Abstract
Background
Many of the health behaviors known to contribute to cardiometabolic risk and disease (CMRD), including physical activity, diet, sleep, and screen time, begin during childhood. Given the population-wide burden of CMRD, novel ways of assessing risk and providing feedback to support behavior change are needed.
Purpose
This paper describes the design and rationale for the Study for using Technology to Reach Individual Excellence (STRIVE), a randomized controlled trial testing the use of an integrated, closed-loop feedback system that incorporates longitudinal, patient-generated, mobile health technology (mHealth) data on health behaviors and provides clinical recommendations to help manage CMRD among at-risk families.
Methods
STRIVE is a 6-month trial among 68 children, ages 6-12 year olds with a body mass index ≥ 85th percentile from Massachusetts with at least one parent with CMRD. Data on several health behaviors will be collected daily over 6 months. Children and parents will each wear wristbands that collect objective physical activity, sleep, and screen time data via accelerometry, noise, and infrared detection. Sugar sweetened beverage consumption will be assessed by self-report via a smartphone application. Weight will be collected using a wireless scale. Intervention group parents receive feedback on their child's health behaviors and personalized CMRD counseling via mobile messaging. Control parents receive standard of care recommendations and weekly health behavior reports for self-guided care.
Conclusion
The STRIVE trial will test the use of mHealth and closed-loop feedback systems to improve health behaviors among families at-risk for or with established CMRD.
Keywords: mHealth, health behaviors, technology, obesity, childhood, cardiometabolic
Introduction and Background
Cardiometabolic disease, which includes obesity, type II diabetes, coronary artery disease, hypertension, dyslipidemia, and liver enzyme dysregulation, is a significant health problem among the US population.1 Obesity alone continues to be a serious problem in the United States with nearly one in three children and two in three adults currently overweight or obese.2 Many of the clinical manifestations of cardiometabolic disease, including obesity, type II diabetes, hyperlipidemia, elevated blood pressure, and liver enzyme abnormalities begin during childhood and track into adulthood.3, 4 Health habits are known to form during childhood and may be harder to change once established during adulthood.5 Therefore, the prevention of cardiometabolic risk and disease (CMRD) and its associated risk factors should start during childhood.6 Examining individual-level health behaviors known to be associated with cardiometabolic risk is an important first step to preventing disease. Primary care clinicians have historically assumed this task as part of an effort to prevent and treat disease. Although clinicians can play a valuable role in identifying risk and providing recommendations, multiple factors limit their effectiveness including infrequent and brief visits and dependence on subjective patient-reported information regarding health behaviors.7–9 Even if health behavior information is collected, clinicians may be uncertain on how to use this information or may lack systems for providing timely feedback to patients.10 Given the myriad health problems and costs associated with cardiometabolic disease and the obstacles clinicians currently face when counseling patients, novel and effective methods for collecting objective risk data and providing timely feedback could help mitigate the population-wide burden of CMRD.
Providing timely feedback on health behaviors has recently been shown to have benefits in other chronic lifestyle-mediated conditions, such as the management of tobacco use. In smoking cessation, as with CRMD, automated feedback and support can be linked with clinical recommendations with the goal of modifying health behaviors. Smoking cessation studies have demonstrated the feasibility and efficacy of this approach by employing several techniques which are transferable to CMRD, namely using mobile phone technology to deliver closed-loop feedback in the form of tailored evidence-based clinical messages.11, 12 Closed-loop feedback can be defined as any information transfer that is automated, recipient-directed, and activity-completing. For example, a movie-finding text message program that prompts the end-user to enter their favorite movie category and then automatically texts back all the movies in that category currently playing in cinemas would be an example of closed-loop feedback: the reply is computer generated (automated), provides information directly back to the end-user (recipient-directed), and fully completes the information transfer task that it initiated (activity-completing). Closed-loop feedback systems can be applied to managing CMRD health behaviors and have several related features that are particularly appealing, including the ability to tailor feedback, the ability to provide evidence-based feedback, and the capacity to markedly reduce the feedback cycle time compared to standard medical practice.
The primary aim of STRIVE is to test a Just-In-Time Adaptive Intervention (JITAI) for pediatric CMRD which delivers daily personalized mobile phone-based messages based on four tailoring variables: daily hours of moderate-to-vigorous physical activity, daily hours of sleep, daily consumption of Sugar Sweetened Beverages, and daily number of hours of screen time. This intervention shall be analyzed as a comparative effectiveness study to determine the feasibility and potential benefit of using a mHealth-based closed-loop feedback system that collects longitudinal patient-generated health behavior data and provides evidence-based clinical recommendations compared to a self-guided disease management approach among families with CMRD. We hypothesize that providing rapid, frequent, personalized clinical feedback on health behaviors will improve weight status among at-risk children. The primary outcome is change in child BMI, the most prevalent and earliest manifestation of CMRD in children. The secondary outcomes are change in parent BMI and change in child and parent CMRD-related health behaviors; physical activity, sleep, screen-time, and sugar-sweetened beverage consumption. In this paper, we report the design and rationale for STRIVE.
Methods
Theoretical Frameworks
STRIVE is informed by two theoretical frameworks that aim to understand and explain health behaviors and disease self-management: 1) the health belief model; and 2) self-determination theory. The Health Belief Model (HBM) was developed to identify, explain, and predict health behaviors. The model is founded on the basic tenet that patients will take healthful actions if they believe i) negative health consequences can be avoided, and ii) they are capable of taking healthful actions.13, 14 HBM is well-suited for studying cardiometabolic health behaviors and has been widely used to develop messages aimed at promoting healthy habits and decisions, including prior pediatric obesity studies aimed at promoting healthy behaviors.15 This study will incorporate and test the application multiple HBM concepts including perceived disease severity (define personalized risk based on objective health behavior quantification and feedback), perceived benefits of action (define goals, define health and non-health outcomes), perceived barriers to action (identify health behaviors that are not at goal, educate, motivate), cues to action (provide motivational messages), and self-efficacy (health behavior achievement feedback). Self-determination theory assumes that humans have an inclination towards activity but also a vulnerability to passivity,16 and has been applied in prior research testing obesity-related treatments using mobile technologies.17 Self-determination theory accounts for the personal motivational factors essential for successfully using patient-driven technology to promote patient engagement in lifestyle modifications.
Comparative Effectiveness Research Evidence Base
Along with having a strong theoretical grounding, STRIVE is also founded on existing comparative effectiveness evidence, and seeks to build new tools that will increase the uptake of proven effective interventions. Prior research among children ages 6-12 years that included computerized decision support has demonstrated that a family-based approach can be beneficial for treating cardiometoblic risk, and that family-based interventions for self-guided behavior change can improve childhood body mass index.18 We designed STRIVE to be a clinical comparative effectiveness study that draws on this evidence to test the benefit of using automated technology to improve the adoption of evidence-based cardiometabolic risk management strategies.
Patients and Recruitment
Patients ages 6-12 years with overweight or obesity (BMI≥85th percentile) followed for obesity care at Massachusetts General Hospital in Boston and who have an adult household family member with one or more elevated cardiometabolic risk (defined as established or elevated risk of overweight, obesity, hypertension, coronary artery disease, diabetes or glucose intolerance, dyslipidemia, non-alcoholic fatty liver disease, cerebrovascular disease) are eligible to participate in this study. Participating parents must also have Wi-Fi Internet at home (required for the bathroom scale), own an Android smartphone, and read English. This study is approved by the Partners HealthCare institutional review board and the protocol is registered on ClinicalTrials.gov (NCT 02659163). Written informed consent is obtained from parents and guardians along with child assent prior to study participation.
Study Design
STRIVE is a prospective randomized controlled trial that will test the feasibility of using mHealth to reduce cardiometabolic risk in children by collecting longitudinal patient-generated health behavior data and providing clinical recommendations in a closed-loop feedback system (Figure 1). Participants will be randomly assigned in a 1:1 ratio to an intervention or control group based on computer-generated randomization output. Study participants will be blinded to their study assignment, and study team members will be blinded to study group assignment during data analyses. Daily health behavior data will be collected over 6 months, and study outcomes will be measured as the change from baseline to study completion. Participating families will receive $100 ($50 for each child participant and $50 for participating parents as remuneration after study completion and return of all study equipment.
Figure 1.
Study design, randomization, and outcomes of the Study for using Technology to Reach Individual Excellence (STRIVE), a randomized controlled trial in greater metropolitan Boston, Massachusetts, 2016–2017.
Study Variables, Measures, and Data Collection
Several types of data sources will be collected from both the child and parent and will be used to compare change over time between the intervention and control groups in body mass index (BMI) and health behaviors. Participants will be informed of all the data sources collected, as well as all the devices and sensors used during the study. The primary outcome is change in BMI. The secondary outcome is change in health behaviors. For the purpose of designing our mHealth intervention, we considered BMI as our primary distal outcome. Individual health behaviors will be used both to determine proximal response as well as the distal outcomes. Proximal response is determined by change in daily health behavior. We defined distal outcomes as aggregated change in health behaviors over the six month study period.
Demographic data: All study families complete a questionnaire at enrollment with self-reported information on age, sex, race/ethnicity, highest level of education, home address, and the child's primary language.
Anthropometric data: Each family is provided with a wireless scale (Withings WS-30). Parent and child weight is measured at baseline and weekly thereafter using the wireless scale. Each family is provided with a paper growth chart. Height is measured at baseline for the parent and child, and then monthly thereafter for the child using the paper growth chart. Families record height by marking height on the growth chart and taking a picture of the measurement with their smartphone camera, and then sending the image via text message to the study team. Weight and height for each participant are used to calculate the body mass index.
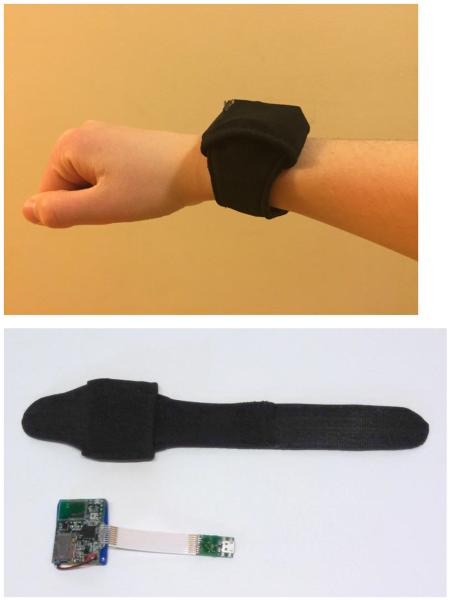
Health Behaviors Data (Tailoring Variables): Our primary tailoring variables are derived from wearable sensors in the form of a water-resistant wristband on the dominant hand containing a 3-axis accelerometer, as well as sensors for light spectrum, temperature, and skin conductance (Figure 2). (1) Physical activity is measured by accelerometry and reported as minutes of moderate-to-vigorous physical activity. (2) Sleep duration is measured using accelerometry along with skin conductance. (3) Screen time is measured by recording changes in color spectrum corresponding with periods of low-movement recorded by accelerometry. (4) Sugar sweetened beverage (SSB) consumption is determined using ecological momentary assessment (EMA); parents are sent a daily mobile message asking them to report on the number of SSB their child consumed on that day.
Figure 2.
Wristband for collecting objective health behavior data. Contains multiple sensors: accelerometry, light spectrum, temperature, and skin conductance. (top) Photo of patient-worn multi-sensor band device inside a wearable wristband sleeve; (bottom) Wearable wristband sleeve and mulit-sensor band device contained within.
Health behavior data is collected daily and uploaded to a central study server platform (openmrs.org) which containts custom software modules which process the data daily and calculate estimates for specific behaviors based on the raw sensor data. The algorithms for estimating the hours of sleep and physical activity were derived from custom machine learning algorithms, which is similar to other published studies; however, the estimation of screen time was developed using a completely new approach (publication on this technology is pending review). The server software also contains the decision rules and a bank of messages that are used to compose the motivational and feedback messages that are delivered to the intervention group in the study (these messages are not delivered to the control group).
Patient Feedback and Intervention
All study participants receive a print out with the standard of care recommendations for physical activity, sleep, screen time, and SSBs at study entry. A custom smart phone mobile application was created to download specific behavior data from the remote server and present information and messaging to the parent and child participants. At study entry, all participating parents download the STRIVE mobile application to their smartphone and are walked through/instructed on how to use the app by the study team. The STRIVE application is the primary means for participants in the intervention group to retrieve information on their health behaviors and behavior change progress (Figure 3), and by providing evidence-based recommendations on four health behaviors that have well-established associations with weight status, this mHealth serves as a tool that will help participants reduce their BMI over 6 months. To ensure proper blinding, eligible families will be informed at the time of enrollment that the STRIVE mobile application will be used to provide them with “regular weekly updates of your their child's health behaviors”. As such, control families will be aware that they will receive feedback via the app, but will not have knowledge of the full range of feedback offered to participants in the intervention group.
Figure 3.
STRIVE mobile application
In the intervention group, parents receive additional messages via the mobile app reporting on the child's health behaviors and providing constructive and motivational feedback. Each weekday, parents receive a mobile message for each of the four health behaviors (physical activity, screen time, SSB consumption, sleep) along with a fifth message corresponding to that week's weakest performing health behavior. The daily messages have been adapted from messages tested in a previous comparative effectiveness pediatric obesity study.19 Daily messages are delivered in random order from a computer-generated program at the same time each evening. The daily message provides feedback on the day's health behavior or prior evening's sleep along with personalized evidence-based clinical recommendations, tailored both to the degree (achieving vs. not achieving the daily clinical recommended level) and directionality over the previous several days (improved vs. no change vs. worse compared to last week) of the health behavior (Figure 3b). For example, a daily message for a participant reaching their health behavior goal may read “Great job! Congratulate Johnny for being on target with this behavior. Remember, you are Johnny's role model! Limit your own TV/screentime to help your children do the same.” Conversely, for a participant not reaching their health behavior goal, the daily message might say “Great progress. Think what the next step could be to help Susan reach the recommended goal. Make sleep a priority. Stick to regular bedtime & wake times for Susan.” Weekly progress reports are delivered via mobile messaging on Saturdays, the 6th day of the week cycle, providing feedback on the health behaviors over the past week, as well as tracking health behavior progress over the course of the study. Weekly progress reports show the weekly averages for each health behavior plotted as points on a graph connected by trend lines. The progress report graphs are color-coded with green (at goal), yellow (near goal), and red zones (not at goal), corresponding to clinical recommendations for that health behavior (Figure 3c). Color-coding is a pictorial technique used in multiple medical conditions including obesity and asthma to improve health literacy and has been shown to help facilitate parental understanding of medical risk.20, 21 After viewing the weekly progress report, parents are prompted to share and discuss the results with their child, also visible to children on a Kid's Zone screen in the mobile application. The Kid's Zone uses a reward system that provides virtual badges to document the child's progress in each of the four health behaviors and to encourage behavior change (Figure 3d). When a child is viewing the Kid's Zone page, the mobile application syncs with the child's wristband to authenticate that the child has viewed the Kid's Zone that week. From the mobile application's main page, participants are also able at any time to click to view the weekly progress report or the Kid's Zone.
In the control group, participants will have access to a modified mobile application, which, as in the intervention group, provides weekly progress reports of their health behaviors on the 6th day of the week cycle for self-guided care, however, does not provide the daily feedback and motivational messages or access to the Kid's Zone.
Analysis Plan
Descriptive statistics will report the study sample by study group assignment and baseline characteristics, including baseline BMI and health behaviors. Study feasibility will be assessed by reporting recruitment and retention statistics, along with mHealth use data including uptake and retention of technology use. We will record the number of times a child visits the Kid's Zone page, as well as, the frequency with which parents access progress reports, and track this over time. If the Kid's Zone page has not been accessed during 2 or more consecutive weeks, a study team member will contact the family to provide reminders about study protocol and assess for and trouble shoot problems. All outcomes will be measured as change at 6 months post enrollment. For the primary outcome, change in child BMI, we will assess change in BMI z-score (standard deviation score) slope based on the intention-to-treat principle using linear mixed effects models, controlling for study group, baseline BMI, age, sex, race/ethnicity, primary language, family education, and the census-derived median household income, with the participant as a random effect. For the secondary outcomes, change in parent BMI will be assessed using paired t-test analysis, and change in child and adult CMRD-related health behaviors will be calculated as an index score - a continuous variable calculated as the sum of Z-scores of mean daily moderate-to-vigorous physical activity (minutes), mean daily sleep (minutes), mean daily screen time (minutes), and mean weekly sugar sweetened beverage intake. A significance level of p<0.05 will be set a priori for all statistical tests.
A power analysis was performed to identify an anticipated change in BMI z-score of −0.05 in the intervention group, based on prior obesity interventions.18 To detect meaningful differences in the number of children successfully achieving this BMI reduction goal at 6 months, allowing for a two-sided 5% Type 1 error and 90% power and assuming an average baseline BMI z-score of 1.73 corresponding to a clinical category of overweight with a standard deviation of 0.06 among study subjects, and assuming 90% retention, we anticipate requiring 31 subjects per arm. Given an anticipated drop-out rate of 10%, 68 subjects will be recruited.
Discussion
The STRIVE will test a novel approach to using mHealth to counsel on health behaviors associated with cardiometabolic risk and disease. Unlike current health behavior assessment and counseling, STRIVE is a Just-in-Time Adaptive Intervention that will collect longitudinal, objective health behavior data and will provide a rapid closed-loop mechanism for providing personalized health behavior counseling.
Prior studies testing different approaches to counseling on cardiometabolic health behaviors have tended to provide generalized health tips without collecting health behavior data, to use self-reported health behavior data, to provide feedback on a single health behavior, or to have prolonged periods between health behavior assessment and provision of feedback.22–24 In the STRIVE study, we sought to overcome these limitations by developing a novel mHealth integrated closed-loop feedback approach that uses patient-generated data to provide daily, personalized, clinical recommendations. While objective assessment of specific individual risk-factors such as weight, physical activity, SSB consumption, and sleep have been well-studied, much less work has been done to assess all of these risk factors simultaneously over time and study their interaction. Recent advances in mHealth technology now enable continuous measurement of simultaneous health behavior data which can be used to enhance cardiometabolic disease care through personally tailored clinical counseling. STRIVE seeks to overcome many of the limitations inherent in current health behavior counseling mechanisms. We will collect data generated by patients in real-time to limit recall and social desirability bias, rather than relying on post-hoc reports. Three of the four health behaviors – physical activity, sleep, screen time – will be objectively measured, with only SSB consumption self-reported using EMA. This study will test an innovative approach using mHealth to simultaneously assess multiple biophysical indicators and health behaviors associated with cardiometabolic risk and disease. This study will collect data longitudinally and will determine the feasibility and measure the efficacy of using mHealth to provide frequent health behavior counseling. By creating an integrated feedback loop, this study will drastically shorten the time interval between health behavior data collection and clinical feedback. In the traditional outpatient healthcare setting, families receive counseling on their child's health behaviors once a year during the annual well-visit setting. In STRIVE, the clinical feedback loop is exponentially shortened, with families receiving daily counseling on health behaviors. Such time-sensitive feedback is more meaningful and understandable, likely to be more actionable, and may as a result be more effective. Prior studies that have not leveraged mHealth technology or created integrated feedback loops, have assessed feedback that is provided over longer time periods, often ranging from weeks to months,25–27 but there is a paucity of data on the efficacy of using daily feedback loops over extended periods of time.
The rapid feedback loop in STRIVE may also be well-suited to meet other specific related national health priorities, including national guidelines for treating obesity in children and adolescents through moderate-to-high intensity programs that provide 25 or more hours of contact with patients and families over 6 months.28 Such clinical recommendations are currently difficult to achieve but may be actionable with the novel technology and clinical feedback innovations tested in STRIVE.
Potential methodological limitations in this study may include equipment failure and data loss. The study has been designed to include mechanisms to overcome these anticipated limitations by leveraging the two-way communication application built into the study. In the case of any equipment failure or technology problem, the study team will be able to rapidly contact the participant and trouble shoot the technical or equipment difficulty through messaging, or, if needed by phone or in person. If a study participant forgets to wear the wristband, as data is collected in real-time via different sensors on the wristband, the lack of data return from the sensors assigned to that participant will alert the study team of the protocol deviation, and a study team member will be able to send a mobile message to the participant reminding him/her to wear the wristband. Similarly, if a participant does not provide weight data on a given day, a mobile message will be sent to the participant reminding him/her to take their weight. Another potential limitation is participant self-selection. Certain populations may not meet the selection criteria, most notably owning an Android smartphone or Wi-Fi access. While technology adoption and brand selection may differ among different populations, there is a priori no reason to believe iPhone and Android users have different health behaviors or cardiometabolic risk profiles that would lead to biased results. Technology use, including the use of smartphone applications, is known to wane over time and may contribute to participant burden, which may limit study participation. In this comparative effectiveness study, both the self-guided care control group and the closed-loop feedback intervention group have access to mHealth, and residual confounding from the different technology components available to each group will make it difficult to fully assign any observed effects.
Conclusion
This study will test a novel integrated closed-loop feedback system that provides personalized counseling on health behaviors among families at risk for or with established CMRD.
Acknowledgements
The authors thank Michael P. Duggan for his outstanding research assistance on this study. This trial is sponsored by the Agency for Healthcare Research and Quality grant # 1R21HS024001 (PI, Oreskovic). Dr. Sharifi is supported by a grant from the Agency for Healthcare Research and Quality (K12HS022986). Dr. Taveras is supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (K24DK10589).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Saydah S, Bullard KM, Imperatore G, Geiss L, Gregg EW. Cardiometabolic risk factors among US adolescents and young adults and risk of early mortality. Pediatrics. 2013;131(3):e679–86. doi: 10.1542/peds.2012-2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365(20):1876–1885. doi: 10.1056/NEJMoa1010112. [DOI] [PubMed] [Google Scholar]
- 4.Magnussen CG, Koskinen J, Chen W, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation. 2010;122(16):1604–1611. doi: 10.1161/CIRCULATIONAHA.110.940809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guyer B, Ma S, Grason H, et al. Early childhood health promotion and its life course health consequences. Acad Pediatr. 2009;9(3):142–149. e1–71. doi: 10.1016/j.acap.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213–56. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pollak KI, Krause KM, Yarnall KS, Gradison M, Michener JL, Ostbye T. Estimated time spent on preventive services by primary care physicians. BMC Health Serv Res. 2008;8 doi: 10.1186/1472-6963-8-245. 245-6963-8-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–641. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melnyk BM, Grossman DC, Chou R, et al. USPSTF perspective on evidence-based preventive recommendations for children. Pediatrics. 2012;130(2):e399–407. doi: 10.1542/peds.2011-2087. [DOI] [PubMed] [Google Scholar]
- 10.Baer HJ, Schneider LI, Colditz GA, et al. Use of a web-based risk appraisal tool for assessing family history and lifestyle factors in primary care. J Gen Intern Med. 2013;28(6):817–824. doi: 10.1007/s11606-013-2338-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naughton F. Nicotine Tob Res. 2016. Delivering `Just-In-Time' smoking cessation support via mobile phones: Current knowledge and future directions. [DOI] [PubMed] [Google Scholar]
- 12.Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;4:CD006611. doi: 10.1002/14651858.CD006611.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Becker MH, editor. The health belief model and personal health behavior. Health Education Monographs. 1974;2:324–473. [Google Scholar]
- 14.Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: theory, research, and practice. 3rd Wiley & Sons; San Francisco: 2002. [Google Scholar]
- 15.Oreskovic NM, Goodman E, Park ER, Robinson AI, Winickoff JP. Design and implementation of a physical activity intervention to enhance children's use of the built environment (the CUBE study) Contemp Clin Trials. 2014;40C:172–179. doi: 10.1016/j.cct.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 17.Woolford SJ, Barr KL, Derry HA, et al. OMG do not say LOL: obese adolescents' perspectives on the content of text messages to enhance weight loss efforts. Obesity (Silver Spring) 2011;19(12):2382–2387. doi: 10.1038/oby.2011.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taveras EM, Marshall R, Kleinman KP, et al. Comparative effectiveness of childhood obesity interventions in pediatric primary care: a cluster-randomized clinical trial. JAMA Pediatr. 2015;169(6):535–542. doi: 10.1001/jamapediatrics.2015.0182. [DOI] [PubMed] [Google Scholar]
- 19.Taveras EM, Marshall R, Horan CM, et al. Rationale and design of the STAR randomized controlled trial to accelerate adoption of childhood obesity comparative effectiveness research. Contemp Clin Trials. 2013;34(1):101–108. doi: 10.1016/j.cct.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 20.Oettinger MD, Finkle JP, Esserman D, et al. Color-coding improves parental understanding of body mass index charting. Acad Pediatr. 2009;9(5):330–338. doi: 10.1016/j.acap.2009.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paul TF, Brennan C. Asthma Charts and Forms. Pedipress Inc; Amherst, MA: 1996. [Google Scholar]
- 22.Pedersen S, Gronhoj A, Thogersen J. Texting your way to healthier eating? Effects of participating in a feedback intervention using text messaging on adolescents' fruit and vegetable intake. Health Educ Res. 2016;31(2):171–184. doi: 10.1093/her/cyv104. [DOI] [PubMed] [Google Scholar]
- 23.Hebden L, Cook A, van der Ploeg HP, Allman-Farinelli M. Development of smartphone applications for nutrition and physical activity behavior change. JMIR Res Protoc. 2012;1(2):e9. doi: 10.2196/resprot.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Militello L, Melnyk BM, Hekler EB, Small L, Jacobson D. Automated Behavioral Text Messaging and Face-to-Face Intervention for Parents of Overweight or Obese Preschool Children: Results From a Pilot Study. JMIR Mhealth Uhealth. 2016;4(1):e21. doi: 10.2196/mhealth.4398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woolford SJ, Clark SJ, Ahmed S, Davis MM. Feasibility and acceptability of a 1-page tool to help physicians assess and discuss obesity with parents of preschoolers. Clin Pediatr (Phila) 2009;48(9):954–959. doi: 10.1177/0009922809338060. [DOI] [PubMed] [Google Scholar]
- 26.Oreskovic NM, Goodman E, Robinson AI, Perrin EM, Perrin JM. Adolescent report of lifestyle counseling. Child Obes. 2014;10(2):107–113. doi: 10.1089/chi.2013.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perrin EM, Skinner AC, Steiner MJ. Parental recall of doctor communication of weight status: national trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2012;166(4):317–322. doi: 10.1001/archpediatrics.2011.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.US Preventive Services Task Force, Barton M Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010;125(2):361–367. doi: 10.1542/peds.2009-2037. [DOI] [PubMed] [Google Scholar]