Abstract
Although the lungs are a critical component of exercise performance, their response to exercise and other environmental stresses is often overlooked when evaluating pulmonary performance during high workloads. Exercise can produce capillary leakage, particularly when left atrial pressure increases related to left ventricular (LV) systolic or diastolic failure. Diastolic LV dysfunction that results in elevated left atrial pressure during exercise is particularly likely to result in pulmonary edema and capillary hemorrhage. Data from race horses, endurance athletes, and triathletes support the concept that the lungs can react to exercise and immersion stress with pulmonary edema and pulmonary hemorrhage. Immersion in water by swimmers and divers can also increase stress on pulmonary capillaries and result in pulmonary edema. Swimming-induced pulmonary edema and immersion pulmonary edema in scuba divers are well-documented events caused by the fluid shifts that occur with immersion, elevated pulmonary venous pressure during extreme exercise, and negative alveolar pressure due to inhalation resistance. Prevention strategies include avoiding extreme exercise, avoiding over hydration, and assuring that inspiratory resistance is minimized.
Keywords: exercise, pulmonary edema, swimming-induced pulmonary edema, SIPE, immersion pulmonary edema, IPE, diastolic dysfunction
Introduction
All forms of exercise involve an increase in whole body oxygen consumption, therefore, the cardiopulmonary system becomes a major focus for functional changes during exercise. Numerous studies on the physiology of exercise have demonstrated a clear relationship between oxygen consumption (VO2) heart rate and cardiac output, ventilatory rate and minute ventilation, energy metabolism, and lactate production.1,2 These relationships have been well defined for several decades. Recently, however, interesting effects of exercise involving swimming and water immersion and extreme aerobic exercise have provided new insights into lung function in various environments and exercise exposures.
Circulatory and Respiratory Changes with Exercise
Ventilatory responses to exercise are well defined.2 Minute ventilation increases linearly with VO2 until it approaches the anaerobic threshold, when ventilation rate increases to compensate for the metabolic acidosis created by excess lactate production.3 Cardiac output also increases linearly with VO2, but heart rate response, while linearly related to VO2 at submaximal exercise, increases disproportionately at high workloads as stroke volume falls. Recent data indicate that an important limiting factor to aerobic exercise is a rising pulmonary venous pressure at high exercise loads that causes interstitial fluid accumulation and reduced oxygen transport (Figure 1). The elevated pulmonary venous pressure is directly related to left ventricular (LV) end diastolic pressure that increases at high levels of exercise as the ventricle fails to relax adequately during diastole.4 The relationship of LV diastolic function to exercise-induced pulmonary congestion has been elucidated in several articles which show that diastolic relaxation is greater in high-capacity aerobic athletes and enhances their ability to withstand very high cardiac outputs during maximal exercise while preserving a low pulmonary venous pressure.4,5 Recent studies demonstrate a training effect on LV diastolic relaxation, indicating that high levels of aerobic exercise are possible because of improved diastolic relaxation in well-trained athletes.6,7
Figure 1.
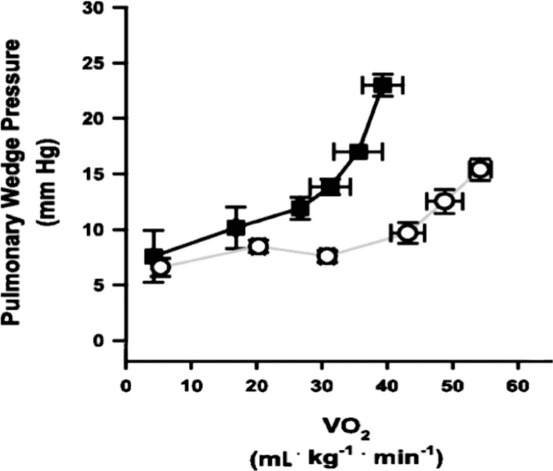
Pulmonary capillary wedge pressure (PCWP) measured during increasing exercise intensity, determined by oxygen consumption (VO2), in well-trained (circles) and average-trained (squares) men with a mean age of 29.6. Note that the well-trained subjects preserved normal levels of PCWP until they reached high levels of exercise, while the average-trained men demonstrated increases in PCWP at lower levels of exercise intensity. Adapted from Stickland et al.4
Exercise-Induced Pulmonary Hemorrhage
Veterinary observations in high-performing race horses documented pulmonary hemorrhage and pulmonary edema in some horses racing at very high speeds. West et al. examined one horse prone to exercise-induced pulmonary hemorrhage (EIPH) with measures of pulmonary pressure during exercise on a treadmill (Figure 2) and postmortem microscopy to determine the source of lung edema and hemorrhage.8,9 They found clear evidence of interstitial hemorrhage and fluid accumulation following a high workload in one horse that developed EIPH. West et al.9 suggested that two factors contributed to this problem in horses: (1) They were likely to have a congenital weakness of pulmonary capillaries that resulted in capillary rupture at high pulmonary venous and capillary pressure, and (2) they developed high pulmonary venous pressure due to failure of the left ventricle with subsequent elevation of LV end diastolic pressure during high workloads.
Figure 2.
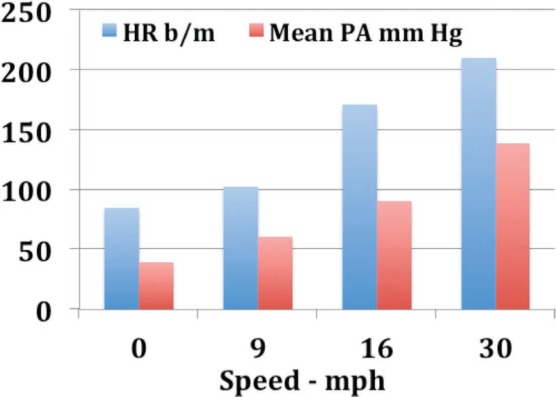
Horse with exercise-induced pulmonary hemorrhage. Heart rate (HR) and mean pulmonary pressure (PA mm Hg) from a horse with exercise-induced pulmonary hemorrhage running on a treadmill.8
Human studies of lung responses to high workloads10 corroborate the studies of West et al. to some extent. Zavorsksy et al.11 studied individuals under several different workloads and performed lung imaging to document the presence or absence of lung edema. Radiographic image readers were blinded to the exposures and reported visual evidence of lung fluid. In individuals undergoing a diagnostic graded exercise test, no evidence of lung edema was noted. However, 15% of individuals who ran on a treadmill at 70% of maximum capacity for 2 hours demonstrated evidence of pulmonary edema, as did 65% of those who ran at maximum capacity for 7 minutes. Similar findings were noted in female athletes.12 Pingitore et al. examined 48 athletes before and after completing an iron man triathlon. They used ultrasound to detect lung edema and reported the incidence of ultrasound lung comets.13 None of the athletes had evidence of lung edema before the event, while 75% showed evidence of pulmonary edema immediately post-race, and 42% had persistent findings of pulmonary edema 12 hours post-race. Their data and several case reports14–16 have demonstrated that extreme exercise can result in pulmonary edema and support the findings of West et al.9
Swimming-Induced Pulmonary Edema
Development of pulmonary edema while participating in competitive swimming events has increased in frequency over the past decade due, in part, to increased participation in triathlon events.17 Shupak et al. described the development of acute pulmonary edema in healthy, highly trained military divers who were swimming in a long-distance competitive swim.18 All were exercising at a high workload when they developed dyspnea and cough associated with production of pink frothy sputum.19 Subsequent cardiac evaluation demonstrated normal cardiac function. Since that report, numerous other reports of swimmers who developed pulmonary edema while swimming competitively have emerged.20–22 All of the military swimmers reported by Schupak et al.18 had hydrated excessively prior to swimming to avoid dehydration during their long exposure. Miller et al. reported on 70 subjects seen in their emergency department for treatment of swimming-induced pulmonary edema (SIPE).22 Significant factors found to correlate with SIPE included a history of hypertension, use of a wet suit for thermal protection, and swimming longer than one mile. Age greater than 50 years old and female gender trended toward significance in relating to SIPE. Of interest in their study was the high number of patients who were ingesting fish oil.22
Wilmshurst et al.23 described a group of swimmers and divers who developed pulmonary edema while immersed (IPE) at rest or with very low exercise activity. Symptoms included sudden onset of dyspnea and cough associated with pink frothy sputum. They compared the edema-prone individuals to a group of age- and exposure-matched individuals who had never experienced IPE.23 Individuals prone to IPE demonstrated increased blood pressure reactivity to cold, oxygen breathing, and exercise compared to the matched control group (Figure 3). The group23 hypothesized that the IPE-prone individuals develop hypertension and elevated LV end diastolic pressure when exposed to cold, increased oxygen intake, and exercise, although more recent studies show that cold exposure is not a prerequisite for developing IPE.24,25 A unique factor related to immersion in both swimming and diving is the well-documented fluid shift that occurs due to pressure effects on venous blood pooling. Hong et al.26 demonstrated a 600- to 700-mL shift of blood from the venous system into the central circulation when immersed to the neck, which in turn increases lung vascular volume and likely contributes to the development of pulmonary edema. This fluid shift can aggravate existing chronic conditions that compromise cardiac and pulmonary function. Carter et al.27 used quantitative measures of lung computed-tomographic density to identify anatomic correlates in individuals who were prone to IPE or high-altitude pulmonary edema (HAPE). They measured lung tissue density, total lung mass, and the thickness of interlobular septae. Edema-prone individuals demonstrated a lower total lung tissue mass and thinner lung septae. Gempp et al.28 found that individuals prone to IPE demonstrated a high incidence of hypertension, and Peacher et al.29 reported a variety of common clinical comorbidities in 70% of individuals who showed evidence of IPE while diving (Table 1).
Figure 3.
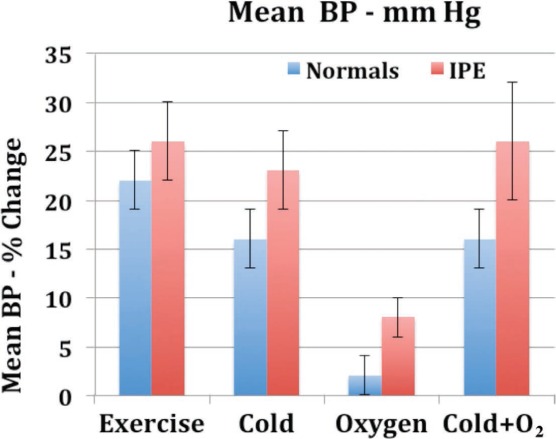
Changes in mean arterial blood pressure after exposure to exercise, cold, and increased inspired oxygen in a group of divers who experienced immersion pulmonary edema (IPE) and a group of similarly exposed divers who did not experience IPE. The IPE-prone subjects demonstrated increased blood pressure responses to all three stimuli compared to the subjects who did not experience IPE with immersion.23
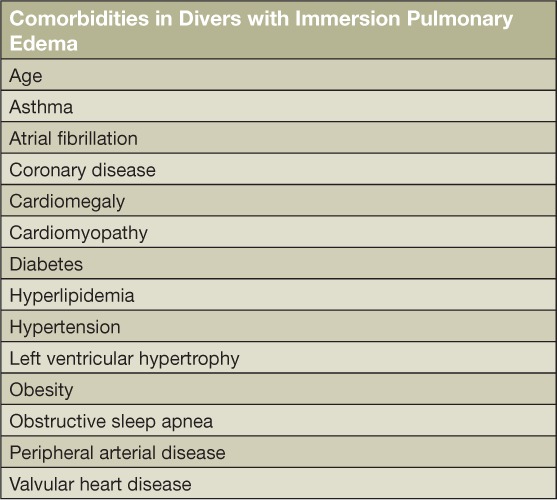
Table 1.
Comorbidities found in a group of divers who developed Immersion pulmonary edema.29
There have been reports30–32 describing the development of pulmonary edema when an individual inhales against a closed glottis (negative pressure pulmonary edema). The sharp fall in intrathoracic and intra-alveolar pressure increases the pressure gradient across the pulmonary capillary wall and can result in fluid and blood entering the interstitial and alveolar spaces. This is seen primarily in postanesthesia care where this type of dynamic situation can arise.31,32 However, a similar pressure change can occur with minor airway restriction that might be found in a mild asthmatic who is exercising at high workload, or in divers who are breathing through a device that adds inspiratory resistance—which, for example, can occur with a faulty diving regulator. Toumpanakis et al.33 studied rats with restricted airways and found a significant negative intrapulmonary pressure that resulted in interstitial and alveolar edema and evidence of inflammatory injury to lung parenchyma within 2 hours of exposure to the increased inspiratory resistance.
Breath-Hold Diving
The earliest experience of diving involved swimming underwater while breatholding.34 The “Ama” (or “sea woman”) divers of the western Pacific are excellent examples of a centuries-old tradition of commercial diving using single-breath descents to harvest food.35 While this form of underwater exposure has traditionally been used for working for brief periods of time, the development of breathing support using either self-contained or surface-supplied equipment has greatly extended the duration of time that individuals can work underwater. Breath-hold diving, however, has not disappeared and more recently has become a competitive sport that seeks to extend the depth of exposure on a single breath. To date, depths of more than 700 feet have been achieved on a single breath.36 However, data obtained from competitive breath-hold divers indicate that they sustain lung injury that involves hemoptysis, lung edema, and cough,37 and several fatalities have been reported in divers seeking to set depth records while breathholding.38–40
Boyles Law Effects on Lung Volume–Pulmonary Barotrauma
A basic physical relationship between pressure and volume of a gas was first stated by Robert Boyle in 1678.41 He described the relationship of pressure and volume for a fixed mass of an ideal gas as the product of pressure and volume as a constant (P • V = Constant). For a fixed lung volume, a diver submerged underwater with a single breath and fixed lung volume will experience a progressive reduction in lung volume as absolute pressure increases (Figure 4). At 5 atmospheres absolute pressure (a depth of 132 feet in seawater, or FSW), lung volume will be reduced to 20% of surface volume, and if residual volume (RV) is 20% of total lung capacity, lung volume will be reduced to residual volume at 132 FSW underwater. Further depth excursion will reduce lung gas volume below RV and require expansion of the lung vasculature to account for the lung volume reduction.42 One can note from Figure 4 that at 10 atmospheres absolute pressure (297 FSW), an initial lung gas volume of 5 L would be reduced to 500 mL, and lung vasculature will become engorged to account for the reduced gas space. Liner et al.43 reported lung injury in competitive breath-hold divers manifested by cough, hemoptysis, and dyspnea with reduced arterial oxygen saturation post dive. Figure 5 shows a theoretical lung volume to depth relationship that includes estimates of blood shifts into the lung vascular space. Note that at record depths for breath-hold diving (> 500 FSW), nearly a liter of blood is shifted into the lung vasculature to account for the reduced gas space. Several fatalities have been reported in extreme breath-hold divers due to massive lung injury and pulmonary hemorrhage.
Figure 4.
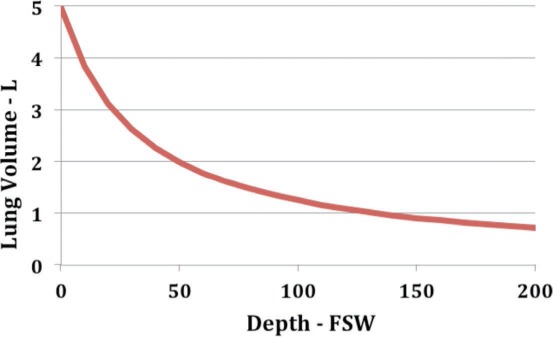
Lung volume vs depth for a breath-hold diver with total lung capacity of 5 L. If residual volume is 20% of total lung volume, at 132 FSW, lung volume will be reduced to residual volume. Further depth changes will result in blood shifting into the pulmonary vascular space to account for reduced gas volume in the lung. Note that the greatest percent volume change occurs in the first 30 feet of depth. FSW: feet seawater.
Figure 5.
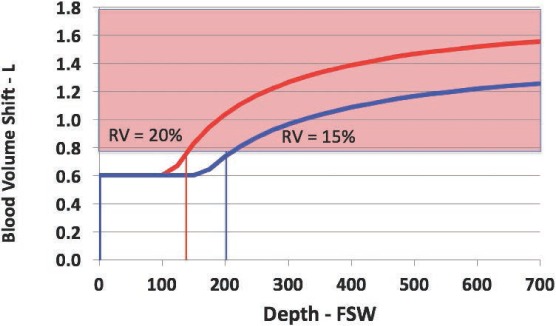
Estimated blood volume shifts vs depth during breath-hold diving. Note that an initial 600 mL of blood shifts from the venous system into the thorax due to pressure effects of immersion alone. Subsequently, based on Boyle's law reductions in lung gas volume, further blood shifts into the pulmonary vasculature will follow lung volume reduction below residual volume. Two lines show changes for a 15% and 20% residual volume fraction of total lung capacity. FSW: feet seawater.
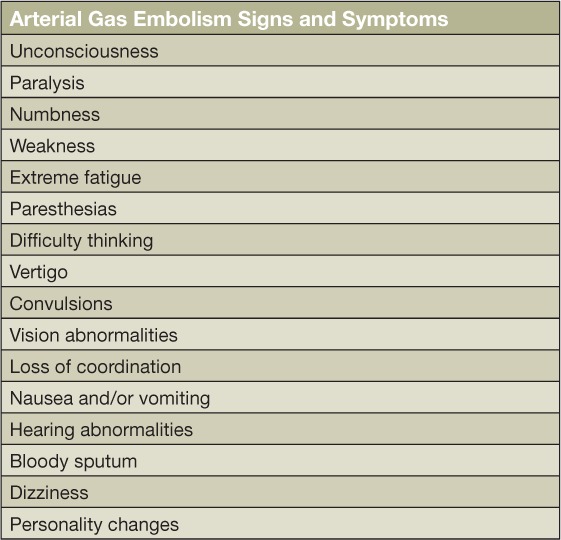
The same pressure–volume relationship can cause injury to the lung during ascent in divers who breathe compressed gas underwater. In this case, compressed air is supplied to the diver at ambient pressure to allow normal ventilation while underwater. During ascent, the compressed gas will expand according to Boyle's law, and if not properly ventilated, the expanding gas will result in lung rupture, pneumothorax, pneumomediastinum, and arterial gas embolism.44,45 The lung injury and air in the arterial system results in a number of well-defined clinical manifestations (Table 2), the most serious of which is injury to the brain due to cerebral air embolism. This syndrome produces stroke-like manifestations in a diver immediately upon ascent.46 Gas embolism to the coronary circulation can produce myocardial ischemia, and large amounts of gas filling the central circulation can obstruct blood flow through the heart and produce shock with pulseless electrical activity.47 Therapy requires treatment in a hyperbaric chamber with increased pressure to compress intra-arterial gas to a smaller, nonobstructive volume and added hyperoxygenation (known as hyperbaric oxygen therapy) to improve tissue viability.48
Table 2.
Signs and symptoms of arterial gas embolism.48
Conclusions
Sports and recreational participation can result in lung injury caused by high pulmonary pressures and increased blood volume that raises intracapillary pressure and results in capillary rupture with subsequent pulmonary edema and hemorrhage. High-intensity exercise can result in accumulation of pulmonary fluid and evidence of pulmonary edema. Competitive swimming can result in both pulmonary edema related to fluid shifts into the thorax from immersion and elevated LV end diastolic pressure related to diastolic dysfunction, particularly in the presence of high-intensity exercise. Underwater diving increases pressure and gas volume changes related to Boyle's law and can result in lung injury during descent in breath-hold diving and with ascent when breathing compressed gas underwater. The most important approach to many of these disorders is prevention. Careful attention to volume loading can reduce the risk for SIPE or IPE, while education regarding Boyle's law in breath-hold diving and compressed air diving will allow the diver to avoid lung injury related to changing gas volume. In addition, avoiding extremes of exercise will reduce the risk of exercise-induced lung injury. It is therefore important when caring for athletes to provide basic education regarding risks for lung injury and means of prevention.
Conflict of Interest Disclosure: The author has completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
Key Points
Left ventricular diastolic relaxation is a key component of aerobic fitness.
Extreme high-intensity exercise can cause transient pulmonary edema.
Triathletes can develop pulmonary edema during the swimming phase of the event due to fluid shifts related to immersion, high-intensity exercise, and impaired diastolic relaxation.
Scuba divers can experience pulmonary edema related to immersion that causes severe dyspnea while underwater.
Breath-hold diving to very deep depths can cause severe lung injury.
References
- 1.Saltin B. Hemodynamic adaptations to exercise. Am J Cardiol. 1985 Apr 26;55(10):42D–47D. doi: 10.1016/0002-9149(85)91054-9. [DOI] [PubMed] [Google Scholar]
- 2.Katz A, Sahlin K. Regulation of lactic acid production during exercise. J Appl Physiol (1985) 1988 Aug;65(2):509–18. doi: 10.1152/jappl.1988.65.2.509. [DOI] [PubMed] [Google Scholar]
- 3.Whipp BJ, Wasserman K. Effect of anaerobiosis on the kinetics of O2 uptake during exercise. Fed Proc. 1986 Dec;45(13):2942–7. [PubMed] [Google Scholar]
- 4.Stickland MK, Welsh RC, Petersen SR et al. Does fitness level modulate the cardiovascular hemodynamic response to exercise? J Appl Physiol. 2006;100:1895–1901. doi: 10.1152/japplphysiol.01485.2005. [DOI] [PubMed] [Google Scholar]
- 5.Zilinski JL, Contursi ME, Isaacs SK et al. Myocardial adaptations to recreational marathon training among middle-aged men. Circ Cardiovasc Imaging. 2015 Feb;8(2):e002487. doi: 10.1161/CIRCIMAGING.114.002487. [DOI] [PubMed] [Google Scholar]
- 6.Brinker SK, Pandey A, Ayers CR et al. Association of cardiorespiratory fitness with left ventricular remodeling and diastolic function: the Cooper Center Longitudinal Study. JACC Heart Fail. 2014 Jun;2(3):238–46. doi: 10.1016/j.jchf.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuchynka P, Palecek T, Vilikus Z et al. Cardiac structural and functional changes in competitive amateur cyclists. Echocardiography. 2010 Jan;27(1):11–16. doi: 10.1111/j.1540-8175.2009.00965.x. [DOI] [PubMed] [Google Scholar]
- 8.West JB, Mathieu-Costello O, Jones JH et al. Stress failure of pulmonary capillaries in racehorses with exercise-induced pulmonary hemorrhage. J Appl Physiol (1985) 1993 Sep;75(3):1097–109. doi: 10.1152/jappl.1993.75.3.1097. [DOI] [PubMed] [Google Scholar]
- 9.West JB. Invited review: pulmonary capillary stress failure. J Appl Physiol. 2000;89:2483–9. doi: 10.1152/jappl.2000.89.6.2483. [DOI] [PubMed] [Google Scholar]
- 10.Hopkins SR. Point: Pulmonary edema does occur in human athletes performing heavy sea-level exercise. J Appl Physiol. 2010;109:1270–2. doi: 10.1152/japplphysiol.01353.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zavorsky GS. Evidence of pulmonary oedema triggered by exercise in healthy humans and detected with various imaging techniques. Acta Physiol (Oxf) 2007;189:305–17. doi: 10.1111/j.1748-1716.2006.01660.x. [DOI] [PubMed] [Google Scholar]
- 12.Zavorsky GS, Saul L, Decker A, Ruiz P. Radiographic evidence of pulmonary edema during high-intensity interval training in women. Respir Physiol Neurobiol. 2006 Sep 28;153(2):181–90. doi: 10.1016/j.resp.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Pingitore A, Garbella E, Piaggi P et al. Early subclinical increase in pulmonary water content in athletes performing sustained heavy exercise at sea level: ultrasound lung comet-tail evidence. Am J Physiol Heart Circ Physiol. 2011 Nov;301(5):H2161–7. doi: 10.1152/ajpheart.00388.2011. [DOI] [PubMed] [Google Scholar]
- 14.Stefanko G, Lancashire B, Coombes JS, Fassett RG. Pulmonary oedema and hyponatraemia after an ironman triathlon. BMJ Case Rep. 2009;2009 doi: 10.1136/bcr.04.2009.1764. pii: bcr04.2009.1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wellershoff G. Hyponatremic encephalopathy with non-cardiogenic pulmonary edema. Development following marathon run. Med Klin Intensivmed Notfmed. 2013;108:234–7. doi: 10.1007/s00063-012-0198-7. [DOI] [PubMed] [Google Scholar]
- 16.Boggio-Alarco JL, Jaume-Anselmi F, Ramirez-Rivera J. Acute pulmonary edema during a triathlon occurrence in a trained athlete. Bol Asoc Med P R. 2006 Apr–Jun;98(2):110–3. [PubMed] [Google Scholar]
- 17.Dähler P, Rüst CA, Rosemann T, Lepers R, Knechtle B. Nation related participation and performance trends in ‘Ironman Hawaii’ from 1985 to 2012. BMC Sports Sci Med Rehabil. 2014 Apr 15;6:16. doi: 10.1186/2052-1847-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shupak A, Weiler-Ravell D, Adir Y, Daskalovic YI, Ramon Y, Kerem D. Pulmonary oedema induced by strenuous swimming: a field study. Respir Physiol. 2000 Jun;121(1):25–31. doi: 10.1016/s0034-5687(00)00109-2. [DOI] [PubMed] [Google Scholar]
- 19.Adir Y, Shupak A, Gil A et al. Swimming-induced pulmonary edema: clinical presentation and serial lung function. Chest. 2004 Aug;126(2):394–9. doi: 10.1378/chest.126.2.394. [DOI] [PubMed] [Google Scholar]
- 20.Lund KL, Mahon RT, Tanen DA, Bakhda S. Swimming-induced pulmonary edema. Ann Emerg Med. 2003 Feb;41(2):251–6. doi: 10.1067/mem.2003.69. [DOI] [PubMed] [Google Scholar]
- 21.Mahon RT, Kerr S, Amundson D, Parrish JS. Immersion pulmonary edema in special forces combat swimmers. Chest. 2002 Jul;122(1):383–4. doi: 10.1378/chest.122.1.383-a. [DOI] [PubMed] [Google Scholar]
- 22.Miller CC, 3rd, Calder-Becker K, Modave F. Swimming-induced pulmonary edema in triathletes. Am J Emerg Med. 2010 Oct;28(8):941–6. doi: 10.1016/j.ajem.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Wilmshurst PT, Nuri M, Crowther A, Webb-Peploe MM. Cold-induced pulmonary oedema in scuba divers and swimmers and subsequent development of hypertension. Lancet. 1989 Jan 14;1(8629):62–5. doi: 10.1016/s0140-6736(89)91426-8. [DOI] [PubMed] [Google Scholar]
- 24.Hampson NB, Dunford RG. Pulmonary edema of scuba divers. Undersea Hyperb Med. 1997;24(1):29–33. [PubMed] [Google Scholar]
- 25.Slade JB, Jr, Hattori T, Ray CS, Bove AA, Cianci P. Pulmonary edema associated with scuba diving: case reports and review. Chest. 2001 Nov;120(5):1686–94. doi: 10.1378/chest.120.5.1686. [DOI] [PubMed] [Google Scholar]
- 26.Hong SK, Cerretelli P, Cruz JC et al. Mechanics of respiration during submersion in water. J Appl Physiol. 1969;27:537–8. doi: 10.1152/jappl.1969.27.4.535. [DOI] [PubMed] [Google Scholar]
- 27.Carter EA, Mayo JR, MacInnis MJ, McKenzie DC, Koehle MS. Individual susceptibility to high altitude and immersion pulmonary edema and pulmonary lymphatics. Aviat Space Environ Med. 2014 Jan;85(1):9–14. doi: 10.3357/asem.3736.2014. [DOI] [PubMed] [Google Scholar]
- 28.Gempp E, Demaistre S, Louge P. Hypertension is predictive of recurrent immersion pulmonary edema in scuba divers. Int J Cardiol. 2014 Mar 15;172(2):528–9. doi: 10.1016/j.ijcard.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 29.Peacher DF, Martina SD, Otteni CE, Wester TE, Potter JF, Moon RE. Immersion pulmonary edema and comorbidities: case series and updated review. Med Sci Sports Exerc. 2015 Jun;47(6):1128–34. doi: 10.1249/MSS.0000000000000524. [DOI] [PubMed] [Google Scholar]
- 30.Udeshi A, Cantie SM, Pierre E. Postobstructive pulmonary edema. J Crit Care. 2010 Sep;25(3):508.e1–5. doi: 10.1016/j.jcrc.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 31.Lang SA, Duncan PG, Shephard DA et al. Pulmonary oedema associated with airway obstruction. Can J Anaesth. 1990 Mar;37(2):210–8. doi: 10.1007/BF03005472. [DOI] [PubMed] [Google Scholar]
- 32.Chuang YC, Wang CH, Lin YS. Negative pressure pulmonary edema: report of three cases and review of the literature. Eur Arch Otorhinolaryngol. 2007 Sep;264(9):1113–6. doi: 10.1007/s00405-007-0379-9. [DOI] [PubMed] [Google Scholar]
- 33.Toumpanakis D, Kastis GA, Zacharatos P et al. Inspiratory resistive breathing induces acute lung injury. Am J Respir Crit Care Med. 2010 Nov 1;182(9):1129–36. doi: 10.1164/rccm.201001-0116OC. [DOI] [PubMed] [Google Scholar]
- 34.Frost FJ. Scyllias: Diving in Antiquity. Greece and Rome (Second Series) 1968 Oct;15(2):180–5. [Google Scholar]
- 35.Mohri M, Torii R, Nagaya K et al. Diving patterns of ama divers of Hegura Island, Japan. Undersea Hyperb Med. 1995 Jun;22(2):137–43. [PubMed] [Google Scholar]
- 36.Nestor J. Deep: Freediving, Renegade Science, and What the Ocean Tells Us About Ourselves. Boston: Houghton Mifflin Harcourt; 2014 Jun 24. p. 272. p. [Google Scholar]
- 37.Lindholm P, Lundgren CE. The physiology and pathophysiology of human breath-hold diving. J Appl Physiol (1985) 2009 Jan;106(1):284–92. doi: 10.1152/japplphysiol.90991.2008. [DOI] [PubMed] [Google Scholar]
- 38.Dujic Z, Breskovic T. Impact of breath holding on cardiovascular respiratory and cerebrovascular health. Sports Med. 2012 Jun 1;42(6):459–72. doi: 10.2165/11599260-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 39.Landsberg PG. Hyperventilation: An unpredictable danger to the sports diver. In: Lundgren CEG, Ferrigno M, editors. The physiology of breath-hold diving. Bethesda, MD: Undersea and Hyperbaric Medical Society; 1987. pp. 256–67. p. [Google Scholar]
- 40.Cialoni D, Sponsiello N, Marabotti C et al. Prevalence of acute respiratory symptoms in breath-hold divers. Undersea Hyperb Med. 2012 Jul–Aug;39(4):837–44. [PubMed] [Google Scholar]
- 41.Boyle R. New Experiments Physico-Mechanical. Touching the Air. Oxford: Oxford University Press; 1662. Defence of the Doctrine Touching the Spring and the Weight of the Air. [Google Scholar]
- 42.Craig AB., Jr. Depth limits of breath hold diving (an example of Fennology) Respir Physiol. 1968;5:14–22. doi: 10.1016/0034-5687(68)90073-x. [DOI] [PubMed] [Google Scholar]
- 43.Linér MH, Andersson JP. Pulmonary edema after competitive breath-hold diving. J Appl Physiol (1985) 2008 Apr;104(4):986–90. doi: 10.1152/japplphysiol.00641.2007. [DOI] [PubMed] [Google Scholar]
- 44.Schaefer KE, McNulty WP, Carey C et al. Mechanisms in development of interstitial emphysema and air embolism on decompression from depth. J Appl Physiol. 1958;13:15–29. doi: 10.1152/jappl.1958.13.1.15. [DOI] [PubMed] [Google Scholar]
- 45.Calder IM. Autopsy and experimental observations on factors leading to barotrauma in man. Undersea Biomed Res. 1985;12:165–82. [PubMed] [Google Scholar]
- 46.Polak B, Adams H. Traumatic air embolism in submarine escape training. US Naval Med Bull. 1932;30:165–77. [Google Scholar]
- 47.Neuman TS, Jacoby I, Bove AA. Fatal pulmonary barotrauma due to obstruction of the central circulation with air. J Emerg Med. 1998 May–Jun;16(3):413–7. doi: 10.1016/s0736-4679(98)00006-7. [DOI] [PubMed] [Google Scholar]
- 48.Navy Department: U. S. Navy Diving Manual, Vol 5. Washington, D.C.: U.S. Navy Department; 2008. Chapter 20, Diagnosis and treatment of decompression sickness and arterial gas embolism. (Publication No. NAVSEA 0910-LP-106–0957) [Google Scholar]


