Abstract
The aim of this study was to describe the process of developing a nursing assessment tool for hospitalized adult patients with liver cirrhosis. A descriptive study was carried out in three stages. First, we conducted a literature review to develop a data collection tool on the basis of the Conceptual Model of Wanda Horta. Second, the data collection tool was assessed through an expert panel. Third, we conducted the pilot testing in hospitalized patients. Most of the comments offered by the panel members were accepted to improve the tool. The final version was in the form of a questionnaire with open-closed questions. The panel members concluded that the tool was useful for accurate nursing diagnosis. Horta's Conceptual Model assisted with the development of this data collection tool to help nurses identify accurate nursing diagnosis in hospitalized patients with liver cirrhosis. We hope that the tool can be used by all nurses in clinical practice.
Liver cirrhosis is an important cause of morbidity and mortality in the world, and among the 10 leading causes of death of adults (Kelso, 2008). Moreover, the burden of chronic liver disease is projected to increase due to the growing prevalence of end-stage liver disease and hepatocellular carcinoma secondary to nonalcoholic fatty liver disease and hepatitis C virus (Lim & Kim, 2008).
Background
In the United States, cirrhosis results in more than 400,000 hospitalizations and 27,000 deaths annually (Kelso, 2008). In England, liver cirrhosis has increased more than the top four cancers during 1998–2009 (Ratib, West, Crooks, & Fleming, 2013), while in Taiwan, chronic liver disease and liver cirrhosis together are the eighth leading causes of overall deaths (Wu, Wu, Lien, Chen, & Tsai, 2012). The prevalence of cirrhosis has also increased in the Brazilian population, especially among the elderly (Barros, Francisco, Zanchetta, & César, 2011). Cirrhosis is the eighth leading cause of death among Brazilian men and contributed to 8.95% of hospital admissions in 2010 (Barros et al., 2011; Brazil Ministry of Health, 2008,2010; Silva, 2010).
Because of the progression of liver cirrhosis, patients often require hospitalization. Assisting these patients can be a challenge to healthcare professionals, especially nurses, because these patients may deteriorate rapidly and are at high risk for complications and death, requiring constant monitoring and surveillance (Kelso, 2008; Merli et al., 2010). Nurses need to know how to apply scientific methods to improve patients' outcomes and should possess extensive knowledge so that they can employ clinical reasoning and judgment skills to provide individualized and appropriate care to these individuals.
Nursing Process
In this context, the nursing process (NP) is recognized as an important tool for nurses to provide competent and safe care. The NP is a system that supports clinical decision-making because it brings together numerous important and specific data from patients, allowing effective communication among nurses, and the transmission of accurate and timely information to members of the multidisciplinary team (Bulechek, Butcher, Dochterman, & Wagner, 2013). The NP involves implementing a sequence of specific and systematized steps to provide professional care to the individual, family, or community, and to consider people's uniqueness (NANDA International, 2012).
Wanda de Aguiar Horta, the first nurse to introduce the concept of NP in Brazil, developed a nursing model that presents this work methodology for nurses. According to Horta (1979), the nursing process is defined as the dynamics of systematized and interrelated actions, aiming at assisting the human being. Thus, the NP is characterized by the interrelationship and dynamism of its phases.
Horta's conceptual model (1979) is based on the Hierarchy of Basic Human Needs (BHN), which influences human behavior. This nursing model seeks to show nursing as an applied science, moving from empirical to scientific stages, through the development of theories, systematization of knowledge and research, to become an independent science.
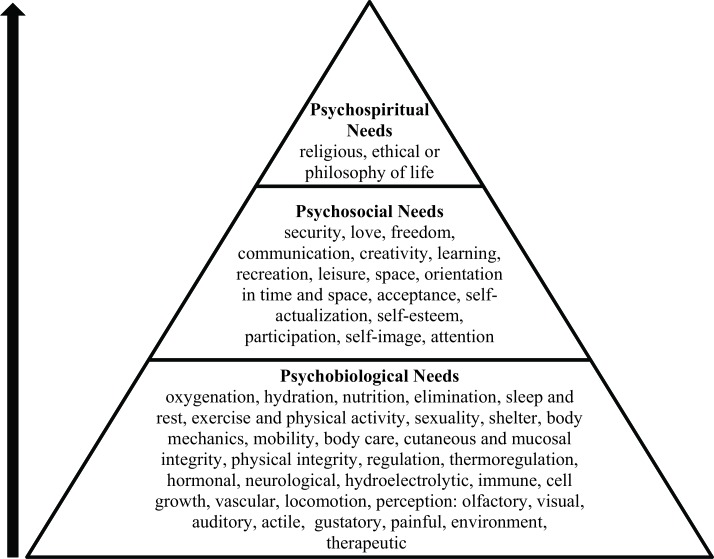
The theoretical model of BHN was introduced by the pioneering work of psychologist Abraham Maslow, who described an integrated set of human needs. The satisfaction and fulfilling of these needs are considered essential for the healthy development of the human being (Taylor, 2003). In addition to Maslow's BHN model, Horta (1979) adopted the classification proposed by John Mohana, where human needs are classified into three levels: psychobiological, psychosocial, and psychospiritual (Neves, 2006) (Figure 1).
FIGURE 1.
Horta's nursing model.
For Horta, all human needs are closely interrelated as they collectively make up the whole person; it is essential to have this holistic viewpoint because a person is an indivisible whole and not the sum of its parts. According to Horta (1979), the NP is divided into six phases:
Assessment: This phase consists of obtaining data through a systematic roadmap, making it possible to identify actual problems and potentials of the individual, family, or community.
Nursing diagnosis: Identifying the basic needs of the individual and then determining the degree of required care in nature and extent.
Healthcare plan: The overall determination of nursing care that individuals should receive, before the nursing diagnosis is confirmed. The healthcare plan is a result of the review of the nursing diagnosis and examines the issues and requirements of nursing care, and the degree of dependence of the individual.
Nursing prescription: The daily (or the appointed) script that coordinates nursing activities toward an adequate care to meet the individual's basic and specific needs.
Nursing evaluation: The daily report or priority of successive changes that occur in individuals. Evaluation is a synthesis, an overall evaluation of the nursing prescriptions implemented.
Prognosis: The estimated capacity of individuals to meet their basic needs, after implementation of the care plan and the data provided by the nursing evaluation.
Although the Nursing Model proposed by Horta is the most used in Brazil, the stages of the NP usually adopted by Brazilian nurses underpin the international references; thus, it has five steps: assessment, diagnosis, planning, implementation, and evaluation (Alfaro-LeFevre, 2010; NANDA International, 2012; The American Nurses Association, 2013).
Among these phases, we emphasize assessment in our study, which is the basis for the NP. Thus, it should be performed as properly and completely as possible. Accurate data indicate the state of health of the patient, enabling the identification of nursing diagnoses. Therefore, data collection requires a specific tool for the systematic survey of significant data.
The development of a data collection tool, based on Horta's model, enables knowledge of the whole individual, fosters clinical reasoning, and develops the nursing diagnoses. The model may help nurses collect relevant data within the framework of nursing rather than medicine. Thus, the model assists nurses in critical thinking. Brazilian researchers have endeavored to develop tools to collect data for different populations (Corrêa et al., 2008; Lima, Silva, & Beltrão, 2009; Ribeiro et al., 2012; Bordinhão, & Almeida, 2012); however, there is a lack of specific tools to help nurses collect essential information from patients with liver cirrhosis.
The development of this data collection tool will assist nurses to obtain objective and subjective data and give support to practitioners in outcome identification and development of nursing care plans. The aim of this research was to describe the process of developing a new nursing assessment tool for hospitalized adult patients with liver cirrhosis.
Methods
We conducted a descriptive study in a Brazilian University Hospital in the São Paulo state. The study was divided into three phases.
Phase 1: Elaboration of the First Version of the Nursing Assessment Tool
In Phase 1, we drafted the first version of the data collection tool to assist nurses in assessing critical information for the nursing diagnoses. The tool was based on Horta's Conceptual Model, the literature review, other instruments, publications about the issue, and the clinical experience of the main researcher. We performed a literature review in the main bibliographic health databases (Literature of Latin American and the Caribbean Health Sciences—LILACS, and Medical Literature Analysis—MEDLINE) during the period of August–October 2012. We used the descriptors: “nursing care,” “liver cirrhosis,” “care,” and “nursing.” We also reviewed semiology books (Bickley & Szilagyi, 2012; Brunner, Smeltzer, Bare, Hinkle, & Cheever, 2010; Jarvis, 2011) to identify the main signs and symptoms that characterize liver cirrhosis.
Phase 2: Assessment of the First Version of the Nursing Assessment Tool
The first version of the data collection tool was assessed through five experts with experience in care of patients with liver cirrhosis, NP, as well as Horta's conceptual model. These experts were asked to participate in the study via letter of invitation sent by e-mail and were selected through the existing curricula in the database of the National Council for Scientific and Technological Development (CNPq), a Brazilian agency of the Ministry of Science, Technology and Innovation. They were also selected for their nursing experience with liver cirrhosis and their existing publications on the issue. Therefore, the panel was composed of four registered nurses with PhDs and one registered nurse with a master's degree.
The first version of the data collection tool was sent to the experts with an evaluation form attached that contained two parts. The first part consisted of the experts' identification, and the second part had instructions for completing the tool. The evaluation form included organization of the instrument, structure of the instrument, presentation of items and categories, consistency, and formatting. Each section and category was evaluated according to four criteria for which the panel members assigned a score from 1 to 4 (1 = disagree; 2 = partially agree; 3 = agree; 4 = strongly agree). The evaluation form had spaces for comments and suggestions about the tool. The experts had 30–60 days to evaluate and return the tool and evaluation form to the researchers.
Phase 3: Pilot Testing of the Nursing Assessment Tool
The modified data collection tool was pilot tested by two registered nurses in five patients with liver cirrhosis admitted to the gastroenterology ward. This ward was selected because it is the unit where adult patients with liver cirrhosis are cared for in our hospital.
The aims of the research were clearly explained to the patients. The study was approved by the appropriate ethics committee. Participants were assured that their identity would remain confidential, and they voluntarily signed a consent form.
The two nurses performed the pilot testing of the nursing assessment tool through interviews with the patients and/or their caregivers, physical examination, and consultation in patients' medical records. After the pilot testing had been completed, the researchers included new data in the tool and reformulated others. These changes led to the final version of the data collection tool.
Results
Horta's conceptual model led to the development of a new clinical data collection tool for people with liver cirrhosis to establish the essential information that should be readily available to nurses. To help nurses collect essential data during patients' assessment, the first version of the assessment tool included the three levels of the human basic needs identified in Horta's model. Also, the categories and variables were further delineated to include specific sections (Table 1).
TABLE 1. Summary of Sections, Categories, and Variables Included in the First Version of the Nursing Assessment Tool.
| Sections | Categories | Variablesa |
|---|---|---|
| I—Demographic information | Record number, initials of the name, date of birth, age, gender, ethical group, marital status, the number of children, educational level, occupation, family income, nationality, and origin | |
| II—Data of hospitalization | Date, time, ward, bed number, past hospitalizations, updated immunizations, history of allergies, family history, reason for hospitalization, medical diagnosis | |
| III—Lifestyle | Use of tobacco, alcohol, uncontrolled substances/drugs, self-medication, physical activity, eating habits, hydration and elimination (bladder pattern and bowel pattern), and usual medication | |
| IV—Psychobiological needs | Oxygenation | Complaints, inspection, palpation, percussion, and auscultation |
| Circulation | Blood pressure (site of measurement, patient position, arm circumference, cuff width), wrist (characteristics), heart rate (characteristics), skin color, presence of edema, peripheral perfusion, presence of venous catheters, venous infusions | |
| Thermoregulation | Body temperature, presence of sweating, tremors | |
| Mental status | Complaints, level of consciousness, visual acuity, pupils, olfactory acuity, hearing acuity, taste acuity, tactile perception | |
| Skin and mucosal integrity | Skin characteristics (color, humidity, lesions), loss of sensation, appearance of the nails, scalp | |
| Nutrition/hydration | Weight (current, usual, changes), height, body mass index, presence of feeding tube, type of diet, amount of diet, fluid intake, complaints (nausea, vomiting), examination of the mouth, lips, oral mucosa, gums, teeth | |
| Elimination | Urinary and intestinal (frequency, appearance, volume), complaints, abdominal examination (inspection, auscultation, palpation and percussion) | |
| Sleep and rest | Sleep pattern, changes in the sleep pattern | |
| Physical activity and mobility | Walking, changes in the gait pattern | |
| Hygiene | Need for bathing self-care, need for toileting self-care, need for dressing self-care | |
| Regulation | Thyroid (inspection, palpation) | |
| Shelter | Type and condition, people living with, existence of sanitation, destination after hospital discharge | |
| Sexuality | Genitals (inspection), changes and/or complaints related to sexual activity, contraceptive use | |
| V—Psychosocial needs | Safety | Presence of anxiety, fear, aggression, afflictions, self-perception of the health state |
| Communication | Type of communication, tone of voice, how communicates, changes | |
| Social interaction | Communicates with others, stands alone, participates in activities, receives visits, family relationship | |
| Leisure/recreation | Watches television, listens to the radio, performs manual labor, reads | |
| Self-esteem | Confidence, negative verbalizations, crying, anguish, poor body presentation | |
| Self-realization | How the disease affects your life, life expectancy | |
| VI—Psychospiritual needs | Religious, ethical, philosophy of life | |
| VII—Drug therapy in hospital | ||
| VIII—Supplementary examinations results |
aNot all variables are shown in this table.
According to the panel members, the first version of the assessment tool correctly used scientific terms and logically sequenced the sections, categories, and variables. The experts found the data collection tool complete, clear, objective, and appropriate for patients with liver cirrhosis. Also, the panel found the font used in the tool appropriate.
As noted by the experts, the new nursing assessment tool was considerably extensive. Thus, the variables presented in the following sections “I—Personal Data” and “II—Data of Hospitalization” needed to be reviewed, and their presentation was modified to make the tool less extensive. The variables relating to gender, ethnic group, marital status, education level, and origin were revised to an open question. Nurses also noticed the need to include extra spaces for recording the “reason for hospitalization” in the section “II—Data of Hospitalization” because in the first version, the spaces were insufficient to record all of the necessary information, given the complexity of patients with liver cirrhosis.
Some variables of the third section “III—Lifestyle” were removed from the original tool and were included in corresponding categories. For example, the variables related to “feeding and hydration habits” were transferred to the category “nutrition/hydration” and the variables related to “urinary and intestinal habits” were transferred to the category “elimination.”
Most of the comments made by the experts were accepted to improve the clarity and understanding of the nursing assessment tool. For example, the word “asylum” from the section “II—Data of Hospitalization” was replaced by “long-stay institution for the elderly” because it includes geriatric clinics, and nursing homes, among others. In the category “oxygenation” from the section “IV—Psychobiological Needs,” the word “nasal oxygen catheter” was replaced by “nasal cannula,” because nasal cannula has been widely used in Brazilian clinical practice, instead of nasal oxygen catheter. Also, we included new variables on the tool as suggested by the experts. In the category “circulation” from the section “IV—Psychobiological Needs,” we added space to record information related to intravenous albumin or other blood products (Table 2).
TABLE 2. Comparison of Original and Revised Nursing Assessment Toolsa.
| Original Nursing Assessment Tool | Revised Nursing Assessment Tool | ||
|---|---|---|---|
| I—Demographic Information | () Gender |
|
Gender: __________ |
| () Marital status |
|
Marital Status: ____________ | |
| II—Data of Hospitalization | () Origin |
|
Origin from: () home () long-stay institution for the elderly () basic health unit () emergency unit () other: ________ |
| Reason for hospitalization:____________________________________________ | Reason for hospitalization:______________________________________________________________________________________________________________ | ||
| III—Lifestyle | Practice physical activity? () Yes () No | Variable included in the category “physical activity and mobility” | |
| Need help for hygiene? () Yes () No | Variable included in the category “hygiene” | ||
| Feeding habits (frequency, amount, timing, type of food preference, intolerance): ______________________ | Variable included in the category “nutrition/hydration” | ||
| Hydration habits (frequency, amount, timing, type of food preference, intolerance): ______________________ | variable included in the category “nutrition/hydration” | ||
| Urinary elimination (frequency, quantity and characteristics): ________________ | variable included in the category “elimination” | ||
| Intestinal elimination (frequency, quantity and characteristics): _________ | variable included in the category “elimination” | ||
| IV—Psychobiological Needs: Oxygenation | Inspection: Breathing: () nasal oxygen catheter | Inspection: Breathing: () nasal cannula | |
| IV—Psychobiological Needs: Circulation | Blood Products: | ||
| () Red cells. Volume:______ | |||
| () Albumin: ___ U Frequency:___ | |||
| () Other: _____________________ | |||
| Last Paracentesis: ___/___/_____ | |||
| Indication: () Relief () Diagnosis | |||
| Volume drained: _____ L | |||
| Appearance: __________________ | |||
| IV—Psychobiological Needs: Nutrition/hydration | Weigh: ____ kg | Current weight: ____ kg | |
| Usual weight: _____ kg | |||
| Percentage of weight loss: ____% | |||
| Triceps skinfold thickness: ____ cm | |||
| Circumference of the middle region of the arm: _____ cm | |||
| IV—Psychobiological Needs: Elimination | Water balance in 24 hours: ____ ml | ||
| () positive fluid wave | |||
| () negative fluid wave | |||
| () shifting dullness | |||
Note. The bold are the changes and/or inclusions made in the nursing assessment tool.
aNot all the changes and/or inclusions made in the nursing assessment tool are shown in this table.
With the aim of providing congruency in the category labels, “tissue integrity” was changed to “skin and mucosal integrity.” In the category “elimination” from the section “IV—Psychobiological Needs,” we included variables related to abdominal examination. For example, after considering a suggestion made by the experts, spaces were inserted in the tool to record data related to abdominal percussion, as there may be changes in chronic liver diseases, including ascites. Thus, we included the assessment for a fluid wave. Also, one expert suggested inserting the inspection of external genitalia because there are common changes occurring in this area. However, this suggestion was not accepted because the examination of the external genitalia was contemplated in the category “sexuality.”
After the pilot testing of the data collection tool, the two registered nurses it found it necessary to make other changes. Among them is; for example, data about paracentesis (such as date and indication of last procedure, volume and aspect of the drained liquid) was added because it is a common procedure in patients with liver cirrhosis. In the category “nutrition/hydration,” nurses verified the need to include variables related to nutritional status, such as the current and usual weight, percentage of weight loss, triceps skinfold thickness, and circumference of the middle region of the arm. In the category “elimination,” open spaces were added for nurses to collect data about the patient's fluid balance (Table 2).
The final version of the data collection tool is in the form of a questionnaire with open-closed questions, and a section called “Observations” was added for nurses to register other relevant information. The expert panel members concluded the tool was useful for accurate nursing diagnosis in adult patients with liver cirrhosis. Judges also considered the data collection tool complete, with sections, categories, and variables presented in a logical sequence. It is worth noting that one expert considered the tool valuable to be used for hospitalized adult patients from other medical specialties. In addition, one expert reported, “The assessment tool has a nursing language and does not just follow the biomedical model, found in many tools that claim to follow a theoretical nursing model.”
The final version of the data collection tool for adult patients with liver cirrhosis, based on the Horta's conceptual model, may facilitate the recording of subjective and objective data in a systematic fashion. Therefore, the tool may help nurses identify accurate nursing diagnoses for individualized care.
Discussion
Providing safe nursing care and promoting quality of life for patients with liver cirrhosis can be a challenge for nurses because of the complexity of the disease and the therapeutic regimens required. There are many complications associated with chronic liver disease, which increases the potential number of hospitalizations and deaths (Kelso, 2008; Werner & Perez, 2012). For this reason, nurses must employ all their repertoire of knowledge to recognize the most frequent nursing diagnoses in patients with liver cirrhosis for further identification of the best planning priorities and strategies to provide supportive care, improve symptom management, and prevent complications associated with further decompensation (Werner & Perez, 2012). Therefore, data collection needs to be comprehensive enough to guide the decision making of nurses in promoting and protecting the health and recovery of these patients (NANDA International, 2012).
According to researchers, assessment is a continuous process of collecting relevant data about the patients' responses, health status, and concerns. Thus, interview, direct observation, and measurement are used frequently by nurses to gather subjective and objective data (Kenney, 1995).
Nurses who use specific tools to collect data in their clinical practice promote better care quality (Guilherme, Carvalho, & Landeros López, 2012) and safety. There is a need for a new nursing assessment tool aimed at collecting objective and subjective data that will assist nurses in critical thinking. Furthermore, this new tool may assist with the process of communication, clinical reasoning, and organizing information of individuals in different contexts of healthcare and in various times across the health-disease continuum. Thus, the tool can also enable a comprehensive database for the implementation of appropriate assistance and consequently improve the quality of care provided to clients and their families, as well as increase the professionalism of nursing staff' across the multidisciplinary team (Ramalho-Neto et al., 2013).
The nursing assessment tool developed in this study is presented in the form of a questionnaire with open-closed questions, and its presentation is similar to other studies that adopted the theories presented in Horta's conceptual model (Bittar, Pereira, & Lemos, 2006; Lima et al., 2009; Ribeiro et al., 2012). During the process of development, we felt the need to add data specific to the population served, which may assist with time management strategies of nurses during data collection, and in the practicalities associated with developing the care plan (Bittar et al., 2006).
Although the assessment tool has been judged suitable for patients with liver cirrhosis, the expert panel also considered it to be extensive, a problem that has also been identified in a previous study (Teixeira, Becker, Citro, Zanetti, & Landim, 2011). In an attempt to decrease the length, some items of the final version are now presented as open-ended questions. This is a positive change as it will allow the nurse to record information that they deem necessary, and in their own words (Polit & Beck, 2009).
There was also a consideration to group similar items together to reduce the tool's length, as has been done in previous research (Galdeano & Rossi, 2002). However, other items specific to patients with liver cirrhosis had to be included in the final version. An example of this is the insertion of data about intravenous albumin infusion. This was necessary because blood transfusion is common in these patients during the care process (McCullough, O'Shea, & Dasarathy, 2011; O'Shea, Dasarathy, & McCullough, 2010).
Another example is the addition of new variables related to nutritional status in category “6—Nutrition/Hydration,” because there are frequent nutritional changes associated with chronic liver disease (Tai, Goh, Mohd-Taib, Rampal, & Mahadeva, 2010). This need to consider other aspects of data collection to provide comprehensive and flexible care to patients has also been identified in previous studies (Bittar et al., 2006; Ribeiro et al., 2012). We believe that this new nursing assessment tool will be useful in patients with liver cirrhosis across other areas of nursing care such as specialized ambulatory services.
Limitations
This study presented limitations. Because of the instability of these patients, some died during data collection, resulting in a small sample for pilot testing. We therefore suggest future studies with larger samples and in multiple healthcare settings, such as ambulatory care. We also encourage future studies to trial this nursing assessment tool to evaluate the applicability in patients with other diseases and in outpatients.
Conclusion
There is a worldwide increase in the number of patients diagnosed with liver cirrhosis who are admitted into hospitals. Nurses need to work within the multidisciplinary team to tailor their approach to each patient's unique needs. Previous data collection methods have been insufficient in assisting nurses to obtain a comprehensive view of the patient's medical and social history, current disease progression, and comorbidities.
The conceptual model presented by Wanda Horta assisted with the development of a new nursing assessment tool to help nurses identify accurate nursing diagnosis in hospitalized patients with liver cirrhosis. We hope that the nursing assessment tool developed in this study can be used in clinical practice for all nurses who assist patients with liver cirrhosis. We also hope that the tool will facilitate the selection of appropriate nursing diagnoses and further support the identification of adequate nursing interventions to improve patient outcomes, thus enhancing patient safety.
ACKNOWLEDGMENTS
The authors thank the São Paulo Research Foundation (FAPESP), Brazil, for funding this research.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- Alfaro-LeFevre R. (2010). Applying the nursing process: A tool for critical thinking (7th ed.). Philadelphia, PA: Wolters Kluwer Health/Lippincott, Williams & Wilkins. [Google Scholar]
- Barros M. B. A., Francisco P. M. S. B., Zanchetta L. M., César C. L. G. (2011). Trends in social and demographic inequalities in the prevalence of chronic diseases in Brazil. PNAD: 2003–2008. Ciência & Saúde Coletiva, 16(9), 3755–3768. [DOI] [PubMed] [Google Scholar]
- Bickley L., Szilagyi P. G. (2012). Bates' Guide to Physical Examination and History-Taking (11th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- Bittar D. B., Pereira L. V., Lemos R. C. A. (2006). Nursing assistance systematization for the critical patient: Proposal of an instrument to collect data. Texto & Contexto–Enfermagem, 15(4), 617–628. [Google Scholar]
- Bordinhão R. C., Almeida M. A. (2012). Instrument to collect data for critical patients based on the theory of basic human needs. Revista Gaúcha de Enfermagem, 33(2), 125–131. [DOI] [PubMed] [Google Scholar]
- Brazil Ministry of Health. (2008). Health Brazil 2007: An analysis of the health situation. Brasília, Brazil: Secretariat of Health Surveillance. [Google Scholar]
- Brazil Ministry of Health. (2010). Notebooks of health information. Brasília, Brazil: Author. [Google Scholar]
- Brunner L. S., Smeltzer S. C. O. C., Bare B. G., Hinkle J. L., Cheever K. H. (2010). Brunner & Suddarth's Textbook of Medical-surgical Nursing. (12th ed.). Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. [Google Scholar]
- Bulechek G., Butcher H. K., Dochterman J. M., Wagner C. (Eds.). (2013). Nursing intervention classification (NIC) (6th ed.). St. Louis, MO: Elsevier Health Sciences. [Google Scholar]
- Corrêa L. C. L., Beccaria L. M., Amorim R. C., Pacheco S. S., Vacondio S., Fechio P. B. (2008). Nursing data collection in a coronary unit: Instrument validation. Revista Arquivos de Ciências da Saúde, 15(2), 65–69. [Google Scholar]
- Galdeano L. E., Rossi L. A. (2002). Development and validation of data collection tools for the perioperative period in heart surgery. Revista Latino-Americana de Enfermagem, 10(6), 800–804. [PubMed] [Google Scholar]
- Guilherme C., Carvalho E., Landeros López M. (2012). Relevance of data collection instruments for quality of care. Enfermería Global, 11(3), 328–336. Retrieved January 25, 2014, from http://revistas.um.es/eglobal/article/viewFile/eglobal.11.3.155221/136401 [Google Scholar]
- Horta W. A. (1979). Nursing process. São Paulo, Brazil: E.P.U. [Google Scholar]
- Jarvis C. (2011). Jarvis's Physical Examination and Health Assessment (6th ed.). St. Louis: MO: Elsevier Health Sciences. [Google Scholar]
- Kelso L. A. (2008). Cirrhosis: Caring for patients with end-stage liver failure. The Nurse Practitioner: The American Journal of Primary Health Care, 33(7), 24–30. [DOI] [PubMed] [Google Scholar]
- Kenney J. W. (1995). Relevance of theory-based nursing practice. In Christensen P. J., Kenney J. W. (Eds.), Nursing process: Application of conceptual models (4th ed., pp. 3–23). St. Louis, MO: Mosby-Year Book. [Google Scholar]
- Lim Y. S., Kim W. R. (2008). The global impact of hepatic fibrosis and end-stage liver disease. Clinical Liver Disease, 12(4), 733–746. [DOI] [PubMed] [Google Scholar]
- Lima N. D. C., Silva V. M. D., Beltrão B. A. (2009). Construction and validation of data collection instrument content in a neonatal intensive care unit. Revista da Rede de Enfermagem do Nordeste, 10(3), 144–149. Retrieved May 10, 2014, from http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-21002013000200007&lng=en&tlng=en.10.1590/S0103-21002013000200007 [Google Scholar]
- McCullough A. J., O'Shea R. S., Dasarathy S. (2011). Diagnosis and management of alcoholic liver disease. Journal of Digestive Disease, 12(4), 257–262. [DOI] [PubMed] [Google Scholar]
- Merli M., Lucidi C., Giannelli V., Giusto M., Riggio O., Falcone M., Venditti M. (2010). Cirrhotic patients are at risk for health care–associated cacterial infections. Clinical Gastroenterology and Hepatology, 8(11), 979–985.e971. [DOI] [PubMed] [Google Scholar]
- NANDA International. (2012). Nursing diagnoses: Definitions and classification 2012–2014 (9th ed.). Oxford: Wiley. [Google Scholar]
- Neves R. D. S. (2006). Nursing attendance systematization in rehabilitation unit, in accordance to Horta's conceptual model. Revista Brasileira de Enfermagem, 59(4), 556–559. [DOI] [PubMed] [Google Scholar]
- O'Shea R. S., Dasarathy S., McCullough A. J. (2010). Alcoholic liver disease. Hepatology, 51(1), 307–328. [DOI] [PubMed] [Google Scholar]
- Polit D. F., Beck C. T. (2009). Essentials of nursing research: Appraising evidence for nursing practice (7th ed.). Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. [Google Scholar]
- Ramalho Neto J. M., Fontes W. D. d., Nóbrega M. M. L. d. (2013). Instrument to collect nursing data in General Intensive Care Unit. Revista Brasileira de Enfermagem, 66(4), 535–542. [DOI] [PubMed] [Google Scholar]
- Ratib S., West J., Crooks C. J., Fleming H. M. (2014). Diagnosis of liver cirrhosis in England, a cohort study, 1998–2009: a comparison with cancer. The American Journal of Gastroenterology, 109(2), 190–198. [DOI] [PubMed] [Google Scholar]
- Ribeiro M. C. O., Pereira C. U., Hora E. C., Nunes M. D. S., Silva C. B., Santos D. S. (2012). The development and validation of instrument of data collection for victims of traumatic brain injury. Revista de enfermagem UFPE On Line, 6(5), 11. [Google Scholar]
- Silva I. S. S. (2010). Liver cirrhosis. Revista Brasileira de Medicina, 67(4), 111–120. [Google Scholar]
- Tai M.-L., Goh K.-L., Mohd-Taib S., Rampal S., Mahadeva S. (2010). Anthropometric, biochemical and clinical assessment of malnutrition in Malaysian patients with advanced cirrhosis. Nutrition Journal, 9(1), 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor A. J. W. (2003). Justice as a basic human need. New Ideas in Psychology, 21(3), 209–219. [Google Scholar]
- Teixeira C. R. D. S., Becker T. A. C., Citro R., Zanetti M. L., Landim C. A. P. (2011). Validation of nursing interventions in people with diabetes mellitus. Revista da Escola de Enfermagem da USP, 45, 173–179. [DOI] [PubMed] [Google Scholar]
- The American Nurses Association. (2013). The nursing process. Retrieved October 3, 2013, from http://www.nursingworld.org/EspeciallyForYou/What-is-Nursing/Tools-You-Need/Thenursingprocess.html
- Werner K. T., Perez S. T. (2012). Role of nurse practitioners in the management of cirrhotic patients. The Journal for Nurse Practitioners, 8(10), 816–821. [Google Scholar]
- Wu L.-J., Wu M.-S., Lien G. I. S., Chen F.-C., Tsai J.-C. (2012). Fatigue and physical activity levels in patients with liver cirrhosis. Journal of Clinical Nursing, 21(1/2), 129–138. [DOI] [PubMed] [Google Scholar]