Abstract
Objective
We examined the outcomes of the Child Health Initiative for Lifelong Eating and Exercise (CHILE) study, a group randomized controlled trial to design, implement, and test the efficacy of a trans-community intervention to prevent obesity in children enrolled in Head Start centers in rural American Indian and Hispanic communities in New Mexico.
Methods
CHILE was a 5-year evidence-based intervention that used a socioecological approach to improving dietary intake and increasing physical activity of 1898 children. The intervention included a classroom curriculum, teacher and food service training, family engagement, grocery store participation, and healthcare provider support. Height and weight measurements were obtained four times (fall of 2008, spring and fall of 2009, and spring of 2010), and body mass index (BMI) z-scores in the intervention and comparison groups were compared.
Results
At baseline, demographic characteristics in the comparison and intervention groups were similar, and 33% of all the children assessed were obese or overweight. At the end of the intervention, there was no significant difference between the two groups in BMI z-scores.
Conclusions
Obesity prevention research among Hispanic and AI preschool children in rural communities is challenging and complex. Although the CHILE intervention was implemented successfully, changes in overweight and obesity may take longer than 2 years to achieve.
Keywords: Childhood obesity, American Indian, Hispanic, rural, intervention, BMI z-score
Introduction1
Obesity in young children remains a major global public health problem, although the prevalence of childhood obesity has recently plateaued in some populations (Ogden et al., 2014; Skinner and Skelton, 2014; Wabitsch et al., 2014; Olds et al., 2011). Obesity is defined by the Centers for Disease Control and Prevention (CDC) as a body mass index (BMI) for age and weight in the 95th percentile or higher (Kuczmarski et al., 2002); overweight is the 85th to less than 95th percentile (Kuczmarski et al., 2002). Childhood overweight/obesity is a particular concern in underrepresented U.S. populations, including Hispanic and American Indian (AI) children. The 2011-2012 NHANES found that the overweight/obesity rate for 2- to 5-year-old Hispanic children was 31.5% and the obesity rate was 16.7% (Ogden et al., 2014); the corresponding values for non-Hispanic white children were 20.9% and 3.5%. National data on AI children remain limited, but the 2010 Pediatric Nutrition Surveillance System of the CDC observed an obesity/overweight rate of 41.2% and an obesity rate of 21.1% among AI or Alaska Native (AN) children aged 2 to 4 years (Dalenius et al., 2011). Compared with non-Hispanic white children, the risk of obesity was 35% higher in Hispanic children and 49% higher in AI/AN children (Pan et al., 2013).
A factor other than race/ethnicity that has been associated with an increased prevalence of childhood overweight/obesity is residence in a rural area. Data from the 1996-2006 NHANES and 2003 National Survey of Children's Health showed that among children aged 2 to 5 years, 27.2% of those in rural areas were overweight and 12.2% were obese; the rates in urban children were 21.8% and 10.7%, respectively (Liu et al., 2010). The increased prevalence of overweight and obesity in rural children has been associated with higher poverty levels; lack of access to healthy, affordable food; limited resources for physical education classes; and lack of access to safe places for physical activity (Liu et al., 2010; Corbett, et al., 2014; White House Task Force on Childhood Obesity, 2010).
In New Mexico, childhood obesity generally follows national trends. In the fall of 2014, 24.7% of children attending NM public kindergartens were overweight or obese and 11.6% were obese (New Mexico Department of Health, Healthy Kids New Mexico, 2014). These values represented a decrease since 2010, but the prevalence of overweight or obesity and obesity among AI and Hispanic kindergarten children remained high: 37.4% of AI and 26.2% of Hispanic children were overweight or obese and 23.5% and 11.8%, respectively, were obese. In non-Hispanic white kindergarteners, the prevalence of overweight and obesity was 18.7% and 6.7%, respectively.
Because of disparities associated with the population and rurality of New Mexico, childhood obesity is a principal health concern in the state. Approximately 47.3% of the population is Hispanic and 10.4% is AI, whereas the U.S. population is 17.1% Hispanic and 1.2% AI/AN (U.S. Census Bureau, 2013). Moreover, New Mexico is the fifth largest state by land mass but has an average of only 17.2 people per square mile; therefore, it is one of the most rural states (New Mexico Department of Health, 2014).
The Child Health Initiative for Lifelong Eating and Exercise (CHILE) trial was an intervention to address childhood obesity in New Mexico. CHILE was a 5-year group randomized controlled trial (RCT) of a trans-community (i.e., across multiple sectors of the community), evidence-based intervention among 1898 preschool children attending 16 Head Start (HS) centers in rural, predominantly Hispanic and AI communities (Cruz, et al., in press, Morshed, et al., 2016, Davis, et al., 2013; Cruz, et al., 2014; Sussman et al., 2010). The intervention, which used a socioecological approach to improving dietary intake and increasing physical activity, included six components directed at the individual, interpersonal, community, and policy levels. This paper describes the results of CHILE pertaining to its primary outcome: BMI z-score (BMIz).
Methods
Study design
The CHILE intervention has been described in detail elsewhere (Davis, et al., 2013; Cruz, et al., 2014; Sussman et al., 2010). Briefly, HS centers were eligible for the study if they had at least two classrooms, 15 or more 3-year-old children enrolled, a retention rate of at least 80% over 2 school years, a primarily Hispanic or AI student population, and a location in a nonmetropolitan community within 150 miles of the research center. HS centers housing other prekindergarten programs were excluded. HS centers were recruited by a community engagement specialist on the research team. Before randomization to intervention (n = 8) or comparison (n = 8) conditions, the HS centers were stratified according to the race/ethnicity and average BMI of the HS center's population. A cut point of 16.4 was used to define the two BMI strata. This value, chosen on the basis of a prerandomization sample of 3-year-old children measured by center staff, was close to the median and allowed a balanced distribution of HS centers within each racial/ethnic group.
A random uniform variable was generated for each HS center, and centers with lower values within each stratum were assigned to the intervention group until desired sample sizes were achieved. The sample size of 16 HS centers was determined by using data on changes in BMI percentile among 3-year-old AI children (unpublished data, RIOS Net, a practice-based research network in New Mexico). These data indicated that an intraclass correlation of between 0.01 and 0.05 was appropriate. For a pre-post randomized group design, we expected that standardized effect sizes of between 0.28 and 0.35 would have 80% power (Raudenbush and Xiao-Feng, 2001).
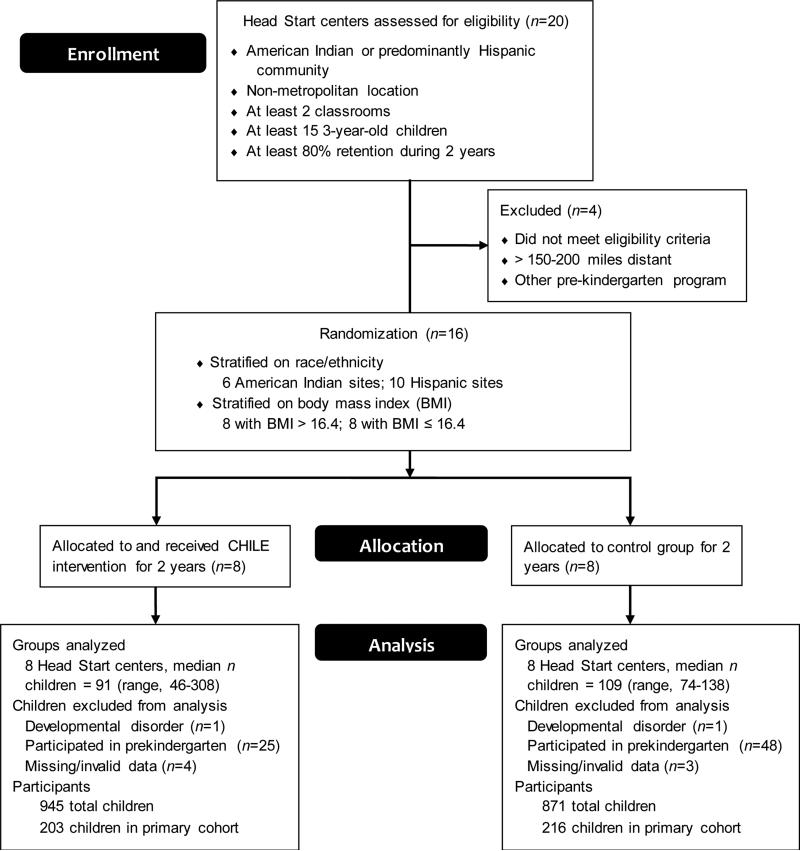
The randomization, intervention, and intention-to-treat analysis were done at the group (HS center) level (Figure 1). Height and weight data were collected at both the group and individual-child level. A parent or guardian provided active informed consent for all children enrolled in the CHILE trial, which was approved by the Human Research Protections Office of the University of New Mexico Health Sciences Center and conducted in accordance with HS center protocols and tribal processes.
Figure 1.
CONSORT diagram showing enrollment and analysis in the CHILE intervention.
Study population
The primary study population was the cohort of children under 4 years of age enrolled in one of the 16 participating HS centers in the fall of 2008 and followed for the 2 school years after randomization. Additional cohorts in the study were children attending the HS centers who were at least 4 years old but younger than 6 in the fall of 2008 and followed for 1 year; children who were at least 4 years old but younger than 6 in the fall of 2009 and followed for 1 year; and children who were under 4 years old in the fall of 2009 and followed for 1 year.
Intervention components
The six components of the CHILE intervention were previously described fully by Davis et al. (2013). Briefly, they are (1) a nutrition and physical activity curriculum for the HS centers that was designed to provide children with repeated opportunities to taste a new fruit or vegetable and to add 30 minutes of physical activity to daily class activities; (2) quarterly professional development training for HS teachers and food service staff to provide assistance in implementing the CHILE intervention and information about physical activity and nutrition; (3) a component focused on integrating policy and behavior change in food purchasing, preparation, and serving by HS food service staff; (4) a family component consisting of take-home materials about nutrition and physical activity and family events reinforcing these messages twice during the school year; (5) a local grocery store component with the goal of increasing availability and visibility of healthier food options and providing recipes and nutrition-related information to families while shopping; and (6) a component that asked local healthcare providers to emphasize healthy eating and physical activity during routine patient visits and invited health professionals to attend CHILE family events to show support for the intervention.
Collection of BMI data
To determine BMI percentiles for the children in the study, height and weight were assessed at the HS centers four times: at baseline (fall of 2008), twice during the intervention period (in the spring and fall of 2009), and after the intervention (spring of 2010). BMI percentiles were converted into BMIz values. The 2000 CDC growth charts (Kuczmarski, et al., 2002) were used to categorize the children as underweight, normal weight, overweight, or obese.
All measurements were performed by trained, certified CHILE personnel who followed a standardized protocol and used research-grade equipment. Three people participated in each measurement: a measurer, an assistant, and a recorder. Children removed heavy clothing, shoes, socks, and hair decorations that might interfere with the measurement. Height was recorded to the nearest 0.1 cm by using a stadiometer (Shorr board, Shorr Productions, Olney, MD). Weight was recorded to the nearest 0.1 kg with a Seca 770 scale (Seca, Chino, CA). Every measurement was done twice to optimize accuracy. Measurements not within tolerable limits (0.1 kg for weight, 0.6 cm for height) were conducted a third time. If two measurements within established limits could not be obtained, the data were excluded from analysis. A quality assurance monitor repeated the measurements on every tenth child to verify results.
Statistical analysis
Age at measurement (in months) was calculated for each child and measurement occasion. Replicated height and weight measurements from each occasion were averaged and used to determine BMI, BMI percentiles, and BMIz by using standard methods and computer codes described by the CDC (Kuczmarski, et al., 2002). Relative frequencies of children in different BMI percentile categories were calculated. BMIz is a relative measure of obesity calculated by subtracting the sex/age-specific median BMI from an external reference population value and dividing by the standard deviation for each reference population (Kuczmarski, et al., 2002). Cole et al. (2005) recommended BMIz for cross-sectional analyses and suggested BMI for longitudinal comparisons, whereas Must and Anderson (2006) recommended BMIz for longitudinal analyses. We used change in BMIz to assess the intervention because it removed the need to model separate sex and age effects and simplified the modeling of change over time because there should be no age-related trend in BMIz. The sample was in the age range in which adiposity rebound may be occurring, which would have required fitting nonlinear models for age separately for boys and girls and testing whether BMI trajectories differed according to study arm.
We used longitudinal mixed-model regression analyses to assess relationships between BMIz and the intervention. The primary analysis model included fixed effects for HS center race/ethnicity strata, prestudy BMI strata, gender, intervention, time in study, and intervention × assessment time interaction. BMIz data obtained before randomization indicated that BMIz values increase with age and therefore a strong intervention effect would be manifested by a significantly negative intervention × assessment time effect in the analysis model. Analyses accounted for repeated measurements for HS centers and children by including random effects for each center and child. Within-child residual errors were allowed to be correlated between periods by using a power function formulation equivalent to a first-order autoregressive correlation. A between-within strategy was used to allocate degrees of freedom so that inferences about the intervention were based on center-level units.
Additional analyses that treated time as a categorical variable were conducted to assess possible nonlinear changes in BMIz during the study. In this analysis, the time × period interaction contrast was used to evaluate whether the longitudinal change since baseline was the same for the intervention and the comparison group. All analyses were performed with SAS version 9.3 (SAS Institute Inc., Cary, NC).
The effects of the intervention were assessed by first analyzing the primary cohort of 3-year-old children who were enrolled in the study during fall 2008 and received the full 2 school years of the intervention. We then added children with partial interventions to the primary cohort results and conducted a combined analysis that included fixed effects for age at first study measurement, year of study, and an indicator for late entry into the study. Additional analyses according to gender, HS community race/ethnicity, center engagement, and secondary cohorts were conducted using the same basic mixed-model structure. Analyses were also conducted to assess whether the intervention effect was different for high, moderate, and low baseline child BMIz by creating an indicator variable for initial BMIz lower than -1.0 (bottom 15%), BMIz more than 1.0 (top 15%), and the middle 70% of BMIz values.
Results
Parents provided consent for 1902 children at 16 HS centers to participate in the study (74% of the eligible population), and 1898 children presented to be measured. Two children were excluded because of medical conditions that precluded use of the standard BMI-for-age growth charts. Other children were excluded from the analysis because they had also attended a prekindergarten class (n = 73) or had missing data (n = 7) (Figure 1); therefore, the analysis included 1816 children. The majority of participants (54%) were measured at baseline (fall of 2008) as part of the first cohort. Demographic characteristics for these 980 children, including their weight status (BMI percentile), are shown in Table 1. The intervention and comparison groups did not differ significantly at baseline. No HS center was lost to follow-up.
Table 1.
Demographic characteristics of the study sample of children at the fall 2008 (baseline) assessment time.a
| Characteristic | Total (n = 980) | Comparison group (n = 480) | Intervention group (n = 500) |
|---|---|---|---|
| Gender | |||
| Female | 464 (47.4) | 231 (48.1) | 233 (46.6) |
| Male | 516 (52.6) | 249 (51.9) | 267 (53.4) |
| Age, years | |||
| 2 | 16 (1.6) | 2 (0.4) | 14 (2.8) |
| 3 | 403 (41.1) | 214 (44.6) | 189 (37.8) |
| 4 | 543 (55.4) | 254 (52.9) | 289 (57.8) |
| 5 | 18 (1.8) | 10 (2.1) | 8 (1.6) |
| Center race/ethnicity | |||
| American Indian | 398 (40.6) | 203 (42.3) | 195 (39.0) |
| Hispanic | 582 (59.4) | 277 (57.7) | 305 (61.0) |
| Child ethnicity | |||
| Hispanic | 561 (57.2) | 253 (52.7) | 308 (61.6) |
| Non-Hispanic | 419 (42.8) | 227 (47.3) | 192 (38.4) |
| Child race | |||
| American Indian | 375(38.3) | 196 (40.8) | 179 (35.8) |
| White | 578 (59.0) | 266 (55.4) | 312 (62.4) |
| Other | 27 (2.7) | 18 (3.8) | 9 (1.8) |
| Weight status b | |||
| Underweight | 16 (1.6) | 12 (2.5) | 4 (0.8) |
| Healthy weight | 644 (65.7) | 319 (66.5) | 325 (65.0) |
| Overweight | 152 (15.5) | 66 (13.8) | 86 (17.2) |
| Obese | 168 (17.1) | 83 (17.3) | 85 (17.0) |
Values are numbers (percentages).
As indicated by BMI percentile for age and weight, with underweight defined as less than the 5th percentile; healthy weight as the 5th to less than the 85th percentile, overweight as the 85th percentile to less than the 95th percentile, and obese as equal to or greater than the 95th percentile.
Table 2 shows weight status, study arm, and assessment times for the primary age 3 cohort.
Table 2.
Weight status of the primary age 3 cohort at the four assessment times.a
| Assessment time | Total | Comparison group | Intervention group |
|---|---|---|---|
| Fall 2008 (baseline) | |||
| Underweight | 6 (1.4) | 4 (1.8) | 2 (1.0) |
| Healthy weight | 294 (67.4) | 148 (65.5) | 146 (69.5) |
| Overweight | 71 (16.3) | 35 (15.5) | 36 (17.1) |
| Obese | 65 (14.9) | 39 (17.3) | 26 (12.4) |
| Total n | 436 | 226 | 210 |
| Spring 2009 | |||
| Underweight | 4 (1.2) | 1 (0.6) | 3 (1.9) |
| Healthy weight | 219 (66.2) | 117 (67.2) | 102 (65.0) |
| Overweight | 54(16.3) | 26 (14.9) | 28 (17.8) |
| Obese | 54 (16.3) | 30 (17.2) | 24 (15.3) |
| Total n | 331 | 174 | 157 |
| Fall 2009 | |||
| Underweight | 4 (1.3) | 1 (0.7) | 3 (1.9) |
| Healthy weight | 197 (63.1) | 96 (63.6) | 101 (62.7) |
| Overweight | 57 (18.3) | 24 (15.9) | 33 (20.5) |
| Obese | 54 (17.3) | 30 (19.9) | 24 (14.9) |
| Total n | 312 | 151 | 161 |
| Spring 2010 | |||
| Underweight | 4 (1.4) | 2 (1.4) | 2 (1.4) |
| Healthy weight | 173 (60.5) | 88 (62.0) | 85 (59.0) |
| Overweight | 55 (19.2) | 26 (18.3) | 29 (20.1) |
| Obese | 54 (18.9) | 26 (18.3) | 28 (19.4) |
| Total n | 286 | 142 | 144 |
Values in parentheses are percentages of each group at the assessment time. Underweight was defined as less than the 5th BMI percentile for age and gender, healthy weight as the 5th to less than the 85th percentile, overweight as the 85th percentile to less than the 95th percentile, and obese as equal to or greater than the 95th percentile.
BMIz in the baseline sample (fall of 2008) of the primary age 3 cohort was greater than the expected value of zero (mean = 0.63; 95% CI, 0.47 to 0.78), with between-site variance, σ2Site = 0.039, and within-site variance, σ2Within = 1.167. BMIz did not differ with respect to center BMI strata (p = 0.8), gender (p = 0.8), or intervention status (p = 0.8). There was a weak trend for BMIz to increase by 0.32 (95% CI, −0.01 to 0.64) per year of age.
Change in BMIz per 6 months of study time for the primary age 3 cohort was similar for the comparison and intervention centers (p = 0.54; comparison slope = 0.038 [95% CI, 0.014 to 0.063]; intervention slope = 0.039 [95% CI, 0.014 to 0.063]; difference = 0.011 [95% CI −0.024 to 0.046]). For this analysis, the between-center variance was 0.002, the between-child variance was 1.004, and the residual within-child variance was 0.139, with autocorrelation equal to 0.62 for adjacent measurement periods. No heterogeneity of intervention effect was observed with respect to center race/ethnicity (p = 0 .38), gender (p = 0.41), or race/ethnicity × gender (p = 0.32). When all children were analyzed with added adjustments for age at entry into the study, year of study, and late entry into the study, no effect of the intervention on change in BMIz was observed (p = 0.69; difference in slopes = −0.006 [95% CI −0.031 to 0.020]). Among older children, BMIz increased more slowly with time in study, but the increase did not differ significantly according to whether they were in the intervention or comparison arm (p = 0.18). No treatment-effect heterogeneity was associated with community race/ethnicity or gender.
We further assessed how BMIz changed with time in study by treating time as a categorical variable. Table 3 shows how adjusted BMIz increased relative to baseline in the primary cohort, and Table 4 shows results for all ages combined.
Table 3.
Adjusted BMI z-score values for the primary age 3 cohort in the comparison and intervention groups, according to assessment time, with the change in BMIz from baseline values and the intervention × period (I × P) effect size.a
| Comparison group |
Intervention group |
|||||
|---|---|---|---|---|---|---|
| BMIz score | Change | BMIz score | Change | I × P effect | p-valueb | |
| Fall 2008 | 0.69 (0.074) | — | 0.64 (0.077) | — | — | 0.09 |
| Spring 2009 | 0.66 (0.075) | −0.02 (0.030) | 0.67 (0.078) | 0.03 (0.032) | 0.05 (0.044) | 0.25 |
| Fall 2009 | 0.78 (0.076) | 0.09 (0.035) | 0.70 (0.078) | 0.06 (0.035) | −0.03 (0.050) | 0.54 |
| Spring 2010 | 0.80 (0.077) | 0.11 (0.040) | 0.81 (0.080) | 0.17 (0.040) | 0.06 (0.057) | 0.34 |
Values in parentheses are standard errors. Scores were adjusted for center race/ethnicity strata, prestudy BMI strata, gender, and whether there were dropouts because of attending prekindergarten.
The fall 2008 p-value is for the overall intervention effect (intervention × assessment time interaction test result); the other p-values are for period-specific intervention effects not adjusted for multiplicity.
Table 4.
Adjusted BMI z-score values in the comparison and intervention groups for children of all ages, according to time since start of intervention, with time × intervention (T × I) contrast.a
| Time since start of intervention | Comparison group | Intervention group | T × I contrastb | p-valuec |
|---|---|---|---|---|
| At start | 0.65 (0.54–0.76) | 0.71 (0.60–0.82) | — | 0.07 |
| 7 months | 0.66 (0.55–0.77) | 0.74 (0.63–0.85) | 0.01 (−0.03–0.06) | 0.57 |
| 12 months | 0.77 (0.60–0.89) | 0.76 (0.65–0.88) | −0.07 (−0.14–0.00) | 0.06 |
| 19 months | 0.82 (0.70–0.94) | 0.86 (0.74–0.98) | −0.02 (−0.03–0.06) | 0.68 |
Values in parentheses are confidence intervals. Scores were adjusted for center race/ethnicity strata, prestudy BMI strata, gender, and whether there were dropouts because of attending prekindergarten.
Comparison of whether the change from baseline within the two arms was different in the comparison and intervention groups.
The at-start p-value is for the overall intervention effect (intervention × time interaction test result); the other p-values are for period-specific intervention effects not adjusted for multiplicity.
The primary cohort and all ages combined had a significantly higher BMIz at the end of the study, and neither group had an intervention-related difference in the final measurement (p > 0.3). Although an intervention effect in the intended direction was observed in the fall 2009 sample for the primary cohort, it was not significantly different from zero (p = 0.54). In the combined analysis, the fall 2009 and spring 2010 samples showed changes in BMIz consistent with the intended intervention effect, but the interaction contrast was not significant in either sample.
Additional analyses showed that overall BMIz increased from baseline by 0.18 (SE = 0.025, p < 0.001) for children with baseline BMI percentile < 85% but did not increase for children with baseline BMI percentile ≥ 85% (mean = −0.02, SE = 0.036, p = 0.57). However, there was no evidence of a differential intervention effect (p = 0.62). Change in BMIz for children in the intervention group with baseline BMI percentile ≥ 85% was 0.03 (SE = 0.073, p = 0.65) more than in the comparison group. Change for children in the intervention group with baseline BMI percentile < 85% was −0.01 (SE = 0.049, p = 0.83) lower than in the comparison group.
Discussion
To our knowledge, the CHILE trial was the first trans-community RCT of an intervention to prevent childhood obesity in preschool children attending HS centers in predominantly AI and Hispanic communities. The overall aim of the study was to design, implement, and test the efficacy of the intervention. CHILE received strong support from HS staff, families, and community members, including grocery store managers and healthcare providers (Cruz, et al., 2014). This paper describes the outcomes of an intervention to reduce the increase in BMI in the intervention group versus the comparison group. At the end of the intervention period, BMI values in the intervention and comparison groups were essentially the same.
As noted by several reviewers (Flynn et al., 2006; Bluford et al., 2007; Waters et al., 2011; Wang et al., 2013; Zhou et al, 2014), few obesity interventions have focused exclusively on preschool children, although more such programs are needed not only because of the consequences of early-life obesity but also to allow assessment of their outcomes in a variety of settings and populations. In their systematic review and metaanalysis, Waters et al. (2011) identified only eight studies of interventions to prevent obesity in children up to 5 years old that included a comparison group. In analyzing the combined results of all eight, Waters et al. found that the change in children's BMI from preintervention to postintervention was 0.26 unit less in the intervention groups than the comparison groups. The difference was not significant, but Waters et al. commented that their analysis indicated a trend toward a positive intervention effect.
Obesity intervention programs that, like CHILE, serve Hispanic preschool children remain uncommon, although Tovar et al. (2014) conducted a systematic review of eight interventions (primarily RCTs) in “immigrant populations” of primarily Hispanic children (51% to 100% of children enrolled; n = 33 to 401), all with a mean age of under 5 years. Five of the eight studies (Fitzgibbon et al., 2006; Yin et al., 2012; Bellows et al., 2013; Slusser et al., 2012; Fitzgibbon et al., 2013) were based in preschools, two (Barkin et al., 2012; Bender et al., 2013) in community or health centers, and one (Haines et al., 2013) in homes. All eight included nutrition and physical activity components, and some also had parenting and social networking components. Only four of the eight interventions (Barkin et al., 2012; Yin et al., 2012; Haines et al., 2013; Slusser et al., 2013) resulted in a significant decrease in the children's weight, weight gain, BMI, or BMIz.
Obesity prevention interventions for preschool AI children are even more uncommon than those for preschool Hispanic children, although two trials recently funded by the National Institutes of Health are now under way (Karanja, et al., 2010; Adams et al., 2012). Only one of the studies reviewed by Waters et al. (2011), a pilot RCT conducted more than 15 years ago in northern New York and southern Canada (Harvey-Berino and Rourke, 2003), focused on preschool AI children (n = 43 mother/child pairs). The intervention was a home visiting program delivered by AI peer educators. No significant changes in weight-for-height z-scores occurred, although children in the obesity prevention arm had a significant decrease in energy intake. A more recent study was an RCT that enrolled 454 AI kindergarten children in South Dakota (Story et al., 2012). The intervention focused on increasing physical activity and healthy eating at school and modifying the home environment to reduce excessive energy intake and television viewing and increase physical activity. By the final assessment, the intervention group had a significantly lower prevalence of overweight compared with the comparison group, but no difference in obesity prevalence, BMI, BMIz, skinfold thickness, or percentage of body fat.
Overall, interventions to prevent childhood obesity in Hispanic and AI preschool children have so far had mixed results with regard to weight gain or loss and adiposity, indicating the challenge of addressing obesity in these populations. Even studies with multiple intervention components have had limited success with respect to BMI outcomes, although some have observed improvements in other measures, including significant decreases in overall energy intake (Harvey-Berino and Rourke, 2003); consumption of sugar-sweetened beverages (Bender et al., 2013; Story et al., 2012), whole milk (Story et al, 2012), or chocolate milk (Story et al, 2012); and significant increases in gross motor skills and consumption of water and 1% or 2% milk (Bender et al., 2013; Bellows et al., 2013).
Limitations of the CHILE study included the drop out of students due to graduation or transfer to prekindergarten classes, the difficulty in instituting environmental and policy changes, and the large effect size required by the small number of study sites, which may have resulted in the study being underpowered. When the original power calculations were made, limited data were available to estimate the effect size. Finally, the study design precluded blinding to intervention status.
Major strengths of the study included the robust group RCT design; the trans-community nature of the intervention; the development and implementation of an evidence-informed developmentally and culturally appropriate curriculum; strong engagement from AI and Hispanic communities; and the high overall level of enrollment: 74% of children attending the HS centers. The translation potential of the study represents another strength. The CHILE curriculum was based on both national dietary (U.S. Department of Health and Human Services, U.S. Department of Agriculture, 2005) and national physical activity (NASPE, 2004) guidelines for 3- and 4-year-old children. Obesity prevention research among Hispanic and AI preschool children in rural communities is challenging and complex. Implementing policies consistent with national nutrition and physical activity guidelines is one component of a comprehensive childhood obesity prevention intervention. Recommendations for practice include involving multiple sectors of the community in the intervention: preschools, healthcare providers, grocery stores, children, and families. Future research should assess long-term outcomes of childhood obesity prevention interventions and the dissemination and implementation of interventions like CHILE in new communities.
Highlights.
CHILE was the first RCT of an obesity intervention in Hispanic and AI preschoolers.
CHILE documented the prevalence of obesity in the studied population.
No significant differences in BMI z-score outcomes were found.
Acknowledgements
We express our sincere thanks to the teachers, staff, and administration at the participating Head Start centers; the families and other community members who assisted in the development, implementation, and evaluation of the CHILE study; our community partners at the local grocery stores, who allowed us to implement CHILE in their stores; the health care providers who gave their time and support to the CHILE study; and members of the CHILE research team, past and present, who contributed their time and expertise to the work reported here. We also thank Renée J. Robillard for editorial assistance.
CHILE was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (grant R01 DK72958).
Footnotes
ClinicalTrials.gov identifier: NCT00428805
Abbreviations: AI, American Indian; AN, Alaska Native; BMI, body mass index; CDC, Centers for Disease Control and Prevention; CHILE, Child Health Initiative for Lifelong Eating and Exercise; HS, Head Start; NHANES, National Health and Nutrition Examination Survey; RCT, randomized controlled trial.
Conflict of Interest Statement
The authors declare no conflicts of interest.
References
- Adams AK, LaRowe TL, Cronin KA, Prince RJ, Wubben DP, Parker T, Jobe JB. The Healthy Children, Strong Families intervention: design and community participation. J. Prim. Prev. 2012;33:175–185. doi: 10.1007/s10935-012-0275-y. http://dx.doi.org/10.1007/s10935-012-0275-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkin SL, Gesell SB, Po'e EK, Escarfuller J, Tempesti T. Culturally tailored, family-centered, behavioral obesity intervention for Latino-American preschool-aged children. Pediatrics. 2012;130:445–456. doi: 10.1542/peds.2011-3762. http://dx.doi.org/10.1542/peds.2011-3762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellows LL, Davies PL, Anderson J, Kennedy C. Effectiveness of a physical activity intervention for Head Start preschoolers: a randomized intervention study. Am. J. Occup. Ther. 2013;67:28–36. doi: 10.5014/ajot.2013.005777. http://dx.doi.org/10.5014/ajot.2013.005777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender MS, Nader PR, Kennedy C, Gahagan S. A culturally appropriate intervention to improve health behaviors in Hispanic mother-child dyads. Child Obes. 2013;9:157–163. doi: 10.1089/chi.2012.0118. http://dx.doi.org/10.1089/chi.2012.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluford DA, Sherry B, Scanlon KS. Interventions to prevent or treat obesity in preschool children: a review of evaluated programs. Obesity (Silver Spring) 2007;15:1356–1372. doi: 10.1038/oby.2007.163. [DOI] [PubMed] [Google Scholar]
- Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur. J. Clin. Nutr. 2005;59:419–425. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- Corbett A, Gratale D, Ellis W, Revere C, Chang DI. Childhood Obesity Prevention Strategies for Rural Communities. The Nemours Foundation; Jacksonville, Florida: 2014. [04/10/15]. Available online at https://www.nemours.org/content/dam/hkhf/filebox/resources/supportingyourcause/Childhood_Obesity_Prevention_Toolkit_for_Rural_Communities.pdf. [Google Scholar]
- Cruz TH, Davis SM, Fitzgerald CA, Canaca GF, Keane PC. Engagement, recruitment, and retention in a trans-community, randomized controlled trial for the prevention of obesity in rural American Indian and Hispanic children. J. Prim. Prev. 2014;35:135–149. doi: 10.1007/s10935-014-0340-9. http://dx.doi.org/10.1007/s10935-014-0340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz TH, Sanders SG, Myers OB, O'Donald ER, Sheche JN, Davis SM. Effects of an obesity prevention intervention on physical activity among preschool children: the CHILE study. Health Promot. Prac. doi: 10.1177/1524839916629974. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalenius K, Borland E, Smith B, Polhamus P, Grummer-Strawn L. Pediatric Nutrition Surveillance 2010 Report. U.S. Department of Human Services, Centers for Disease Control and Prevention; Atlanta, Georgia: 2012. [04/10/15]. Available online at http://www.cdc.gov/pednss/pdfs/PedNSS_2010_Summary.pdf. [Google Scholar]
- Davis SM, Sanders SG, Fitzgerald CA, Keane PC, Canaca GF, Volker-Rector R. CHILE: an evidence-based preschool intervention for obesity prevention in Head Start. J. Sch. Health. 2013;83:223–229. doi: 10.1111/josh.12018. http://dx.doi.org/10.1111/josh.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Kong A, Braunschweig CL, Gomez-Perez SL, Odoms-Young A, Van Horn L, Christoffel KK, Dyer AR. Family-based Hip-Hop to Health: outcome results. Obesity (Silver Spring) 2013;21:274–283. doi: 10.1038/oby.2012.136. http://dx.doi.org/10.1002/oby.20269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino preschool children. Obesity. 2006;14:1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- Flynn MA, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, Tough SC. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’ recommendations. Obes. Rev. 2006;7(suppl. 1):7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- Haines J, McDonald J, O'Brien A, Sherry B, Bottino CJ, Schmidt ME, Taveras EM. Healthy Habits, Happy Homes: randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatr. 2013;167:1072–1079. doi: 10.1001/jamapediatrics.2013.2356. http://dx.doi.org/10.1001/jamapediatrics.2013.2356. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, Rourke J. Obesity prevention in preschool Native-American children. A pilot study using home visiting. Obes. Res. 2003;11:606–609. doi: 10.1038/oby.2003.87. [DOI] [PubMed] [Google Scholar]
- Karanja N, Lutz T, Ritenbaugh C, Maupome G, Jones J, Becker T, Aickin M. The TOTS community intervention to prevent overweight in American Indian toddlers: a feasibility and efficacy study. J. Community Health. 2010;35:667–675. doi: 10.1007/s10900-010-9270-5. http://dx.doi.org/10.1007/s10900-010-9270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- Liu J, Jones SJ, Sun H, Probst JC. Diet, Physical Activity, and Sedentary Behaviors as Risk Factors for Childhood Obesity: An Urban and Rural Comparison. South Carolina Rural Health Research Center; Columbia, South Carolina: 2010. [04/10/15]. Available online at http://rhr.sph.sc.edu/report/(9-1)Diet,%20Physical%20Activity%20and%20Sedentary%20Behaviors.pdf. [Google Scholar]
- Morshed AB, Davis SM, Keane PC, Mishra SI, Myers OB. The impact of the CHILE intervention on the food served in Head Start centers in rural New Mexico. J Sch Health. 2016;86(6):414–23. doi: 10.1111/josh.12393. doi: 10.1111/josh.12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Must A, Anderson SE. Body mass index in children and adolescents: considerations for population-based applications. Int. J. Obes. (Lond.) 2006;30:590–594. doi: 10.1038/sj.ijo.0803300. [DOI] [PubMed] [Google Scholar]
- NASPE . Physical Activity for Children: A Statement of Guidelines. 2nd ed. National Association for Sport and Physical Education; Reston, Virginia: 2004. [Google Scholar]
- New Mexico Department of Health [03/09/15];Health Equity in New Mexico: A Report on Racial and Ethnic Health Disparities. (9th ed.). 2014 Available online at http://nmhealth.org/publication/view/report/1346.
- New Mexico Department of Health, Healthy Kids New Mexico [04/10/15];New Mexico Childhood Obesity 2014 Update. 2014 Available online at http://nmhealth.org/data/view/chronic/1585/
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. http://dx.doi.org/10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds T, Maher C, Zumin S, Péneau S, Lioret S, Castetbon K, Bellisle, de Wilde J, Hohepa M, Maddison R, Lissner L, Sjöberg A, Zimmerman M, Aeberli I, Ogden C, Flegal K, Summerbell C. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int. J. Pediatr. Obes. 2011;6:342–360. doi: 10.3109/17477166.2011.605895. http://dx.doi.org/10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- Pan L, May AL, Wethington H, Dalenius K, Grummer-Strawn LM. Incidence of obesity among young U.S. children living in low-income families, 2008-2011. Pediatrics. 2013;132:1006–1013. doi: 10.1542/peds.2013-2145. http://dx.doi.org/10.1542/peds.2013-2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168:561–566. doi: 10.1001/jamapediatrics.2014.21. http://dx.doi.org/10.1001/jamapediatrics.2014.21. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Xiao-Feng L. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychol. Methods. 2001;6:387–401. [PubMed] [Google Scholar]
- Slusser W, Frankel F, Robison K, Fischer H, Cumberland WG, Neumann C. Pediatric overweight prevention through a parent training program for 2-4 year old Latino children. Child Obes. 2012;8:52–59. doi: 10.1089/chi.2011.0060. http://dx.doi.org/10.1089/chi.2011.0060. [DOI] [PubMed] [Google Scholar]
- Story M, Hannan PJ, Fulkerson JA, Rock BH, Smyth M, Arcan C, Himes JH. Bright Start: description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity (Silver Spring) 2012;20:2241–2249. doi: 10.1038/oby.2012.89. http://dx.doi.org/10.1038/oby.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman AL, Davis S. Integrating formative assessment and participatory research: building healthier communities in the CHILE Project. Am. J. Health Educ. 2010;41:244–249. doi: 10.1080/19325037.2010.10599150. http://dx.doi.org/10.1080/19325037.2010.10599150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tovar A, Renzaho AM, Guerrero AD, Mena N, Ayala GX. A systematic review of obesity prevention intervention studies among immigrant populations in the US. Curr. Obes. Rep. 2014;3:206–222. doi: 10.1007/s13679-014-0101-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau [5/19/ 2015];Annual estimates of the resident population by sex, age, race, and Hispanic origin for the United States and states: April 1, 2010 to July 1, 2013; 2013 population estimates. 2013 Available online at http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=PEP_2013_PEPASR6H&prodType=table.
- U.S. Department of Health and Human Services, U.S. Department of Agriculture [March 14, 2016];Dietary Guidelines for Americans. 2005 2005 Available online at http://health.gov/dietaryguidelines/dga2005/document/
- Wabitsch M, Moss A, Kromeyer-Hauschild K. Unexpected plateauing of childhood obesity rates in developed countries. B.M.C. Med. 2014;12:17. doi: 10.1186/1741-7015-12-17. http://dx.doi.org/10.1186/1741-7015-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Wu Y, Wilson RF, Bleich S, Cheskin L, Weston C, Showell N, Fawol O, Lau B, Segal J. Childhood Obesity Prevention Programs: Comparative Effectiveness Review and Meta-analysis. Comparative Effectiveness Review No. 115. Agency for Healthcare Research and Quality; Rockville, Maryland: 2013. Available online at http://www.ncbi.nlm.nih.gov/books/NBK148737/pdf/TOC.pdf. [PubMed] [Google Scholar]
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, Armstrong R, Prosser L, Summerbell CD. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011:CD00187. doi: 10.1002/14651858.CD001871.pub3. http://dx.doi.org/10.1002/14651858.CD001871.pub3. [DOI] [PubMed]
- White House Task Force on Childhood Obesity . Report to the President: Solving the Problem of Childhood Obesity Within a Generation. Executive Office of the President of the United States; 2010. [04/10/15]. Available online at http://www.letsmove.gov/sites/letsmove.gov/files/TaskForce_on_Childhood_Obesity_May 2010_FullReport.pdf. [DOI] [PubMed] [Google Scholar]
- Yin Z, Parra-Medina D, Cordova A, He M, Trummer V, Sosa E, Gallion KJ, Sintes-Yallen A, Huang Y, Wu X, Acosta D, Kibbe D, Ramirez A. Míranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Child Obes. 2012;8:429–439. doi: 10.1089/chi.2012.0125. http://dx.doi.org/10.1089/chi.2012.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou YE, Emerson JS, Levine RS, Kihlberg CJ, Hull PC. Childhood obesity prevention interventions in childcare settings: systematic review of randomized and nonrandomized controlled trials. Am. J. Health Promot. 2014;28:e92–103. doi: 10.4278/ajhp.121129-LIT-579. http://dx.doi.org/10.4278/ajhp.121129-LIT-579. [DOI] [PubMed] [Google Scholar]