Abstract
Background:
Massive bone allograft is an option in cases of limb preservation and reconstruction after massive benign and malignant bone tumor resection. The purpose of this study was to analyze the outcome of these procedures at Imam Reza Hospital, Mashhad University of Medical Sciences.
Methods:
In this study, 113 cases have been presented. Eleven cases were excluded (patients has a traumatic defect or they passed away before the completion of the study’s two-year follow up period). Each patient completed a questionnaire, went through a physical examination and, if indicated, X-ray information was collected. The patients were divided into three groups: chemotherapy, chemotherapy plus radiation therapy, and no-adjuvant-therapy.
Results:
Fifty-four cases were male and the mean age was 24.5±5.39. The number of cases and indications for surgery were: 33 cases of aggressive benign tumors or low grade malignant bone tumors (large bone defects) including 16 germ cell tumors, eight aneurysmal bone cysts, five low grade osteosarcomas, and four chondrosarcomas. Another 69 cases were high-grade malignant bone tumors including 42 osteosarcomas, 21 Ewing’s sarcoma, and six other high grade osteosarcomas. Patients were divided into three groups: the first group received no adjuvant therapy, the second group received chemotherapy, and the third group received chemotherapy plus radiotherapy. The location of tumors were as follows: eight cases in the pelvic bone, 12 in the proximal femur, 18 in the femoral shaft, 36 in the distal femur, 12 in the proximal tibia, and 16 in the humeral bone. The 12 cases of proximal femoral defects were reconstructed by allograft composite prosthesis, 18 diaphyseal defects with intercalary allograft, and 36 distal femoral defects were reconstructed using osteoarticular allograft. The rate of deep infection was 7:8% (eight patients) and in this regard, we found a significant difference among the three groups, such that most cases of infection occurred in the adjuvant chemotherapy plus radiation therapy group. Allograft fracture occurred in six patients and prevalence was the same in all groups. Only in six cases of radio-chemotherapy nonunion occurred, so we used autogenous bone graft for union. Local recurrence was observed in six patients: three belonged to the adjuvant chemotherapy group and the other three were in the chemo-radiotherapy group; no significant difference was observed between these two groups. However, there was a significant difference between these two and the group that received no adjuvant therapy. Also, there were 11 cases of metastases and Restriction of knee joint motion occurred in 48 cases of osteo-cartilaginous grafts of the distal femur and proximal tibia.
Conclusion:
Although structural allograft is an appropriate choice in limb reconstruction after massive resection of involved tissues in malignant and invasive bone tumors, the risk of complications such as nonunion and infection in massive allograft increases in cases of adjuvant (chemotherapy and radiotherapy) modalities of treatment. Whereas the rate of tumor recurrence, metastasis, and restrictions in range of motion during a short term follow up after implantation showed no significant difference among the evaluated groups. Consequently, further attention and constant periodic visits of the patients and checking for local recurrence and distant metastasis should be done after surgery.
Keywords: Allograft, Bone tumor, Chemotherapy, Limb-salvage, Radiotherapy
Introduction
Limb salvage is an important goal in bone tumor surgery. In recent years the number of limb sparing surgeries for bone tumors has increased due to advances in imaging techniques, chemotherapy, radiation therapy, and operations that increase patient survival. Bone tumor excision often develops a large defect in the bone, prompting physicians to look for an appropriative function-preserving alternative after massive resection of the bone tumor and affected soft tissue. Limb sparing surgeries take place only when major vessels and nerves are not involved and the surgeon can reconstruct the limb with required function and performance after resection of the tumor with secure clear margins (1). There are several methods for preserving limb length and filling bone defects after excision of the tumor. Preferred methods in bone reconstruction in these operations include: megaprostheses (custom made, modular replacement, and endoprostheses), allograft-prosthetic composite, and allograft alone (2). Structural allograft, massive cortical allograft, large endoprosthesis, or a combination forms the art of bone reconstruction (3). Endoprostheses are made for this goal, but they are expensive and not easily available. Allograft is a tissue obtained from human corpses and is available in bone banks as fresh-frozen bone allograft, freeze-dried bone allograft, or demineralized freeze-dried bone allograft with decreased immunization properties (4). Figures 1-6 show patients with allografts.
Figure 1.
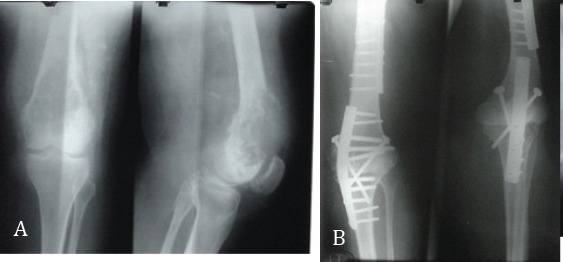
Knee allograft arthrodesis in a 35-year-old patient with germ cell tumors.
Figure 2.
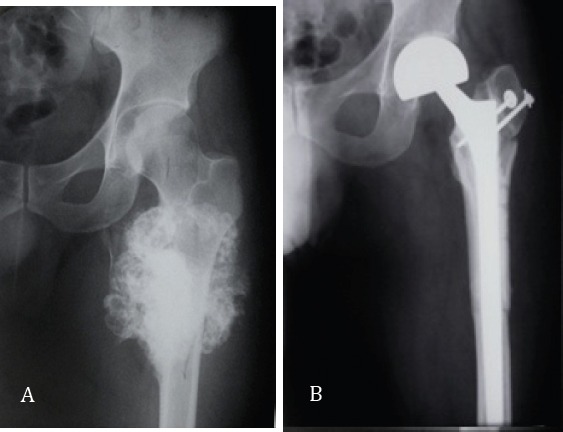
A: 27-year-old man with proximal femoral chondrosarcoma, B: The same patient with allograft prosthesis composite.
Figure 3.

A. A 12-year-old girl with proximal tibia osteosarcomaB. The same patient 1 year after proximal tibial osteoarticular allograft; union is seen.
Figure 4.
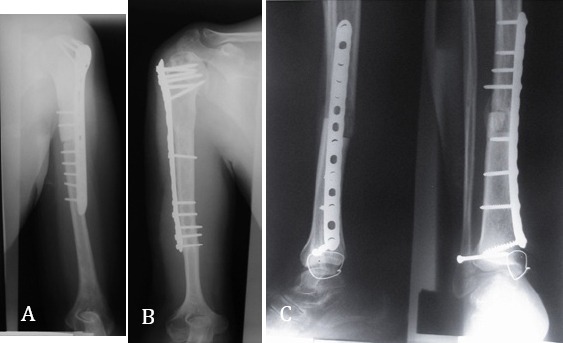
A: Proximal humerus osteoarticular allograft in a 30-year-old woman with chondrosarcoma, B: Proximal humerus osteoarticular allograft in a 20-year-old man with osteosarcoma seven years after surgery, C: Distal tibial osteoarticular allograft in a 30-year-old man with osteosarcoma.
Figure 5.
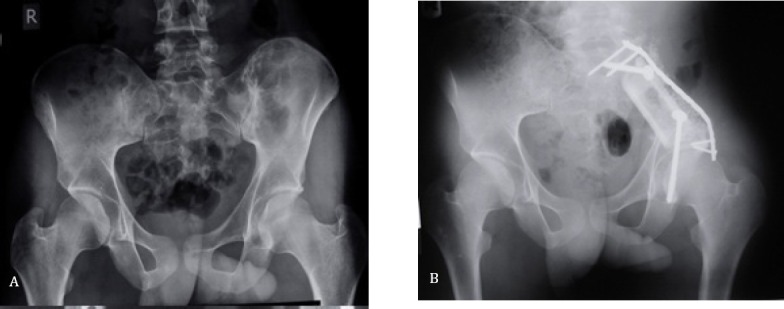
A: 20-year-old man with left iliac bone Ewing sarcoma, B: Pelvic intercalary allograft (three years after surgery).
Figure 6.
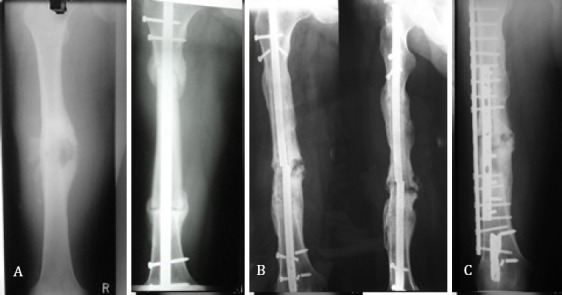
A: 26-year-old male with telangiectatic osteosarcoma, B:Three years after intercalary allograft union was seen, C: D Eleven years after surgery on the allograft fracture that was fixed with a dynamic compression plate.
Other treatment options in young patients with large bone defects (due to massive tumor excision) and structural allograft exist, but allograft is the preferred treatment for substitute bone defects (1). Since the establishment of a bone bank in Iran, many patients with massive bone or joint resection due to bone tumors have undergone structural allograft as a replacement in the Imam Reza Hospital of the Mashhad University of Medical Sciences. The aim of this study was to investigate complications (fracture, infection, and non-union) and clinical results (stability and joint range of motion) in the patients.
Materials and Methods
In this study, we evaluated 113 patients who underwent massive bone tumor resection and structural allograft implantation. Demographic data were obtained from the patients’ clinical records and then they were invited for follow up studies, and the efficacy of limb function, we used to do physical exam and x rays, and for evaluating patient satisfaction we asked them to fillout questionnaire forms. 11 cases; consisting trauma patients or those patient died before 2 years of follow up completion, were excluded from this study. The rest of the patients were classified into three groups: 46 patients who received adjuvant chemotherapy, 23 patients who received both adjuvant chemotherapy and radiation therapy, plus 33 patients who received no adjuvant therapy.
Results
Indications for surgery were: aggressive benign tumors or low grade sarcomas (33 cases), large bone defects including Giant cell tumors 16, eight aneurysmal bone cysts 8, low grade osteosarcomas 5, and chondrosarcomas 4, and high grade malignant tumors were 69 cases: included osteosarcomas 42, Ewing’s sarcomas 21, and other high grade sarcomas osteosarcomas 6.
The localization of tumors were as follows: eight cases in the pelvic bone, 12 in the proximal femur, 18 in the femoral shaft, 36 in the distal femur, 12 in the proximal tibia, and 16 in the humeral bone.
Twelve cases of proximal femoral defects were reconstructed by the allograft composite prosthesis, 18 diaphyseal defects with intercalary allograft, and 36 distal femoral defects were reconstructed using osteoarticular allograft.
The rate of deep infection was 7:8 % (eight patients), and we found a significant difference among the three groups, such that most cases of infection occurred in the adjuvant chemotherapy and radiation therapy group. Six patients experienced allograft fracture with two cases each in the no-adjuvant-therapy (giant cell tumor), chemotherapy, and chemo-radiotherapy group. The K score test did not indicate any significant difference among the mentioned groups.
Only in six cases from the radio-chemotherapy group did nonunion occur, in which we used autogenous bone graft for the union. According to the K score test, the mentioned three groups were different in this regard and the maximum rate of nonunion occurred in the group that received both chemotherapy and radiation therapy. Local recurrence was observed in six patients, in which three were in the adjuvant chemotherapy group and the other three were in the chemo-radiotherapy group; no meaningful difference was observed between these two groups using the K score test.
Follow up for metastases was two years minimum. The total number of metastases was 11, in which two were in the lungs in the no adjuvant therapy group (giant cell tumor), five in the chemotherapy group (four in the lungs and one in another bone), four in the chemo-radiotherapy group (three in the lungs and one in both the lungs and another bone).
Restriction of knee joint motion occurred in 48 cases of osteocartilaginous grafts of the distal femur and proximal tibia. Twenty-two cases were in the chemotherapy, 11 in the chemo-radiotherapy, and 15 in the no adjuvant therapy groups; there was no significant difference found using the K score test.
In the short-term follow up, instability occurred in all 16 cases of osteoarticular grafts around the knee joint and stability was established by using knee support, and in two patients we did knee joint arthrodesis.
In the long-term follow up, range of motion had no change, but all cases of knee osteoarticular allograft developed degenerative joint disease. In the proximal of the humorous shoulder, suspension (static and dynamic) was done for all cases (16 patients) that were stable; the goal was preserving normal motion of the elbow, wrist, and fingers.
Discussion
According to several reports, a surgeon who uses allograft cannot predict the end results (5). Complications after massive allograft surgery in patients who received chemotherapy was estimated at about 60% in a study by Dick et al. that included nonunion (26%), pin and plate fracture (11%), allograft fracture (7%), and infection (11%) (6). On the other hand, survival in patients with malignant bone tumors is highly associated with effective chemotherapy, increasing patient survival rates from 20% to 58-80% after two years (7). However, it can also influence the clinical result of the allograft implantation as we have shown in our study.
Fifty-four of our patients were male (52%) with an average age of 24.41±5.43 years. Most were young, which is an important factor, because youth is attributed to better improvement in this age group and faster return to daily activities. In addition to psychological problems, high mortality and morbidity after limb amputation and the underlying disease creates a high socioeconomic load on the health and economic system. This issue also shows the importance of determining the advantages and disadvantages of such treatments in these patients.
Allograft infection
The rate of infection in our study was 7.8% (eight cases) and we found a significant difference among the three groups in this respect. Similarly, Dick et al. reported an infection rate of 11% and in other reports the rate of infection in structural allograft was between 12-15% that generally led to limb amputation or dislodging of the allograft.
Infection is the most common complication that may occur after allograft implantation. Allograft infection is extremely difficult to treat particularly when osteoarticular allograft is used, and it may ultimately lead to limb amputation. It was quite a frequent complication in our study, particularly when the patients received adjuvant chemotherapy and radiation therapy. Due to malignant systemic diseases and chemotherapy and radiotherapy in these patients, the immune system became compromised and the patient was thus predisposed to resistant infection.
Structural allograft works as a foreign body and prepares an appropriate environment for proper microorganism growth (8). Allograft preparation and packaging was done by skilled surgeons and educated orthopedic assistants and this can explain the occurrence of rather low infection rates in our study. In a similar study, Farfalli reported that infection was seen in 11% of patients (9). In another study by Jamshidi, acute infection in one patient and chronic infection in two patients (15%) was reported (10). In Bullens et al.’s study, they reported the overall infection rate at 16%. Menkin also reported that the risk of infection was 10% after the first year of implantation (3, 11). However, in a study by Nekouie no wound or bone infection was observed in the patients (12).
Precise and exact observation of sterilization standards in allograft preparation, covering of soft tissue lesions, prescribing appropriate antibiotics at the proper dosage during and after surgery, and proper wound closure without any undesired pressure during surgery are important in preventing infection. Deep infection in osteoarticular allograft and intercalary allograft with more than 12 centimeters of length is extremely difficult to control and might lead to limb amputation. Therefore, any action in favor of preventing the occurrence of infection is highly preferred (13).
Allograft fracture
Allograft fractures after surgery is another complication of reconstructive surgery, particularly when gamma radiation is used in their preparation process, because this radiation makes the bone and its surrounding soft tissue extremely brittle (13). In our study, we observed six allograft fractures (5.88%) and in two patients this occurred due to failure in properly protecting the allograft with a plate. The underlying cause of allograft fracture in the other cases was unknown. Fracture occurred in the proximal of the femur in two patients, proximal of the tibia in one, and distal of the femur in three. We found no significant difference among the three groups based on the K score test (P=0.881). Similarly, in another study the fracture rate of osteoarticular allograft was reported at 17% during the first two years after surgery (14). In another study, Donati et al. reported that the rate of pin and plate fracture in patients that underwent limb salvage surgery for osteosarcoma was 4.9% In a study by Farfalli, three of 26 patients (11%) experienced incomplete allograft fracture (15, 9). Jamshidi reported a pin and plate fracture rate of 5% (10). In this latter study done on patients who received osteoarticular allograft, pin and plate fracture occurred in 23% and bone graft fracture in 16% of cases. However, in patients who received bone allograft, pin and plate fracture occurred in 48% of cases and there was no graft fracture (1). Bullens et al. reported an overall fracture rate of 13% (3) and Menkin showed that allograft was associated with an increased risk of fracture (19%) after the third year following surgery (3, 11). It seems that the high incidence of pin and plate fracture in bone allograft recipients is due to the existence of only two points that connects the allograft to the patient’s bone, causing the union to form slowly because of callus produced by the host bone. The fusion takes about a year and the callus will never find a natural configuration (16). Observation of the primary principles of harvesting and preparing grafts, properly inserting pin and plates, and embedding orthopedic cement, if necessary, will prevent the fractures to some extent. In most cases, the fragments become separated and the patient should have another surgery to correct the fracture using larger plate; and to facilitate the union, autogenous bone graft has to be used (17). In other cases, the surgeon may decide to remove the broken bone and use either a new graft or another method.
Nonunion of allograft to the bone of the patient
Only six cases (5.88%) of nonunion were observed in our study, leading to autogenous grafting. Most of them were in the chemoradiation group (P= 0.04), indicating that the rate of nonunion in patients who received chemotherapy and radiation therapy together was rather high compared to the other two groups. In a study by Farfalli, nonunion was observed in 7% of patients (9). Bullens et al. reported that the overall rate of nonunion was 65% (3). Friedlaneder et al. declared that using adjuvant chemotherapy with methotrexate and Adriamycin significantly postponed the formation of callus (18).
On the one hand, nonunion of allograft bone might be due to lack of proper plate insertion or orthopedic cement penetration into the space between the allograft and recipient bone. However, the rate of allograft fractures in those patients in which allograft is fused to their bone is quite rare.
In massive surgeries for malignant tumors due to vast extended surgery, soft tissue injuries, and the removal of large amounts of muscle with the tumor, perfusion at the junction of the allograft to the recipient bone is largely impaired leading to nonunion of the allograft (19).
Metastasis
Metastasis was seen in 11 patients (10.78%). Similarly, in a study by Farfalli, the allograft was removed in two cases out of 26 patients (7%) due to tumor recurrence (9). Six patients (5.88%) had evidence of local recurrence: three of them were in the adjuvant chemotherapy group and the other three were in the chemoradiotherapy group. However, the K score test did not show any significant difference between these two groups (P=0.881), although there was a meaningful difference between these two and the group that received no adjuvant therapy. Similar to our study, this recurrence was observed in two patients (7%) in the study of Farfalli (18). In a study by Nekouie, local recurrence of a tumor was seen in two patients out of 20 recruited cases (10%) (12). In Bullens’ study, three patients (10%) from 32 patients who received allograft showed evidence of disease after local recurrence.
When we evaluated the number of metastases during the first two years after surgery, we found 11 patients (10.78%) developed metastases. Similar to our study, Nekouie mentioned that during the average 27 months of follow-up, out of the 20 evaluated patients, two (10%) showed distant metastases, one in the lungs and thorax, and the other in the vertebral column (12). In another similar study by Bullens that followed 32 structural allograft recipients after bone tumor excision with an average interval of five years and three months, our patients (12%) died of pulmonary metastases and the other 25 patients remained disease free.
Regarding the development of restriction in range of motion (30-60 degrees), the short and long term functional score was 47.8% in our study. We observed short-term instability in all knee osteoarticular grafts (distal of the femur and proximal of the tibia) again during perennial follow up, and we concluded degenerative joint disease. Farfalli evaluated patients using the Musculoskeletal Tumor Society scoring system and reported a score of 29, indicating good allograft survival in spite of mentioned complications.
Osteoarticular allograft can be used in limb reconstruction after bone tumor resection and it seems that complications including infection and nonunion is relatively high in patients receiving chemotherapy and radiotherapy. Accordingly, further attention should be given to these patients such as observing precautions like: complete sterilization during surgery, regular and proper follow up, evaluations of infection, nonunion, local recurrence and distant metastases, and informing patients properly after surgery.
Structural allograft complications including infection and nonunion significantly increased parallel to the increase in treatment modalities, particularly when chemotherapy was used in combination with radiation therapy. In spite of several curable complications that occur in limb salvage surgeries, the preserved extremity is - functionally and psychologically - more effective for the patient rather than amputating the limb and using prostheses. Also; these surgeries do not influence the survival of patients in comparison with amputation. Furthermore, limb reconstruction with bone allograft is an appropriate solution for a time and has a relatively significant recuperation rate and fewer complications compared with other treatment options. Factors that affect grafted tissue survival include recurrence of disease, infection, fracture, and nonunion, requiring a great effort to prevent these complications.
Table 1.
Rate of complications in the three groups of patients
| Groups | ||||
|---|---|---|---|---|
| Chemotherapy | Chemo-radiotherapy | No adjuvant | Total | |
| Nonunion | 1(0.98%) | 1(0.98%) | 4(3.92%) | 6(5.88%) |
| Infection | 2(1.96%) | 0 | 6(5.88%) | 8(7.84%) |
| Fracture | 2(1.96%) | 2(1.96%) | 2(1.96%) | 6(5.88%) |
| Local recurrence | 3(2.94%) | 0 | 3(2.94%) | 6(5.88%) |
| Metastases | 5(4.90%) | 2(1.96%) | 4(3.92%) | 11(10.78%) |
| Limited knee joint range of motion | 22 (21.56%) | 11(10.78%) | 15 (14.70%) | 48 (47.05%) |
References
- 1.Jamshidi KH, Jabal Ameli M, Ameri Mahabadi E. The results of limb-salvage procedures for high grade osteosarcoma of the limbs. Razi J Med Sci. 2004;10(38):835–43. [Google Scholar]
- 2.Anract P, Coste J, Vastel L, Jeanrot C, Mascard E, Tomeno B. Proximal femoral reconstruction with megaprosthesis versus allograft prosthesis composite. A comparative study of functional results, complications and longevity in 41 cases. Rev Chir Orthop Reparatrice Appar Mot. 2000;86(3):278–88. [PubMed] [Google Scholar]
- 3.Bullens PH, Minderhoud NM, de Waal Malefijt MC, Veth RP, Buma P, Schreuder HW. Survival of massive allografts in segmental oncological bone defect reconstructions. Int Orthop. 2009;33(3):757–60. doi: 10.1007/s00264-008-0700-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuominen T, Jämsä T, Tuukkanen J, Nieminen P, Lindholm TC, Lindholm TS, et al. Native bovine bone morphogenetic protein improves the potential of biocoral to heal segmental canine ulnar defects. Int Orthop. 2000;24(5):289–94. doi: 10.1007/s002640000164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mankin HJ, Doppelt S, Tomford W. Clinical experience with allograft implantation. The first ten years. Clin Orthop Relat Res. 1983;174:69–86. [PubMed] [Google Scholar]
- 6.Dick HM, Malinin TI, Mnaymneh WA. Massive allograft implantation following radical resection of high-grade tumors requiring adjuvant chemotherapy treatment. Clin Orthop Relat Res. 1985;197:88–95. [PubMed] [Google Scholar]
- 7.Glasser DB, Lane JM. Stage IIB osteogenic sarcoma. Clin Orthop Relat Res. 1991;270:29–39. [PubMed] [Google Scholar]
- 8.Deijkers RL, Bloem RM, Petit PL, Brand R, Vehmeyer SB, Veen MR. Contamination of bone allografts: analysis of incidence and predisposing factors. J Bone Joint Surg Br. 1997;79(1):161–6. doi: 10.1302/0301-620x.79b1.7137. [DOI] [PubMed] [Google Scholar]
- 9.Farfalli GL, Aponte-Tinao L, Lopez-Millan L, Ayerza MA, Muscolo DL. Clinical and functional outcomes of tibial intercalary allografts after tumor resection. Orthopedics. 2012;35(3):e391–6. doi: 10.3928/01477447-20120222-25. [DOI] [PubMed] [Google Scholar]
- 10.Jamshidi K, Jabalameli M, Ameri E. The early results of massive osteoarticular allograft in the surgical treatment of lower limb bone tumors. J Kerman Univ Med Sci. 1998;5(3):117–22. [Google Scholar]
- 11.Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW. Long-term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res. 1996;324:86–97. doi: 10.1097/00003086-199603000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Nekouei A, Solouki S. The results of treatment of bone allograft transplantation in the treatment of primary malignant bone tumors in Namazi and Chamran Hospital. Shiraz: Shiraz University of Medical Sciences; 2013. [Google Scholar]
- 13.Donati D, Biscaglia R. The use of antibiotic-impregnated cement in infected reconstructions after resection for bone tumours. J Bone Joint Surg Br. 1998;80(6):1045–50. doi: 10.1302/0301-620x.80b6.8570. [DOI] [PubMed] [Google Scholar]
- 14.Rodl RW, Ozaki T, Hoffmann C, Bottner F, Lindner N, Winkelmann W. Osteoarticular allograft in surgery for high-grade malignant tumours of bone. J Bone Joint Surg Br. 2000;82(7):1006–10. doi: 10.1302/0301-620x.82b7.10644. [DOI] [PubMed] [Google Scholar]
- 15.Donati D, Di Liddo M, Zavatta M, Manfrini M, Bacci G, Picci P, et al. Massive bone allograft reconstruction in high-grade osteosarcoma. Clin Orthop Relat Res. 2000;377:186–94. doi: 10.1097/00003086-200008000-00025. [DOI] [PubMed] [Google Scholar]
- 16.Vander Griend RA. The effect of internal fixation on the healing of large allografts. J Bone Joint Surg Am. 1994;76(5):657–63. doi: 10.2106/00004623-199405000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Masterson EL, Masri BA, Duncan CP, Rosenberg A, Cabanela M, Gross M. The cement mantle in femoral impaction allografting. A comparison of three systems from four centres. J Bone Joint Surg Br. 1997;79(6):908–13. doi: 10.1302/0301-620x.79b6.7690. [DOI] [PubMed] [Google Scholar]
- 18.Friedlaender GE, Tross RB, Doganis AC, Kirkwood JM, Baron R. Effects of chemotherapeutic agents on bone. I. Short-term methotrexate and doxorubicin (adriamycin) treatment in a rat model. J Bone Joint Surg Am. 1984;66(4):602–7. [PubMed] [Google Scholar]
- 19.Kumta SM, Leung PC, Griffith JF, Roebuck DJ, Chow LT, Li CK. A technique for enhancing union of allograft to host bone. J Bone Joint Surg Br. 1998;80(6):994–8. doi: 10.1302/0301-620x.80b6.8982. [DOI] [PubMed] [Google Scholar]


