Abstract
[Purpose] The aim of this study was to investigate the effects of sequential pneumatic compression therapy on venous blood flow, refilling time, pain level, and quality of life in women with varicose veins. [Subjects and Methods] Twenty-eight females with varicose veins were selected and randomly allocated to a control group, and experimental group. Maximum and mean venous blood velocities, the refilling time, pain by visual analog scale and quality of life by Aberdeen Varicose Veins Questionnaire were measured in all patients before and after six weeks of treatment. Both groups received lower extremity exercises; in addition, patients in the experimental group received sequential pneumatic compression therapy for 30 minutes daily, five days a week for six weeks. [Results] All measured parameters improved significantly in both groups, comparison of post treatment measurements between groups showed that the maximum and mean blood flow velocity, the pain level, and quality of life were significantly higher in the experimental group compared with the control group. On the other hand there was no significant difference between groups for refilling time. [Conclusion] Sequential pneumatic compression therapy with the applied parameters was an effective modality for increasing venous blood flow, reducing pain, and improving quality of women life with varicose veins.
Key words: Varicose veins, Pneumatic compression therapy, Quality of life
INTRODUCTION
Varicose veins are a common progressive medical condition with widely ranging estimates of prevalence that will steadily worsen1). The veins become dilated (greater than 3 mm) with twisting and bulging due to weakness of their walls or valves, which usually occurs in the superficial veins of the lower extremities2). Half of the adult population has the stigmata of minor venous disease3), and about 25% of the population has lower extremity varicose veins4). The prevalence of varicose veins is greater in women (26–32%) than in men (10–40%)5).
Varicose veins are more than an esthetic problem. They often affect individual’s physical appearance, and quality of life and may also result in lost time from work and lost wages. Insurance companies may be hesitant about paying for their treatment6).
Symptomatic varicose veins are not a life threatening condition, but the condition is usually progressive and may result in leg ulcer. The treatment of leg ulcers is intensive and very expensive. A non-healing ulcer can require prolonged primary care, and it’s the odor may lead to social exclusion. It is very difficult to predict which patient with varicose veins will develop a leg ulcer. However, it has been estimated that about half of venous leg ulcers are the result of varicose veins7).
Varicose veins management can range from conservative treatment to surgical approaches, all of which have different advantages, disadvantages, and long-term outcomes1). There are three main reasons for management with these approaches. The first is prevention of complications, such as edema, bleeding, eczema, lipodermatosclerosis, and leg ulcers1), the second is relief of complaints caused by varicose veins, such as heaviness, tired legs, and cramps, and the third is the importance of cosmetic appearance. Many patients only find their way to a phlebologic clinic because their varicose veins are cosmetically disturbing, and this may affect patients’ quality of life8).
Chronic diseases such as varicose veins have an important impact on a patient’s quality of life (QoL)9, 10). Different studies have confirmed that treatment of venous disease improved QoL11). The Aberdeen Varicose Veins Questionnaire (AVVQ) is a disease-specific questionnaire that measures QoL for patients with varicose veins12). The questionnaire, designed in 1993, consists of 13 questions related to all aspects of the problem of varicose veins13, 14).
Vascular compression therapies that include elastic wraps, elastic stockings, and intermittent pneumatic compression devices are the mainstay of conservative treatment for varicose veins. Other conservative treatments include drugs, lifestyle changes, exercise, and massage. Surgical treatment is reserved for severe or medically refractory varicose veins10).
Intermittent pneumatic compression (IPC) devices composed of sleeve- or boot-shaped chambers that fill with air and electrical pumps with gauges that provide intermittent compression to the lower extremities. The compression force may be applied either uniformly to the calf using a single chamber device or through a series of chambers inflated in a sequential manner from the ankle to thigh to achieve venous emptying15) which is termed sequential pneumatic compression (SPC).
The efficacy of IPC in the treatment of varicose veins is well documented10, 16). It reduces venous stasis by promoting venous blood flow17,18,19) and it stimulates fibrinolytic activity18, 20). It had been found to be an effective modality for treatment for venous ulceration21, 22).
Measurement of QoL is a comprehensive assessment of the effect of such a treatment intervention for varicose veins on patients to determine if the treatment results provides improvement. A new combined QoL and clinical instrument is needed to validly assess and compare the outcomes of venous treatments23). This study was conducted to investigate the effects of SPC therapy on venous blood flow, refilling time, pain level, and QoL of women with varicose veins.
SUBJECTS AND METHODS
The study protocol and designed were approved by the Local Ethics Committee of the Faculty of Physical Therapy, Cairo University. Fifty-five women with bilateral varicose veins were investigated at the vascular outpatient clinic of El Kasr El Ainy Teaching Hospital and National Heart Institute. Patients were enrolled in the study if they had a symptomatic varicose veins (clinical severity class C2 according to the CEAP classification, a comprehensive classification system) of the lower limb (pain, soreness, burning, aching, throbbing, heavy legs, cramping, muscle fatigue, and/or night cramps) over a period of at least six months24). Patients were required to have an educational level sufficient to allow them to read and understand AVVQ in English independently without any help. Patients were excluded if they were pregnant or breastfeeding; had any local leg condition interferes with sleeve wear, such as dermatitis, vein ligation, gangrene, or recent skin graft; had severe leg arteriosclerosis or any other ischemic vascular disease; had massive leg edema or pulmonary edema from congestive heart failure; had a suspecting existing or previous venous thromboembolism; had an extreme leg deformity or size (thigh circumference <55 cm or >71 cm); or had medical disorders such as diabetes16). Patients were excluded if they could not read and understand the AVVQ in English on their own. Twenty-seven patients were excluded from the study because of venous thromboembolism (9%, 5/55), size of the leg (16.3%, 9/55), and diabetic limitations (23.6%, 13/55), and the remaining 28 patients were enrolled.
This study was a randomized control trial (Fig. 1). The patients who fulfilled the inclusion criteria and provided a written informed consent were randomly divided into two groups by using sealed envelopes. Thirteen patients were allocated to the control group, and fifteen patients were allocated to the experimental group. The sample size was calculated based on previous studies16, 29). A power analysis with α=0.05 and power=80% determined that a group size of 15 was adequate to demonstrate a 25% change in the venous blood velocity, refilling time, and pain level between the groups.
Fig. 1.
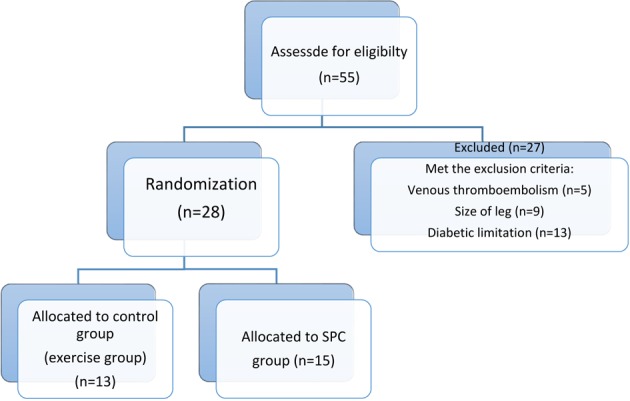
Flow chart for design of study
The Venous system of the lower extremities of the patients was examined by duplex ultrasound (ProSound SSD-4000, Hitachi Aloka Medical, Ltd., Japan) in order to measure the maximum and mean venous blood velocities in centimeters per second (cm/sec) and the refilling time in seconds. A Visual analog scale (VAS) was used to measured pain level, and the AVVQ was used to measured QoL of all patients in both groups before and after six weeks of treatment. All measurements were performed in a similar fashion at the same time of the day for both groups to reduce variability.
Venous blood velocity was measured by ultrasonographic imaging performed by the same radiologist. Each subject was placed in the supine position for a minimum of five minutes before the evaluation and baseline venous velocities were recorded in cm/sec. Maximal and mean venous blood velocities were obtained from the common femoral vein cephalad to the saphenofemoral junction, and the refilling time was also measured. The angle of insonation of the ultrasound scan beam with the vein was 60 degrees25). All measurements were repeated three times, and the mean was used for analysis.
Pain level was measured by VAS. The VAS is 10 cm horizontal line with one end described as no pain (0 cm) and the other end described as the worst pain (10 cm). The distance between the extreme left of the scale (no pain) and the subject’s mark was measured to the nearest millimeter. High levels of reliability and validity have been reported for the VAS26).
The AVVQ consists of questions relating to all aspects of the problem of varicose veins13, 14). The questionnaire has a section in which patients can indicate diagrammatically the distribution of their varicose veins. There are other questions relating to pain severity, ankle edema, ulcers, compression therapy use, and limitations on daily activities, as well as questions on the cosmetic effect of varicose veins. The questionnaire is scored from 0 (no effect) to 100 (severe effect)27, 28). The AVVQ therefore fulfilled all attributes necessary for an instrument to be used as a measure of health outcome and QoL23). The patients were requested to fill in a copy of this questionnaire on day zero and then again at the end of the six weeks. Grading of the answers was performed according to the manual for the AVVQ.
Patients in both groups received a physiotherapy program that consisted of lower extremity exercises, which included gluteal and quadriceps isometric exercises, active hip and knee flexion/extension, ankle dorsiflexion/ plantar flexion, and straight leg raising. The patients were instructed to perform ten repetitions of each exercise three times a day, five time per week for six weeks29).
In addition, patients in the experimental group were treated with an SPC device (EUREDUC TPO5, Japan). Each of the lower extremities was treated for thirty minutes daily, five days a week for six weeks. The device had three separate chambers, one over the distal calf, one over the proximal calf, and one over the distal thigh, that inflated sequentially. It was adjusted to apply a pressure of 65, 55, and 45 mmHg respectably in a distal to proximal direction for 12 seconds followed by 2.4 seconds of non-compression to allow venous refilling.
Statistical analyses were carried out using PASW Statistics for Windows, Version 18.0 (SPSS Inc., Chicago, IL, USA). Normality of the data was assessed using graphical methods, including the frequency distribution on a histogram and normal Q-Q plot. The Kolmogorov-Smirnov and Shapiro-Wilk tests were used as a confirmation. Descriptive data were expressed as the mean ± standard deviation (SD) for demographic characteristics of patients. The Independent t-was used to test for significant difference between mean values of two groups of normally distributed variables. Mann-Whitney U test was used to test difference between mean values of two groups of non-normally distributed variables. The Paired t-test (for normally distributed data) and Wilcoxon signed-rank test (for non-normally distributed data) for paired data were applied with 95% confidence intervals (95% CI). A difference was considered significant if the p-value was <0.05. Statistical analysis included only patients with both pre- and post-treatment values.
RESULTS
The baseline characteristics of the patients are summarized in Table 1. There were no statistically significant differences between the two groups with regard to age, weight, height, and body mass index.
Table 1. Baseline characteristics of the patients.
| Characteristic | Control group (n=13) |
Experimental group (n=15) |
p-value |
|---|---|---|---|
| Age (years) | 43.4 ± 4.35 | 40.3 ± 4.80 | 0.390 |
| Weight (kg) | 83.6 ± 6.47 | 84.5 ± 6.57 | 0.627 |
| Height (cm) | 160.0 ± 5.02 | 158.9 ± 2.92 | 0.518 |
| BMI (kg/m2) | 32.65 ± 1.9 | 33.5 ± 2.82 | 0.924 |
Data represent the mean ± standard deviation. n: number; BMI: body mass index
At baseline, there were no statistically significant differences between the groups with regard to maximum blood flow velocity, mean blood flow velocity, and refilling time (Table 2). In both groups, maximum blood flow velocity, and mean blood flow velocity were significantly increased (p=0.000 in both groups). Refilling time was significantly decreased in both groups (p=0.000 in both groups) (Table 2). Comparison of posttreatment measurement values between groups showed that maximum blood flow velocity, and mean blood flow velocity were significantly higher in the SPC group compared with the control group (p=0.002, and p=0.024 respectively); while for refilling time, there was no significant difference between the groups (p=0.065) (Table 2).
Table 2. Statistical analysis of venous blood flow variables within and between groups.
| Measure | Groups | Pre | Post |
|---|---|---|---|
| Maximum blood flow velocity (cm/sec) | Control (25) | 10.3 ± 2.54 | 15.6 ± 3.33* |
| Experimental (26) | 10.6 ± 3.57 | 19.0 ± 3.93* | |
| ** | |||
| Mean blood flow velocity (cm/sec) | Control (25) | 5.6 ± 0.97 | 9.5 ± 3.25* |
| Experimental (26) | 6.2 ± 1.26 | 11.3 ± 2.31* | |
| ** | |||
| Refilling time (sec) | Control (25) | 29.3 ± 3.19 | 20.8 ± 2.67* |
| Experimental (26) | 30.5 ± 4.06 | 22.5 ± 3.65* |
Data represent the mean ± standard deviation. Experimental group, sequential pneumatic compression. *p<0.05 Statistically significant difference within the group before and after the intervention. **p<0.05 Statistically significant difference between groups at baseline and after the intervention period.
The results of the VAS and AVVQ for both groups are summarized in Table 3. Before treatment no significant difference was found between the groups for either the VAS or AVVQ (p=0.120, and p=0.460 respectively). Both groups demonstrated significant reductions in both the VAS and AVVQ (p=0.001 in both groups). After treatment there was significant difference between the groups in the VAS and AVVQ. Participants in the SPC group had greater reductions in both the VAS and AVVQ compared with those in the control group after the treatment period (Table 3).
Table 3. Statistical analysis of visual analogue scale and Aberdeen Varicose Veins Questionnaire within and between groups.
| Measure | Groups | Pre | Post |
|---|---|---|---|
| VAS (mm) | Control (n=13) | 8 (7–8) | 5.5 (4.5–6)* |
| Experimental (n=15) | 8 (7–9) | 4.0 (3–4)* | |
| ** | |||
| AVVQ | Control (n=13) | 65.1 (61.20–67.05) | 57.2 (53.60–61.91)* |
| Experimental (n=15) | 67.1 (61.80–68.50) | 39.3 (32.12–56.20)* | |
| ** |
Data are presented as the median (interquartile range). VAS: Visual Analog Scale; AVVQ: Aberdeen Varicose Veins Questionnaire; experimental: sequential pneumatic compression. *p<0.001 Statistically significant difference within the group before and after the intervention. **p<0.001 Statistically significant difference between groups at baseline and after the intervention period.
DISCUSSION
Varicose veins are widely seen as medically unimportant and deserving low priority for treatment30). On the other hand, they are one of the most common symptoms of chronic venous disease, causing a dramatic impact on the quality of patient life31). For accurate evaluation of treatment outcomes, QoL, and clinical aspects must be assessed23).
There was no available published research about the impact of SPC on clinical aspects and QoL of varicose veins patients. This study was designed as an initial study to investigate the effects of SPC therapy on venous blood flow, pain level, and QoL in women with varicose veins.
The gold standard for diagnosing varicose veins is ultrasound examination. It is ideal for optimal visualization of anatomy, hemodynamics, the diameter of the veins, and reflux time which can be measured accurately32).
Varicose veins patients previously showed a reduction in QoL compared with the general population, and this discrepancy was significantly improved at 6 weeks after surgey23). The AVVQ is a valid measure of quality of life for patients with varicose veins12). The National Health Service in the United Kingdom, has been collecting AVVQ scores for varicose vein surgeries since 2009, and the results have been correlated with both EuroQol five dimensions questionnaire (EQ-5D) and EQ VAS scores; as a result, the AVVQ has been found to be a sensitive tool for assessing disease burden in varicose vein patients33). In the Netherlands, a similar study matched AVVQ scores with 36-Item Short Form Health Survey (SF-36) scales and showed a strong correlation between the AVVQ and generic QoL outcomes34).
The data obtained in this study revealed that the measured parameters, maximum, mean blood flow velocity, refilling time, pain level, and QoL were improved significantly in both the control and experimental groups. Comparison of the posttreatment measurement values between the groups revealed that the maximum and mean blood flow velocity, pain level, and QoL were significantly higher in the SPC group compared with the control group, while no significant difference was observed between groups for refilling time.
The significant results found in the control group could be related to the effect of exercise on the venous system. Regular exercise such as walking, biking, and swimming has beneficial effects that maximize calf pump function. The calf musculature functions as a “peripheral heart,” and a “poor ejection fraction” associated with poor leg conditioning results in progressive edema and increased varicose veins symptoms. A regular exercise program can improve the overall “ejection fraction,” resulting in symptom improvement35).
In this study, all patients performed lower limb exercises; these exercises result in blood being pumped back to the heart from the thigh, calf muscles, and veins in the arch of the foot. A strong calf and thigh muscles promote healthy blood circulation and minimizes vein disease29, 36, 37).
IPC is generally a painless and non-invasive technique with proven efficacy as a valuable adjunct in the management of patients with venous, lymphatic, and arterial disease38).
The current study proved that IPC has significant effects on venous blood flow based on the following physiological effects. IPC increases the velocity of venous return and reduces the amount of blood inside the veins at any time through stimulation of endothelial cell production of nitric oxide and creates shear stress on the walls of blood vessels, which is the probable physiologic mechanism for enhanced nitric oxide production. Increased nitric oxide production inhibits platelet aggregation and neutrophil adherence, both of which play important roles in the creation of secondary hypoxic injury. Nitric oxide is also a neurotransmitter that can influence vascular tone, thereby increasing blood flow39, 40). Delis et al., found that IPC applied to thefoot and calf produced maximal venous emptying from the leg41).
The SPC therapy used in this study delivers sequential graded compression; that is, at any time, the pressure in any chamber is higher than the adjacent most proximal one. There is evidence of distal blood trapping and incomplete calf vein evacuation as a result of uniform compression42). SPC allows greater venous blood clearance or less stasis and prevents reversed pressure gradient and blood trapping during uniform compression.
Pain develops in varicose vein patients as a result of increased tissue tension caused by swelling. Therefore, if swelling is minimized pain will be reduced. Compression therapy counteracts venous hypertension by facilitating venous return toward the heart, improving venous pump function and lymphatic drainage. It reduces edema by increasing the local hydrostatic pressure and lowering the superficial venous pressure, preventing the leakage of fluids and macromolecules, improving cutaneous blood flow, and therefore decreasing pain43).
These results are in agreement with the study of Kakkos et al.42) who revealed the hemodynamic superiority of sequential compression compared with other compression device16). Figueiredo et al.44), found that use of IPC improves blood flow when applied in legs or thighs. Other studies have consistently concluded that all intermittent compression systems produce changes in femoral vein velocity. At pressures of around 40 mmHg, the typical maximum velocities achieved with calf and/or thigh compression would be 35–60 cm/sec with augmentations (maximum velocity during compression compared with maximum velocity at rest) of around 50–250%45, 46).
Assessment of the QoL status at baseline and on completion of the six-week active study period using the AVVQ showed that SPC can significantly improve the QoL of patients by improving venous blood flow and reducing pain. Physical functioning, bodily pain, vitality, and social functioning all improved significantly within six weeks of treatment with SPC. The aspects of QoL measured by the AVVQ are known to be impaired in patients with varicose vains12). SPC improves these aspects of life. On the other hand, the exercise brings about minimal changes in QoL.
A limitation of this study was its small sample of patients due to the required educational level for patient who had to be able to read and understand the AVVQ in English independently without any help. As there are no valid Arabic versions of the AVVQ available, it is necessary to conduct translation, cultural adaptation, and validation to produce an Arabic version of the AVVQ.
In this study, women with varicose veins were treated with SPC along with regular lower limbs exercise, five days/week for six weeks. SPC therapy emerged as an effective treatment in the management of varicose veins, offering a clinically significant improvement in both venous blood flow and pain. These benefits were paralleled by significant improvements in all evaluated aspects of quality of life.
Acknowledgments
The authors are grateful to Professor Samia A. Elkady and Professor Ahmed Sabry for their encouragement and support; Mrs. Dalia Mohamed for her assistance; and the Department of Physical Therapy, National Heart Institute, for the loan of SPC equipment.
REFERENCES
- 1.Wright N, Fitridge R: Varicose veins—natural history, assessment and management. Aust Fam Physician, 2013, 42: 380–384. [PubMed] [Google Scholar]
- 2.Fitridge R, Thompson MM: Mechanisms of vascular disease: a textbook for vascular surgeons. Cambridge: Cambridge University Press, 2011, pp 125–156. [Google Scholar]
- 3.Callam MJ: Epidemiology of varicose veins. Br J Surg, 1994, 81: 167–173. [DOI] [PubMed] [Google Scholar]
- 4.Rabe E, Pannier-Fischer F, Bromen K, et al. : Epidemiological investigation into the question of the frequency and severity of chronic venous diseases in the urban and rural population. Phlebology, 2003, 32: 1–14. [Google Scholar]
- 5.Evans CJ, Fowkes FG, Ruckley CV, et al. : Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health, 1999, 53: 149–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartholomew JR, King T, Sahgal A, et al. : Varicose veins: newer, better treatments available. Cleve Clin J Med, 2005, 72: 312–314, 319–321, 325–328. [DOI] [PubMed] [Google Scholar]
- 7.Magnusson MB, Nelzén O, Risberg B, et al. : A colour Doppler ultrasound study of venous reflux in patients with chronic leg ulcers. Eur J Vasc Endovasc Surg, 2001, 21: 353–360. [DOI] [PubMed] [Google Scholar]
- 8.Margolis DJ, Bilker W, Santanna J, et al. : Venous leg ulcer: incidence and prevalence in the elderly. J Am Acad Dermatol, 2002, 46: 381–386. [DOI] [PubMed] [Google Scholar]
- 9.Kurz X, Kahn SR, Abenhaim L, et al. : Chronic venous disorders of the leg: epidemiology, outcomes, diagnosis and management. Summary of an evidence-based report of the VEINES task force. Venous Insufficiency Epidemiologic and Economic Studies. Int Angiol, 1999, 18: 83–102. [PubMed] [Google Scholar]
- 10.Campbell WB, Decaluwe H, Macintyre JB, et al. : Most patients with varicose veins have fears or concerns about the future, in addition to their presenting symptoms. Eur J Vasc Endovasc Surg, 2006, 31: 332–334. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan RM, Criqui MH, Denenberg JO, et al. : Quality of life in patients with chronic venous disease: San Diego population study. J Vasc Surg, 2003, 37: 1047–1053. [DOI] [PubMed] [Google Scholar]
- 12.Smith JJ, Garratt AM, Guest M, et al. : Evaluating and improving health-related quality of life in patients with varicose veins. J Vasc Surg, 1999, 30: 710–719. [DOI] [PubMed] [Google Scholar]
- 13.Garratt AM, Macdonald LM, Ruta DA, et al. : Towards measurement of outcome for patients with varicose veins. Qual Health Care, 1993, 2: 5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garratt AM, Ruta DA, Abdalla MI, et al. : Responsiveness of the SF-36 and a condition-specific measure of health for patients with varicose veins. Qual Life Res, 1996, 5: 223–234. [DOI] [PubMed] [Google Scholar]
- 15.Morris RJ, Woodcock JP: Intermittent pneumatic compression or graduated compression stockings for deep vein thrombosis prophylaxis? A systematic review of direct clinical comparisons. Ann Surg, 2010, 251: 393–396. [DOI] [PubMed] [Google Scholar]
- 16.Griffin M, Kakkos SK, Geroulakos G, et al. : Comparison of three intermittent pneumatic compression systems in patients with varicose veins: a hemodynamic study. Int Angiol, 2007, 26: 158–164. [PubMed] [Google Scholar]
- 17.Keith SL, McLaughlin DJ, Anderson FA, Jr, et al. : Do graduated compression stockings and pneumatic boots have an additive effect on the peak velocity of venous blood flow? Arch Surg, 1992, 127: 727–730. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs DG, Piotrowski JJ, Hoppensteadt DA, et al. : Hemodynamic and fibrinolytic consequences of intermittent pneumatic compression: preliminary results. J Trauma, 1996, 40: 710–716, discussion 716–717. [DOI] [PubMed] [Google Scholar]
- 19.Malone MD, Cisek PL, Comerota AJ, Jr, et al. : High-pressure, rapid-inflation pneumatic compression improves venous hemodynamics in healthy volunteers and patients who are post-thrombotic. J Vasc Surg, 1999, 29: 593–599. [DOI] [PubMed] [Google Scholar]
- 20.Comerota AJ, Chouhan V, Harada RN, et al. : The fibrinolytic effects of intermittent pneumatic compression: mechanism of enhanced fibrinolysis. Ann Surg, 1997, 226: 306–313, discussion 313–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith PC, Sarin S, Hasty J, et al. : Sequential gradient pneumatic compression enhances venous ulcer healing: a randomized trial. Surgery, 1990, 108: 871–875. [PubMed] [Google Scholar]
- 22.McCulloch JM, Marler KC, Neal MB, et al. : Intermittent pneumatic compression improves venous ulcer healing. Adv Wound Care, 1994, 7: 22–24, 26. [PubMed] [Google Scholar]
- 23.Catarinella FS, Nieman FH, Wittens CH: An overview of the most commonly used venous quality of life and clinical outcome measurements. J Vasc Surg Venous Lymphat Disord, 2015, 3: 333–340. [DOI] [PubMed] [Google Scholar]
- 24.Eklöf B, Rutherford RB, Bergan JJ, et al. American Venous Forum International Ad Hoc Committee for Revision of the CEAP Classification: Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg, 2004, 40: 1248–1252. [DOI] [PubMed] [Google Scholar]
- 25.Coleridge-Smith P, Labropoulos N, Partsch H, et al. : Duplex ultrasound investigation of the veins in chronic venous disease of the lower limbs—UIP consensus document. Part I. Basic principles. Eur J Vasc Endovasc Surg, 2006, 31: 83–92. [DOI] [PubMed] [Google Scholar]
- 26.Jensen MP, Karoly P, Braver S: The measurement of clinical pain intensity: a comparison of six methods. Pain, 1986, 27: 117–126. [DOI] [PubMed] [Google Scholar]
- 27.Davies A, Rudarakanchana N: Quality of life and outcome assessment in patients with varicose veins. In: Davies AH, Lees TA, Lane IF (eds.), Venous Disease Simplified. Shrewsbury. TFM Publishing Ltd., 2006. [Google Scholar]
- 28.Michael A, Carolyn E: Venous Clinical Severity Score and quality-of-life assessment tools: application to vein practice. Phlebolymphology, 2010, 17: 108–115. [Google Scholar]
- 29.Gucuk A, Peker O, Bircan C, et al. : The effectiveness of intermittent pneumatic compression in patients with chronic venous insufficiency. Arastirma, 2001, 7: 117–122. [Google Scholar]
- 30.Campbell B: Varicose veins and their management. BMJ, 2006, 333: 287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas G, Guilliams R: Venous Disorders: More than a cosmetic concern. Standard, 1998, 1: 1–4. [Google Scholar]
- 32.Coleridge-Smith P, Labropoulos N, Partsch H, et al. UIP: Duplex ultrasound investigation of the veins in chronic venous disease of the lower limbs—UIP consensus document. Part I. Basic principles. Vasa, 2007, 36: 53–61. [DOI] [PubMed] [Google Scholar]
- 33.Nesbitt C, Wilson WR, Lees TA, et al. : Interpretation of patient-reported outcome measures for varicose vein surgery. Phlebology, 2012, 27: 173–178. [DOI] [PubMed] [Google Scholar]
- 34.Klem TM, Sybrandy JE, Wittens CH: Measurement of health-related quality of life with the Dutch translated Aberdeen Varicose Vein Questionnaire before and after treatment. Eur J Vasc Endovasc Surg, 2009, 37: 470–476. [DOI] [PubMed] [Google Scholar]
- 35.Jeavons L, Kochhar S: Vascular examination: varicose veins. Student BMJ, 2004, 12: 448–449. [Google Scholar]
- 36.Kan YM, Delis KT: Hemodynamic effects of supervised calf muscle exercise in patients with venous leg ulceration: a prospective controlled study. Arch Surg, 2001, 136: 1364–1369. [DOI] [PubMed] [Google Scholar]
- 37.Agu O, Baker D, Seifalian AM: Effect of graduated compression stockings on limb oxygenation and venous function during exercise in patients with venous insufficiency. Vascular, 2004, 12: 69–76. [DOI] [PubMed] [Google Scholar]
- 38.Comerota A, Aziz F: The case for intermittent pneumatic compression. Clinical review. J Lymphoedema, 2009, 4: 57–64. [Google Scholar]
- 39.Dai G, Tsukurov O, Chen M, et al. : Endothelial nitric oxide production during in vitro simulation of external limb compression. Am J Physiol Heart Circ Physiol, 2002, 282: H2066–H2075. [DOI] [PubMed] [Google Scholar]
- 40.Capps SG: Cryotherapy and intermittent pneumatic compression for soft tissue trauma. Athl Ther Today, 2009, 14: 2–4. [Google Scholar]
- 41.Delis KT, Azizi ZA, Stevens RJ, et al. : Optimum intermittent pneumatic compression stimulus for lower-limb venous emptying. Eur J Vasc Endovasc Surg, 2000, 19: 261–269. [DOI] [PubMed] [Google Scholar]
- 42.Kakkos SK, Nicolaides AN, Griffin M, et al. : Comparison of two intermittent pneumatic compression systems. A hemodynamic study. Int Angiol, 2005, 24: 330–335. [PubMed] [Google Scholar]
- 43.Berliner E, Ozbilgin B, Zarin DA: A systematic review of pneumatic compression for treatment of chronic venous insufficiency and venous ulcers. J Vasc Surg, 2003, 37: 539–544. [DOI] [PubMed] [Google Scholar]
- 44.Figueiredo M, Simao PP, Pereira BM, et al. : Efficacy of intermittent pneumatic compression (IPC) in lower limbs on the blood flow of common femoral veins. J Vasc Bras, 2008, 7: 321–324. [Google Scholar]
- 45.Whitelaw GP, Oladipo OJ, Shah BP, et al. : Evaluation of intermittent pneumatic compression devices. Orthopedics, 2001, 24: 257–261. [DOI] [PubMed] [Google Scholar]
- 46.Delis KT, Slimani G, Hafez HM, et al. : Enhancing venous outflow in the lower limb with intermittent pneumatic compression. A comparative haemodynamic analysis on the effect of foot vs. calf vs. foot and calf compression. Eur J Vasc Endovasc Surg, 2000, 19: 250–260. [DOI] [PubMed] [Google Scholar]


