Abstract
This phase I study in Japanese patients evaluated the safety, pharmacokinetics, and preliminary efficacy of palbociclib, a highly selective and reversible oral cyclin‐dependent kinase 4/6 inhibitor, as monotherapy for solid tumors (part 1) and combined with letrozole as first‐line treatment of postmenopausal patients with estrogen receptor‐positive, human epidermal growth factor receptor 2‐negative advanced breast cancer (part 2). Part 1 evaluated palbociclib 100 and 125 mg once daily (3 weeks on/1 week off; n = 6 each group) to determine the maximum tolerated dose. Part 2 evaluated palbociclib maximum tolerated dose (125 mg) plus letrozole 2.5 mg (n = 6). The most common treatment‐related adverse event was neutropenia (all grades/grade 3/4): 100 mg, 83%/67%; 125 mg, 67%/33%; and palbociclib plus letrozole, 100%/83%. Heavier pretreatment with chemotherapy may have resulted in higher neutropenia rates observed with the 100‐mg dose. Palbociclib exposure was higher with 125 vs 100 mg (mean area under the plasma concentration–time curve over dosing interval [τ]: 1322 vs 547.5 ng·h/mL [single dose], 2838 vs 1276 ng·h/mL [multiple dose]; mean maximum plasma concentration: 104.1 vs 41.4 ng/mL [single dose], 185.5 vs 77.4 ng/mL [multiple dose]). Half‐life was 23–26 h. No drug–drug interactions between palbociclib and letrozole occurred. Four patients had stable disease (≥24 weeks in one patient with rectal cancer [100 mg] and one with esophageal cancer [125 mg]) in part 1; two patients had partial response and two had stable disease (both ≥24 weeks) in part 2. Palbociclib at the 125‐mg dose (schedule 3/1) was tolerated and is the recommended dose for monotherapy and letrozole combination therapy in Japanese patients. The trials are registered with www.ClinicalTrials.gov: A5481010 and NCT01684215.
Keywords: Breast cancer, cyclin‐dependent kinase, Japanese, letrozole, palbociclib
Palbociclib (PD‐0332991) is a potent and highly selective, reversible, oral inhibitor of cyclin‐dependent kinases 4 and 6 that blocks G1‐ to S‐phase progression of the cell cycle, thereby preventing DNA synthesis.1, 2, 3, 4 Cyclin‐dependent kinase 4/6 inhibition is thought to have broad applicability to the treatment of advanced cancers.5 In estrogen receptor‐positive (ER+) luminal breast cancer cell lines, palbociclib was shown to arrest tumor cell growth, accompanied by an inhibition of retinoblastoma protein hyperphosphorylation, and it also showed synergistic antitumor activity when combined with tamoxifen.6
Currently, endocrine therapies such as tamoxifen, fulvestrant, and aromatase inhibitors are the standard of care for women with ER+ advanced or metastatic breast cancer; however, many patients develop resistance to these therapies.7 A randomized phase II trial (PALOMA‐1/TRIO‐18) evaluated palbociclib (125 mg once daily) in combination with the aromatase inhibitor letrozole (2.5 mg once daily) compared with letrozole alone as first‐line therapy for postmenopausal women with ER+, human epidermal growth factor receptor 2‐negative (HER2−) advanced breast cancer.8 The combination group had significantly longer progression‐free survival (PFS) compared with the letrozole monotherapy group: median PFS of 20.2 months vs 10.2 months (hazard ratio, 0.488; 95% confidence interval, 0.319–0.748; one‐sided P = 0.0004). Palbociclib plus letrozole was generally well tolerated, with patients most commonly developing uncomplicated neutropenia.
Based on this encouraging activity and tolerability, but a lack of clinical experience with palbociclib in Japanese patients, a phase I study was designed to evaluate the safety, pharmacokinetics (PK), and preliminary efficacy of palbociclib as a single agent in Japanese patients with solid tumors and in combination with letrozole in first‐line treatment of Japanese postmenopausal patients with ER+/HER2− advanced breast cancer.
Materials and Methods
Study design
This was a phase I, single‐country, non‐randomized, open‐label, clinical study in Japanese patients (NCT01684215). As shown in Figure 1, the study comprised two parts: (i) dose escalation study of palbociclib given as a single agent to identify the maximum tolerated dose (MTD) and assess the PK and preliminary efficacy of palbociclib in patients with advanced solid tumors in part 1, including the lead‐in phase for PK evaluation after a single dose; and (ii) evaluation of the overall safety, PK, and preliminary efficacy of the combination of the MTD of palbociclib plus 2.5 mg letrozole in the first‐line treatment of patients with ER+/HER2− advanced breast cancer in part 2. Part 1 used the 3 + 3 dose escalation scheme; target accrual for part 1 was approximately 6–12 patients, depending on the observed safety profile. For part 2, the target sample size was six patients.
Figure 1.
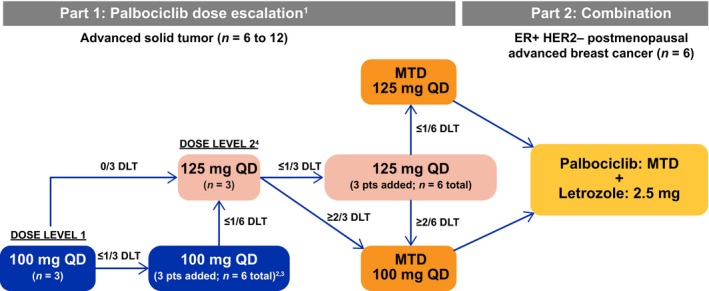
Design of this phase I study of palbociclib in Japanese patients. 1In principle, two dosages (100 mg once daily [QD] and 125 mg QD) were examined; where necessary, additional/lower dose levels (75 mg QD, dose level −1) were explored. 2If two or more patients of three to six patients at dose level 1 experienced a dose‐limiting toxicity (DLT) during cycle 1, the dose was considered intolerable and a lower dose (75 mg QD, dose level −1) was used. 3If no further DLTs occurred in the three additional patients such that only one of six patients at dose level 1 experienced DLT(s) during the first cycle, then the dose was escalated to dose level 2 (125 mg QD) in a subsequent cohort of patients. 4If two or more patients of three to six patients at dose level 2 experienced a DLT during the first cycle, the dose was de‐escalated to dose level 1 (100 mg QD) unless six patients were enrolled and evaluated at dose level 1 at that time. ER+, estrogen receptor‐positive; HER2−, human epidermal growth factor receptor‐negative; MTD, maximum tolerated dose; pts, patients.
The study protocol was approved by the Institutional Review Board of the National Cancer Center (Japan), and all patients gave written informed consent for participation. The study was carried out in accordance with applicable local laws and regulatory requirements, as well as the International Conference on Harmonisation's Note for Guidance on Good Clinical Practice and the Declaration of Helsinki.
Patients
Key inclusion criteria (both study parts) included: age ≥20 years; Eastern Cooperative Oncology Group performance status 0–1; and adequate bone marrow, renal, and liver function. Additional inclusion criteria were as follows. For part 1, patients were required to have an advanced solid tumor, other than small‐cell lung cancer or retinoblastoma, that was refractory to standard therapy or lacked an available standard therapy. For part 2, postmenopausal patients had ER+/HER2− adenocarcinoma of the breast that showed evidence of locoregionally recurrent or metastatic disease (including bone‐only disease) and was not amenable to resection or radiation therapy with curative intent, and for which chemotherapy was not clinically indicated.
Key exclusion criteria (both study parts) were baseline corrected QT (QTc) interval >470 ms, history (or documented family history) of long‐QT syndrome, history of clinically significant ventricular dysrhythmias, or current treatment with antiarrhythmic medication or implanted defibrillation device for ventricular dysrhythmias. Additional exclusion criteria were as follows. For part 1, recent receipt of cytotoxic chemotherapy or radiation (within 3 weeks); hormone therapy, immunotherapy, or other biologic therapy (within 14 days), or palliative radiotherapy (within 7 days) was not allowed. For part 2, patients must not have received previous systemic anticancer treatment for advanced breast cancer, prior neoadjuvant or adjuvant therapy with a non‐steroidal aromatase inhibitor with disease recurrence on or within 12 months of treatment, or chemotherapy, radiotherapy, investigational agents, or other anticancer therapy within 2 weeks of the study.
Study treatment
In part 1, palbociclib 100 or 125 mg once daily was taken orally without any food or drink (except for water) consumption within ± 2 h of dosing and continually in a 3‐weeks‐on/1‐week‐off treatment schedule, defining a 28‐day treatment cycle; intrapatient dose escalation was not permitted. For cycle 1 (in part 1 only), there was a PK lead‐in phase in which a single dose was given 7 days before day 1 of cycle 1. In part 2, palbociclib was given at the MTD determined in part 1 (given once daily) plus letrozole; letrozole was to be taken continually (or alone in the event of palbociclib dosing interruption). In parts 1 and 2, palbociclib dose was interrupted or reduced if drug‐related toxicity occurred according to predefined dose‐modification criteria. Minimum available palbociclib dose was 75 mg once daily. Patients continued treatments until intolerable toxicity, progressive disease, or withdrawal of consent.
Assessments
Dose‐limiting toxicity criteria (part 1)
In part 1, any of the following treatment‐related adverse events (AEs) during the first cycle were to be classified as dose‐limiting toxicities (DLTs): (i) grade 4 neutropenia lasting >7 days, febrile neutropenia (grade ≥3 with body temperature ≥38.5°C), grade ≥3 thrombocytopenia with bleeding, or grade 4 thrombocytopenia; (ii) grade ≥3 non‐hematologic toxicity with the exception of grade ≥3 nausea, vomiting, and/or diarrhea controllable with antiemetics and antidiarrheals, or grade ≥3 electrolyte abnormalities controllable with electrolyte supplementation or lacking significant clinical symptoms; and (iii) grade 3 QTc prolongation persisting after correction of any reversible cause. Additional DLT criteria included an inability to receive the next dose within 1 week of the last day of the previous cycle because of lack of hematologic recovery (platelets <50 000/μL, absolute neutrophil count [ANC] <1000/μL, or hemoglobin <8.0 g/dL) or prolonged non‐hematologic toxicities attributable to palbociclib, as well as receipt of <75% of the planned dose of palbociclib in the first cycle due to toxicities attributable to palbociclib. The MTD was defined as the highest dose level studied for which the incidence of first‐cycle DLT is less than 33%.
Safety
Safety assessments included AEs (graded by the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0), with the exception of febrile neutropenia and QTc DLT criteria, laboratory testing (hematology, blood chemistry, coagulation profiles, and urinalysis), 12‐lead electrocardiogram monitoring, physical examination, pulse oximetry, and Eastern Cooperative Oncology Group performance status assessment. Monitoring of AEs was continuous, whereas the other parameters were assessed on days 1 and 15 of each cycle (with hematology and pulse oximetry also assessed on day 8 in cycle 1 only).
Pharmacokinetic sampling
Pharmacokinetic samples were obtained: predose and 1, 2, 4, 6, 8, 12, 24, 48, 72, 96, and 120 h postdose during the lead‐in phase in part 1 (single dose); predose and 1, 2, 4, 6, 8, 12, and 24 h postdose on day 8 of cycle 1 in part 1 (multiple doses); and predose and 4 h postdose on day 15 of cycles 1 and 2, as well as predose on day 1 of cycles 2 and 3 in part 2.
Antitumor activity
Tumor measurement by computed tomography or MRI were carried out at screening, every 8 (part 1) or 12 (part 2) weeks during the study treatment period, and at the end of study treatment. Radionuclide bone scans were required at screening in part 2, every 24 weeks during study treatment, and at the end of study treatment if bone lesions were identified at screening. Assessments of tumor response and progression were carried out using computed tomography or MRI scans and categorized using Response Evaluation Criteria in Solid Tumors version 1.1. Objective responses required confirmation at least 4 weeks after the initial documented response.
Data analysis
The DLT evaluation set included all patients in whom DLTs were evaluable in cycle 1, with the PK analysis set consisting of all patients who had completed at least one day of PK blood sampling. Plasma palbociclib and letrozole concentrations were determined using a validated HPLC method with tandem mass spectrometry (lower limit of quantification, 1.00 ng/mL for palbociclib, 2.00 ng/mL for letrozole) at PPD (Richmond, VA, USA) for palbociclib and at WuXi AppTec (Shanghai, China) for letrozole. Pharmacokinetic parameters on day −7 in the lead‐in phase of part 1 and day 8 of cycle 1 in part 1 were estimated using non‐compartmental methods (internal software eNCA, version 2.2.4; Pfizer, Groton, CT, USA). The PK parameters assessed after single and multiple doses included maximum plasma concentration (Cmax), terminal half‐life (t½), time at which Cmax was observed (tmax), area under the plasma concentration–time curve from time 0 to time of last measurable plasma concentration (AUClast) and AUC from time 0 to infinity (AUCinf) for only a single dose, AUC over dosing interval τ (AUCτ) for only multiple doses. Accumulation ratio (Rac) and predicted accumulation ratio to estimate linearity (Rss) were also evaluated after multiple doses. The drug–drug interaction potential between palbociclib and letrozole was assessed using trough plasma concentration (Ctrough) and plasma concentration at 4 h postdosing (C4) of palbociclib and letrozole.
In both parts 1 and 2, the safety analysis set included all enrolled patients who receive at least one dose of study drugs. Objective response rate (complete response [CR] or partial response [PR]) and disease control rate (DCR; CR, PR, or stable disease ≥24 weeks) were calculated. Progression‐free survival was also assessed; PFS data were censored on the date of the last tumor assessment during the study for patients without objective tumor progression who did not die while on the study.
Results
Each group of six patients was enrolled at two dose levels in parts 1 or 2; a total of 18 patients were enrolled. The data cut‐off date was March 31, 2015. Baseline characteristics for the 18 treated patients are shown in Table 1. Overall, the study population had a good performance status and was heavily pretreated in part 1, with more than 80% of patients having received three or more prior systemic therapies.
Table 1.
Baseline characteristics of Japanese patients participating in a two‐part phase I trial of palbociclib
| Part 1 | Part 2 | ||
|---|---|---|---|
| Palbociclib 100 mg, n = 6 | Palbociclib 125 mg, n = 6 | Palbociclib 125 mg + letrozole, n = 6 | |
| Median age (range), years | 59 (44–65) | 49 (24–69) | 62 (59–76) |
| Female sex, n (%) | 5 (83) | 2 (33) | 6 (100) |
| Median weight (range), kg | 65 (47–94) | 58 (36–81) | 55 (42–62) |
| ECOG PS, n (%) | |||
| 0 | 5 (83) | 4 (67) | 3 (50) |
| 1 | 1 (17) | 2 (33) | 3 (50) |
| Tumor types, n (%) | |||
| Breast cancer | 2 (33) | 1 (17) | 6 (100) |
| Other† | 4 (67) | 5 (83) | 0 (0) |
| Prior systemic therapies,‡ n (%) | 6 (100) | 6 (100) | 4 (67)‡ , § |
| Regimens | |||
| 1 | 0 (0) | 0 (0) | 0 (0) |
| 2 | 0 (0) | 2 (33) | 2 (33) |
| 3 | 1 (17) | 2 (33) | 1 (17) |
| >3 | 5 (83) | 2 (33) | 1 (17) |
†Including colon cancer, medullary thyroid cancer, ovarian cancer, and rectal cancer (n = 1 each) in the 100‐mg group; fibroma, esophageal carcinoma, rectal cancer, inflammatory myofibroblastic tumor, and pancreatic cancer (n = 1 each) in the 125‐mg group. ‡Including adjuvant or neoadjuvant therapy. §Patients who had received adjuvant therapy (recorded as a prior systemic therapy) were eligible if therapy was not used for their locoregionally recurrent or metastatic estrogen receptor‐positive breast cancer. ECOG PS, Eastern Cooperative Oncology Group performance status.
Safety
Dose‐limiting toxicity by dose level
Dose‐limiting toxicity was observed in one patient per dose level in part 1 (Table 2). Both patients had breast cancer and were heavily pretreated relative to the other patients; one patient received <75% of the planned 100‐mg dose because of grades 3 and 4 decreased neutrophil count, and the other patient had a decreased platelet count (grade 4) on palbociclib 125 mg. The MTD for palbociclib was determined to be 125 mg once daily and was used in part 2 in combination with letrozole.
Table 2.
Dose‐limiting toxicities observed in part 1 of a two‐part phase I trial of palbociclib
| Tumor type | Disease stage at time of study entry | Sex | Age, years | Duration from histopathologic diagnosis, years | DLT |
|---|---|---|---|---|---|
| 100‐mg dose group | |||||
| Ovarian cancer | III C | Female | 62 | 3.49 | None |
| Breast cancer | IV | Female | 65 | 10.28 | Yes† |
| Colon cancer | IV | Female | 49 | 1.46 | None |
| Medullary thyroid cancer | IV | Male | 44 | 3.05 | None |
| Rectal cancer | IV | Female | 56 | 2.46 | None |
| Breast cancer | IV | Female | 65 | 2.36 | None |
| 125‐mg dose group | |||||
| Inflammatory myofibroblastic tumor | IV B | Male | 24 | 1.86 | None |
| Pancreatic acinar cell carcinoma | IV | Female | 24 | 0.52 | None |
| Esophageal cancer | IV | Male | 42 | 2.27 | None |
| Fibroma | IV | Male | 58 | 3.00 | None |
| Breast cancer | IV | Female | 69 | 12.08 | Yes‡ |
| Rectal cancer | IV | Male | 55 | 2.01 | None |
†Less than 75% of planned dose received because of decreased neutrophil count (grades 3 and 4). ‡Decreased platelet count (grade 4). DLT, dose‐limiting toxicity.
Treatment‐related adverse events
Common treatment‐related AEs were hematologic toxicities, most often neutropenia and leukopenia (Table 3). All patients in part 2 developed neutropenia and leukopenia, with grade 3/4 incidences of 83% and 50%, respectively. Generally, ANC decreased with palbociclib treatment and recovered during the treatment‐off period (Fig. 2).
Table 3.
Treatment‐related adverse events (AEs) occurring in two or more patients in any palbociclib treatment cohort
| Part 1 | Part 2 | |||||
|---|---|---|---|---|---|---|
| AE,† n (%) | Palbociclib 100 mg, n = 6 | Palbociclib 125 mg, n = 6 | Palbociclib 125 mg + letrozole, n = 6 | |||
| All grades | Grade 3/4 | All grades | Grade 3/4 | All grades | Grade 3/4 | |
| Any AE | 6 (100) | 4 (67) | 5 (83) | 4 (67) | 6 (100) | 5 (83) |
| Neutrophils decreased | 5 (83) | 4 (67) | 4 (67) | 2 (33) | 6 (100) | 5 (83) |
| WBCs decreased | 4 (67) | 2 (33) | 5 (83) | 2 (33) | 6 (100) | 3 (50) |
| Blood creatinine increased | 2 (33) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Platelets decreased | 1 (17) | 0 (0) | 2 (33) | 1 (17) | 3 (50) | 0 (0) |
| Lymphocytes decreased | 1 (17) | 1 (17) | 3 (50) | 2 (33) | 0 (0) | 0 (0) |
| Fatigue | 0 (0) | 0 (0) | 2 (33) | 0 (0) | 2 (33) | 0 (0) |
| Diarrhea | 0 (0) | 0 (0) | 2 (33) | 0 (0) | 1 (17) | 0 (0) |
†Graded using National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. WBC, white blood cell.
Figure 2.
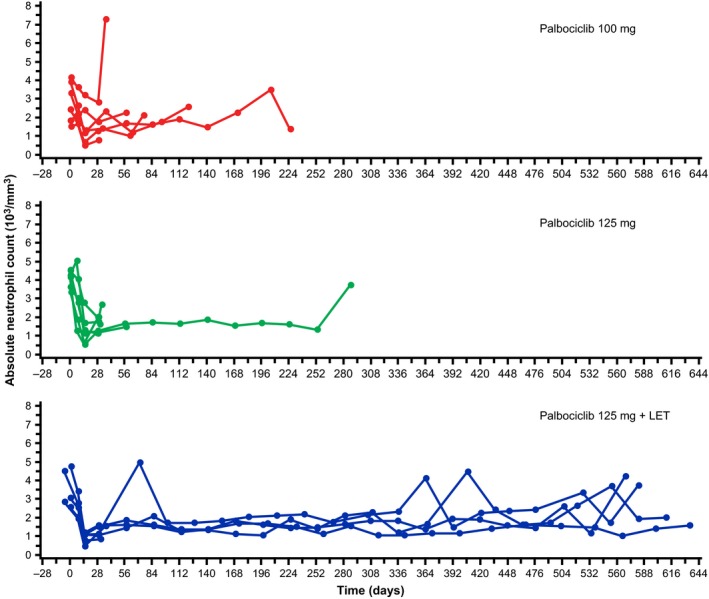
Time course change in absolute neutrophil count in a phase I study of palbociclib in Japanese patients. LET, letrozole.
Non‐hematologic toxicities were infrequently seen, with the most commonly reported events limited to two cases per cohort. The most common all‐grade non‐hematologic events were increased blood creatinine with palbociclib 100 mg and fatigue and diarrhea with palbociclib 125 mg, whether given as monotherapy or with letrozole (Table 3). No grade ≥3 treatment‐related non‐hematologic AEs were observed.
Serious adverse events and deaths
Only one serious AE was reported in this study (grade 4 gastrointestinal perforation in the palbociclib plus letrozole cohort), which was not considered treatment‐related. No deaths were reported in the study.
Pharmacokinetics
In the PK assessment of palbociclib 100 and 125 mg (part 1), higher than dose‐proportional exposure was observed at 125 mg (Table 4, Fig. 3), whereas median tmax (4–5 h) and t½ (23–26 h) values remained relatively constant (Table 4).
Table 4.
Summary of plasma palbociclib pharmacokinetic parameter values (day 8 of cycle 1) following single and once‐daily multiple dosing
| Parameter (unit) | Summary statistics for palbociclib† | |||
|---|---|---|---|---|
| 100 mg | 125 mg | |||
| Single dose | Multiple doses | Single dose | Multiple doses | |
| n | 6 | 6 | 6 | 6 |
| Cmax (ng/mL) | 41.4 (15) | 77.4 (33) | 104.1 (39) | 185.5 (27) |
| tmax (h) | 5.0 (4.0–8.0) | 4.0 (4.0–6.0) | 4.0 (3.9–8.0) | 4.0 (4.0–6.0) |
| t½ (h) | 25.7 ± 5.3 | 23.8 ± 6.8 | 23.9 ± 2.7 | 23.2 ± 7.7 |
| AUClast (ng·h/mL) | 971.7 (31) | NA | 2396 (48) | NA |
| AUCinf (ng·h/mL) | 1039 (32) | NA | 2483 (49) | NA |
| AUCτ ‡ (ng·h/mL) | 547.5 (19) | 1276 (45) | 1322 (42) | 2838 (43) |
| Rac | NA | 2.1 (1.8–3.5) | NA | 1.9 (1.7–3.1) |
| Rss | NA | 1.1 (1.0–1.7) | NA | 1.1 (0.9–1.5) |
†Data are geometric mean (geometric %CV), except for tmax, Rac, and Rss (median [range]) and t½ (arithmetic mean ± SD).
‡AUCτ is the same as AUC from time 0–24 h (AUC0–24) in this study.
AUClast, area under the plasma concentration‐time curve from time zero to time of last measurable plasma concentration; AUCτ, area under the plasma concentration‐time curve over dosing interval; AUCinf, area under the plasma concentration‐time curve from time 0 extrapolated to infinity; Cmax, maximum plasma concentration; NA, not applicable; Rac, ratio of AUCτ after multiple doses/AUCτ after single dose; Rss, ratio of AUC? after multiple doses/AUCinf after single dose; t½, half‐life; tmax, time at which Cmax was observed.
Figure 3.
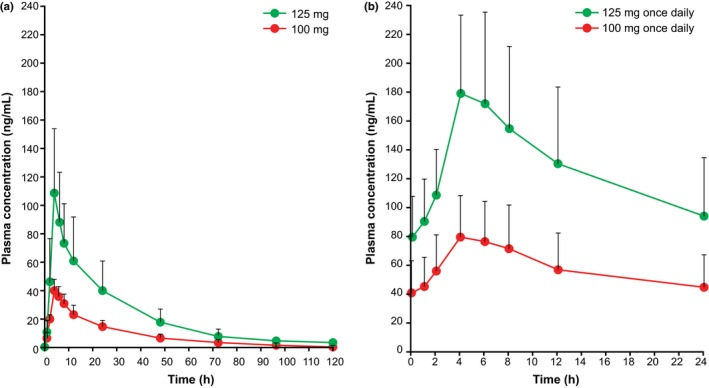
Mean ± SD plasma palbociclib concentration–time profiles on pharmacokinetic lead‐in phase day −7 following single oral dosing (a) and day 8 of cycle 1 following multiple oral dosing (b) in Japanese patients.
Following multiple oral doses of palbociclib plus letrozole in part 2, the geometric mean ratios of the predose (Ctrough) and 4 h postdose (C4) plasma palbociclib concentrations for palbociclib plus letrozole (part 2) versus palbociclib 125 mg alone (part 1) were 1.2 and 0.9, respectively (Table 5). Similarly, the geometric mean ratio of the predose plasma letrozole concentration for palbociclib plus letrozole versus letrozole alone (part 2) was 0.9 (Table 6). Therefore, there was no evidence of a drug–drug interaction between palbociclib and letrozole.
Table 5.
Summary of palbociclib plasma concentrations following multiple oral doses of palbociclib 125 mg and letrozole 2.5 mg once daily
| Parameter (unit) | Plasma palbociclib concentrations | |
|---|---|---|
| Predose [Ctrough] | 4 h Postdose [C4] | |
| Geometric meana (ng/mL) | 88.5 | 155 |
| Geometric CV (%)a | 49 | 32 |
| Geometric mean on day 8of part 1 (ng/mL) | 72.8 | 172 |
| Geometric mean ratio (palbociclib + letrozole [part 2]/ palbociclib 125 mg alone [part 1]) | 1.2 | 0.9 |
Calculated using arithmetic mean values for each patient on day 15 of cycles 1 and 2. C4, plasma concentration at 4 h postdose; Ctrough, trough plasma concentration; CV, coefficient of variation.
Table 6.
Summary of trough plasma letrozole concentrations following multiple oral doses of palbociclib 125 mg and letrozole 2.5 mg once daily
| Parameter (unit) | Predose plasma letrozole concentrations | |
|---|---|---|
| Letrozole alone | Palbociclib + letrozole | |
| Geometric mean Ctrough (ng/mL) | 146† | 131‡ |
| Geometric CV (%) | 59† | 53‡ |
| Geometric mean ratio (palbociclib + letrozole/letrozole alone [part 2]) | 0.9 | |
†Calculated by using arithmetic mean values for each patient on day 1 of cycles 2 and 3. ‡Calculated by using arithmetic mean values for each patient on day 15 of cycles 1 and 2. Ctrough, trough plasma concentration; CV, coefficient of variation.
Relationship between change in absolute neutrophil count and pharmacokinetics
The maximum percentage change in ANC in cycle 1 correlated with PK parameters AUCτ and Cmax, with correlation coefficients of −0.5292 and −0.4581, respectively (Fig. 4).
Figure 4.
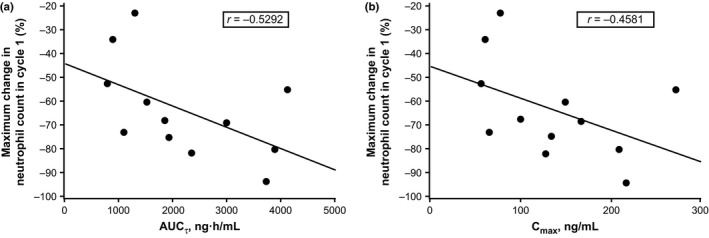
Relationship between change in absolute neutrophil count and pharmacokinetic parameters area under the plasma concentration–time curve over dosing interval (AUC τ) (a) and maximum plasma concentration (Cmax) (b).
Antitumor activity
In part 1, objective responses (CR or PR) were not reported; stable disease was observed in three of six patients (Table 7) receiving palbociclib 100 mg (one with stable disease lasting ≥24 weeks; patient with rectal cancer) and in one of six patients receiving palbociclib 125 mg (stable disease lasted ≥24 weeks; patient with esophageal cancer; Table 7). Among the six patients receiving palbociclib 125 mg plus letrozole in part 2, objective response was reported in two patients (PR; Table 7), and two patients had stable disease (lasting ≥24 weeks in both patients; Table 7). The DCR (objective response or stable disease ≥24 weeks) was 17% in patients receiving palbociclib 100 or 125 mg in part 1 and 67% in patients receiving palbociclib 125 mg combined with letrozole in part 2. Maximum tumor reductions are shown in Figure 5; the greatest tumor shrinkage was observed in patients with breast cancer treated with palbociclib 125 mg plus letrozole.
Table 7.
Individual tumor response in patients treated with palbociclib as monotherapy for solid tumors (part 1) or palbociclib combined with letrozole for estrogen receptor‐positive, human epidermal growth factor receptor 2‐negative advanced breast cancer (part 2)
| Primary diagnosis | Best response | Duration of objective response, days | Progression‐free survival, days |
|---|---|---|---|
| Palbociclib 100 mg (part 1) | |||
| Ovarian cancer | SD | 121 | |
| Breast cancer | Indeterminate | 29 | |
| Colon cancer | PD | 29 | |
| Medullary thyroid cancer | PD | 57 | |
| Rectal cancer | SD | 223 | |
| Breast cancer | SD | 75 | |
| Palbociclib 125 mg (part 1) | |||
| Inflammatory myofibroblastic tumor | PD | 28 | |
| Acinar cell carcinoma of pancreas | PD | 29 | |
| Esophageal carcinoma | SD | 280 | |
| Fibroma | PD | 28 | |
| Breast cancer | PD | 57 | |
| Rectal cancer | PD | 32 | |
| Palbociclib 125 mg plus letrozole (part 2) | |||
| Invasive ductal breast carcinoma | SD | ≥582† | |
| Invasive ductal breast carcinoma | PR | ≥498† | ≥582† |
| Invasive ductal breast carcinoma | SD | ≥592† | |
| Invasive ductal breast carcinoma | Indeterminate | 36 | |
| Invasive ductal breast carcinoma | Indeterminate | 31 | |
| Invasive ductal breast carcinoma | PR | ≥421† | ≥505† |
†Ongoing at the data cut‐off date. PD, progressive disease; PR, partial response; SD, stable disease.
Figure 5.
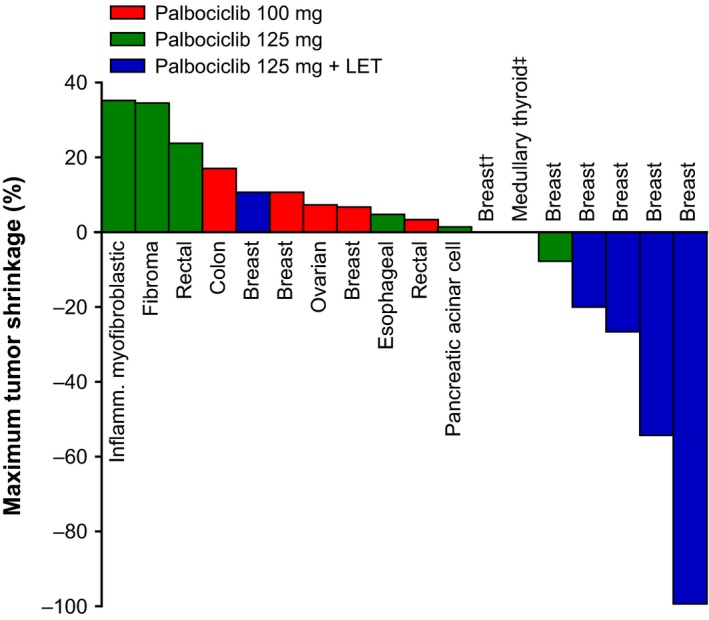
Maximum shrinkage of solid tumors and estrogen receptor‐positive, human epidermal growth factor receptor 2‐negative advanced breast cancer tumors treated with palbociclib 100 or 125 mg once daily and palbociclib 125 mg combined with letrozole (LET). Tumors were assessed using Response Evaluation Criteria in Solid Tumors version 1.1. †Palbociclib 125 mg + LET. ‡Palbociclib 100 mg.
Among patients receiving palbociclib 100 or 125 mg in part 1, duration of PFS ranged from 29 to 223 days and 28 to 280 days, respectively. In patients receiving palbociclib 125 mg plus letrozole in part 2, duration of PFS ranged from 31 to ≥592 days (Table 7).
Discussion
In part 1, we evaluated two dose levels of palbociclib and confirmed that the MTD of single‐agent palbociclib in Japanese patients was 125 mg, although additional higher doses were not investigated. The 125‐mg dose (schedule 3/1) was tolerated and considered a recommended dose for Japanese patients and western populations as monotherapy based on the observed DLTs and overall safety profile. After identification of the recommended dose for Japanese patients, we initiated part 2 to evaluate palbociclib (125 mg) plus letrozole (2.5 mg) in Japanese women with ER+/HER2− advanced breast cancer. The observed safety profile, both with palbociclib monotherapy and the palbociclib plus letrozole combination in Japanese patients, was consistent with AE data derived from prior Western phase I and phase II studies,8, 9 as common treatment‐related AEs were hematologic toxicities, particularly uncomplicated neutropenia. Palbociclib (125 mg) plus letrozole (2.5 mg) was well tolerated in Japanese women with ER+/HER2− advanced breast cancer. Regardless of the doses and regimens of palbociclib evaluated in this study, neutrophil counts were decreased during the 3‐week treatment period and quickly recovered in the 1‐week‐off treatment period, although an additional week of recovery was needed in some patients. In part 1, two patients who experienced DLTs were discontinued from the study; one patient because of decreased neutrophil count, the other because of disease progression. Although one serious AE (gastrointestinal perforation) was reported in this study, it was considered treatment‐unrelated; treatment‐related deaths were not reported. Overall, AEs were manageable and reversible with dose interruptions or dose reductions of palbociclib. No new safety signals were seen in either palbociclib monotherapy or palbociclib plus letrozole in Japanese patients.
In the present study, increased drug exposure, which was greater than dose proportional, was observed for palbociclib 125 mg, supporting further PK investigations for palbociclib in Japanese patients. For both single‐dose and multiple‐dose palbociclib, mean AUC and Cmax values with the 125‐mg dose were 2.2‐ to 2.6‐fold higher than those for the 100‐mg dose; however, tmax and t½ were similar between the 100‐ and 125‐mg dose groups. No apparent differences in the safety profiles were noted between the 100‐ and 125‐mg groups. Moreover, the safety profile with palbociclib monotherapy and the palbociclib plus letrozole combination in Japanese patients was similar to that observed in non‐Japanese patients.8, 9 In addition, the results from the population PK analysis using PK data from 183 patients whose body weight ranged from 37.9 kg to 123 kg in three multinational clinical trials indicated that the effect of body weight on the PK of palbociclib was not considered to be clinically important, suggesting dose adjustment is not necessary by body weight.10 This result supported that the recommended dose for Japanese patients identified in part 1 was the same as that recommended for non‐Japanese patients. Of note, a phase I study evaluating the PK parameters of palbociclib in healthy Japanese versus non‐Asian subjects has been completed recently (NCT02059330), which should provide additional insight. Importantly, there was no evidence of a drug–drug interaction between palbociclib and letrozole in the present study. The maximum change of ANC was correlated with the PK parameters (C max and AUCτ) of palbociclib, although the patient who observed DLT did not show the highest C max or AUC in each dose level (data not shown).
In part 1, extended stable disease (≥24 weeks) was observed in two patients (rectal and esophageal cancer) with palbociclib monotherapy at the 100‐ or 125‐mg dose, who failed standard of care at the study entry, suggesting monotherapy may be effective in some tumor types. Further investigation is warranted for the evaluation of palbociclib monotherapy.
Part 2 of our study focused on the combination of palbociclib plus letrozole for the first‐line treatment of postmenopausal patients with ER+/HER2− advanced breast cancer, which was preceded and supported by the encouraging PFS results reported in PALOMA‐1 carried out at study sites in North America, Europe, Africa, and Asia (but not Japan).8 In the present phase I study, four of six ER+/HER2− advanced breast cancer patients still continue the treatment for over 1 year and two showed objective responses, suggesting a similar benefit is offered by the combination regimen with letrozole in postmenopausal Japanese women with ER+/HER2− advanced breast cancer as seen in PALOMA‐1.8 The DCR was 67%, although two of six patients had no post‐treatment tumor assessment because of discontinuation of the study in cycle 1 due to AEs or at the patient's request. To further evaluate the efficacy of the combination of palbociclib plus letrozole in Japanese patients, a phase II study is ongoing, for which enrolment is now complete. Two global randomized phase III studies (PALOMA‐2 [NCT01740427] and PALOMA‐3 [NCT01942135]) are also ongoing, assessing PFS as the primary endpoint in patients with advanced breast cancer.
The results from the ongoing PALOMA‐3 trial showed significantly longer PFS with palbociclib plus fulvestrant compared with fulvestrant alone in patients with ER+/HER2− advanced breast cancer that had progressed during prior endocrine therapy.11 Further evaluation of these therapies in Japanese patients is also warranted.
In conclusion, although a higher than dose‐proportional increase in exposure was observed with palbociclib 125 mg relative to 100 mg, no interaction between palbociclib and letrozole was observed in this group of Japanese patients with advanced cancer, and one patient with esophageal cancer treated with the 125‐mg dose experienced stable disease >24 weeks. The 125‐mg dose (schedule 3/1) was tolerated and considered a recommended dose for monotherapy and letrozole combination therapy in Japanese patients. Based on these findings, the present study was expanded in Japan to phase II to further evaluate the efficacy and safety of palbociclib 125 mg once daily (3/1 schedule) in combination with letrozole for first‐line treatment of postmenopausal patients with ER+/HER2− advanced breast cancer.
Disclosure Statement
Authors S.H., Y.M., T.N., and Y.U. are employees of Pfizer. H.M. received honoraria from AstraZeneca, Eisai, and Taiho Pharmaceutical and received research funding from Chugai Pharmaceutical, Daiichi Sankyo, Eisai, Nippon Kayaku, Novartis Pharma, Pfizer Japan, and Sanofi. N.Y. received honoraria from Eli Lilly and Company, Chugai, and AstraZeneca and received research funding from Takeda, Quintiles, Chugai, Bristol‐Myers Squibb, Astellas, Taiho, Esai, Daiichi Sankyo, Kyowa Hakko Kirin, and Boehringer Ingelheim. T.Y. received research funding from Pfizer. This study (Study A5481010; NCT01684215) was sponsored by Pfizer. All authors had full access to all of the data in the study and had final responsibility for the decision to submit for publication. Authors K.T., M.K., S.O., M.S., Y.T., K.Y., and Y.N. have no conflict of interest.
Acknowledgments
Editorial support was provided by Laurie Orloski and Cynthia Gobbel of Complete Healthcare Communications, LLC, and was funded by Pfizer Inc.
Cancer Sci 107 (2016) 755–763
Funding Information
Pfizer Inc.
References
- 1. Fry DW, Harvey PJ, Keller PR et al Specific inhibition of cyclin‐dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol Cancer Ther 2004; 3: 1427–38. [PubMed] [Google Scholar]
- 2. Toogood PL, Harvey PJ, Repine JT et al Discovery of a potent and selective inhibitor of cyclin‐dependent kinase 4/6. J Med Chem 2005; 48: 2388–406. [DOI] [PubMed] [Google Scholar]
- 3. Marzec M, Kasprzycka M, Lai R et al Mantle cell lymphoma cells express predominantly cyclin D1a isoform and are highly sensitive to selective inhibition of CDK4 kinase activity. Blood 2006; 108: 1744–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saab R, Bills JL, Miceli AP et al Pharmacologic inhibition of cyclin‐dependent kinase 4/6 activity arrests proliferation in myoblasts and rhabdomyosarcoma‐derived cells. Mol Cancer Ther 2006; 5: 1299–308. [DOI] [PubMed] [Google Scholar]
- 5. Roberts PJ, Bisi JE, Strum JC et al Multiple roles of cyclin‐dependent kinase 4/6 inhibitors in cancer therapy. J Natl Cancer Inst 2012; 104: 476–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Finn RS, Dering J, Conklin D et al PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor‐positive human breast cancer cell lines in vitro . Breast Cancer Res 2009; 11: R77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Milani A, Geuna E, Mittica G, Valabrega G. Overcoming endocrine resistance in metastatic breast cancer: current evidence and future directions. World J Clin Oncol 2014; 5: 990–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Finn RS, Crown JP, Lang I et al The cyclin‐dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first‐line treatment of oestrogen receptor‐positive, HER2‐negative, advanced breast cancer (PALOMA‐1/TRIO‐18): a randomised phase 2 study. Lancet Oncol 2015; 16: 25–35. [DOI] [PubMed] [Google Scholar]
- 9. Flaherty KT, Lorusso PM, Demichele A et al Phase I, dose‐escalation trial of the oral cyclin‐dependent kinase 4/6 inhibitor PD 0332991, administered using a 21‐day schedule in patients with advanced cancer. Clin Cancer Res 2012; 18: 568–76. [DOI] [PubMed] [Google Scholar]
- 10. Sun W, Wang DD. A population pharmacokinetic (PK) analysis of palbociclib (PD‐0332991) in patients (pts) with advanced solid tumors [abstract 462P]. Ann Oncol 2014; 25: iv146–64. [Google Scholar]
- 11. Turner NC, Ro J, Andre F et al Palbociclib in hormone‐receptor‐positive advanced breast cancer. N Engl J Med 2015; 373: 209–19. [DOI] [PubMed] [Google Scholar]


