Abstract
There are clear health benefits to exercise; even so, patients with cardiac conditions who engage in exercise and athletic competition may on rare occasion experience sudden cardiac death (SCD). This article reviews the epidemiology and common causes of SCD in specific athlete populations. There is ongoing debate about the optimal mechanism for SCD prevention, specifically regarding the inclusion of the ECG and/or cardiac imaging in routine preparticipation sports evaluation. This controversy and contemporary screening recommendations are also reviewed.
Keywords: sudden cardiac death, sudden cardiac arrest, exercise, athlete, electrocardiogram
Introduction
Exercise is one of the most powerful tools for improving health and has been associated with beneficial change in most cardiovascular risk factors, including lipids, blood pressure, insulin sensitivity, and weight.1–4 Numerous epidemiological studies have consistently shown an association between moderate aerobic exercise and decreased risk of coronary heart disease (CHD) and death, and even a small amount of exercise provides significant risk reduction compared to a sedentary lifestyle.5–9 While there is controversy about the potential connection between intense endurance exercise and increased risk of some cardiac conditions (i.e., atrial fibrillation, ventricular fibrosis), on balance, exercise is clearly health-promoting for the large majority of individuals.10,11 However, for a small number of individuals who harbor cardiac conditions, exercise can sometimes be associated with the risk of sudden death (i.e., the exercise paradox). Sudden cardiac death (SCD) is the most frequent medical cause of sudden death in athletes, and estimates vary widely based on the population. A recent estimate of SCD incidence ranged from 1 in 40,000 to 1 in 80,000 athletes per year.12 Though SCD is rare, its occurrence in athletes who are often young and presumably healthy has a large emotional and social impact on the surrounding community. Therefore, considerable effort has been made to better understand the causes of SCD in athletes and to discover optimal strategies for prevention.
SCD in Athletes: Definitions and Epidemiology
The definition of an athlete varies. A competitive athlete has been proposed to be “one who participates in an organized team or individual sport that requires competition against others as a central component, places a high premium on excellence and achievement, and requires some form of systematic (and usually intense) training.”13 This definition is considerably easier to apply to high school, collegiate, and professional organized sport participants but more difficult to apply to younger and older populations who participate in recreational activities (i.e., a heterogeneous group of adults participating in a running race). Therefore, when estimating SCD incidence, the population of athletes “at risk” may be difficult to quantify. The definition of SCD in athletes also varies; some estimates of incidence include only deaths with exertion or shortly (< 1 hour) after exertion, while others include any SCD in an athlete (exertional or outside of exertion) and also episodes of resuscitated sudden cardiac arrest (SCA).12 These inconsistencies help account for the wide range of estimated incidence of SCD in athletes in prior reports, from 1 in 3,000 up to 1 in 1 million.12
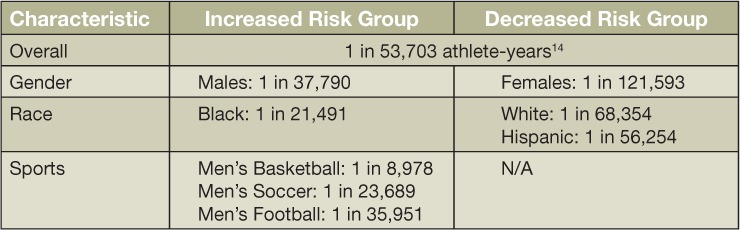
It also has been increasingly recognized that some populations of athletes may be at substantially higher risk than others for SCD. Among National Collegiate Athletic Association (NCAA) athletes, increased risk has been found with male gender, black race, and basketball participation (Table 1).14 The risk among male Division 1 basketball players has been estimated at more than 10 times that in the overall athlete population (1 in 5,200 vs. 1 in 53,703 athletes per year), which is consistent with prior findings in collegiate and high-school athletes.14 The mechanism of increased risk is not clear; though Marfan syndrome and resulting aortic dissection have most commonly occurred in male basketball players, this accounts for a small fraction of the deaths in this population.14
Table 1.
Risk factors for sudden cardiac death in National Collegiate Athletic Association (NCAA) athletes.
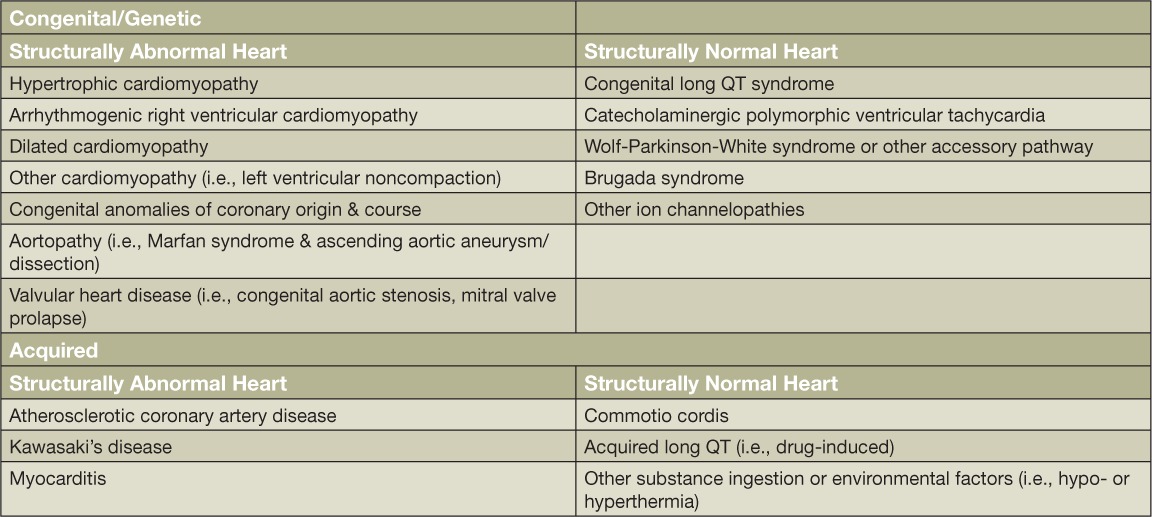
Causes of SCD in Athletes
The most common causes of SCD in athletes are shown in Table 2. In athletes under 35 years of age, inherited cardiac conditions predominate, with hypertrophic cardiomyopathy (HCM) and anomalous origin of a coronary artery being the two most common causes in the United States. In athletes older than 35, most SCD events are due to acquired atherosclerotic coronary artery disease (CAD).15,16 Many of these diagnoses may not be clinically apparent and may first present with sudden death. Estimates of the proportion of athletes with prodromal symptoms is difficult given that the account does not come from the victim and is subject to substantial bias; however, upwards of approximately 30% of athletes with SCD have been reported to have had symptoms such as chest pain, shortness of breath, performance decline, palpitations, pre-syncope, or syncope leading up to the event.17 Evaluation of such exertional symptoms by a qualified team of sports medicine and cardiology physicians is an important aspect of the medical care of athletes and of SCD prevention.18
Table 2.
Common cardiovascular conditions associated with sudden cardiac death (SCD) in athletes.
The Older Athlete
Though most SCDs in “competitive athletes” occur in younger populations, SCD during sports is far more common in older athletes, with an estimated incidence of around 21 per 1 million participants per year.17 As the population ages and the popularity of running, cycling, and other endurance sports increases, the burden of SCD risk in this group is likely to grow. As noted above, the most common identified cause of SCD in the older athlete population is atherosclerotic CAD. Although regular physical activity clearly reduces the risk of acquiring CAD and of suffering a related cardiovascular event, those who already have the disease have clearly been shown to have elevated risk of cardiovascular events with vigorous exercise.19,20 There remains debate as to whether the predominant mechanism for SCD is plaque rupture or supply/demand mismatch in the context of exercise.21 In an evaluation of SCD/SCA during long-distance running races (i.e., marathon and half marathon distance), the average age of those who had SCD/SCA was 42 years old, and CAD was second to HCM as a cause of SCA.15 There was no associated plaque rupture on angiography in any participants with CAD, suggesting that the SCA was due to supply/demand mismatch. Those who suffered SCA due to CAD were far more likely to survive than those with HCM (44% vs. 0%, odds ratio 0.13). In general, SCD with exercise is more common in males, older sports participants who are not regularly active, and those who have known cardiac disease or risk factors for CAD.17,19 These characteristics provide an opportunity for clinicians to target screening and other risk reduction strategies, as further discussed below, to those at highest risk.
The Younger Athlete
In the majority of U.S. studies, the most commonly identified cause for SCD in young athletes is HCM, a genetic condition characterized by left ventricular hypertrophy and cardiac myocyte disarray predisposing to ventricular arrhythmias (Table 2).22 The prevalence of HCM in the general population is up to 1 in 200 individuals, and in many the first presenting symptom may be SCD.23 Congenital coronary artery anomalies, consisting of a variety of abnormalities of coronary origin and proximal course, are the second most common cause of SCD in young U.S. athletes, responsible for around 17% of SCD cases.22 The remaining causes of SCD in athletes include other inherited or acquired myocardial diseases, other structural cardiovascular disease, or primary arrhythmogenic disorders (Table 2).
More recent data in NCAA athletes suggests that the most common rank list of causes of SCD may merit re-evaluation.14 In a study by Harmon et al., which reviewed all deaths among NCAA athletes from 2003 to 2013, the most common finding at autopsy for SCD cases was a structurally normal heart (25%), implying that arrhythmias and other electrical disorders may be the most common etiology. Coronary anomalies were the second most common finding and were present at a similar proportion as was previously reported (11%), but definitive HCM was far less frequent—only 8% of SCD cases vs. 30% to 40% in prior studies. The authors note that this may be due to different definitions of HCM (as opposed to potential athletic remodeling) used at autopsy as well as the population included in their study compared to prior studies.14
It is also notable that reports from other countries such as Italy and Denmark have found that the most common cause of SCD in young athletes is arrhythmogenic right ventricular cardiomyopathy (ARVC), responsible for around 25% of SCD cases in athletes from those countries.24,25 ARVC is a genetic cardiomyopathy with an estimated prevalence of 1 in 5,000 that is typified by fibro-fatty infiltration and dilation of the right ventricle. Risk of ventricular arrhythmia is increased by exercise, and exercise training itself may accelerate phenotypic expression of ARVC.26 ARVC remains an important diagnosis to consider in U.S. athletes but is less common (< 5% of SCD cases).22 It is not clear whether the higher rate of ARVC-related SCD in international populations reflects a higher prevalence of this disease, exclusion of athletes with alternative diagnoses (i.e., HCM) due to systematic preparticipation screening in other countries, or under-recognition of ARVC in the U.S. athlete population.
SCD Prevention: Athlete Screening and Evaluation
Since many of the cardiac conditions that cause SCD in athletes may not present with warning symptoms, there has been considerable discussion about the role of preparticipation screening tests to evaluate for occult cardiovascular disease. A flowchart of common tools for screening and evaluating athletes is shown in Figure 1. The value of any screening test is determined by the characteristics of the population to which it is applied. As demonstrated above, the incidence and causes of SCD vary widely depending on the age, gender, race, country, and sport of the athlete group. Therefore, it is unlikely that any single screening program will be effective across all groups. Issues such as resource utilization and cost-effectiveness also must be considered.
Figure 1.
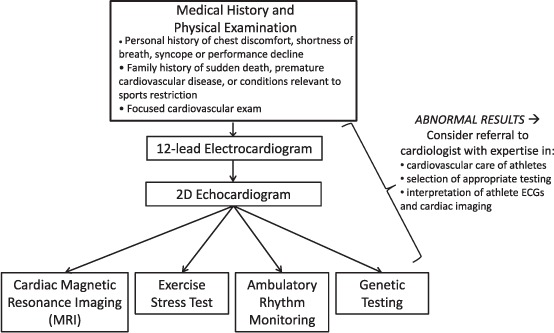
Screening and diagnostic tools for the cardiovascular evaluation of the athlete.
Accordingly, there are major differences in contemporary guidelines for preparticipation screening of athletes. The American Heart Association (AHA) and American College of Cardiology (ACC) recommend screening that is limited to a targeted medical history and physical exam.27 The specific 12-element list recommended by the AHA includes questions regarding a personal history of concerning cardiovascular symptoms (i.e., chest pain, syncope, dyspnea) and a family history of premature sudden death or disability from heart disease in addition to a focused physical exam. In our experience, specific inquiries about family history (i.e., “Does anyone in the family have a history of hypertrophic cardiomyopathy or implantable defibrillator/pacemaker?”) may be more beneficial than general questions (i.e., “Is there family history of heart disease?”), particularly with younger athletic populations. In contrast to the American recommendations, the European Society of Cardiology (ESC) and International Olympic Committee (IOC) advocate for screening that also includes a resting 12-lead electrocardiogram (ECG).28,29 The role of the ECG in preparticipation screening has garnered considerable debate.30,31 ECG-inclusive screening appears to increase the sensitivity of preparticipation screening for identifying cardiovascular disorders that predispose to SCD.32 However, there is a paucity of well-designed prospective randomized studies to evaluate whether this translates into a reduction in SCD rates.
The interpretation of ECGs in athletes is also complicated by the fact that exercise may be associated with a number of ECG findings that are not pathologic but can be perceived as such, especially by clinicians unaccustomed to interpreting ECGs in athletic individuals.33,34 Several guidelines and expert consensus statements have been designed to help clinicians interpret ECGs in athletes, with the goal of preserving sensitivity and improving specificity.28,35,36 This has led to reductions in the false positive rate as these criteria have been refined over time.33,37,38 However, even a relatively low false positive rate (< 5%) may significantly add to the burden of downstream testing if ECG screening were applied to the entire population of competitive athletes in the United States. In summary, the role of the ECG in preparticipation athlete screening remains unclear, and athletic programs should consider using ECG-inclusive screening based on the characteristics of their athlete population, the local screening resources available, and access to expert ECG interpretation specific to athletes.
Evaluation extending beyond a history, physical exam, and ECG is indicated if any of these preparticipation tests are abnormal and/or an athlete presents with symptoms during the course of practice or competition (Figure 1). It is critical that downstream testing, which can include cardiac imaging, exercise testing, and electrophysiological evaluation, is delivered and interpreted by physicians (typically cardiologists) who understand the cardiovascular adaptations to exercise training and resultant physiologic changes in the heart's structure and function—the so-called “athlete's heart.” In most athletes, cardiac changes induced by exercise are modest and easily distinguishable from cardiac pathology. However, in a small subset of athletes, vigorous training is associated with more profound electrical and structural changes that may overlap with phenotypically mild manifestations of cardiac disease. For example, sports with significant isometric exercise may induce left ventricular hypertrophy with wall thicknesses in the 12- to 14-mm range, the same range as that of mild HCM (“gray zone” hypertrophy).39 A small but significant proportion of endurance athletes will have dilated left ventricular (LV) cavities with low normal LV function, which overlaps with findings of a dilated cardiomyopathy.40 These physiologic changes to the left ventricle may be accompanied by right ventricular (RV) dilation and reduced systolic function, which could raise concern for ARVC in the appropriate context. In these types of cases, it is crucial that an expert team—including cardiologists familiar with the care of athletic patients—select and interpret the required testing to more clearly distinguish cardiac pathology from physiologic remodeling. Comprehensive exercise testing (typically including cardiopulmonary exercise testing) is a critical component of the evaluation of such patients. For the cases of gray zone hypertrophy, techniques such as prescribed detraining (assessing for LV hypertrophy regression after a period of inactivity) may need to be employed.41
Finally, most of the debate about preparticipation evaluation of athletes revolves around the infrastructure for screening school-aged or professional athletes. There is large population of older athletes who may still participate in high-level sports (i.e., Master's athletes), but do so outside the structure of an organized team. Therefore, they may not be subject to any form of screening yet may harbor high risk for adverse events with exercise, primarily due to CAD. The AHA and American College of Sports Medicine recommend a similar targeted history aimed at identifying those at high risk of cardiac events prior to participation in activities at fitness facilities, and the ACC/AHA guidelines recommend that exercise testing is reasonable, even in the absence of symptoms, for the evaluation of persons at high risk of CAD (i.e,, diabetics) or in men older than 45 years or women older than 55 years who plan to start a vigorous exercise program.42,43
Conclusion
Although rare, SCD in the athlete is a traumatic event that has a large impact on society. The incidence of SCD varies widely depending on the athlete population. In older athletes, SCD is primarily due to CAD and associated complications. In younger athletes, it is due to congenital or genetically mediated cardiovascular disease, such as HCM, coronary artery anomalies, other cardiomyopathies, or primary arrhythmogenic disorders. All preparticipation screening programs aimed at identifying athletes at high risk of SCD begin with a focused history and physical. The addition of the 12-lead ECG and/or additional cardiac testing is a source of considerable ongoing debate. The optimal preparticipation evaluation for a given group depends on the athlete population and the available screening resources, including clinicians with expertise in the cardiovascular care of athletes. It is highly unlikely that any screening program will be effective at appropriately identifying all athletes at risk of SCD; therefore, increased access to automated external defibrillators as well as training in cardiopulmonary resuscitation at a community level are important means of reducing SCD in athletes.
Conflict of Interest Disclosure: The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
Key Points
Though exercise is, in general, health-promoting, it is associated with an increased risk of sudden cardiac death for a small number of individuals who harbor cardiac conditions.
Sudden cardiac death is the most common medical cause of death in athletes, with an incidence of around 1 in 40,000 to 1 in 80,000 athletes per year according to the most recent estimates.
The risk and causes of sudden cardiac death vary based upon the athlete population. Male gender, black race, and basketball participation all place an athlete at higher risk. Sudden cardiac death in younger athletes (< 35 years) is commonly due to inherited cardiac conditions, while in older athletes (> 35 years) it is most often due to atherosclerotic coronary artery disease.
There remains significant debate over the best strategy to prevent sudden cardiac death in athletes and the role of the electrocardiogram in preparticipation screening. The optimal preparticipation evaluation for a given group of athletes depends on the risk of the population and available expert resources.
References
- 1.Kraus WE, Houmard JA, Duscha BD et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N Engl J Med. 2002 Nov 7;347(19):1483–92. doi: 10.1056/NEJMoa020194. [DOI] [PubMed] [Google Scholar]
- 2.Williams PT. Attenuating effect of vigorous physical activity on the risk for inherited obesity: a study of 47,691 runners. PloS One. 2012;7(2):e31436. doi: 10.1371/journal.pone.0031436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parker ED, Schmitz KH, Jacobs DR, Jr, Dengel DR, Schreiner PJ. Physical activity in young adults and incident hypertension over 15 years of follow-up: the CARDIA study. Am J Public Health. 2007 Apr;97(4):703–9. doi: 10.2105/AJPH.2004.055889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laaksonen DE, Lakka HM, Salonen JT, Niskanen LK, Rauramaa R, Lakka TA. Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care. 2002 Sep;25(9):1612–8. doi: 10.2337/diacare.25.9.1612. [DOI] [PubMed] [Google Scholar]
- 5.Arem H, Moore SC, Patel A et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015 Jun;175(6):959–67. doi: 10.1001/jamainternmed.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wen CP, Wai JP, Tsai MK et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011 Oct 1;378(9798):1244–53. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 7.Chomistek AK, Cook NR, Flint AJ, Rimm EB. Vigorous-intensity leisure-time physical activity and risk of major chronic disease in men. Med Sci Sports Exerc. 2012 Oct;44(10):1898–905. doi: 10.1249/MSS.0b013e31825a68f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paffenbarger RS, Jr, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993 Feb 25;328(8):538–45. doi: 10.1056/NEJM199302253280804. [DOI] [PubMed] [Google Scholar]
- 9.Shiroma EJ, Lee IM. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. 2010 Aug 17;122(7):743–52. doi: 10.1161/CIRCULATIONAHA.109.914721. [DOI] [PubMed] [Google Scholar]
- 10.La Gerche A, Heidbuchel H. Can intensive exercise harm the heart? You can get too much of a good thing. Circulation. 2014 Sep 16;130(12):992–1002. doi: 10.1161/CIRCULATIONAHA.114.008141. [DOI] [PubMed] [Google Scholar]
- 11.Levine BD. Can intensive exercise harm the heart? The benefits of competitive endurance training for cardiovascular structure and function. Circulation. 2014 Sep 16;130(12):987–91. doi: 10.1161/CIRCULATIONAHA.114.008142. [DOI] [PubMed] [Google Scholar]
- 12.Harmon KG, Drezner JA, Wilson MG, Sharma S. Incidence of sudden cardiac death in athletes: a state-of-the-art review. Br J Sports Med. 2014 Aug;48(15):1185–92. doi: 10.1136/bjsports-2014-093872. [DOI] [PubMed] [Google Scholar]
- 13.Maron BJ, Douglas PS, Graham TP, Nishimura RA, Thompson PD. Task Force 1: preparticipation screening and diagnosis of cardiovascular disease in athletes. J Am Coll Cardiol. 2005 Apr 19;45(8):1322–6. doi: 10.1016/j.jacc.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Harmon KG, Asif IM, Maleszewski JJ et al. Incidence, Cause, and Comparative Frequency of Sudden Cardiac Death in National Collegiate Athletic Association Athletes: A Decade in Review. Circulation. 2015 Jul 7;132(1):10–9. doi: 10.1161/CIRCULATIONAHA.115.015431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim JH, Malhotra R, Chiampas G. Cardiac arrest during long-distance running races. N Engl J Med. 2012 Jan 12;366(2):130–40. doi: 10.1056/NEJMoa1106468. et al.; Race Associated Cardiac Arrest Event Registry (RACER) Study Group. [DOI] [PubMed] [Google Scholar]
- 16.Maron BJ, Epstein SE, Roberts WC. Causes of sudden death in competitive athletes. J Am Coll Cardiol. 1986 Jan;7(1):204–14. doi: 10.1016/s0735-1097(86)80283-2. [DOI] [PubMed] [Google Scholar]
- 17.Marijon E, Uy-Evanado A, Reinier K et al. Sudden cardiac arrest during sports activity in middle age. Circulation. 2015 Apr 21;131(16):1384–91. doi: 10.1161/CIRCULATIONAHA.114.011988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lawless CE, Olshansky B, Washington RL et al. Sports and exercise cardiology in the United States: cardiovascular specialists as members of the athlete healthcare team. J Am Coll Cardiol. 2014 Apr 22;63(15):1461–72. doi: 10.1016/j.jacc.2013.12.033. [DOI] [PubMed] [Google Scholar]
- 19.Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993 Dec 2;329(23):1677–83. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- 20.Williams PT, Thompson PD. Increased cardiovascular disease mortality associated with excessive exercise in heart attack survivors. Mayo Clin Proc. 2014 Sep;89(9):1187–94. doi: 10.1016/j.mayocp.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Chugh SS, Weiss JB. Sudden cardiac death in the older athlete. J Am Coll Cardiol. 2015 Feb 10;65(5):493–502. doi: 10.1016/j.jacc.2014.10.064. [DOI] [PubMed] [Google Scholar]
- 22.Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009 Mar 3;119(8):1085–92. doi: 10.1161/CIRCULATIONAHA.108.804617. [DOI] [PubMed] [Google Scholar]
- 23.Maron BJ, Olivotto I, Spirito P et al. Epidemiology of hypertrophic cardiomyopathy-related death: revisited in a large non-referral-based patient population. Circulation. 2000 Aug 22;102(8):858–64. doi: 10.1161/01.cir.102.8.858. [DOI] [PubMed] [Google Scholar]
- 24.Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003 Dec 3;42(11):1959–63. doi: 10.1016/j.jacc.2003.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Holst AG, Winkel BG, Theilade J et al. Incidence and etiology of sports-related sudden cardiac death in Denmark--implications for preparticipation screening. Heart Rhythm. 2010 Oct;7(10):1365–71. doi: 10.1016/j.hrthm.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 26.James CA, Bhonsale A, Tichnell C et al. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol. 2013 Oct 1;62(14):1290–7. doi: 10.1016/j.jacc.2013.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maron BJ, Thompson PD, Ackerman MJ. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2007 Mar 27;115(12):1643–455. doi: 10.1161/CIRCULATIONAHA.107.181423. et al.; American Heart Association Council on Nutrition, Physical Activity, and Metabolism. [DOI] [PubMed] [Google Scholar]
- 28.Bille K, Figueiras D, Schamasch P et al. Sudden cardiac death in athletes: the Lausanne Recommendations. Eur J Cardiovasc Prev Rehabil. 2006 Dec;13(6):859–75. doi: 10.1097/01.hjr.0000238397.50341.4a. [DOI] [PubMed] [Google Scholar]
- 29.Corrado D, Pelliccia A, Bjørnstad HH. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005 Mar;26(5):516–24. doi: 10.1093/eurheartj/ehi108. et al.; Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. [DOI] [PubMed] [Google Scholar]
- 30.Myerburg RJ, Vetter VL. Electrocardiograms should be included in preparticipation screening of athletes. Circulation. 2007 Nov 27;116(22):2616–26. doi: 10.1161/CIRCULATIONAHA.107.733519. discussion 2626. [DOI] [PubMed] [Google Scholar]
- 31.Chaitman BR. An electrocardiogram should not be included in routine preparticipation screening of young athletes. Circulation. 2007 Nov 27;116(22):2610–4. doi: 10.1161/CIRCULATIONAHA.107.711465. discussion 2615. [DOI] [PubMed] [Google Scholar]
- 32.Baggish AL, Hutter AM, Jr, Wang F et al. Cardiovascular screening in college athletes with and without electrocardiography: A cross-sectional study. Ann Intern Med. 2010 Mar 2;152(5):269–75. doi: 10.7326/0003-4819-152-5-201003020-00004. [DOI] [PubMed] [Google Scholar]
- 33.Wasfy MM, DeLuca J, Wang F et al. ECG findings in competitive rowers: normative data and the prevalence of abnormalities using contemporary screening recommendations. Br J Sports Med. 2015 Feb;49(3):200–6. doi: 10.1136/bjsports-2014-093919. [DOI] [PubMed] [Google Scholar]
- 34.Brosnan M, La Gerche A, Kalman J et al. Comparison of frequency of significant electrocardiographic abnormalities in endurance versus nonendurance athletes. Am J Cardiol. 2014 May 1;113(9):1567–73. doi: 10.1016/j.amjcard.2014.01.438. [DOI] [PubMed] [Google Scholar]
- 35.Drezner JA, Ackerman MJ, Anderson J et al. Electrocardiographic interpretation in athletes: the ‘Seattle criteria’. Br J Sports Med. 2013 Feb;47(3):122–4. doi: 10.1136/bjsports-2012-092067. [DOI] [PubMed] [Google Scholar]
- 36.Corrado D, Pelliccia A, Heidbuchel H. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J. 2010 Jan;31(2):243–59. doi: 10.1093/eurheartj/ehp473. et al.; Section of Sports Cardiology, European Association of Cardiovascular Prevention and Rehabilitation. [DOI] [PubMed] [Google Scholar]
- 37.Weiner RB, Hutter AM, Wang F et al. Performance of the 2010 European Society of Cardiology criteria for ECG interpretation in athletes. Heart. 2011 Oct;97(19):1573–7. doi: 10.1136/hrt.2011.227330. [DOI] [PubMed] [Google Scholar]
- 38.Brosnan M, La Gerche A, Kalman J et al. The Seattle Criteria increase the specificity of preparticipation ECG screening among elite athletes. Br J Sports Med. 2014 Aug;48(15):1144–50. doi: 10.1136/bjsports-2013-092420. [DOI] [PubMed] [Google Scholar]
- 39.Pelliccia A, Maron BJ, Spataro A, Proschan MA, Spirito P. The upper limit of physiologic cardiac hypertrophy in highly trained elite athletes. N Engl J Med. 1991 Jan 31;324(5):295–301. doi: 10.1056/NEJM199101313240504. [DOI] [PubMed] [Google Scholar]
- 40.Pelliccia A, Culasso F, Di Paolo FM, Maron BJ. Physiologic left ventricular cavity dilatation in elite athletes. Ann Intern Med. 1999 Jan 5;130(1):23–31. doi: 10.7326/0003-4819-130-1-199901050-00005. [DOI] [PubMed] [Google Scholar]
- 41.Weiner RB, Wang F, Berkstresser B et al. Regression of “gray zone” exercise-induced concentric left ventricular hypertrophy during prescribed detraining. J Am Coll Cardiol. 2012 May 29;59(22):1992–4. doi: 10.1016/j.jacc.2012.01.057. [DOI] [PubMed] [Google Scholar]
- 42.American College of Sports Medicine Position Stand and American Heart Association. Recommendations for cardiovascular screening, staffing, and emergency policies at health/fitness facilities. Med Sci Sports Exerc. 1998 Jun;30(6):1009–18. [PubMed] [Google Scholar]
- 43.Gibbons RJ, Balady GJ, Bricker JT et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines) J Am Coll Cardiol. 2002 Oct 16;40(8):1531–40. doi: 10.1016/s0735-1097(02)02164-2. [DOI] [PubMed] [Google Scholar]


