Abstract
Athletic heart syndrome refers to the physiological and morphological changes that occur in a human heart after repetitive strenuous physical exercise. Examples of exercise-induced changes in the heart include increases in heart cavity dimensions, augmentation of cardiac output, and increases in heart muscle mass. These cardiac adaptations vary based on the type of exercise performed and are often referred to as sport-specific cardiac remodeling. The hemodynamic effects of endurance and strength training exercise lead to these adaptations. Any abnormalities in chamber dilatation and left ventricular function usually normalize with cessation of exercise. Athletic heart syndrome is rare and should be differentiated from pathologic conditions such as hypertrophic cardiomyopathy, left ventricular noncompaction, and arrhythmogenic right ventricular dysplasia when assessing a patient for athletic heart syndrome. This paper describes specific adaptations that occur in athletic heart syndrome and tools to distinguish between healthy alterations versus underlying pathology.
Keywords: athletic heart syndrome, isotonic exercise, isometric exercise, cardiac adaptations, cardiac remodeling
Introduction
Athletic heart syndrome is an umbrella term covering various significant physiological and morphological changes that occur in a human heart after repetitive strenuous physical exercise. This type of exercise results in increased maximal oxygen uptake due to increased cardiac output and arteriovenous oxygen difference. Prolonged intensive training induces hemodynamic effects on all cardiac chambers and the aorta. Endurance exercise predominantly results in volume load on the left ventricle (LV), whereas strength exercise produces pressure load.1 The mild biventricular remodeling is seen more often in large male athletes participating in endurance sports, with the greatest degree of LV wall thickening seen in athletes of African or Afro–Caribbean origin. A clear understanding of the broad spectrum of normal cardiac adaptations to exercise is required to differentiate healthy cardiac adaptations from potentially life-threatening cardiac pathology.
Left Ventricular Adaptations in Athletic Heart Syndrome
Characteristic changes of an athlete's heart include mild LV hypertrophy and increased chamber dimensions.2,3 Cardiac output, the product of stroke volume and heart rate, may increase 5- to 6-fold during maximal exercise effort. Heart rate in the athlete may range from 40 bpm at rest to ≥ 200 bpm in a young maximally exercising athlete. Heart rate increase is responsible for the majority of cardiac output augmentation during exercise. Early studies with electrocardiography (ECG) demonstrated a high prevalence of increased cardiac voltage suggestive of LV enlargement in trained athletes.4 Subsequent work with 2-dimensional echocardiography confirmed underlying LV hypertrophy and dilation.5
To help understand the physiological mechanisms involved in various exercises, they can be broadly classified as either “isotonic” or “isometric” based on the hemodynamic mechanisms that occur during these activities. Isotonic (endurance) exercise involves sustained elevations in cardiac output with normal or reduced peripheral vascular resistance. These exercises primarily pose a volume challenge for the heart that affects all four chambers. Isometric (strength training) exercise involves activity characterized by increased peripheral vascular resistance and normal or only slightly elevated cardiac output. This increase in peripheral vascular resistance causes transient but potentially marked systolic hypertension and LV afterload. American football, weight lifting, and track and field throwing events are some examples of sports involving isometric training.
Hemodynamic conditions, specifically changes in cardiac output and peripheral vascular resistance, vary widely across different sports. A previously accepted Morganroth hypothesis was based on a study that compared M-mode echocardiographic LV measurements in wrestlers (strength training), swimmers (endurance training), and sedentary control subjects and found significant differences across these three groups. Athletes exposed to strength training demonstrated concentric LV hypertrophy, whereas individuals exposed to endurance training demonstrated eccentric LV enlargement with balanced increases in LV cavity size and wall thickness. This study led to the concept of sport-specific cardiac remodeling.6,7 Interestingly, many athletes today participate in sporting disciplines that involve a great deal of overlap between endurance and strength training.
However, subsequent studies indicated that the classification of LV hypertrophy in athletes as eccentric or concentric does not follow an absolute pattern but instead takes a relative course.8,9 Frequent combined endurance and power training (such as soccer, lacrosse, basketball, hockey, and field hockey) result in both volume and pressure load.
Although most amateur athletes have normal chamber dimensions following exercise training, in some cases pronounced LV dilation can occur.10,11 Pellicia et al. found that approximately 15% of highly trained athletes demonstrated significant LV dilation with LV chamber dimensions of > 60 mm. In their cohort of Italian athletes, the LV diastolic dimension exceeded normal values in 40% of subjects. This chamber enlargement can be accompanied by a relatively mild increase in absolute LV wall thickness that exceeds upper normal limits (from 13 to 15 mm).12 These cardiac adaptations reverse following cessation of exercise. Athletes may also show relatively small increases of wall thickness and cavity size on echocardiography. Maron et al. showed that approximately 10% to 20% of athlete hearts demonstrate a statistically significant increase in wall thickness or cavity size. Importantly, they also demonstrated that these values remain within accepted normal limits in most athletes.13 Of note, LV systolic function is usually at the low end of normal in athletes; however, with exercise they demonstrate evidence of contractile reserve with improved LV and RV function.
Figure 1.

Parasternal long axis of an athletic heart.
Use of 3-dimensional (3D) echocardiography improves assessment of left- and right-ventricular volumes and helps to characterize different cardiovascular adaptations in athletes. 3D echocardiography takes into account differences in the length and shape of the LV chamber and provides data on geometry and function of the LV as well as synchronicity of LV contraction. These variables differ in patients with hypertrophic or dilated cardiomyopathy that do not show LV harmonic remodeling.14 Studies using newer functional myocardial imaging techniques in athletes, such as tissue Doppler echocardiography and strain echocardiography, indicate that exercise training may lead to changes in LV systolic function such as normal-to-high tissue velocities and normal-to-low-normal tissue strain, respectively. These indices are not detected by assessment of a global index such as LV ejection fraction.15,16
As cardiologists, we encounter pathologies such as hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), and arrhythmogenic right ventricular dysplasia (ARVD) in our patients, some of whom may be athletes, and differentiating among these entities can be difficult. Knowledge of some morphological distinguishing characteristics can prove vital in diagnosing and managing these cases. The pattern of LV hypertrophy (LVH) may help to distinguish between pathology and an athletic heart. In the athlete's heart, LVH is almost always symmetrical. Pathology such as HCM results in asymmetric septal hypertrophy in approximately 60% and apical hypertrophy in about 10% of patients. Importantly, in an athletic heart, concomitant LVH and cavity dilatation results in preservation of LV relative wall thickness or the ratio between posterior LV wall thickness and the LV end-diastolic diameter. Patients with HCM have pathological hypertrophy that results in a reduced LV cavity size. Additionally, abnormal morphology and attachment of the papillary muscles to the mitral valve apparatus can also be observed in HCM.17 Asymmetric septal hypertrophy or abnormal attachment of the papillary muscles can both lead to systolic anterior motion of the mitral valve and LV outflow tract obstruction,18 although the latter is typically not seen in an athletic heart. Overall, the LV ejection fraction is usually low-normal to normal in athletes but hyperdynamic in HCM. A significant reduction in systolic LV function should alert the physician to the possibility of DCM, particularly if ejection fraction does not augment with exercise.
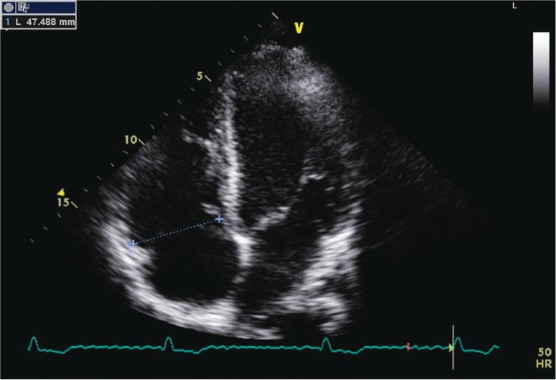
Figure 2.

Four-chamber view of an athletic heart.
Figure 3.

Normal septal tissue Doppler of an athletic heart showing e' velocities ~ 0.12 m/s.
Figure 4.

Normal lateral tissue Doppler of an athletic patient with e' of ~ 0.17 m/s.
Figure 5.

Parasternal long axis of a patient with hypertrophic cardiomyopathy.
Doppler assessment of mitral diastolic inflow patterns, tissue Doppler imaging of the LV walls, and assessment of tissue deformation can reveal impairment of relaxation and longitudinal function that usually precede the development of pathological LVH. On the contrary, early diastolic relaxation velocities are usually normal or increased in athletes with exercise-induced LVH.19 Studies by Afonso et al. have shown that global longitudinal strain (GLS) is normal in athletes and abnormal in HCM.20
The Right Ventricle
Exercise-induced cardiac remodeling is not confined to the left ventricle. Endurance exercise requires both the left and right ventricle (RV) to accept and eject relatively large quantities of blood. In the absence of significant shunting, both chambers must augment function to accomplish this task.
Figure 6.

Clip A shows a parasternal long axis of a patient with hypertrophic cardiomyopathy. Clip B shows anterior systolic motion of the anterior mitral leaflet. Clip C is M mode through the mitral valve level showing extensive left ventricular hypertrophy and systolic anterior motion. Clip D is a normal patient.
Table 1.
Echocardiographic findings comparing exercise-induced cardiac adaptations to pathology. LV: left ventricle; LVOT: left ventricular outflow tract.

Emerging data from Oxborough et al. and Teske et al.,21,22 supported by recent prospective studies, have stimulated interest in RV adaptation to exercise.23,24 Additional data have provided further insights into RV adaptation by showing that the RV has to endure a disproportionately higher increase in hemodynamic afterload compared to the LV during intense exercise.25 Right ventricular structure in collegiate endurance-trained (rowing) and strength-trained (football) athletes was recently assessed before and after 90 days of team-based exercise training. There was a statistically significant dilation of the RV in the endurance-trained athletes but not in the strength-trained athletes.26 Neilan et al. showed the dynamic nature of RV size and function in the setting of marathon running,27 and they also showed myocardial injury and ventricular dysfunction related to training levels among non-elite participants in the Boston marathon. A recently published study showed similar changes in the form of higher absolute RV diastolic area.28 These findings emphasize the notion of sports-specific alteration in RV morphology.
Figure 7.

Strain rate imaging in an athlete.
Athletic adaptations of the heart need to be differentiated from arrhythmogenic RV dysplasia (ARVD), where, unlike the symmetric remodeling and mild dilatation seen in the athlete heart, localized areas of akinesia, dyskinesia, or aneurysmal wall motion are usually seen. Newer echocardiographic techniques such as tissue deformation imaging may reveal pathological strain patterns, including regional postsystolic shortening seen in ARVD patients but not in healthy athletes.29
Atria
Left atrial remodeling is an important physiological adaptation present in highly trained athletes, most commonly those who engage in combined static and dynamic sports (i.e., cycling and rowing), and is largely explained by associated LV cavity enlargement and volume overload.30 Larger left atria were first noted in 1985 in a small study of endurance athletes.31 Another study revealed left atrial enlargement in older individuals with a significant history of exercise training.32
Figure 8.
Right ventricular dilatation seen in a marathon runner.
Pelliccia et al. showed increased transverse left atrial dimensions (≥ 40 mm) in 20% of athletes and more substantially enlarged dimensions (≥ 45 mm) in approximately 2%.30 Importantly, left atrial enlargement appeared benign and largely confined to endurance training. Despite the left atrial enlargement, atrial fibrillation is rarely associated with atrial enlargement (< 1% of athletes evaulated in a small study).33 In an athletic heart, the left atrium may measure large but should remain proportional to the LV cavity size. Atrial dilation is less likely to occur in HCM patients compared to patients with exercise-induced LV remodeling. Caselli et al. found that a left atrial transverse diameter measurement > 40 mm was highly reliable in excluding HCM (sensitivity 92% and specificity 71%).34
Aorta
The aorta experiences a significant hemodynamic load during exercise, and the nature of this load is dependent on the type of sport. Endurance activity causes high-volume aortic flow with modest systemic hypertension and strength activity, resulting in normal-volume aortic flow with potentially profound systemic hypertension. A meta-analysis by Iskandar et al. showed that elite athletes have a small but significantly larger aortic root diameter at the sinuses of Valsalva and aortic valve annulus. These differences were deemed clinically insignificant. Therefore, marked aortic root dilatation should be considered a pathological process in athletes.35
Other Imaging Modalities
In some cases, cardiac magnetic resonance imaging (CMR) may provide additional diagnostic and prognostic information, allowing for better visualization of the cardiac apex and lateral LV wall compared to standard echocardiography. Administration of gadolinium may demonstrate characteristic patterns of myocardial fibrosis in HCM and DCM.36 The cardiovascular response to exercise is a powerful discriminator between physiological changes and a pathological disease process.
In healthy individuals, the blood pressure rises during exercise as stroke volume is augmented. Individuals with cardiomyopathies such as HCM are unable to demonstrate these changes and may exhibit a flat response or even a fall in blood pressure during exercise.37 In some cases, particularly with families in which a definitive genetic mutation has already been identified, genetic testing may be considered. However, this can create challenges in terms of availability and expense, and test results generally may not be available for several weeks after ordering the exam.
Long-Term Consequences
Concern exists regarding long-term sequelae of significant LV remodeling evident in some highly trained athletes. Approximately 15% of these athletes show striking LV cavity enlargement (end-diastolic dimensions ≥ 60 mm) similar in magnitude to that evident in pathological forms of dilated cardiomyopathy. One longitudinal echocardiographic study reported incomplete reversal of extreme LV cavity dilatation with deconditioning; significant chamber enlargement persisted in 20% of retired and deconditioned former elite athletes after 5 years.38 There is no current evidence showing a correlation between an athlete's remodeled heart and long-term prognosis, cardiovascular disability, or sudden cardiac death.39
Conclusion
Athlete heart syndrome encompasses a variety of cardiac morphological changes, some of which are still not well understood. The variation from normal cardiac physiology found within the athletic population is similar to some of the other conditions discussed above. Familiarity with the differentiating factors will help discriminate at-risk individuals from those with athletic adaptations. Pathologic conditions such as HCM, DCM, and arrhythmogenic RV dysplasia are important differentials to consider when assessing a patient for athletic heart syndrome.
Figure 9.

Focused right ventricular view of a patient with arrhythmogenic right ventricular cardiomyopathy.
Figure 10.

Short axis of the left and right ventricles showing profound enlargement of the right ventricle in a patient with arrhythmogenic right ventricular cardiomyopathy.
Key Points:
Athletic heart syndrome is an umbrella term covering various significant physiological and morphological changes that occur in a human heart after repetitive strenuous physical exercise.
Isotonic (endurance) exercise poses a volume challenge for the heart, whereas isometric (strength training) exercise causes a transient pressure challenge for the heart.
Left ventricular hypertrophy, left atrial enlargement, and right ventricular enlargement may occur in the athletic heart; however, the overall heart remains proportional in size.
An athlete's heart may share similar characteristics to pathologic conditions such as HCM, DCM, and arrhythmogenic right ventricular dysplasia, and it is important to exclude these pathologic entities when assessing a patient for athletic heart syndrome.
Conflict of Interest Disclosure: The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
References
- 1.Maron BJ, Pelliccia A. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Circulation. 2006 Oct 10;114(15):1633–44. doi: 10.1161/CIRCULATIONAHA.106.613562. [DOI] [PubMed] [Google Scholar]
- 2.Maron BJ. Structural features of the athlete heart as defined by echocardiography. J Am Coll Cardiol. 1986 Jan;7(1):190–203. doi: 10.1016/s0735-1097(86)80282-0. [DOI] [PubMed] [Google Scholar]
- 3.La Gerche A, Taylor AJ, Prior DL. Athlete's heart: the potential for multimodality imaging to address the critical remaining questions. JACC Cardiovasc Imaging. 2009 Mar;2(3):350–63. doi: 10.1016/j.jcmg.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Arstila M, Koivikko A. Electrocardiographic and vectorcardiographic signs of left and right ventricular hypertrophy in endurance athletes. J Sports Med Phys Fitness. 1966 Sep;6(3):166–75. [PubMed] [Google Scholar]
- 5.Roeske WR, O'Rourke RA, Klein A, Leopold G, Karliner JS. Noninvasive evaluation of ventricular hypertrophy in professional athletes. Circulation. 1976 Feb;53(2):286–91. doi: 10.1161/01.cir.53.2.286. [DOI] [PubMed] [Google Scholar]
- 6.Morganroth J, Maron BJ, Henry WL, Epstein SE. Comparative left ventricular dimensions in trained athletes. Ann Intern Med. 1975 Apr;82(4):521–4. doi: 10.7326/0003-4819-82-4-521. [DOI] [PubMed] [Google Scholar]
- 7.Gilbert CA, Nutter DO, Felner JM, Perkins JV, Heymsfield SB, Schlant RC. Echocardiographic study of cardiac dimensions and function in the endurance-trained athlete. Am J Cardiol. 1977 Oct;40(4):528–33. doi: 10.1016/0002-9149(77)90067-4. [DOI] [PubMed] [Google Scholar]
- 8.Fagard RH. Athlete's heart: a meta-analysis of the echocardiographic experience. Int J Sports Med. 1996 Nov;17(Suppl 3):S140–4. doi: 10.1055/s-2007-972915. [DOI] [PubMed] [Google Scholar]
- 9.Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE. The athlete's heart. A meta-analysis of cardiac structure and function. Circulation. 2000 Jan 25;101(3):336–44. doi: 10.1161/01.cir.101.3.336. [DOI] [PubMed] [Google Scholar]
- 10.Utomi V, Oxborough D, Whyte GP et al. Systematic review and meta-analysis of training mode, imaging modality and body size influences on the morphology and function of the male athlete's heart. Heart. 2013 Dec;99(23):1727–33. doi: 10.1136/heartjnl-2012-303465. [DOI] [PubMed] [Google Scholar]
- 11.Pelliccia A, Culasso F, Di Paolo FM, Maron BJ. Physiologic left ventricular cavity dilatation in elite athletes. Ann Intern Med. 1999 Jan 5;130(1):23–31. doi: 10.7326/0003-4819-130-1-199901050-00005. [DOI] [PubMed] [Google Scholar]
- 12.Pelliccia A, Maron BJ, Spataro A, Proschan MA, Spirito P. The upper limit of physiologic cardiac hypertrophy in highly trained elite athletes. N Engl J Med. 1991 Jan 31;324(5):295–301. doi: 10.1056/NEJM199101313240504. [DOI] [PubMed] [Google Scholar]
- 13.Maron BJ. Structural features of the athlete heart as defined by echocardiography. J Am Coll Cardiol. 1986 Jan;7(1):190–203. doi: 10.1016/s0735-1097(86)80282-0. [DOI] [PubMed] [Google Scholar]
- 14.Vitarelli A, Capotosto L, Placanica G et al. Comprehensive assessment of biventricular function and aortic stiffness in athletes with different forms of training by three-dimensional echocardiography and strain imaging. Eur Heart J Cardiovasc Imaging. 2013 Oct;14(10):1010–20. doi: 10.1093/ehjci/jes298. [DOI] [PubMed] [Google Scholar]
- 15.Baggish AL, Yared K, Wang F et al. The impact of endurance exercise training on left ventricular systolic mechanics. Am J Physiol Heart Circ Physiol. 2008 Sep;295(3):H1109–H1116. doi: 10.1152/ajpheart.00395.2008. [DOI] [PubMed] [Google Scholar]
- 16.Cardim N, Oliveira AG, Longo S et al. Doppler tissue imaging: regional myocardial function in hypertrophic cardiomyopathy and in athlete's heart. J Am Soc Echocardiogr. 2003 Mar;16(3):223–32. doi: 10.1067/mje.2003.13. [DOI] [PubMed] [Google Scholar]
- 17.Cavalcante JL, Barboza JS, Lever HM. Diversity of mitral valve abnormalities in obstructive hypertrophic cardiomyopathy. Prog Cardiovasc Dis. 2012 May–Jun;54(6):517–22. doi: 10.1016/j.pcad.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 18.Gersh BJ, Maron BJ, Bonow RO. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011 Dec 13;58(25):e212–60. doi: 10.1016/j.jacc.2011.06.011. et al.; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. [DOI] [PubMed] [Google Scholar]
- 19.Pelà G, Bruschi G, Montagna L, Manara M, Manca C. Left and right ventricular adaptation assessed by Doppler tissue echocardiography in athletes. J Am Soc Echocardiogr. 2004 Mar;17(3):205–11. doi: 10.1016/j.echo.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Afonso L, Kondur A, Simegn M et al. Two-dimensional strain profiles in patients with physiological and pathological hypertrophy and preserved left ventricular systolic function: a comparative analyses. BMJ Open. 2012 Aug 17;2(4) doi: 10.1136/bmjopen-2012-001390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oxborough D, Sharma S, Shave R et al. The right ventricle of the endurance athlete: the relationship between morphology and deformation. J Am Soc Echocardiogr. 2012 Mar;25(3):263–71. doi: 10.1016/j.echo.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 22.Teske AJ, Prakken NH, De Boeck BW, Velthuis BK, Doevendans PA, Cramer MJ. Effect of long term and intensive endurance training in athletes on the age related decline in left and right ventricular diastolic function as assessed by Doppler echocardiography. Am J Cardiol. 2009 Oct 15;104(8):1145–51. doi: 10.1016/j.amjcard.2009.05.066. [DOI] [PubMed] [Google Scholar]
- 23.Poh KK, Ton-Nu TT, Neilan TG, Tournoux FB, Picard MH, Wood MJ. Myocardial adaptation and efficiency in response to intensive physical training in elite speedskaters. Int J Cardiol. 2008 Jun 6;126(3):346–51. doi: 10.1016/j.ijcard.2007.04.051. [DOI] [PubMed] [Google Scholar]
- 24.Baggish AL, Wang F, Weiner RB et al. Training-specific changes in cardiac structure and function: a prospective and longitudinal assessment of competitive athletes. J Appl Physiol (1985) 2008 Apr;104(4):1121–8. doi: 10.1152/japplphysiol.01170.2007. [DOI] [PubMed] [Google Scholar]
- 25.La Gerche A, Heidbüchel H, Burns AT et al. Disproportionate exercise load and remodeling of the athlete's right ventricle. Med Sci Sports Exerc. 2011 Jun;43(6):974–81. doi: 10.1249/MSS.0b013e31820607a3. [DOI] [PubMed] [Google Scholar]
- 26.King G, Wood MJ. The right ventricle of the elite high end endurance athlete cannot be underestimated. J Am Soc Echocardiogr. 2012 Mar;25(3):272–3. doi: 10.1016/j.echo.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 27.Neilan TG, Januzzi JL, Lee-Lewandrowski E et al. Myocardial injury and ventricular dysfunction related to training levels among nonelite participants in the Boston marathon. Circulation. 2006 Nov 28;114(22):2325–33. doi: 10.1161/CIRCULATIONAHA.106.647461. [DOI] [PubMed] [Google Scholar]
- 28.Utomi V, Oxborough D, Ashley E et al. The impact of chronic endurance and resistance training upon the right ventricular phenotype in male athletes. Eur J Appl Physiol. 2015 Aug;115(8):1673–82. doi: 10.1007/s00421-015-3147-3. [DOI] [PubMed] [Google Scholar]
- 29.Yoerger DM, Marcus F, Sherrill D. Echocardiographic findings in patients meeting task force criteria for arrhythmogenic right ventricular dysplasia: new insights from the multidisciplinary study of right ventricular dysplasia. J Am Coll Cardiol. 2005 Mar 15;45(6):860–5. doi: 10.1016/j.jacc.2004.10.070. et al.; Multidisciplinary Study of Right Ventricular Dysplasia Investigators. [DOI] [PubMed] [Google Scholar]
- 30.Pelliccia A, Maron BJ, Di Paolo FM et al. Prevalence and clinical significance of left atrial remodeling in competitive athletes. J Am Coll Cardiol. 2005 Aug 16;46(4):690–6. doi: 10.1016/j.jacc.2005.04.052. [DOI] [PubMed] [Google Scholar]
- 31.Hauser AM, Dressendorfer RH, Vos M, Hashimoto T, Gordon S, Timmis GC. Symmetric cardiac enlargement in highly trained endurance athletes: a two-dimensional echocardiographic study. Am Heart J. 1985 May;109(5 Pt 1):1038–44. doi: 10.1016/0002-8703(85)90247-9. [DOI] [PubMed] [Google Scholar]
- 32.Höglund C. Enlarged left atrial dimension in former endurance athletes: an echocardiographic study. Int J Sports Med. 1986 Jun;7(3):133–6. doi: 10.1055/s-2008-1025750. [DOI] [PubMed] [Google Scholar]
- 33.Mont L, Sambola A, Brugada J et al. Long-lasting sport practice and lone atrial fibrillation. Eur Heart J. 2002 Mar;23(6):477–82. doi: 10.1053/euhj.2001.2802. [DOI] [PubMed] [Google Scholar]
- 34.Caselli S, Maron MS, Urbano-Moral JA, Pandian NG, Maron BJ, Pelliccia A. Differentiating left ventricular hypertrophy in athletes from that in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2014 Nov 1;114(9):1383–9. doi: 10.1016/j.amjcard.2014.07.070. [DOI] [PubMed] [Google Scholar]
- 35.Iskandar A, Thompson PD. A meta-analysis of aortic root size in elite athletes. Circulation. 2013 Feb 19;127(7):791–8. doi: 10.1161/CIRCULATIONAHA.112.000974. [DOI] [PubMed] [Google Scholar]
- 36.O'Hanlon R, Grasso A, Roughton M et al. Prognostic significance of myocardial fibrosis in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2010 Sep 7;56(11):867–74. doi: 10.1016/j.jacc.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 37.Kawasaki T, Azuma A, Kuribayashi T et al. Vagal enhancement due to subendocardial ischemia as a cause of abnormal blood pressure response in hypertrophic cardiomyopathy. Int J Cardiol. 2008 Sep 16;129(1):59–64. doi: 10.1016/j.ijcard.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 38.Pelliccia A, Maron BJ, De Luca R, Di Paolo FM, Spataro A, Culasso F. Remodeling of left ventricular hypertrophy in elite athletes after long-term deconditioning. Circulation. 2002 Feb 26;105(8):944–9. doi: 10.1161/hc0802.104534. [DOI] [PubMed] [Google Scholar]
- 39.Maron BJ, Pelliccia A. The heart of trained athletes: cardiac remodeling and the risks of sports, including sudden death. Circulation. 2006 Oct 10;114(15):1633–44. doi: 10.1161/CIRCULATIONAHA.106.613562. [DOI] [PubMed] [Google Scholar]
- 40.Baggish AL, Yared K, Weiner RB. Differences in cardiac parameters among elite rowers and subelite rowers. Med Sci Sports Exerc. 2010 Jun;42(6):1215–20. doi: 10.1249/MSS.0b013e3181c81604. [DOI] [PubMed] [Google Scholar]


