Abstract
Objective
Infants born to HIV-infected women receiving antiretroviral treatment (ART) can breastfeed through at least 6 months with very low risk of HIV acquisition. We aimed to identify demographic and cultural factors that may influence mothers’ willingness to breastfeed for the recommended duration.
Methods
We evaluated factors associated with early cessation of breastfeeding (i.e before 5 months post-partum) in a randomized clinical trial evaluating different ART regimens used for prevention of mother to child transmission during breastfeeding in Botswana. Univariate and multivariable Cox regression were used to describe predictors of early exclusive BF cessation.
Results
Among 677 women who started breastfeeding, the median time to breastfeeding cessation was 178 days (IQR 150–181) and 25.1% weaned early. In multivariable analysis, urban location (aHR=1.86 95%CI 1.27–2.73; p=0.002) salaried employment or being a student (aHR=2.78 95% CI 1.63–4.75); p<0.001), and infant hospitalization before weaning (aHR=2.04 95% CI 1.21 – 3.45; p=0.008) were independently and significantly associated with early BF cessation.
Conclusions
Improved support for breastfeeding among employed mothers, especially in urban settings, may allow HIV-infected women who are receiving ART prophylaxis to breastfeed longer.
Keywords: Breastfeeding, Botswana, PMTCT, HIV
Introduction
The rollout of three-drug antiretroviral therapy (ART) for prevention of mother to child transmission (PMTCT) has dramatically reduced HIV transmission between mothers and infants in low-resource settings[1–3]. Breastfeeding (BF) is a critical component of childhood survival in these same settings [4–7], and recent evidence suggests that HIV-infected women receiving ART may be able to safely breastfeed their infants [1, 8]. WHO recommends 1 year of breastfeeding (6 months exclusive, and 6 months with complementary feeding) with maternal ART prophylaxis for HIV-exposed infants to achieve optimal health, growth and development of the child [9].
HIV-infected women in poor settings face challenges in breastfeeding their infants for a full year [10–12]. In Botswana, where either formula feeding (formula provided free for up to a year) or 6 months of breastfeeding with maternal ART use are recommended feeding options for HIV-infected women, breastfeeding remains uncommon and short breastfeeding duration is the norm. While the choice to formula feed may reflect local counseling practices, it may also reflect concerns on the part of women that they may not be able to breastfeed for more than a few months due to work, school, or other obligations. Few studies have reported on factors that predict initiation and duration of breastfeeding among HIV-infected women [2, 13–17]. In the Mma Bana Study [2], we reported that more than a quarter of women who had chosen to breastfeed weaned their infants prior to 5 months. In this analysis, we set out to identify the risk factors associated with early breastfeeding cessation in the Mma Bana Study.
Methods
Study population
The Mma Bana study enrolled 730 HIV-infected women who intended to breastfeed their infants, and was conducted in two urban and two rural communities in southern Botswana. The study evaluated the safety and efficacy of different ART regimens for PMTCT during breastfeeding (9). The study randomized 560 HIV-positive pregnant women to either abacavir + zidovudine + lamivudine or to lopinavir/ritonavir + zidovudine + lamivudine from 26–34 weeks gestation to 6 months postpartum. A total of 170 women enrolled into the Botswana standard of care arm, which at the time of the study was combivir and nevirapine for HIV-infected pregnant women with a CD4 count < 200 copies/ml. All women were counseled to exclusively breastfeed for 5 months, and to wean to formula in the week prior to their 6-month visit (with complementary feeding added after 6 months). The study started enrolment in July 2006 and follow-up was completed in September 2010. All women who participated in the study provided written informed consent. The study was approved by the Botswana National Ethics Committee (Health Research Development Committee) and the Harvard School of Public Health ethics committee (Office of Human Research Administration). The study was registered with ClinicalTrials.gov (NCT00270296).
Data analysis
For the purpose of this analysis, the following data were extracted from the study database: baseline maternal characteristics (age, marital status, employment status, income, location) baseline CD4 cell count, maternal ART regimen, viral load, parity, gestational age of infants at birth, any documented ARV toxicity (mother and infants), illness of mothers and infants, duration of total breastfeeding and reasons for discontinuation earlier than recommended.
Univariate regression analysis using Cox’s proportional hazards model was used to assess baseline characteristics associated with early cessation of BF prior to 5 months. Women who reached 5 months while still breastfeeding were censored at that point, since weaning was recommended between 5 and 6 months. Women were counseled to wean within the 3 days prior to the 6 month visit, but because weaning counseling began at the 5-month visit (and prior to this visit exclusive BF was encouraged), any woman who opted to wean her baby after the 5-month visit and less than 3 days prior to the 6-month visit as encouraged, was supported by the study team. We used 5 months as the time point to evaluate the ability of women to adhere to exclusive BF. Women who did not initiate BF or those we did not have information on infant feeding practices were excluded from the analysis. Kaplan-Meier (KM) survival analysis was carried out to describe BF duration by variables of interest. We used visual inspection of KM curves in order to confirm non-violation of the proportionality assumption. Multivariable Cox proportional hazards regression model was carried out to determine hazard ratios (HRs) to estimate the instantaneous relative risk of early cessation of breastfeeding. All predictive variables with a p-value < 0.10 were considered for inclusion in the final multivariate model. The HRs and the corresponding 95% confidence intervals (CIs) were calculated. Statistical significance was defined at a p-value < 0.05. All analysis was conducted in STATA version 13.1 (StataCorp LP, College Station, Texas).
Results
Of 730 women enrolled in the Mma Bana Study, 677 (93%) initiated breastfeeding. Among these, 660 (97%) had a known weaning date and were assumed to BF throughout follow-up. The median time to BF cessation was 178 days (IQR 150–181), and 170 (25.1%) weaned prior to 5 months. Those who weaned early did so after a median of 75 days (IQR 46 – 107).
Table 1 summarizes univariate and multivariable associations of maternal and infant characteristics with early BF cessation. Univariate analysis showed that urban sites were significantly associated with early weaning (HR = 2.71; 95 CI1.95 – 3.75; p<0.001), Figure 1. Women who were either employed or students (54%) were mostly likely to wean before 5 months as compared with unemployed women (HR = 4.43; 95% CI 3.27 – 6.00; p <0.001). Lack of electricity and higher level of income (>500 BWP; approximately US$50 per month) were significantly associated with early cessation of BF (HR = 1.63 95% CI 1.22 – 2.17), (HR = 2.98; 95% CI 2.10 – 4.23; p < 0.001), respectively. Early BF cessation was significantly associated with younger maternal age [18–24 years (HR 1.38 95%CI 0.81–2.37; p=0.24); 25–34 years (HR 1.94 95%CI 1.16 – 3.23; p=0.011) vs. ≥ 35 years], higher education level (HR 1.79 95%CI 1.18–2.70; p=0.006), and more people in the household (>=5) [(HR 1.44 95% 1.07–1.95; p=0.017)]. Other significant predictors of BF cessation were infant hospitalization before weaning (HR = 1.62; 95% CI 1.08 – 2.42; p = 0.018), and infant grade 3/4 adverse events before weaning (HR = 1.60 95%CI 1.00 – 2.54; p= 0.048).
Table 1.
Characteristics of women and infants associated with early breastfeeding cessation
| Characteristic | Total | Weaned before 5 months |
Univariate Analysis Hazard Ratio (95% CI) |
P-value | Multivariate Hazard Ratio Analysis (95% CI) |
P-value |
|---|---|---|---|---|---|---|
| Sites | ||||||
| Rural | 315 | 49 (15.6%) | Ref | Ref | ||
| Urban | 362 | 137 (37.9%) | 2.71 (1.95 – 3.75) | < 0.001 | 1.86 (1.27–2.73) | 0.002 |
| Mothers Age (years) | ||||||
| 18 – 24 | 244 | 58 (23.8%) | 1.38 (0.81 – 2.38) | 0.239 | 1.36 (0.69 – 2.67) | 0.375 |
| 25 – 34 | 340 | 111 (32.7%) | 1.94 (1.16 – 3.23) | 0.011 | 1.63 (0.87 – 3.03) | 0.125 |
| 35 – 49 | 93 | 17 (18.3%) | Ref | Ref | ||
| Mothers Educational level | ||||||
| Primary and below | 146 | 26 (17.8%) | Ref | Ref | ||
| At least Secondary | 531 | 160 (30.1%) | 1.79 (1.18 – 2.70) | 0.006 | 1.58 (0.94 – 2.65) | 0.083 |
| Mothers Employment Status | ||||||
| Unemployed | 445 | 71 (16.0%) | Ref | Ref | ||
| employed or student | 192 | 104 (54.2%) | 4.43 (3.27 – 6.00) | < 0.001 | 2.78 (1.63 – 4.75) | <0.001 |
| Self-employed | 40 | 11 (27.5%) | 1.78 (0.94 – 3.36) | 0.075 | 1.23 (0.57 – 2.66) | 0.606 |
| Electricity in Household | ||||||
| Yes | 232 | 82 (35.3%) | Ref | Ref | ||
| No | 445 | 104 (23.4%) | 1.63 (1.22 – 2.17) | 0.001 | 0.79 (0.55 – 1.14) | 0.212 |
| Income | ||||||
| < 500 BWP (approx. US$50) | 238 | 87 (36.6%) | Ref | Ref | ||
| >= 500 BWP | 345 | 49 (14.2%) | 2.98 (2.10 – 4.23) | < 0.001 | 0.70 (0.41 – 1.20) | 0.195 |
| Number of People in Household | ||||||
| <5 People | 388 | 120 (30.9%) | Ref | Ref | ||
| ≥ 5 people | 289 | 66 (22.8%) | 1.44 (1.07 – 1.95) | 0.017 | 0.95 (0.67 – 1.36) | 0.793 |
| Infant Hospitalization before weaning | ||||||
| Yes | 72 | 28 (38.9%) | 1.62 (1.08 – 2.42) | 0.018 | 2.04 (1.21 – 3.45) | 0.008 |
| No | 605 | 158 (26.1%) | Ref | Ref | ||
| Infant Toxicity before weaning | ||||||
| Yes | 102 | 20 (19.6%) | 1.60 (1.00 – 2.54) | 0.048 | 1.70 (0.99 – 2.95) | 0.056 |
| No | 575 | 166 (28.9%) | Ref | |||
Figure 1.
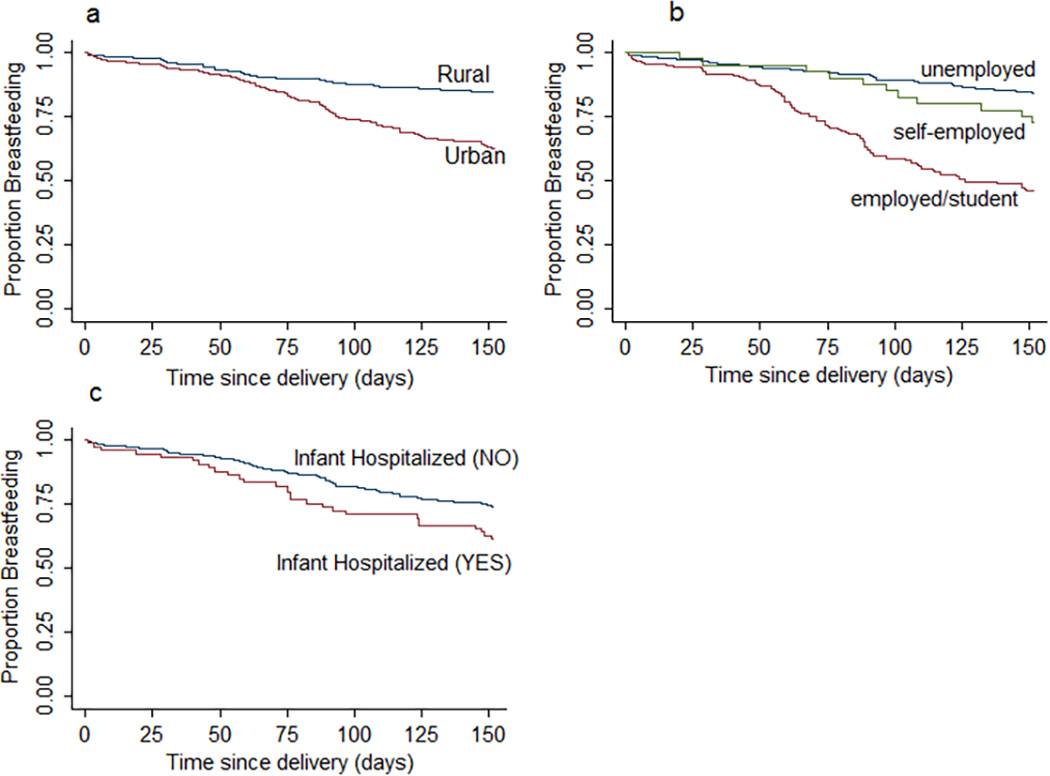
Kaplan- Meier curves for time to cessation of breastfeeding
In multivariable analysis (Table 1), urban location (aHR 1.86 95%CI 1.27–2.73; p=0.002), salaried employment or students (aHR 2.78 95%CI 1.63–4.75); p<0.001), and infant hospitalization before weaning (aHR 2.04 95% CI 1.21 – 3.45; p=0.008) were independently and significantly associated with early BF cessation. Variables that were assessed and found not to be significantly associated with breastfeeding cessation included marital status, parity, occurrence of mastitis, availability of toilet facilities, baseline CD4 cell count, baseline viral load, gestational age, birth weight, adherence to ARVs, prematurity and TB diagnosis (data not shown).
Discussion
Breastfeeding is a critical component of child survival and maybe most important among HIV-exposed children (both infected or uninfected) who have high rates of infant mortality [5, 11, 12, 18, 19]. Early cessation of breastfeeding has been associated with increased risk of infant mortality and morbidity in several studies in Africa [11, 19]. In this sub-analysis of the Mma Bana Study, we identified salaried employment, urban location, and infant hospitalization as the most import risk factors for early weaning. To our knowledge, this is the first study to describe factors associated with early cessation of breastfeeding among HIV-infected women in Botswana.
Previous studies in other settings have identified that maternal age, marital status or living with a partner, employment status, desire to return to work, ART regimen and experience of toxicity while breastfeeding may influence the duration of BF [10, 11, 15]. BF support and ongoing counseling, maternal illness, parity, previous BF experience have also been identified as key factors that predict duration of BF in HIV-negative women [13, 15]. In other studies, among HIV-infected women, it was suggested that breast infection or cracked nipples, prematurity or low birth weight in infants, delayed initiation of breastfeeding, insufficient breast milk, fear of transmitting the virus to the child, advice by relatives and friends, illness or drug-related toxicity in the infant and child’s refusal may also influence a mothers ability to breastfeed the child for the recommended duration [14, 16, 20, 21]. Our study did not find an association between breast infection (mastitis) or birth weight with cessation of BF.
We found three very clear risk factors for early BF cessation in our study: urban location, employment, and infant hospitalization. Rural women tended to breastfeed longer than urban women (even when adjusted for employment status) and may have more family and social support to continue BF in the pre-ART era in Botswana [22]. Women in urban areas may have had social or economic influences on their weaning decisions, and counseling may have differed in these regions [23]. Some studies have also found that women in urban settings face extremely complex situations with regard to breastfeeding due to multiple challenges related to work commitments[24]. Likewise, salaried employment was an independent predictor for early weaning. We believe that support mechanisms should be made available to help urban, employed women breastfeed longer, such as flexible working hours, locations at the workplace to either breastfeed or use manual breast pumps to maintain a diet of breast milk when mothers and infants are separated. Finally, infant hospitalization predicted early weaning, and we believe that nutritional support services and the availability of manual breast pumps might allow more infants to continue to receive breast milk while hospitalized and to continue breastfeeding upon discharge.
The primary limitation of our study was the protocol-driven recommendation that weaning occur prior to the 6-month visit, which was in accordance with WHO and Botswana guidelines at the time. This limited our ability to evaluate a more natural period of weaning later in infancy, and may have underestimated the number of women who would have weaned prior to the current WHO recommendation of 12 months. However, even this protocol-constrained duration of breastfeeding was similar to what has been observed in the region [25]. Another limitation was that women in this study were participating in a clinical trial and all agreed to breastfeed as part of the enrolment criteria, so we cannot generalize the findings to all women in Botswana. However, we believe that the high acceptance rate of breastfeeding among women referred to the study (only 9% declined because they preferred to formula feed [2]) and the comparable demographics of women in the study to the general population (data not shown) make these results broadly interpretable.
In summary, in this clinical trial of urban and rural HIV-infected women in Botswana, a large proportion started BF after detailed counseling, but >25% did not breastfeed for the recommended duration. Among those who stopped BF early, we identified urban location, salaried employment, and infant hospitalization as independent risk factors for early cessation. As countries continue to scale up BF among HIV-infected women who are receiving ART, it is critical to understand local factors that may influence HIV-infected women’s ability and willingness to initiate and adhere to the infant feeding recommendations. BF promotion interventions should address those who are less likely to initiate BF or less likely to maintain it for the recommended duration. In Botswana, improved support for BF among employed mothers in urban settings, and among hospitalized infants, may allow children to benefit from longer BF.
Acknowledgments
We would like to acknowledge the Mma Bana participants, study team members, the Botswana Ministry of Health and the Botswana-Harvard HIV Reference Laboratory for their support and contribution to the success of the Mma Bana study. The Mma Bana study was funded by the US government through an NICHD/NIAID grant. KP received salary funding during manuscript preparation from NICHD. SM’s effort was partially supported by a grant from OAK Foundation and from the Fogarty International Center. We thank Professor Marcello Pagano for his assistance to AO and SM during their McGoldrick Fellowship in Biostatistics Training at the Harvard T.H. Chan School of Public Health. The opinions, findings, and conclusions expressed in this article are those of the authors and do not necessarily reflect the views of the sponsors.
References
- 1.Chasela CS, Hudgens MG, Jamieson DJ, Kayira D, Hosseinipour MC, Kourtis AP, Martinson F, Tegha G, Knight RJ, Ahmed YI, et al. Maternal or infant antiretroviral drugs to reduce HIV-1 transmission. The New England Journal of Medicine. 2010;362(24):2271–2281. doi: 10.1056/NEJMoa0911486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shapiro R, Hughes M, Ogwu A, Kitch D, Lockman S, Moffat C, Makhema J, Moyo S, Thior I, McIntosh K. Antiretroviral regimens in pregnancy and breast-feeding in Botswana. The New England journal of medicine. 2010;362(24):2282. doi: 10.1056/NEJMoa0907736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shapiro RL, Kitch D, Ogwu A, Hughes MD, Lockman S, Powis K, Souda S, Moffat C, Moyo S, McIntosh K, et al. HIV transmission and 24-month survival in a randomized trial of HAART to prevent MTCT during pregnancy and breastfeeding in Botswana. AIDS. 2013;27(12):1911–1920. doi: 10.1097/qad.0b013e32836158b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Creek TL, Kim A, Lu L, Bowen A, Masunge J, Arvelo W, Smit M, Mach O, Legwaila K, Motswere C, et al. Hospitalization and mortality among primarily nonbreastfed children during a large outbreak of diarrhea and malnutrition in Botswana, 2006. Journal Acquired Immune Deficiency Syndrome. 2010;53(1):14–19. doi: 10.1097/QAI.0b013e3181bdf676. [DOI] [PubMed] [Google Scholar]
- 5.Boerma RS, Wit FW, Orock SO, Schonenberg-Meinema D, Hartdorff CM, Bakia A, van Hensbroek MB. Mortality risk factors among HIV-exposed infants in rural and urban Cameroon. Tropical medicine & international health : TM & IH. 2015;20(2):170–176. doi: 10.1111/tmi.12424. [DOI] [PubMed] [Google Scholar]
- 6.Goga AE, Doherty T, Jackson DJ, Sanders D, Colvin M, Chopra M, Kuhn L. Infant feeding practices at routine PMTCT sites, South Africa: results of a prospective observational study amongst HIV exposed and unexposed infants - birth to 9 months. International Breastfeed Journal. 2012;7:4. doi: 10.1186/1746-4358-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shapiro RL, Lockman S, Kim S, Smeaton L, Rahkola JT, Thior I, Wester C, Moffat C, Arimi P, Ndase P, et al. Infant morbidity, mortality, and breast milk immunologic profiles among breast-feeding HIV-infected and HIV-uninfected women in Botswana. J Infect Dis. 2007;196(4):562–569. doi: 10.1086/519847. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro RL, Hughes MD, Ogwu A, Kitch D, Lockman S, Moffat C, Makhema J, Moyo S, Thior I, McIntosh K, et al. Antiretroviral regimens in pregnancy and breast-feeding in Botswana. N Engl J Med. 2010;362(24):2282–2294. doi: 10.1056/NEJMoa0907736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. Guidelines on HIV and infant feeding 2010: principles and recommendations for infant feeding in the context of HIV and a summary of evidence. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 10.Doherty T, Sanders D, Jackson D, Swanevelder S, Lombard C, Zembe W, Chopra M, Goga A, Colvin M, Fadnes LT, et al. Early cessation of breastfeeding amongst women in South Africa: an area needing urgent attention to improve child health. BMC Pediatrics. 2012;12:105. doi: 10.1186/1471-2431-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haile D, Belachew T, Birhanu G, Setegn T, Biadgilign S. Predictors of breastfeeding cessation among HIV infected mothers in Southern Ethiopia: a survival analysis. PLoS One. 2014;9(3):e90067. doi: 10.1371/journal.pone.0090067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marquez C, Okiring J, Chamie G, Ruel TD, Achan J, Kakuru A, Kamya MR, Charlebois ED, Havlir DV, Dorsey G. Increased morbidity in early childhood among HIV-exposed uninfected children in Uganda is associated with breastfeeding duration. J Trop Pediatr. 2014;60(6):434–441. doi: 10.1093/tropej/fmu045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott JA, Binns CW, Oddy WH, Graham KI. Predictors of Breastfeeding Duration: Evidence From a Cohort Study. Pediatrics. 2006;117(4):e646–e655. doi: 10.1542/peds.2005-1991. [DOI] [PubMed] [Google Scholar]
- 14.Coovadia HM, Rollins NC, Bland RM, Little K, Coutsoudis A, Bennish ML, Newell ML. Mother-to-child transmission of HIV-1 infection during exclusive breastfeeding in the first 6 months of life: an intervention cohort study. The Lancet. 2007;369(9567):1107–1116. doi: 10.1016/S0140-6736(07)60283-9. [DOI] [PubMed] [Google Scholar]
- 15.McInnes RJ, Love JG, Stone DH. Evaluation of a community-based intervention to increase breastfeeding prevalence. Journal of Public Health. 2000;22(2):138. doi: 10.1093/pubmed/22.2.138. [DOI] [PubMed] [Google Scholar]
- 16.Mmiro FA, Aizire J, Mwatha AK, Eshleman SH, Donnell D, Fowler MG, Nakabiito C, Musoke PM, Jackson JB, Guay LA. Predictors of early and late mother-to-child transmission of HIV in a breastfeeding population: HIV Network for Prevention Trials 012 experience, Kampala, Uganda. Journal Acquired Immune Defic Syndrome. 2009;52(1):32–39. doi: 10.1097/QAI.0b013e3181afd352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kramer MS, Kakuma R. The optimal duration of exclusive breastfeeding: a systematic review. Adv Exp Med Biol. 2004;554:63–77. doi: 10.1007/978-1-4757-4242-8_7. [DOI] [PubMed] [Google Scholar]
- 18.Bork KA, Cournil A, Read JS, Newell ML, Cames C, Meda N, Luchters S, Mbatia G, Naidu K, Gaillard P, et al. Morbidity in relation to feeding mode in African HIV-exposed, uninfected infants during the first 6 mo of life: the Kesho Bora study. Am J Clin Nutr. 2014;100(6):1559–1568. doi: 10.3945/ajcn.113.082149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rollins NC, Ndirangu J, Bland RM, Coutsoudis A, Coovadia HM, Newell ML. Exclusive breastfeeding, diarrhoeal morbidity and all-cause mortality in infants of HIV-infected and HIV uninfected mothers: an intervention cohort study in KwaZulu Natal, South Africa. PLoS One. 2013;8(12):e81307. doi: 10.1371/journal.pone.0081307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nagelkerke NJD, Moses S, Embree JE, Jenniskens F, Plummer FA. The duration of breastfeeding by HIV-1-infected mothers in developing countries: balancing benefits and risks. JAIDS Journal of Acquired Immune Deficiency Syndromes. 1995;8(2):176. [PubMed] [Google Scholar]
- 21.Shapiro RL, Lockman S, Thior I, Stocking L, Kebaabetswe P, Wester C, Peter T, Marlink R, Essex M, Heymann SJ. Low adherence to recommended infant feeding strategies among HIV-infected women: results from the pilot phase of a randomized trial to prevent mother-to-child transmission in Botswana. AIDS Educ Prev. 2003;15(3):221–230. doi: 10.1521/aeap.15.4.221.23830. [DOI] [PubMed] [Google Scholar]
- 22.Omondi LO, Persson LA, Staugard F. Determinants for breast feeding and bottle feeding in Botswana. J Trop Pediatr. 1990;36(1):28–33. doi: 10.1093/tropej/36.1.28. [DOI] [PubMed] [Google Scholar]
- 23.Jacobson LT, Twumasi-Ankrah P, Redmond ML, Ablah E, Hines RB, Johnston J, Collins TC. Characteristics associated with breastfeeding behaviors among urban versus rural women enrolled in the Kansas WIC program. Maternal Child Health Journal. 2015;19(4):828–839. doi: 10.1007/s10995-014-1580-2. [DOI] [PubMed] [Google Scholar]
- 24.Kimani-Murage EW, Wekesah F, Wanjohi M, Kyobutungi C, Ezeh AC, Musoke RN, Norris SA, Madise NJ, Griffiths P. Factors affecting actualisation of the WHO breastfeeding recommendations in urban poor settings in Kenya. Maternal Child Nutrition. 2015;11(3):314–332. doi: 10.1111/mcn.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bland RM, Little KE, Coovadia HM, Coutsoudis A, Rollins NC, Newell ML. Intervention to promote exclusive breast-feeding for the first 6 months of life in a high HIV prevalence area. Aids. 2008;22(7):883–891. doi: 10.1097/QAD.0b013e3282f768de. [DOI] [PubMed] [Google Scholar]


