Abstract
Background
To describe the study methods, baseline characteristics and burden of study procedures of an intervention designed to reduce family stress symptoms through early support from the palliative care team. Length of stay of ≥8 days was the trigger for early palliative care involvement.
Methods
Cluster-randomized trial with children as the unit of randomization. Up to 3 family members per child were recruited. Family stress symptoms were recorded at baseline, discharge from the ICU, and 3 months post-enrollment. Questionnaire burden was assessed on a 1–10 point scale at each time point and open-ended comments were analyzed to describe the participants’ experience in the study.
Results
380 family members of 220 children (control=115 children and 204 family members; intervention=105 children and 176 family members) were recruited, which represented 50% of all eligible families. Most family participants were parents (86% control; 92% intervention) and female (66% both groups). Retention rates were high through the 3-month follow-up: 93% and 90% for the control and intervention groups respectively. Questionnaire burden was very low: mean (sd) scores were 1.1 (1.6), 0.7 (1.5), and 0.9 (1.6) for the baseline, discharge and follow-up questionnaires, respectively. Comments suggest that participation was beneficial by promoting reflection and self-awareness about stress, coping and resilience, and feeling cared for because the intervention and questionnaires focused on their own well-being.
Conclusions
The participants’ comments regarding the focus on them as the point of intervention reflects the value of conducting research with family members of seriously ill children during ICU stays.
Keywords: pediatrics, family/caregivers psychology, stress disorders, psychological adaptation, intensive care unit, randomized trial
1. Introduction
The pediatric intensive care unit (PICU) is an emotionally-charged atmosphere that places significant demands on patients and families. Conflicts between the family and the ICU team regarding care decisions are common, occurring in over 50% of cases when children are hospitalized in intensive care for more than a week [1]. The stress of having a child in the PICU can have negative effects on parents’ short- and long-term psychosocial outcomes, including reduced capacity to resume parental caregiving [2–5]. Studies conducted in different pediatric hospital settings suggest that 11–21% of parents report clinical post-traumatic stress disorder (PTSD), with over 80% of parents reporting 1 or more post-traumatic stress symptom (PTSS) [2, 6, 7]. Parental acute and long-term stress symptoms are associated with worries about a child’s death, unintentional injury, and unexpected hospital admissions – all common scenarios in pediatric ICUs [2, 7, 8].
Good communication skills are essential in the PICU setting because of the high stakes decisions, informational needs of families, and the numerous potential differences in understanding, values and preferences between clinicians and families [9–12]. Communication is critical to establishing trust and providing the foundation for family-centered care [13–15]. Parents often prefer that the detailed technical information given during rounds or daily updates be integrated into a larger context so that they can understand individual treatments, changes in status and decisions within a “big picture” perspective of their child’s overall care [12]. While clinical data are important, many families prioritize quality of life in their decision making, but this aspect of care is rarely addressed until the child is in crisis. Frequently, PICU clinicians engage in frank discussions about prognosis only after they gauge the future quality of life as unacceptable, at which point they use this information to suggest discontinuation of life-support interventions [12], despite research that documents parents’ desires for communication that is “honest, inclusive, compassionate, clear, and comprehensive” throughout their stay [15].
This paper reports on the design and methods of a randomized trial of an intervention designed to reduce stress symptoms among family members by providing support with clinician-family communication and decision making early in the course of long pediatric ICU admissions. Length of stay of ≥8 days was the trigger for routine palliative care consultation. Participants’ characteristics at baseline and family evaluations of the burden of study participation are also reported.
2. Materials and Methods
2.1 Study aims
The aims of the randomized trial were to: (1) evaluate the effectiveness of prospective involvement of the palliative care team on reducing family members’ acute and long-term stress symptoms; (2) examine the efficacy of the intervention on PICU length of stay and total costs; and (3) elicit family views on the stressors and supports of their experience in the ICU using qualitative interviews. Family members’ perceptions of the burdens and benefits of study participation were also examined.
This trial is registered with Clinicaltrials.gov (number NCT02144779) and all procedures were reviewed and approved by the Institutional Review Board of Seattle Children’s Hospital. All family participants signed consent forms and parents signed medical records release forms giving permission to use their child’s medical records data.
2.2 Study setting
The study took place at Seattle Children’s Hospital (SCH) which serves a culturally and linguistically diverse population, drawn from a 5-state region. SCH has 3 separate ICUs including a PICU that provides critical care for a range of conditions, including bone marrow and organ transplantation; a cardiac ICU (CICU) that does advanced surgeries for congenital and neonatal conditions; and a level IV neonatal ICU (NICU). It also is 1 of 3 pediatric institutions in the Pacific Northwest that offers extracorporeal life support for neonates and children [16]. In 2010 when the study began, there were 35 intensive care unit beds including, 12 cardiac (CICU), 14 pediatric ICU (PICU) and 19 neonatal (NICU) beds. In 2013, the ICUs expanded to a new wing and added 31 more beds for a total of 66 beds for all 3 units.
2.3 Sample size and power calculations
Sample size was determined by power calculations, performed using Optimal Design for Multi-level and Longitudinal Research, version 1.76, to detect an effect size of 0.20 on the primary outcome of PTSD symptoms at 3 months. Sample size estimates were based on the following assumptions, given that patient and family member data were clustered: (1) an intraclass correlation coefficient of 0.20 [17]; (2) an average cluster size of 2, assuming an average of 2 family members per patient; (3) an effect size of 0.20; and (4) alpha coefficient of 0.05. A sample size of 156 patients was determined to have 0.80 power to detect an effect size of 0.20; the final target sample of 220 children and their families was selected to allow for an estimated 30% loss to follow-up.
2.4 Recruitment and randomization
Participants were recruited between July 2010 and March 2014. Study staff made rounds in the ICUs 3–5 times per week to ask charge nurses to identify children who did not have a current discharge plan on day 4, as this was a reliable indicator that the child was likely to still be in the ICU on day 8. The patient’s primary nurse served as an intermediary and introduced the study to the patient’s family with a short written information statement, and obtained verbal consent for study staff to discuss potential study participation. Study staff followed up with families and recruited 1 to 3 family members per child. Families were given several days to consider participation and study staff were sensitive not to approach families on or after days when the child was going to surgery or when the primary nurse advised against it (for example, citing that the family was having a challenging day or processing information and not amenable to meeting anyone else that day). In these cases, study staff followed up the next day. Families who were not enrolled by day 15 of the ICU stay became ineligible for participation.
A random number table in blocks of 8 was used to assure that any changes in the environment over time would be distributed between the 2 groups. The recruiter drew blinded assignments from sealed envelopes that were numbered consecutively from 1–225. After family members gave consent to participate and completed the baseline questionnaire, the recruiter opened the next envelope in the series and informed family members of their group assignment. Intervention families were assigned to a specific member of the palliative care team based on team member availability at the time of randomization.
2.5 Description of the theoretical framework
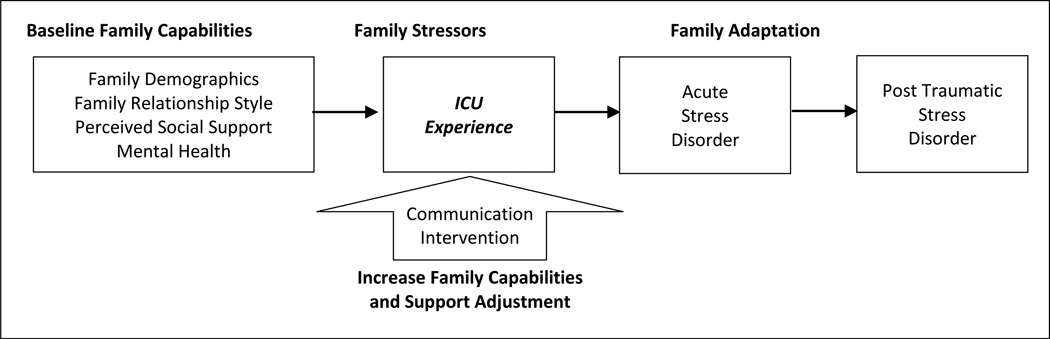
The intervention was based on concepts from Patterson’s theory of Family Adjustment and Adaptation Response (FAAR) [18], and adapted to incorporate elements of successful communication interventions [2, 19, 20]. The FAAR theory articulates the ways in which families adjust and adapt to the demands imposed on them in times of crisis (in this instance, their child’s admission to the ICU), given their capabilities and resources [18]. Figure 1 illustrates the operative concepts supporting this intervention: (1) at baseline, families possess different capabilities in terms of their tangible and psychosocial resources, as well as their coping behaviors that help them deal with the stress of having their child in the ICU; (2) the experience of long stays in the PICU is inherently stressful and disruptive to family capabilities and demands; (3) the intervention will bolster family capabilities and reduce sources of stress by improving communication, reducing conflict, and providing emotional and instrumental support earlier in the child’s ICU stay; (4) the intervention will improve family adaptation by reducing acute stress symptoms (a precursor to PTSD) at ICU discharge; and (5) the reduction in acute stress symptoms in the intervention group at discharge will reduce the incidence of PTSD symptoms at 3 months post enrollment.
Figure 1.
Family Adjustment and Adaptation Response Framework (FAAR) Informing Intervention Design
Lengths of stay in the ICU of 8 days or longer were selected as the trigger for enrollment as the literature suggests that stress accumulates with longer admissions [2, 6, 7] and the eighth day represented the 85th percentile for length of stay in ICUs at SCH. This alone is an indicator of the severity of the child’s condition and reason enough to warrant early involvement of an extra layer of support provided by the palliative care team. In addition, there is scant evidence about what patient- or family-level characteristics are reliably predictive of developing these stress symptoms. Thus, this trigger was selected as it was an objective criterion that could be clearly defined, implemented, and evaluated.
2.6 Control and intervention activities
The control condition was usual care in the ICU, which included state-of-the-art clinical care in a highly technical and interdisciplinary environment. Clinician-family communication typically occurs during informal bedside conversations with members of the child’s care team and during daily rounds, which are optional for families.
The intervention comprised an automatic consultation with families within 72 hours of randomization by 1 of the members of the Pediatric Advanced Care Team (PACT). Starting around day 8 of their child’s ICU stay, PACT members (who included 2 nurses, 2 social workers, 3 chaplains, and a child life specialist) contacted intervention families to develop and maintain relationships, and follow them through the transition to a lower acuity setting in the hospital. The focus of their expertise is on providing communication and decision-making support, and developing and implementing a care plan that incorporates the medical condition and is consistent with the patient’s and family’s understanding of the long-term prognosis in the context of their values and preferences. The intervention included (but was not limited to) the following activities: (1) an initial assessment of the family’s values and understanding of their child’s situation and any communication, support, or information needs; (2) documentation of this initial assessment using a structured template (described below); (3) a minimum of 2 weekly check-ins with the family (and more, as needed); (4) relaying information between the families and their care teams about the families’ context, values and preferences; (5) facilitation of goals of care discussions and care conferences; and (6) the provision of care coordination and referrals for instrumental and social support.
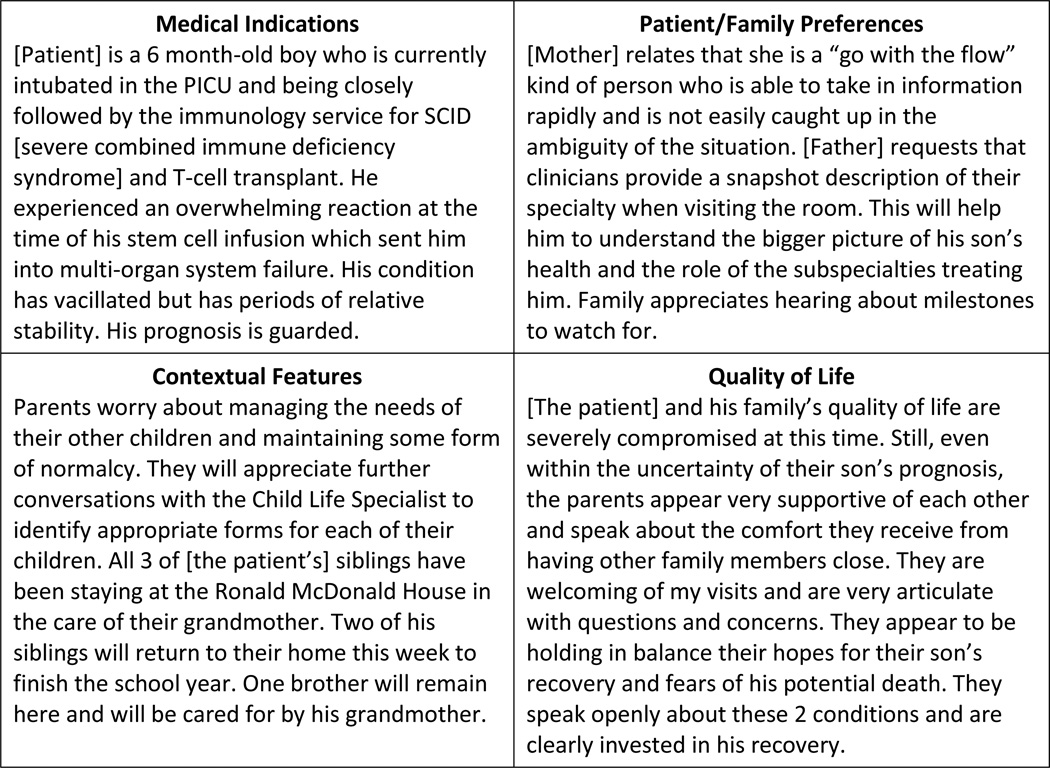
PACT consultants served as an additional layer of support for family members and provided continuity across multiple attending physicians who rotate off service weekly. They use a documentation template based on Jonsen, Siegler and Winslade’s 4-box structure for ethics consultations. This template is used to elicit and document the medical indications, patient and family preferences, quality of life issues, and contextual features related to the child’s illness and medical decision making [21]. This structured template was part of a successful demonstration project with the PACT team [22] and is now used to document and communicate important features of the family’s experience. Figure 2 shows an example of the content in a typical note; some of the details have been changed to preserve the family’s anonymity.
Figure 2.
Example of Consult Note Template
2.7 Data collection procedures and measures
Information was collected from families at baseline, when the patient was discharged from the ICU, and at 90-days post enrollment. Data were collected using paper questionnaires at baseline and ICU discharge, and by phone for the 90-day outcomes assessment. Each participant was offered a $20 gift card for each questionnaire they completed for a possible total of $60 if all 3 assessments were done. Families with 2–3 participating members could thus receive up to $180 over the 3-month study period.
Table 1 describes the measures and when they were collected. The questionnaires included the Family Relationships Index (FRI) to assess relationship cohesiveness, expressiveness and conflict [23]; the Multidimensional Scale of Perceived Social Support (MSPSS) for perceived social support from family, friends and a significant other [24, 25]; the Wake Forest Trust Scale to assess family perceptions of the physicians and nurses caring for their child [26]; the Patient Health Questionnaire (PHQ-9)[27, 28], General Anxiety Disorder (GAD-7) [29], the Acute Stress Disorder Scale (ASDS) [30], and the PTSD Checklist (PCLC) [31] to assess symptoms of depression, anxiety, and acute- and post-traumatic stress disorder. All questionnaires were available in either English or Spanish.
Table 1.
Measures collected
| MEASURES | No. of items | Enrollment | Discharge | 3 mos |
|---|---|---|---|---|
| Family: | ||||
| Family relationship index (FRI) | 12 | X | X | |
| Acute Stress Disorder Scale (ASDS) | 18 | X | ||
| Prior illness & hospitalizations for the child | 8 | X | ||
| Depression symptoms (PHQ-9) | 9 | X | X | X |
| Generalized anxiety disorder (GAD-7) | 7 | X | X | X |
| Wake Forest Trust Scale | 8 | X | ||
| Perceived social support (MSPSS) | 12 | X | X | |
| Demographics | 14 | X | ||
| Questionnaire burden | 2 | X | X | X |
| Quality of Communication (QOC) | 8 | X | ||
| Conflict with ICU care team | 1 | X | ||
| Evaluating intervention team (intervention group only) | 4 | X | ||
| Transition from the ICU to lower acuity setting | 6 | X | ||
| Post-Traumatic Stress Disorder (PCL-C) | 17 | X | ||
| Child: | ||||
| Length of stay (ICU & total hospitalization) | 2 | X | ||
| Resource utilization (ICU and total) | 2 | X | ||
| Demographics | 5 | X | ||
| Severity of illness | 1 | X | ||
| Vital status | 1 | X | X | |
In addition to these measures, at baseline family members answered questions about their demographics, past history with their child’s illness, and specific worries related to this hospitalization. At approximately weekly intervals during the ICU stay, family members completed questionnaires assessing satisfaction with communication and perceptions of conflict using 8 items from the Quality of Communication (QOC) scale [32]. For the intervention families, QOCs were collected weekly after PACT visits and organized care conferences; and at weekly intervals for control group families.
Child outcomes included length of stay and total costs, both in the ICU and for the overall hospitalization. Cost data were provided by the hospital’s finance department. Demographic, clinical, and administrative data for the child were extracted from the electronic medical record. Severity of illness was computed for each child using the APR Severity Rating, version 26 [33]. Scores are computed from ICD-9 codes assigned at discharge and range from 1 (mild) to 4 (severe).
The baseline, discharge, and 3-month follow-up questionnaire included 93, 28 and 70 items, respectively. To assess the burden of completing these questionnaires, the last item on each was a 1–10 point Likert scale rating of the question “how much of a burden was it to complete this questionnaire?” This was followed by a space for participants to provide comments on any aspect of the study or questionnaire they wished to share with the study team.
2.8 Analytic methods
This report includes the details of the intervention as well as the recruitment, participation rates, and an analysis of the burden of completing study questionnaires. This paper provides more detail on these components of the trial than would be possible in a report of the main results; the analyses for the main results and qualitative interviews will be reported in future papers.
Descriptive statistics were used to summarize the family and child demographics. For the analysis of questionnaire burden, mean scores were computed at each time point. We also conducted a thematic content analysis [34, 35] of the written comments to identify the themes associated with the burdens and benefits of study participation.
3. Results
3.1 Enrollment and retention
To achieve the target sample size of 220 children, we screened 4,645 admissions to the ICU. As expected, the vast majority of these admissions (91%; n=4,208) did not meet inclusion criteria. Seventy-six families declined to participate and 141 families were excluded for other reasons including: study staff could not reach family members despite multiple attempts (n=71); the child was discharged prior to enrollment (n=26); study staff were not available (n=11); recruitment was on hold when the interventionists were at capacity (n=7); and the parent was too distressed (n=1). The reason was not determined for another 25 families. Recruitment totaled 220 children and 380 of their family members (control=115 children and 204 family members; intervention=105 children and 176 family members), which represented 50% of all eligible children. The overall retention rate was 92% (control=93%, 14/204; intervention= 90%, 17/176).
3.2 Participant characteristics at baseline
Tables 2 and 3 report the details of the child and family member characteristics at baseline. There were no significant differences between the groups for any of these measures. The children’s ages at admission ranged from 0 days (birth) to 19 years. They were all seriously ill, as reflected in the average severity of illness score of 3.8 (range 2–4, both groups). Most family participants were parents (86% control; 92% intervention) and female (66% both groups).
Table 2.
Children’s characteristics
| All | Control | Intervention | |
|---|---|---|---|
| Characteristics | 220 | 115 | 105 |
| Unit, N (%) | |||
| CICU | 91 (42%) | 51 (44%) | 40 (38%) |
| PICU | 74 (33%) | 38 (33%) | 36 (34%) |
| NICU | 55 (25%) | 26 (23%) | 29 (28%) |
| Female, N (%) | 90 (41%) | 46 (40%) | 44 (42%) |
| Age at admission, mean (sd) | |||
| CICU (y=years) | 1.7 (4.4) y | 1.3 (3.9) y | 2.2 (5.0) y |
| PICU (y=years) | 4.0 (6.3) y | 3.5 (6.0) y | 4.6 (6.7) y |
| NICU (d=days) | 25.7 (36.1) d | 22.6 (38.7) d | 28.4 (34.0) d |
| Ethnicity, N (%) | |||
| White | 131 (60%) | 64 (56%) | 67 (64%) |
| Black | 11 (5%) | 7 (6%) | 4 (4%) |
| American Indian/Alaska Native | 11 (5%) | 7 (6%) | 4 (4%) |
| Asian | 7 (3%) | 3 (3%) | 4 (4%) |
| Pacific Islander | 2 (1%) | 2 (2%) | 0 (0%) |
| Other/Not answered | 27 (12%) | 12 (10%) | 15 (14%) |
| Multiple | 31 (14%) | 20 (17%) | 11 (10%) |
| Hispanic, N (%) | 44 (20%) | 23 (20%) | 21 (20%) |
| Severity of illnessa, mean (sd) | 3.8 (0.5) | 3.8 (0.5) | 3.8 (0.5) |
| PACT involved, N (% yes) | 125 (57%) | 26 (23%) | 99 (94%) |
| PACT referral day, mean (SD) | 13.7 (9.4) | 26 (14.1) | 10.4 (3.1) |
| PACT length of involvement, median (IQR) | 40 (15–68) | 31 (14–52) | 41 (18–76) |
Severity of illness measured by the APR Severity Rating (v. 26) [33]. Scores range from 1 (mild) to 4 (severe).
Table 3.
Family member characteristics at baseline
| All | Control | Intervention | |
|---|---|---|---|
| Characteristics | 380 | 204 | 176 |
| Age, mean (sd) | 33.8 (10.3) | 34.1 (11.0) | 33.4 (9.6) |
| Ethnicity, N (%) | |||
| White | 251 ( 68%) | 127 ( 64%) | 124 ( 72%) |
| Black | 20 (5%) | 11 (6%) | 9 (5%) |
| American Indian/Alaska Native | 19 (5%) | 9 (5%) | 10 (6%) |
| Asian | 12 (3%) | 5 (3%) | 7 (4%) |
| Pacific Islander | 5 (1%) | 5 (3%) | 0 (0%) |
| Other | 34 (9%) | 19 (10%) | 15 (9%) |
| Multiple categories | 29 (8%) | 22 (11%) | 7 (4%) |
| Hispanic, N (%) | 42 (11%) | 27 (14%) | 15 (9%) |
| Language, N (%) | |||
| English | 334 (89%) | 182 (90%) | 152 (87%) |
| Spanish | 24 (6%) | 12 (6%) | 12 (7%) |
| Other | 19 (5%) | 8 (4%) | 11 (6%) |
| Working at time of child’s hospitalization, N (%) | 221 (59%) | 110 (55%) | 111 (64%) |
| Household size, mean (sd) | 4 (1.7) | 4.1 (1.7) | 3.9 (1.7) |
| Marital status, N (%) | |||
| Never married | 75 (20%) | 41 (20%) | 34 (19%) |
| Married/living with partner | 273 (73%) | 146 (73%) | 127 (73%) |
| Divorced/separated | 25 (7%) | 13 (6%) | 12 (7%) |
| Widowed | 3 (1%) | 1 (<1%) | 2 (1%) |
| Annual income, N (%) | |||
| ≤$25,000 | 90 (24%) | 55 (27%) | 35 (20%) |
| $25–50,000 | 75 (20%) | 36 (18%) | 39 (22%) |
| $50–75,000 | 69 (18%) | 37 (18%) | 32 (18%) |
| >$75,000 | 96 (25%) | 44 (22%) | 52 (30%) |
| Declined to answer | 50 (13%) | 32 (16%) | 18 (10%) |
| Education, N (%) | |||
| 8th grade or less | 11 (3%) | 5 (3%) | 6(3%) |
| Some high school | 30 (8%) | 9 (5%) | 21 (13%) |
| High school/GED | 92 (24%) | 51 (25%) | 41(23%) |
| College | 196 (52%) | 107 (53%) | 86 (49%) |
| > 4 year college | 40 (10%) | 22 (11%) | 18 (10%) |
| Declined to answer | 11 (3%) | 7 (3%) | 4 (2%) |
3.3 Burden and benefits of participation
The burden scores were very low on the 0–10 point scale: for the baseline, discharge and follow-up questionnaires, respectively, the mean (sd) scores were 1.1 (1.6), 0.7 (1.5), and 0.9 (1.6). Participants' comments were mostly positive and described several benefits of participation. Participants wrote that the questionnaires gave them an opportunity to “vent” their feelings and "get things off [their] chest." The questionnaires also gave them increased self-awareness about their stress, coping and resilience. For example, a mother said, “[I] just want to thank you for this survey. It made me realize how I am doing, concerning the situation. I am holding on pretty well.” Another said, “The questionnaire was helpful for me to see the stress and anxiety this experience has created for me.” Family members also reported feeling cared about. Two examples are: “I would just like to say it’s nice to see someone care about these things that affect me – no one has ever shown that before, so I thank you” and “It’s nice to know that the well-being of the families are being considered.” Many offered that their primary motivation for participation was a desire to help other families in the future who might be going through similar stressful situations. As another family member said: “I think this study can be used to strengthen the ICU teams. It will help other families if used correctly.”
4. Discussion
The purpose of this paper is to provide a detailed description of the methods and the sample of this randomized trial of prospective palliative care consultation with families in the pediatric ICU setting. From this report, there are several feasibility and research design issues to highlight. First, these data demonstrate that recruitment and retention of families is feasible in the high stress environment of the PICU. The recruitment rate of 50% provides important information for other investigators planning supportive intervention trials with family members in the PICU. The recruitment rate is in between previous studies that have reported recruitment rates ranging from 42–90% depending on the nature of the study and its relevance to family members [36–40]. However, the retention of over 90% of the families far exceeded our expectations and what has been reported in this previous research. We attribute these recruitment and retention rates to several factors. First, we were careful not to approach families on days when their child was scheduled for surgery or when there was a serious decision that needed to be made. We also allowed families several days to decide about study participation. These practices align with previous research articulating how best to approach families [41]. In addition, as noted in the discussion of the benefits of participation, families appreciated the opportunity to reflect on their ICU experience. Their comments about wanting to contribute to research and improve the experience of future families also explains the high retention rates. The provision of gift cards also may have positively influenced retention rates.
We were concerned that the study questions might add to the stressful environment, however, only 1 family declined participation based on being “too distressed”. Among those who agreed to participate, the low burden scores and comments suggest the opposite: that asking family members to reflect on their experience was helpful and gave them perspective on how they were coping, at least among participating family members. This finding supports other recent research demonstrating that families of critically ill children value research participation despite concerns from funders and institutional review boards that postulate potential harms from the burden of answering sensitive questions [40]. This positive experience was also reflected in a very high retention rate: 92% of all respondents completed questionnaires at all 3 time points. The participants’ comments regarding the focus on them as the point of intervention reflects the value of conducting research with family members of seriously ill children during ICU stays.
In summary, we found that a randomized trial of a routine palliative care intervention was feasible in the pediatric ICU setting with half of eligible families participating and excellent retention of family members in the study. We also found that participating family members reported very low burden of participation. We are currently evaluating the efficacy of the intervention for our proposed outcomes and will describe these results in future reports.
Acknowledgments
This project was supported by the National Institutes of Health (NIH) under award numbers R01NR011179, K24NR015340, and K24HL068593. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial Registration: NCT02144779
References
- 1.Studdert DM, Burns JP, Mello MM, Puopolo AL, Truog RD, Brennan TA. Nature of conflict in the care of pediatric intensive care patients with prolonged stay. Pediatrics. 2003;112:553–558. doi: 10.1542/peds.112.3.553. [DOI] [PubMed] [Google Scholar]
- 2.Balluffi A, Kassam-Adams N, Kazak A, Tucker M, Dominguez T, Helfaer M. Traumatic stress in parents of children admitted to the pediatric intensive care unit. Pediatr. Crit. Care Med. 2004;5:547–553. doi: 10.1097/01.PCC.0000137354.19807.44. [DOI] [PubMed] [Google Scholar]
- 3.Marsac ML, Hildenbrand AK, Kohser KL, Winston FK, Li Y, Kassam-Adams N. Preventing posttraumatic stress following pediatric injury: a randomized controlled trial of a web-based psycho-educational intervention for parents. J. Pediatr. Psychol. 2013;38:1101–1111. doi: 10.1093/jpepsy/jst053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meert KL, Thurston CS, Thomas R. Parental coping and bereavement outcome after the death of a child in the pediatric intensive care unit. Pediatr. Crit. Care Med. 2001;2:324–328. doi: 10.1097/00130478-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Crit. Care Med. 2012;40:618–624. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 6.Bronner MB, Peek N, Knoester H, Bos AP, Last BF, Grootenhuis MA. Course and predictors of posttraumatic stress disorder in parents after pediatric intensive care treatment of their child. J. Pediatr. Psychol. 2010;35:966–974. doi: 10.1093/jpepsy/jsq004. [DOI] [PubMed] [Google Scholar]
- 7.Nelson LP, Gold JI. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: a review. Pediatr. Crit. Care Med. 2012;13:338–347. doi: 10.1097/PCC.0b013e3182196a8f. [DOI] [PubMed] [Google Scholar]
- 8.Colville G, Pierce C. Patterns of post-traumatic stress symptoms in families after paediatric intensive care. Intensive Care Med. 2012;38:1523–1531. doi: 10.1007/s00134-012-2612-2. [DOI] [PubMed] [Google Scholar]
- 9.Hinds PS, Schum L, Baker JN, Wolfe J. Key factors affecting dying children and their families. J. Palliat. Med. 2005;8(Suppl 1):S70–S78. doi: 10.1089/jpm.2005.8.s-70. [DOI] [PubMed] [Google Scholar]
- 10.Contro N, Larson J, Scofield S, Sourkes B, Cohen H. Family perspectives on the quality of pediatric palliative care. Arch. Pediatr. Adolesc. Med. 2002;156:14–19. doi: 10.1001/archpedi.156.1.14. [DOI] [PubMed] [Google Scholar]
- 11.Azoulay E, Pochard F, Chevret S, Lemaire F, Mokhtari M, Le Gall JR, et al. Meeting the needs of intensive care unit patient families: a multicenter study. Am. J. Respir. Crit. Care Med. 2001;163:135–139. doi: 10.1164/ajrccm.163.1.2005117. [DOI] [PubMed] [Google Scholar]
- 12.Meyer EC, Ritholz MD, Burns JP, Truog RD. Improving the quality of end-of-life care in the pediatric intensive care unit: parents’ priorities and recommendations. Pediatrics. 2006;117:649–657. doi: 10.1542/peds.2005-0144. [DOI] [PubMed] [Google Scholar]
- 13.Graham RJ, Pemstein DM, Curley MAQ. Experiencing the pediatric intensive care unit: perspective from parents of children with severe antecedent disabilities. Crit. Care Med. 2009;37:2064–2070. doi: 10.1097/CCM.0b013e3181a00578. [DOI] [PubMed] [Google Scholar]
- 14.Latour JM, van Goudoever JB, Duivenvoorden HJ, van Dam NAM, Dullaart E, Albers MJIJ, et al. Perceptions of parents on satisfaction with care in the pediatric intensive care unit: the EMPATHIC study. Intensive Care Med. 2009;35:1082–1089. doi: 10.1007/s00134-009-1491-7. [DOI] [PubMed] [Google Scholar]
- 15.DeLemos D, Chen M, Romer A, Brydon K, Kastner K, Anthony B, et al. Building trust through communication in the intensive care unit: HICCC. Pediatr. Crit. Care Med. 2010;11:378–384. doi: 10.1097/PCC.0b013e3181b8088b. [DOI] [PubMed] [Google Scholar]
- 16.Doorenbos AZ, Starks H, Bourget E, McMullan DM, Lewis-Newby M, Rue TC, et al. Examining palliative care team involvement in automatic consultations for children on extracorporeal life support in the pediatric intensive care unit. J. Palliat. Med. 2013;16:492–495. doi: 10.1089/jpm.2012.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs. Res. 2001;50:105–115. doi: 10.1097/00006199-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Patterson JM. Understanding family resilience. J. Clin. Psychol. 2002;58:233–246. doi: 10.1002/jclp.10019. [DOI] [PubMed] [Google Scholar]
- 19.Shudy M, de Almeida ML, Ly S, Landon C, Groft S, Jenkins TL, et al. Impact of pediatric critical illness and injury on families: a systematic literature review. Pediatrics. 2006;118(Suppl):S203–S218. doi: 10.1542/peds.2006-0951B. [DOI] [PubMed] [Google Scholar]
- 20.Melnyk BM, Alpert-Gillis L, Feinstein NF, Crean HF, Johnson J, Fairbanks E, et al. Creating opportunities for parent empowerment: program effects on the mental health/coping outcomes of critically ill young children and their mothers. Pediatrics. 2004;113:e597–e607. doi: 10.1542/peds.113.6.e597. [DOI] [PubMed] [Google Scholar]
- 21.Jonsen A, Siegler M, Winslade W. Clinical Ethics: A Practical Approach to Ethical Decisions in Clinical Medicine. 7th. McGraw-Hill; 2010. [Google Scholar]
- 22.Hays RM, Valentine J, Haynes G, Geyer JR, Villareale N, McKinstry B, et al. The Seattle Pediatric Palliative Care Project: effects on family satisfaction and health-related quality of life. J. Palliat. Med. 2006;9:716–728. doi: 10.1089/jpm.2006.9.716. [DOI] [PubMed] [Google Scholar]
- 23.Hoge RD, Andrews DA, Faulkner P, Robinson D. The Family Relationship Index: validity data. J. Clin. Psychol. 1989;45:897–903. doi: 10.1002/1097-4679(198911)45:6<897::aid-jclp2270450611>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 24.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 25.Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: a confirmation study. J. Clin. Psychol. 1991;47:756–761. doi: 10.1002/1097-4679(199111)47:6<756::aid-jclp2270470605>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 26.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv. Res. 2002;37:1419–1439. doi: 10.1111/1475-6773.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 28.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J. Gen. Intern. Med. 2006;21:547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 30.Bryant RA, Moulds ML, Guthrie RM. Acute Stress Disorder Scale: a self-report measure of acute stress disorder. Psychol. Assess. 2000;12:61–68. [PubMed] [Google Scholar]
- 31.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav. Res. Ther. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 32.Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit. Care Med. 2006;34:1679–1685. doi: 10.1097/01.CCM.0000218409.58256.AA. [DOI] [PubMed] [Google Scholar]
- 33.Averill RF, Goldfield N, Hughes JS, Bonazelli J, McCullough EC, Mullin R, et al. 3M APR DRG Classification System Version 26.1 Methodology Overview. 2008 [Google Scholar]
- 34.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 35.Attride-Stirling J. Thematic networks: an analytic tool for qualitative research. Qual. Res. 2001;1:385–405. [Google Scholar]
- 36.Menon K, Ward RE, Gaboury I, Thomas M, Joffe A, Burns K, et al. Factors affecting consent in pediatric critical care research. Intensive Care Med. 2012;38:153–159. doi: 10.1007/s00134-011-2412-0. [DOI] [PubMed] [Google Scholar]
- 37.Menon K, Ward R. A study of consent for participation in a non-therapeutic study in the pediatric intensive care population. J. Med. Ethics. 2014;40:123–126. doi: 10.1136/medethics-2012-101075. [DOI] [PubMed] [Google Scholar]
- 38.Rosenberg AR, Bona K, Wharton CM, Bradford M, Shaffer ML, Wolfe J, et al. Adolescent and Young Adult Patient Engagement and Participation in Survey-Based Research: A Report From the “Resilience in Adolescents and Young Adults With Cancer” Study. Pediatr. Blood Cancer. 2016;63:734–736. doi: 10.1002/pbc.25843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Denhoff ER, Milliren CE, de Ferranti SD, Steltz SK, Osganian SK. Factors Associated with Clinical Research Recruitment in a Pediatric Academic Medical Center--A Web-Based Survey. PLoS One. 2015;10:e0140768. doi: 10.1371/journal.pone.0140768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steele R, Cadell S, Siden H, Andrews G, Smit Quosai T, Feichtinger L. Impact of research participation on parents of seriously ill children. J. Palliat. Med. 2014;17:788–796. doi: 10.1089/jpm.2013.0529. [DOI] [PubMed] [Google Scholar]
- 41.Thomas M, Menon K. Consenting to pediatric critical care research: understanding the perspective of parents. Dynamics. 2013;24:18–24. [PubMed] [Google Scholar]