Abstract
Older adults represent the fastest-growing age demographic of the population. Physiological changes associated with primary aging and concurrent chronic disease adversely impact functional capacity, health outcomes, and quality of life. For these reasons, there is a national emphasis for healthcare providers to improve the health, function, and quality of life of older adults to preserve independent living and psychological well-being. The benefits of regular physical activity or exercise with regard to aging and disease are indisputable, yet many clinicians do not prescribe exercise to older adults. This reluctance may be attributable to a lack of knowledge regarding appropriate exercise prescription for older adults in light of the potential risks and benefits of various doses and types of exercise. In addition, clinicians and patients may have concerns about potential health considerations relevant to older adults such as comprehensive pre-exercise screening and exercise-drug interactions. In light of this, the following review presents (1) guidelines for exercise prescription in older adults and modification of these guidelines for patients with the most common age-associated comorbidities; (2) recommendations for pre-exercise screening prior to initiating an exercise program in older adults; (3) considerations for older adults on one or more medications; and (4) common barriers to adopting and maintaining exercise in an older population. Our goal is to provide a framework that clinicians can follow when prescribing exercise in older adults while considering the unique characteristics and concerns present in this population.
Keywords: elderly, exercise training, health promotion, physical activity, exercise prescription
Introduction
Older adults are among the fastest growing age groups in the United States, with more than 47 million adults ≥ 65 years old.1 It is projected that by the year 2030, the number of individuals aged 65 years and over will reach 74 million, making those aged 85 years and older the fastest-growing segment of our population.1 Presently, two out of every three older adults manage multiple chronic conditions, and treatment for these conditions accounts for 66% of the country's health care budget.2 Accordingly, the U.S. government's Healthy People 2020 initiative has set measureable objectives to be achieved by the year 2020, with the overarching goal to “improve the health, function, and quality of life of older adults.”3 While participation in a regular exercise training program is a cost-effective intervention with known health benefits to improve health, delay physical dysfunction, and prevent/treat chronic disease among older adults,4 only 22% of adults ≥ 65 years meet the recommendations for physical activity.5 On the provider side, older adults have the ability to adapt and respond to both aerobic and strength training,4 yet only 32% of clinicians deliver exercise counseling or education to older adults during an office visit.6
Because the majority of risk factors associated with chronic disease increase with age, the adoption of regular physical activity is essential to buffer the functional declines associated with aging and to improve health outcomes and disability among older adults.4 Therefore, it is vital that clinicians understand the unique aspects surrounding exercise prescription in older adults so that effective recommendations and clinical interventions can be designed to maximize benefit among the fastest-growing segment of our population.
The following review presents guidelines for exercise prescription in older adults, the rationale for pre-exercise screening prior to initiating an exercise program in older adults, modification of an exercise prescription for patients with the most common age-associated comorbidities, considerations for older adults on one or more medications, and common barriers to adopting and maintaining exercise in an older population. The overall purpose is to provide a framework for clinicians to follow for the prescription of exercise in older adults while keeping in mind the unique characteristics and concerns present in this population.
Exercise Prescription for Older Adults
An exercise prescription (ExRx) is a recommended physical activity program designed in a systematic and individualized manner in terms of the Frequency, Intensity, Time, Type, Volume, and Progression, known as the FITT-VP principle. The American College of Sports Medicine's (ACSM) general ExRx recommendations for adults ≥ 65 years are detailed in Table 1.7 Of note, these guidelines also apply to individuals aged 50 to 64 years with clinically significant conditions or physical limitations that affect movement. Deconditioning, low muscle tone, and/or low functional capacity contribute to poor health outcomes and low quality of life4; therefore, the ACSM recommends that older adults engage in a combination of aerobic, resistance, flexibility, and balance training to promote and maintain health.7 Specifically, the ACSM recommends the following FITT-VP ExRx7 for older adults:
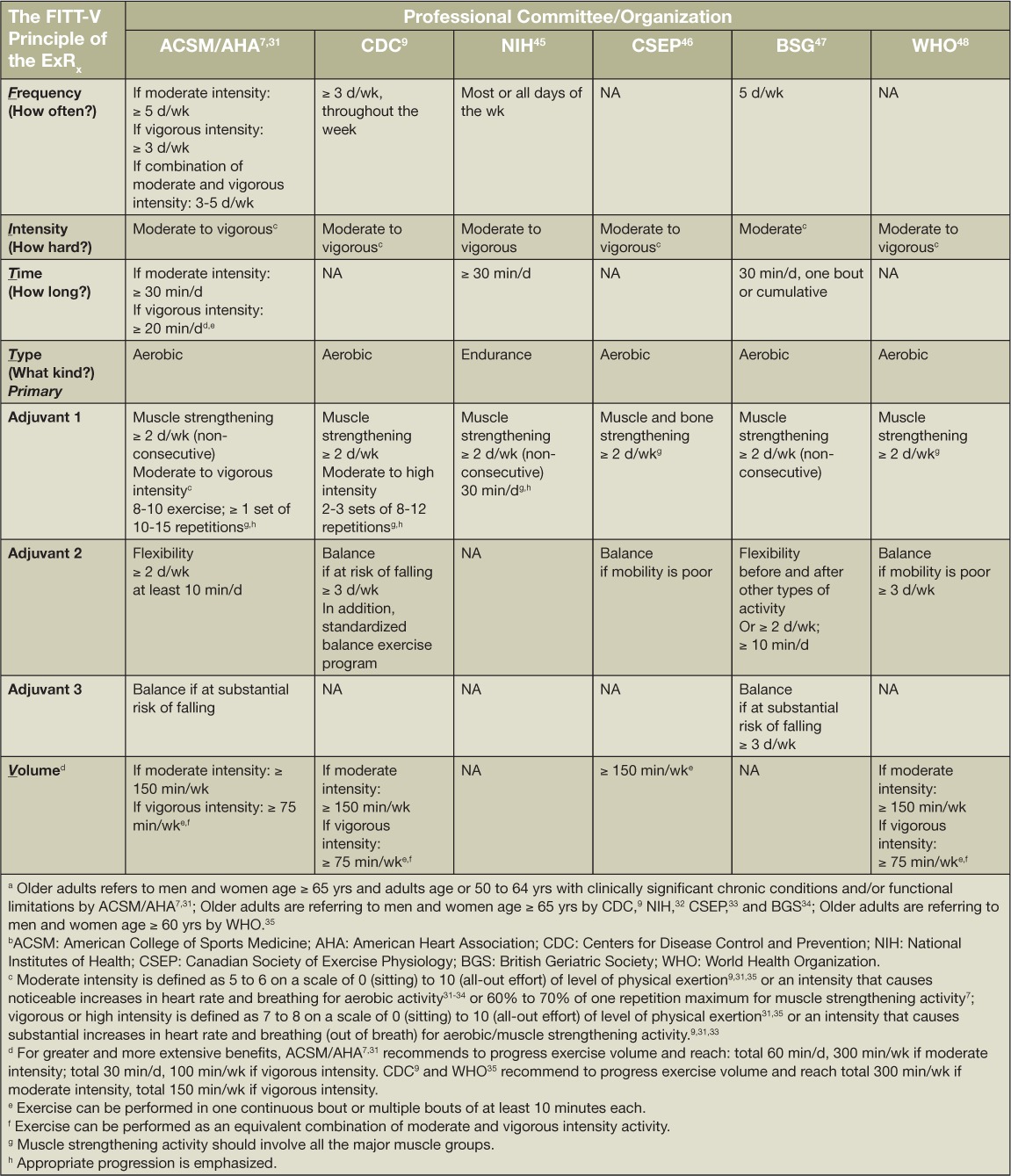
Table 1.
Exercise prescription guidelines, scientific statements, and recommendations for older adults a by the various professional committees and organizations. b FITT-V: Frequency, Intensity, Time, Type, and Volume of the exercise prescription; ExRx: exercise prescription; NA: not available.
Frequency: ≥ 5 days per week (d/wk) for moderate-intensity aerobic exercise (or ≥ 3 d/wk for vigorous-intensity aerobic exercise, or 3 to 5 d/wk for a combination of moderate- and vigorous-intensity exercise) supplemented by resistance exercise ≥ 2 d/wk and flexibility exercise ≥ 2 d/wk.
Intensity: On a scale of 0–10 for level of physical exertion, 5–6 for moderate-intensity aerobic exercise, 7–8 for vigorous-intensity aerobic exercise, and 5–6 for moderate-intensity resistance exercise.
Time: A minimum of 30 minutes or up to 60 minutes per day (m/d) for moderate intensity aerobic exercise or at least 20 to 30 m/d for vigorous intensity aerobic exercise.
Type: Emphasis should be placed on aerobic activities that do not impose excessive orthopedic stress, such as walking. Resistance training may supplement as an adjuvant to aerobic training and should consist of 8 to 10 different exercises targeting the major muscle groups. Flexibility exercise training is recommended ≥ 2 d/wk holding each muscle 30 to 60 seconds. Balance (neuromotor) training is also recommended 2 to 3 d/wk in individuals at high risk for fall.
Volume: Should total 150 m/wk of moderate intensity exercise or 75 m/wk of combined moderate- and vigorous-intensity exercise.
Progression: The FITT components may be increased, as tolerated, to achieve the recommended volume, up to 300 m/wk of moderate-intensity aerobic exercise or 100 m/wk of vigorous-intensity aerobic exercise. Progression may be individualized based on tolerance and preference in a conservative manner.
The ACSM is considered the gold standard for exercise recommendations. Other organizations with formal recommendations for the optimal ExRx for older adults present with slight but notable departures from the ACSM (Table 1). Despite the small differences in the FITT of the recommended prescriptions in Table 1, the overall consensus is for older adults to participate in 30 m/d or more of moderate-intensity aerobic exercise for at least 3 to 5 d/wk to total 150 m/wk and to supplement with resistance, flexibility, and balance exercise training.
Exercise Preparticipation Health Screening Recommendations
Before any older adult adopts a new or increases an existing structured exercise program, appropriate preparticipation health screening should be implemented to identify at-risk individuals who may require medical clearance before they begin an exercise program. Although exercise is safe for most individuals, there is a small but measureable acute risk of cardiovascular complications in certain susceptible individuals. The risk for acute exercise-related cardiovascular events are highest among sedentary adults with known or underlying cardiovascular disease (CVD) who perform unaccustomed vigorous-intensity exercise.8 Therefore, the goal of preparticipation health screening is to assess and mitigate this risk but not to present unnecessary obstacles or excessive burden on the individual or clinician (i.e., unwarranted referrals, false-positive exercise stress tests, invasive diagnostic testing).8
The ACSM has recently updated their preparticipation health screening recommendations using an evidence-informed model with the goal of eliminating possible barriers to exercise8 and emphasizing the U.S. Surgeon General's message that regular physical activity is important for all individuals.9 It is notable that age is no longer a consideration for aerobic exercise participation. In addition, the new guidelines focus on (1) the current level of exercise, (2) presence or absence of asymptomatic/symptomatic known disease, and (3) desired intensity of exercise.8 Following the ACSM preparticipation health screening logic model, individuals are initially triaged based on the current level of exercise, in which “physically active” is defined as one who engages in planned, structured physical activity at least 30 minutes at moderate intensity on at least 3 d/wk for at least the last 3 months.
Physically active: Physically active asymptomatic individuals with known cardiovascular, metabolic, or renal disease whose health care provider has cleared them to exercise within the last 12 months do not need to revisit their health care provider to continue a moderate-intensity exercise program unless they develop resting or exertional symptoms of cardiovascular, metabolic, or renal disease or experience a change in health status. However, physically active individuals who develop signs or symptoms of cardiovascular, metabolic, or renal disease should discontinue exercise and seek medical clearance before resuming exercise of any intensity.8
Physically inactive: Physically inactive but otherwise healthy asymptomatic persons may begin light- to moderate-intensity exercise without medical clearance and, in the absence of symptoms, progress gradually in intensity as recommended by current ACSM exercise prescription guidelines.7 Physically inactive individuals with known cardiovascular, metabolic, or renal disease and/or those with signs or symptoms suggestive of these diseases should seek medical clearance before starting an exercise program, regardless of the intensity.8
Older adults may benefit from counseling on how to quantify subjective intensity and recognize limiting signs or symptoms. Light-intensity exercise is defined as an intensity that causes slight increases in heart rate (HR) and breathing; moderate intensity causes noticeable increases in HR and breathing; and vigorous intensity causes substantial increases in HR and breathing.8 Signs and symptoms that are suggestive of cardiovascular, metabolic, or renal disease and may necessitate the need for medical clearance are shortness of breath at rest or with mild exertion, chest discomfort of any type, dizziness or syncope, orthopnea or paroxysmal nocturnal dyspnea, ankle edema, palpitations or tachycardia, intermittent claudication, known heart murmur, or unusual fatigue or shortness of breath with usual activities.8
Due to a lack of evidence that exercise testing is effective in mitigating the risk of exercise-related cardiovascular events,100 general exercise testing guidelines are no longer universally endorsed. Rather, clinicians are encouraged to evaluate the need for medical examination, exercise stress test, or diagnostic imaging using their own clinical judgment and on an individualized basis.
Special Considerations in Exercise Prescription
Chronic diseases and comorbidities such as CVD, cancer, diabetes, and chronic lower respiratory infections are the leading causes of death among older adults.11 Two of three older adults have multiple chronic conditions, and medical treatment for this population accounts for 66% of the U.S. health care budget.2 Exercise has been shown to be an effective lifestyle therapy for most chronic conditions such as hypertension,12,13 type 2 diabetes,14 and chronic obstructive pulmonary disease.15 Special considerations or modifications to the FITT-VP principle of ExRx should be considered in the treatment paradigm for a given chronic disease or condition, but it should not replace good clinical judgment. The ACSM currently has 18 published ExRx for special populations that may be relevant for older adults. These include those with arthritis, cancer, cardiovascular and cerebrovascular disease, cerebral palsy, diabetes mellitus, dyslipidemia, human immunodeficiency virus, hypertension, intellectual disability and Down syndrome, kidney disease, metabolic syndrome, multiple sclerosis, osteoporosis, overweight and obesity, Parkinson's disease, peripheral artery disease, pulmonary diseases, and spinal cord injury.7
Table 2 presents an example of FITT-VP modifications for the top four leading medical conditions (hypertension, type 2 diabetes, dyslipidemia, and arthritis) based on prevalence, Medicare utilization, and spending for the years 2008–2012.16 As an example, consider a case study of a 67-year-old man with hypertension (146/92 mm Hg) seeking to initiate an exercise program in an effort to better control his blood pressure (BP). Modifications to the FITT ExRx for an older adult with hypertension can be made to maximize health benefits for this particular individual. Referring to Table 2, we can see that the recommendations surrounding flexibility, resistance, and balance training remain the same as the older adult ExRx previously outlined. However, in the setting of hypertension, substantial emphasis should now be placed on the FIT for aerobic exercise training due to the established BP-lowering effects of aerobic exercise. Aerobic exercise training has been shown to reduce resting BP by 5 to 7 mm Hg in individuals with hypertension.17 Specifically, the ACSM recommends the following FIT, aerobic ExRx modifications for individuals with hypertension7:
Table 2.
Exercise prescription modifications and special considerations for common medical conditions in older adults. FITT: Frequency, Intensity, Time, and Type of the exercise prescription; ExRx: exercise prescription
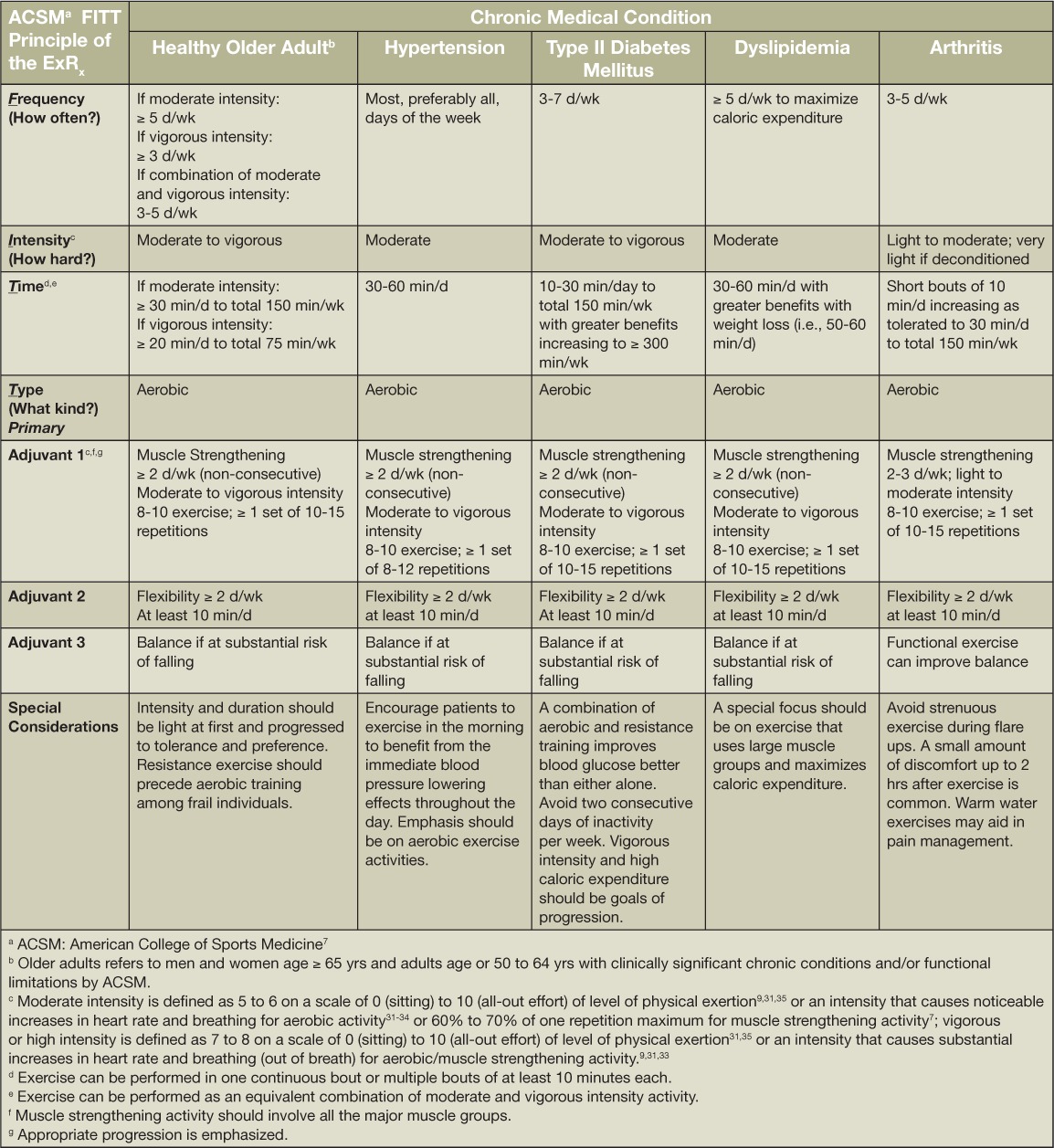
Frequency: Aerobic exercise on most and preferably all days of the week (as opposed to 3–5 d/wk). This recommendation is made due to the immediate and sustained BP-lowering effects of acute aerobic exercise (i.e., postexercise hypotension; PEH).18,19 In other words, BP is lower on days when individuals with hypertension exercise than when they do not exercise.
Intensity: Moderate-intensity remains the suggested intensity of aerobic exercise. However, due to emerging evidence that greater BP reductions can be achieved with greater levels of physical exertion,18 vigorous-intensity aerobic exercise may be more beneficial for the patient assuming they are able to tolerate higher levels of physical exertion;
Time: Recommended time is 30 to 60 min/d of continuous or intermittent aerobic exercise. If intermittent, bouts should be at least 10 min in duration. This recommendation is consistent with the emerging evidence that PEH is a low-threshold phenomenon regarding the time of the acute exercise bout, and several short bouts of intermittent exercise may be a viable therapeutic lifestyle option for BP control among individuals with hypertension.18
Pharmacological Interactions with Exercise
An additional consideration for ExRx in older adults is the use of concomitant medications that may influence physical activity and alter exercise tolerance. An obvious example is the risk of hypotension following a bout of aerobic exercise in older adults who are prescribed multiple BP-lowering drugs to treat chronic hypertension. Since aerobic exercise evokes an acute drop in BP (i.e., PEH), older adults on several antihypertensive medications may experience a more significant drop in BP with exercise, evoking a transient orthostatic intolerance that translates into balance disturbance and increased fall risk. By contrast, however, recent evidence finds that certain medications, in conjunction with exercise, facilitate greater improvements in health outcomes and risk factors than with exercise alone—such as combining aerobic exercise training with antihypertensive drug use.13 Therefore, clinicians and patients need to carefully weigh the benefits and adverse side effects of medication use within each individual's ExRx.
The use of statin therapy in older adults illustrates the need for this nuanced assessment when weighing the benefits and risks of drug therapy against exercise efficacy and safety. Data suggest that the combination of exercise training and cholesterol-lowering drugs may be most beneficial for patients with elevated low-density lipoprotein cholesterol (LDL-C). For example, after 12 weeks of resistance training in older adults, LDL-C was reduced on average by 18 mg/dL and further lowered by another 12 mg/dL with the concurrent use of cholesterol-lowering drugs.20 Similarly, an analysis of more than 10,000 veterans21 found that while both high fitness and statin drug use decreased mortality risk, individuals who were both highly fit and taking a statin had the lowest mortality risk of any study participants. This was above and beyond the benefits achieved with fitness or statin therapy alone.
However, statins may potentially have adverse effects on routine physical activity. The most frequently experienced statin side effect is muscle complaints (i.e., cramping, myalgia, soreness, and weakness), occurring in approximately 5% to 10% of patients,22 and these statin-related side effects can negatively impact medication compliance and physical activity. These muscle complaints may also be exacerbated by exercise. Several reports indicate that athletes and/or physically active individuals are less likely to tolerate statin therapy.23 In addition, the muscle damage associated with downhill and marathon running is augmented by concurrent statin therapy,24,25 which may have implications for master's athletes being treated with statins. Therefore, certain susceptible older adults may experience reduced benefit from the interactions between exercise and statin therapy and may need to tailor their doses accordingly. Weighing the benefits and side effects of statin use illustrates the need for clinician and patient discretion when considering pharmacological interventions alone, in conjunction with, and as a barrier to physical activity in older adults.
Barriers and Motivation for Exercise Adherence
Approximately 87% of older adults have at least one barrier to exercise participation,26 including low self-efficacy, fear of injury, lack of social support, and social isolation.7 However, pain (i.e., fear of pain or exacerbation of existing pain) is often reported as the most common barrier among older adults.27 Because of the increased rates of social isolation and depression, group-based exercise has been shown to be more effective for long-term adherence than home-based individual exercise programs in older adults.28 Exercise Rx approaches that encompass education, positive social support, and behavior theories to promote exercise and build self-efficacy—for example, health belief model, theory of planned behavior—are necessary to improve exercise adherence among older adults and optimize health through physical fitness.
Conclusion
Physical activity is a complex behavior with myriad physiological and environmental determinants that are unique to older adults. Despite known barriers, older adults have the ability to adapt and respond to both aerobic and strength training, but only 32% of clinicians deliver exercise counseling or education to older adults.6 Initiatives such as the ACSM's Exercise is Medicine campaign encourages healthcare providers to (1) record physical activity as a vital sign, and (2) prescribe exercise as they might a medication for patients.29 Initiatives such as these have been shown to increase exercise participation 6-fold when compared to adults not receiving exercise counseling.30 In general, older adults can be encouraged to participate in 30 min/d or more of moderate-intensity aerobic exercise 3 to 5 d/wk to total 150 min/wk and supplement with resistance, flexibility, and balance training ≥ 2 d/wk. Given the known efficacy of exercise to improve health and treat chronic disease, it is imperative for clinicians to understand the multifaceted nature of exercise in older adults so that effective ExRx can be designed that maximize benefit among the fastest-growing segment of our population.
Key Points
An ExRx should be designed in a systematic and individualized manner in terms of the Frequency (how often?), Intensity (how hard?), Time (how long?), Type (what kind?), Volume, and Progression—or the FITT-VP principle.
Components of the FITT-VP within an ExRx may be modified in the setting of certain chronic conditions to maximize therapeutic benefit of exercise.
Older adults can be encouraged to participate in 30 min/d or more of moderate-intensity aerobic exercise 3 to 5 d/wk to total 150 min/wk and supplement with resistance, flexibility, and balance training ≥ 2 d/wk. For greater and more intensive benefits, vigorous intensity aerobic exercise is encouraged, if tolerated.
Preparticipation health screening should be implemented to identify at-risk individuals, taking into consideration the patient's current level of exercise, desired intensity of exercise, diagnosed disease, and signs and symptoms suggestive of disease.
Potential additive or deleterious interactions between exercise and concomitant medications commonly used by older adults highlight the need for clinicians to appraise the effects of each medication alone and in combination with exercise.
Conflict of Interest Disclosure: The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
Footnotes
Editor's Note: We are pleased to offer 1 credit of Continuing Medical Education for successfully completing an online quiz about this article. You may access the quiz at www.houstonmethodist.org/cme-online.
References
- 1.United States Census Bureau [Internet] Washington, DC: United States Census; 2015. 2014 national projections; 2014 [cited 2016 Jan 15]. Available from: https://www.census.gov/population/projections/data/national/2014.html. [Google Scholar]
- 2.Centers for Disease Control and Prevention [Internet] Atlanta: U.S. Department of Health and Human Services; 2013. The state of aging and health in America 2013; 2013 [Cited 2016 Jan 15]. Available from; http://www.cdc.gov/features/agingandhealth/state_of_aging_and_health_in_america_2013.pdf. [Google Scholar]
- 3.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion [Internet] Washington, D.C.: U.S. Department of Health and Human Services; Healthy people 2020: Older adults; 2015 [cited 2016 Jan 16]. Available from: www.healthypeople.gov. [Google Scholar]
- 4.American College of Sports Medicine. Chodzko-Zajko WJ, Proctor DN et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009 Jul;41(7):1510–30. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 5.Federal Interagency Forum on Aging-Related Statistics (U. S). Older americans 2004: Key indicators of well-being. 2004. p. 141.
- 6.Barnes PM, Schoenborn CA. Trends in adults receiving a recommendation for exercise or other physical activity from a physician or other health professional. NCHS Data Brief. 2012;(86):1–8. (86) [PubMed] [Google Scholar]
- 7.Pescatello L, Arena R, Riebe D, Thompson P. ACSM's guidelines for exercise testing and prescription. 9th edition ed. Baltimore, ML: Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- 8.Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M et al. Updating ACSM's recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47(11):2473–79. doi: 10.1249/MSS.0000000000000664. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion [Internet] Washington, D.C.: U.S. Department of Health and Human Services; Physical activity guidelines advisory committee report; 2008 Jun [cited 2016 Jan 15]. Available from: http://health.gov/paguidelines/report/pdf/CommitteeReport.pdf. [Google Scholar]
- 10.Lauer M, Froelicher ES, Williams M, Kligfield P, American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention Exercise testing in asymptomatic adults: a statement for professionals from the American Heart Association Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2005 Aug 2;112(5):771–6. doi: 10.1161/CIRCULATIONAHA.105.166543. [DOI] [PubMed] [Google Scholar]
- 11.Kochanek KD, Murphy SL, Xu J, Arias E. Mortality in the United States, 2013. NCHS Data Brief. 2014 Dec;(178):1–8. [PubMed] [Google Scholar]
- 12.Ash GI, Macdonald HV, Pescatello LS. Antihypertensive effects of exercise among those with resistant hypertension. Hypertension. 2013;61(1):e1. doi: 10.1161/HYPERTENSIONAHA.111.00126. [DOI] [PubMed] [Google Scholar]
- 13.Ammar T. Effects of aerobic exercise on blood pressure and lipids in overweight hypertensive postmenopausal women. J Exerc Rehabil. 2015;11(3):145–150. doi: 10.12965/jer.150204. doi: 10.12965/jer.150204[doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karstoft K, Pedersen BK. Exercise and type 2 diabetes: Focus on metabolism and inflammation. Immunol Cell Biol. 2015 doi: 10.1038/icb.2015.101. [DOI] [PubMed] [Google Scholar]
- 15.Watz H, Pitta F, Rochester CL, Garcia-Aymerich J, ZuWallack R, Troosters T et al. An official european respiratory society statement on physical activity in COPD. Eur Respir J. 2014;44(6):1521–37. doi: 10.1183/09031936.00046814. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Medicare and Medicaid Services [Internet] Atlanta: U.S. Department of Health and Human Services; 2015. Chronic conditions; 2015 [cited 2016 Jan 15]. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/CC_Main.html. [Google Scholar]
- 17.Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA et al. American college of sports medicine position stand. exercise and hypertension. Med Sci Sports Exerc. 2004;36(3):533–53. doi: 10.1249/01.mss.0000115224.88514.3a. [DOI] [PubMed] [Google Scholar]
- 18.Pescatello LS, MacDonald HV, Johnson BJ. Effects of exercise on hypertension. Switzerland: Springer International Publishing; 2015. pp. 3–23. Part I, The effects of aerobic exercise on hypertension: current consensus and emerging research; p. [Google Scholar]
- 19.Pescatello LS, MacDonald HV, Ash GI, Lamberti LM, Farquhar WB, Arena R et al. Assessing the existing professional exercise recommendations for hypertension: A review and recommendations for future research priorities. Mayo Clin Proc. 2015;90(6):801–12. doi: 10.1016/j.mayocp.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Arnarson A, Ramel A, Geirsdottir OG, Jonsson PV, Thorsdottir I. Changes in body composition and use of blood cholesterol lowering drugs predict changes in blood lipids during 12 weeks of resistance exercise training in old adults. Aging Clin Exp Res. 2014;26(3):287–92. doi: 10.1007/s40520-013-0172-0. [DOI] [PubMed] [Google Scholar]
- 21.Kokkinos PF, Faselis C, Myers J, Panagiotakos D, Doumas M. Interactive effects of fitness and statin treatment on mortality risk in veterans with dyslipidaemia: A cohort study. Lancet. 2013;381(9864):394–9. doi: 10.1016/S0140-6736(12)61426-3. [DOI] [PubMed] [Google Scholar]
- 22.Parker BA, Capizzi JA, Grimaldi AS, Clarkson PM, Cole SM, Keadle J et al. Effect of statins on skeletal muscle function. Circulation. 2013;127(1):96–103. doi: 10.1161/CIRCULATIONAHA.112.136101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sinzinger H, O'Grady J. Professional athletes suffering from familial hypercholesterolaemia rarely tolerate statin treatment because of muscular problems. Br J Clin Pharmacol. 2004;57(4):525–8. doi: 10.1111/j.1365-2125.2004.02044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parker BA, Augeri AL, Capizzi JA, Ballard KD, Troyanos C, Baggish AL et al. Effect of statins on creatine kinase levels before and after a marathon run. Am J Cardiol. 2012;109(2):282–7. doi: 10.1016/j.amjcard.2011.08.045. [DOI] [PubMed] [Google Scholar]
- 25.Thompson PD, Zmuda JM, Domalik LJ, Zimet RJ, Staggers J, Guyton JR. Lovastatin increases exercise-induced skeletal muscle injury. Metabolism. 1997;46(10):1206–10. doi: 10.1016/s0026-0495(97)90218-3. [DOI] [PubMed] [Google Scholar]
- 26.O'Neill K, Reid G. Perceived barriers to physical activity by older adults. Can J Public Health. 1991;82(6):392–6. [PubMed] [Google Scholar]
- 27.Costello E, Kafchinski M, Vrazel J, Sullivan P. Motivators, barriers, and beliefs regarding physical activity in an older adult population. J Geriatr Phys Ther. 2011;34(3):138–47. doi: 10.1519/JPT.0b013e31820e0e71. [DOI] [PubMed] [Google Scholar]
- 28.van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: A review. Am J Prev Med. 2002;22(2):120–33. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- 29.Sallis R. Exercise is medicine: A call to action for physicians to assess and prescribe exercise. Phys Sportsmed. 2015;43(1):22–6. doi: 10.1080/00913847.2015.1001938. [DOI] [PubMed] [Google Scholar]
- 30.Hirvensalo M, Heikkinen E, Lintunen T, Rantanen T. The effect of advice by health care professionals on increasing physical activity of older people. Scand J Med Sci Sports. 2003;13(4):231–6. doi: 10.1034/j.1600-0838.2003.00313.x. [DOI] [PubMed] [Google Scholar]
- 31.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC et al. Physical activity and public health in older adults: Recommendation from the american college of sports medicine and the american heart association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 32.National Institute on Aging [Internet] Bethesda, MD: National Institutes of Heath; 2015. Exercise & physical activity: Your Everyday Guide from the National Institute on Aging; 2011 May [cited 2016 Jan 15]. Available from: https://www.nia.nih.gov/health/publication/exercise-physical-activity/introduction. [Google Scholar]
- 33.Canadian Society for Exercise Physiology [Internet] Ottowa, Ontario: Canadian Society for Exercise Physiology; 2016. Canadian Physical Activity and Sedentary Behaviour Guidelines; 2012 [cited 2016 Jan 15). Available from: http://www.csep.ca/cmfiles/guidelines/csep_guidelines_handbook.pdf. [Google Scholar]
- 34.British Geriatrics Society [Internet] London: British Geriatrics Society; 2015. Physical Activity in Older Age - BGS Best Practice Guide; 2010 Nov 25 [cited 2016 Jan 16]. Available from: http://www.bgs.org.uk/index.php/topresources/publicationfind/goodpractice/1116-bpgphysicalactivity. [Google Scholar]
- 35.World Health Organization [Internet] Geneva, Switzerland: World Health Organization; 2015. Global recommendations on physical activity for health; 2010 [cited 2016 Jan 16]. Available from http://www.who.int/dietphysicalactivity/publications/9789241599979/en/ [Google Scholar]


