Abstract
Objective
This study tested whether discrepancy between patients' and therapists' ratings of the therapeutic alliance, as well as convergence in their alliance ratings over time, predicted outcome in chronic depression treatment.
Method
Data derived from a controlled trial of partial or non-responders to open-label pharmacotherapy subsequently randomized to 12 weeks of algorithm-driven pharmacotherapy alone or pharmacotherapy plus psychotherapy (Kocsis et al., 2009). The current study focused on the psychotherapy conditions (N = 357). Dyadic multilevel modeling was used to assess alliance discrepancy and alliance convergence over time as predictors of two depression measures: one pharmacotherapist-rated (Quick Inventory of Depressive Symptoms-Clinician; QIDS-C), the other blind interviewer-rated (Hamilton Rating Scale for Depression; HAMD).
Results
Patients' and therapists' alliance ratings became more similar, or convergent, over the course of psychotherapy. Higher alliance convergence was associated with greater reductions in QIDS-C depression across psychotherapy. Alliance convergence was not significantly associated with declines in HAMD depression; however, greater alliance convergence was related to lower HAMD scores at 3-month follow-up.
Conclusions
The results partially support the hypothesis that increasing patient-therapist consensus on alliance quality during psychotherapy may improve treatment and longer-term outcomes.
Keywords: alliance, alliance convergence, chronic depression, dyadic data analysis, REVAMP
A strong therapeutic alliance has consistently related to positive psychotherapy outcomes. A meta-analysis of 190 independent studies revealed that the alliance had a modest but significant effect (weighted r = .28, p < .0001), explaining about 7.5% of outcome variance (Horvath, Del Re, Flückiger, & Symonds, 2011). Few major moderators of the alliance-outcome effect have emerged, suggesting that alliance quality relates to outcome irrespective of treatment type, clinical condition, outcome rated, timing of alliance measurement, or alliance rater. Moreover, several studies have shown that the alliance relates to subsequently-rated outcome after controlling for prior change on the outcome measure (Arnow et al., 2013; Falkenström, Grantström, & Holmqvist, 2014; Klein et al., 2003). This stringent test of the alliance-outcome link implies that a good alliance generates symptom change, as opposed to simply representing a positive byproduct of symptom improvement. Thus, evidence suggests that psychotherapists can improve outcomes by establishing quality alliances with their patients (Muran & Barber, 2010).
As Bordin (1979) theorized, the alliance is fundamentally dyadic, reflecting patient-therapist instrumental coordination and interwoven subjective experiences. Yet there has historically been a mismatch between the dyadic nature of the construct and the way it is measured (Krasikova & LeBreton, 2012; Markin, Kivlighan, Gelso, Hummel, & Spiegel, 2014). Although many existing measures assess various dyadic properties of the relationship (e.g., perceived agreement on goals), and can do so through patient, therapist, or observer lenses, the vast majority of studies model alliance-outcome associations from one perspective at a time, thus obscuring the dyad (Elvins & Green, 2008; Horvath et al., 2011). Although equal in predictive importance, patient and therapist alliance ratings are not interchangeable (Stiles, Agnew-Davies, Hardy, Barkham, & Shapiro, 1998). Therapist and patient alliance ratings likely carry distinct information because of the inherent asymmetry in the psychotherapy relationship (Markin et al., 2014). Supporting this theoretical point, research has shown that therapist and patient alliance ratings are only moderately correlated with one another, despite their comparable associations with outcome (Horvath et al., 2011; Tryon, Blackwell, & Hammel, 2007). Thus, to understand better how the alliance relates to clinical processes and outcomes, it seems important to investigate patient-therapist (a) discrepancies/similarities in their perceptions of their alliance (i.e., level of agreement on alliance quality at one particular time point) and (b) divergences/convergences in their perceptions of their alliance (i.e., degree of change in agreement on alliance quality over time).
Such inquiry dovetails with research distinguishing different sources of variability in therapeutic alliance (Baldwin, Wampold, & Imel, 2007; DeRubeis et al., 2005), separating factors related to patient or therapist individual characteristics versus dyadic factors uniquely attributable to the specific patient-therapist pairing and relationship. Some recent studies have utilized dyadic analysis techniques that decompose which aspects of the alliance derive from therapist effects rather than unique aspects of the relationship (see Marcus, Kashy, & Baldwin, 2009, and Manne et al., 2012, for descriptions of the one-with-many design). Notably, these studies found that when accounting for the variability in alliance scores due to therapist factors (i.e., variance in the alliance ratings that were true for therapists no matter which patient's therapy was being assessed), the majority of the variation in alliance scores was due to unique factors within a particular patient-therapist relationship. In the present study, we focused on that part of the alliance that is attributable to the therapy dyad, with an emphasis on discrepancy/similarity and divergence/convergence in patients' and therapists' perspectives of alliance quality.
We argue that the discrepancy or divergence between patients' and therapists' alliance ratings may approximate part of the dynamic interplay that occurs during psychotherapy (Swift & Callahan, 2009; Tryon et al., 2007). For example, differences in perceived alliance quality, at one time or gradually over time, may reflect a lack of mutual clarity or shared understanding of the therapy goals, which could impede change. Even if they agree on treatment goals and tasks, therapists and patients could still have different views on how strong a bond they share. Such differences could represent alliance ruptures, which have been shown to relate to poorer treatment outcomes (Eubanks-Carter, Muran, & Safran, 2010). On the other hand, momentary similarity or convergence over time between patients' and therapists' alliance perceptions might indicate shared understanding of the therapy process and shared subjective experience of the relationship. This could reflect a natural relationship progression, or perhaps a rupture repair that might in turn be associated with better psychotherapy outcome.
Our discrepancy/similarity and divergence/convergence conceptualization is consistent with several researchers' calls for using both patient and therapist ratings to capture the alliance both statically and dynamically (Elvins & Green, 2008; Laurenceau, Hayes, & Feldman, 2007; Kivlighan, 2007). A small literature has used both patient and therapist data together when considering alliance discrepancy/similarity at a particular time point and divergence/convergence over time. For example, one study examined patient-therapist alliance rating similarity at the third session of psychotherapy for 63 therapy dyads from counseling clinics (Marmarosh & Kivlighan, 2012); the authors found that more similarity was related to greater symptom improvement. This finding, though, was specific to therapy dyads with higher-rated alliances, suggesting an interaction between early alliance levels and patient-therapist perceptual similarity of their alliance. In a study of 270 dyads, similarity in patients' and therapists' alliance perspectives increased from week 3 to week 12 of psychotherapy (Hersoug, Høglend, Monsen, & Havik, 2001). Similarly, a more recent study utilizing repeated measures of patient-therapist ratings of the therapeutic bond found evidence that therapists' ratings were systematically lower than patients' but also found that the discrepancy between their viewpoints decreased over the course of psychotherapy (Atzil-Slonim et al., 2015). Although alliance convergence has been found in several studies its relation to psychotherapy outcome was not examined. Thus, there is limited evidence that examining divergence/convergence in alliance ratings over time, and not just discrepancy/similarity cross-sectionally, may elucidate understanding of fluctuations in alliance ratings and how they relate to outcome (Kramer, de Roten, Beretta, Michel, & Despland, 2008; Laurenceau et al., 2007).
The dyadic interplay between patients and therapists may have particular relevance in treating chronic depression, where interpersonal issues are often salient (Constantino et al., 2008; Markowitz, 1998). Researchers who have examined the interactional nature of depression posit that interpersonal processes lie at its core and maintenance (Joiner, 2002; Joiner, Coyne, & Blalock, 1999). Chronically depressed patients often present with interpersonal wariness, distorted perceptions of interpersonal encounters, and impaired empathy and responsiveness (McCullough, 2000), and improvement in certain interpersonal characteristics (e.g., decreased hostile-submissiveness) has been shown to relate positively to outcome in chronic depression treatment studies (e.g., Constantino et al., 2012). Thus, there is evidence that interpersonal processes matter for chronically depressed individuals and their treatment. Moreover, basic research on depression has suggested that greater interpersonal attunement (e.g., of nonverbal support-giving and support-seeking behaviors) relates to a more favorable course of subsequent depression (Geerts, Bouhuys, & Van den Hoofdakker, 1996). In light of these various works, examining discrepancy/similarity (at a particular time) and divergence/convergence (across time) in patient-therapist views of their alliance quality may inform the treatment of chronic depression. Such work complements studies that have shown that the alliance, at least when using single perspective ratings, predicts positive outcomes in psychotherapies for this clinical population (Arnow et al., 2013; Klein et al., 2003).
The specific aims of this study were to test whether alliance discrepancy/similarity and divergence/convergence were associated with psychotherapy outcome in a sample of chronically depressed patients. We used dyadic statistical modeling techniques that incorporate both therapists' and patients' reports of the alliance and appropriately account for the interdependence between them (Kenny, Kashy, & Cook, 2006; Laurenceau et al., 2007). Based on the few prior studies of alliance discrepancy/similarity and divergence/convergence, we had several hypotheses. First, consistent with limited prior research (Hersoug et al, 2001), we hypothesized that discrepancy in alliance ratings (i.e., patient and therapist differences in their experience/perception of their relationship) would decrease over the course of psychotherapy, indicating perspective convergence (i.e., coming to see the state of the relationship more similarly). Theoretically, this might reflect an ongoing negotiation of the therapeutic relationship that becomes more attuned as the relationship evolves; that is, whatever the state of the relationship, the participants are able to read it more similarly whether it is thriving or in rupture. Second, and also consistent with limited prior research (Marmarosh & Kivlighan, 2012), we hypothesized that alliance perspective discrepancy measured in early therapy would be associated with less depression reduction (or, conversely, that greater alliance perspective similarity would be associated with greater depression reduction). Third, we predicted that convergence in patient-therapist alliance ratings over the course of therapy would be associated with greater depression reduction. The notion for this novel analysis is that such convergence would indeed reflect a successfully attuned relationship negotiation (see the first hypothesis above), which would positively influence therapeutic change.
Method
Sample and Procedure
Data derived from a large multisite study of chronic depression—the Research Evaluating the Value of Augmenting Medication with Psychotherapy (REVAMP) trial (Kocsis et al., 2009). This trial had two phases, each lasting 12 weeks. In the first 12-week phase, 808 chronically depressed adults received open-label, algorithm-driven medication and were monitored for treatment response. Patients who did not fully respond (N = 491) after 12 weeks entered the study's second phase, in which they were randomized to receive either continued antidepressant medication alone (N = 96) or combined medication and a psychotherapy (N = 395) for an additional 12 weeks. The psychotherapy comprised 16-20 sessions of either cognitive-behavioral analysis system of psychotherapy (CBASP; N = 200) or brief supportive psychotherapy (BSP; N = 195). Results from phase 2 of the study showed that depression improved in all three continuation conditions, with no significant differences between them (Kocsis et al., 2009). The current study excluded patients in the medication-alone arm, as pharmacotherapist-patient alliances were not assessed. Psychotherapy patients who had no alliance ratings (either self- or therapist-rated; n = 38) were also excluded, leaving a subsample of 357 psychotherapy dyads.1 Patients and therapists rated their perceptions of the alliance at weeks 2 (early), 6 (middle), and 12 (late) of psychotherapy. The subsample was primarily Caucasian, college-educated, and middle-aged (see Table 1).
Table 1. Subsample Characteristics (N = 357).
| Age in years, M (SD) | 46.96 (11.62) |
| % Female | 56% |
| Ethnicitya | |
| African American | 5.6% |
| Caucasian | 92.4% |
| Other | 5.0% |
| Hispanic ethnicity b | |
| Yes | 7.6% |
| No | 91% |
| Education in years, M (SD) | 16 (3) |
| Marital status | |
| Divorced, widowed or separated | 27.7% |
| Married or cohabitating | 41.7% |
| Never married | 30.6% |
| Baseline HAMD, M (SD), range | 19.29 (8.18), 1 - 38 |
| Baseline QIDS-C, M (SD), range | 10.08 (4.25), 0 - 22 |
Note.
Percentages are greater than 100 because participants could select more than one category;
Percentages do not total 100 due to missing data.
Treatments
Pharmacotherapy was algorithm-driven, based on empirically derived regimens (Kocsis et al., 2009). Prior treatment history determined the initial medication patients received; study medications included sertraline, escitalopram, buproprion XL, venlafaxine XR, mirtazapine, and lithium. Participants were evaluated biweekly, and were moved to the next option in the sequence if intolerant to a medication.
CBASP is a manualized cognitive-behavioral intervention specifically created to treat chronic depression (McCullough, 2000). CBASP conceptualizes chronically depressed individuals as having difficulty accurately perceiving the relationship between their thoughts, behaviors, and environmental consequences. A key CBASP intervention is situational analysis, a structured, directive intervention that uses detailed accounts of patients' social interactions between sessions to enhance awareness of how their thoughts influence their behavior and associated outcomes.
BSP is a supportive, client-centered intervention with added psychoeducation about chronic depression (Markowitz, Manber, & Rosen, 2008). This treatment attempted to capture the nonspecific aspects of psychotherapy and to provide a contrast to the structure of the CBASP intervention. BSP therapists empathically responded, normalized patients' feelings of anger and sadness, conveyed therapeutic hope, and non-directively encouraged patients to find their own solutions. Treatment pace and session focus was patient-driven, in contrast with the more structured CBASP intervention. Also unlike CBASP, BSP required no formal homework.
Therapists
Pharmacotherapists dispensed medications and did not provide psychotherapy. As noted, they did not complete alliance measurements and, thus, were not a focus of the present analyses.2 Psychotherapists, nested within the two psychotherapy conditions, were licensed practitioners with at least two years of postdoctoral clinical experience after completing a psychology doctorate or psychiatry residency, or five years of clinical experience after completing a master's in social work degree. There were 20 therapists in the CBASP condition (M patients = 12.60, SD = 5.29, range 1-22), and 21 in the BSP condition (M patients = 11.44, SD = 5.29, range 2-19). All therapists engaged in weekly supervision with on-site supervisors, and monthly phone-based supervision with CBASP and BSP expert supervisors. Randomly selected session tapes in each condition were rated for protocol adherence. Of the 152 tapes rated for adherence, only one CBASP session evinced inadequate protocol adherence (Kocsis et al., 2009).
Measures
Working Alliance Inventory-Short Form
The Working Alliance Inventory (WAI; Horvath & Greenberg, 1989) is the most widely used self-report measure of alliance quality (Elvins & Green, 2008; Horvath et al., 2011). Based on Bordin's (1979) tripartite, pantheoretical conceptualization of the alliance (i.e., agreement on goals, agreement on tasks, and emotional bond), the WAI has parallel patient and therapist versions. A 12-item short form, adapted by Tracey and Kokotovic (1989), provides an acceptable and valid abbreviated version of the longer measure. Items are rated on a 7-point scale from 1 (Never) to 7 (Always). Total scores summed across the three subscales can range from 12 to 84, with higher values indicating a stronger alliance. WAI total score internal consistency (alpha) was excellent in this sample for both patient (early = .903, mid = .928, late = .926) and therapist (early = .932, mid = .963, late = .957) ratings.
Quick Inventory of Depressive Symptomatology-Clinician Version (QIDS-C)
Pharmacotherapists administered the clinician version of the Quick Inventory of Depressive Symptomatology (QIDS-C; Rush et al., 2003) at each of the six visits. The QIDS-C, a 16-item measure, assesses Diagnostic and Statistical Manual of Mental Disorders-4th edition (DSM-IV; American Psychiatric Association, 1994) depressive symptom categories in the previous week. Clinicians rate each item on a 0 to 3 scale, reflecting lower to higher symptom frequency and severity. Item responses were summed to create an overall depression index, with higher values indicating greater depression (possible range = 0 to 48). In the current sample, the QIDS-C showed adequate internal consistency, with alphas ranging from .722 to .785 across the biweekly assessments.
Hamilton Rating Scale for Depression
Trained assessors, blind to treatment condition, assessed patient depression using the Hamilton Rating Scale for Depression (HAMD; Hamilton, 1967), a widely used interview assessment. The 24-item version used in this trial includes cognitive items characteristic of chronically depressed individuals. Assessors rate HAMD items on 0 to 2, 0 to 3, or 0 to 4 scales depending on the symptom assessed. Items are summed to create a total score ranging from 0 to 75, with higher values indicating greater depression. During each of the multiple HAMD administrations, patients were instructed not to mention their psychotherapy or psychotherapists to preserve rater blinding. In the current sample, the HAMD showed good internal consistency, with alphas ranging from .845 to .899 across the biweekly assessments.
Statistical Analyses
Data analyses were conducted in three steps. In the first step, we used a difference score model to estimate the difference between patient and therapists' alliance ratings to create measures of dyadic alliance differences at each measurement occasion (Lyons & Sayer, 2005). In the second step, we used a linear growth model of dyadic alliance discrepancy over the 12 weeks of psychotherapy. This growth model tested whether patient-therapist discrepancies in alliance ratings changed over the course of psychotherapy (i.e., became more convergent or divergent over time). In the third modeling step, we used measures of early (week 2) alliance discrepancy/similarity and across-therapy alliance divergence/convergence to predict depression symptom change trajectories over the course of psychotherapy. We used the Hierarchical Linear Modeling program (HLM7; Raudenbush, Bryk, & Congdon, 2011) to estimate the models in each step. The key statistical advantage of HLM is that it controls for the three sources of dependency in the models: the correlation among the repeated measures over time, the correlation in the pair of alliance scores within each dyad (patient and therapist), and the correlations due to multiple patients having the same therapists. In addition, HLM employs maximum likelihood estimation, which provides model-based estimates for all missing values and is one of several recommended means of handling missing data (Allison, 2009).
Results
Convergence in Alliance Ratings Across Psychotherapy
To examine alliance divergence/convergence, we first descriptively examined the mean alliance scores for patients and therapists. Raw mean discrepancies were largest at week 2 (Mraw discrepancy = 7.76, SD = 12.47) and smallest at Week 12 (M raw discrepancy = 5.17, SD = 12.02). Bivariate Pearson correlations showed a similar pattern: therapists' and patients' scores were significantly correlated, with a descriptive trend of increased correlations as psychotherapy progressed (rearly = .370, rmiddle = .525, rlate = .553, all ps < .001). Based on this descriptive evidence, alliance rating discrepancies decreased in magnitude over time (or, stated differently, they converged). However, more complex modeling was needed to test whether this decrease was statistically significant. In addition, observed data contains measurement error that may distort the underlying discrepancies. We used multilevel models to estimate the latent difference between patients' and therapists' alliance ratings.
This first modeling step accounted for three sources of nesting: repeated measures within individuals (Level 1), individuals within psychotherapy dyads (Level 2), and psychotherapy relationships within therapists (Level 3). For each dyad, the average alliance level and the difference between patients' and therapists' alliance ratings were modeled at weeks 2 (early), 6 (middle), and 12 (late). Two coefficients characterized the basic discrepancy model for each time point: one capturing the dyad average (the model intercept) at each measurement occasion, and one capturing the difference between the reports at each occasion. This was a multivariate outcomes model (Raudenbush, Brennan, & Barnett, 1995), which modeled the three measurement occasions simultaneously to account for between-dyad correlations among the scores. The difference variable was effects-coded to ensure that the zero value represented the dyad average; that is, therapist scores were coded (-.5), while patient scores were coded (.5). In addition, nesting of dyadic relationships within therapists was accounted for at Level 3. The equations for this model were:
Level 1
Level 2
Level 3
WAIij represents the alliance score i in dyad j (i = 1,…6 scale scores per dyad). Under this formulation, coefficients labeled “Average” (π1, π3, π5) represent the expected value of the outcome “WAI” when the predictor “Difference” is zero (i.e., the average of the two alliance reports). The model “Difference” coefficients (π2, π4, π6) represent the difference in WAI between the two members of the therapy dyad. Three alliance measures per dyad member (the bond, task, and goals WAI subscales) at each measurement occasion were used rather than the composite score, to address the issue of limited information and avoid model identification problems (Cano, Johansen, & Franz, 2005). Random effects (r1 - r6) for each variable were included at level 2, so that dyadic alliance average and difference were allowed to vary across therapy dyads. Finally, a third level was included with therapist random effects (u1 - u6) to appropriately control for variation in dyadic alliance due to therapist effects, rather than unique features of the dyad (Wampold & Brown, 2005). Model coefficients and variance components are presented in Table 2. Post-estimation coefficients (in HLM, empirical Bayes or EB estimates) were output from the HLM residual file. Figure 1 provides model estimated alliance patterns for four unique dyads in the dataset. This figure demonstrates the significant variability in patient-therapist discrepancy/similarity and divergence/convergence present in this sample.
Table 2. Parameter Estimates and Associated Standard Errors for Dyad Average and Dyad Difference for Early, Middle, and Late Alliancea.
| Coefficients | S.E | |
|---|---|---|
|
|
||
| Fixed Effects | ||
| Early Alliance | ||
| Average, γ10 | 63.34 | .89 |
| Difference, γ20 | 7.16 | 1.30 |
| Middle Alliance | ||
| Average, γ30 | 65.97 | .91 |
| Difference, γ40 | 5.65 | 1.39 |
| Late Alliance | ||
| Average, γ50 | 68.59 | .62 |
| Difference, γ60 | 4.94 | .76 |
| Random Effects | Variance Components | |
|
|
||
| Level 1, eijk (Individual-level residuals) | 43.22 | |
| Level 2 (Dyad Effects) | ||
| Early Average, τπ11 | 74.76 | |
| Early Difference, τπ22 | 100.79 | |
| Middle Average, τπ33 | 87.31 | |
| Middle Difference, τπ44 | 80.67 | |
| Late Average, τπ55 | 98.62 | |
| Late Difference, τπ66 | 76.84 | |
| Level 3 (Therapist Effects) | ||
| Early Average, τβ11 | 17.57 | |
| Early Difference, τβ22 | 38.30 | |
| Middle Average, τβ33 | 16.49 | |
| Middle Difference, τβ44 | 47.84 | |
| Late Average, τβ55 | 15.52 | |
| Late Difference, τβ66 | 38.60 | |
| Model Deviance (df) | 31036.32 (49) | |
All values were statistically significant, p < .001 with the exception of residual variance at level 1, which does not have an associated significance test within the HLM program.
Figure 1.

Patterns of dyadic alliance change over time. Panel A shows a therapy dyad with a convergent alliance process and high alliance levels, in which the patient rated the alliance higher than the therapist. Ratings were more divergent early in psychotherapy, and became more similar as psychotherapy progressed. This was the most common pattern found in this study, as indicated by fixed effects results from the convergence model (Table 3). Panel B shows a convergent but low alliance, with the therapist rating slightly higher than the patient. Panel C shows a divergent alliance process, in which the patient rated the alliance lower and the discrepancy between the ratings increased. Panel D shows a divergent dyadic alliance process, in which the patient and therapist viewed their alliance relatively similarly at the beginning of treatment (low discrepancy), but became more divergent over time (divergence). Here, the therapist saw the alliance as poorer, while the patient rated it highly and also reported increased alliance as the therapy progressed. Exemplars are drawn from the Empirical Bayes coefficients of dyadic alliance discrepancy and dyadic alliance level output from the first step of HLM analyses.
The next analytic step modeled absolute alliance discrepancy scores longitudinally to test for change over time.3 This was a growth curve model, with the outcome (Alliance Discrepancy) measured at three time points (weeks 2, 6, and 12). The original coding for time was rescaled to capture the total change over the entire therapeutic period (Bolger & Laurenceau, 2013). That is, the value of the first measure (week 2) was set to 0, the value of the second measure (week 6) was set to .4, and the value of the final session (week 12) was set to 1. Thus, a one-unit change in the linear slope parameter would represent alliance discrepancy change across the entire psychotherapy period. The equations for the absolute discrepancy change model were as follows:
Level 1:
Level 2:
Level 3:
At level 1, the within-dyad model, π0j is the model intercept and represents the expected value of dyadic alliance discrepancy early in therapy (at Week 2). π1 is the model slope and represents the change in discrepancy for a 1-unit change in time, or the change over the course of psychotherapy based on our coding of time. At level 2, the between-dyad model, these coefficients become outcomes, where β00 represents the average dyad's discrepancy at Week 2 and β10 represents the average dyad's linear change in discrepancy over the course of 12 weeks. The r's are the level-2 random effects and represent the dyad-specific deviation from the average dyad score. Finally, level 3 accounted for therapists effects, with variability around both the intercept and slope (u's).
Results from the fixed effects portion of this model indicated that, on average, alliance discrepancy significantly decreased over the course of psychotherapy, indicating increasing convergence in patients' and therapists' views of their alliance. The final model included psychotherapy condition, but as expected found no significant difference between CBASP and BSP in either alliance discrepancy (intercept) or convergence (slope) of alliance ratings (see Table 3). For the random effects portion of the model, significant variability was found both around the average alliance discrepancy early in psychotherapy, as well as in the alliance divergence over time. Of particular interest, while the majority (77%) of psychotherapy dyads demonstrated alliance convergence, some dyads became divergent in their views of the alliance as the therapy progressed. As in the previous step, EB estimates of each dyad's unique estimated alliance discrepancy early in therapy and the change in patients' and therapists' perception of their alliance across the therapy (i.e., convergence) were output for use as predictors of depression symptomatology in the final step of analyses.
Table 3. Parameter Estimates and Associated Standard Errors for the Alliance Discrepancy Growth Model.
| Coefficient | S.E. | |
|---|---|---|
| Fixed Effects | ||
| Early Alliance Discrepancy (Intercept), γ00 | 2.81*** | .11 |
| Psychotherapy Condition, γ01 | -.09 | .19 |
| Alliance Divergence/Convergence-over time (Slope), γ10 | -.27*** | .08 |
| Psychotherapy Condition, γ11 | .12 | .14 |
| Estimate | χ2 Statistic | |
| Variance Components | ||
| Early Alliance Discrepancy, τπ00 | .79*** | 1327.97 |
| Alliance Divergence/Convergence-over time, τπ11 | .16*** | 388.67 |
| Early Alliance Discrepancy, τβ00 | .31*** | 148.17 |
| Alliance Divergence—over time, τβ11 | .13*** | 96.37 |
| e | .57 | |
| Model Fit Statistics | ||
| Deviance (df) | 2704.93 (11) |
Note: Absolute dyadic discrepancy in alliance was derived from relative difference scores obtained in the first modeling step. Significance for the Level 1 residual is not tested in the HLM program. Psychotherapy condition was coded -.5 (BSP) and .5 (CBASP) so that the model estimates reflect early alliance discrepancy and convergence averaging across the treatments (i.e., when treatment condition = 0).
Alliance Discrepancy and Convergence as Predictors of Depression Outcome
Finally, we used the estimates of early alliance discrepancy/similarity and divergence/convergence as predictors in a model that tested whether they related to outcome. We modeled change in depression over time using a linear growth curve model, characterized by two parameters (intercept and slope). The time variable was rescaled from 0 to 1 so that the linear change coefficient would reflect change in depression across the entire treatment course (Bolger & Laurenceau, 2013). We then centered the time variable so that it reflected symptomatology at the end of psychotherapy (Week 12). This model was estimated twice, first using the QIDS ratings and then the HAMD depression ratings as the repeated measures. Although previous studies from this clinical trial found no significant difference between BSP and CBASP in their prediction of depression change, we included the psychotherapy condition variable in all models to accurately account for the original study design. This model was hierarchically structured with three levels to account for nesting of repeated measurements within patients as well as nesting due to multiple patients having the same therapist. Random effects were included on depression intercept and slope at both levels 2 and 3.
QIDS results
Results from the baseline model with only the time course as a predictor showed that the average QIDS depression score at the end of treatment was estimated as γ = 6.37, p < .001, and the average depression decline across treatment was significant (γ = -2.82, p < .001). There was significant dyad-level (level 2) variability around both endpoint depression intercept (γ = 12.57, p < .001) and depression slope (γ = 7.21, p < .001), supporting the addition of predictors to the model to try to explain some of this variability. We next added discrepancy in early alliance (at week 2) and alliance divergence/convergence predictors simultaneously to the next model, with results displayed in column 1 of Table 4. As in other analyses of this RCT, we found no significant effect for treatment type on either endpoint depression or depression change. Contrary to our hypotheses, discrepancy in alliance ratings early in psychotherapy predicted neither depression level at the end of in treatment nor rate of depression decline over the course of treatment. Consistent with our hypotheses, we found that divergence (lower convergence) in alliance ratings during psychotherapy was related to higher depression scores at the end of psychotherapy, as well as slower rates of change during psychotherapy. Put in terms of healthy process, convergence in therapists' and patients' alliance ratings over the course of psychotherapy related to lower depressive symptoms. Figure 2 illustrates the association of convergence with a steeper depression decline in depressive symptoms, while divergent dyads had a less steep depression decline. Adding these predictors accounted for 2.5% of the variance in depression level at week 12, and 4.1% of the variance in depression change over the course of psychotherapy.4
Table 4. Parameter Estimates and Associated Standard Errors for Predicting Level and Change in Depression from Early Alliance Discrepancy and Alliance Convergence over Time.
| QIDS-C | HAMD24 | |||
|---|---|---|---|---|
|
|
||||
| Fixed Effects | Coefficient (SE) | p | Coefficient (SE) | p |
|
|
||||
| Week 12 Depression (Intercept), γ00 | 6.37 (.25) | <.001 | 12.42 (.59) | <.001 |
| Psychotherapy Condition, γ01 | .55 (.49) | .264 | 1.78 (1.14) | .119 |
| Alliance Discrepancy/Similarity Week 2, γ02 | .51 (.33) | .122 | .61 (.67) | .362 |
| Alliance Divergence/Convergence, γ03 | 3.50 (1.43) | .015 | 2.83 (2.87) | .325 |
| Change in Depression (Slope), γ10 | -2.82 (.27) | <.001 | -5.58 (.44) | <.001 |
| Psychotherapy Condition, γ11 | .23 (.52) | .650 | 1.47 (.87) | .094 |
| Alliance Discrepancy/Similarity Week 2, γ12 | .62 (.33) | .065 | .94 (.64) | .144 |
| Alliance Divergence/Convergence, γ13 | 3.75 (1.44) | .010 | 2.32 (2.77) | .401 |
| Random Effects | Variance Component | p | Variance Component | p |
|
|
||||
| Level 1, σ2 | 5.62a | 21.14a | ||
| Level 2, Depression Intercept, τπ00 | 12.16 | <.001 | 50.33 | <.001 |
| Level 2, Depression Slope, τπ11 | 6.91 | <.001 | 25.21 | <.001 |
| Level 3, Depression Intercept, τβ00 | .69 | .088 | 5.86 | .002 |
| Level 3, Depression Slope, τβ11 | .92 | .007 | 1.03 | .153 |
| Model Deviance (df) | 10261.85 (15) | 12891.73 (15) | ||
Significance test for σ2 are not provided within the HLM program.
Note: Positive values for the Divergence/Convergence predictors mean that smaller discrepancy declines over time, or discrepancy increases over time (divergence), were associated with increased depression at Week 12, and flatter depression declines over the course of psychotherapy. Conversely, steeper declines in alliance discrepancy were associated with lower Week 12 depression, and steeper depression declines across psychotherapy.
Figure 2.
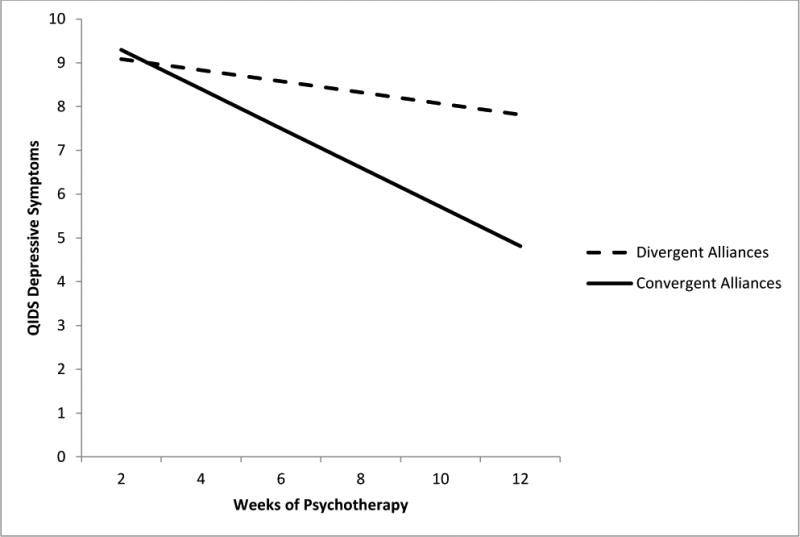
Change in depressive symptomatology as a function of alliance convergence, displayed at the 10th percentile of discrepancy change (i.e., divergent alliance patterns) and 90th percentile values of the change in alliance discrepancy over time (i.e., highly convergent alliance patterns). Therapy dyads who became more similar in their views of the working alliance showed stronger improvement in depression (as measured by the QIDS) than those who became more discrepant over time. Follow-up analyses indicated that patients with divergent alliance patterns had higher depression levels at follow-up, even when controlling for prior depression and alliance levels.
Exploratory analyses were conducted to better understand the nature of these findings and to rule out alternate explanations. Three was no significant interaction between early alliance discrepancy and convergence in predicting depression level (γ = -1.03, p =.229) or change (γ = -.21, p =.749) over the course of psychotherapy. Importantly, the alliance convergence finding remained a significant predictor of depression improvement (γ = 2.92, p =.033) even when controlling for alliance level and change in alliance. Note its prediction of endpoint depression level (rather than depression improvement), however, failed to reach statistical significance when controlling for alliance level and change in the same model (γ = 2.02, p = .149). The convergence-outcome link did not depend on whether the patient or therapist rated the alliance higher (depression level at endpoint, γ = -.33, p =.825; depression change γ = .93, p =.546). Nor did we find significant differences in either the convergence-outcome link (depression level at endpoint, γ = .02, p =.710; depression change γ = -.04, p =.592) or the discrepancy-outcome link (depression level at endpoint, γ = .02, p =.348; depression change γ = -.004, p =.877) by early alliance level. In addition, these findings were not confounded with treatment dropout (applicable to only 7.3% of this sample, n = 26). The convergence finding held even when controlling for dropout status (γ = 3.60, p =.012, QIDS depression level; γ = 3.75, p =.010, QIDS depression slope), and so could not be attributed to the notion that divergent dyads dropped out of treatment prematurely. Supplemental Table S1 and the associated paragraph in the online supplement provide further statistics from follow-up analyses of potential moderators of findings for the QIDS depression outcome.
HAMD results
We conducted an identical model with the HAMD as the depression outcome. Results from the baseline model with only the time course as a predictor showed that the average HAMD depression score at the end of treatment was estimated as γ = 12.31, p < .001, and the average depression decline across treatment was significant (γ = -5.63, p < .001). There was significant variability around both the HAMD endpoint depression intercept (γ = 57.62, p < .001) and slope (γ = 27.15, p < .001), supporting the addition of predictors to the model to try to explain some of this variability. As in the QIDS models, discrepancy in alliance ratings early did not significantly predict depression level late in treatment or rate of depression decline across treatment. In contrast to the QIDS-C models, however, there was also no significant association between alliance convergence over time and depression level or change. Results appear in Table 4, column 2. Similar follow-up analyses testing moderators listed above (e.g., alliance level as a moderator of discrepancy and convergence) were conducted with no significant findings. See Table S2 of the supplement for statistics from these exploratory models.
Consequences of Dyadic Alliance Divergence/Convergence
Finally, we conducted additional exploratory analyses to better understand the longer term consequences of alliance divergence/convergence. In the REVAMP trial, the only depression measure used at follow-up assessment was the blind observer-rated HAMD; the QIDS was not administered at this follow-up assessment. Because these follow-up data also allowed for tests of temporal process (whereas convergence and depression change were co-occurring in the primary analyses reported above), we conducted exploratory analyses to assess potential alternate explanations for our interpretation of these results. To test the alternate hypothesis that patients' symptoms were driving the changes in alliance, we included HAMD level at the end of psychotherapy as a predictor of follow-up depression. To assess the alternate hypothesis that alliance convergence is simply a proxy for higher alliance ratings, we also controlled for alliance level late in psychotherapy. We conducted these follow-up analyses using a two level HLM model which accounted for therapist nesting at level 2. Follow-up depression was the outcome, and continuous level 1 predictors (late alliance, endpoint HAMD) were grand mean centered. As in prior analyses, psychotherapy condition was included as well. Results indicated that greater alliance divergence was associated with significantly higher depression at follow-up (γ = 3.23, p = .044), even when controlling for end of psychotherapy depression and alliance levels. Statistics from the 3 month follow-up HLM model are presented in Table S3 of the online supplement.
Discussion
As predicted, we found evidence that patients and therapists became significantly more convergent in their alliance ratings as therapy progressed. This pattern suggests a therapeutic process of increased consensus between chronically depressed patients and their therapists on alliance judgments over the course of psychotherapy. We found partial support for our prediction that progressive convergence in alliance ratings over time would significantly relate to outcome over the course of treatment. Greater convergence related to lower depression levels at the end of treatment and more rapid reductions in depressive symptoms during treatment, but only when depression was measured with the QIDS (not the HAMD). However, our hypothesis was further supported when considering longer-term follow-up, as greater alliance convergence predicted lower HAMD scores at 3 months after treatment. Counter to our hypotheses, patient-therapist alliance discrepancy/similarity early in therapy did not predict outcome for either depression measure.
This study's primary contribution is the finding that patient-therapist alliance ratings converged over the course of psychotherapy; that is, the discrepancy between therapists' and patients' alliance ratings decreased (on average) as the psychotherapy progressed. This finding is consistent with Bordin's (1979) conceptualization of the formation of the alliance, which posited that a good working alliance is one in which patients and therapists build toward consensus about the goals and tasks in the psychotherapy, while negotiating a shared affective bond. The statistically significant decrease in discrepancy in patient-therapist alliance ratings across psychotherapy may be an indicator of this alliance development over time.
We found mixed support for our hypothesis that the process of convergence in alliance ratings over time was associated with better psychotherapy outcome as indicated by depressive symptoms at the end of treatment and change in depressive symptoms over time. As noted, convergence was associated with steeper declines in depression over the course of psychotherapy and lower endpoint depression only as measured by the QIDS, not the HAMD.
It is possible that the differential findings of QIDS versus HAMD in the primary analyses were due to the measures' different raters. Pharmacotherapists rated the QIDS, whereas independent assessors blind to treatment condition rated the HAMD. Pharmacotherapists may have been more sensitive to nuances in patient symptomatology, and thus more reliable raters of their symptom change. Conversely, it is possible that pharmacotherapists were biased to see patients as improving, thus introducing additional error into the QIDS measure that resulted in a stronger association than was truly present. Differences in the measures themselves may also have accounted for the divergent findings. Some research that has shown that the Inventory of Depressive Symptomatology (IDS), the longer version of the QIDS, is more sensitive to changes in and severity of depressive symptomatology than the HAMD (Helmreich et al., 2011). The magnitude of depression change in the two measures in this study, however, was similar, thus countering this possibility. Another study found that HAMD responses tended to be more restricted than intended (Rush et al., 2006). Still, even with psychometric limitations, the HAMD is considered a gold-standard measure of clinician-rated depressive symptomatology (Bagby, Ryder, Schuller, & Marshall, 2004), especially when raters are blind to treatment condition to combat bias and increase internal validity. Thus, discussion of alliance convergence findings should be cautiously considered, and replication of results with blind observer-based measures of depression change is required to solidify the clinical implications.
However, countering the possibility that the QIDS findings were only an artifact of rater bias is that we did find associations with the 3-month follow-up HAMD scores measured by blind raters. Our follow-up data revealed that patients with convergent alliance patterns had lower depression 3 months after treatment than those with divergent alliance patterns. Considered together with findings from the primary analyses showing significant effects on the QIDS but not the HAMD, we posit that alliance convergence may be an important theoretical construct to consider, but may have a modest clinical impact (at least as assessed through dyadic modeling of the two separate reports). The small effect size for convergence would explain why our analyses showed a similar direction of results across both depression measures and at both posttreatment and follow-up, but non-significance for one measure in the primary analyses. Note that alliance convergence did maintain its significant prediction of depression change above and beyond early alliance level and change, but the magnitude of its effect did diminish when alliance level was included in the model. Thus, alliance convergence appears to have both overlapping and distinct qualities with early alliance level. Future studies should assess alliance convergence through multiple modalities, such as observer coding of dyadic process or more frequent measurement of the alliance, to explore further how it differs from alliance level.
If future studies find a convergence-outcome link, the alliance convergence findings may have implications for clinical practice. Although the lack of association between early dyadic discrepancy/similarity and outcome contradicted our hypothesis, it may provide meaningful information for alliance research in general and for the treatment of chronically depressed individuals in particular. Most prominently, the results suggest that no matter how discrepant patient-therapist alliance perspectives are at the beginning of psychotherapy, moving toward dyadic consensus on the alliance may benefit ultimate treatment outcome. In other words, when treating chronically depressed patients, early alliance mismatch may not doom subsequent relational attunement or outcome. In fact, this might reflect a natural therapeutic relationship progression in psychotherapy. Whether true or perceived disagreement existed early, our convergence finding may suggest that a positive therapy outcome can be achieved provided that over the course of treatment the patient and therapist come to view the goals and tasks of the therapy more similarly. The results tentatively and indirectly support the widely accepted notion that the alliance represents a dynamic negotiation between two people and their respective interpersonal needs and experiences (Castonguay, Constantino, Boswell, & Kraus, 2010; Safran & Muran, 2000). More research focused directly on need negotiation is needed to substantiate further this notion of dynamic alliance development.
To address early misattunement, the therapist (and patient) may have to maneuver to foster convergence over time. Convergence could plausibly reflect active efforts to foster shared understanding of the alliance, or to repair ruptures stemming from initial misalignment or from direct relational missteps during any phase of treatment. Although we did not assess specific therapist behaviors in this regard, it is possible that the therapists, on average, successfully negotiated alliance ruptures. The dominant pattern of alliance convergence was one in which therapists' alliance ratings changed more than patients' ratings as psychotherapy progressed (see Figure 1, panel A for one example). This pattern may indicate therapists' (perceived) successful efforts to improve transparency or repair ruptures during the psychotherapy process. Even without knowing specific therapist behaviors, the convergence results suggest that therapists, in any approach that they employ, may want to engage in strategies to enhance agreement on facets of the alliance throughout the treatment process (for reviews of such strategies, see Crits-Christoph, Crits-Christoph, & Connolly Gibbons, 2010; Constantino, Castonguay, Zack, & DeGeorge, 2010; Hilsenroth et al., 2013; Muran, Safran, and Eubanks-Carter, 2010). Acknowledging that such claims are speculative without more detailed information about therapists' intervention strategies, this notion would be consistent with CBASP and BSP, as both treatments emphasize relational attunement in the therapy process.
This study also has implications for how psychotherapy researchers conceptualize and measure the therapeutic alliance. Our study supports the contention that using both patient and therapist data can help researchers better model and understand the dynamic interplay that occurs between patients and therapists during psychotherapy. Our analyses would not have been possible with only one rater's perspective of the alliance, or if the alliance had only been measured at one time point. Because of the repeated measures and dyadic data available in the REVAMP trial, we were able to model the process of psychotherapy with greater refinement than simple pre- and post-treatment assessments would have allowed. However, even in the present analyses, there was evidence that more intensive measurement may have yielded more refined results. Specifically, the alliance convergence change process may be curvilinear; examination of the mean trends showed that the convergence process is likely steeper early in psychotherapy. Unfortunately, with only three alliance measurements, we could not test whether a curvilinear trajectory better explained the nature of the alliance convergence process than the linear change modeled here. In future research, more frequently collected alliance data from multiple perspectives would have considerable value.
Several additional limitations characterize the study. First, the current analyses could not measure the effect of pharmacotherapy (including alliance with pharmacotherapist) on outcome; thus, a potential confound existed. Second, our sample was restricted to chronically depressed patients, and we do not know the extent to which findings would generalize to non-chronically depressed or other patient groups (including those with a different non-diagnostic demographic composition). Third, the convergence predictor represents a change process in the dyadic alliance that co-occurred with depression symptom improvement, so symptom improvement may have been responsible for alliance convergence. To address this alternate hypothesis, we did perform analyses of follow-up data, finding that convergence was associated with significantly lower depression at follow-up, even when controlling for depressive symptomatology at the endpoint of the 12 weeks of psychotherapy. Thus, at least for the subsample that had follow-up data, we do have some evidence that alliance convergence provided benefits over and above symptom improvement.
Fourth, we only had a small number of therapy dyads (67 dyads) in which therapists rated the early alliance higher than patients. We did test whether alliance discrepancy or convergence was differentially associated with outcome for these dyads, but found no significant results. These non-significant findings, however, may have been due to the relatively small number of dyads in which the therapist rated the alliance higher. Because of the asymmetry in the therapeutic relationship, it is likely that the relative difference between the two reports is clinically meaningful: future studies should consider the implications of therapists rating the alliance higher than the patients, and the possibility that this type of bias works differently than that of dyads in which the patient sees the alliance as being higher than does the therapist.
Fifth, the small effect size observed for alliance convergence in the present study makes it difficult to determine the clinical import of this finding. It is possible that the small effect of dyadic convergence is due to the unexpected lack of augmentation found in the REVAMP psychotherapy arms, as compared with the medication-only arm. Other studies finding larger psychotherapy effects may find larger effect sizes for alliance convergence. Alternately, it may be that we are tapping into the theorized process of dyadic attunement that is part of a healthy psychotherapy relationship, but another form of measurement is needed to better capture the clinical importance of this process. For example, observational coding schemes of dyadic-level processes and changes during psychotherapy may more directly measure of the alliance convergence process.
An additional limitation is the use of multiple steps to create the dyadic measures of alliance discrepancy and attunement. While empirical Bayes estimates carry some benefits over raw calulations from observed data (e.g. Hedeker, 2004), using them as inputs in a sequence of models is not optimal. Future studies could advance this methodological problem by providing simultaneous creation of alliance discrepancy and convergence and a test of their association with outcome if possible. A final study limitation was that we had alliance measurement only from Week 2 of the early weeks of psychotherapy. Research suggests that the dependability of alliance-outcome assessments is greater when aggregating at least four successive alliance assessments (Crits-Christoph, Connolly Gibbons, Gallop, Hamilton, & Rign-Kurtz, 2011). Thus, future research should examine alliance convergence over multiple successive sessions at each phase of therapy to understand more fully the relation between convergence and outcome.
To conclude, our findings preliminarily suggest that convergence in therapists' and patients' ratings of the alliance may be associated with better psychotherapy outcome, and that divergent patterns may be a marker of poorer outcome in chronic depression treatment. The findings indicate that future research should examine the alliance from a dyadic perspective, as increasing convergence in alliance perspectives over time may hold promise for understanding relational mechanisms of therapeutic change.
Supplementary Material
Acknowledgments
This research was supported by the National Institute of Mental Health U01 MH61504 awarded to James H. Kocsis, Department of Psychiatry, Weill Medical College of Cornell University.
Footnotes
Ten of the 38 patients with missing data dropped out between phases 1 and 2 of treatment. The remaining 28 completed some portion of phase 2, but were missing alliance data due to study error. The only significant difference between the study subsample and the 38 cases excluded because they had no alliance ratings was that the patients in the subsample were older, Mdiff = 5.98, t391 = 3.00, p = .003. Subsample patients did not significantly differ from excluded patients in race/ethnicity, χ2(1,394)= .27, p = .605, gender distribution, χ2(1,394)= 1.34, p = .248, or depression levels at the beginning of phase 2 (based on either the HAMD, t393 = -.66, p = .508, or QIDS, t393 = -1.41, p = .159).
Of course, patients did inherently develop alliances with their pharmacotherapists, meaning that patients in the psychotherapy conditions were negotiating multiple professional relationships. Unfortunately, the influence of the pharmacotherapist-patient alliance was unaccounted for in study design, which represents a methodological limitation.
Prior to fitting the HLM model, the data required transformation. At each measurement occasion, the vast majority of alliances had patients with higher alliance scores than therapist scores. Given the coding of the difference score indicator in the first step (patients .5, therapists -.5), this resulted in a positive relative score when patient scores were higher (n = 290), and a negative score when therapist scores were higher (n = 67). Because the primary study aims were simply to test for similarity in alliance ratings and to model convergence over time, we elected to take the absolute value of the relative differences estimated in the first step of analyses. The EB estimates of the relative differences were transformed by first taking the absolute value, which resulted in a positively skewed distribution. We then applied a square root transformation to correct the skew (Tukey, 1977). These transformations were also applied to the middle and late alliance measures. While taking an absolute discrepancy obscures potentially useful information about who saw the alliance as worse or better at a given time point, prior studies have found that the magnitude of the absolute discrepancy predicted outcome, and found that there was no difference between dyads with a therapist versus a patient rating the alliance higher (Marmarosh & Kivlighan, 2012). In addition, we performed follow-up, exploratory analyses in our own data to test whether the convergence process was differentially associated with outcome depending on whether the therapy dyad had therapists who rated the alliance higher versus dyads in which patients rated the alliance higher. We found no significant difference in the convergence-outcome association depending on who rated the alliance higher.
These were calculated as pseudo-R2 difference in unexplained variance from the baseline model with only the treatment condition as a predictor to the model with discrepancy and divergence/convergence predictors.
Versions of this paper were presented at the International meeting of the Society for Psychotherapy Research in 2011 and the North American Chapter of the Society for Psychotherapy Research in 2012. In addition, this work was reported in the first author's dissertation from the Clinical Psychology program at University of Massachusetts Amherst.
Contributor Information
Holly B. Laws, Yale University School of Medicine, Department of Psychiatry
Michael J. Constantino, Department of Psychological and Brain Sciences, University of Massachusetts Amherst
Aline G. Sayer, Department of Psychological and Brain Sciences, University of Massachusetts Amherst
Daniel N. Klein, Department of Psychology, Stony Brook University
James H. Kocsis, Department of Psychiatry, Weill Medical College of Cornell University
Rachel Manber, Stanford University Department of Psychiatry and Behavioral Sciences.
John C. Markowitz, New York State Psychiatric Institute, Columbia University College of Physicians and Surgeons
Barbara O. Rothbaum, Department of Psychiatry, Emory University School of Medicine
Dana Steidtmann, Department of Family Medicine, University of Colorado School of Medicine.
Michael E. Thase, Perlman School of Medicine, University of Pennsylvania
Bruce A. Arnow, Stanford University Department of Psychiatry and Behavioral Sciences
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Allison PD. Missing Data. In: Millsap RE, Maydeu-Olivares A, editors. The SAGE Handbook of Quantitative Methods in Psychology. Thousand Oaks, CA: Sage Publications Inc; 2009. pp. 72–89. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Arnow BA, Steidtmann D, Blasey C, Manber R, Constantino MJ, Klein DN, Kocsis JH. The relationship between the therapeutic alliance and treatment outcome in two distinct psychotherapies for chronic depression. Journal of Consulting and Clinical Psychology. 2013;81:627–638. doi: 10.1037/a0031530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atzil-Slonim D, Bar-Kalifa E, Rafaeli E, Lutz W, Rubel J, Schiefele AK, Peri T. Therapeutic bond judgments: Congruence and incongruence. Journal of Consulting and Clinical Psychology. 2015;83(4):773–784. doi: 10.1037/ccp0000015. [DOI] [PubMed] [Google Scholar]
- Bagby R, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: Has the gold standard become a lead weight? The American Journal of Psychiatry. 2004;161:2163–2177. doi: 10.1176/appi.ajp.161.12.2163. [DOI] [PubMed] [Google Scholar]
- Baldwin SA, Wampold BE, Imel ZE. Untangling the alliance outcome correlation: Exploring the relative importance of therapist and patient variability in the alliance. Journal of Consulting and Clinical Psychology. 2007;75:842–852. doi: 10.1037/0022-006X.75.6.842. [DOI] [PubMed] [Google Scholar]
- Bolger N, Laurenceau JP. Intensive longitudinal methods: An introduction to diary and experience sampling research. New York, NY: Guilford Press; 2013. [Google Scholar]
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy. 1979;16:252–260. doi: 10.1037/h0085885. [DOI] [Google Scholar]
- Cano A, Johansen AB, Franz A. Multilevel analysis of couple congruence on pain, interference, and disability. Pain. 2005;118:369–379. doi: 10.1016/j.pain.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castonguay LG, Constantino MJ, Boswell JF, Kraus DR. The therapeutic alliance: Research and theory. In: Horowitz LM, Strack S, editors. Handbook of interpersonal psychology: Theory, research, assessment, and therapeutic interventions. Hoboken, NJ: John Wiley and Sons, Inc; 2010. pp. 509–518. [Google Scholar]
- Constantino MJ, Castonguay LG, Zack S, DeGeorge J. Engagement in psychotherapy: Factors contributing to the facilitation, demise, and restoration of the therapeutic alliance. In: Castro-Blanco D, Carver MS, editors. Elusive alliance: Treatment engagement strategies with high-risk adolescents. Washington, DC: American Psychological Association; 2010. pp. 199–209. [DOI] [Google Scholar]
- Constantino MJ, Manber R, DeGeorge J, McBride C, Ravitz P, Zuroff D, Arnow BA. Interpersonal styles of chronically depressed outpatients: Profiles and therapeutic change. Psychotherapy. 2008;45:491–506. doi: 10.1037/a0014335. [DOI] [PubMed] [Google Scholar]
- Constantino MJ, Laws HB, Arnow BA, Klein DN, Rothbaum BO, Manber R. The relation between changes in patients' interpersonal impact messages and outcome in treatment for chronic depression. Journal of Consulting and Clinical Psychology. 2012;80:354–364. doi: 10.1037/a0028351. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Connolly Gibbons MB, Gallop R, Hamilton J, Ring-Kurtz S. The dependability of alliance-outcome correlation is larger than you might think. Journal of Consulting and Clinical Psychology. 2011;79:267–278. doi: 10.1037/a0023668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crits-Christoph P, Crits-Christoph K, Connolly Gibbons MB. Training in alliance-fostering techniques. In: Muran J, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York, NY: Guilford Press; 2010. pp. 304–319. [Google Scholar]
- DeRubeis RJ, Brotman MA, Gibbons CJ. A Conceptual and Methodological Analysis of the Nonspecifics Argument. Clinical Psychology: Science and Practice. 2005;12:174–183. doi: 10.1093/clipsy/bpi022. [DOI] [Google Scholar]
- DeRubeis RJ, Feeley M. Determinants of change in cognitive therapy for depression. Cognitive Therapy and Research. 1990;14:469–482. doi: 10.1007/BF01172968. [DOI] [Google Scholar]
- Dyrenforth PS, Kashy DA, Donnellan M, Lucas RE. Predicting relationship and life satisfaction from personality in nationally representative samples from three countries: The relative importance of actor, partner, and similarity effects. Journal of Personality and Social Psychology. 2010;99:690–702. doi: 10.1037/a0020385. [DOI] [PubMed] [Google Scholar]
- Elvins R, Green J. The conceptualization and measurement of therapeutic alliance: An empirical review. Clinical Psychology Review. 2008;28:1167–1187. doi: 10.1016/j.cpr.2008.04.002. [DOI] [PubMed] [Google Scholar]
- Eubanks-Carter C, Muran J, Safran JD. Alliance ruptures and resolution. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York, NY: Guilford Press; 2010. pp. 74–94. [Google Scholar]
- Falkenström F, Granström F, Holmqvist R. Working alliance predicts psychotherapy outcome even while controlling for prior symptom improvement. Psychotherapy Research. 2014;24:146–159. doi: 10.1080/10503307.2013.847985. [DOI] [PubMed] [Google Scholar]
- Geerts E, Bouhuys N, Van den Hoofdakker RH. Nonverbal attunement between depressed patients and an interviewer predicts subsequent improvement. Journal of Affective Disorders. 1996;40(96):15–21. 00037–7. doi: 10.1016/0165-0327. [DOI] [PubMed] [Google Scholar]
- Hamilton M. Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- Hedeker D. An introduction to growth modeling. In: Kaplan D, editor. Quantitative Methodology for the Social Sciences. Thousand Oaks CA: Sage Publications; 2004. [Google Scholar]
- Helmreich I, Wagner S, Mergl R, Allgaier A, Hautzinger M, Henkel V, Tadić A. The Inventory of Depressive Symptomatology (IDS-C28) is more sensitive to changes in depressive symptomatology than the Hamilton Depression Rating Scale (HAMD17) in patients with mild major, minor or subsyndromal depression. European Archives of Psychiatry and Clinical Neuroscience. 2011;261:357–367. doi: 10.1007/s00406-010-0175-1. [DOI] [PubMed] [Google Scholar]
- Hersoug A, Høglend P, Monsen JT, Havik OE. Quality of working alliance in psychotherapy: Therapist variables and patient/therapist similarity as predictors. Journal of Psychotherapy Practice & Research. 2001;10:205–216. [PMC free article] [PubMed] [Google Scholar]
- Hilsenroth MJ, Cromer TD, Ackerman SJ. How to make practical use of therapeutic alliance research in your clinical work. In: Levy RA, Ablon J, Kächele H, editors. Psychodynamic psychotherapy research: Evidence-based practice and practice-based evidence. Totowa, NJ: Humana Press; 2012. pp. 361–380. [DOI] [Google Scholar]
- Horvath AO, Bedi RP. The alliance. In: Norcross JC, Norcross JC, editors. Psychotherapy relationships that work: Therapist contributions and responsiveness to patients. New York, NY: Oxford University Press; 2002. pp. 37–69. [Google Scholar]
- Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48:9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. doi: 10.1037/0022-0167.36.2.223. [DOI] [Google Scholar]
- Joiner TE. Depression in its interpersonal context. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York, NY: Guilford Press; 2002. pp. 295–313. [Google Scholar]
- Joiner T, Coyne JC, Blalock J. On the interpersonal nature of depression: Overview and synthesis. In: Joiner T, Coyne J, editors. The interactional nature of depression: Advances in interpersonal approaches. Washington, DC: American Psychological Association; 1999. pp. 3–19. [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York, NY: Guilford Press; 2006. [Google Scholar]
- Kivlighan D. Where is the relationship in research on the alliance? Two methods for analyzing dyadic data. Journal of Counseling Psychology. 2007;54:423–433. doi: 10.1037/0022-0167.54.4.423. [DOI] [Google Scholar]
- Klein DN, Schwartz JE, Santiago, Vivian D, Vocisano C, Castonguay LG, Keller MB. Therapeutic alliance in depression treatment: Controlling for prior change and patient characteristics. Journal of Consulting and Clinical Psychology. 2003;71:997–1006. doi: 10.1037/0022-006X.71.6.997. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Gelenberg AJ, Rothbaum BO, Klein DN, Trivedi MH, Manber R, Thase ME. Cognitive Behavioral Analysis System of Psychotherapy and brief supportive psychotherapy augmentation of antidepressant nonresponse in chronic depression. Archives of General Psychiatry. 2009;66:1178–1188. doi: 10.1001/archgenpsychiatry.2009.144. (for the REVAMP Trial) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer U, de Roten Y, Beretta V, Michel L, Despland J. Patient's and therapist's views of early alliance building in dynamic psychotherapy: Patterns and relation to outcome. Journal of Counseling Psychology. 2008;55:89–95. doi: 10.1037/0022-0167.55.1.89. [DOI] [Google Scholar]
- Krasikova DV, LeBreton JM. Just the two of us: Misalignment of theory and methods in examining dyadic phenomena. Journal of Applied Psychology. 2012;97:739–757. doi: 10.1037/a0027962. [DOI] [PubMed] [Google Scholar]
- Laurenceau J, Hayes AM, Feldman GC. Some methodological and statistical issues in the study of change processes in psychotherapy. Clinical Psychology Review. 2007;27:682–695. doi: 10.1016/j.cpr.2007.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons KS, Sayer AG. Using multilevel modeling in caregiving research. Aging & Mental Health. 2005;9:189–195. doi: 10.1080/13607860500089831. [DOI] [PubMed] [Google Scholar]
- Manne SL, Kashy DA, Rubin S, Hernandez E, Bergman C. Therapist and patient perceptions of alliance and progress in psychological therapy for women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology. 2012;80:800–810. doi: 10.1037/a0029158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus DK, Kashy DA, Baldwin SA. Studying psychotherapy using the one- with-many design: The therapeutic alliance as an exemplar. Journal of Counseling Psychology. 2009;56:537–548. doi: 10.1037/a0017291. [DOI] [Google Scholar]
- Marcus DK, Kashy DA, Wintersteen MB, Diamond GS. The therapeutic alliance in adolescent substance abuse treatment: A one-with-many analysis. Journal of Counseling Psychology. 2011;58:449–455. doi: 10.1037/a0023196. [DOI] [PubMed] [Google Scholar]
- Markin RD, Kivlighan Dm, Jr, Gelso CJ, Hummel AM, Spiegel EB. Clients' and therapists' real relationship and session quality in brief therapy: An actor partner interdependence analysis. Psychotherapy. 2014 doi: 10.1037/a0036069. Advanced online publication. [DOI] [PubMed] [Google Scholar]
- Markowitz JC. Interpersonal psychotherapy for dysthymic disorder. Washington, DC: American Psychiatric Press; 1998. [Google Scholar]
- Markowitz JC, Manber R, Rosen P. Therapists' responses to training in brief supportive psychotherapy. American Journal of Psychotherapy. 2008;62:67–81. doi: 10.1176/appi.psychotherapy.2008.62.1.67. [DOI] [PubMed] [Google Scholar]
- Marmarosh CL, Kivlighan DR. Relationships among client and counselor agreement about the working alliance, session evaluations, and change in client symptoms using response surface analysis. Journal of Counseling Psychology. 2012;59:352–367. doi: 10.1037/a0028907. [DOI] [PubMed] [Google Scholar]
- McCullough JP., Jr . Treatment for chronic depression: Cognitive-Behavioral Analysis System of Psychotherapy. New York, NY: Guilford; 2000. [DOI] [PubMed] [Google Scholar]
- Muran JC, Barber JP. The therapeutic alliance: An evidence-based guide to practice. New York, NY: Guilford Press; 2010. [Google Scholar]
- Muran JC, Safran JD, Eubanks-Carter C. Developing therapist abilities to negotiate alliance ruptures. In: Muran JC, Barber JP, editors. The therapeutic alliance: An evidence-based guide to practice. New York, NY: Guilford Press; 2010. pp. 320–340. [Google Scholar]
- Raudenbush SW, Brennan RT, Barnett RC. A multivariate hierarchical model for studying psychological change within married couples. Journal of Family Psychology. 1995;9:161–174. doi: 10.1037/0893-3200.9.2.161. [DOI] [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM 7 for Windows [Computer software] Lincolnwood, IL: Scientific Software International, Inc; 2011. [Google Scholar]
- Rush A, Bernstein IH, Trivedi MH, Carmody TJ, Wisniewski S, Mundt JC, Fava M. An evaluation of the quick inventory of depressive symptomatology and the Hamilton rating scale for depression: A sequenced treatment alternatives to relieve depression trial report. Biological Psychiatry. 2006;59:493–501. doi: 10.1016/j.biopsych.2005.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush A, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Keller MB. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry. 2003;54(02):573–583. 01866–8. doi: 10.1016/S0006-3223. [DOI] [PubMed] [Google Scholar]
- Safran JD, Muran JC. Negotiating the therapeutic alliance: A relational treatment guide. New York: Guilford; 2000. [Google Scholar]
- Stiles WB, Agnew-Davies R, Hardy GE, Barkham M, Shapiro DA. Relations of the alliance with psychotherapy outcome: Findings in the second Sheffield Psychotherapy Project. Journal of Consulting and Clinical Psychology. 1998;66:791–802. doi: 10.1037/0022-006X.66.5.791. [DOI] [PubMed] [Google Scholar]
- Strunk DR, Brotman MA, DeRubeis RJ. The process of change in cognitive therapy for depression: Predictors of early inter-session symptom gains. Behaviour Research and Therapy. 2010;48:599–606. doi: 10.1016/j.brat.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swift J, Callahan J. Early psychotherapy processes: An examination of client and trainee clinician perspective convergence. Clinical Psychology & Psychotherapy. 2009;16:228–236. doi: 10.1002/cpp.617. [DOI] [PubMed] [Google Scholar]
- Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:207–210. doi: 10.1037/1040-3590.1.3.207. [DOI] [Google Scholar]
- Tryon G, Blackwell S, Hammel E. A meta-analytic examination of client-therapist perspectives of the working alliance. Psychotherapy Research. 2007;17:629–642. doi: 10.1080/10503300701320611. [DOI] [Google Scholar]
- Tukey JW. Exploratory data analysis. Reading, MA: Addison-Wesley Publishing Company; 1977. [Google Scholar]
- Wampold BE, Brown GSJ. Estimating variability in outcomes attributable to therapists: a naturalistic study of outcomes in managed care. Journal of Consulting and Clinical Psychology. 2005;73(5):914. doi: 10.1037/0022-006X.73.5.914. [DOI] [PubMed] [Google Scholar]
- Webb CA, DeRubeis RJ, Amsterdam JD, Shelton RC, Hollon SD, Dimidjian S. Two aspects of the therapeutic alliance: Differential relations with depressive symptom change. Journal of Consulting and Clinical Psychology. 2011;79:279–283. doi: 10.1037/a0023252. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


