Abstract
We herein report the first case of a prosthetic joint infection caused by Raoultella ornithinolytica in an immunocompetent patient. The clinical outcome was favorable after a two-stage prosthetic exchange and a six-month course of antimicrobial therapy.
Keywords: Raoultella ornithinolytica, Prosthetic joint infection, Arthroplasty infection, Osteomyelitis, Infection, Human, Bacteria
Background
Raoultella ornithinolytica (formerly Klebsiella ornithinolytica) is a Gram-negative bacillus that belongs to the Enterobacteriaceae family [1]. Its role in the pathogenesis of human infections has recently been recognized [2]. Bone and joint infection caused by R. ornithinolytica is rare [2]. In this paper, we report the successful treatment of the first case of prosthetic joint infection caused by R. ornithinolytica with a two-stage prosthetic exchange and six-months of antimicrobial treatment.
Clinical presentation
In November 2014, a 67-year-old French male was admitted to our center for a loosening of both the femoral and acetabular components of his right hip arthroplasty. He had a medical history of chronic obstructive pulmonary disease, peripheral artery disease and arterial hypertension. He had received a left hip prosthesis in 2003 and a right hip prosthesis in 2004 for degenerative arthritis. In April 2009, he underwent fixation of the right femur fracture. Few weeks following surgery, he presented with a painful right hip; cultures of periprosthetic effusion aspirate were negative. In 2010, he underwent plate osteosynthesis for the right periprosthetic femur fracture. Two years later, he present with worsening right hip pain that limited hip mobility.
In 2014, he presented to our medical center for evaluation. He denied fever. Laboratory investigations revealed a leukocyte count of 9000 μL−1, low hemoglobin concentration (8.3 g/l; normal = 135–175 g/l), normal platelet count of 400,000 μL−1 and high C-reactive protein levels (72 mg/l; normal values ≤5mg/l). The hip radiograph revealed loosening of both the femoral and acetabular components of the right hip prosthesis (Fig. 1) and 18F FDG PET/CT showed right hip hypermetabolism, compatible with infected hip prosthesis with effusion (Fig. 2). Microbiological cultures of the periprosthetic effusion were positive for R. ornithinolytica, as identified by MALDI-TOF mass spectrometry and 16 s rRNA gene sequencing. Antimicrobial susceptibility testing showed that the isolate was susceptible to amoxicillin/clavulanic acid, ticarcillin/clavulanic acid, ceftriaxone, ciprofloxacin, doxycycline, aminoglycosides and cotrimoxazole, and was resistant to amoxicillin, ticarcillin and rifampin. A two-stage prosthetic exchange was performed with retention of plate osteosynthesis for the right periprosthetic femur fracture (Fig. 3). He was treated with one-month curse of intravenous ceftriaxone 2 g once daily and oral ciprofloxacin 500 mg three times daily, followed by five-month of oral doxycycline 200 mg twice daily and oral ciprofloxacin 500 mg three times daily. He recovered and a new hip prosthesis was implanted in April 2015. No relapse was observed during the one-year post-antimicrobial follow-up.
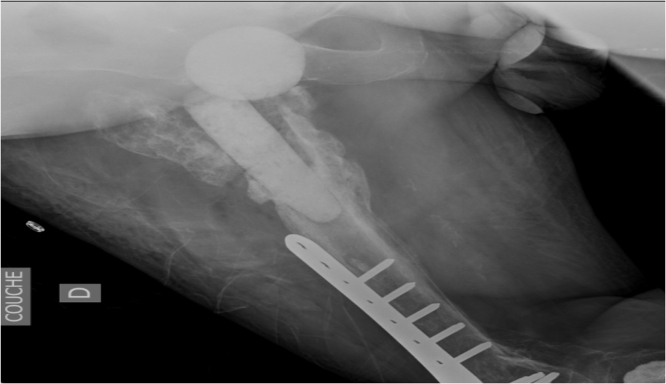
Fig. 1.
The hip radiograph revealed loosening of both the femoral and acetabular components of the right hip prosthesis.
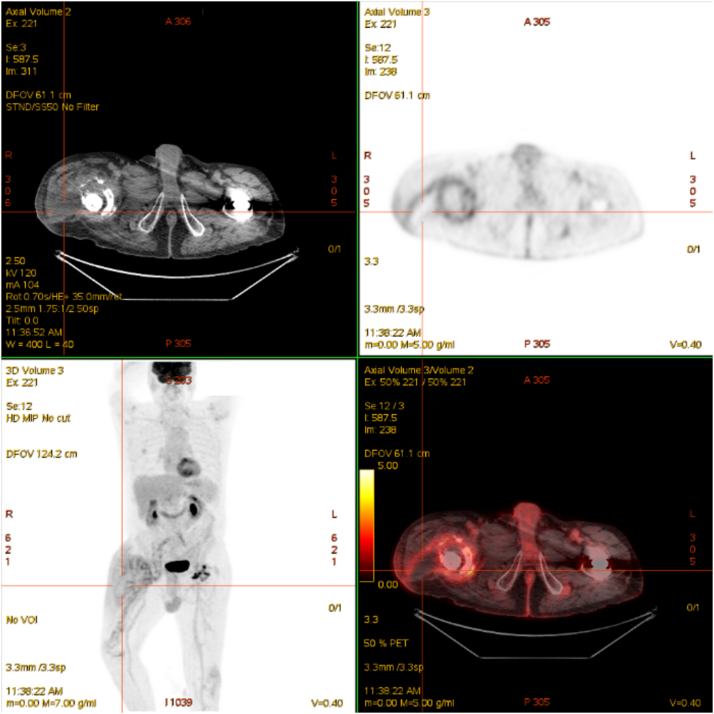
Fig. 2.
18F FDG PET/CT showed a right hip hypermetabolism, compatible with infected hip prosthesis with effusion.
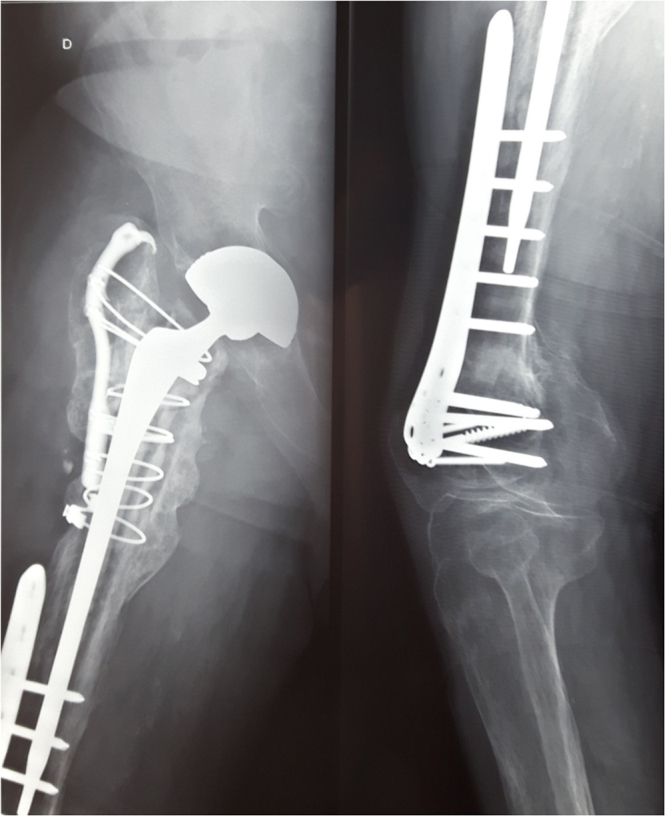
Fig. 3.
The hip radiograph showed a spacer prostheses in two-stage prosthesis exchange and retention of plate osteosynthesis.
Discussion
This paper presents the first known case of chronic prosthetic joint infection caused by R. ornithinolytica which were successfully treated with a two-stage prosthetic exchange and six months treatment with antimicrobials. R. ornithinolytica is a Gram-negative aquatic-commensal Enterobacteriaceae [3] and its pathogenic role in community and hospital-acquired infections such as cholangitis, intravascular catheter-related infections, urinary tract infections, skin infections, lower respiratory tract infections, central nervous system infections, mediastinitis, pericarditis, conjunctivitis and otitis has recently been elucidated [2].
To our knowledge, only five cases of chronic osteomyelitis have been reported to date, including one case of osteomyelitis of a distal phalanx of the right ring finger [4], one case of tibia pandiaphyseal osteomyelitis (an osteomyelitis extending to the entire the diaphysis or as involvement of the opposite metaphysis), two cases of chronic osteomyelitis of diabetic foot infections and one case of foot osteomyelitis related to a peripheral artery disease [2].
The main treatment of the cases of osteoarticular infection caused by R. ornithinolytica reported in the literature has been surgical lavage and debridement followed by prolonged antimicrobial treatment. The duration of treatment varied from 30 to 90 days [2], [4]. All of these cases recovered, but one case of tibia pandiaphysitis and one case of chronic osteomyelitis in diabetic foot infection required amputation [2]. Based on the duration of symptoms was more than one year and retention of plate osteosynthesis for the right periprosthetic femur fracture, we decided to treat our case with a two-stage prosthetic exchange and six months of antimicrobial therapy. A good clinical outcome was achieved.
Cases of R. ornithinolytica may be misidentified as a Klebsiella species in clinical laboratories using conventional phenotypic identification [5] and therefore the organisms may be under-recognized as a human pathogen [2].
R. ornithinolytica appears to be a Gram-negative aquatic-commensal Enterobacteriaceae with the ability to adhere to human tissues and to form biofilms in urinary catheters [6], [7]. These two mechanisms could play a role in the pathogenesis of bone and joint infections caused by R. ornithinolytica. The identification of virulence factors in the genomic study of clinical isolates is important to understanding the mechanisms by which R. ornithinolytica infects bone and orthopedic devices.
Conclusion
Although bone and joint infections due to R. ornithinolytica are rare, the organism should not be dismissed as a contaminant when isolated from surgical samples and the diagnosis should be further investigated. Prolonged antimicrobial treatment following surgical debridement and lavage is needed.
Conflict of interest
The authors declare no conflicts of interest.
Consent
This study was approved by the institutional research ethics board (Comité de Protection des Personnes Sud Méditerranée 1), and written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Funding
The authors have no relevant affiliations or involvement with any organization or entity with a financial interest or conflict with the subject matter or materials discussed in the manuscript. No medical writer or editor was involved in drafting this manuscript.
Contributions
-
•
PS: First and corresponding author, involved in clinical data collection, substantial contributions to study conception and drafting the manuscript.
-
•
FT: Second author, microbiological data collection, revision of the manuscript.
-
•
EH: Third author, clinical data verification, revision of the manuscript.
-
•
DP: Fourth author, surgical data verification and revision of the manuscript.
-
•
PEF: Fifth author, microbiological data collection, revision of the manuscript.
-
•
AS: last author, clinical data verification, discussion section, final approval of the version to be published.
-
•
All authors read and approved the final manuscript.
References
- 1.Drancourt M., Bollet C., Carta A., Rousselier P. Phylogenetic analyses of Klebsiella species delineate Klebsiella and Raoultella gen nov., with description of Raoultella ornithinolytica comb. nov. Raoultella terrigena comb. nov. and Raoultella planticola comb. nov. Int J Syst Evol Microbiol. 2001;51:925–932. doi: 10.1099/00207713-51-3-925. [DOI] [PubMed] [Google Scholar]
- 2.Seng P., Boushab B.M., Romain F., Gouriet F., Bruder N. Emerging role of Raoultella ornithinolytica in human infections: a series of cases and review of literature. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2016 doi: 10.1016/j.ijid.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 3.Kanki M., Yoda T., Tsukamoto T., Shibata T. Klebsiella pneumoniae produces no histamine: Raoultella planticola and Raoultella ornithinolytica strains are histamine producers. Appl Environ Microbiol. 2002;68:3462–3466. doi: 10.1128/AEM.68.7.3462-3466.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmutz N., Adler T., Schelhorn N., Wirz S., Fricker R. Postoperative osteomyelitis of a distal phalanx caused by Raoultella ornithinolytica. Handchir Mikrochir Plast Chir Organ Deutschsprachigen Arbeitsgemeinschaft Handchir Organ Deutschsprachigen Arbeitsgemeinschaft Mikrochir Peripher Nerven Gefasse Organ V. 2015 [Google Scholar]
- 5.Park J.S., Hong K.H., Lee H.J., Choi S.H., Song S.H., Song K.-H. Evaluation of three phenotypic identification systems for clinical isolates of Raoultella ornithinolytica. J Med Microbiol. 2011;60:492–499. doi: 10.1099/jmm.0.020768-0. [DOI] [PubMed] [Google Scholar]
- 6.Solak Y., Gul E.E., Atalay H., Genc N., Tonbul H.Z. A rare human infection of Raoultella ornithinolytica in a diabetic foot lesion. Ann Saudi Med. 2011;31:93–94. doi: 10.4103/0256-4947.75794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Djeribi R., Bouchloukh W., Jouenne T., Menaa B. Characterization of bacterial biofilms formed on urinary catheters. Am J Infect Control. 2012;40:854–859. doi: 10.1016/j.ajic.2011.10.009. [DOI] [PubMed] [Google Scholar]