Abstract
Cell autonomous circadian clocks have emerged as critical mediators of twenty four hour rhythms in cellular processes. In doing so, these molecular timekeepers confer the selective advantage of anticipation, allowing cells/organs to prepare for stimuli/stresses before their onset. The heart is subjected to dramatic fluctuations in energetic demand and nutrient supply in association with sleep/wake and fasting/feeding cycles. Recent studies suggest that the cardiomyocyte circadian clock orchestrates daily rhythms in both oxidative and non-oxidative glucose and fatty acid metabolism, as well as protein turnover. Here, we review this evidence, and discuss whether disruption of these rhythms can contribute towards cardiovascular disease.
Time-of-day-dependent rhythms are observed in multiple aspects of life, as well as death. In terms of cardiovascular parameters, blood pressure, heart rate, and cardiac output all increase sharply at the beginning of the awake period, which is associated with increased risk of adverse ischemic events, arrhythmias, and sudden cardiac death at this time (reviewed in (Durgan & Young, 2010)). Classically, daily rhythms in cardiovascular physiology and pathophysiology have been attributed to fluctuations in neurohumoral factors and sheer stress associated with sleep/wake and fasting/feeding cycles (Young, 2006; Durgan & Young, 2010). Elegant studies by Shea and Scheer have recently revealed that 24-hr oscillations in multiple cardiovascular functions are intrinsically driven in healthy human subjects, thus highlighting a need to reevaluate our understanding of the mechanisms modulating cardiovascular processes (Scheer et al., 1999; Scheer et al., 2010). One intrinsic mechanism capable of driving 24-hr rhythms in cellular processes is the circadian clock.
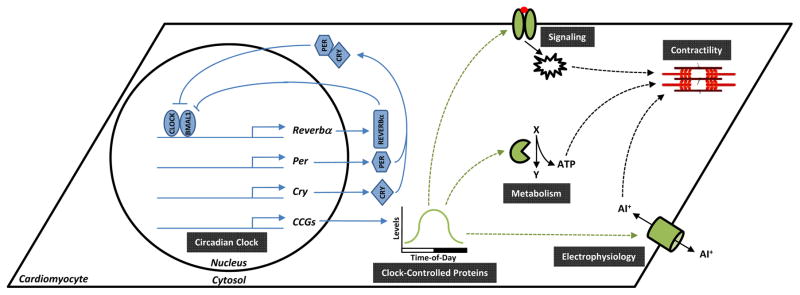
Circadian clocks are cell autonomous mechanisms composed of transcriptional positive and negative feedback loops, with a free running period of approximately 24-hr (reviewed in (Takahashi et al., 2008)). Clock components are expressed within individual cells, in a ubiquitous manner, and can operate in the absence of extrinsic cues. At the core of the mammalian mechanism are two transcription factors, CLOCK and BMAL1, which heterodimerize and bind to E-boxes in the promoters of target genes (Gekakis et al., 1998; Hogenesch et al., 1998). Target genes include repressors of CLOCK/BMAL1 (e.g., PER1/2/3, CRY1/2, REV-ERBα), thus resulting in 24-hr oscillations in the activity of this heterodimer (Takahashi et al., 2008). The CLOCK/BMAL1 heterodimer also modulates expression of non-core clock components, so called clock output genes (CCGs). Translation of CCG mRNAs enables circadian clocks to influence cellular processes over the course of the day (Figure 1). In general, circadian clocks confer a selective advantage by temporally partitioning cellular processes in anticipation of predicted daily fluctuations in the environment. Two major cycles that the heart must contend with on a daily basis include sleep/wake and fasting/feeding cycles.
Figure 1.
The cardiomyocyte circadian clock mechanism. Figure illustrates the positive and negative feedback loops of the cardiomyocyte circadian clock (blue), hypothetical clock controlled proteins (green), and the possible ways in which this mechanism influences cardiac contractility over the course of the day (black). Abbreviations include: AI+, anion; CCGs, clock-controlled genes; Cry, cryptochrome isoforms 1 and 2; Per, period isoforms 1, 2, and 3; X and Y, hypothetical metabolites.
Following initial characterization of the cell autonomous cardiomyocyte circadian clock (Durgan et al., 2005), we development two distinct mouse models wherein this mechanism was genetically disrupted, namely cardiomyocyte-specific CLOCK mutant (CCM) and cardiomyocyte-specific BMAL1 knockout (CBK) mice (Durgan et al., 2006; Bray et al., 2008; Durgan et al., 2011b; Young et al., 2014). Given the transcriptional nature of this mechanism, unbiased gene expression microarrays were performed initially, revealing that approximately 10% of the cardiac transcriptome is regulated by the cardiomyocyte circadian clock (Bray et al., 2008; Young et al., 2014). Gene ontology analysis clustered CCGs into various categories, including transcription, signal transduction, transport, and metabolism (Bray et al., 2008; Young et al., 2014). The latter was reinforced by an unbiased proteomics approach, indicating that approximately 4% of the cardiac proteome is modulated by the cardiomyocyte circadian clock, and that many of the identified proteins influence metabolic processes (Podobed et al., 2014). Collectively, these observations led to the hypothesis that the cardiomyocyte circadian clock allows the heart to predict/prepare for fluctuations in energetic demand and/or nutrient availability associated with sleep/wake and fasting/feeding cycles, through metabolic modulation.
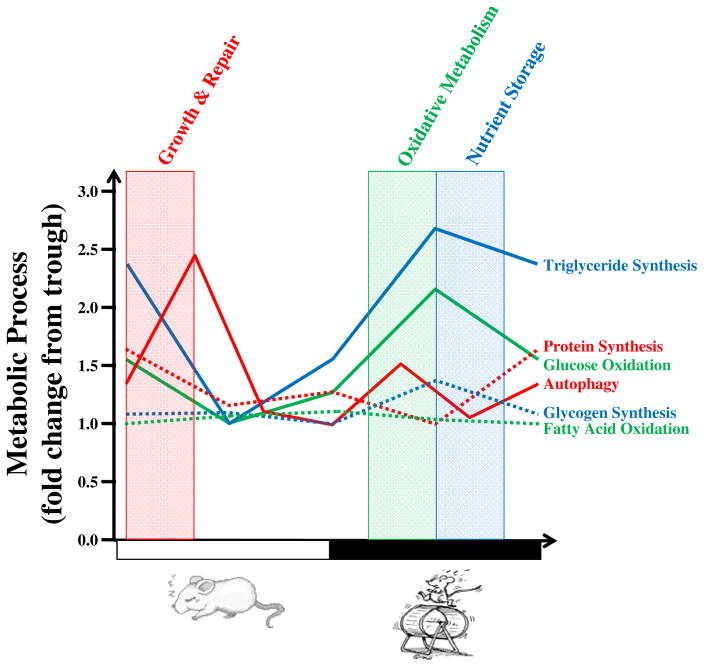
During periods of physical activity (i.e., increased workload), the heart matches increased energetic demand primarily through stimulation of glucose utilization (Allard et al., 1994; Goodwin et al., 1998). Consistent with this knowledge, glucose oxidation is more than 2-fold higher in rodent hearts during the middle of the active (dark) phase (relative to the sleep (light) phase; Figure 2) (Young et al., 2001; Durgan et al., 2007; Durgan et al., 2011a). Evidence suggesting mediation by the cardiomyocyte circadian clock includes: 1) glucose oxidation rhythms are observed in ex vivo perfused hearts (in the absence of neurohumoral influence), even when cardiac work was constant (Durgan et al., 2011a); 2) rhythms are absent in CCM hearts, which exhibit chronically low glucose oxidation rates (Durgan et al., 2011a); and 3) peak glucose oxidation rates are markedly attenuated in CBK hearts (Young et al., 2014). In contrast, cardiac fatty acid oxidation rates do not exhibit a robust time-of-day-dependent oscillation, consistent with baseline requirements of this parameter independent of workload (although fatty acid oxidation is slightly higher at the sleep-to-wake transition; Figure 2) (Bray et al., 2008).
Figure 2.
Temporal partitioning of metabolic processes in the heart. Figure illustrates fold changes in distinct cardiac metabolic processes with respect to time-of-day, which is based on both published and unpublished findings in the ad libitum fed mouse. Assessments include metabolic flux (glucose and fatty acid oxidation, glycogen and triglyceride synthesis, as well as protein synthesis) and protein levels (LC3II/I ratio for autophagy). Shaded areas indicate the 4-hr periods of greatest oxidative metabolism, nutrient storage, and growth/repair.
Unlike sleep/wake cycles, feeding/fasting cycles are less predictable for the animal in the wild, being dependent on successful forage for food during the awake period. For the ad libitum fed laboratory rodent (mimicking a constant abundance of food, independent of time-of-day or season, much like humans in Westernized countries), one might predict increased nutrient storage during the awake/feeding period, in anticipation of an upcoming sleep/fasting period. Indeed, both glycogen and triglyceride synthesis oscillate in the ex vivo perfused mouse heart, peaking in the middle and end of the active (dark) phase (respectively; Figure 2) (Tsai et al., 2010; Durgan et al., 2011a). Importantly, these 24-hr oscillations are absent in CCM hearts, indicative of mediation by the cardiomyocyte circadian clock (Tsai et al., 2010; Durgan et al., 2011a). Less is known regarding whether the cardiomyocyte circadian clock also anticipates unsuccessful forage for food (i.e., prolongation of the sleep phase fast); during this situation, energetic demand of the heart will remain elevated during the continued search for food (and predation avoidance). Whether 24-hr rhythms in glycogen and triglyceride turnover persist in the heart during prolonged fasting has not been addressed (although glycogen rhythms persist in the liver during fasting) (Ishikawa & Shimazu, 1976).
Less is known regarding circadian influences on cardiac protein metabolism. Unpublished studies suggest that protein synthesis exhibits a 24-hr oscillation in the murine heart, peaking at the beginning of the sleep (light) phase, with a prominent trough in the middle of the awake (dark) phase (Figure 2). Circumstantial evidence suggests possible mediation by an intrinsic mechanism (e.g., the clock), as: 1) these rhythms persist ex vivo; 2) pro-growth signals such as sheer stress/workload, insulin, and amino acids, all peak in the middle of the active (dark) phase, when cardiac protein synthesis troughs; and 3) protein synthesis is altered (elevated) in CBK hearts (He et al., 2016b). These observations have led us to hypothesize that the cardiomyocyte circadian clock decreases protein synthesis during the active period to spare ATP for contraction, yet increases protein synthesis at the beginning of the sleep phase in an attempt to replace damaged proteins (in anticipation of the next awake period). If true, one would predict that the cardiomyocyte circadian clock would also promote protein degradation at the beginning of the sleep phase, thus facilitating replacement of damaged proteins. Consistent with this hypothesis, recent studies reveal that both autophagy (He et al., 2016a) and proteasome activity (unpublished observations) are increased in the heart at the beginning of the sleep phase (Figure 2).
Figure 2 summarizes evidence-based temporal partitioning of cardiac metabolic processes by the cardiomyocyte circadian clock. Major questions that now can be asked include: 1) How do intrinsic (i.e., cardiomyocyte circadian clock) and extrinsic (e.g., neurohumoral factors, such as insulin, b-adrenergic stimulation, and various nutrients) influences coordinate cardiac metabolism in the in vivo setting?; 2) What are the molecular links between the cardiomyocyte circadian clock and metabolic processes?; and 3) What, if any, are the pathological consequences of cardiomyocyte circadian clock control of cardiac metabolism? With regards to the latter, evidence has emerged suggesting that the heart exhibits profound time-of-day-dependent oscillations in its responsiveness to pathologic stresses, including ischemia/reperfusion and pro-hypertrophic stimuli (Durgan et al., 2010; Durgan et al., 2011b). Consistent with greater protein synthesis at the beginning of the sleep phase, challenging mice with isoproterenol at this time leads to greater hypertrophic growth of the heart (compared to isoproterenol challenge during the awake phase) (Durgan et al., 2011b). Such observations may provide insight regarding the pathogenesis of hypertrophic cardiomyopathy associated with non-dipping hypertension and sleep apnea, when the heart is challenged at an inappropriate time of day. Interestingly, ischemia/reperfusion tolerance is highest in the heart at the beginning of the sleep phase (Durgan et al., 2010), a time when autophagy (a cardioprotective mechanism) is activated. We speculate that disruption of the cardiomyocyte circadian clock by common behaviors such as sleep/wake disruption, shift work, frequent travel across time zones, and nighttime eating significantly contribute towards cardiovascular disease risk through impairment of normal metabolic rhythms.
Recent Findings.
Cardiac glucose utilization peaks during the middle of the active period, likely to meet increased energetic demands at this time.
Synthesis of glycogen and triglyceride peak in the heart in the middle and end of the active period (respectively), likely in anticipation of the upcoming sleep/fasting period.
Protein turnover increases in the heart at the beginning of the sleep phase, likely to promote growth and repair at this time.
Temporal partitioning of metabolic processes in the heart is mediated in large part by the cardiomyocyte circadian clock.
Acknowledgments
This work was supported by the National Heart, Lung, and Blood Institute (HL106199, HL074259, HL123574, HL122975).
Footnotes
Competing Interests
None of the authors have any conflicts of interests.
References
- Allard M, Schonekess B, Henning S, English D, Lopaschuk G. Contribution of oxidative metabolism and glycolysis to ATP production in hypertrophied hearts. Am J Physiol. 1994;267:H742–H750. doi: 10.1152/ajpheart.1994.267.2.H742. [DOI] [PubMed] [Google Scholar]
- Bray MS, Shaw CA, Moore MW, Garcia RA, Zanquetta MM, Durgan DJ, Jeong WJ, Tsai JY, Bugger H, Zhang D, Rohrwasser A, Rennison JH, Dyck JR, Litwin SE, Hardin PE, Chow CW, Chandler MP, Abel ED, Young ME. Disruption of the circadian clock within the cardiomyocyte influences myocardial contractile function, metabolism, and gene expression. Am J Physiol Heart Circ Physiol. 2008;294:H1036–1047. doi: 10.1152/ajpheart.01291.2007. [DOI] [PubMed] [Google Scholar]
- Durgan D, Hotze M, Tomlin T, Egbejimi O, Graveleau C, Abel E, Shaw C, Bray M, Hardin P, Young M. The intrinsic circadian clock within the cardiomyocyte. Am J Physiol Heart Circ Physiol. 2005;289:H1530–H1541. doi: 10.1152/ajpheart.00406.2005. [DOI] [PubMed] [Google Scholar]
- Durgan D, Moore M, Ha N, Egbejimi O, Fields A, Mbawuike U, Egbejimi A, Shaw C, Bray M, Nannegari V, Hickson-Bick D, Heird W, Dyck J, Chandler M, Young M. Circadian rhythms in myocardial metabolism and contractile function: influence of workload and oleate. Am J Physiol Heart Circ Physiol. 2007;293:H2385–H2393. doi: 10.1152/ajpheart.01361.2006. [DOI] [PubMed] [Google Scholar]
- Durgan D, Trexler N, Egbejimi O, McElfresh T, Suk H, Petterson L, Shaw C, Hardin P, Bray M, Chandler M, Chow C, Young M. The circadian clock within the cardiomyocyte is essential for responsiveness of the heart to fatty acids. J Biol Chem. 2006;281:24254–24269. doi: 10.1074/jbc.M601704200. [DOI] [PubMed] [Google Scholar]
- Durgan DJ, Pat BM, Laczy B, Bradley JA, Tsai JY, Grenett MH, Ratcliffe WF, Brewer RA, Nagendran J, Villegas-Montoya C, Zou C, Zou L, Johnson RL, Jr, Dyck JR, Bray MS, Gamble KL, Chatham JC, Young ME. O-GlcNAcylation, novel post-translational modification linking myocardial metabolism and cardiomyocyte circadian clock. J Biol Chem. 2011a;286:44606–44619. doi: 10.1074/jbc.M111.278903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durgan DJ, Pulinilkunnil T, Villegas-Montoya C, Garvey ME, Frangogiannis NG, Michael LH, Chow CW, Dyck JR, Young ME. Short communication: ischemia/reperfusion tolerance is time-of-day-dependent: mediation by the cardiomyocyte circadian clock. Circ Res. 2010;106:546–550. doi: 10.1161/CIRCRESAHA.109.209346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durgan DJ, Tsai JY, Grenett MH, Pat BM, Ratcliffe WF, Villegas-Montoya C, Garvey ME, Nagendran J, Dyck JR, Bray MS, Gamble KL, Gimble JM, Young ME. Evidence suggesting that the cardiomyocyte circadian clock modulates responsiveness of the heart to hypertrophic stimuli in mice. Chronobiol Int. 2011b;28:187–203. doi: 10.3109/07420528.2010.550406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durgan DJ, Young ME. The cardiomyocyte circadian clock: emerging roles in health and disease. Circ Res. 2010;106:647–658. doi: 10.1161/CIRCRESAHA.109.209957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gekakis N, Staknis D, Nguyen H, Davis F, Wilsbacher L, King D, Takahashi J, Weitz C. Role of the CLOCK protein in the mammalian circadian mechanism. Science. 1998;280:1564–1569. doi: 10.1126/science.280.5369.1564. [DOI] [PubMed] [Google Scholar]
- Goodwin G, Taylor C, Taegtmeyer H. Regulation of energy metabolism of the heart during acute increase in heart work. J Biol Chem. 1998;273:29530–29539. doi: 10.1074/jbc.273.45.29530. [DOI] [PubMed] [Google Scholar]
- He L, Brewer RA, Shanmugam G, Rajasekaran NS, Darley-Usmar V, Chatham JC, Zhang J, Young ME. Influence of the Cardiomyocyte Circadian Clock on Autophagy in the Heart. FASEB J. 2016a Experimental Biology Abstract. [Google Scholar]
- He L, Hamm JA, Reddy A, Sams D, Peliciari-Garcia RA, McGinnis GR, Bailey SM, Chow CW, Rowe GC, Chatham JC, Young ME. Biotinylation: A Novel Posttranslational Modification Linking Cell Autonomous Circadian Clocks with Metabolism. Am J Physiol Heart Circ Physiol. 2016b doi: 10.1152/ajpheart.00959.2015. ajpheart 00959 02015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogenesch J, Gu Y, Jain S, Bradfield C. The basic-helix-loop-helix-PAS orphan MOP3 forms transcriptionally active complexes with circadian and hypoxia factors. Proc Natl Aad Sci US A. 1998;95:5474–5479. doi: 10.1073/pnas.95.10.5474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa K, Shimazu T. Daily rhythms of glycogen synthetase and phosphorylase activities in rat liver: influence of food and light. Life Sci. 1976;19:1873–1878. doi: 10.1016/0024-3205(76)90119-3. [DOI] [PubMed] [Google Scholar]
- Podobed P, Pyle WG, Ackloo S, Alibhai FJ, Tsimakouridze EV, Ratcliffe WF, Mackay A, Simpson J, Wright DC, Kirby GM, Young ME, Martino TA. The day/night proteome in the murine heart. Am J Physiol Regul Integr Comp Physiol. 2014;307:R121–137. doi: 10.1152/ajpregu.00011.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer FA, Hu K, Evoniuk H, Kelly EE, Malhotra A, Hilton MF, Shea SA. Impact of the human circadian system, exercise, and their interaction on cardiovascular function. Proc Natl Acad Sci U S A. 2010;107:20541–20546. doi: 10.1073/pnas.1006749107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer FA, van Doornen LJ, Buijs RM. Light and diurnal cycle affect human heart rate: possible role for the circadian pacemaker. J Biol Rhythms. 1999;14:202–212. doi: 10.1177/074873099129000614. [DOI] [PubMed] [Google Scholar]
- Takahashi JS, Hong HK, Ko CH, McDearmon EL. The genetics of mammalian circadian order and disorder: implications for physiology and disease. Nat Rev Genet. 2008;9:764–775. doi: 10.1038/nrg2430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai JY, Kienesberger PC, Pulinilkunnil T, Sailors MH, Durgan DJ, Villegas-Montoya C, Jahoor A, Gonzalez R, Garvey ME, Boland B, Blasier Z, McElfresh TA, Nannegari V, Chow CW, Heird WC, Chandler MP, Dyck JR, Bray MS, Young ME. Direct regulation of myocardial triglyceride metabolism by the cardiomyocyte circadian clock. J Biol Chem. 2010;285:2918–2929. doi: 10.1074/jbc.M109.077800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young M. The circadian clock within the heart: potential influence on myocardial gene expression; metabolism; and function. Am J Physiol Heart Circ Physiol. 2006;290:H1–H16. doi: 10.1152/ajpheart.00582.2005. [DOI] [PubMed] [Google Scholar]
- Young M, Razeghi P, Cedars A, Guthrie P, Taegtmeyer H. Intrinsic diurnal variations in cardiac metabolism and contractile function. Circ Res. 2001;89:1199–1208. doi: 10.1161/hh2401.100741. [DOI] [PubMed] [Google Scholar]
- Young ME, Brewer RA, Peliciari-Garcia RA, Collins HE, He L, Birky TL, Peden BW, Thompson EG, Ammons BJ, Bray MS, Chatham JC, Wende AR, Yang Q, Chow CW, Martino TA, Gamble KL. Cardiomyocyte-specific BMAL1 plays critical roles in metabolism, signaling, and maintenance of contractile function of the heart. J Biol Rhythms. 2014;29:257–276. doi: 10.1177/0748730414543141. [DOI] [PMC free article] [PubMed] [Google Scholar]