Abstract
This paper examined how many older adults (65+ yrs) are meeting physical activity (PA) Guidelines (PAG; 150 min/wk of moderate-to-vigorous PA) using data from three leading national surveys (NHANES, BRFSS and NHIS). The proportion of individuals meeting aerobic PAG was determined for the most recent cycle available for each survey (NHANES 2011–12, NHIS and BRFSS 2013). We also assessed whether PAG adherence has changed over time. Predicted margins from multinomial logistic regression were computed after adjusting for age, race/ethnicity and gender and sample weights. The proportion of older adults meeting PAG was 27.3% for NHANES, 35.8% for NHIS and 44.3% for BRFSS. Across all surveys, men reported higher levels of activity than women, Non-Hispanic Whites reported higher levels than Non-Hispanic Blacks and Hispanics, activity declined with age and was lower in those with functional limitations, all P<0.05. The proportion of older adults meeting PAG in the NHIS survey, the only survey where PA questions remained the same over time, increased from 25.7% in 1998 to 35.8% in 2013 (P<0.01). Point-estimates for activity levels are different between surveys but they consistently identify sub-groups who are less active. Although older adults are reporting more activity over time, adherence to aerobic and strength training PAG remains low in this population and there is a need for effective interventions are needed to prevent age-related declines in PA and address health disparities among older adults.
Introduction
The population of older adults (≥65 yrs) in the United States is estimated to double over the next 25 years.(Vincent and Velkoff, 2010) As longevity increases, maintaining physical function, independence and quality of life among older adults are both public health and economic imperatives.(Parekh and Meyers, 2014) Older adults with multiple chronic conditions (e.g., cancer, hypertension, diabetes) account for 66% of the health care budget in the US.(Vincent and Velkoff, 2010) For many of these chronic conditions, there is strong evidence that physical activity (PA) is important for primary prevention, disease management and preventing mobility decline.(Pahor et al., 2014; Physical, 2008) Increasing PA, therefore, could have a profound effect on the health and quality of life of older adults, and provide major economic benefits to the US.(Carlson et al., 2015)
Physical activity is a leading health indicator for the Healthy People 2020 objectives, which are 10-year benchmarks for improving the health of Americans.(Services.) Currently, PA is monitored through national surveillance systems and these data are used to inform disease burden estimates, assess progress from programs designed to increase PA, and inform policy decisions related to PA and older adults.(Centers for Disease Control and Prevention; Prevention.; Statistics). In a previous paper, Carlson et al. [10] identified substantial differences in activity when comparing the three leading surveillance systems in the US (i.e., National Health and Nutrition Examination Survey [NHANES], Behavioral Risk Factor Surveillance System [BRFSS] and National Health Interview Survey [NHIS]). However, their analysis preceded changes to NHANES and BRFSS questionnaires and the 2008 PA Guidelines for Americans (referred to hereafter as the Guidelines). The Guidelines recommend 150 min/week moderate (3 – 5.99 Metabolic equivalents [METs]) and/or 75 min/week vigorous (≥ 6 METs) intensity activity or an equivalent combination and 2 days per week of strength training activities.(Committee, 2008; Services.) Additionally, previous analyses did not focus on older adults. Quantifying whether adherence to Guidelines among older adults differs across- and within-surveys over time is necessary to avoid conflating behavioral change with artifact due to survey questions or characteristics.
To our knowledge, data from updated surveys and adherence to current Guidelines have not been systematically compared for older adults. This paper examined adherence to Healthy People 2020 goals among older adults across three leading national surveys: PA-1 Reduce the proportion of adults who engage in no leisure-time PA [LTPA]; and PA-2 Increase the proportion of adults who meet 2008 Guidelines for aerobic and muscle-strengthening activity. We also examined adherence to the Guidelines by gender, race/ethnicity, age, and among those with functional limitations and trends over time. In addition to aerobic and muscle-strengthening activity, the National Institute on Aging’s “Go4Life® initiative recommends balance and flexibility activities for older adults and we documented whether these are assessed in existing surveillance systems.(National Insitute on Aging)
Methods
Table 1 provides an overview of each of the three surveys and the characteristics of the older adult population with available PA data. Briefly, NHANES uses a four-stage stratified cluster probability sample design to sample the non-institutionalized, civilian US population to obtain results that are nationally representative of the US population.(Prevention et al., 2013) For persons >16 yrs, the self-reported PA data is obtained during the interview portion. For this analysis we included data collected from 1999–2012, which encompasses seven, 2-year data cycles. Response rates ranged from 73% (2011–12) to 84% (2001–02) and sample sizes for older adults ranged from 1189 (2005–06) to 2556 (2007–08). (Centers for Disease Control and Prevention) In 2011–2012, PA data were available for 1,166 adults (Table 1), who were similar to the 1,250 older adults that completed the survey (Table A.1).
Table 1.
Survey and older adult population characteristics for three leading surveillance systems in the United States
| NHANES | NHIS | BRFSS | |
|---|---|---|---|
| Year | 2011–2012 | 2013 | 2013 |
| Total (N) | 1166 | 7590 | 139,724 |
| Response rate | 72.6% | 75.7% | 37.8–49.4%* |
| Contact method | In-person interview | In-person interview | Telephone |
|
| |||
| Stratified groups | N (weighted %) | ||
|
| |||
| Age | |||
| 65–74 years | 637 (57.4) | 4274 (57.6) | 79,282 (57.3) |
| 75–84 years | 529 (42.6) | 2317 (30.4) | 60,442 (42.7) |
| 85+ years | NA (NA) | 999 (12.0) | NA (NA) |
| Gender | |||
| Male | 581 (44.1) | 3053 (44.1) | 51,560 (43.5) |
| Female | 585 (55.9) | 4537 (55.9) | 88,164 (56.5) |
| Race/Ethnicity | |||
| Non-Hispanic White | 565 (77.9) | 5368 (78.8) | 118,000 (77.4) |
| Non-Hispanic Black | 284 (8.5) | 1001 (8.4) | 8527 (8.6) |
| Hispanic or Latino | 178 (7.1) | 752 (7.6) | 5588 (7.6) |
| Other | 139 (6.5) | 469 (5.2) | 7609 (6.3) |
| Functional Limitations | |||
| Yes | 560 (42.8) | 4880 (63.3) | 43,313 (29.6) |
| No | 606 (57.2) | 2710 (36.7) | 95,451 (69.5) |
Note: N’s are for those with available physical activity data
response rates were 37.8% for cell-phone and 49.4% for landline.
NA’s for age group 85+ yrs are due to top-coding of variables at age 80yrs.
Sub-categories may not equal 100 due to missing values or rounding. For race/ethnicity, there was an “other” category that was included in models as a covariate, but no estimated separately due to small samples and unreliable estimates. Categories not equal to 100 are due to missing values or rounding.
NHIS is a face-to-face household interview annual survey of the non-institutionalized US population. (Centers for Disease Control and Prevention) The survey uses a four-stage stratified cluster probability sample design. Participants were queried about PA and other health behaviors within the adult core sample. For this analysis we included data from 1998–2013. Response rates ranged from 67.8% (2007) to 74.3% (2002) and older adult sample sizes ranged from 4,444 in 2008 to 7,732 in 2013. (Centers for Disease Control and Prevention) The 7,732 participants who completed in the survey in 2013 (Table A.1) were similar to the 7,590 with available PA data (Table 1).
BRFSS is a state-based random digit-dialed telephone survey of the civilian, non-institutionalized US adult population ≥ 18 years of age.(Prevention.) Until 2011, all interviews were conducted via landlines and since then a combination of cell phone and landline interviews have been conducted. The data can be used to provide estimates at a national, state and some regional/city levels. This analysis included PA data that were collected biennially on even-years from 1994–2000 and on odd-years from 2001–2013. Response rates, a weighted average of the state-specific response rates, ranged from 46.4% in 2013 to 70.0% in 1994 and sample sizes for older adults ranged from 21,330 in 1994 to 160,882 in 2013. The 160,882 participants who completed in the survey in 2013 (Table A.1) were similar to the 139,724 with available PA data (Table 1).
Aerobic Physical Activity Assessment (See Appendix 1 for detailed descriptions)
To be included, an activity had to be: 1) aerobic – involving aerobic energy pathways (e.g., no weight-lifting); 2) reported for at least 10 minutes in duration and 3) of sufficient intensity (≥ 3 METs). The response time frames varied across surveys (i.e., past month, past two weeks, past week); therefore, all values were converted to minutes per week for consistency. To estimate the moderate intensity equivalent of total minutes per week, minutes of vigorous activity were multiplied by two and added to minutes of moderate activity. Although the Guidelines recommend all domains of aerobic activity (i.e., transportation, occupation and household activity), (Pettee Gabriel et al., 2012; Physical, 2008) for the present analysis we assessed only leisure-time since that is all that is available in NHIS and BRFSS.
Individuals were categorized as:
no-LTPA: reporting no qualifying PA
Insufficiently active: between 0 min and 149 min/week moderate intensity activity
Meets Guidelines: at least 150 min/week of moderate and/or 75 min/week vigorous-intensity activity
NHANES
1999–2006 (4 cycles)
Participants recalled specific vigorous and moderate intensity activities they engaged in the past 30 days along with the frequency and duration.(Statistics) Each activity was assigned a MET value based on the Compendium of Physical Activities.(Ainsworth et al., 2011) Participants reported frequency and duration of transportation activity and household activity.
2007–12 (3 cycles)
The Global PA Questionnaire was used to assess the frequency and duration of PA at work (vigorous and moderate), for transportation (bicycling and walking) and general leisure-time (vigorous and moderate) and the World Health Organization scoring protocol was followed.(Surveillance and Population-Based Prevention)
NHIS
1998–2013
Participants were asked how often they did vigorous or light/moderate intensity activity per week and then the average duration in each intensity. (Division of Health Interview Statistics, 2015)
BRFSS
No-LTPA
For all years, participants answered a yes/no question asking whether they did any physical activities or exercises. A “no” response determined the proportion reporting no-LTPA. For some years this variable was not structured as a skip pattern, which impacted the proportion of people categorized as inactive (See Table A.2. and Figure A.1.). The specific questions about PA are found below:
1994–2000; 2011–2013
Participants reported the two physical activities they spent the most time doing in the previous month, frequency and duration of activity in the past month. We applied the MET values from the 2013 analytic guidelines to these data.(The Physical Activity and Health Branch, 2011)
2001–2009
Participants reported the number of days per week and time per day they engaged in moderate and vigorous PA for at least 10-minutes at a time.
Strength training
The Guidelines recommend muscle strengthening activity 2 or more times per week.(Physical, 2008) NHANES only assessed muscle strengthening behaviors in 1999–2006, thus we did not report on these values due to the lack of recent data points. NHIS questionnaires included strength training from 1998–2013, BRFSS assessed strength training in 2011 and 2013.
Go4Life® Components
In addition to aerobic activity and strength training, Go4Life® promotes balance and flexibility activities for falls prevention. For each survey, we examined all primary and supplemental modules to determine which domains of aerobic activity and components of Go4Life® were assessed.
Statistical analyses
To assess the current level of PA among older adults, we restricted analysis to the most recent publically available data (i.e., NHANES 2011–12, NHIS and BRFSS 2013). For LTPA, we used multinomial logistic regression to identify the proportion of older individuals categorized as no-LTPA, insufficiently active and meeting Guidelines after adjusting for age (yrs), racial/ethnic categories (Non-Hispanic white, Non-Hispanic black, Hispanic, other and missing), and gender (male or female). For simplicity, we present only no-LTPA and meeting Guidelines in the main text, with insufficiently active estimates available in Table A.3. Strength training was categorized as sufficient (≥ 2 times/wk) or insufficient (<2 times/wk). Estimates were also compared by strata of relevant population sub-groups including age groups, gender, and race/ethnicity. The “other” race sample was insufficient to provide reliable estimates. The age, gender and race/ethnicity strata were mutually adjusted (i.e., age category adjusted for race/ethnicity and gender). Functional limitation category was adjusted for age (continuous), race/ethnicity and gender.
Using multinomial logistic regression analyses we tested whether the proportion of older adults who reported meeting aerobic or strength Guidelines changed over time by entering survey year as a continuous independent variable along with age, race/ethnicity and gender as covariates. (Graubard and Korn, 1999; Korn and B.I., 1999; Prevention.) In separate models with survey year as a categorical variable, predicted margins were used to compute proportions from the regression models adjusting for age, race and gender. (Graubard and Korn, 1999; Korn and B.I., 1999) CDC-recommended sample weights were included in the analyses to address differential sample selection, sample nonresponse and post-stratification adjustments. For time-trends, NHIS data from 1998–2013 were pooled and sample weights were adjusted accordingly.(Botman SL, 2000; Prevention et al., 2013) NHANES data within the two time-periods (1999–2006 and 2007–2008) were pooled but the trends were analyzed separately.(Prevention et al., 2013) BRFSS data were pooled within the three time periods (1994–2000–2001–2009 and 2001–2013).
All analyses were performed using SAS (version 9.3) (Cary, NC, USA) and the SAS-callable SUDAAN software (proc multilog and proc rlogistic) for analysis of multistage-stratified complex survey data. Two-sided P-values of <0.05 were used to indicate statistically significant associations.
Results
Guideline adherence among Older Adults
In the recent surveys, the proportion of older adults who met Guidelines was 27.3% for NHANES, 35.8% for NHIS and 44.3% for BRFSS; the estimates and 95% confidence intervals are shown in Table 2. The proportion of older adults who reported no-LTPA was 60.9% for NHANES, 42.6% for NHIS and 36.1% for BRFSS. In NHIS, 16.7% of older adults met strength training recommendations compared to 21.6% in BRFSS (Table 3).
Table 2.
Physical activity prevalence among older adults in the United States overall and stratified by sub-group
| No Leisure-time PA | Meeting PA Guidelines | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| NHANES 2011–2012 |
NHIS 2013 |
BRFSS 2013 |
NHANES 2011–2012 |
NHIS 2013 |
BRFSS 2013 |
|
| Overall | 60.9 (56.0, 65.6) | 42.6 (41.0, 44.2) | 36.1 (35.6, 36.7) | 27.3 (23.6, 31.2) | 35.8 (34.2, 37.4) | 44.3 (43.7, 44.8) |
|
| ||||||
| Age | ||||||
| 65–74 years | 55.4 (49.3, 61.3) | 35.6 (33.8, 37.5) | 32.2 (31.6, 32.9) | 30.7 (26.5, 35.2) | 41.7 (39.6, 43.8) | 47.8 (47.1, 48.5) |
| 75–84 years | 68.5 (61.9, 74.4) | 47.2 (44.4, 50.0) | 41.4 (40.5, 42.2) | 22.6 (16.7, 29.9) | 31.3 (28.5, 34.3) | 39.5 (38.7, 40.4) |
| 85 years and over | NA | 64.2 (60.2, 68.0) | NA | NA | 18.4 (15.3, 22.0) | NA |
|
| ||||||
| Gender | ||||||
| Male | 55.1 (49.8, 60.2) | 39.3 (37.0, 41.6) | 33.1 (32.2, 33.9) | 33.9 (29.7, 38.4) | 40.5 (38.2, 42.9) | 48.2 (47.3, 49.0) |
| Female | 65.6 (59.1, 71.6) | 45.2 (43.3, 47.1) | 38.5 (37.8, 39.2) | 21.9 (16.5, 28.4) | 31.9 (30.1, 33.8) | 41.2 (40.5, 41.9) |
|
| ||||||
| Race/Ethnicity | ||||||
| N-H White | 58.9 (53.3, 64.4) | 40.3 (38.4, 42.1) | 34.3 (33.8, 34.8) | 30.1 (26.0, 34.6) | 37.2 (35.3, 39.1) | 46.4 (45.9, 47.0) |
| N-H Black | 69.6 (63.3, 75.2) | 53.8 (50.2, 57.4) | 43.2 (40.8, 45.7) | 16.3 (12.2, 21.5) | 27.5 (24.0, 31.4) | 33.5 (31.3, 35.7) |
| Hispanic or Latino | 74.2 (65.5, 81.3) | 53.0 (48.7, 57.3) | 46.8 (43.9, 49.7) | 14.6 (9.8, 21.1) | 29.6 (25.7, 33.7) | 33.5 (30.9, 36.2) |
|
| ||||||
| Functional Limitations | ||||||
| Yes | 71.2 (65.0, 76.7) | 48.6 (46.7, 50.4) | 50.5 (49.5, 51.5) | 19.3 (14.4, 25.5) | 27.4 (25.7, 29.1) | 31.8 (30.9, 32.7) |
| No | 53.6 (47.7, 59.5) | 32.1 (29.6, 34.8) | 30.0 (29.4, 30.6) | 32.8 (27.8, 38.1) | 49.7 (47.0, 52.5) | 49.7 (49.0, 50.3) |
Note: Overall values are adjusted for age (yrs), gender (male or female), and race/ethnicity (Non-Hispanic white, Non-Hispanic Black, Hispanic or Latino and other). Gender and race are adjusted for age (yrs) and mutually adjusted. Age categories are adjusted for gender and race/ethnicity.
data on ages above 80 are not publically available for NHANES of BRFSS, for those surveys this category represented 75+yrs.
Table 3.
Proportion (95% Confidence interval) of older adults in the United States meeting strength training (2+ times/wk) recommendations
| NHIS | BRFSS | |
|---|---|---|
| Year | 2013 | 2013 |
|
| ||
| Overall | 16.7 (15.5, 18.0) | 21.6 (21.1, 22.0) |
|
| ||
| Age | ||
| 65–74 years | 19.2 (17.6, 21.0) | 22.8 (22.2, 23.4) |
| 75–84 years# | 15.0 (13.1, 17.2) | 19.9 (19.3, 20.6) |
| 85 years and over | 9.0 (7.0, 11.4) | NA |
|
| ||
| Gender | ||
| Male | 17.4 (15.7, 19.3) | 24.7 (24.0, 25.5) |
| Female | 16.2 (14.7, 17.7) | 19.1 (18.6, 19.6) |
|
| ||
| Race/Ethnicity | ||
| Non-Hispanic White | 17.7 (16.2, 19.3) | 22.4 (22.0, 22.8) |
| Non-Hispanic Black | 11.8 (9.6, 14.4) | 20.1 (18.4, 22.0) |
| Hispanic or Latino | 13.7 (10.8, 17.1) | 14.0 (12.2, 15.9) |
|
| ||
| Functional Limitations | ||
| Yes | 13.7 (12.5, 15.0) | 19.3 (18.6, 20.1) |
| No | 21.6 (19.5, 23.8) | 22.5 (22.0, 23.0) |
Note: Overall values are adjusted for age (yrs), gender (male or female), and race/ethnicity (Non-Hispanic white, Non-Hispanic Black, Hispanic or Latino and other). Gender and race are adjusted for age (yrs) and mutually adjusted. Age categories are adjusted for gender and race/ethnicity.
data on ages above 80 are not publically available for BRFSS, this category represented 75+yrs.
Stratified analyses
More men were meeting aerobic Guidelines than women with differences of 12 percentage points in NHANES, 9 percentage points in NHIS and 7.5 percentage points in BRFSS, all P<0.05. There was a clear age-related decline; for NHIS, the proportion meeting Guidelines decreased from 41.7% for 65–74 y, 31.3% for 75–84y and 18.4% for those aged 85 yrs or above (P<0.05). For NHANES and BRFSS, the younger category (65–74 y) was significantly more active than the 75+yr category (P<0.05), more granular age comparisons were not possible because age was top-coded at 80y. Non-Hispanic whites reported more LTPA than Hispanic or non-Hispanic Black individuals in all surveys (all P<0.05) (Table 2).
There were differences in the proportion of people who were classified as functionally limited across surveys. For NHANES, 42.8% were considered limited, 63.3% in NHIS and 29.6% in BRFSS (Table 1). In all surveys, the proportion of people meeting Guidelines was significantly higher (P<0.05) for those who were not-limited compared to those who were functionally limited (i.e., NHANES 32.8% vs 19.3%, NHIS 49.7% vs 27.4%; BRFSS 49.7% vs 31.8%) (Table 2).
The proportion reporting strength training twice per week was not different for men (17.4%) vs women (16.2%) in NHIS (P>0.05), but in BRFSS was significantly higher in men (24.7%) than women (19.1%) (P<0.05) (Table 3). In NHIS, non-Hispanic Whites had significantly higher prevalence of meeting strength Guidelines (17.7%) compared to Hispanic individuals (13.7%) and non-Hispanic Blacks (11.8%) (P<0.05). Non-Hispanic Whites (22.4%) in BRFSS had higher rates than Hispanics (14.0%) but were not significantly different from non-Hispanic Blacks (20.1%) (Table 2). In NHIS, the proportion meeting strength training declined significantly with age (9.0% ≥ 85y vs 19.2% 65–74y) (P<0.05). In BRFSS, there were small but statistically significant differences in strength training between those 64–75y (22.8%) compared to those ≥ 75y (19.9%), P<0.05. Similarly, those considered limited reported lower levels of strength training compared to those without functional limitations (P<0.05) (Table 3).
Trends in Physical Activity
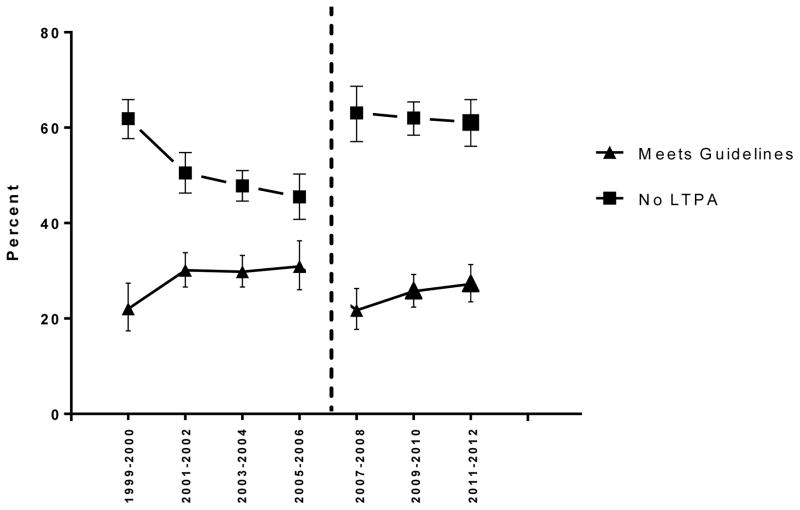
In NHANES, a new questionnaire was introduced in 2007–08, which precludes conclusions about activity trends over the entire study period (1909–2012). When the new questionnaire was introduced in 2007–08, the proportion reporting no-LTPA increased by approximately 20 percentage points compared to the previous cycle (Figure 1). Within the period with consistent questions, from 2007–08 to 2011–12, the proportion meeting Guidelines increased from 21.7% to 27.2% (P<0.05), while the proportion reporting no-LTPA remained stable (2007–08: 63.1%, 2011–12: 61.1%).
Figure 1. NHANES: Trends in leisure-time aerobic physical activity among older adults between 1999–2012.
Note: Dashed lines indicate where the physical activity questions within the survey were changed.
Values are adjusted means are predicted margins from multinomial regression models, adjusting for age (yrs), gender (male or female), and race/ethnicity (Non-Hispanic white, Non-Hispanic Black, Hispanic or other). Meeting Guidelines is reporting >150 min/wk of moderate activity and/or 75 min/week of vigorous intensity activity.
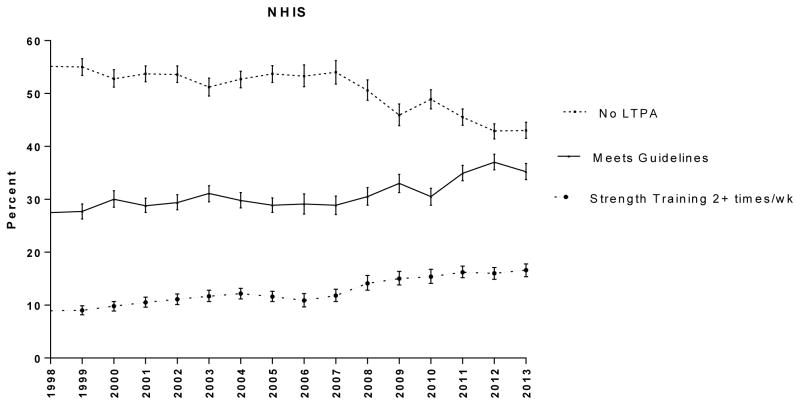
NHIS was the only survey where the questions remained the same over the entire time period. Based on this survey, the proportion meeting Guidelines increased from 25.7% in 1998 to 35.2% in 2013 and the proportion engaging in no LTPA decreased from 55.9% to 43.0% over the same time period (Figure 2), with both trends statistically significant (P<0.01).
Figure 2. NHIS: Trends in leisure-time aerobic physical activity and strength training among older adults between 1998–2013.
Note: Values are adjusted means are predicted margins from multinomial regression models, adjusting for age (yrs), gender (male or female), and race/ethnicity (Non-Hispanic white, Non-Hispanic Black, Hispanic or other). Meeting Guidelines is reporting >150 min/wk of moderate activity and/or 75 min/week of vigorous intensity activity.
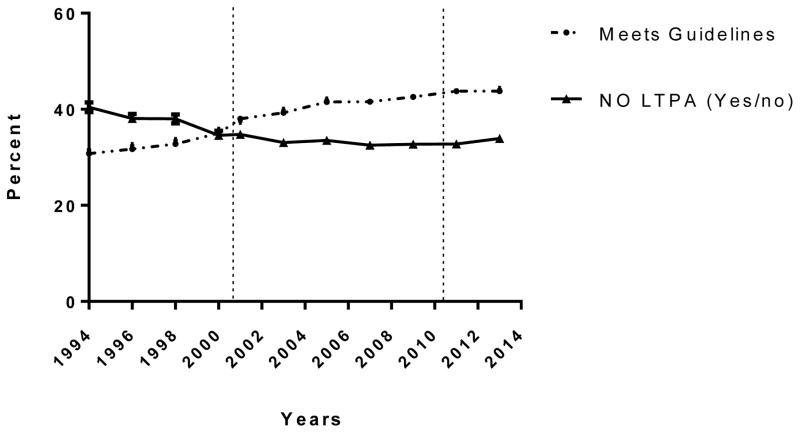
In BRFSS, the proportion of adults reporting no-LTPA decreased from 40.4% in 1994 to 33.9% in 2013 (Figure 3). Within both of the two time-periods that had consistent questions (i.e.,1994–2000 and 2001–09) the estimated proportion meeting Guidelines increased (P<0.05).
Figure 3. BRFSS: Trends in leisure-time aerobic physical activity among older adults between 1994–2013.
Note: Dashed lines indicate where physical activity questions within the survey were changed.
Values are adjusted means are predicted margins from multiple regression models, adjusting for age (yrs), gender (male or female), and race/ethnicity (Non-Hispanic white, Non-Hispanic Black, Hispanic or other). Meeting Guidelines is reporting >150 min/wk of moderate activity and/or 75 min/week of vigorous intensity activity. No LTPA is from yes/no question “During the past month, other than your regular job, did you participate in any physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise?”
Components of activity that are assessed in surveys
Table 4 shows the Go4Life® components that are currently assessed by each survey. All surveys measure some form of aerobic activity and NHIS and BRFSS assess strength training while NHANES does not. None of the surveys routinely assess balance or flexibility-though in BRFSS participants could report activities (e.g., tai chi) but they are not scored in the current protocol. (The Physical Activity and Health Branch, 2011)
Table 4.
Current components of PA assessed by each survey
| NHANES | NHIS | BRFSS | |
|---|---|---|---|
| Aerobic leisure time | Yes | Yes | Yes |
| Aerobic transportation | Yes | No | No |
| Aerobic occupational | Yes | No | No |
| Aerobic household | No* | No | No |
| Strength | No | Yes | Yes |
| Flexibility | No | No# | No** |
| Balance | No | No# | No** |
Notes:
Combined with occupational activity
was assessed in 2001 NHIS Sample Adult Core 2002; 2012 Complementary and Alternative Medicine Supplement and 2008 Adult Balance and Dizziness Supplement
Individual activities could be reported (yoga/tai chi/stretching) if one of top two-activities.
Discussion
This paper sought to determine the proportion of older adults who meet aerobic and strength training Guidelines. We found that the answer differed by survey, with estimates for aerobic activity ranging from 27.3% (NHANES 2011–12) to 44.3% (BRFSS 2013) (Table 2). The proportion currently meeting strength-training recommendations (2 sessions per week) also differed between NHIS (16.7%) and BRFSS (21.6%). Based on NHIS and BRFSS, which had consistent questions over time, it appeared that the proportion of older adults reporting no-LTPA was declining. Using three national surveillance systems, these data provide a comprehensive examination of current activity levels and temporal trends in activity among older adults that may inform policy decisions and progress of programs designed to promote PA among older adults.
Although the point-estimates differed, there were important differences in activity levels for population sub-groups that were consistent across surveys. First, there is a clear age-related decline in activity. For NHIS, adults 65–74 yrs old were twice as likely to meet Guidelines (41.7%) compared to those over 85 yrs (18.4%). Although specific age data are available via proposals in the National Center for Health Statistics Research Data Center, the publically available datasets for both NHANES and BRFSS have top-coded age at 80 yrs. Adults >85 yrs are the fastest growing segment of the population and increasing activity among this older group is beneficial.(Pahor et al., 2014) Therefore, public access to relevant data for those aged 80+ in more granular form may be important. Second, males were consistently more active than females, and third, non-Hispanic Whites were more active than Non-Hispanic Blacks and Hispanic/Latinos populations. These findings are consistent with Carlson et al. (Carlson et al., 2009) based on data through 2008 and demonstrate a continued need for targeted interventions to reduce health disparities among older adults.
The differences in Guidelines adherence across the three surveys could be related to the survey design (e.g., sampling strategies, response rates and in-person vs. telephone surveys) or the PA questions themselves (e.g., domain, time-scale). The factors related to the surveys are discussed in detail by others. (Carlson et al., 2009; Fahimi et al., 2008; Nelson et al., 2003) Briefly, NHIS and NHANES conduct in-person interviews while BRFSS is telephone-based, which results in lower response rates for BRFSS and could lead to selection bias, though this is considered in sample weighting.(Blumberg and Luke, 2009) Li et al. compared questions (i.e., smoking, BMI, prevalence of chronic diseases) that are similarly assessed between the surveillance systems and noted differences (0–3.9%) that were much smaller in magnitude than for physical activity (11–25%). (Li et al., 2012) Thus, rather than survey-specific factors, the observed PA differences are likely due to differences in the questions included in the surveys, which is supported by the large changes when the PA questions changed within a survey. There was no clear pattern for whether “global” or “specific” questions produced higher prevalence estimates. In NHANES, the proportion who reported meeting Guidelines went down when the global questions were instituted (Figure 1), while in BRFSS the proportion who reported meeting Guidelines went up when global questions were instituted (Figure 3). This may be due to the fact that NHANES allowed for an unlimited number of activities to be reported, while BRFSS participants reported just the top two most common activities.
Based on NHIS, the only survey with consistent questions over an extended time-period (1998–2013), across all age strata more older adults are meeting Guidelines (Figure A.2.). However, only about one-third of older adults are meeting aerobic Guidelines, and strength training rates have nearly doubled but remain low (16.7%). In BRFSS, the proportion of older adults reporting no-LTPA also declined, consistent with trends in NHIS. Our findings are similar to Carlson et al., (Carlson et al., 2010) who showed small but significant improvement in Guidelines adherence for all US adults between 1998 and 2008 using NHIS. While surveys will inevitably change due to advances in science and space/resource allocation, it seems imperative that some key questions or components remain stable to allow researchers and policy makers to adequately assess trends over time. Analysts should strongly consider the impact changes in questionnaires may have on observed results and resulting conclusions, as it was not possible to examine temporal trends in NHANES due to a substantial change in activity levels when the survey questions changed.(Bassett and Lee, 2015; Ladabaum et al., 2014)
A final goal of this paper was to identify whether existing surveillance systems currently assess the types of PA recommended for older adults and promoted by the Go4Life® initiative. Over the past 50 years, the focus of PA research has shifted from activity for improving fitness (i.e., exercise), to activity for health, which includes moderate-intensity activity in any domain (e.g., walking for transportation, household activities).(Physical, 2008) Existing surveillance programs focus primarily on LTPA (all) and only NHANES routinely assesses other aerobic domains (transportation and occupation). The definition and examples for leisure-time activity may have changed over time within surveys. Future research is needed to explore how aerobic activity domains are interpreted by older adults; for example, retired individuals may consider all time as “leisure-time” and the term “exercise” may discourage older adults (as well as others) from reporting a walk to the store. Unsurprisingly, in NHANES the proportion meeting Guidelines (46.4%) when all domains were included was higher than for leisure-time alone (27.3%). NHIS has included supplemental questions (Cancer supplement: 2000, 2005, 2010) that included transportation-related aerobic activity. Strength training is only assessed in NHIS and BRFSS. Balance and flexibility activities have been shown to prevent falls and have particular importance for older adults, but are not routinely assessed.(Province et al., 1995) In NHIS, these activities have been assessed in supplements (e.g., stretching, 2001; yoga and tai chi, 2012, Table 4) and perhaps could be evaluated in future supplements.(Division of Health Interview Statistics, 2015) Since NHANES combines the interview with medical examinations, there is an opportunity to objectively assess strength, balance and flexibility. From 1999–2004 balance was objectively assessed and lower extremity muscle strength was assessed from 1999–2002. Beginning in 2011–2012, handgrip strength was assessed but questions about frequency of strength training behaviors are no longer included in the survey for comparison.
Self-reported PA is subject to recall and desirability biases, which may lead to misclassification of activity status. Accelerometers provide an objective estimate of PA-related movement and were used in NHANES sample from 2003–2006 and 2011–2014 (data release pending). However, the Guidelines are based on self-reported data and there are currently no public health recommendations based on accelerometer data. (Troiano et al., 2014) Therefore, we restricted our analysis to self-reported data. While the point-estimates of Guidelines adherence are different between self-report and accelerometers (Troiano et al., 2008), we do see similar age-related declines and differences by sex. (Matthews et al., 2008; Matthews et al., 2012; Troiano et al., 2008) Prospective studies with accelerometer-assessed PA are needed to inform recommendations and surveillance efforts.
Although providing an accurate point-estimate of current activity levels among older adults is challenging, the data reported here provide insights on the current levels of activity and identify sub-groups who are less active. There is a need for greater attention of surveillance of PA in older adults given the aging population in the US and the particular benefits of PA for this population. More research is needed to broaden the focus from leisure-time aerobic activity to other forms of PA and to determine the types of questions in the existing surveys that are most appropriate for older adults. It appears that the proportion of older adults meeting aerobic and strength Guidelines is increasing and the proportion engaging in no LTPA is declining over the time period from 1998–2013, but there is still a great deal of room for improvement as less than half of adults met aerobic Guidelines in all surveys. Effective interventions are needed to encourage PA, prevent age-related declines in PA, and address health disparities among older adults.
Supplementary Material
Highlights.
This study examined Physical Activity Guideline (PAG) adherence in older adults
PAG adherence varied across the three leading surveillance systems
PAG adherence modestly improved over time but remains low
Interventions are needed to address health disparities among older adults
Acknowledgments
The authors would like to thank Lisa Kahle for her programming assistance. This work is funded in part by the Intramural Research Program at the National Cancer Institute.
Footnotes
The authors declare they have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, et al. 2011 Compendium of Physical Activities: A Second Update of Codes and MET Values. Medicine and science in sports and exercise. 2011;43:1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- Bassett DR, Lee IM. Trends in Physical Inactivity. Am J Med. 2015;128:E24–E24. doi: 10.1016/j.amjmed.2014.12.019. [DOI] [PubMed] [Google Scholar]
- Blumberg SJ, Luke JV. Reevaluating the Need for Concern Regarding Noncoverage Bias in Landline Surveys. American journal of public health. 2009;99:1806–10. doi: 10.2105/AJPH.2008.152835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botman SL, MT, Moriarity CL, Parsons VL. Design and Estimation for the National Health Interview Survey, 1995–2004. Vital Health Stat. 2000;2:200. [Google Scholar]
- Carlson SA, Densmore D, Fulton JE, Yore MM, Kohl HW., 3rd Differences in physical activity prevalence and trends from 3 U.S. surveillance systems: NHIS, NHANES, and BRFSS. J Phys Act Health. 2009;6(Suppl 1):S18–27. doi: 10.1123/jpah.6.s1.s18. [DOI] [PubMed] [Google Scholar]
- Carlson SA, Fulton JE, Pratt M, Yang Z, Adams EK. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis. 2015;57:315–23. doi: 10.1016/j.pcad.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson SA, Fulton JE, Schoenborn CA, Loustalot F. Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. American journal of preventive medicine. 2010;39:305–13. doi: 10.1016/j.amepre.2010.06.006. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, N.C.f.H.S. National Health and Nutrition Examination Survey Response Rates. p. http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm.
- Committee, P.A.G.A. Physical Activity Guidelines Advisory Committee Report. Department of Health and Human Services; Washington, DC: 2008. [Google Scholar]
- Division of Health Interview Statistics, N.C.f.H.S. Adult Physical Activity Questions on the National Health Interview Survey. 2015 p. http://www.cdc.gov/nchs/nhis/physical_activity/pa_questions.htm.
- Fahimi M, Link M, Mokdad A, Schwartz DA, Levy P. Tracking chronic disease and risk behavior prevalence as survey participation declines: statistics from the behavioral risk factor surveillance system and other national surveys. Prev Chronic Dis. 2008;5:A80. [PMC free article] [PubMed] [Google Scholar]
- Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55:652–9. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- Korn EL, BIG . Analysis of Health Surveys. John Wiley and Sons; Hoboken, NJ: 1999. [Google Scholar]
- Ladabaum U, Mannalithara A, Myer PA, Singh G. Obesity, abdominal obesity, physical activity, and caloric intake in US adults: 1988 to 2010. The American journal of medicine. 2014;127:717–27. e12. doi: 10.1016/j.amjmed.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev Med. 2012;54:381–7. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003–2004. American journal of epidemiology. 2008;167:875–81. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews CE, George SM, Moore SC, Bowles HR, Blair A, Park Y, Troiano RP, Hollenbeck A, Schatzkin A. The American journal of clinical nutrition. Vol. 95. National Insitute on Aging, N.I.o.H; 2012. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults; pp. 437–45. p. https://go4life.nia.nih.gov/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson DE, Powell-Griner E, Town M, Kovar MG. A comparison of national estimates from the National Health Interview Survey and the Behavioral Risk Factor Surveillance System. Am J Public Health. 2003;93:1335–41. doi: 10.2105/ajph.93.8.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, Espeland MA, Fielding RA, Gill TM, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014;311:2387–96. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parekh AK, Meyers DS. The Strategic Framework on Multiple Chronic Conditions. Medical care. 2014;52(Suppl 3):S1–2. doi: 10.1097/MLR.0000000000000094. [DOI] [PubMed] [Google Scholar]
- Pettee Gabriel KK, Morrow JR, Jr, Woolsey AL. Framework for physical activity as a complex and multidimensional behavior. J Phys Act Health. 2012;9(Suppl 1):S11–8. doi: 10.1123/jpah.9.s1.s11. [DOI] [PubMed] [Google Scholar]
- Physical, P.A.G.C.R. 2008 [Google Scholar]
- Prevention, C.f.D.C.a. National Health Interview Survey. p. http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm.
- Prevention, C.f.D.C.a., Statistics, N.C.f.H., Surveys, D.o.H.a.N.E. National Health and Nutrition Examination Survey: Analytic Guidelines, 2011–2012. 2013 p. http://www.cdc.gov/nchs/data/nhanes/analytic_guidelines_11_12.pdf.
- Prevention, S.a.P.-B; Department, P.o.N.D, editor. Global Physical Activity Questionnaire (GPAQ) Analysis Guide. World Health Organization; Geneva, Switzerland: p. http://www.who.int/chp/steps/GPAQ/en/ [Google Scholar]
- Prevention., C.f.D.C.a. Behavioral Risk Factor Surveillance System. p. http://www.cdc.gov/brfss.
- Province MA, Hadley EC, Hornbrook MC, Lipsitz LA, Miller JP, Mulrow CD, Ory MG, Sattin RW, Tinetti ME, et al. The effects of exercise on falls in elderly patients. A preplanned meta-analysis of the FICSIT Trials. Frailty and Injuries: Cooperative Studies of Intervention Techniques. JAMA : the journal of the American Medical Association. 1995;273:1341–7. [PubMed] [Google Scholar]
- Services., U.D.o.H.a.H. Healthy People 2020. US Government Printing Office; Washington, DC: p. http://www.healthypeople.gov/ [Google Scholar]
- Statistics, N.C.f.H. National Health and Nutrition Examination Survey. p. http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- The Physical Activity and Health Branch, D.o.N., Physical Activity, and Obesity, Centers for Disease Control and Prevention. A Data Users Guide to the BRFSS Physical Activity Questions How to Assess the 2008 Physical Activity Guidelines for Americans. 2011 p. http://www.cdc.gov/brfss/pdf/PA%20RotatingCore_BRFSSGuide_508Comp_07252013FINAL.pdf.
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. British journal of sports medicine. 2014;48:1019–23. doi: 10.1136/bjsports-2014-093546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent GK, Velkoff VA. US Department of Commerce, E.a.S.A., US Census Bureau, editor. The Next Four Decades The Older Population in the United States: 2010 to 2050. Washington, DC: 2010. p. 10. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.