Abstract
Objective
Medical professionals adequately trained to prevent and treat substance use disorders are in short supply in most areas of the world. While physician training in addiction medicine can improve patient and public health outcomes, the coverage estimates have not been established. We estimated the extent of the need for medical professionals skilled in addiction medicine in a Canadian setting.
Methods
We used Monte Carlo simulations to generate medians and 95% credibility intervals for the burden of alcohol and drug use harms, including morbidity and mortality, in British Columbia, by geographic health region. We obtained prevalence estimates for the models from the Medical Services Plan (MSP) billing, the Discharge Abstract Database (DAD) data, and the government surveillance data. We calculated a provider availability index (PAI), a ratio of the size of the labour force per 1,000 affected individuals, for each geographic health region, using the number of American Board of Addiction Medicine certified physicians in each area.
Results
Depending on the data source used for population estimates, the availability of specialized addiction care providers varied across geographic health regions. For drug-related harms, we found the highest PAI of 23.72 certified physicians per 1,000 affected individuals, when using the MSP and DAD data. Drawing on the surveillance data, the drug-related PAI dropped to 0.46. The alcohol-related PAI ranged between 0.10 and 86.96 providers, depending on data source used for population estimates.
Conclusions
Our conservative estimates highlight the need to invest in health-care provider training and to develop innovative approaches for more rural health regions.
Keywords: substance use disorder, medical education, needs assessment, workforce, alcohol, SBIRT, opioids, agonist treatment, methadone, family medicine, implementation
INTRODUCTION
Medical professionals adequately trained in the prevention and treatment of substance use disorders are in short supply (Wood, et al., 2013). Furthermore, the historical lack of physician training in the discipline of Addiction Medicine has been described as “a monumental lost opportunity” in a report by the United State's (U.S.) National Centre on Addiction and Substance Abuse (CASA, 2000). This lack of accredited training and knowledge results in physicians failing to adequately diagnose and treat alcohol and substance use disorders (Ayu, et al., 2015; Klimas, 2015). Though advances in addiction science have helped to identify effective treatments for a variety of substance use disorders; these interventions are often under-utilized (Park, et al., 2014).
In North America, the treatment of substance use disorders is often provided by non-medical professionals without formal addiction training (e.g., counselors) (Columbia, 2012). Moreover, physicians who primarily treat people with a substance use disorder, may be providing care that does not approximate being evidence-based because their addiction training has failed to equip them with appropriate skills and knowledge “at every level—in medical school, residency training, continuing education and in practice” (National Center on Addiction and Substance Abuse at Columbia University, 2000). Currently, there is no recognized specialty in Addiction Medicine from the Royal College of Physicians and Surgeons of Canada or the College of Family Physicians of Canada (Oetter, 2005; BC Medical Association, 2009). As a result, most Canadian physicians with a focused interest in addiction medicine complete the American Board of Addiction Medicine examination.
To address this gap, new educational training programs devoted to the field of addiction medicine are being created internationally (The National Centre on Addiction and Substance Abuse at Columbia University, 2012). British Columbia (BC), Canada, is known as the first Western fellowship in Addiction Medicine (ADM), and, more recently, the host of the only Canadian fellowship in Addiction Medicine Research, funded by the National Institute of Drug Abuse (NIDA). There are three ADM fellowships in Canada, although no fellows have yet graduated from the two recently accredited programs. Although British Columbia has traditionally been known to have a persistent drug and HIV problem, innovative programming has led to success, by many measures (Hogg, et al., 2012). While government bodies have allocated funding for a number of health initiatives for the care of people with addiction, there remains an unmet need for physicians trained in Addiction Medicine.
The shortage in the addiction medicine workforce has been documented by several recent reports. A U.S. report indicated a shortage in the behavioral health workforce, which was defined as “professionals and support staff working in the field of Addiction and Mental Health”, when looking at service need (Advocates for Human Potential Inc., 2014). Similarly, the American Board of Addiction Medicine (ABAM) determined in another needs assessment that there is a need to certify at least 5,089 new physicians between 2010 and 2020 to satisfy a specialist-to-patient ratio of 1:1,000 (Tontchev, et al., 2011), in the U.S. In British Columbia, it is expected that this provider shortage will only increase with the new emphasis on integrating substance use disorder treatment with primary health care – a process that is paralleled across Canada. Canada's ageing workforce and staff turnover are likely to challenge the retention of specialist trained providers as well.
Addiction medicine training will expand the availability of physician education - among both fellows and eventually all physicians. While the benefit of physician training and education on patient- and public-health outcomes has yet to be determined (Humphreys, 2013), to our knowledge, coverage estimates have not been established in any Canadian setting. Therefore, we undertook a local need assessment, using a demand-side approach, to estimate the number of skilled addiction care providers required in a Canadian province.
METHODS
We assessed the extent of the need for medical professionals formally trained in addiction medicine in British Columbia, Canada. From publicly available sources, we obtained estimates of the prevalence of high-risk alcohol and drug use, as well as rates of substance use disorder in British Columbia, and used Monte Carlo simulation methods to generate a median value and 95% credibility interval for the burden of alcohol and drug use harms, including morbidity and mortality, in British Columbia, by geographic health region known as health authorities. For each of British Columbia's geographic health regions, we produced a provider availability index (PAI), a ratio of the size of the labour force per 1,000 affected people, using the registry of American Board of Addiction Medicine (ABAM) certified physicians “in good standing” to determine the number of addiction care providers, as of July 9, 2015 (table 1).
Table 1.
Number of American Board of Addiction Medicine (ABAM) certified physicians in “good standing” in BC by regional geographic health region, as of July 9, 2015.
| Provincial geographic health region | ABAM physicians in British Columbia (2015) (N=25) |
|---|---|
| Interior Health Authority | 3 |
| Fraser Health Authority | 2 |
| Vancouver Coastal Health Authority | 20 |
| Island Health Authority | 0 |
| Northern Health Authority | 0 |
‡ Note: the specifics of the diagnoses can be found in the reference.
Although used interchangeably throughout this report, terms “training” and “education” appear to have different meaning. Education usually refers to Continued Medical Education (CME) and medical school education. Training usually refers to residency or fellowship training, of at least 12-month duration.
Monte Carlo methods
People with alcohol use disorders (AUD) and substance use disorders (SUD) remain, in many ways, hidden populations; there is a high degree of uncertainty in hidden population estimates as many surveillance studies rely on self-reported use and are affected by bias (Degenhardt, et al., 2004; Van de Mortel, 2008; Roberts, et al., 2014). Therefore, Monte Carlo simulation with repeat random sampling based on parameter distribution estimates, was used to determine point estimates and credibility interval ranges for the burden of AUDs and SUDs in British Columbia. Monte Carlo simulation has been used in similar applications, using random sampling to accommodate population estimate uncertainty (Werb, et al., 2012). In a previous study, we used the simulation for estimating drug- and HIV- related indicators (Kuyper, et al., 2004; Hogg, et al., 2005; Milloy, et al., 2008).
Assumptions of the model
This model assumed parameter estimates for the population of people with AUDs and SUDs, as well as the regional population, by geographic health region. In an effort to triangulate numerous estimates provided in the literature, more than one definition and data source was used for the population estimates of AUD and SUD, to elicit a more meaningful range and estimate. The population affected by AUD was defined as those “chronically in excess of low-risk drinking guidelines” (LRDG) by self-report as documented by the Canadian Tobacco, Alcohol and Drugs Survey (CTADS) (CTADS, 2013), and those identified with alcohol use morbidity and mortality by geographic health region, as reported through the Medical Services Plan billing (MSP), the Discharge Abstract Database (DAD), and the alcohol sales data (Macdonald, et al., 2014). (Table 2) The population affected by SUD was defined as those with “any drug-related harm to self in the past year by self-report,” as was estimated by CTADS (CTADS, 2013), and those identified with drug use morbidity and mortality by geographic health region, as reported through MSP and DAD data in the MacDonald et al study (Macdonald, et al., 2014).
Table 2.
Monte Carlo model parameters, data sources, and values
| Parameter | Values | Source |
|---|---|---|
| Geographic health region population (2012) | BC Stats | |
| Interior Health Authority | 722,443 | |
| Fraser Health Authority | 1,661,375 | |
| Vancouver Coastal Health Authority | 1,122,946 | |
| Island Health Authority | 751,480 | |
| Northern Health Authority | 285,064 | |
| Geographic health region population (2013) | BC Stats | |
| Interior Health Authority | 720,694 | |
| Fraser Health Authority | 1,685,022 | |
| Vancouver Coastal Health Authority | 1,136,201 | |
| Island Health Authority | 754,066 | |
| Northern Health Authority | 285,995 | |
| Alcohol use morbidity per 100,000 (2013) | MacDonald et al. 2014 | |
| Interior Health Authority | 604.4 | |
| Fraser Health Authority | 331.6 | |
| Vancouver Coastal Health Authority | 337.9 | |
| Island Health Authority | 503.9 | |
| Northern Health | 741.0 | |
| Alcohol use mortality per 100,000 (2013) | MacDonald et al. 2014 | |
| Interior Health Authority | 33.0 | |
| Fraser Health Authority | 16.4 | |
| Vancouver Coastal Health Authority | 17.4 | |
| Island Health Authority | 28.6 | |
| Northern Health Authority | 35.3 | |
| Drug use morbidity per 100,000 (2013) | MacDonald et al. 2014 | |
| Interior Health Authority | 117.1 | |
| Fraser Health Authority | 77.4 | |
| Vancouver Coastal Health Authority | 69.3 | |
| Island Health Authority | 92.1 | |
| Northern Health Authority | 140.6 | |
| Drug use mortality per 100,000 (2013) | MacDonald et al. 2014 | |
| Interior Health Authority | 6.9 | |
| Fraser Health Authority | 7 | |
| Vancouver Coastal Health Authority | 6.3 | |
| Island Health Authority | 7.7 | |
| Northern Health Authority | 5.8 | |
* Province-wide, based on consumption in last 7 days; Butt et al. (2011)
† At least one of 8 harms to: physical health; friendships and social life; financial position; home life or marriage; work, studies, or employment opportunities; legal problems; difficulty learning; housing problems.
‡ Note: the specifics of the diagnoses can be found in the reference.
Derivation of model estimates
Where only province-wide population estimates were available, geographic health region-specific estimates were calculated using British Columbia Stats geographic health region population estimates by year (BC Stats, 2015). Where appropriate, and required, Standard Errors (SE) were derived from the Confidence Intervals (CI) and CIs were calculated using the Modified Wald Method (Agresti, et al., 1998; Higgins, et al., 2014). The Monte Carlo simulation model ran 10,000 trials using Oracle Crystal Ball (11.1.2.4) and assumed normal distribution of the population estimates.
Provider Availability Index (PAI)
Provider Availability Index (PAI) is an accepted metric used to express a ratio of the labour force in a certain medical field to the burden of disease in the population served by the medical field (Advocates for Human Potential Inc., 2014). A PAI was produced for each geographic health region, based on its size of the addiction physician labour force per 1,000 people with SUD and AUD, consistent with the previous research (Tontchev, et al., 2011; Advocates for Human Potential Inc., 2014).
The number of the American Board of Addiction Medicine (ABAM) certified physicians in “good standing” was used as a denominator for the number of addiction care providers, in lieu of a recognized speciality registry by either the Royal College of Physicians and Surgeons of Canada or the College of Family Physicians of Canada. Other potential data sources for addiction specialists in British Columbia, such as lists of Methadone or Suboxone licensed practitioners, are biased because they also include practitioners that are not actively prescribing or providing addiction care; moreover, there are no certifications that would allow us to estimate the number of providers that specialize in the care of people with AUDs. As a result, we decided that the only conservative measure for the number of current addiction care providers is the “ABAM certification in good standing”. We acknowledge that perhaps not all persons with alcohol or drug harm need a physician certified in addiction medicine, but for the purposes of this analysis assumed that all people with alcohol or drug harm would benefit from care provided by a physician certified in addiction medicine (ADM), because we didn't know about any morbidity cut-off for a non-ADM physician to pass on the treatment of substance use patients.
A new status of addiction medicine as an American Board of Medical Specialties (ABMS) subspecialty has been publically announced in late February 2016 (ASAM, 2015). The Addiction Medicine Foundation (recently renamed from The ABAM Foundation) has accredited the existing Canadian fellowships. At the time of writing this article, the Accreditation Council for Graduate Medical Education (ACGME), which is the official gold-standard accreditation body for physician training in the US, is developing accreditation requirements for addiction medicine fellowships. It is anticipated that information will be posted at www.abam.net by March 21, 2016.
RESULTS
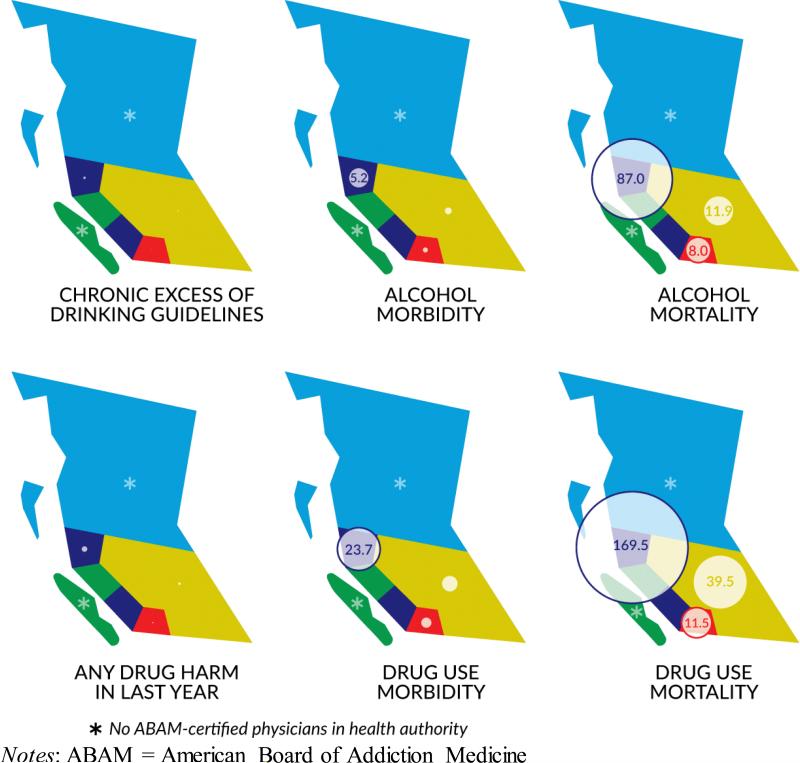
We identified significant variability in provider availability indices across geographic health regions depending on the data source used for population estimates. For drug use related harms, we found the highest PAI of 23.72 certified physicians per 1,000 affected people, using MSP billing and DAD data. However, using the self-reported CTADS data, the PAI dropped to 0.46 certified providers per 1,000 affected people. There was a similar, data-dependent variability in the PAI for alcohol use related harms, which ranged between 0.10 and 86.96 certified providers per 1,000 affected people in Vancouver Coastal Health Authority. The PAI was listed as zero for the Northern and Island Health Authorities, due to an absence of certified physicians.
Extent of the burden of alcohol and drug use harms
The forecasted number of individuals chronically exceeding low-risk drinking guidelines by self-report ranged from a median of 46,891 individuals (95% credibility interval (CI) 39,687-53,885) in Northern Health Authority to 276,271 individuals (95% CI 233,825-317,481) in Fraser Health Authority. The PAI for those in chronically in excess of low-risk drinking guidelines by self-report ranged from 0 providers per 1,000 in Northern and Island Health Authority to 0.10 providers per 1,000 in Vancouver Coastal Health Authority.
The forecasted number of individuals affected by alcohol use morbidity, by DAD, MSP, and liquor sale data, ranged from a median of 2,109 individuals (95% CI 2,006-2,211) in Northern Health Authority to 5,482 individuals (95% CI 5,284-5,680) in Fraser Health Authority. The PAI for alcohol use morbidity, by DAD, MSP, and liquor sale data, ranged from 0 providers per 1,000 in Northern and Island Health Authorities to 5.24 providers per 1,000 in Vancouver Coastal Health Authority.
The forecasted number of individuals affected by alcohol use mortality, by DAD, MSP, and liquor sale data, ranged from a median of 100 individuals (95% CI 83-117) in Northern Health Authority to 253 individuals (95% CI 211-297) in Interior Health Authority. The PAI for alcohol use mortality, by DAD, MSP, and liquor sale data, ranged from 0 providers per 1,000 in Northern and Island Health Authorities to 86.96 providers per 1,000 in Vancouver Coastal Health Authority.
The forecasted number of individuals affected by drug-related harms by self-report ranged from a median of 10,861 individuals (95% CI 7,124-14,587), in Northern Health Authority, to 63,988 individuals (95% CI 41,972-85,944) in Fraser Health Authority. The PAI for self-reported drug related harms in the last year ranged from 0 providers per 1,000 in Northern and Island Health Authorities to 0.46 providers per 1,000 in Vancouver Coastal Health Authority.
The forecasted number of individuals affected by drug use morbidity, by DAD and MSP data, ranged from a median of 399 individuals (95% CI 365-433) in Northern Health Authority to 1,337 individuals (95% CI 1,327-1,347) in Fraser Health Authority. The PAI for drug use morbidity by DAD and MSP data ranged from 0 providers per 1,000 in Northern and Island Health Authorities to 23.72 providers per 1,000 in Vancouver Coastal Health Authority.
The forecasted number of individuals affected by drug use mortality, by DAD and MSP data, ranged from a median of 30 individuals (95% CI 28-32) in Northern Health Authority to 174 individuals (95% CI 165-184) in Fraser Health Authority. The PAI for drug use mortality by DAD and MSP data ranged from 0 providers per 1,000 in Northern and Island Health Authorities to 169.49 providers per 1,000 in Vancouver Coastal Health Authority.
DISCUSSION
We found varying availability of comprehensive addiction medicine providers across British Columbia's health regions, depending on the data source used for population estimates. Previous studies in other countries have confirmed a widespread consensus that shortages in the provision of addiction-related care exist, particularly in rural areas (Knopf, 2014; Zornitsky, 2014). While some suggested that this body of research might have overestimated the extent of the problem, because it was based on provider surveys, our conservative estimates indicate the opposite effect (Ryan, et al., 2012). Moreover, previous labor-force research has relied on databases that were not specific for SUDs (Knopf, 2014). Therefore, the workforce deficit is likely to be underestimated, as the reliable data isn't there (De Silva, et al., 2014).
In light of our results, and the unique characteristics of the education system of British Columbia, a number of steps to address the variable availability of skilled addiction care providers could be taken moving forward. As most Canadian physicians who provide addiction care are primary care physicians, an emphasis should be placed on improving addiction medicine training specifically within family medicine residency programs. Additionally, since there is currently a service disparity between geographic health regions in British Columbia when looking at the availability of addiction specialists, and the prevalence of substance use disorders, innovative strategies (e.g. telemedicine support for primary care physicians) may be the most cost effective way to help improve access to specialized addiction care in more remote communities, while also working to expand addiction training for physicians local to the areas.
One could interpret the recognized rural shortage as the dislike of medical professionals to obtain specialist training in addiction medicine and their preference to live in that area upon training completion. Financial remuneration may also be a factor, as addiction physicians generally require more time per patient without any additional billing fees available to them (Woodward, et al., 2008; Cousins, et al., 2012). Nonetheless, our findings indicate that several regions in British Columbia, have problems with a specialized addiction care provider shortage that are likely to be improved by investing into addiction medicine training and education and improving remuneration. Such results are consistent with previous research in North America (Substance Abuse and Mental Health Services Administration, 2013).
Regardless of the reasons for the provider shortage, our assessment identified a great need for formal training in addiction medicine. Given the high burden of problematic substance use and the variable availability of local providers, our conservative estimates suggest that British Columbia needs to invest in addiction-care provider training and education to address the problem, particularly in Northern- and Island- Health Authorities which both currently lack physicians trained and certified by ABAM. Documenting the impact of fellowship training on the quality of care is a priority.
Our estimates are limited mainly by the sources of data and it is noteworthy that substance use disorder is often an under-reported disease. In a study by MacDonald et al (Macdonald, et al., 2014), alcohol and drug use-related population estimates were largely defined by physical morbidity and mortality data. Therefore, they were limited to those presenting to hospital or community clinicians, often with substance use as their main issue of concern. Data available through CTADS (CTADS, 2013) only reported the population affected by province. Geographic health region-specific figures(1) had to be extrapolated from province-wide estimates, and the burden of substance use disorder is likely to be variable between geographic health regions in British Columbia. This survey also relied on self-reported drug and alcohol use, and their associated harms that may be affected by social desirability and recall bias. There may also be sampling bias due to the survey being conducted through household landlines, which many youth, especially vulnerable youth, would not be accessible through. The definition of addiction specialists using ABAM certification may not accurately convey the number of practitioners with additional training or practical experience, pursued in lieu of formalized training access and college licensing requirements, in the field of addiction medicine. Finally, in areas with no “ABAM physicians in good standing”, such as Northern Health Authority and Island Health Authority, the PAI was not meaningful. Nevertheless, the Monte Carlo simulation yielded estimates and their confidence intervals that can serve as a first step in assessing the need for and planning the educational activities in the province. Addiction Medicine is a new budding specialty and both the Royal College and The College of Family Physicians do not have certifications in addiction currently but this does not mean that only ABAM certified physicians practice addiction medicine in Canada. Although ABAM certified physicians might be more likely to have focused addiction practices, using them as the only denominator metric may have underestimated the current number of physicians practicing addiction medicine, such as methadone or suboxone prescribers, or those involved in treatment of nicotine addiction. These physicians may not necessarily be comprehensive addiction medicine specialists, as they only practice one area of addiction medicine, but need to be acknowledged.
Figure 1.
Geographical representation of the provider availability index by geographic health region in a Canadian setting
Also in the future, with ABAM possibly no longer being available to certify Canadian physicians, and with the recent recognition of addiction medicine as an official subspecialty of ABMS, another metric will have to be used, pending the development of ‘Area of Focused Competency’ by the Royal College, or the ‘Certificate of Added Competency’ by the College of Family Physicians. Currently in Canada, there is also the Canadian Society of Addiction Medicine (CSAM) that offers certification to its members who have successfully completed the ABAM or ISAM examination (added the following text to the second to last paragraph).
Another limitation of the study is that we did not include data for physicians certified by the ABMS (American Board of Medical Specialties) member board ABPN (American Board of Psychiatry and Neurology) in the subspecialty of Addiction Psychiatry, American Osteopathic Association (AOA) or Academy of Osteopathic Addiction Medicine (AAOAM) certified physicians, physicians with methadone and suboxone licenses, members of Canadian Society of Addiction Medicine (CSAM) who completed the ABAM or ISAM examination, members of CSAM without the ABAM or ISAM certification, American Academy of Addiction Psychiatry (AAAP) certified psychiatrists and members of ASAM without certification. Future studies should strive to expand on our attempts to estimate the size of the addiction workforce shortage and include data for those professions, as well as for youth and pre-teens.
In summary, given the high burden of problematic substance use and the low local skilled provider availability, conservative estimates demonstrate the need to invest in health care provider training and education in addiction medicine. Since the health ministry locally is increasing its emphasis on the delivery of care through primary care providers, and since primary care physicians are perfectly positioned to provide addiction care, emphasis should be placed on training and education of primary care physicians in addiction medicine. In addition, given that more rural health regions have a dearth of comprehensive addiction care providers, innovative delivery models are likely required.
Table 3.
Monte Carlo simulation estimates of alcohol and drug related harms in British Columbia
| Parameter | Median | 95% Credible Interval | Provider availability index (per 1,000) |
|---|---|---|---|
| Chronic excess of low-risk drinking guidelines (2012)† | |||
| Interior Health Authority | 118,163 | 100,008-135,789 | 0.03 |
| Fraser Health Authority | 276,271 | 233,825-317,481 | 0.01 |
| Vancouver Coastal Health Authority | 186,288 | 157,667-214,076 | 0.10 |
| Island Health Authority | 123,634 | 104,639-142,076 | * |
| Northern Health Authority | 46,891 | 39,687-53,885 | * |
| Alcohol use morbidity (2013) | |||
| Interior Health Authority | 4,371 | 4,243-4,499 | 0.69 |
| Fraser Health Authority | 5,482 | 5,284-5,680 | 0.37 |
| Vancouver Coastal Health Authority | 3,817 | 3,684-3,956 | 5.24 |
| Island Health Authority | 3,794 | 3,660-3,931 | * |
| Northern Health Authority | 2,109 | 2,006-2,211 | * |
| Alcohol use mortality (2013) | |||
| Interior Health Authority | 253 | 211-297 | 11.86 |
| Fraser Health Authority | 250 | 149-347 | 8.00 |
| Vancouver Coastal Health Authority | 230 | 224-237 | 86.96 |
| Island Health Authority | 229 | 225-234 | * |
| Northern Health Authority | 100 | 83-117 | * |
| Any drug harm in the last year (2012)‡ | |||
| Interior Health Authority | 27,368 | 17,952-36,759 | 0.11 |
| Fraser Health Authority | 63,988 | 41,972-85,944 | 0.03 |
| Vancouver Coastal Health Authority | 43,147 | 28,302-57,952 | 0.46 |
| Island Health Authority | 28,636 | 18,783-38,461 | * |
| Northern Health Authority | 10,861 | 7,124-14,587 | * |
| Drug use morbidity (2013) | |||
| Interior Health Authority | 867 | 782-953 | 3.46 |
| Fraser Health Authority | 1,337 | 1,327-1,347 | 1.50 |
| Vancouver Coastal Health Authority | 843 | 776-909 | 23.72 |
| Island Health Authority | 677 | 588-766 | * |
| Northern Health Authority | 399 | 365-433 | * |
| Drug use mortality (2013) | |||
| Interior Health Authority | 76 | 72-80 | 39.47 |
| Fraser Health Authority | 174 | 165-184 | 11.50 |
| Vancouver Coastal Health Authority | 118 | 111-125 | 169.49 |
| Island Health Authority | 79 | 74-83 | * |
| Northern Health Authority | 30 | 28-32 | * |
Notes: BC= British Columbia, Canada
No ABAM certified physicians in this Geographic health region
Based on consumption in last 7 days; Butt et al. (2011)(Butt, et al., 2011)
At least one of 8 harms to: physical health; friendships and social life; financial position; home life or marriage; work, studies, or employment opportunities; legal problems; difficulty learning; housing problems.
Acknowledgments
Source of Funding:
We thank our colleagues and collaborators for their advice and help: Kanna Hayashi, Cheyenne Johnson, M-J Milloy, Bohdan Nosyk, Diane Pepin, Dan Riest, Kenneth Tupper and Dan Werb. This research was also undertaken, in part, by funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine, and by the US National Institutes of Health (R25DA037756) that supports Dr. Evan Wood. The ELEVATE grant: Irish Research Council International Career Development Fellowship – co-funded by Marie Cure Actions (ELEVATEPD/2014/6); and the Marie Sklodowska Curie Fellowship (701698) supports Dr. Jan Klimas.
Footnotes
Authors’ contributions:
JM collected and analysed all data. JK was a Postdoctoral Fellow, supervised the study. EW was his Mentor, conceived the study. JK and JM led preparation of the manuscript with feedback from all co-authors. KA, SN and AM contributed to the study design, focus group guide and/or facilitated access to participants. All authors read and approve the final manuscript.
Conflicts of Interest:
We report no conflicts of interest.
References
- 1.Wood E, Samet JH, Volkow ND. Physician education in addiction medicine. JAMA. 2013;310:1673–1674. doi: 10.1001/jama.2013.280377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CASA . Missed Opportunity: National survey of primary care physicians and patients on substance abuse, 2000. National Center on Addiction and Substance Abuse (CASA), Universidad de Columbia; Nueva York: 2000. [Google Scholar]
- 3.Ayu AP, Schellekens AFA, Iskandar S, Pinxten L, De Jong CAJ. Effectiveness and Organization of Addiction Medicine Training Across the Globe. European Addiction Research. 2015;21:223–239. doi: 10.1159/000381671. [DOI] [PubMed] [Google Scholar]
- 4.Klimas J. Training in addiction medicine should be standardised and scaled up. BMJ. 2015:351. doi: 10.1136/bmj.h4027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park TW, Friedmann PD. Medications for Addiction Treatment: An Opportunity for Prescribing Clinicians to Facilitate Remission from Alcohol and Opioid Use Disorders. Rhode Island medical journal (2013) 2014;97:20. [PMC free article] [PubMed] [Google Scholar]
- 6.Columbia C. Addiction medicine: closing the gap between science and practice. The National Center on Addiction and Substance Abuse (CASA) at Columbia University; New York: 2012. pp. 1–573. [Google Scholar]
- 7.National Center on Addiction and Substance Abuse at Columbia University . Missed opportunity: CASA national survey of primary care physicians and patients on substance abuse. National Center on Addiction and Substance Abuse at Columbia University; 2000. [Google Scholar]
- 8.Oetter H. Addiction medicine is a specialty- let's recognize it. BC Medical Journal. 2005;47:526. [Google Scholar]
- 9.BC Medical Association. Stepping forward: Improving addiction care in British Columbia. BC Medical Association. 2009 [Google Scholar]
- 10.The National Centre on Addiction and Substance Abuse at Columbia University Addiction medicine: closing the gap between science and practice. 2012 [Google Scholar]
- 11.Hogg RS, Heath K, Lima VD, et al. Disparities in the burden of HIV/AIDS in Canada. 2012 [Google Scholar]
- 12.Advocates for Human Potential Inc. The adequacy of the behavioral health workforce to meet the need for services: Overview of key findings. APH; 2014. [Google Scholar]
- 13.Tontchev GV, Housel TR, Callahan JF, Kunz KB, Miller MM, Blondell RD. Specialized training on addictions for physicians in the United States. Substance Abuse. 2011;32:84–92. doi: 10.1080/08897077.2011.555702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Humphreys K. Commentary on Gustafson et al. (2013): Can we know that addiction treatment has been improved without evidence of better patient outcomes? Addiction. 2013;108:1158–1159. doi: 10.1111/add.12144. [DOI] [PubMed] [Google Scholar]
- 15.Degenhardt L, Hall W, Warner-Smith M, Lynskey M. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. World Health Organization; Geneva: 2004. Illicit drug use. pp. 1109–1176. [Google Scholar]
- 16.Van de Mortel TF. Faking it: social desirability response bias in self-report research. 2008 [Google Scholar]
- 17.Roberts SP, Siegel MB, DeJong W, Jernigan DH. A comparison between brand-specific and traditional alcohol surveillance methods to assess underage drinkers’ reported alcohol use. The American journal of drug and alcohol abuse. 2014;40:447–454. doi: 10.3109/00952990.2014.938160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Werb D, Nosyk B, Kerr T, Fischer B, Montaner J, Wood E. Estimating the economic value of British Columbia's domestic cannabis market: Implications for provincial cannabis policy. International journal of drug policy. 2012;23:436–441. doi: 10.1016/j.drugpo.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Kuyper LM, Hogg RS, Montaner JS, Schechter MT, Wood E. The cost of inaction on HIV transmission among injection drug users and the potential for effective interventions. J Urban Health. 2004;81:655–660. doi: 10.1093/jurban/jth148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hogg RS, Strathdee S, Kerr T, Wood E, Remis R. HIV prevalence among aboriginal British Columbians. Harm reduction journal. 2005;2:26. doi: 10.1186/1477-7517-2-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Milloy MJ, Kerr T, Tyndall M, Montaner J, Wood E. Estimated drug overdose deaths averted by North America's first medically-supervised safer injection facility. PLoS One. 2008;3:e3351. doi: 10.1371/journal.pone.0003351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.CTADS [November 16, 2015];Canadian Tobacco, Alcohol and Drugs Survey (CTADS) 2013 Available at: http://healthycanadians.gc.ca/science-research-sciences-recherches/data-donnees/ctads-ectad/index-eng.php.
- 23.Macdonald S, Joordens C, Slaunwhite A, Greer A. Estimates of alcohol and other drug-related harms across british columbia. Centre for Addiction Research of BC; Victoria, BC: 2014. [Google Scholar]
- 24.BC Stats [November 16, 2015];Sub-provincial population projections. 2015 Available at: http://www.bcstats.gov.bc.ca.ezproxy.library.ubc.ca/StatisticsBySubject/Demography/PopulationProjections.aspx.
- 25.Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. The American Statistician. 1998;52:119–126. [Google Scholar]
- 26.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. 5.1.0 ed. Wiley Online Library; 2014. [Google Scholar]
- 27.ASAM . ASAM Magazine. ASAM; Chevy Chase, MD: 2015. American Board of Preventive Medicine (ABPM) Begins Formal Process to Bring Addiction Medicine into American Board of Medical Specialties as Subspecialty, Available to Diplomates of all ABMS Boards. [Google Scholar]
- 28.Knopf A. Firm quantifies extent of addiction workforce shortage. Addiction Professional. Vendome Group, LLC; 2014. [Google Scholar]
- 29.Zornitsky J. The Adequacy of the Behavioral Health Workforce to Meet the Need for Services Overview of Key Findings. Advocates for Human Potential, Inc.; Albany, NY: 2014. [Google Scholar]
- 30.Ryan O, Murphy D, Krom L. Vital Signs: Taking the Pulse of the Addiction Treatment Workforce, A National Report, Version 1. Addiction Technology Transfer Center National Office in residence at the University of Missouri-Kansas City; Kansas City, MO: 2012. [Google Scholar]
- 31.De Silva MJ, Lee L, Fuhr DC, et al. Estimating the coverage of mental health programmes: a systematic review. International Journal of Epidemiology. 2014;43:341–353. doi: 10.1093/ije/dyt191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woodward AM, Raskin IE, Blacklow B. A profile of the substance abuse treatment industry: organization, costs, and treatment completion. Subst Use Misuse. 2008;43:647–679. doi: 10.1080/10826080601096640. [DOI] [PubMed] [Google Scholar]
- 33.Cousins SJ, Antonini VP, Rawson RA. Utilization, measurement, and funding of recovery supports and services. J Psychoactive Drugs. 2012;44:325–333. doi: 10.1080/02791072.2012.718924. [DOI] [PubMed] [Google Scholar]
- 34.Substance Abuse and Mental Health Services Administration . Report to the congress on the nation's substance abuse and mental health workforce issues. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; Rockville, MD: 2013. [Google Scholar]
- 35.Butt P, Beirness D, Gliksman L, Paradis C, Stockwell T. Alcohol and health in Canada: A summary of evidence and guidelines for low-risk drinking: Canadian Centre on Sustance Abuse. 2011 [Google Scholar]