordinal plot). Discounting in alcohol sessions was significantly less steep than discounting in placebo sessions (p = .02), indicating decreased sensitivity to risk.
Discussion
This study provides novel evidence that the robust relations between binge alcohol use and risky sexual behavior may be related to acute alcohol effects on delay and probability discounting. Our finding that alcohol led to significantly steeper discounting in the Sexual Delay Discounting Task highlights the previously unexamined role of delay to reinforcement in influencing intoxicated individuals’ condom use choices. Discounting in the Sexual Probability Discounting Task was also significantly steeper in alcohol sessions for 1 partner condition, demonstrating sensitivity of the task to the effect of alcohol on STI risk. Although alcohol significantly increased risk taking involving hypothetical probabilistic money, it had no effect on the discounting of real or hypothetical delayed money. Thus, the specificity of alcohol-related effects observed in the present study emphasizes the importance of examining multiple independent variables (e.g., delay, probability, outcome type) likely to influence decision making while intoxicated.
Following administration of alcohol, participants reported being significantly less likely to wait for a delayed condom in 3 of 4 partner conditions in the Sexual Delay Discounting Task. This finding joins a growing literature documenting an association between alcohol intoxication in controlled research settings and increased self-reported likelihood of engaging in unprotected sex (e.g., Davis et al., 2014; George et al., 2014; Rehm et al., 2012; Wray et al., 2015b). However, unlike procedures typically used to investigate alcohol effects on condom use intentions, the Sexual Delay Discounting Task is able to dissociate participants’ likelihood of using a condom when one is immediately available (condom preference) from the effect of delay on participants’ likelihood of condom use (delay discounting of condom-protected sex). This innovative feature of the task enabled us to discern that only 1 of these behavioral processes was affected by alcohol, namely delay discounting of condom-protected sex. Intriguingly, alcohol had no effect on participants’ likelihood of using an immediately available condom in any partner condition. While the latter finding may appear at odds with the extant literature, a non-trivial minority of experimental studies show a null effect of alcohol on condom use intentions (see Rehm et al., 2012). In the present study, the absence of significant alcohol effects on immediate condom use likelihood may have been due to a lack of statistical power. Of the 6 sexual discounting partner conditions examined (4 from the Sexual Delay Discounting Task, 2 from the Sexual Probability Discounting Task), median likelihoods of condom use in placebo sessions were either greater than or equivalent to likelihood values observed in alcohol sessions, suggesting a larger sample size may have enabled us to observe significant alcohol-related reductions in immediate condom preference. Nonetheless, even if such reductions were observed in a larger sample, the present results indicate a significant effect of alcohol on condom-use decisions when delay is involved. The present study is the first to document an alcohol-induced increase in the discounting of a delayed sexual outcome, suggesting that, in addition to being reliable and internally and externally valid, the Sexual Delay Discounting Task is sensitive to pharmacological manipulation.
Alcohol also increased the likelihood that participants would engage in unprotected sex given a specified level of STI risk in the Sexual Probability Discounting Task. Research on the effects of alcohol administration on intentions to engage in unprotected sex with risky partners (e.g., Kruse and Fromme, 2005; Purdie et al., 2011) remains limited and mixed. An important determinant of alcohol's effects on STI risk behavior may be one's position on the BrAC curve (i.e., ascending vs. descending limb). In a study by Kruse and Fromme (2005), men's intentions to use condoms with a hypothetical sexual partner were less likely to be influenced by perceived risks (e.g., likelihood of partner having an STI) during the descending limb of the BrAC time course compared to the ascending limb. This finding suggests that potential negative consequences associated with unprotected sex such as STI contraction may affect sexual decision making less under the influence of alcohol, and that this is especially true for decisions made on the descending limb as was the case in the present study.
Probability discounting of hypothetical money was also significantly increased in alcohol sessions. That is, participants valued a probabilistic $100 reward to a higher degree and were therefore more likely to take risks involving money when intoxicated relative to when they had not consumed alcohol. Although this finding is consistent with a report by Bidwell et al. (2013) in which alcohol (0.4 and 0.8 g/kg) produced significantly less steep probability discounting of money on the descending limb in non-dependent drinkers, it is in contrast to a report by Richards et al. (1999) in which similar alcohol doses (0.5 and 0.8 g/kg) had no effect on probability discounting of money in non-dependent drinkers. One possible explanation for these discrepant outcomes involves the timing of task administration. Specifically, participants in Richards and colleagues (1999) completed the probability discounting task 30 minutes after the beginning of administration and, although not reported, likely during the ascending limb. Interestingly, Bidwell and colleagues (2013) reported less change in probability discounting during the ascending limb compared to the descending limb, a finding consistent with Kruse and Fromme's (2005) result showing that sexual risks were less likely to influence unprotected sex intentions on the descending limb. Beyond these experimental data, the clinical implications of limb-specific insensitivity to risk is especially concerning given the relative brevity of the ascending limb, which only further increases the likelihood that alcohol-related sexual encounters occur during a prolonged descending limb.
As in previous studies (e.g., Richards et al., 1999), alcohol did not significantly affect delay discounting of hypothetical money. While this null finding may have been due to limited statistical power in the present study, other studies have failed to detect significant drug effects using this particular task (Weafer et al., 2014). Interestingly, of the studies that have shown an acute effect of alcohol on delay discounting measures, all have implemented procedures involving real rewards, and in some cases, real delays (Dougherty et al., 2008; Reed et al., 2012; Reynolds et al., 2006). However, although Dougherty and colleagues (2008) and Reynolds and colleagues (2006) used experiential versions of the task, both procedures, like the QDOT (Johnson, 2012), enabled participants to maximize local rates of reinforcement if smaller-sooner rewards were chosen consistently. If, in alcohol sessions, participants were more likely to exploit this contingency, then discounting in these studies would have appeared to be steeper relative to placebo. We addressed this confound in the present study through our use of the QDOT-2 and found no effect of alcohol on performance in an experiential discounting task. This suggests intoxicated participants in previous studies may have been more motivated to choose smaller-sooner rewards because their selection maximized local rates of reinforcement. However, it should be acknowledged that discounting curves obtained via the QDOT-2 were extremely shallow in both sessions. Barring evidence of sensitivity to reward delays in placebo sessions, it is difficult to determine whether the lack of discounting in alcohol sessions is a null effect of the drug or an artifact of the procedure itself. This potential confound notwithstanding, our findings speak to the impact of procedural differences on conclusions regarding the effects of alcohol on delay discounting.
One study limitation is that the sexual scenarios presented were hypothetical. Still, the Sexual Delay Discounting Task is significantly correlated with self-reported sexual HIV risk behavior (Dariotis and Johnson, 2015; Herrmann et al., 2014; Herrmann et al., 2015; Johnson and Bruner, 2012), suggesting the task is a valid measure of real-world sexual risk, and several studies have shown that individuals discount hypothetical and real rewards in a similar manner (e.g., Johnson and Bickel, 2002; Baker et al., 2003; Johnson et al., 2007). A second limitation is that previous studies examining condom use intentions have shown reliable increases in sexual arousal in women (e.g., George et al., 2011; Norris et al., 2009; Schacht et al., 2007) and both genders (George et al., 2009) following alcohol administration. Although we observed significant increases in self-reported sexual arousal in the SEQ, at none of the relevant time points did mean ratings exceed 1 on a 5-point scale. Moreover, we observed only limited sensitivity of the SADI to alcohol administration with only scores on the Negative/Aversive factor (e.g., “restrained,” “anxious,” “frigid”) increasing significantly. Low levels of arousal may have been related to our use of sexual fantasizing, whereas the aforementioned studies have used either erotic vignettes or films, which may produce higher levels of sexual arousal (Carvalho et al., 2013). Third, it is unknown whether the alcohol effects observed in the present study are dose dependent. Future studies should examine how doses other than 1 g/kg affect the likelihood of condom-protected sex. Finally, excluding females who were not using effective contraception, while based on ethical concerns regarding alcohol and pregnancy, might have resulted in a sample with lower sexual HIV risk behavior than the intended target population. Age and gender may interact in determining alcohol effects on sexual HIV risk behavior. Discounting in our relatively young sample—all but 3 participants were under 30 years old—might have been more sensitive to alcohol than discounting in older participants. Similarly, the racial distribution within the sample could have been more representative of the surrounding area.
The present study demonstrates the utility and specificity of a discounting-based approach to the evaluation of drug effects on sexual HIV risk behavior. Results suggested that the effects of alcohol were limited to discounting of sexual and/or probabilistic outcomes. Moreover, our finding that discounting of delayed condom-protected sex, but not immediate condom preference, was negatively impacted by alcohol suggests that increased condom availability may mitigate sexual HIV risk. This is especially pertinent if intoxicated individuals are less likely to have a condom available in casual-sex situations because such sexual encounters may be unplanned. High-risk individuals may therefore benefit from strategies that encourage planning ahead and possessing condoms prior to drinking. Overall, discounting-based approaches may prove critical in deciphering the interaction of biological and behavioral variables that contribute to decision making in sexual risk situations.
Acknowledgements
Portions of these data were presented at the 2014 annual meetings of the Association for Behavior Analysis International, the College on Problems of Drug Dependence, and the 2015 meeting of the Behavioral Pharmacology Society. The authors thank Grant Glatfelter, Crystal Fridy, and Curtis Bradley for their assistance in conducting the study.
This research was supported by National Institutes of Health grants R01DA032363 (MWJ) and T32DA007209 (PSJ, MMS, ESH). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
The authors do not have any conflicts of interest to report.
References
- Ammons RB, Ammons CH. The Quick Test (QT): Provisional manual. Psychol Rep. 1962;11:111–161. [Google Scholar]
- Baker F, Johnson MW, Bickel WK. Delay discounting in current and never-before cigarette smokers: Similarities and differences across commodity, sign, and magnitude. J Abnorm Psychol. 2003;112:382–392. doi: 10.1037/0021-843x.112.3.382. [DOI] [PubMed] [Google Scholar]
- Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: A meta-analysis. Int J Public Health. 2010;55:159–166. doi: 10.1007/s00038-009-0095-x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Koffarnus MN, Gatchalian KM. Excessive discounting of delayed reinforcers as a trans-disease process contributing to addiction and other disease-related vulnerabilities: Emerging evidence. Pharmacol Therapeut. 2012;134:287–297. doi: 10.1016/j.pharmthera.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidwell LC, MacKillop J, Murphy JG, Grenga A, Swift RM, McGeary JE. Biphasic effects of alcohol on delay and probability discounting. Exp Clin Psychopharm. 2013;21:214–221. doi: 10.1037/a0032284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho J, Gomes AQ, Laja P, Oliveira C, Vilarinho S, Janssen E, Nobre P. Gender differences in sexual arousal and affective responses to erotica: The effects of type of film and fantasy instructions. Arch Sex Behav. 2013;42:1011–1019. doi: 10.1007/s10508-013-0076-2. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Likely Female-to-Female Sexual Transmission of HIV. [September 15, 2015];Morbidity and Mortality Weekly Report. 2014 63:209–210. http://www.cdc.gov/mmwr/pdf/wk/mm6310.pdf. [Google Scholar]
- Cooper ML. Alcohol use and risky sexual behavior among college students and youth: Evaluating the evidence. J Stud Alcohol Suppl. 2002;14:101–117. doi: 10.15288/jsas.2002.s14.101. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Does drinking promote risky sexual behavior? A complex answer to a simple question. Curr Dir Psychol Sci. 2006;15:19–23. [Google Scholar]
- Dariotis JK, Johnson MW. Sexual discounting among high-risk youth ages 18–24: Implications for sexual and substance use risk behaviors. Exp Clin Psychopharm. 2015;23:49–58. doi: 10.1037/a0038399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behavior among intravenous drug users. AIDS. 1991;5:181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Davis KC, Masters NT, Eakins D, Danube CL, George WH, Norris J, Heiman JR. Alcohol intoxication and condom use self-efficacy effects on women's condom use intentions. Addict Behav. 2014;39:153–158. doi: 10.1016/j.addbeh.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Marsh-Richard DM, Hatzis ES, Nouvion SO, Mathias CW. A test of alcohol dose effects on multiple behavioral measures of impulsivity. Drug Alcohol Depend. 2008;96:111–120. doi: 10.1016/j.drugalcdep.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George WH, Davis KC, Masters NT, Jacques-Tiura AJ, Heiman JR, Norris J, Gilmore AK, Nguyen HV, Kajumolo KF, Otto JM, Andrasik MP. Sexual victimization, alcohol intoxication, sexual-emotional responding, and sexual risk in heavy episodic drinking women. Arch Sex Behav. 2014;43:645–658. doi: 10.1007/s10508-013-0143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George WH, Davis KC, Heiman JR, Norris J, Stoner SA, Schacht RL, Hendershot CS, Kajumulo KF. Women's sexual arousal: Effects of high alcohol dosages and self-control instructions. Horm Behav. 2011;59:730–738. doi: 10.1016/j.yhbeh.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George WH, Davis KC, Norris J, Heiman JR, Stoner SA, Schacht RL, Hendershot CS, Kajumulo KF. Indirect effects of acute alcohol intoxication on sexual risk-taking: The roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38:498–513. doi: 10.1007/s10508-008-9346-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George WH, Stoner SA. Understanding acute alcohol effects on sexual behavior. Annu Rev Sex Res. 2000;11:92–124. [PubMed] [Google Scholar]
- Herrmann ES, Hand DJ, Johnson MW, Badger GJ, Heil SH. Examining delay discounting of condom-protected sex among opioid-dependent women and non-drug-using control women. Drug Alcohol Depend. 2014;144:53–60. doi: 10.1016/j.drugalcdep.2014.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann ES, Johnson PS, Johnson MW. Examining delay discounting of condom-protected sex among men who have sex with men using crowdsourcing technology. AIDS Behav. 2015;19:1655–1665. doi: 10.1007/s10461-015-1107-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudziak JJ, Helzer JE, Wetzel MW, Kessel KB, McGee B, Janca A, Przybeck T. The use of the DSM-III-R Checklist for initial diagnostic assessments. Comp Psychiat. 1993;34:375–383. doi: 10.1016/0010-440x(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Johnson MW. An efficient operant choice procedure for assessing delay discounting in humans: Initial validation in cocaine-dependent and control individuals. Exp Clin Psychopharm. 2012;20:191–204. doi: 10.1037/a0027088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. Within-subject comparison of real and hypothetical money rewards in delay discounting. J Exp Anal Behav. 2002;77:129–146. doi: 10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. An algorithm for identifying nonsystematic delay-discounting data. Exp Clin Psychopharm. 2008;16:264–274. doi: 10.1037/1064-1297.16.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK, Baker F. Moderate drug use and delay discounting: A comparison of heavy, light, and never smokers. Exp Clin Psychopharm. 2007;15:187–194. doi: 10.1037/1064-1297.15.2.187. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR. The Sexual Discounting Task: HIV risk behavior and the discounting of delayed sexual rewards in cocaine dependence. Drug Alcohol Depend. 2012;123:15–21. doi: 10.1016/j.drugalcdep.2011.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bruner NR. Test–retest reliability and gender differences in the sexual discounting task among cocaine-dependent individuals. Exp Clin Psychopharm. 2013;21:277–286. doi: 10.1037/a0033071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Johnson PS, Herrmann ES, Sweeney MM. Delay and probability discounting of sexual and monetary outcomes in individuals with cocaine use disorders and matched controls. PLoS One. 2015;10:e0128641. doi: 10.1371/journal.pone.0128641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson PS, Herrmann ES, Johnson MW. Opportunity costs of reward delays and the discounting of hypothetical money and cigarettes. J Exp Anal Behav. 2015;103:87–107. doi: 10.1002/jeab.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse MI, Fromme K. Influence of physical attractiveness and alcohol on men's perceptions of potential sexual partners and sexual behavior intentions. Exp Clin Psychopharm. 2005;13:146–156. doi: 10.1037/1064-1297.13.2.146. [DOI] [PubMed] [Google Scholar]
- Lawyer SR, Schoepflin FJ. Predicting domain-specific outcomes using delay and probability discounting for sexual versus monetary outcomes. Behav Process. 2013;96:71–78. doi: 10.1016/j.beproc.2013.03.001. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Johnson PS. A delay-discounting primer. In: Madden GJ, Bickel WK, editors. Impulsivity: The Behavioral and Neurological Science of Discounting. American Psychological Association; Washington, DC.: 2010. pp. 11–37. [Google Scholar]
- Myerson J, Green L. Discounting of delayed rewards: Models of individual choice. J Exp Anal Behav. 1995;64:263–276. doi: 10.1901/jeab.1995.64-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) NIAAA Council Approves Definition of Binge Drinking. 3. NIAAA Newsletter; 2004. Winter Available at: http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf. [Google Scholar]
- Norris J, Stoner SA, Hessler DM, Zawacki T, Davis KC, George WH, Morrison DM, Parkhill MR, Abdallah DA. Influences of sexual sensation seeking, alcohol consumption, and sexual arousal on women's behavioral intentions related to having unprotected sex. Psychol Addict Behav. 2009;23:14–22. doi: 10.1037/a0013998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortner CN, MacDonald TK, Olmstead MC. Alcohol intoxication reduces impulsivity in the delay-discounting paradigm. Alcohol Alcoholism. 2003;38:151–156. doi: 10.1093/alcalc/agg041. [DOI] [PubMed] [Google Scholar]
- Purdie MP, Norris J, Davis KC, Zawacki T, Morrison DM, George WH, Kiekel PA. The effects of acute alcohol intoxication, partner risk level, and general intention to have unprotected sex on women's sexual decision making with a new partner. Exp Clin Psychopharm. 2011;19:378–388. doi: 10.1037/a0024792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachlin H, Raineri A, Cross D. Subjective probability and delay. J Exp Anal Behav. 1991;55:233–244. doi: 10.1901/jeab.1991.55-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed SC, Levin FR, Evans SM. Alcohol increases impulsivity and abuse liability in heavy drinking women. Exp Clin Psychopharm. 2012;20:454–465. doi: 10.1037/a0029087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: Systematic review and meta-analysis of experimental studies. Addiction. 2012;107:51–59. doi: 10.1111/j.1360-0443.2011.03621.x. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Richards JB, de Wit H. Acute-alcohol effects on the Experiential Discounting Task (EDT) and a question-based measure of delay discounting. Pharmacol Biochem Be. 2006;83:194–202. doi: 10.1016/j.pbb.2006.01.007. [DOI] [PubMed] [Google Scholar]
- Richards JB, Zhang L, Mitchell SH, de Wit H. Delay or probability discounting in a model of impulsive behavior: Effect of alcohol. J Exp Anal Behav. 1999;71:121–143. doi: 10.1901/jeab.1999.71-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schacht RL, George WH, Heiman JR, Davis KC, Norris J, Stoner SA, Kajumulo KF. Effects of alcohol intoxication and instructional set on women's sexual arousal vary based on sexual abuse history. Arch Sex Behav. 2007;36:655–665. doi: 10.1007/s10508-006-9147-y. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Walstrom P, Carey KB, Johnson BT, Carey MP, MASH Research Team Alcohol use and sexual risk behaviors among individuals infected with HIV: A systematic review and meta-analysis 2012 to early 2013. Curr HIV/AIDS Rep. 2013;10:314–323. doi: 10.1007/s11904-013-0177-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toledano R, Pfaus J. The Sexual Arousal and Desire Inventory (SADI): A Multidimensional Scale to Assess Subjective Sexual Arousal and Desire. J Sex Med. 2006;3:853–877. doi: 10.1111/j.1743-6109.2006.00293.x. [DOI] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- Weafer J, Mitchell SH, de Wit H. Recent translational findings on impulsivity in relation to drug abuse. Curr Addict Rep. 2014;1:289–300. doi: 10.1007/s40429-014-0035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray TB, Celio MA, Kahler CW, Barnett NP, Mastroleo NR, Operario D, Monti PM. Daily co-occurrence of alcohol use and high-risk sexual behavior among heterosexual, heavy drinking emergency department patients. Drug Alcohol Depend. 2015;152:109–115. doi: 10.1016/j.drugalcdep.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray TB, Simons JS, Maisto SA. Effects of alcohol intoxication and autonomic arousal on delay discounting and risky sex in young adult heterosexual men. Addict Behav. 2015;42:9–13. doi: 10.1016/j.addbeh.2014.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi R, Johnson MW, Bickel WK. Relationship between cooperation in an iterated prisoner's dilemma game and the discounting of hypothetical outcomes. Learn Behav. 2005;33:324–336. doi: 10.3758/bf03192861. [DOI] [PubMed] [Google Scholar]