Abstract
Purpose
To evaluate the accuracy of the optical coherence tomography–based (OCT formula) and Barrett True K (True K) intraocular lens (IOL) calculation formulas in eyes with previous radial keratotomy (RK).
Methods
In 95 eyes of 65 patients, using the actual refraction following cataract surgery as target refraction, the predicted IOL power for each method was calculated. The IOL prediction error (PE) was obtained by subtracting the predicted IOL power from the implanted IOL power. The arithmetic IOL PE and median refractive PE were calculated and compared.
Results
All formulas except the True K produced hyperopic IOL PEs at 1 month, which decreased at ≥4 months (all P < 0.05). For the double-K Holladay 1, OCT formula, True K, and average of these three formulas (Average), the median absolute refractive PEs were, respectively, 0.78 diopters (D), 0.74 D, 0.60 D, and 0.59 D at 1 month; 0.69 D, 0.77 D, 0.77 D, and 0.61 D at 2 to 3 months; and 0.34 D, 0.65 D, 0.69 D, and 0.46 D at ≥4 months. The Average produced significantly smaller refractive PE than did the double-K Holladay 1 at 1 month (P < 0.05). There were no significant differences in refractive PEs among formulas at 4 months.
Conclusions
The OCT formula and True K were comparable to the double-K Holladay 1 method on the ASCRS (American Society of Cataract and Refractive Surgery) calculator. The Average IOL power on the ASCRS calculator may be considered when selecting the IOL power. Further improvements in the accuracy of IOL power calculation in RK eyes are desirable.
Keywords: optical coherence tomography, cataract surgery, intraocular lens calculation formulas, radial keratotomy
Radial keratotomy (RK) was the most common treatment for myopia in the late 1970s to 1980s.1 The treatment used 4 to 32 radial incisions to flatten the central cornea and correct myopia.1,2 The challenges in intraocular lens (IOL) power calculations in eyes following RK include2–4 (1) difficulties in determining true corneal refractive power due to the anterior and posterior corneal irregularities induced by the RK incisions, (2) inaccurate estimation of the effective lens position,5 and (3) hyperopic shift over time.6–8 Studies have reported accuracy of IOL power calculations in eyes with previous RK, using corneal powers obtained from various corneal topography/tomography, such as Orbscan,9 EyeSys,10 Tomey,11 Atlas,12 and Pentacam.13 Unfortunately, the refractive outcomes after cataract surgery in these RK eyes are still very challenging to predict, and no single method has been reported to be superior to others in determining IOL powers.
The internet-based IOL power calculator at American Society of Cataract and Refractive Surgery (ASCRS) Web site (www.ascrs.org; provided in the public domain by ASCRS) has modules for eyes with prior myopic laser in situ keratomileusis (LASIK) or excimer laser photorefractive keratectomy (PRK), hyperopic LASIK/PRK, or RK. In a recent major update (2015 updates, version 4.7), two newer IOL power calculation formulas have been added to the calculator: the optical coherence tomography (OCT)–based IOL power formula (OCT formula) and the Barrett True K formula (True K). The OCT formula, proposed by Tang and colleagues,14 uses data from the RTVue (Optovue, Inc., Fremont, CA, USA). For this formula, the OCT is used to measure anterior and posterior corneal power within the central 3 mm. Barrett15,16 proposed a universal theoretical formula more than 20 years ago, and the True K formula was developed for eyes with previous corneal refractive surgery and was derived from the Barrett Universal II formula, which is a modified version of the original universal theoretical formula.
Promising results using the OCT formula, True K formula, and the ASCRS calculator have been reported in eyes with previous myopic LASIK/PRK.14,17–21 In this study, using data from two study centers, we evaluated the accuracy of the IOL power calculation methods on the ASCRS postrefractive calculator in eyes with previous RK.
Patients and Methods
Patients
Institutional Review Board (IRB) approval was obtained for this study, and the study adhered to the tenets of the Declaration of Helsinki. This study was conducted at two academic eye centers (Cullen Eye Institute and Casey Eye Institute). Retrospectively, for the dates September 2010 to October 2015, we reviewed consecutive cases of cataract surgery in eyes that had previously undergone RK. Inclusion criteria were eyes that (1) had OCT scans using the RTVue device, (2) had no complications during or after the cataract surgery, and (3) had manifest refraction performed at 3 weeks or later after the cataract surgery with best spectacle-corrected visual acuity of 20/40 or better.
Ocular biometry was measured by using partial coherence interferometry (IOLMaster, V.5.4 and V.7.5; Carl Zeiss Meditec, Inc., Dublin, CA, USA). Optical coherence tomography scans were obtained with the RTVue (version No. 6, 2, 0, 68 to 6, 8, 0, 27). At one center (Baylor College of Medicine), in some cases, corneal curvatures were also measured with the Atlas corneal topography system (Zeiss). All cataract surgeries were performed by one surgeon at the Cullen Eye Institute (DDK) and by six surgeons at the Casey Eye Institute, using a temporal clear corneal incision (except in eyes with 16 or more cuts where limbal incisions were used), phacoemulsification, and implantation of IOLs in the capsular bag. Before the cataract surgery, various methods were used for corneal power estimation and IOL power calculation. The surgeon selected the IOL power to be implanted depending on his judgment. Implanted IOLs included the Alcon lenses (SN60WF and SN6ATT, n = 41; Fort Worth, TX, USA) and the Abbott Medical Optics lenses (ZCB00, ZA9003, and ZCT toric series, n = 54; Santa Ana, CA, USA).
Intraocular Lens Power Calculation Methods
The postrefractive IOL calculator at the ASCRS Web site was used for IOL power calculation (version 4.7). Depending on the data availability, the following methods were evaluated (ordered as they appear at the ASCRS RK calculator).
Double-K Holladay 1 Based on IOLMaster/Atlas Data.
With the ASCRS calculator, the double-K Holladay 1 formula uses a corneal power of 43.86 diopters (D) to calculate the effective lens position, and the corneal power measured before the cataract surgery for IOL power calculation. In this study, we evaluated the double-K Holladay 1 with corneal power values from two devices: (1) the mean corneal power from the IOLMaster (DK-Holladay–IOLM)—on the calculator, result using this method is listed as IOLMaster; and (2) the 4-mm zone corneal power from the Atlas (DK-Holladay–Atlas)—on the calculator, this value was entered as Average Central Power at the Topographic/OCT data section, and result using this method is listed as Average Central Power.
Optical Coherence Tomography Formula.
The OCT formula for RK eyes was derived with an earlier data set and is a modification of the OCT formula for eyes with previous myopic LASIK/PRK described in the study by Huang and colleagues.17 This method uses the anterior corneal power, posterior corneal power, and central corneal thickness obtained from the RTVue, and axial length (AL) and anterior chamber depth (ACD, defined as the distance from the corneal epithelium to the crystalline lens) obtained from the IOLMaster. The effective lens position was predicted by using a regression-derived formula based on ACD constant, AL of the eye, and a fixed posterior corneal power of −5.65 D, which was the mean posterior corneal power in a group of normal eyes with the OCT (data not published). For IOL power calculation, the net corneal power was converted to an effective corneal power based on linear regression analysis, and an eye model consisting of three optical surfaces (cornea, IOL, and retina) was used to calculate the OCT IOL power.17 The detailed formulas have been described by Huang and colleagues.17 Briefly, both the cornea and the IOL were modeled as thin lenses. Light traveled through the first three surfaces and was focused on the retina.
True K Formula.
The True K formula for RK eyes was developed recently. The Universal II formula, a modified version of original universal theoretical formula,15,16 was used to calculate the IOL power. This formula uses corneal power, AL, and ACD values obtained from the IOLMaster. Details regarding the design of the True K and Universal II formulas are not published.
Method Using Average IOL Power.
We also evaluated the method of averaging IOL powers predicted by using various formulas (Average), which is displayed as Average IOL Power on the ASCRS RK calculator, and compared its performance to each single formula. For this study, the Average value was calculated from three formulas in the whole group (DK-Holladay–IOLM, OCT formula, and True K) and four formulas in the subgroup (DK-Holladay–Atlas, DK-Holladay–IOLM, OCT formula, and True K).
Data Analyses
IOL Prediction Error.
Using the optimized lens constant in normal eyes for each surgeon and targeting at the actual refraction following cataract surgery, the predicted IOL power for each formula was calculated. The IOL prediction error (PE) was then obtained by subtracting the IOL power indicated by each formula from the implanted IOL. A positive IOL PE indicates that the calculation method predicts an IOL of lower power than the power of the implanted IOL, which would leave the patient hyperopic. The mean arithmetic IOL PEs were calculated.
Refractive Prediction Error.
Using the assumption that 1 D of IOL PE produces 0.7 D of refractive error at spectacle plane,22 with each formula for each eye, the refractive PE was calculated from the IOL PE. In this study, we calculated the absolute refractive PE both with and without adjusting the mean PE to zero. The median absolute refractive PEs were calculated. The percentage of eyes within refractive PE of ±0.50 D, ±1.00 D, ±1.50 D, and ±2.00 D were computed for each method.
Analyses in Subgroups.
Owing to refraction changes following cataract surgery in RK eyes, the IOL PE and refractive PE were calculated in eyes at 1 month visits (postoperative 3 to 6 weeks), 2 to 3 months (postoperative 7 weeks to 3½ months), and ≥4 months postoperatively (postoperative 3½ months to 1 year). We performed analyses in the whole group and the subgroup in eyes with Atlas data:
Comparison of methods in the whole group: Results using four methods were compared: DK-Holladay–IOLM, OCT formula, True K, and Average of these three formulas; and
Comparison of methods in the subgroup: In eyes with Atlas corneal topography measurements, results using five methods were compared: DK-Holladay–Atlas, DK-Holladay–IOLM, OCT formula, True K, and Average of these four methods.
Statistical Analysis.
Depending on the data distribution, one sample t-test or Wilcoxon one-sample signed rank test was used to assess if the mean arithmetic IOL PEs produced by various methods were significantly different from zero. A nonparametric method, Wilcoxon test, was performed to compare the absolute refractive PEs using different formulas. The McNemar test was used to compare percentages of eyes ±0.5 D, ±1.0 D, ±1.5 D, and ±2.0 D of refractive PEs. Bonferroni correction was applied to adjust for multiple comparisons. The Bonferroni correction is a multiple-comparison correction used when several dependent or independent statistical tests are being performed simultaneously, in order to avoid spurious positives. The SPSS 22.0 for Windows (SPSS, Inc., Chicago, IL, USA) was used for statistical analysis, and P < 0.05 was considered statistically significant. For sample size, we wished to detect a difference of one-half of the standard deviation of differences between two formulas. With a significance level of 5% and a test power of 80%, 32 eyes were required in each group.
Results
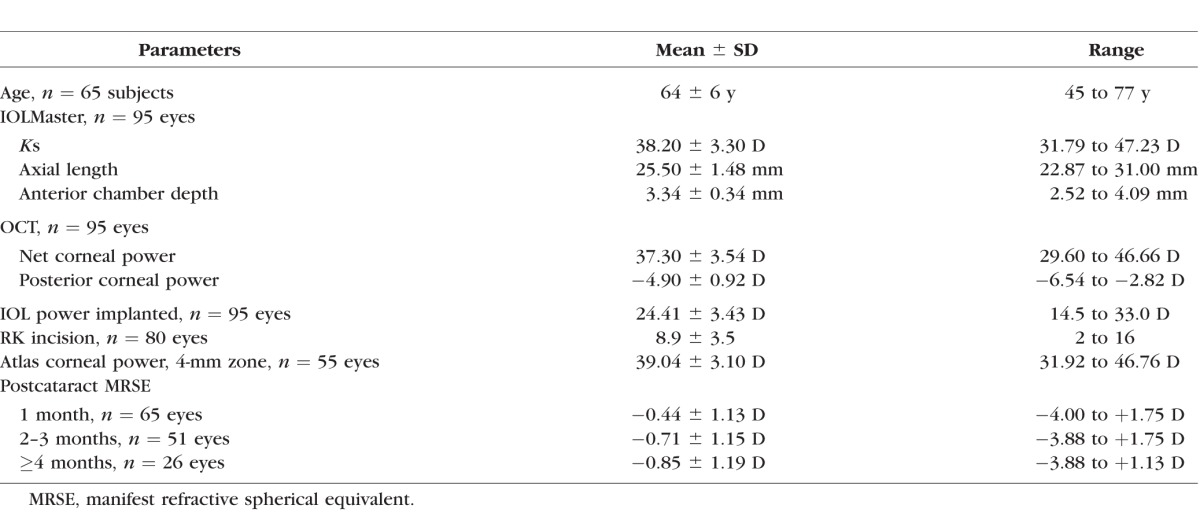
Table 1 lists patients' demographic data. A total of 95 eyes of 65 patients were included.
Table 1.
Demographic Summary of 95 Eyes of 65 Patients
Comparison of Methods in the Whole Group
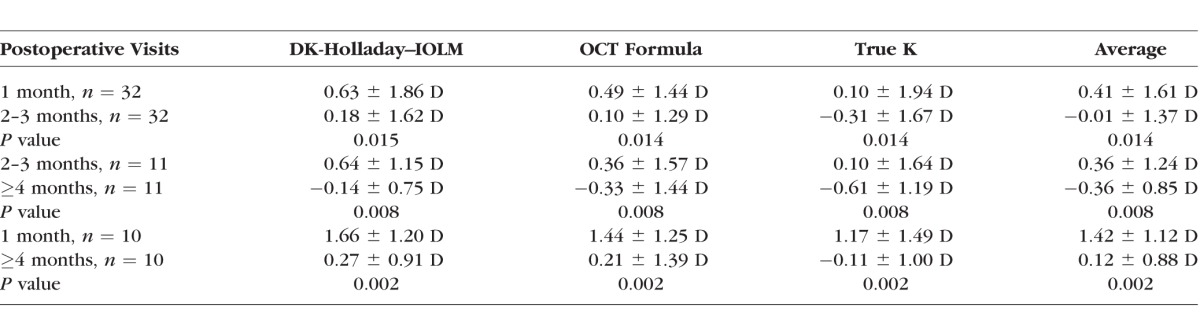
The mean IOL PEs ranged from −0.15 to 0.54 D at postoperative 1 month, −0.35 to 0.13 D at 1 to 2 months, and −0.77 to −0.46 D at ≥4 months, respectively (Table 2). The DK-Holladay–IOLM and OCT formula produced hyperopic IOL PEs at 1 month, and the True K produced a myopic IOL PE at ≥4 months (all P < 0.05). The True K formula had more myopic IOL PEs than did the DK-Holladay–IOLM, OCT formula, and Average at all visits (all P < 0.05). The IOL PEs for all formulas shifted in a myopic direction at each subsequent visit after the surgery (all P < 0.05) (Table 3).
Table 2.
Mean Arithmetic IOL Prediction Error (Implanted IOL Power − Predicted IOL Power) (Mean ± Standard Deviation, Range)
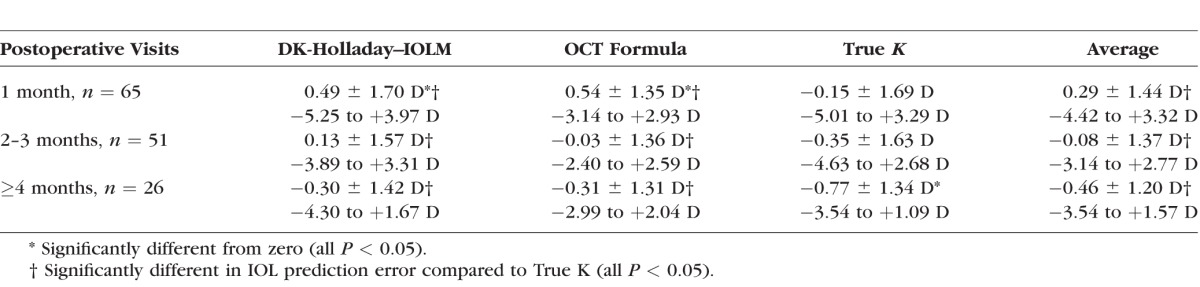
Table 3.
Mean Arithmetic IOL Prediction Error (Implanted IOL Power − Predicted IOL Power) (Mean ± Standard Deviation) Over Time
Median absolute refractive PEs without adjusting the mean refractive PEs to zero ranged from 0.59 to 0.78 D at 1 month, 0.61 to 0.77 D at 2 to 3 months, and 0.34 to 0.69 D at ≥4 months (Table 4). The Average IOL power produced a significantly smaller mean absolute refractive PE than did the DK-Holladay–IOLM at 1 month (P < 0.05). There were no significant differences among other formulas.
Table 4.
Median Absolute Refractive Prediction Error (SD) and Percentage of Eyes Within 0.5 D, 1.0 D, 1.5 D, and 2.0 D of Refractive Prediction Error by Assuming That 1 D of IOL Prediction Error Produces 0.7 D of Refractive Error at the Spectacle Plane
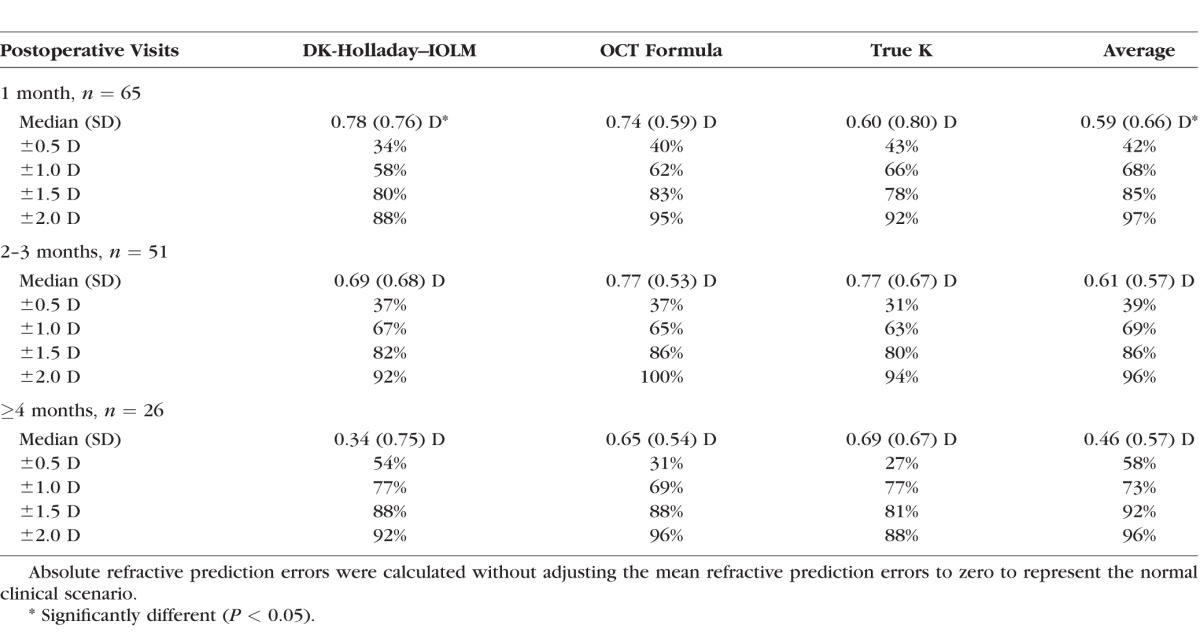
The percentages of eyes within ±0.5 D and ±1.0 D of refractive PE ranged from 34% to 43% and 58% to 68% at 1 month, 31% to 39% and 63% to 69% at 2 to 3 months, and 27% to 54% and 69% to 77% at ≥4 months, respectively. There were no significant differences among formulas.
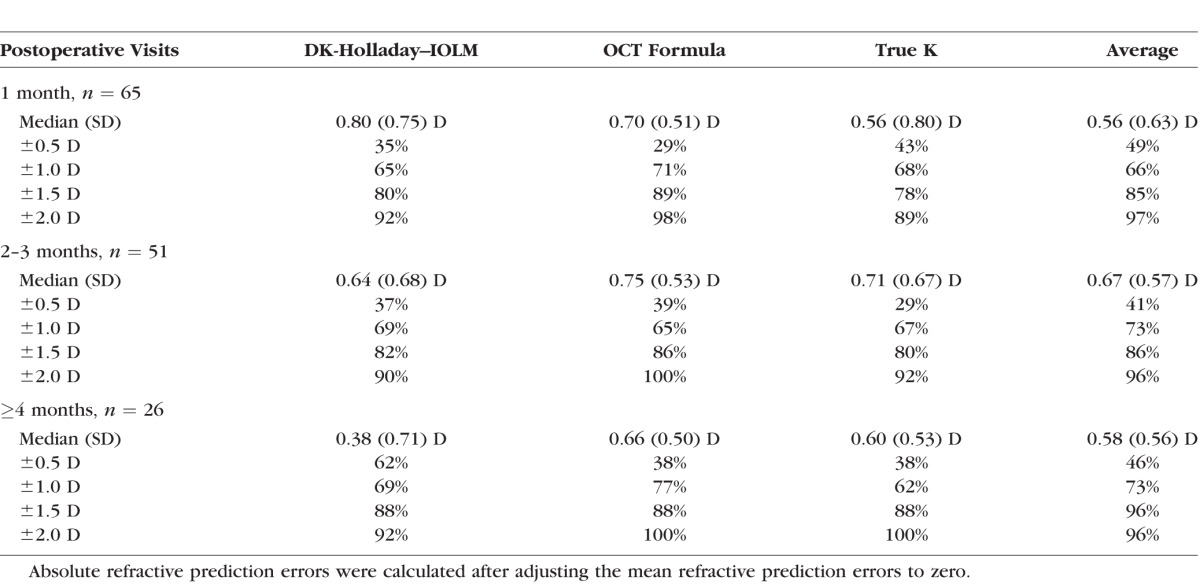
Median absolute refractive PEs after adjusting the mean refractive PEs to zero ranged from 0.56 to 0.80 D at 1 month, 0.64 to 0.75 D at 2 to 3 months, and 0.38 to 0.66 D at ≥4 months (Table 5). The percentages of eyes within ±0.5 D and ±1.0 D of refractive error ranged from 29% to 49% and 65% to 71% at 1 month, 29% to 41% and 65% to 73% at 2 to 3 months, and 38% to 62% and 62% to 77% at ≥4 months, respectively. There were no significant differences among these formulas.
Table 5.
Median Absolute Refractive Prediction Error (SD) and Percentage of Eyes Within 0.5 D, 1.0 D, 1.5 D, and 2.0 D of Refractive Prediction Error by Assuming That 1 D of IOL Prediction Error Produces 0.7 D of Refractive Error at the Spectacle Plane
Comparison of Methods in the Subgroup
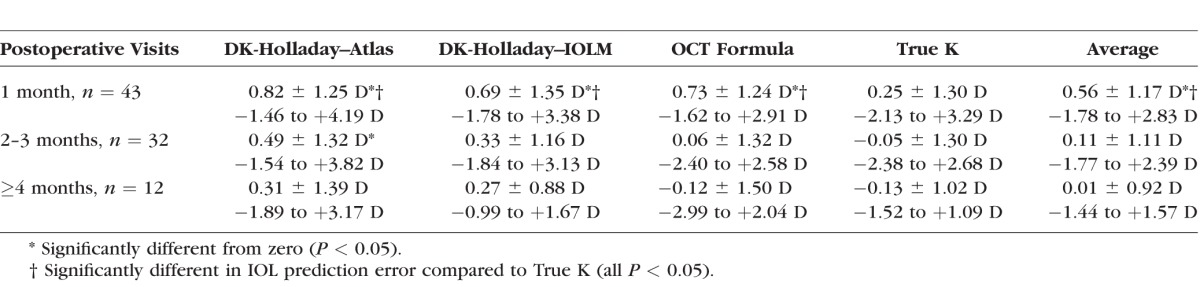
All formulas except the True K produced hyperopic IOL PEs at 1 month, and the DK-Holladay–Atlas had hyperopic IOL PEs at 2 to 3 months (all P < 0.05) (Table 6). The True K formula had significant smaller IOL PEs than did all other formulas at 1 month (all P < 0.05). There were no significant differences among other formulas.
Table 6.
Mean Arithmetic IOL Prediction Error (Implanted IOL Power − Predicted IOL Power) (Mean ± Standard Deviation, Range) in Eyes With Atlas Topography Measurements
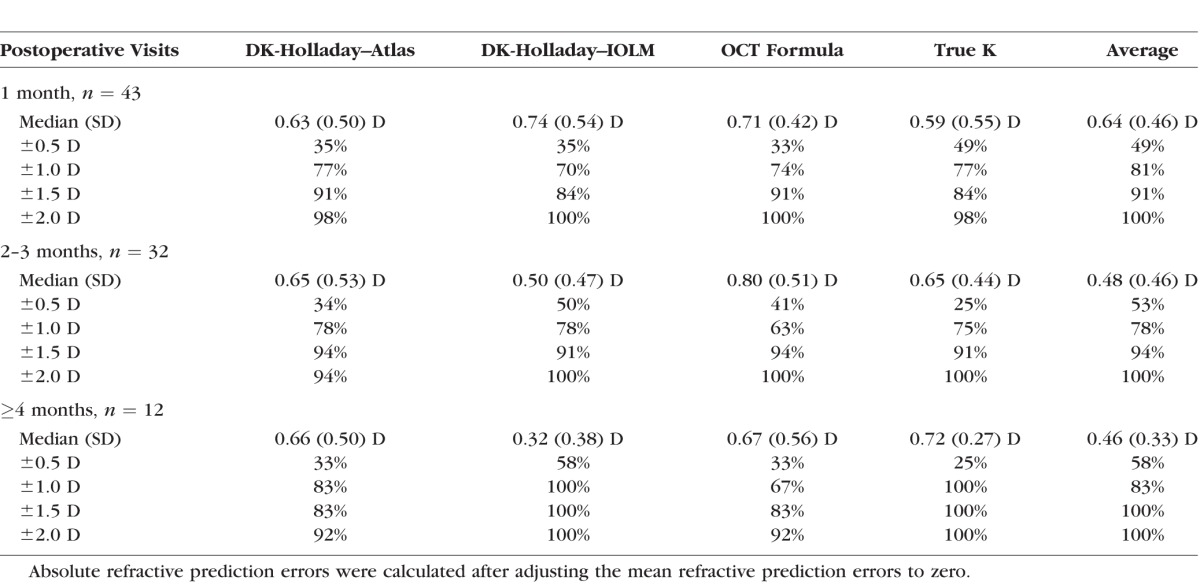
Median absolute refractive PEs without adjusting the mean refractive PEs to zero ranged from 0.53 to 0.82 D at 1 month, 0.51 to 0.76 D at 2 to 3 months, and 0.22 to 0.65 D at ≥4 months (Table 7). Median absolute refractive PEs after adjusting the mean refractive PEs to zero ranged from 0.59 to 0.74 D at 1 month, 0.48 to 0.80 D at 2 to 3 months, and 0.32 to 0.72 D at ≥4 months (Table 8). There were no significant differences among formulas in median absolute refractive PEs and in the percentages of eyes within ±0.5 D, ±1.0 D, ±1.5 D, and ±2.0 D of refractive PE.
Table 7.
Median Absolute Refractive Prediction Error and Percentage of Eyes Within 0.5 D, 1.0 D, 1.5 D, and 2.0 D of Refractive Prediction Error by Assuming That 1 D of IOL Prediction Error Produces 0.7 D of Refractive Error at the Spectacle Plane in Eyes With Atlas Topography Measurements
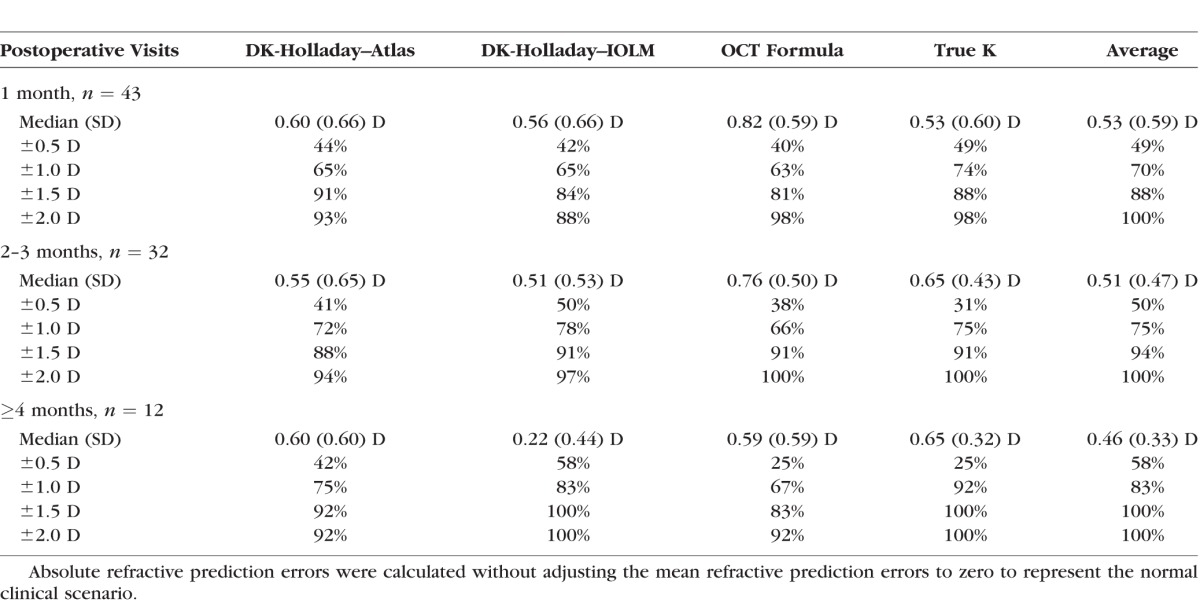
Table 8.
Median Absolute Refractive Prediction Error and Percentage of Eyes Within 0.5 D, 1.0 D, 1.5 D, and 2.0 D of Refractive Prediction Error by Assuming That 1 D of IOL Prediction Error Produces 0.7 D of Refractive Error at the Spectacle Plane in Eyes With Atlas Topography Measurements
Discussion
In this study, we reported the first published outcomes of the OCT formula and the True K formula in eyes with previous RK and compared their performance to those on the ASCRS calculator.
Our results showed that all formulas except the True K produced hyperopic IOL PEs at 1 month, which decreased over time. The Average IOL power had significantly smaller absolute refractive PE than did the DK-Holladay–IOLM at 1 month. In a subgroup, we also compared the IOL power calculation, using the Atlas corneal topographic data to other formulas. Again, hyperopic IOL PEs were found at 1 month for all formulas except the True K. There were no significant differences in absolute refractive PEs. The percentages of eyes within ±0.5 D, ±1.0 D, ±1.5 D, and ±2.0 D of refractive PEs among formulas were not significantly different in both the whole group and the subgroup.
Koch et al.4 have reported that, following cataract surgery, RK eyes experience an initial hyperopic shift caused by an early postoperative corneal flattening of greater than or equal to 1 D, which partially regresses. In this study, we separated all cases into subgroups with postoperative follow-up at 1 month, 2 to 3 months, and ≥4 months. At 1 month postoperatively, all formulas except the True K produced hyperopic IOL PEs. As anticipated, compared to IOL PEs at 1 month, IOL PEs shifted in a more myopic direction with all formulas over time. The RK incisions swell during cataract surgery, and the swelling can induce central corneal flattening, which results in excessive hyperopia immediately postoperatively.4 As the swelling subsides over time, refraction may shift to less hyperopic or more myopic. These RK patients may experience fluctuations in their refractive state for many weeks after the cataract surgery.
DeMill and colleagues12 have evaluated the ASCRS calculator for eyes with previous RK. Two formulas on the calculator were assessed: the average central power, using the equivalent keratometry reading at a 4.5-mm optical zone obtained from the Pentacam and the Atlas 1-4 mm. In 15 eyes with postcataract refraction at an average of 4.33 ± 3.70 months, the authors report that, with the Atlas 1-4 mm, the mean IOL PE is 1.07 D, and the percentages of eyes within 0.5 D and 1.0 D of refractive PEs are 0.0% and 46.67%, respectively. In our study, with the Atlas 4-mm zone (DK-Holladay–Atlas), we found slightly smaller (or less hyperopic) IOL PEs, and the percentages of eyes within ±0.5 D and ±1.0 D of refractive PEs ranged from 41% to 44% and 65% to 75%, respectively. In 10 eyes, Canto et al.23 report that the ASCRS calculator, using the IOLMaster data, produces 14% and 43% of eyes within ±0.5 D and ±1.0 D of IOL PE. In our study, the IOLMaster, using the ASCRS calculator, had 25% to 54% and 49% to 62% of eyes within ±0.5 D and ±1.0 D of IOL PEs at different visits.
In this study, we calculated the absolute refractive PEs with and without adjusting the mean IOL PEs to zero. Results after adjusting the mean IOL PE to zero eliminate the bias of the lens factor chosen. In contrast, data without adjusting the mean IOL PE to zero represent the normal clinical scenario, since surgeons routinely use their lens constants in normal cataract patients and do not have specific optimized lens constants for post-RK eyes. Our results showed similar median absolute refractive PEs with and without adjusting the mean IOL PE to zero.
The RK eyes and eyes with previous LASIK/PRK have some similarities in respect to the difficulty in determining the true corneal refractive power. However, it is more difficult for accurate IOL power calculations in RK eyes than those in LASIK/PRK eyes, owing to more marked anterior and posterior corneal irregularities induced by the RK incisions and the greater flattening that can occur, with some corneas 30 D or less. Additional challenges with RK eyes are that some experience diurnal fluctuation, hyperopic shift over time, or both.
A recent study19 nicely demonstrates the differences in outcomes between RK eyes and LASIK/PRK eyes. In that study, we compare the OCT formula, the True K formula, and the methods on the ASCRS calculator in eyes with previous myopic LASIK/PRK. The median absolute refractive PEs are 0.35 D, 0.42 D, and 0.35 D for the OCT formula, the True K formula, and the average of formulas on the ASCRS calculator, respectively; 58.7% to 68.3% of eyes are within 0.5 D of refractive PEs, and 90.4% to 94.2% of eyes are within 1.0 D of refractive PEs. In contrast, for the RK eyes in our current study, results were much poorer. We found that the median absolute refractive PEs were 0.65 to 0.77 D, 0.60 to 0.77 D, and 0.46 to 0.61 D for the OCT formula, the True K formula, and the average of formulas on the ASCRS calculator, respectively; and only 27% to 58% of eyes were within 0.5 D of refractive PEs and 62% to 77% of eyes within 1.0 D of refractive PEs.
There were some limitations in this study. (1) Although standard cataract surgery procedures were used by these surgeons, certainly some differences existed. Different IOL platforms were used, which might induce variation of effective lens position. (2) Both eyes of some subjects were included. Subgroup analysis with each eye from each subject showed similar results as in the whole group (data not shown); therefore, we included all consecutive cases that met the inclusion criteria of this study. (3) Owing to lack of access to other devices, we could not evaluate methods using other devices on the calculator. (4) The refractive prediction errors were calculated by assuming that 1 D of IOL PE produces 0.7 D of refractive PE at spectacle plane.22 Calculating IOL power PEs using the ASCRS calculator is a readily reproducible method for evaluating calculation errors using various formulas on the calculator in eyes with previous corneal refractive surgery. This method has been used by other authors who have evaluated outcomes with the ASCRS calculator.12,19,23–25 Additionally, the IOL power PEs provide direct information for surgeons when they select IOL powers.
In summary, our results demonstrated that all formulas except the True K produced hyperopic IOL PEs at 1 month, which decreased over time. The OCT formula and the True K formula were comparable to the double-K Holladay 1 formula with IOLMaster and Atlas corneal powers. The Average IOL power tended to produce smaller refractive PEs. Further studies with larger samples and longer follow-up are desirable. Overall, the data remain disappointing, as no formula was able to predict 80% of eyes within 1 D of target refraction at >4 months postoperatively. Clearly, improvements in the accuracy of corneal power measurements and IOL power calculations in RK eyes are required.
Acknowledgments
Supported by the AED OCT National Institutes of Health Grant R01 EY018184 and in part by an unrestricted grant from Research to Prevent Blindness, New York, New York, United States.
Disclosure: J.X. Ma, None; M. Tang, Optovue, Inc. (F); L. Wang, None; M.P. Weikert, None; D. Huang, Optovue, Inc. (F); D.D. Koch, Alcon (C), Albott Medical Optics (C), Revision Optics (C)
References
- 1. Cowden JW. Radial keratotomy—a retrospective study of cases observed at the Kresge Eye Institute for six months. Arch Ophthalmol. 1982; 100: 578–580. [DOI] [PubMed] [Google Scholar]
- 2. Kwitko S,, Gritz DC,, Garbus JJ,, Gauderman WJ,, McDonnell PJ. Diurnal variation of corneal topography after radial keratotomy. Arch Ophthalmol. 1992; 110: 351–356. [DOI] [PubMed] [Google Scholar]
- 3. Garana RM,, Petroll WM,, Chen WT,, et al. Radial keratotomy, II: role of the myofibroblast in corneal wound contraction. Invest Ophthalmol Vis Sci. 1992; 33: 3271–3282. [PubMed] [Google Scholar]
- 4. Koch DD,, Liu JF,, Hyde LL,, Rock RL,, Emery JM. Refractive complications of cataract surgery after radial keratotomy. Am J Ophthalmol. 1989; 108: 676–682. [DOI] [PubMed] [Google Scholar]
- 5. Aramberri J. IOL power calculation after corneal refractive surgery: the double-K method. J Cataract Refract Surg. 2003; 29: 2063–2068. [DOI] [PubMed] [Google Scholar]
- 6. Chhadva P,, Cabot F,, Galor A,, Yoo SH. Long-term outcomes of radial keratotomy, laser in situ keratomileusis, and astigmatic keratotomy performed consecutively over a period of 21 years. Case Rep Ophthalmol Med. 2015; 2015: 592495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chavez S,, Celikkol L,, Feldman ST. Hyperopic shift and myopic regression in a patient 7 years after bilateral refractive keratotomy. J Refract Surg. 1996; 12: 160–162. [DOI] [PubMed] [Google Scholar]
- 8. Waring GO,, III, Lynn MJ,, McDonnell PJ. Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery. Arch Ophthalmol. 1994; 112: 1298–1308. [DOI] [PubMed] [Google Scholar]
- 9. Arce CG,, Soriano ES,, Weisenthal RW,, et al. Calculation of intraocular lens power using Orbscan II quantitative area topography after corneal refractive surgery. J Refract Surg. 2009; 25: 1061–1074. [DOI] [PubMed] [Google Scholar]
- 10. Bardocci A,, Lofoco G. Corneal topography and postoperative refraction after cataract phacoemulsification following radial keratotomy. Ophthalmic Surg Lasers. 1999; 30: 155–159. [PubMed] [Google Scholar]
- 11. Awwad ST,, Dwarakanathan S,, Bowman RW,, et al. Intraocular lens power calculation after radial keratotomy: estimating the refractive corneal power. J Cataract Refract Surg. 2007; 33: 1045–1050. [DOI] [PubMed] [Google Scholar]
- 12. Demill DL,, Hsu M,, Moshirfar M. Evaluation of the American Society of Cataract and Refractive Surgery intraocular lens calculator for eyes with prior radial keratotomy. Clin Ophthalmol. 2011; 5: 1243–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Potvin R,, Hill W. New algorithm for post-radial keratotomy intraocular lens power calculations based on rotating Scheimpflug camera data. J Cataract Refract Surg. 2013; 39: 358–365. [DOI] [PubMed] [Google Scholar]
- 14. Tang M,, Li Y,, Huang D. An intraocular lens power calculation formula based on optical coherence tomography: a pilot study. J Refract Surg. 2010; 26: 430–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barrett GD. An improved universal theoretical formula for intraocular lens power prediction. J Cataract Refract Surg. 1993; 19: 713–720. [DOI] [PubMed] [Google Scholar]
- 16. Barrett GD. Intraocular lens calculation formulas for new intraocular lens implants. J Cataract Refract Surg. 1987; 13: 389–396. [DOI] [PubMed] [Google Scholar]
- 17. Huang D,, Tang M,, Wang L,, et al. Optical coherence tomography-based corneal power measurement and intraocular lens power calculation following laser vision correction (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2013. ; 111: 34–45. [PMC free article] [PubMed] [Google Scholar]
- 18. Tang M,, Wang L,, Koch D,, Li Y,, Huang D. Intraocular lens power calculation after previous myopic laser vision correction based on corneal power measured by Fourier-domain optical coherence tomography. J Cataract Refract Surg. 2012. ; 38: 589–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang L,, Tang M,, Huang D,, Weikert MP,, Koch DD. Comparison of newer IOL power calculation methods for post-corneal refractive surgery eyes. Ophthalmology. 2015; 122: 2443–2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fram NR,, Masket S,, Wang L. Comparison of intraoperative aberrometry OCT-based IOL formula, Haigis-L, and Masket formulae for IOL power calculation after laser vision correction. Ophthalmology. 2015; 122: 1096–1101. [DOI] [PubMed] [Google Scholar]
- 21. Abulafia A,, Hill WE,, Koch DD,, Wang L,, Barrett GD. Accuracy of the Barrett True-K formula for intraocular lens power prediction after LASIK/PRK to correct myopia. J Cataract Refract Surg. In press. [DOI] [PubMed]
- 22. Feiz V,, Mannis MJ,, Garcia-Ferrer F,, et al. Intraocular lens power calculation after laser in situ keratomileusis for myopia and hyperopia: a standardized approach. Cornea. 2001; 20: 792–797. [DOI] [PubMed] [Google Scholar]
- 23. Canto AP,, Chhadva P,, Cabot F,, et al. Comparison of IOL power calculation methods and intraoperative wavefront aberrometer in eyes after refractive surgery. J Refract Surg. 2013; 29: 484–489. [DOI] [PubMed] [Google Scholar]
- 24. Wang L,, Hill WE,, Koch DD. Evaluation of IOL power prediction methods using the ASCRS post-keratorefractive IOL power calculator. J Cataract Refract Surg. 2010; 36: 1466–1473. [DOI] [PubMed] [Google Scholar]
- 25. Yang R,, Yeh A,, George MR,, Rahman M,, Boerman H,, Wang M. Comparison of intraocular lens power calculation methods after myopic laser refractive surgery without previous refractive surgery data. J Cataract Refract Surg. 2013; 39: 1327–1335. [DOI] [PubMed] [Google Scholar]


