Summary
Background
Superior mesenteric artery aneurysm (SMAA) is an uncommon vascular disorder. Complications such as rupture have been reported. Once complication has been encountered both surgical and endovascular treatment techniques can be considered.
Case Report
We present a case of 68-year old male patient with SMAA rupture treated by endovascular modality.
Conclusions
Endovascular therapy is an effective and less invasive option for rupture of superior mesenteric artery aneurysm.
MeSH Keywords: Aneurysm, Ruptured; Endovascular Procedures; Mesenteric Artery, Superior
Background
Superior mesenteric artery aneurysm (SMAA) is an uncommon vascular disorder accounting for 5.5–8% of all splanchnic artery aneurysms [1]. An isolated branch of SMAA is extremely rare. The most common complaint of patients with SMAA is acute onset of abdominal pain, due to intestinal ischemia. In rare cases, complications such as rupture have been reported. We present a case of SMAA rupture treated by endovascular modality.
Case Report
A 68-year-old male patient was admitted to our hospital with a complaint of rectal hemorrhage. Bleeding was persistent for 3 days. Non-invazive blood pressure (NIBP) was 110/60 mmHg and pulse rate was 81 beats/minute on admission. Rectal examination revealed acute hematochezia. He was hospitalized and followed in Intensive Care Unit (ICU). Hemoglobin level was measured as 8.4 g/dL but unfortunately dropped gradually to 7.8 g/dL and a total of 4 units of erythrocyte suspension were administered for 24 hours. Colonoscopy was performed immediately, revealing hematoma in the rectum and multiple diverticula in the entire colon but no obvious active bleeding site was observed. Due to rectal bleeding and hemoglobin decline, mesenteric angiography was perfromed and a rupture of an aneurysm of the second left branch (jejunal) of the superior mesenteric artery was detected (Figure 1). Endovascular therapy was performed on the proximal and distal end of the aneurysm with 3×3.3-mm (5 in number) and 4×3.7-mm (1 in number) pushable and 3×8-mm (3 in number) and 4×8-mm (1 in number) detachable coils, respectively (Figure 2). Bleeding ceased and hemoglobin level remained stable after the procedure. On day 6 of hospitalization the patient was discharged without complications.
Figure 1.

Image of an aneurysm in the left branch of the superior mesenteric artery. Yellow arrow shows the aneurysm.
Figure 2.
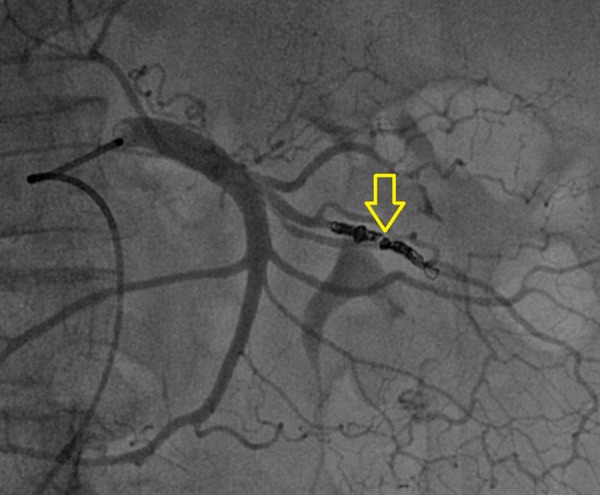
Image of the left branch of the superior mesenteric artery after endovascular coil embolization. Yellow arrow shows an endovascular coil.
Discussion
SMAA is the third most common splanchnic artery aneurysm [1]. The aneurysm of the branches of the superior mesenteric artery is extremely rare. The most common cause of SMAA is considered to be infection while others include: pancreatitis, trauma, atherosclerosis and connective tissue disease. However, the etiology remains unknown. Acute diverticulitis could be the reason of this condition in our patient.
The most common symptom of SMAA is described as abdominal pain. However, it may present itself by gastrointestinal bleeding in case of rupture, a fatal complication. In a series of Stone et al., 38% patients presented with rupture, and the operative mortality for repair was found to be 37.5% [2]. Hirsch et al. found mortality rates reaching up to 38% [3].
Various treatment procedures have been reported for the treatment of SMAA with intestinal ischemia or rupture. Surgery is usually performed, according to the recent studies [4]. Multiple surgical techniques have been described including ligation and bypass with autologous graft, thrombectomy and fixation of an intimal flap. Endovascular therapy shows the advantage in both diagnosis and treatment and is also less invasive than surgery. However, it may fail in complicated or major aneurysms and in case of intestinal ischemia surgery should be preferred. Regarding endovascular treatment for SMAA, most reports have focused on the embolization of SMAA with coils, cyanoacrylate, and thrombin. Recently, several authors have shown the results of stent placement into the true lumen as well as stent graft placement [5]. The small left branch of the superior mesenteric artery was involved in our case, thus we performed endovascular coil embolization for both diagnosis and treatment. The small caliber of the artery made it difficult to use an endovascular-covered stent. For larger branches or for the superior mesenteric artery itself, stenting seems to be a good option. Smaller arteries can be treated by coil embolization to prevent hemorrhage but for larger arteries stenting should be used in order to ensure distal continuity for prevention of ischemia.
Rupture of SMAA may either cause intraabdominal or intraluminal (into the small bowel lumen) hemorrhage. In our case it caused intraluminal hemorrhage. However, Gunduz et al. reported rupture of SMAA causing intraabdominal hematoma, treated by surgical exploration [6]. Therefore, complications of this small aneurysm affect the treatment strategy. Kurdal et al. also reported rupture of the aneurysm of the jejunal branch of the superior mesenteric artery, similar to our case [4]. The second branch of SMA that is likely to be the jejunal branch was involved in our case. Thus, our case was unique regarding the location of the aneurysm. Moreover, our case was treated by coil embolisation whereas other cases by surgical intervention.
Conclusions
In order to prevent mortality and life-threatening complications of SMAA, urgent diagnosis and treatment strategy should be considered. Endovascular therapy is an effective and less invasive option technique for rupture of SMAA. It should be chosen as an alternative treatment to surgery, especially in selected cases with intraluminal hemorrhage. In patients with major intraabdominal hemorrhage surgery remains the only treatment option.
Footnotes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Statement
This study did not receive any specific funding or grants.
References
- 1.Kopatsis A, D’Anna JA, Sithian N, Sabido F. Superior mesenteric artery aneurysm: 45 years later. Am Surg. 1998;64:263–66. [PubMed] [Google Scholar]
- 2.Stone WM, Abbas M, Cherry KJ, et al. Superior mesenteric artery aneurysms: Is presence an indication for intervention? J Vasc Surg. 2002;36:234–37. doi: 10.1067/mva.2002.125027. [DOI] [PubMed] [Google Scholar]
- 3.Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung and Blood Institute; Society for Vascular Nursing; Trans-Atlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47(6):1239–312. doi: 10.1016/j.jacc.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 4.Kurdal AT, Cerrahoglu M, Iskesen I, Sirin H. Superior mesenteric artery branch jejunal artery aneurysm. Interact Cardiovasc Thorac Surg. 2010;11(6):859–61. doi: 10.1510/icvts.2010.243253. [DOI] [PubMed] [Google Scholar]
- 5.Baldi S, Zander T, Rabellino M, Maynar M. Endovascular management of a spontaneous dissecting aneurysm of the superior mesenteric artery: Case report and discussion of treatment options. Ann Vasc Surg. 2009;23:e1–4. doi: 10.1016/j.avsg.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Gunduz Y, Sipahi S, Kara R, Tamer A. A rare cause of intraabdominal hematoma: Rupture of mesenteric artery branch aneurysm. JBR-BTR. 2013;96(6):354–56. doi: 10.5334/jbr-btr.455. [DOI] [PubMed] [Google Scholar]


