Abstract
Objective
The number of older adults with cancer is increasing. Given the limited amount of research and the inconsistent findings regarding age differences in common physical symptoms associated with cancer and its treatments, the purposes of this study, in a sample of oncology outpatients receiving chemotherapy (CTX), were to evaluate for age differences in demographic and clinical characteristics, as well as in occurrence rates of and severity ratings for fatigue, decrements in energy, and sleep disturbance. In addition, using regression analysis techniques, within and across age groups, demographic and clinical characteristics associated with the severity of each symptom were evaluated.
Methods
Patients (n=1343) were dichotomized into younger (<65 years) and older (≥65 years) age groups. Patients completed self-report questionnaires prior to their next dose of CTX.
Results
Overall, our findings suggest that compared to younger patients, older adults experience a lower or similar level of fatigue, decrements in energy, and sleep disturbance. However, it should be noted that both age groups experienced high occurrence rates and moderate to severe levels of all three symptoms.
Conclusions
Clinicians need to assess all oncology patients receiving CTX for these three symptoms. Future research needs to determine the biopsychosocial reasons that underlie these age-related differences in fatigue, decrements in energy, and sleep disturbance.
Keywords: age differences, older adults, elderly, cancer, chemotherapy, fatigue, energy, sleep disturbance, occurrence, severity, diurnal variations
INTRODUCTION
While the number of older adults diagnosed with cancer is expected to increase by 67% between 2010 and 2030 (Smith, Smith, Hurria, Hortobagyi, & Buchholz, 2009), little is known about the symptom experience of these patients. Fatigue, decrements in energy, and sleep disturbance are three of the most common physical symptoms associated with cancer and its treatment (Gilbertson-White, Aouizerat, Jahan, & Miaskowski, 2011). However, very few studies have evaluated for age differences in the occurrence and severity of these three symptoms as well as for demographic and clinical characteristics associated with a higher symptom burden.
Approximately 80% of patients who receive chemotherapy (CTX) report fatigue during treatment (Berger, et al., 2010; Ratcliff, Lam, Arun, Valero, & Cohen, 2014). In a recent review of six studies that compared the relative effectiveness of CTX for stage III colon cancer (Hung & Mullins, 2013), older patients had higher fatigue occurrence rates than younger patients. In terms of severity, in one large, cross-sectional study (Butt, et al., 2010), increasing age was associated with higher fatigue severity scores. In contrast in two studies that used the Memorial Symptom Assessment Scale (MSAS) to assess the occurrence and severity of fatigue (Cataldo, et al., 2013; Oksholm, et al., 2013), no differences were found in the occurrence rates for fatigue between younger and older patients. In both of these studies, no age-related differences in fatigue severity scores were reported.
In oncology patients, fatigue is defined as a distressing, persistent sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or its treatment that is not proportional to recent activities and interferes with usual functioning (Berger, et al., 2015). In contrast, energy can be defined as an individual's potential to perform physical and mental activity (Lerdal, 2002). Of note, a growing body of phenotypic and molecular evidence from our research team (Aouizerat, et al., 2015) and others (Lerdal, 2002) suggests that energy is a distinct symptom from fatigue. Because an evaluation of decrements in energy is a relatively new concept in symptom management research, no studies were found that evaluated for age differences in energy levels in oncology patient receiving CTX.
Sleep disturbance occurs in approximately 35% of cancer patients, which is about double the prevalence rate in the general population (Berger, 2009). While studies in the general population suggest that older adults experience higher levels of insomnia (Ohayon, Zulley, Guilleminault, Smirne, & Priest, 2001; Rosekind, 1992), in two studies that evaluated for age differences in the occurrence and severity of sleep disturbance in oncology outpatients (Cataldo, et al., 2013; Oksholm, et al., 2013), no differences were found. In contrast, in one study of patients with hepatocellular cancer (Chu, Yu, Chen, Peng, & Wu, 2011), older age was associated with higher occurrence rates for sleep disturbance.
Given the limited amount of research and the inconsistent findings regarding age differences in common physical symptoms associated with cancer and its treatments, the purposes of this study, in a sample of oncology outpatients receiving CTX (n = 1343), were to evaluate for age differences (i.e., < 65 years old versus ≥ 65 years old) in demographic and clinical characteristics, as well as in occurrence rates of and severity ratings for fatigue, decrements in energy, and sleep disturbance. In addition, after controlling for potential confounding characteristics, differences between the age groups in symptom severity scores were evaluated. Finally, within each age group, demographic and clinical characteristics associated with the severity of each symptom were evaluated.
PATIENTS AND METHODS
Patients and Settings
This study is part of a larger, longitudinal study of the symptom experience of oncology outpatients receiving CTX. Eligible patients were ≥18 years of age; had a diagnosis of breast, gastrointestinal (GI), gynecological (GYN), or lung cancer; had received CTX within the preceding four weeks; were scheduled to receive at least two additional cycles of CTX; were able to read, write, and understand English; and gave written informed consent. Patients were recruited from two Comprehensive Cancer Centers, one Veteran's Affairs hospital, and four community-based oncology programs. A convenience sample of 2235 patients were approached and 1343 consented to participate (60.1% response rate). The major reason for refusal was being overwhelmed with their cancer treatment.
Instruments
Demographic questionnaire obtained information on age, gender, ethnicity, marital status, living arrangements, education, employment status, and income. Alcohol use was evaluated using the Alcohol Use Disorders Identification Test (AUDIT) (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). Functional status was evaluated using the Karnofsky Performance Status (KPS) scale (Karnofsky, 1977; Karnofsky, Abelmann, Craver, & Burchenal, 1948). The Self-Administered Comorbidity Questionnaire (SCQ) was used to evaluate the comorbidity associated with 13 common medical conditions (Sangha, Stucki, Liang, Fossel, & Katz, 2003).
Lee Fatigue Scale (LFS) consists of 18 items that assesses physical fatigue and energy (Lee, Hicks, & Nino-Murcia, 1991). Each item was rated on a 0 to 10 numeric rating scale (NRS). Total fatigue and energy scores were calculated as the mean of the 13 fatigue items and the 5 energy items, with higher scores indicating greater fatigue severity and higher levels of energy. Patients were asked to rate each item based on how they felt “right now,” within 30 minutes of awakening (i.e., morning fatigue, morning energy) and prior to going to bed (i.e., evening fatigue, evening energy). Cutoff scores of ≥3.2 and ≥5.6 indicate high levels of morning and evening fatigue, respectively. Cutoff scores of ≤6.0 and ≤3.5 indicate low levels of morning and evening energy, respectively (Fletcher, et al., 2008). LFS has well established validity and reliability (Gay, Lee, & Lee, 2004; Lee, et al., 1991; Lee, Portillo, & Miramontes, 1999; Miaskowski, et al., 2006; Miaskowski & Lee, 1999; Miaskowski, et al., 2008). In this study, Cronbach's alphas for evening and morning fatigue were 0.95 and 0.96, respectively. Cronbach's alphas for evening and morning energy were 0.93 and 0.95, respectively.
General Sleep Disturbance Scale (GSDS) consists of 21 items that assesses the quality of sleep in the past week. Each item was rated on a 0 (never) to 7 (everyday) NRS. GSDS total score is the sum of the seven subscale scores that can range from 0 (no disturbance) to 147 (extreme sleep disturbance). Each mean subscale score can range from 0 to 7. Higher subscale and total scores indicate higher levels of sleep disturbance. Subscale scores of ≥3 and a GSDS total score of ≥43 indicate a significant level of sleep disturbance (Fletcher, et al., 2008). GSDS has well-established validity and reliability (Lee, 1992; Lee & DeJoseph, 1992; Miaskowski & Lee, 1999). In the current study, the Cronbach's alpha for the GSDS total score was 0.83.
Study Procedures
The study was approved by the Committee on Human Research at the University of California, San Francisco and by the Institutional Review Board at each of the study sites. Written informed consent was obtained from all patients. Depending on the length of their CTX cycles, patients completed questionnaires in their homes, a total of six times over two cycles of CTX. For this analysis, symptom occurrence and severity data for the week prior to the administration of the patients’ next cycle of CTX, were analyzed. Medical records were reviewed for disease and treatment information.
Data Analysis
Data were analyzed using SPSS version 22 (IBM, Armonk, NY). Descriptive statistics and frequency distributions were calculated for demographic and clinical characteristics. Differences in demographic, clinical, and symptom characteristics were evaluated using independent sample t-tests, Chi square analyses, Fisher Exact tests, or Mann Whitney U tests. Bonferroni corrected post hoc contrasts were performed for categorical variables with more than two groups.
To evaluate whether age group made a significant independent contribution to the variance in each of the symptom severity scores, a separate multiple regression analysis was done for each symptom in which all of the demographic and clinical characteristics that differed between the age groups (see Table 1) were entered in Block 1 and age group was entered in Block 2 (i.e., to assess its unique contribution).
Table 1.
Differences in Demographic and Clinical Characteristics Between Younger and Older Oncology Patients
| Characteristic | <65 years (1) 72.2% (n=970) | ≥65 years (2) 27.8% (n=373) | Statistics |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Age (years) | 51.71 (9.60) | 71.38 (5.53) | t = −46.77; p < .001 |
| Education (years) | 16.08 (2.97) | 16.45 (3.13) | t = −2.00; p = .045 |
| Body mass index (kg/m2) | 26.17 (5.82) | 26.18 (5.41) | t = −0.03; p = .976 |
| Karnofsky Performance Status score | 79.17 (12.42) | 82.50 (12.92) | t = −4.13; p < .001 |
| Number of comorbidities | 2.23 (1.36) | 2.86 (1.51) | t = −7.08; p < .001 |
| SCQ score | 5.19 (3.06) | 6.23 (3.43) | t = −5.14, p < .001 |
| AUDIT score | 2.98 (2.50) | 2.95 (2.42) | t = 0.15, p = .884 |
| Time since cancer diagnosis (years) | 1.65 (3.19) | 2.85 (5.16) | U; p < .001 |
| Time since diagnosis (median) | 0.41 | 0.49 | |
| Number of prior cancer treatments | 1.55 (1.50) | 1.72 (1.53) | t = −1.79; p = .074 |
| Number of metastatic sites including lymph node involvement | 1.20 (1.25) | 1.35 (1.20) | t = −2.05; p = .041 |
| Number of metastatic sites excluding lymph node involvement | 0.74 (1.05) | 0.91 (1.04) | t = −2.66; p = .008 |
| % (N) | % (N) | ||
| Gender | |||
| Female | 81.4 (790) | 68.1 (254) | FE; p < .001 |
| Male | 18.6 (180) | 31.6 (118) | |
| Transgender* | 0.0 (0) | 0.3 (1) | |
| Ethnicity | X2 = 31.42; p < .001 | ||
| White | 65.1 (615) | 79.9 (294) | 2 > 1 |
| Black | 15.3 (144) | 6.5 (24) | 2 < 1 |
| Asian or Pacific Islander | 7.4 (70) | 6.8 (25) | NS |
| Hispanic Mixed or Other | 12.2 (115) | 6.8 (25) | 2 < 1 |
| Married or partnered (% yes) | 66.4 (635) | 59.6 (217) | FE; p = .024 |
| Lives alone (% yes) | 18.5 (177) | 29.2 (107) | FE; p < .001 |
| Child care responsibilities (% yes) | 28.8 (272) | 4.9 (18) | FE; p < .001 |
| Care of adult responsibilities (% yes) | 9.0 (80) | 5.1 (17) | FE; p = .024 |
| Currently employed (% yes) | 40.2 (386) | 21.5 (79) | FE; p < .001 |
| Income | |||
| < $30,000 | 16.4 (144) | 23.9 (77) | |
| $30,000 to <$70,000 | 19.7 (173) | 25.2 (81) | U, p<.001 |
| $70,000 to < $100,000 | 16.8 (148) | 17.1 (55) | |
| ≥ $100,000 | 47.1 (414) | 33.9 (109) | |
| Specific comorbidities (% yes) | |||
| Heart disease | 3.3 (32) | 12.1 (45) | FE; p < .001 |
| High blood pressure | 23.9 (232) | 46.6 (174) | FE; p < .001 |
| Lung disease | 7.9 (77) | 20.4 (76) | FE; p < .001 |
| Diabetes | 6.9 (67) | 14.7 (55) | FE; p = .001 |
| Ulcer or stomach disease | 5.1 (49) | 4.3 (16) | FE; p = .670 |
| Kidney disease | 1.2 (12) | 1.9 (7) | FE; p = .438 |
| Liver disease | 6.2 (60) | 7.2 (27) | FE; p = .536 |
| Anemia or blood disease | 13.4 (130) | 9.1 (34) | FE; p = .032 |
| Depression | 19.8 (192) | 17.4 (65) | FE; p = .353 |
| Osteoarthritis | 7.7 (75) | 23.9 (89) | FE; p < .001 |
| Back pain | 25.5 (247) | 26.5 (99) | FE; p = .667 |
| Rheumatoid arthritis | 3.0 (29) | 3.8 (14) | FE; p = .490 |
| Exercise on a regular basis (% yes) | 73.1 (693) | 64.7 (236) | FE; p = .003 |
| Smoking, current or history of (% yes) | 30.6 (292) | 47.8 (175) | FE; p < .001 |
| Cancer diagnosis | X2 = 95.71; p < .001 | ||
| Breast | 46.9 (455) | 22.8 (85) | 2 < 1 |
| Gastrointestinal | 29.2 (283) | 32.4 (121) | NS |
| Gynecological | 16.0 (155) | 21.7 (81) | 2 > 1 |
| Lung | 7.9 (77) | 23.1 (86) | 2 > 1 |
| Type of prior cancer treatment | X2 = 20.22; p < .001 | ||
| No prior treatment | 25.2 (238) | 24.0 (87) | NS |
| Only surgery, CTX, or RT | 44.8 (422) | 35.1 (127) | 2 < 1 |
| Surgery & CTX, or surgery & RT, or CTX & RT | 17.0 (160) | 27.3 (99) | 2 > 1 |
| Surgery & CTX & RT | 13.0 (123) | 13.5 (49) | NS |
| Any metastasis | |||
| Yes | 65.3 (625) | 73.8 (271) | FE; p = .003 |
| No | 34.7 (332) | 26.2 (96) | |
Abbreviations: AUDIT = Alcohol Use Disorders Identification Test, CTX = chemotherapy, dl = deciliter, FE = Fisher Exact test, gm = grams; kg = kilograms, m2 = meter squared, NS = not significant, RT = radiation therapy, SCQ = Self-Administered Comorbidity Questionnaire, SD = standard deviation, U = Mann Whitney U test
Fisher Exact test and Chi Square analyses and post hoc contrasts done without the transgender patient included in the analyses
In addition, for each age group, stepwise linear regression analyses were performed for each symptom to determine which demographic and clinical characteristics were associated with higher symptom severity scores. A p-value of <.05 was considered statistically significant.
RESULTS
Age Differences in Demographic Characteristics
As shown in Table 1, 27.8% of the sample was ≥65 years of age. Compared to the younger patients, older patients were significantly more likely to be male, white, not married or partnered, living alone, and had more years of education. In addition, older patients were less likely to be Black or of Hispanic, Mixed, or Other Ethnic Background, less likely to be employed, and less likely to report having child or adult care responsibilities. Finally, a higher percentage of older patients reported annual household incomes below $30,000.
Age Differences in Clinical Characteristics
Older patients had a higher KPS score, a higher number of comorbidities, a higher SCQ score, a longer time since their cancer diagnosis, and a higher number of metastatic sites when lymph node involvement was or was not included (Table 1). In addition, the older patients reported higher occurrence rates for heart disease, high blood pressure, lung disease, diabetes, and osteoarthritis and a lower rate of anemia. The older group was more likely to have a history of smoking and less likely to exercise on a regular basis. In terms of cancer diagnoses, the older group had lower rates of breast cancer and higher rates of GYN and lung cancer. The older group was more likely to have had two types of prior cancer treatments and more likely to have metastatic disease.
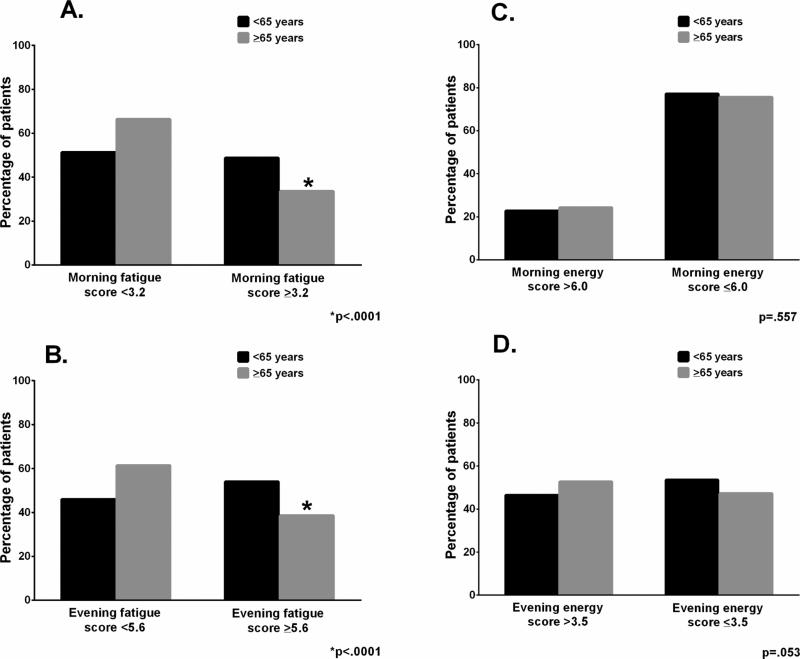
Age Differences in Fatigue
Significantly fewer older adults had morning and evening fatigue scores above the clinically meaningful cutoff scores, respectively (Figure 1). For both morning and evening fatigue, older patients reported significantly lower severity scores (Table 2).
Figure 1.
Age differences in the percentages of patients who reported morning fatigue (A), evening fatigue (B), morning energy (C), and evening energy (D) scores that were above the clinically meaning cutoff score for each symptom.
Table 2.
Differences in Fatigue, Energy, and Sleep Disturbance Scores Between Younger and Older Oncology patients
| Symptom* | <65 years 72.2% (n=970) | ≥65 years 27.8% (n=373) | Statistics |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Morning fatigue score | 3.33 (2.28) | 2.59 (2.12) | t = 5.33; p < .001 |
| Evening fatigue score | 5.56 (2.11) | 4.76 (2.16) | t = 5.98; p < .001 |
| Morning energy score | 4.45 (2.16) | 4.26 (2.48) | t = 1.27; p = .205 |
| Evening energy score | 3.46 (2.01) | 3.77 (2.10) | t = −2.43; p = .015 |
| General Sleep Disturbance Scale (GSDS) scores | |||
| Quality of sleep | 3.41 (1.80) | 3.05 (1.69) | t = 3.29; p = .001 |
| Quantity of sleep | 4.66 (1.66) | 4.46 (1.40) | t = 2.25; p = .025 |
| Sleep onset latency | 2.82 (2.31) | 2.46 (2.15) | t = 2.65; p = .008 |
| Mid-sleep awakenings | 4.93 (2.23) | 4.94 (2.15) | t = −0.10; p = .917 |
| Early awakenings | 3.77 (2.47) | 3.14 (2.36) | t = 4.09; p < .001 |
| Medications for sleep | 0.65 (0.83) | 0.52 (0.65) | t = 2.98; p = .003 |
| Excessive daytime sleepiness | 2.71 (1.45) | 2.43 (1.39) | t = 3.16; p = .002 |
| Total sleep disturbance score | 53.95 (20.65) | 48.66 (18.54) | t = 4.44; p < .001 |
| Pittsburgh Sleep Quality Index (PSQI) scores | |||
| Sleep quality | 1.28 (0.80) | 1.08 (0.76) | t = 4.10; p < .001 |
| Sleep latency | 1.30 (0.73) | 1.15 (0.69) | t = 3.52; p < .001 |
| Sleep duration | 1.05 (0.94) | 0.93 (0.92) | t = 2.11; p = .035 |
| Habitual sleep efficiency | 0.92 (1.10) | 0.94 (1.08) | t = −0.36; p = .719 |
| Sleep disturbances | 1.53 (0.56) | 1.37 (0.51) | t = 5.05; p < .001 |
| Use of sleep medications | 1.22 (1.33) | 1.17 (1.32) | t = 0.59; p = .552 |
| Daytime dysfunction | 1.01 (0.67) | 0.85 (0.64) | t = 3.90; p < .001 |
| Global PSQI score | 8.16 (3.82) | 7.28 (3.79) | t = 3.77; p < .001 |
Abbreviation: SD = standard deviation
Clinically meaningful cutoff scores: morning fatigue = ≥ 3.2, evening fatigue = ≥ 5.6, morning energy = ≤ 6.0, evening energy = ≤ 3.5, total GSDS sleep disturbance score = ≥ 43.0, global PSQI score = ≥ 5.0
In the regression analysis, after controlling for all of the characteristics that differed between the groups, age group continued to make a significant independent contribution to the explained variance in morning fatigue (adjusted difference = −0.572 (i.e., older age group had lower scores), R2 change = .010, p = <.001). For younger patients, the final predictive model explained 22.8% of the variance in morning fatigue (Table 3). Characteristics associated with a significantly higher morning fatigue score included: being female, living alone, having child care responsibilities, lack of regular exercise, having a lower KPS score, having a higher SCQ, and having a diagnosis of hypertension. For older patients, the final predictive model explained 25.3% of the variance in morning fatigue. Characteristics associated with a significantly higher morning fatigue score included: living alone, lack of regular exercise, having a lower KPS score, and having a higher SCQ score.
Table 3.
Effect of Selected Demographic and Clinical Characteristics on Total Symptom Scores in Younger and Older Oncology Patients
| MORNING FATIGUE TOTAL SCORE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Younger Patients (n = 832) | Older Patients (n = 307) | ||||||||||
| Characteristic | R2 | r | β | R2-change (sr2) | p-value | Characteristic | R2 | r | β | R2 change (sr2) | p-value |
| Overall | .228 | -- | -- | -- | <.001 | Overall | .253 | -- | -- | -- | <.001 |
| Male | -- | −.129 | −.110 | .012 | <.001 | Lives alone | -- | .139 | .129 | .017 | .010 |
| Lives alone | -- | .100 | .109 | .011 | .001 | Regular exercise | -- | −.251 | −.136 | .017 | .008 |
| Child care | -- | .061 | .077 | .005 | .018 | KPS score | -- | −.377 | −.240 | .048 | <.001 |
| Regular exercise | -- | −.117 | −.068 | .004 | .029 | SCQ score | -- | .396 | .280 | .067 | <.001 |
| KPS score | -- | −.401 | −.309 | .080 | <.001 | ||||||
| SCQ score | -- | .293 | .219 | .033 | <.001 | ||||||
| Hypertension | -- | −.018 | −.109 | .009 | .002 | ||||||
| EVENING FATIGUE TOTAL SCORE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Younger Patients (n = 810) | Older Patients (n=312) | ||||||||||
| Characteristic | R2 | r | β | R2-change (sr2) | p-value | Characteristic | R2 | r | P | R2 change (sr2) | p-value |
| Overall | .125 | -- | -- | -- | <.001 | Overall | .114 | -- | -- | -- | <.001 |
| Male | -- | −.131 | −.122 | .015 | <.001 | Nonwhite | -- | −.155 | −.169 | .029 | .002 |
| Nonwhite | -- | −.110 | −.149 | .021 | <.001 | KPS score | -- | −.257 | −.219 | .042 | <.001 |
| Education | -- | .066 | .090 | .008 | .008 | SCQ score | -- | .218 | .142 | .019 | .013 |
| Child care | -- | .126 | .129 | .016 | <.001 | ||||||
| KPS score | -- | −.239 | −.201 | .035 | <.001 | ||||||
| SCQ score | -- | .166 | .146 | .018 | <.001 | ||||||
| MORNING ENERGY TOTAL SCORE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Younger Patients (n = 855) | Older Patients (n=303) | ||||||||||
| Characteristic | R2 | r | β | R2-change (sr2) | p-value | Characteristic | R2 | r | β | R2 change (sr2) | p-value |
| Overall | .098 | -- | -- | -- | <.001 | Overall | .049 | -- | -- | -- | <.001 |
| Regular exercise | -- | .170 | .128 | .016 | <.001 | Smoker | -- | −.173 | −.175 | .031 | .002 |
| KPS score | -- | .287 | .267 | .070 | <.001 | Higher income | -- | .137 | .140 | .020 | .014 |
| EVENING ENERGY TOTAL SCORE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Younger Patients (n = 814) | Older Patients (n=317) | ||||||||||
| Characteristic | R2 | r | β | R2-change (sr2) | p-value | Characteristic | R2 | r | β | R2 change (sr2) | p-value |
| Overall | .051 | -- | -- | -- | <.001 | Overall | .045 | -- | -- | -- | <.001 |
| Nonwhite | -- | .061 | .084 | .007 | .016 | KPS score | -- | .213 | .213 | .045 | <.001 |
| Regular exercise | -- | .102 | .076 | .006 | .028 | ||||||
| KPS score | -- | .185 | .181 | .032 | <.001 | ||||||
| Years since diagnosis | -- | .065 | .080 | .006 | .021 | ||||||
| GENERAL SLEEP DISTURBANCE SCALE TOTAL SCORE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Younger Patients (n = 812) | Older Patients (n = 316) | ||||||||||
| Characteristic | R2 | r | β | R2-change (sr2) | p-value | Characteristic | R2 | r | β | R2 change (sr2) | p-value |
| Overall | .207 | -- | -- | .022 | <.001 | Overall | .168 | -- | -- | -- | <.001 |
| Nonwhite | -- | −.046 | −.098 | .009 | .002 | Nonwhite | -- | −.100 | −.126 | .016 | .016 |
| Lives alone | -- | .130 | .121 | .013 | <.001 | KPS score | -- | −.355 | −.306 | .082 | <.001 |
| Child care | -- | .073 | .123 | .014 | <.001 | SCQ score | -- | .274 | .172 | .026 | .002 |
| KPS score | -- | −.357 | −.295 | .076 | <.001 | ||||||
| SCQ score | -- | .273 | .200 | .033 | <.001 | ||||||
| Diagnosis | -- | <.001 | |||||||||
| GI vs breast | −.042 | −.057 | .003 | .092 | |||||||
| GYN vs breast | .097 | .036 | .001 | .289 | |||||||
| Lung vs breast | −.092 | −.134 | .016 | <.001 | |||||||
Abbreviations: KPS = Karnofsky Performance Status, SCQ = Self-Administered Comorbidity Questionnaire, vs = versus
In the regression analysis, after controlling for all of the characteristics that differed between the groups, age group continued to make a significant independent contribution to the explained variance in evening fatigue (adjusted difference = −0.751 (i.e., older age group had lower scores), R2 change = .017, p<.001). For younger patients, the final predictive model explained 12.5% of the variance in evening fatigue (Table 3). Characteristics associated with a significantly higher evening fatigue score included: being female, being White, having a higher level of education, having child care responsibilities, having a lower KPS score, and having a higher SCQ score. For older patients, the final predictive model explained 11.4% of the variance in evening fatigue. Characteristics associated with a significantly higher evening fatigue score included: being white, having a lower KPS score, and having a higher SCQ score.
Age Differences in Decrements in Energy
No age group differences were found in the occurrence rates for morning and evening energy scores that were below the clinically meaningful cutoff (Figure 1). While no age differences were found in morning energy scores, older patients reported significantly higher evening energy scores (Table 2).
In the regression analysis for decrements in morning energy, for younger patients, the final predictive model explained 9.8% of the variance in morning energy (Table 3). Characteristics associated with a significantly lower morning energy score (i.e., higher decrements in morning energy levels) included: lack of regular exercise and having a lower KPS score. For older patients, the final predictive model explained 4.9% of the variance in morning energy. Characteristics associated with a significantly lower morning energy score included: being a smoker and having a lower annual household income.
In the regression analysis, after controlling for all of the characteristics that differed between the groups, age group did not make a significant independent contribution to the explained variance in evening energy (p = .145). For younger patients, the final predictive model explained 5.1% of the variance in evening energy (Table 3). Characteristics associated with significantly lower evening energy scores included: being White, lack of regular exercise, having a lower KPS score, and fewer years since the cancer diagnosis. For older patients, the final predictive model explained 4.5% of the variance in evening energy. The only characteristic associated with significantly lower evening energy scores was having a lower KPS score.
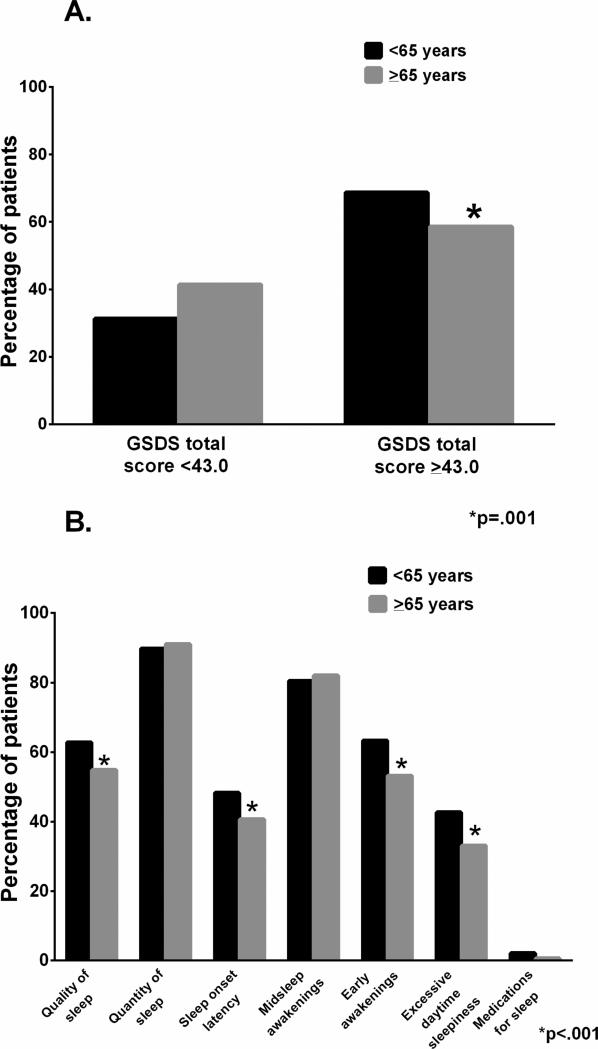
Age Differences in Sleep Disturbance
Significantly fewer older adults had total GSDS scores above the clinically meaningful cutoff score (Figure 2A). In terms of GSDS subscales, significantly fewer older patients reported occurrence rates for decreases in sleep quality that were above the clinically meaningful cutoff of ≥3.0. Likewise, significantly fewer older patients reported occurrence rates for increased sleep onset latency, increased number of early awakenings, and excessive daytime sleepiness that were above the clinically meaningful cutoff score (Figure 2B). For the various GSDS severity scores, older adults had significantly lower scores for both quality and quantity of sleep, as well as significantly lower scores for sleep onset latency, early awakenings, excessive daytime sleepiness, use of medications for sleep, and total sleep disturbance (Table 2).
Figure 2.
Age differences in the percentages of patients who reported General Sleep Disturbance Scale (GSDS) total (A) and subscale (B) scores that were above the clinically meaning cutoff score.
In the regression analysis, after controlling for all of the characteristics that differed between the groups, age group continued to make a significant independent contribution to the explained variance in GSDS total score (adjusted difference = −4.484 (i.e., older age group had lower scores), R2 change = .007, p = .007). For the younger patients, the final predictive model explained 20.7% of the variance in GSDS total score (Table 3). Characteristics associated with a significantly higher GSDS total score included: being White, living alone, having child care responsibilities, having a lower KPS score, having a higher SQC score, and having breast cancer compared to lung cancer. For older patients, the final predictive model explained 16.8% of the variance in GSDS total score. Characteristics associated with a significantly higher GSDS total score included: being White, having a lower KPS score, and having a higher SQC score.
DISCUSSION
This study is the first to evaluate for age differences in the occurrence and severity of fatigue, decrements in energy, and sleep disturbance in a large sample of oncology patients receiving CTX, as well as to identify demographic and clinical characteristics associated with higher symptom severity scores in older versus younger oncology patients. Overall, our findings suggest that, older patients experience lower or similar levels of all three symptoms and that except for decrements in evening energy, these age differences persisted after controlling for potential confounding characteristics. In addition, some of the demographic and clinical characteristics associated with more severe symptoms are similar between the two age groups. At the outset of this discussion, we need to acknowledge that given the differences in sample sizes between the younger and older age groups, our ability to identify additional characteristics associated with higher symptom severity scores in the older age group was limited. However, the common characteristics for both age groups, as well as the unique characteristics identified for each age group, should assist clinicians to identify patients at higher risk for more severe symptoms.
Differences in fatigue
Consistent with previous reports (Cataldo, et al., 2013; Oksholm, et al., 2013), older patients in our study reported lower occurrence rates for clinically meaningful levels of morning and evening fatigue, as well as lower severity ratings for both symptoms. While our findings contrast with studies that reported increased occurrence rates for fatigue in older oncology patients (Butt, et al., 2010; Hung & Mullins, 2013), neither of these studies evaluated for diurnal variations in fatigue. Of note, for both age groups in our study, the occurrence rates for clinically meaningful levels of morning and evening fatigue were above 30%. In addition, for both morning and evening fatigue, the younger patients’ fatigue severity scores were above the clinically meaningful cutoffs. Potential reasons for the inconsistent findings across studies include differences in: patients’ cancer diagnoses, the instruments used to assess fatigue, and the timing of the assessments. In addition, compared to younger patients, older patients in our study had fewer care giving responsibilities which may have reduced fatigue. Finally, the fact that older adults in this study had less sleep disturbance may have contributed to decreased levels of morning fatigue.
In both age groups, morning fatigue was the symptom with the largest percentage of explained variance. Across both age groups and for both morning and evening fatigue, patients with a poorer functional status and a higher number of comorbidities reported higher symptom severity scores. While for both age groups, the overall percentage of explained variance was relatively equal, for the younger patients, a higher percentage of the variance in morning fatigue was uniquely explained by their KPS score (i.e., 8.0%) compared to their SCQ score (i.e., 3.3%). In the older age group, the patients’ KPS (i.e., 4.8%) and SCQ (i.e., 6.7%) scores uniquely explained relatively similar amounts of variance. While previous studies found positive associations between both poorer functional status (Dhruva, et al., 2013; Hofso, Miaskowski, Bjordal, Cooper, & Rustoen, 2012) and higher levels of comorbidity (Berger, Gerber, & Mayer, 2012) and more severe fatigue, findings from our study suggest differential age effects for these two characteristics. In the older patients, research is warranted to determine which comorbidities and/or associated treatments contribute to higher levels of both morning and evening fatigue.
In both age groups, lack of regular exercise was associated with higher levels of morning, but not evening fatigue. Given the inconsistent results regarding the effects of exercise on fatigue in oncology patients (for reviews see Meneses-Echavez, Gonzalez-Jimenez, & Ramirez-Velez, 2015; Minton, Jo, & Jane, 2015), future studies should evaluate the effects of exercise on diurnal variations in fatigue severity.
In the younger patients, being female and having child care responsibilities were associated with higher levels of both morning and evening fatigue. Both of these characteristics were reported to have positive associations with fatigue severity (Dhruva, et al., 2013; Kober, et al., 2016). In addition, for the younger patients, the other two characteristics that were associated with higher levels of morning fatigue were living alone and having hypertension. Patients who live alone may lack the necessary supports to assist with routine activities that could result in increased fatigue. In terms of hypertension, depending on the class of antihypertensive medications, their adverse effects can include nocturia, nightmares, and insomnia (Dharmarajan & Dharmarajan, 2015). These adverse effects could disrupt sleep and result in morning fatigue. Given the high occurrence rates of hypertension in both age groups, additional research is warranted to confirm this finding.
Differences in decrements in energy
No studies were found that compared energy levels in older versus younger oncology patients receiving CTX. It should be noted that on the MSAS, the symptom that is used as the proxy for fatigue is “lack of energy.” So consistent with the MSAS findings cited above related to fatigue (Cataldo, et al., 2013; Oksholm, et al., 2013), no age-related differences were found in either the occurrence or severity of morning and evening energy. Of note, for both age groups, morning and evening energy levels were just at or below the clinically meaningful cutoff scores.
Compared to morning and evening fatigue, only relatively small amounts of the variance in morning and evening energy scores were explained in both age groups. In the older patients, poorer functional status was associated with more severe decrements in morning and evening energy. In the younger patients, lack of exercise was associated with more severe decrements in both morning and evening energy. This finding suggests that future studies of the efficacy of exercise interventions should evaluate for changes in both fatigue and energy.
Differences in sleep disturbance
While fewer older adults in our study experienced sleep disturbance prior to the administration of the next dose of CTX, approximately 50% of patients in both age groups reported GSDS total scores that were above the clinically meaningful cutoff. This level of sleep disturbance is consistent with previous studies of patients receiving active treatment (Cataldo, et al., 2013) and in patients prior to lung cancer surgery (Oksholm, et al., 2013) in which no age-related differences were found. Similar trends were seen for the subscale and total severity scores for the GSDS. The most common problems in both age groups were: high levels of mid-sleep awakenings, poor sleep quality, and insufficient quantity of sleep. Taken together, these findings suggest that regardless of age, oncology outpatients experience significant problems with sleep maintenance during CTX.
For both age groups, approximately 20% of the variance in sleep disturbance scores was explained by three to five characteristics. For both age groups, a lower functional status and a higher comorbidity profile made the largest independent contributions to the percentage of explained variance. In our study, the most common comorbidities were hypertension, back pain, and depression which in previous studies were associated with sleep disturbance (Agmon & Armon, 2014; Alsaadi, et al., 2014; Ford, Cunningham, Giles, & Croft, 2015; Haynes, 2015; Li, et al., 2015; Murphy & Peterson, 2015; Tang, et al., 2015). In addition, while previous findings regarding the association between sleep disturbance and ethnicity are inconsistent (Baldwin, et al., 2010; Jean-Louis, et al., 2008; Paine, Gander, Harris, & Reid, 2004; Sanford, et al., 2006), in our study, younger and older patients who reported their ethnicity as White had a higher level of sleep disturbance. As noted with morning fatigue in the younger age group, living alone and having child care responsibilities were associated with higher levels of sleep disturbance.
Conclusions and limitations
As previously reported by our group (Cataldo, et al., 2013), older patients appear to have a lower symptom burden than younger patients. Several factors may explain these age-related differences. First, older patients often have higher rates of dose reductions in their CTX regimens than younger patients (Brunello, Loaldi, & Balducci, 2009; Hamaker, Schreurs, Uppelschoten, & Smorenburg, 2009; Townsley, et al., 2005). In addition, it is possible that a “response shift” in the perception of symptoms occurs in older adults. This response shift is characterized by a change in patients’ internal standards that can be catalyzed by a change in their health status (Schwartz & Sprangers, 1999; Sprangers & Schwartz, 1999). As noted in Table 1, compared to younger patients, older patients reported a higher number of comorbidities, a higher level of comorbidity, and higher rates of heart disease, hypertension, lung disease, diabetes, and osteoarthritis. It is possible that, due to this increased comorbidity profile, older adults’ perceptions of fatigue, changes in energy levels, and sleep disturbance shifted over time. Alternatively, these differences in symptom occurrence rates and severity ratings may be explained by some of the age associated phenotypic differences found in this sample. For example, in our study, older patients had fewer child care and older adult care responsibilities which may have allowed for more time for rest and relaxation and afforded less sleep disruptions. Additional research is warranted to determine the phenotypic characteristics and molecular mechanisms that contribute to age-related differences in patients’ symptom experiences.
Regardless of age group, the two characteristics that were associated with higher severity scores were poorer functional status and a more severe comorbidity profile. In terms of functional status, clinicians can recommend interventions like regular exercise and strength training to improve patients’ functional status before, during, and after CTX. While, as was the case in our study, one might expect a higher level of comorbidity in older patients, this characteristics was associated with a higher symptom burden in the younger patients. Additional research is warranted to determine how and why comorbidities and associated treatments are associated with more severe symptom profiles.
Some study limitations need to be acknowledged. First, patients were recruited during their second to fourth cycle CTX which did not allow for an assessment of symptoms prior to the initiation of CTX. Second, controversy exists about the choice of the age cutoff to evaluate for age differences. While in our study and other studies (Butt, et al., 2010; Mohile, et al., 2011), >65 years of age was used as the cutoff, other studies used >60 years of age (Buffum, et al., 2011; Cataldo, et al., 2013). Therefore, our findings may not be generalizable to all studies of age differences in symptoms in oncology patients. In addition, it is possible that the findings from this study underestimate the symptom burden of both the younger and older oncology patients because the major reason patients refused to participate in this study was being overwhelmed with their cancer treatment. Finally, while the sample size was relatively large for both age groups, future studies need to recruit a larger sample of older adults, particularly those >75 years of age to make the findings more generalizable to older patients receiving CTX.
In conclusion, our findings provide new insights into age differences in and characteristics associated with increased levels of fatigue, decrements in energy, and increased levels of sleep disturbance in oncology patients. While older patients reported less severe symptoms, both age groups experienced high occurrence rates and moderate to severe levels of all three symptoms. Therefore, clinicians need to assess all oncology patients receiving CTX for these three symptoms as well as their associated characteristics. Future research needs to determine specific reasons for and phenotypic and molecular characteristics associated with these age-related differences in patients’ symptom experiences.
Supplementary Material
The number of older adults with cancer is increasing. Given the limited amount of research and the inconsistent findings regarding age differences in common physical symptoms associated with cancer and its treatments, the purposes of this study, in a sample of oncology outpatients receiving chemotherapy (CTX), were to evaluate for age differences in demographic and clinical characteristics, as well as in occurrence rates of and severity ratings for fatigue, decrements in energy, and sleep disturbance. Overall, our findings suggest that compared to younger patients, older adults experience a lower or similar level of fatigue, decrements in energy, and sleep disturbance. However, it should be noted that both age groups experienced high occurrence rates and moderate to severe levels of all three symptoms.
Acknowledgements
This study was supported by a grant from the National Cancer Institute (NCI, CA134900). Dr Miaskowski is supported by a grant from the American Cancer Society and a K05 award (CA168960) from the NCI.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agmon M, Armon G. Increased insomnia symptoms predict the onset of back pain among employed adults. PLoS One. 2014;9(8):e103591. doi: 10.1371/journal.pone.0103591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsaadi SM, McAuley JH, Hush JM, Bartlett DJ, McKeough ZM, Grunstein RR, et al. Assessing sleep disturbance in low back pain: the validity of portable instruments. PLoS One. 2014;9(4):e95824. doi: 10.1371/journal.pone.0095824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aouizerat BE, Dhruva A, Paul SM, Cooper BA, Kober KM, Miaskowski C. Phenotypic and molecular evidence suggest that decrements in morning and evening energy are distinct but related symptoms. Journal of Pain and Symptom Management. 2015;50(5):599–614. doi: 10.1016/j.jpainsymman.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin CM, Ervin AM, Mays MZ, Robbins J, Shafazand S, Walsleben J, et al. Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. Journal of Clinical Sleep Medicine. 2010;6(2):176–183. [PMC free article] [PubMed] [Google Scholar]
- Berger AM. Update on the state of the science: sleep-wake disturbances in adult patients with cancer. Oncology Nursing Forum. 2009;36(4):E165–177. doi: 10.1188/09.ONF.E165-E177. [DOI] [PubMed] [Google Scholar]
- Berger AM, Abernethy AP, Atkinson A, Barsevick AM, Breitbart WS, Cella D, et al. Cancer-related fatigue. Journal of the National Comprehensive Cancer Network. 2010;8(8):904–931. doi: 10.6004/jnccn.2010.0067. [DOI] [PubMed] [Google Scholar]
- Berger AM, Gerber LH, Mayer DK. Cancer-related fatigue: implications for breast cancer survivors. Cancer. 2012;118(8 Suppl):2261–2269. doi: 10.1002/cncr.27475. [DOI] [PubMed] [Google Scholar]
- Berger AM, Mooney K, Alvarez-Perez A, Breitbart WS, Carpenter KM, Cella D, et al. Cancer-Related Fatigue, Version 2.2015. Journal of the National Comprehensive Cancer Network. 2015;13(8):1012–1039. doi: 10.6004/jnccn.2015.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunello A, Loaldi E, Balducci L. Dose adjustment and supportive care before and during treatment. Cancer Treatment Reviews. 2009;35(6):493–498. doi: 10.1016/j.ctrv.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Buffum D, Koetters T, Cho M, Macera L, Paul SM, West C, et al. The effects of pain, gender, and age on sleep/wake and circadian rhythm parameters in oncology patients at the initiation of radiation therapy. Journal of Pain. 2011;12(3):390–400. doi: 10.1016/j.jpain.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butt Z, Rao AV, Lai JS, Abernethy AP, Rosenbloom SK, Cella D. Age-associated differences in fatigue among patients with cancer. Journal of Pain and Symptom Management. 2010;40(2):217–223. doi: 10.1016/j.jpainsymman.2009.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cataldo JK, Paul S, Cooper B, Skerman H, Alexander K, Aouizerat B, et al. Differences in the symptom experience of older versus younger oncology outpatients: a cross-sectional study. BMC Cancer. 2013;13(1):6. doi: 10.1186/1471-2407-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu TL, Yu WP, Chen SC, Peng HL, Wu MJ. Comparison of differences and determinants between presence and absence of sleep disturbance in hepatocellular carcinoma patients. Cancer Nursing. 2011;34(5):354–360. doi: 10.1097/NCC.0b013e3182037bf3. [DOI] [PubMed] [Google Scholar]
- Dharmarajan TS, Dharmarajan L. Tolerability of Antihypertensive Medications in Older Adults. Drugs and Aging. 2015;32(10):773–796. doi: 10.1007/s40266-015-0296-3. [DOI] [PubMed] [Google Scholar]
- Dhruva A, Aouizerat BE, Cooper B, Paul SM, Dodd M, West C, et al. Differences in morning and evening fatigue in oncology patients and their family caregivers. European Journal of Oncology Nursing. 2013;17(6):841–848. doi: 10.1016/j.ejon.2013.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher BS, Paul SM, Dodd MJ, Schumacher K, West C, Cooper B, et al. Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. Journal of Clinical Oncology. 2008;26(4):599–605. doi: 10.1200/JCO.2007.12.2838. [DOI] [PubMed] [Google Scholar]
- Ford ES, Cunningham TJ, Giles WH, Croft JB. Trends in insomnia and excessive daytime sleepiness among U.S. adults from 2002 to 2012. Sleep Medicine. 2015;16(3):372–378. doi: 10.1016/j.sleep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay CL, Lee KA, Lee SY. Sleep patterns and fatigue in new mothers and fathers. Biological Research for Nursing. 2004;5(4):311–318. doi: 10.1177/1099800403262142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbertson-White S, Aouizerat BE, Jahan T, Miaskowski C. A review of the literature on multiple symptoms, their predictors, and associated outcomes in patients with advanced cancer. Palliative and Supportive Care. 2011;9(1):81–102. doi: 10.1017/S147895151000057X. [DOI] [PubMed] [Google Scholar]
- Hamaker ME, Schreurs WH, Uppelschoten JM, Smorenburg CH. Breast cancer in the elderly: retrospective study on diagnosis and treatment according to national guidelines. Breast Journal. 2009;15(1):26–33. doi: 10.1111/j.1524-4741.2008.00667.x. [DOI] [PubMed] [Google Scholar]
- Haynes P. Application of cognitive behavioral therapies for comorbid insomnia and depression. Sleep Medicine Clinics. 2015;10(1):77–84. doi: 10.1016/j.jsmc.2014.11.006. [DOI] [PubMed] [Google Scholar]
- Hofso K, Miaskowski C, Bjordal K, Cooper BA, Rustoen T. Previous chemotherapy influences the symptom experience and quality of life of women with breast cancer prior to radiation therapy. Cancer Nursing. 2012;35(3):167–177. doi: 10.1097/NCC.0b013e31821f5eb5. [DOI] [PubMed] [Google Scholar]
- Hung A, Mullins CD. Relative effectiveness and safety of chemotherapy in elderly and nonelderly patients with stage III colon cancer: a systematic review. Oncologist. 2013;18(1):54–63. doi: 10.1634/theoncologist.2012-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean-Louis G, Magai C, Casimir GJ, Zizi F, Moise F, McKenzie D, et al. Insomnia symptoms in a multiethnic sample of American women. Journal of Womens Health. 2008;17(1):15–25. doi: 10.1089/jwh.2006.0310. [DOI] [PubMed] [Google Scholar]
- Karnofsky D. Performance scale. Plenum Press; New York: 1977. [Google Scholar]
- Karnofsky D, Abelmann WH, Craver LV, Burchenal JH. The use of nitrogen mustards in the palliative treatment of carcinoma. Cancer. 1948;1:634–656. [Google Scholar]
- Kober KM, Cooper BA, Paul SM, Dunn LB, Levine JD, Wright F, et al. Subgroups of chemotherapy patients with distinct morning and evening fatigue trajectories. Supportive Care in Cancer. 2016;24(4):1473–1485. doi: 10.1007/s00520-015-2895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KA. Self-reported sleep disturbances in employed women. Sleep. 1992;15(6):493–498. doi: 10.1093/sleep/15.6.493. [DOI] [PubMed] [Google Scholar]
- Lee KA, DeJoseph JF. Sleep disturbances, vitality, and fatigue among a select group of employed childbearing women. Birth. 1992;19(4):208–213. doi: 10.1111/j.1523-536x.1992.tb00404.x. [DOI] [PubMed] [Google Scholar]
- Lee KA, Hicks G, Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatry Research. 1991;36(3):291–298. doi: 10.1016/0165-1781(91)90027-m. [DOI] [PubMed] [Google Scholar]
- Lee KA, Portillo CJ, Miramontes H. The fatigue experience for women with human immunodeficiency virus. Journal of Obstetrics Gynecology and Neonatal Nursing. 1999;28(2):193–200. doi: 10.1111/j.1552-6909.1999.tb01984.x. [DOI] [PubMed] [Google Scholar]
- Lerdal A. A theoretical extension of the concept of energy through an empirical study. Scandinavian Journal of Caring Science. 2002;16(2):197–206. doi: 10.1046/j.1471-6712.2002.00079.x. [DOI] [PubMed] [Google Scholar]
- Li Y, Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Sun Y, Zhou J, et al. Insomnia with physiological hyperarousal is associated with hypertension. Hypertension. 2015;65(3):644–650. doi: 10.1161/HYPERTENSIONAHA.114.04604. [DOI] [PubMed] [Google Scholar]
- Meneses-Echavez JF, Gonzalez-Jimenez E, Ramirez-Velez R. Effects of Supervised multimodal exercise interventions on cancer-related fatigue: systematic review and meta-analysis of randomized controlled trials. Biomedical Research International. 2015;2015:328636. doi: 10.1155/2015/328636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miaskowski C, Cooper BA, Paul SM, Dodd M, Lee K, Aouizerat BE, et al. Subgroups of patients with cancer with different symptom experiences and quality-of-life outcomes: a cluster analysis. Oncology Nursing Forum. 2006;33(5):E79–89. doi: 10.1188/06.ONF.E79-E89. [DOI] [PubMed] [Google Scholar]
- Miaskowski C, Lee KA. Pain, fatigue, and sleep disturbances in oncology outpatients receiving radiation therapy for bone metastasis: a pilot study. Journal of Pain and Symptom Management. 1999;17(5):320–332. doi: 10.1016/s0885-3924(99)00008-1. [DOI] [PubMed] [Google Scholar]
- Miaskowski C, Paul SM, Cooper BA, Lee K, Dodd M, West C, et al. Trajectories of fatigue in men with prostate cancer before, during, and after radiation therapy. Journal of Pain and Symptom Management. 2008;35(6):632–643. doi: 10.1016/j.jpainsymman.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minton O, Jo F, Jane M. The role of behavioural modification and exercise in the management of cancer-related fatigue to reduce its impact during and after cancer treatment. Acta Oncology. 2015;54(5):581–586. doi: 10.3109/0284186X.2014.996660. [DOI] [PubMed] [Google Scholar]
- Mohile SG, Heckler C, Fan L, Mustian K, Jean-Pierre P, Usuki K, et al. Age-related Differences in symptoms and their interference with quality of life in 903 cancer patients undergoing radiation therapy. Journal of Geriatric Oncology. 2011;2(4):225–232. doi: 10.1016/j.jgo.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy MJ, Peterson MJ. Sleep disturbances in depression. Sleep Medicine Clinics. 2015;10(1):17–23. doi: 10.1016/j.jsmc.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon MM, Zulley J, Guilleminault C, Smirne S, Priest RG. How age and daytime activities are related to insomnia in the general population: Consequences for older people. Journal of American Geriatrics Society. 2001;49(4):360–366. doi: 10.1046/j.1532-5415.2001.49077.x. [DOI] [PubMed] [Google Scholar]
- Oksholm T, Miaskowski C, Kongerud JS, Cooper B, Paul SM, Laerum L, et al. Does age influence the symptom experience of lung cancer patients prior to surgery? Lung Cancer. 2013;82(1):156–161. doi: 10.1016/j.lungcan.2013.06.016. [DOI] [PubMed] [Google Scholar]
- Paine SJ, Gander PH, Harris R, Reid P. Who reports insomnia? Relationships with age, sex, ethnicity, and socioeconomic deprivation. Sleep. 2004;27(6):1163–1169. doi: 10.1093/sleep/27.6.1163. [DOI] [PubMed] [Google Scholar]
- Ratcliff CG, Lam CY, Arun B, Valero V, Cohen L. Ecological momentary assessment of sleep, symptoms, and mood during chemotherapy for breast cancer. Psychooncology. 2014;23(11):1220–1228. doi: 10.1002/pon.3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosekind MR. The epidemiology and occurrence of insomnia. Journal of Clinical Psychiatry. 1992;53(Suppl):4–6. [PubMed] [Google Scholar]
- Sanford SD, Lichstein KL, Durrence HH, Riedel BW, Taylor DJ, Bush AJ. The influence of age, gender, ethnicity, and insomnia on Epworth sleepiness scores: a normative US population. Sleep Medicine. 2006;7(4):319–326. doi: 10.1016/j.sleep.2006.01.010. [DOI] [PubMed] [Google Scholar]
- Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis and Rheumatism. 2003;49(2):156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schwartz CE, Sprangers MA. Methodological approaches for assessing response shift in longitudinal health-related quality-of-life research. Social Science and Medicine. 1999;48(11):1531–1548. doi: 10.1016/s0277-9536(99)00047-7. [DOI] [PubMed] [Google Scholar]
- Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. Journal of Clinical Oncology. 2009;27(17):2758–2765. doi: 10.1200/JCO.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- Sprangers MA, Schwartz CE. The challenge of response shift for quality-of-life-based clinical oncology research. Annals of Oncology. 1999;10(7):747–749. doi: 10.1023/a:1008305523548. [DOI] [PubMed] [Google Scholar]
- Tang NK, Lereya ST, Boulton H, Miller MA, Wolke D, Cappuccio FP. Nonpharmacological treatments of insomnia for long-term painful conditions: A systematic review and meta-analysis of patient-reported outcomes in randomized controlled trials. Sleep. 2015;38(11):1751–1764. doi: 10.5665/sleep.5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsley C, Pond GR, Peloza B, Kok J, Naidoo K, Dale D, et al. Analysis of treatment practices for elderly cancer patients in Ontario, Canada. Journal of Clinical Oncology. 2005;23(16):3802–3810. doi: 10.1200/JCO.2005.06.742. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.