Introduction
In about 40–80% of children with ADHD, the disorder is chronic and continues into adolescence (Barkley, 2006; Barkley, DuPaul, & McMurray, 1990; Brown & Borden, 1986; Hill & Schoener, 1996; Wender, 1995; Wilens, Biederman, & Spencer, 2002; Wilson & Marcotte, 1996). Despite being highly informative regarding course of ADHD, early longitudinal studies of ADHD into adulthood,( including the Milwaukee Study, the New York Study, the Swedish study, and the Montreal Study) report wide ranges of rates of adult ADHD, likely related to methodological challenges. (Barkley, Fischer, et al., 2002; Mannuzza, Klein, Bessler, Malloy, & LaPadula, 1993; Mannuzza, Klein, Bessler, Malloy, & LaPadula, 1998; Rasmussen & Gillberg, 2000; Weiss, Hechtman, Milroy, & Perlman, 1985). This wide range has been attributed to attrition of participants, use of different informants, use of varied diagnostic criteria, and a variation in methods of assessment and ascertainment (e.g. asking about persistence of symptoms vs. current diagnostic status, use of self-ratings vs. observations) (Faraone et al., 2006; Mannuzza, Klein, & Moulton, 2003). Most recent longitudinal studies of ADHD into adulthood suggest symptoms persist in approximately 66% of cases (Uchida, Spencer, Faraone & Biederman, 2015; Karam, Breda, Picon, Rovaris, Victor, Salgado, et al.,2015). ADHD continues to be described as a lifespan disorder in a majority of studies (Barkley, 2006; Halperin & Healey, 2011; Spencer, Biederman, & Mick, 2007; Turgay et al., 2012), though a recent, unreplicated longitudinal investigation suggests that childhood and adulthood ADHD may be different disorders with different etiologies (Moffitt, Houts, Asherson, Belsky, Corcoran, Hammerle, et al., 2015).
A number of longitudinal investigations about childhood ADHD have informed persistence, but not without limitations. Empirical studies have underscored the importance of comorbid and early childhood conduct problems as a significant predictor of persistence of ADHD through adolescence. (Gittelman, Mannuzza, Shenker, & Bonagura, 1985; Hart, Lahey, Loeber, Applegate, & Frick, 1995; Lahey, McBurnett, & Loeber, 2000; Loney, Kramer, & Milich, 1981; Taylor, Sandberg, Thorley, & Giles, 1991). In addition to psychiatric comorbidity, Rutter’s adversity indicators (such as family size and conflict, paternal criminality, social status and maternal psychopathology) have been suggested to contribute to ADHD persistence into adolescence (Biederman et al., 1992; Biederman et al., 1995). An 11-year follow-up study also suggested that persistence was related not only to comorbidity of conduct, mood, and anxiety disorders, but also to ADHD impairment at baseline and exposure to maternal psychopathology; however, the study combined adolescent and adult outcomes (participants were 15–31yo at follow-up) making it difficult to disentangle outcomes specific to adulthood (Biederman, Petty, Clarke, Lomedico, & Faraone, 2011). Another study combining adolescent and adult outcomes of ADHD suggested IQ and socioeconomic status acted as moderators of ADHD persistence (Cheung et al., 2015). In addition to combining outcomes of adolescence and adulthood, longitudinal investigations of ADHD into adulthood include use of referred populations, limiting generalizability to less severe populations (Biederman, Petty, Evans, Small, & Faraone, 2010). Furthermore, many past samples have focused exclusively on males, and only more recently included a focus on females (Biederman, Petty, Monuteaux, et al., 2010; Hinshaw et al., 2012; Monuteaux, Mick, Faraone, & Biederman, 2010).
What remains under investigated is which factors characterize individuals with ADHD who will remit or resolve with development versus experience a chronic and persistent course into adulthood (Karam et al, 2015; Lara et al., 2009; Nigg, Butler, Huang-Pollock, & Henderson, 2002). A number of longitudinal studies of ADHD have tracked outcomes over 10 years, but there has been less focus on temperament and other features of participants that might contribute to persistent course (Barkley, Murphy, Dupaul, & Bush, 2002; Mannuzza et al., 1993; Mannuzza et al., 1998; Mannuzza et al., 2003; Pingault et al., 2011; Rasmussen & Gillberg, 2000; Weiss et al., 1985). This is important to elucidate because personality factors including low agreeableness and high neuroticism have been associated with persistent ADHD (Miller, Miller, Newcorn, & Halperin, 2008). Studies distinguishing key factors that characterize persistence versus remission of ADHD into adulthood are still needed (Barkley, Murphy, & Fischer, 2008; Halperin, Trampush, Miller, Marks, & Newcorn, 2008). The present study benefits from low attrition of participants with ADHD over a 10-year course into adulthood. Understanding how to distinguish these groups is important to determine who are in need of early and ongoing intervention versus those more likely to have symptoms that resolve with development.
The current study capitalized on a large 10 -year longitudinal dataset that tracked ADHD severity in participants with ADHD alone and in those with a Bipolar phenotype with comorbid ADHD (as well as healthy controls) from childhood into adulthood. The aim was to investigate trajectories of ADHD severity across development and investigate factors that characterized the variation in the longitudinal course of ADHD into adulthood using growth mixture modeling, while carefully controlling for bipolar comorbidity. Personality factors and Substance Use Disorders (SUD) were included given their established relationship to ADHD (Miller et al., 2008; Molina et al., 2009; Wilens & Upadhyaya, 2007).
Methods
Participants
N=268 participants ages 7–16 at baseline were comprehensively assessed using the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) as part of the longitudinal Phenomenology and Course of Pediatric BP-I study (Geller, PI MH-53063). Inclusion criteria for all participants at baseline were 7–16 years of age, males and females, and good physical health. Exclusion criteria were IQ<70, epilepsy or other major medical or neurological disorders, pervasive developmental disorders, schizophrenia, baseline substance dependency, and pregnancy. Participants who developed SUD or became pregnant after baseline were retained in the study. Additional details of and rationale for study inclusion/exclusion criteria have been previously reported (Geller, Tillman, Craney, & Bolhofner, 2004). Participants were comprehensively assessed (see measures below) every 2 years for a 10 or 12-year period, as detailed in Table 1. The study ended mid-way through data collection at the 12-year wave.
Table 1.
Number of Subjects Assessed at Each Wave by Baseline Diagnostic Group
| Assessment | ADHD N | Bipolar N | Healthy N |
|---|---|---|---|
| Baseline | 81 | 93 | 94 |
| 2-Year | 80 | 89 | 94 |
| 4-Year | 80 | 86 | 94 |
| 6-Year | 78 | 86 | 94 |
| 8-Year | 76 | 86 | 93 |
| 10-Year | 75 | 84 | 92 |
ADHD participants, like BP-I participants, were consecutively ascertained from outpatient pediatric and psychiatric clinics. Screenings for exclusion criteria for all new consecutive cases were conducted by non-blind research nurses who were different than the blinded nurses who conducted in-laboratory psychiatric assessment once telephone screenings occurred. Healthy control participants were obtained through a random survey that matched them to BP-I participants by age, gender, socioeconomic status (SES), ethnicity, and zip code. The Human Studies Committee at Washington University School of Medicine in St. Louis approved the study.
There were N=81 participants in the ADHD group at baseline. These participants met DSM-IV criteria for ADHD (with hyperactivity, i.e., hyperactive/impulsive subtype [H] or combined type [C], not inattentive type [I]) at baseline without mood comorbidity and were clinically impaired, as evidenced by a CGAS score of ≤60. ADHD participants were required to have onset of ADHD symptoms prior to age 7 and duration greater than or equal to 6 months. ADHD-H and ADHD-C, but not ADHD-I, were included as a psychiatric comparison group (given focused study goals). ADHD-I was an exclusion for the ADHD group at baseline, and was not an exclusion for the BP-I group at baseline; however, there was only n=1 BP-I subjects with ADHD-I at baseline. Children in the ADHD group could not have BP-I or MDD (based on original study aims), but could have Conduct Disorder (CD) and/or Oppositional Defiant Disorder (ODD), given their common comorbidity with ADHD in children. ADHD participants could have BP-I and/or MDD at follow-up.
There were N=93 participants in the BP-I group at baseline. Child BP-I participants in this study were required to have elated mood and/or grandiosity as one of the mania criteria. Because high rates of ADHD comorbidity have been observed in child BP-I disorder, an ADHD diagnosis was not exclusionary in the BP-I group. These participants had a Children’s Global Assessment Scale (CGAS) (Bird, Canino, Rubiostipec, & Ribera, 1987; Shaffer et al., 1983) score of ≤60, signifying definite clinical impairment.
There were N=94 healthy control participants at baseline. Healthy control subjects were required to not have BP-I, MDD, or ADHD at baseline. It was found that no healthy control subjects had any Axis I disorders at baseline.
Measures
Diagnostic Assessment
The WASH-U-KSADS (Geller, William, Zimerman, & Frazier, 1996) is a semi-structured interview that was administered by experienced research clinicians to mothers about their children and to children about themselves. It was developed from the KSADS (Puig-Antich & Ryan, 1986) by adding onset and offset of lifetime and current symptoms for DSM-IV diagnoses. The WASH-U-KSADS has established validity (Geller, Warner, Williams, & Zimerman, 1998; Geller et al., 2001). To score the WASH-U-KSADS, child and parent responses were combined by using the most severe rating, in accordance with the methods described by Bird, Gould, and Staghezza (1992). Of note, the correlation between combined parent and child report and parent only report of number of baseline ADHD symptoms was 0.97. This is consistent with children under-reporting ADHD symptoms. Combined parent and child report were therefore not separated in the analyses. Teacher ratings were not addressed in the current study as they were inconsistently available. All research materials, including school reports and separate videotapes of mothers and children, were reviewed in consensus conference with research nurses and a senior clinician. Raters were blind to group status at baseline assessment. Clinicians were trained to inter-rater reliability (kappa = 0.82–1.00) and recalibrated yearly (Geller et al., 2001).
Personality: Temperament and Character
The Junior Temperament and Character Inventory (JTCI) measures four temperament and four character traits of children. Temperament traits include novelty-seeking, harm avoidance, reward dependence, and persistence. Character traits include self-directedness, cooperativeness, fantasy, and spirituality. The JTCI is made up of 108 true/false items to assess children’s behaviors, opinions, and feelings (Luby, Svrakic, McCallum, Przybeck, & Cloninger, 1999). Temperament traits are considered relatively stable after the preschool years, though dynamic processes with the environment continue (Roberts & DelVecchio, 2000; Shiner et al., 2012). The JTCI was administered at the 2-year follow-up separately to children and their parents. Data from the two informants was combined (after reverse scoring negatively phrased items) by considering any items endorsed as true by either informant as true.
Global Functioning
The CGAS measures severity based on global impairment from psychiatric symptoms and related adaptation in psychosocial functioning in school, social, work, and family contexts. On this scale, 0 is worst, 100 is best, and ≤ 60 is definite clinical impairment. The CGAS score is the lowest level of functioning during the rating period.
SES was established from the Hollingshead Four-Factor Index of Social Status (Hollingshead, 1976).
Substance Use Disorders (SUD) were defined using DSM-IV (American Psychiatric Association, 1994) criteria including for alcohol, marijuana, and other illicit drug use (eg sedatives, opioids, cocaine, other). A subset of N=155 participants were assessed as adults approximately 3 and a half years after the original study was completed. SUD was assessed at this time with the NetSCID (Structured Clinical Interview for DSM Disorders).
Statistical Analysis
Growth mixture modeling (GMM) in Mplus version 7.3 was used to group participants into subgroups based on ADHD severity scores across the longitudinal course of the study. Specifically, an ADHD severity score was calculated at each of the 6 waves (baseline through 10-year follow-up) as the number of ADHD symptoms endorsed at each wave (maximum of 18). A quadratic growth mixture model with these 6 severity scores as the outcome variables was used to determine a categorical latent class variable for grouping participants with similar ADHD severity trajectories. Mania severity was calculated as the number of mania symptoms endorsed at each wave (maximum of 8) and was included in the model as a time-varying covariate. Baseline age and gender were also included as covariates in the growth mixture model. Each subject’s probability of belonging to each of the latent classes was evaluated, and participants were assigned to the latent class with the greatest probability.
N=17 participants were not included in the analysis because they dropped out of the study, so growth mixture modeling was conducted on N=251 of the original N=268 participants. Several growth mixture models with varying numbers of classes for the latent class variable were compared, and the best model according to the Bayesian Information Criterion (BIC) and the Lo- Mendell-Rubin adjusted likelihood ratio test was selected.
Once latent class assignment was complete, baseline demographic and diagnostic characteristics were compared across classes using posthoc linear regression for continuous variables and logistic regression for categorical variables.
Psychiatric diagnoses through the 10-year follow-up, adult substance use disorders, and temperament and character factors obtained at the 2-year follow-up were compared across classes using posthoc logistic regression for dichotomous outcomes and linear regression for continuous outcomes. These models included baseline age, SES, gender, race, baseline mania, and use of stimulants or other medication for ADHD at any time during the study as covariates. Contrast statements were included in these models to make pairwise comparisons of the classes. Bonferroni correction was used to account for the 6 pairwise class comparisons, resulting in a significant p-value of p<0.0083. All analyses other than GMM were completed in SAS version 9.3.
Results
Of the N=268 baseline study participants, N=17 (6.3%) dropped out (N=6 ADHD, N=9 BP-I, N=2 healthy controls) through the 10-year assessment. The only missed assessments were those occurring after a subject discontinued from the study by design, i.e., no subject missed an assessment but was then assessed at a later data collection wave. As previously noted, the N=17 participants who discontinued the study were not included in these analyses. At baseline, 87.1% of the N=93 BP-I subjects had comorbid ADHD.
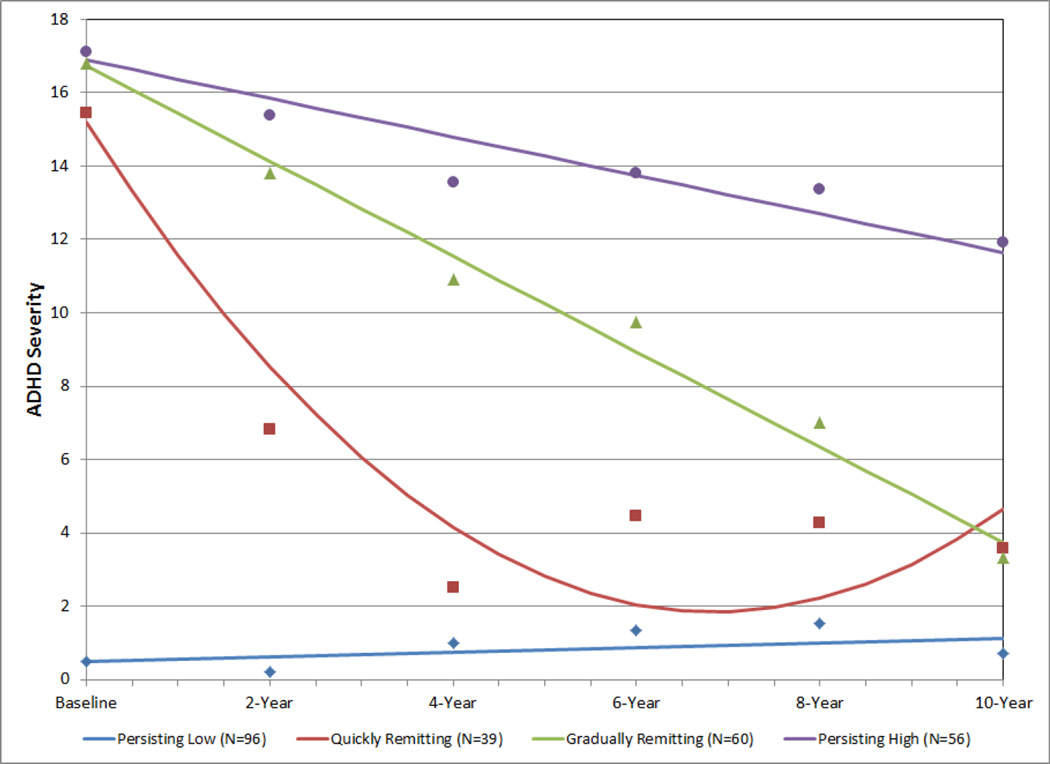
Fit statistics for growth mixture models with latent class variables with 1, 2, 3, 4, and 5 classes were compared. The BIC was lowest in the 4-class model (BIC=8158.8) compared to the others (1-class BIC=17129.3, 2-class BIC=8579.6, 3-class BIC=8253.0, 5-class BIC=8235.9). The 4-class model also fit significantly better than the 3-class model according to the Lo-Mendell-Rubin adjusted likelihood ratio test (p=0.0037), while the 5-class model was not a significant improvement over the 4-class model (p=0.4727). Therefore, the model that best fit the data included a latent class variable with 4 classes; 1 of these had significant intercept, linear, and quadratic components, and the other 3 classes had significant intercepts and linear components. Details of the growth mixture model with 4 latent classes are shown in Table 2. There were N=251 total participants: N=96 in class 1 (persisting low), N=39 in class 2 (quickly remitting), N=60 in class 3 (gradually remitting), and N=56 in class 4 (persisting high). Figure 1 illustrates the trajectories of ADHD severity scores in the 4 latent classes.
Table 2.
Growth Mixture Model with 4 Latent Classes in N=251 Participants
| Estimate | S.E. | Est./S.E. | Two-tailed p | |
|---|---|---|---|---|
| Persisting low class: Intercept | 0.480 | 0.122 | 3.941 | 0.000 |
| Persisting low class: Slope | 0.130 | 0.051 | 2.551 | 0.011 |
| Persisting low class: Quadratic | term removed from model, because non-significant | |||
| Quickly remitting class: Intercept | 15.180 | 0.418 | 36.316 | 0.000 |
| Quickly remitting class: Slope | −7.794 | 0.434 | −17.957 | 0.000 |
| Quickly remitting class: Quadratic | 1.138 | 0.097 | 11.774 | 0.000 |
| Gradually remitting class: Intercept | 16.737 | 0.205 | 81.526 | 0.000 |
| Gradually remitting class: Slope | −2.599 | 0.110 | −23.645 | 0.000 |
| Gradually remitting class: Quadratic | term removed from model, because non-significant | |||
| Persisting high class: Intercept | 16.894 | 0.210 | 80.268 | 0.000 |
| Persisting high class: Slope | −1.049 | 0.130 | −8.080 | 0.000 |
| Persisting high class: Quadratic | term removed from model, because non-significant | |||
Figure 1.
Four Latent Class Trajectories of ADHD Severity Across 10-Year Follow-Up in N=251 Participants
Baseline demographic and diagnostic characteristics of the N=251 participants by latent class are shown in Table 3. Participants in the persistently high class were significantly younger than participants in all 3 other classes. Also, subjects in the gradually remitting class were significantly younger than quickly remitting subjects. In addition, there were more males in the gradually remitting and persisting high classes compared to the persisting low and quickly remitting classes. The racial breakdown of the gradually remitting class was significantly different than those of the persisting low and persisting high classes, with fewer white subjects and more black and other race subjects. There were no differences in SES. Baseline CGAS score, mania severity, and ADHD severity were significantly lower in the persisting low class compared to the 3 other classes. Additionally, baseline ADHD severity was significantly lower in the quickly remitting class compared to the gradually remitting and persisting high classes. All N=92 baseline healthy control participants were in the persisting low class. Rate of stimulant use was significantly lower in the persisting low class compared to the 3 other classes, and participants in the quickly remitting class used stimulants significantly less than participants in the persisting high class.
Table 3.
Baseline Demographic and Diagnostic Characteristics of N=251 Participants by Latent Class
| Persisting Low |
Quickly Remitting |
Gradually Remitting |
Persisting High |
PL vs. |
PL vs. |
PL vs. |
QR vs. |
QR vs. |
GR vs. |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | QR p |
GR p |
PH p |
GR p |
PH p |
PH p |
|
| Baseline age | 11.1 (2.8) | 11.5 (2.7) | 10.4 (2.2) | 9.2 (1.9) | 0.3952 | 0.0714 | <0.0001 | 0.0263 | <0.0001 | 0.0109 |
| SESa | 4.1 (0.8) | 4.2 (0.7) | 4.2 (0.8) | 3.9 (1.0) | 0.2979 | 0.4569 | 0.2361 | 0.7140 | 0.0576 | 0.0840 |
| Baseline CGAS | 82.4 (9.9) | 47.2 (10.3) | 50.5 (8.8) | 49.5 (7.9) | <0.0001 | <0.0001 | <0.0001 | 0.0855 | 0.2234 | 0.5888 |
| Baseline mania | 0.3 (1.1) | 4.5 (1.9) | 4.3 (2.0) | 4.7 (2.1) | <0.0001 | <0.0001 | <0.0001 | 0.6001 | 0.5971 | 0.2410 |
| Baseline ADHD severity | 0.5 (1.3) | 15.5 (2.2) | 16.8 (1.4) | 17.1 (1.3) | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.2745 |
| N (%) | N (%) | N (%) | N (%) | p | p | p | p | p | p | |
| Male gender | 56 (58.3) | 20 (51.3) | 45 (75.0) | 47 (83.9) | 0.4547 | 0.0358 | 0.0017 | 0.0167 | 0.0010 | 0.2387 |
| Race | 0.8981 | 0.0223 | 0.8045 | 0.0778 | 0.9329 | 0.0365 | ||||
| White | 88 (91.7) | 36 (92.3) | 47 (78.3) | 52 (92.9) | ||||||
| Black | 5 (5.2) | 2 (5.1) | 8 (13.3) | 2 (3.6) | ||||||
| Other | 3 (3.1) | 1 (2.6) | 5 (8.3) | 2 (3.6) | ||||||
| Baseline diagnostic group | b | -- | -- | -- | -- | -- | ||||
| ADHD | 0 (0.0) | 12 (30.8) | 33 (55.0) | 30 (53.6) | ||||||
| Bipolar | 4 (4.2) | 27 (69.2) | 27 (45.0) | 26 (46.4) | ||||||
| Healthy | 92 (95.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||||||
| Stimulant usec | 9 (9.4) | 29 (74.4) | 53 (88.3) | 56 (92.9) | <0.0001 | <0.0001 | <0.0001 | 0.0779 | 0.0182 | 0.4104 |
On a 1–5 scale, with 5 being the highest SES
Comparisons could not be made for baseline diagnostic group because of 0-count cells
Use of stimulants or other medication for ADHD during the study;
PL=Persisting Low, QR=Quickly Remitting, GR=Gradually Remitting, PH=Persisting High
Table 4 shows psychiatric diagnoses through 10-year follow-up, adult substance use disorders, and temperament and character factors by latent class. Comorbid disorders were considered anytime through 10 year follow-up, and temperament assessments took place 2 years after baseline. They were correlates of course. In general, the persisting low class had the least psychopathology. Because this class contained primarily baseline healthy controls who remained consistently healthy over the 10 years of study, comparisons of interest are those between the quickly remitting, gradually remitting, and persisting high latent classes.
Table 4.
Characteristics of N=251 Participants by Latent Class Controlling for Baseline Age, Socioeconomic Status, Gender, Race, Baseline Mania, and Stimulant Use
| Persisting Low |
Quickly Remitting |
Gradually Remitting |
Persisting High |
PL vs. |
PL vs. |
PL vs. |
QR vs. |
QR vs. |
GR vs. |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Diagnoses through 10-Year Follow-Up |
(N=96) N (%) |
(N=39) N (%) |
(N=60) N (%) |
(N=56) N (%) |
QR p |
GR p |
PH p |
GR p |
PH p |
PH p |
| Maniaa | 5 (5.2) | 28 (71.8) | 35 (58.3) | 42 (75.0) | <0.0001 | <0.0001 | <0.0001 | 0.5764 | 0.1604 | 0.0210 |
| MDD | 18 (18.8) | 25 (64.1) | 33 (55.0) | 45 (80.4) | 0.0293 | 0.0200 | <0.0001 | 0.9345 | 0.0057 | 0.0014 |
| ADHD | 13 (13.5) | 38 (97.4) | 60 (100.0) | 56 (100.0) | -- | -- | -- | -- | -- | -- |
| Oppositional Defiant | 4 (4.2) | 27 (69.2) | 35 (58.3) | 47 (83.9) | <0.0001 | 0.0001 | <0.0001 | 0.2536 | 0.1195 | 0.0030 |
| Conduct | 0 (0.0) | 8 (20.5) | 13 (21.7) | 11 (19.6) | -- | -- | -- | -- | -- | -- |
| Separation Anxiety | 0 (0.0) | 6 (15.4) | 5 (8.3) | 6 (10.7) | -- | -- | -- | -- | -- | -- |
| Generalized Anxiety | 9 (9.4) | 5 (12.8) | 9 (15.0) | 13 (23.2) | 0.7574 | 0.5339 | 0.2165 | 0.7311 | 0.2865 | 0.3545 |
| Post-Traumatic Stress | 0 (0.0) | 1 (2.6) | 0 (0.0) | 0 (0.0) | -- | -- | -- | -- | -- | -- |
| Obsessive Compulsive | 3 (3.1) | 4 (10.3) | 4 (6.7) | 10 (17.9) | 0.8785 | 0.8125 | 0.4527 | 0.6092 | 0.4063 | 0.1215 |
| Panic Attack | 13 (13.5) | 9 (23.1) | 19 (31.7) | 18 (32.1) | 0.2616 | 0.0060 | 0.0054 | 0.0617 | 0.0491 | 0.7751 |
| Specific Phobia | 8 (8.3) | 6 (15.4) | 12 (20.00) | 15 (26.8) | 0.3587 | 0.1346 | 0.0673 | 0.5221 | 0.2879 | 0.5737 |
| Social Phobia | 6 (6.3) | 7 (18.0) | 5 (8.3) | 17 (30.4) | 0.3333 | 0.8786 | 0.1197 | 0.1815 | 0.4251 | 0.0193 |
| Adult Substance Use Disorder | N (%) | N (%) | N (%) | N (%) | p | p | p | p | p | p |
| Any Substance Use | 12 (19.4) | 5 (18.5) | 12 (36.4) | 19 (59.4) | 0.2166 | 0.5450 | 0.8725 | 0.4092 | 0.0826 | 0.2845 |
| Alcohol Use Dx | 9 (14.5) | 2 (7.4) | 9 (27.3) | 16 (50.0) | 0.0202 | 0.1697 | 0.5012 | 0.1401 | 0.0235 | 0.2530 |
| Cannabis Use Dx | 7 (11.3) | 2 (7.4) | 6 (18.2) | 16 (50.0) | 0.5226 | 0.7290 | 0.2741 | 0.6873 | 0.0426 | 0.0341 |
| Other Illicit Use Dx | 0 (0.0) | 2 (7.4) | 2 (6.1) | 6 (18.8) | -- | -- | -- | -- | -- | -- |
| Temperament and Character Factors | (N=96) Mean (SD) | (N=39) Mean (SD) | (N=60) Mean (SD) | (N=56) Mean (SD) | QR p | GR p | PH p | GR p | PH p | PH p |
| Novelty Seeking | 9.9 (3.3) | 14.0 (2.6) | 13.9 (3.4) | 14.4 (2.9) | 0.0010 | 0.0002 | <0.0001 | 0.7087 | 0.2058 | 0.2870 |
| Harm Avoidance | 9.4 (4.9) | 10.7 (5.0) | 10.4 (4.7) | 11.9 (5.0) | 0.0678 | 0.1343 | 0.0337 | 0.6591 | 0.7004 | 0.3474 |
| Reward Dependence | 7.8 (1.4) | 7.5 (1.5) | 7.0 (1.8) | 7.3 (1.9) | 0.4371 | 0.0869 | 0.4869 | 0.2930 | 0.9387 | 0.2081 |
| Persistence | 5.0 (1.3) | 4.2 (1.4) | 3.8 (1.6) | 3.4 (1.5) | 0.0496 | 0.0008 | <0.0001 | 0.1156 | 0.0050 | 0.1211 |
| Self-directedness | 19.3 (1.1) | 18.3 (2.2) | 17.3 (3.1) | 16.4 (3.6) | 0.5413 | 0.0039 | 0.0003 | 0.0093 | 0.0004 | 0.2104 |
| Cooperativeness | 19.3 (1.0) | 18.3 (1.6) | 17.6 (3.5) | 17.4 (3.1) | 0.1943 | 0.0029 | 0.0076 | 0.0559 | 0.1066 | 0.8086 |
| Fantasy | 1.8 (1.4) | 1.8 (1.3) | 2.3 (1.6) | 2.8 (1.5) | 0.1085 | 0.8111 | 0.0554 | 0.0305 | <0.0001 | 0.0240 |
| Spirituality | 4.0 (1.1) | 3.8 (1.3) | 3.8 (1.2) | 3.8 (1.4) | 0.6265 | 0.3547 | 0.6728 | 0.6254 | 0.9497 | 0.5374 |
Baseline mania was not a covariate in the model, because all participants with baseline mania had mania through 10-year follow-up;
PL=Persisting Low, QR=Quickly Remitting, GR=Gradually Remitting, PH=Persisting High
The persisting high class had significantly higher rates of MDD and ODD than the gradually remitting class and higher rates of MDD than the quickly remitting class. Rates of Mania and Social Phobia were higher in the persisting high class compared to the gradually remitting class, but significance did not remain after Bonferroni correction. Similarly, the persisting high class had higher rates of Panic Attack than the quickly remitting class, but these results did not hold up to correction for multiple comparisons. The persisting high class had the highest rate of SUD in adulthood (60%), although this rate was not significantly greater than the rates in the other classes (PL: 19.4%, QR: 18.5%, GR: 36.4%). There were no significant differences in rates of Alcohol Use Disorder or Cannabis Use Disorder. However, the persisting high class had marginally higher rates of both alcohol and marijuana use than the quickly remitting class and marginally higher rates of Cannabis Use Disorder than the gradually remitting class.
Temperament and character differences were evident between the quickly remitting and persisting high classes, with the persisting high class having less persistence, less self-directedness, and more fantasy.
Discussion
Study findings elucidate key psychopathological features that characterize severe trajectories of ADHD that persist into adulthood. A persisting high ADHD trajectory had the highest rates of comorbid Major Depressive Disorder and Oppositional Defiant Disorder. These findings are in line with a number of studies finding comorbid psychopathology among persisting cases of ADHD in both clinical and non-clinical samples (Barbaresi et al., 2013; Barkley et al., 2008; Kessler et al., 2011; Lara et al., 2009; Mannuzza et al., 1998). In contrast to other longitudinal studies, CD was not found to be more common in the persisting high class. This may be because of the inclusion of females in the sample and the low prevalence of CD found in the overall sample at baseline (see Geller et al., 2002). The lack of SUD findings may also be related to the low base rate of CD, as CD symptoms are thought to account for the relationship of ADHD and SUD in some larger longitudinal investigations (Lynskey & Fergusson, 1995); however, alcohol and cannabis use were marginally significant in the persisting high group compared to the others, suggesting power limitations could also account for the lack of SUD in persistent ADHD.
Importantly, the persisting high ADHD group had less persistence, less self-directedness, and more fantasy on temperament and character measures than the quickly remitting group, whose severity of ADHD diminished into adulthood. It is not altogether surprising that the group characterized by persisting high ADHD had low self-directedness and persistence, as lack of persistence in effortful tasks has been well described in lab and actual settings and speculated to be related to motivational and reward sensitivity differences in ADHD (for review, see Barkley, 2006; Rettew, Copeland, Stanger, & Hudziak, 2004). Similarly, children with ADHD may be described by teachers as seemingly off-task or fantasizing, though fantasy specifically assessed as a character trait (e.g. tendency to imagine/daydream) in ADHD is not empirically well investigated (Rettew et al., 2004).
Limitations of the study include the secondary analysis of a dataset originally ascertained for the investigation of BP-I; most of the affected subjects at baseline had BP-I as their primary diagnosis, which is a possible confounder. However, the vast majority of the BP-I sample had comorbid ADHD, and mania severity was included as a time-varying covariate in the growth mixture models that determined the ADHD trajectories. Further, baseline BP-I diagnosis was controlled for in statistical comparisons of the ADHD trajectory classes. Given the richness and comprehensive nature of this large longitudinal dataset, the comparison ADHD group and the ADHD severity in the BP group meaningfully informs trajectories of ADHD. Despite the rigorous statistical control, ADHD in the BP-I group could reflect a unique pathology and this should be considered in future studies. The study did not include the inattentive type of ADHD and study findings are not generalizable to this group. A potential limitation was the use of medications in the sample. However, this was also addressed statistically by covarying for stimulant use. Another limitation is the lack of teacher informed ADHD in children; however, because the study tracked individuals over 10 years, teacher reports became inconsistently available. This is not an uncommon problem in longitudinal studies of ADHD into adulthood and does not minimize the merit of the study in adding to a critical body of literature informing long term clinical outcomes. A recent study suggested teacher reports did not predict persistence of ADHD (Cheung et al.,2015). Finally, the higher SES of the overall sample may limit generalizability to other populations.
Conclusions
Despite the limitations, the present investigation tracked participants over 10 years from middle childhood into early adulthood, informing characteristic trajectories of ADHD severity into adulthood using advanced statistical methodology. Current findings add to the literature on the characteristics of childhood ADHD that persist into adulthood and begin to elucidate what factors may emerge in such a consistently severe group of individuals with ADHD. Findings suggest that key temperament features may be important markers of a persistent course and therefore might be key targets for early intervention. Taken together, findings highlight the need for additional, larger investigations that could shed light on ADHD subjects most at risk for adverse adult outcomes so that limited public health resources can be optimized.
Acknowledgments
Funding Support: This research was supported by the National Institutes of Health: DA000357; DA023668; DA032573; MH064769; MH53063 and MH57451
Biographies
Mini Tandon, D.O. is an Assistant Professor in the Child Division of the Department of Psychiatry at Washington University School of Medicine. She also directs the Preschool Clinic at BJC Behavioral Health, a comprehensive community assessment, treatment, and teaching clinic. Her research is in early diagnosis and treatment development for preschool ADHD and disruptive behaviors, including understanding risks from nicotine exposure. She is the author of a children's book that aims to raise awareness of early childhood mental health.
Rebecca Tillman received a Master’s degree in statistics from the University of Illinois – Urbana/Champaign in 2002. She has worked in the Washington University psychiatry department as a statistical data analyst since 2002. She is responsible for data management and statistical analysis for several of the research studies being conducted in the Early Emotion Development Program.
Arpana Agrawal, PhD., is a psychiatric geneticist who is an Associate Professor of Psychiatry at Washington University School of Medicine. Her research focuses on identifying and examining factors that contribute to the comorbidity between substance use and other psychopathology, such as ADHD. She is also particularly interested in methodologies that explore the onset and course of behavior and mental illness.
Joan Luby, M.D. is a child psychiatrist who is the Samuel and Mae S. Ludwig Professor of Psychiatry at Washington University School of Medicine. Her research focuses on the identification and treatment of early childhood mood disorders as well as longitudinal follow-up and brain development in these samples.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4th. Washington, D.C: American Psychiatric Association; 1994. [Google Scholar]
- Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: a prospective study. Pediatrics. 2013;131(4):637–644. doi: 10.1542/peds.2012-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley R. Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 3rd. New York: NY Guilford Press; 2006. [Google Scholar]
- Barkley R, DuPaul G, McMurray M. Comprehensive evaluation of attention deficit disorder with and without hyperactivity as defined by research criteria. Journal of Consulting and Clinical Psychology. 1990;58(6):775–789. doi: 10.1037//0022-006x.58.6.775. [DOI] [PubMed] [Google Scholar]
- Barkley R, Fischer M, Smallish L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology. 2002;111(2):279–289. [PubMed] [Google Scholar]
- Barkley R, Murphy K, Dupaul G, Bush T. Driving in young adults with attention deficit hyperactivity disorder: Knowledge, performance, adverse outcomes, and the role of executive functioning. Journal of the International Neuropsychological Society. 2002;8(5):655–672. doi: 10.1017/s1355617702801345. [DOI] [PubMed] [Google Scholar]
- Barkley R, Murphy KR, Fischer M. Adult ADHD: What the science says. New York: Guilford; 2008. [Google Scholar]
- Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, et al. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder. Patterns of comorbidity in probands and relatives psychiatrically and pediatrically referred samples. Archives of General Psychiatry. 1992;49(9):728–738. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- Biederman J, Milberger S, Faraone SV, Kiely K, Guite J, Mick E, Ablon S, Warburton R, Reed E. Family-environment risk factors for attention-deficit hyperactivity disorder: A test of Rutter’s indicators of adversity. Archives of General Psychiatry. 1995;52(6):464–470. doi: 10.1001/archpsyc.1995.03950180050007. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty C, Monuteaux M, Fried R, Byrne D, Mirto T, Spencer T, Wilens T, Faraone S. Adult Psychiatric Outcomes of Girls With Attention Deficit Hyperactivity Disorder: 11-Year Follow-Up in a Longitudinal Case-Control Study. American Journal of Psychiatry. 2010;167(4):409–417. doi: 10.1176/appi.ajp.2009.09050736. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Clarke A, Lomedico A, Faraone SV. Predictors of persistent ADHD: an 11-year follow-up study. Journal of Psychiatric Research. 2011;45(2):150–155. doi: 10.1016/j.jpsychires.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Evans M, Small J, Faraone SV. How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Research. 2010;177(3):299–304. doi: 10.1016/j.psychres.2009.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird H, Canino G, Rubiostipec M, Ribera JC. Further measures of the psychometric properties of the Childrens Global Assessment Scale. Archives of General Psychiatry. 1987;44(9):821–824. doi: 10.1001/archpsyc.1987.01800210069011. [DOI] [PubMed] [Google Scholar]
- Bird H, Gould M, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(1):78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Brown RT, Borden KA. Hyperactivity at adolescence: some misconceptions and new directions. Journal of Clinical Child Psychology. 1986;15(3):194–209. [Google Scholar]
- Cheung CH, Rijdijk F, McLoughlin G, Faraone SV, Asherson P, Kuntsi J. Childhood predictors of adolescent and young adult outcome in ADHD. Journal of Psychiatric Research. 2015;62:92–100. doi: 10.1016/j.jpsychires.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychological Medicine. 2006;36(2):159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Geller B, Tillman R, Craney JL, Bolhofner K. Four-year prospective outcome and natural history of mania in children with a prepubertal and early adolescent bipolar disorder phenotype. Archives of General Psychiatry. 2004;61(5):459–467. doi: 10.1001/archpsyc.61.5.459. [DOI] [PubMed] [Google Scholar]
- Geller B, Warner K, Williams M, Zimerman B. Prepubertal and young adolescent bipolarity versus ADHD: assessment and validity using the WASH-U-KSADS, CBCL and TRF. Journal of Affective Disorders. 1998;51(2):93–100. doi: 10.1016/s0165-0327(98)00176-1. [DOI] [PubMed] [Google Scholar]
- Geller B, William M, Zimerman B, Frazier J. Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) St Louis, MO: Washington University in St Louis; 1996. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo C. Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(4):450–455. doi: 10.1097/00004583-200104000-00014. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Delbello MP, Bolhofner K, Craney JL, Frazier J, Beringer L, Nickelsburg MJ. DSM-IV mania symptoms in a prepubertal and early adolescent bipolar disorder phenotype compared to attention-deficit hyperactive and normal controls. Journal of Child and Adolescent Psychopharmacology. 2002;12(1):11–25. doi: 10.1089/10445460252943533. [DOI] [PubMed] [Google Scholar]
- Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost grown up: I. Psychiatric status. Archives of General Psychiatry. 1985;42(10):937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- Halperin J, Healey D. The influences of environmental enrichment, cognitive enhancement, and physical exercise on brain development: can we alter the developmental trajectory of ADHD? Neuroscience and Biobehavioral Reviews. 2011;35(3):621–634. doi: 10.1016/j.neubiorev.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halperin J, Trampush J, Miller C, Marks D, Newcorn J. Neuropsychological outcome in adolescents/young adults with childhood ADHD: Profiles of persisters, remitters and controls. Journal of Child Psychology and Psychiatry. 2008;49(9):958–966. doi: 10.1111/j.1469-7610.2008.01926.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart E, Lahey B, Loeber R, Applegate B, Frick P. Developmental change in attention-deficit hyperactivity disorder in boys: A four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23(6):729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, Swanson EN. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology. 2012;80(6):1041–1051. doi: 10.1037/a0029451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale University Department of Sociology; 1976. [Google Scholar]
- Karam RG, Breda V, Picon FA, Rovaris DL, Victor MM, Salgado CAI, Caye A. Persistence and remission of ADHD during adulthood: a 7-year clinical follow-up study. Psychological medicine. 2015;45(10):2045–2056. doi: 10.1017/S0033291714003183. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Ustun TB. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Archives of General Psychiatry. 2011;68(1):90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey B, McBurnett K, Loeber R. Are Attention-Deficit/Hyperactivity Disorder and Oppositional Defiant Disorder Developmental Precursors to Conduct Disorder? In: Sameroff A, Lewis M, Miller S, editors. Handbook of Developmental Psychopathology. New York: Plenum; 2000. pp. 431–446. [Google Scholar]
- Lara C, Fayyad J, de Graaf R, Kessler RC, Aguilar-Gaxiola S, Angermeyer M, Demytteneare K, de Girolamo G, Haro JM, Jin R. Childhood predictors of adult attention-deficit/hyperactivity disorder: Results from the World Health Organization World Mental Health Survey Initiative. Biological Psychiatry. 2009;65(1):46–54. doi: 10.1016/j.biopsych.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loney J, Kramer J, Milich RS. The hyperactive child grows up: predictors of symptoms, delinquincy and achievement at follow-up. In: Gadow KD, Loney J, editors. Psychosocial Aspects of Drug Treatment for Hyperactivity. Boulder, CO: Westview Press; 1981. pp. 381–416. [Google Scholar]
- Luby J, Svrakic D, McCallum K, Przybeck T, Cloninger C. The Junior Temperament and Character Inventory: preliminary validation of a child self-report measure. Psychological Reports. 1999;84(3 Pt 2):1127–1138. doi: 10.2466/pr0.1999.84.3c.1127. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Fergusson DM. Childhood conduct problems, attention deficit behaviors, and adolescent alcohol, tobacco, and illicit drug use. Journal of Abnormal Child Psychology. 1995;23(3):281–302. doi: 10.1007/BF01447558. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult outcome of hyperactive boys: educational achievement, occupational rank, and psychiatric status. Archives of General Psychiatry. 1993;50(7):565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. The American Journal of Psychiatry. 1998;155(4):493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Moulton JL. Persistence of attention-deficit/hyperactivity disorder into adulthood: What have we learned from the prospective follow-up studies? Journal of Attention Disorders. 2003;7(2):93–100. doi: 10.1177/108705470300700203. [DOI] [PubMed] [Google Scholar]
- Miller CJ, Miller SR, Newcorn JH, Halperin JM. Personality characteristics associated with persistent ADHD in late adolescence. Journal of Abnormal Child Psychology. 2008;36(2):165–173. doi: 10.1007/s10802-007-9167-7. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Houts R, Asherson P, Belsky DW, Corcoran DL, Hammerle M, Poulton R. Is Adult ADHD a Childhood-Onset Neurodevelopmental Disorder? Evidence From a Four-Decade Longitudinal Cohort Study. American Journal of Psychiatry. 2015 doi: 10.1176/appi.ajp.2015.14101266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Houck PR. The MTA at 8 Years: prospective follow-up of children treated for Combined-Type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(5):484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monuteaux MC, Mick E, Faraone SV, Biederman J. The influence of sex on the course and psychiatric correlates of ADHD from childhood to adolescence: A longitudinal study. Journal of Child Psychology and Psychiatry. 2010;51(3):233–241. doi: 10.1111/j.1469-7610.2009.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Butler KM, Huang-Pollock CL, Henderson JM. Inhibitory processes in adults with persistent childhood onset ADHD. Journal of Consulting and Clinical Psychology. 2002;70(1):153–157. doi: 10.1037//0022-006x.70.1.153. [DOI] [PubMed] [Google Scholar]
- Pingault J-B, Tremblay RE, Vitaro F, Carbonneau R, Genolini C, Falissard B, Côté SM. Childhood trajectories of inattention and hyperactivity and prediction of educational attainment in early adulthood: a 16-Year longitudinal population-based study. American Journal of Psychiatry. 2011;168(11):1164–1170. doi: 10.1176/appi.ajp.2011.10121732. [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, Ryan N. The Schedule for Affective Disorders and Schizophrenia for School-Age Children (Kiddie-SADS)-1986. Pittsburgh, PA: Western Psychiatric Institute and Clinic; 1986. [Google Scholar]
- Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: A controlled, longitudinal, community-based study. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(11):1424–1431. doi: 10.1097/00004583-200011000-00017. [DOI] [PubMed] [Google Scholar]
- Rettew DC, Copeland W, Stanger C, Hudziak JJ. Associations between temperament and DSM-IV externalizing disorders in children and adolescents. Journal of Developmental and Behavioral Pediatrics. 2004;25(6):383–391. doi: 10.1097/00004703-200412000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: a quantitative review of longitudinal studies. Psychological Bulletin. 2000;126(1):3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A Childrens Global Assessment Scale (CGAS) Archives of General Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Shiner RL, Buss KA, McClowry SG, Putnam SP, Saudino KJ, Zentner M. What is temperament now? Assessing progress in temperament research on the twenty-fifth anniversary of Goldsmith et al. Child Development Perspectives. 2012;6(4):436–444. [Google Scholar]
- Spencer TJ, Biederman J, Mick E. Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. Journal of Pediatric Psychology. 2007;32(6):631–642. doi: 10.1093/jpepsy/jsm005. [DOI] [PubMed] [Google Scholar]
- Taylor E, Sandberg S, Thorley G, Giles S. The Epidemiology of Childhood Hyperactivity. Vol. 33. Oxford: Institute of Psychiatry/Oxford University Press; 1991. [Google Scholar]
- Turgay A, Goodman DW, Asherson P, Lasser RA, Babcock TF, Pucci ML, Barkley R. Lifespan persistence of ADHD: the life transition model and its application. The Journal of clinical psychiatry. 2012;73(2):192–201. doi: 10.4088/JCP.10m06628. [DOI] [PubMed] [Google Scholar]
- Uchida M, Spencer TJ, Faraone SV, Biederman J. Adult Outcome of ADHD An Overview of Results From the MGH Longitudinal Family Studies of Pediatrically and Psychiatrically Referred Youth With and Without ADHD of Both Sexes. Journal of attention disorders. 2015 doi: 10.1177/1087054715604360. 1087054715604360. [DOI] [PubMed] [Google Scholar]
- Weiss G, Hechtman L, Milroy T, Perlman T. Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. Journal of the American Academy of Child Psychiatry. 1985;24(2):211–220. doi: 10.1016/s0002-7138(09)60450-7. [DOI] [PubMed] [Google Scholar]
- Wender EH. Attention-deficit hyperactivity disorders in adolescence. Journal of Developmental and Behavioral Pediatrics. 1995;16(3):192–195. [PubMed] [Google Scholar]
- Wilens T, Biederman J, Spencer TJ. Attention deficit/hyperactivity disorder across the lifespan. Annual Review of Medicine. 2002;53:113–131. doi: 10.1146/annurev.med.53.082901.103945. [DOI] [PubMed] [Google Scholar]
- Wilens T, Upadhyaya H. Impact of substance use disorder on ADHD and its treatment. The Journal of Clinical Psychiatry. 2007;68(8):e20–e20. doi: 10.4088/jcp.0807e20. [DOI] [PubMed] [Google Scholar]
- Wilson JM, Marcotte AC. Psychosocial adjustment and educational outcome in adolescents with a childhood diagnosis of Attention Deficit Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(5):579–587. doi: 10.1097/00004583-199605000-00012. [DOI] [PubMed] [Google Scholar]