Abstract
Background:
Variations of the brachial plexus are common and a better awareness of the variations is of crucial importance to achieve successful results in its surgical procedures. The aim of the present study was to evaluate the anatomical variations of the brachial plexus in adult cadavers.
Methods:
Bilateral upper limbs of 32 fresh cadavers (21 males and 11 females) consecutively referred to Guilan legal medicine organization from November 2011 to September 2014, were dissected and the trunks, cords and terminal nerves were evaluated.
Results:
Six plexuses were prefixed in origin. The long thoracic nerve pierced the middle scalene muscle in 6 cases in the supra clavicular zone. The suprascapular nerve in 7 plexuses was formed from posterior division of the superior trunk. Five cadavers showed anastomosis between medial brachial cutaneous nerve and T1 root in the infra clavicular zone. Terminal branches variations were the highest wherein the ulnar nerve received a communicating branch from the lateral cord in 3 cases. The median nerve was formed by 2 lateral roots from lateral cord and 1 medial root from the medial cord in 6 cadavers. Some fibers from C7 root came to the musculocutaneous nerve in 8 cadavers.
Conclusion:
The correlation analysis between the variations and the demographic features was impossible due to the small sample size. The findings of the present study suggest a meta-analysis to assess the whole reported variations to obtain a proper approach for neurosurgeons.
Keywords: Anatomical variations, Brachial plexus, Cords, Peripheral nerves, Trunks
Introduction
A good awareness of human neural system anatomy can be a passport to success in elective neurosurgeries (1). Due to critical conditions of traumatic patients, a speedy surgical promptitude in emergency circumstances requires knowledge of the human neural system anatomy (2).
Variations in human anatomy are one of the most important challenges. The extremities, particularly upper limbs, are susceptible to traumas, but unfortunately, the anatomical variations of brachial plexus are not rare (3-4). More than 50% of anatomical variations in cadaveric studies of human neural system have been reported to belong to the brachial plexus (5-7). The plexus supplies both motor and sensory innervations to the upper limb as well as the extrinsic thoracic muscles (8).
Normal anatomy of the Brachial Plexus
The brachial plexus is constituted by the ventral rami of spinal cervical nerves including C5-C8 and the first thoracic spinal nerve (9). A complex of nerves originating from the neck and axilla shapes the brachial plexus. The brachial plexus extends laterally towards the cervico-axillary canal located below the clavicle, but above the first rib and then enters the axilla through this passage. The brachial plexus provides a network of terminal nerves innervating the upper limb (9-10).
Three trunks lie in human brachial plexus, stemming from the spinal roots of C5-T1. The ventral rami of C5 and C6 are joined to make the superior trunk. C7 root continues and becomes the middle trunk, and the inferior trunk is shaped by the union of C8 and T1 roots (11).
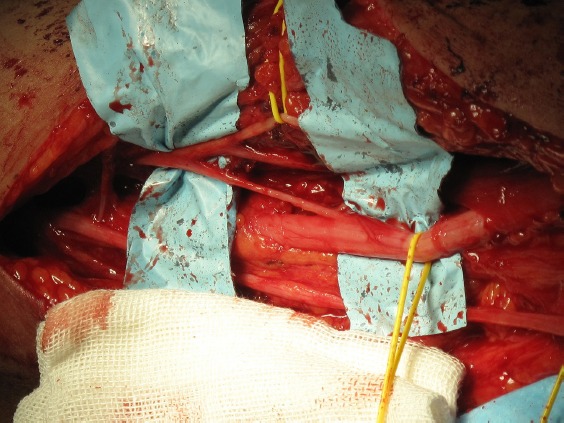
These three trunks bifurcate into anterior and posterior divisions enumerating the origin of the cords. The posterior cord is formed by the fusion of the posterior divisions of all the trunks. However, the anterior divisions of the superior and middle trunks unite to shape lateral cord. The anterior division of the inferior trunk continues to form the medial cord and the peripheral nerves emanate from these cords (10-12) [Figure 1].
Figure 1.
Normal Brachial Plexus pattern.
Effective local anesthesia and successful surgical interventions in the axillary region and the arm depend on a comprehensive appreciation of the plexus anatomy. The aim of the present study was to evaluate the anatomical variations of the brachial plexus in Iranian cadavers. More precisely, we determined the length of the plexus compartments including the cord branches and peripheral nerves in the origin and described the variations of brachial plexus in the origin and respective branches.
Materials and Methods
The Study Protocol
An observational design was selected to explore human cadavers (age of death between 18 to 75 years), consecutively referred to Guilan legal medicine organization for dissection between November 2011 to September 2014. A total of 32 adult cadavers were included in the ongoing research and 64 bilateral upper extremities were finally assessed. All the cadavers were fresh and non formalinated and the maximum duration between the death and dissection times was 12 hours. Impairments and surgical interventions of the brachial plexus before death were the exclusion criteria. All these cadavers were Iranian and born in Guilan province. The dissection procedures were performed by the senior author of this article (an expert neurosurgeon) and the study protocol approved by the ethics committee of Guilan University of Medical Sciences. Informed consents were obtained from all the legal representatives of the cadavers.
The Dissection Protocol
Initially an incision was made in the lateral section of sternocleidomastoid muscle and continued to above the clavicle to mid-clavicle (supra clavicular zone), where the origins of the long thoracic and suprascapular nerves were assessed.
The incision was thereafter exerted toward the delto-pectoral groove going on to the insertion point of pectoralis major muscle (infra clavicular zone), where the origins of subscapular, thoracodorsal, medial pectoral, lateral pectoral, medial brachial cutaneous and medial antebrachial cutaneous nerves were investigated. The incision ultimately opens the area between the biceps and triceps muscles vertically (terminal branches of the brachial plexus). Here, the axillary, radial, ulnar, musculocutaneous and median nerves were perceived as terminal branches of the brachial plexus and assessed for origination. Furthermore, the length of the nerves (measured from the nerve origin towards the target muscle) and variations of the trunks, divisions and cords were scrutinized.
Statistical Analysis
Data analysis were carried out using SPSS software (Version 21.0). The data were shown as N (%) and mean ± SD and 95% confidence interval (CI 95%) was reported.
Results
A total of 32 adult cadavers (64 upper extremities including; 21 males and 11 females; mean age of death: 48.75±13.31; mean height: 174.5±7.4) were included in the present study.
The variations of the brachial plexus origin
56 (87.5%) plexus showed usual origin, 6 plexuses (9.4%; 5 males and 1 female) were pre-fixed (fourth cervical root contributed to the origin) and 2 plexus in a young male cadaver (3.1%) was post-fix (second thoracic spinal root contributed to the origin).
In addition, we reassessed the data wherein the cases were divided into the following groups:
1) Supra clavicular zone: The long thoracic nerve pierced the middle scalene muscle in 6 cases (12 plexus). The variation of suprascapular nerve encompassed the nerve formation from posterior division of the superior trunk in 7 plexuses [Table 1].
Table 1.
Brachial Plexus in Supra Clavicular Zone
| Mean of Length (cm) | 95% Confidence Interval | Variations | |||||
|---|---|---|---|---|---|---|---|
| Male (n=42) | Female (n=22) | Total Cadavers (n=32)* | |||||
| Right (n=21) | Left (n=21) | Right (n=11) | Left (n=11) | ||||
| Long thoracic | 21.94 ± 11.68 | 22.75-18.86 | 5 | 5 | 1 | 1 | 6 (18.75 %) |
| suprascapular | 11.58 ± 3.57 | 10.4438-12.7312 | 2 | 3 | 1 | 1 | 4 (12.5 %) |
Some cases suffered from the variation in their both upper extremities
2) Infra clavicular Zone: In the majority of the cadavers, the medial brachial cutaneous nerve was separated from the medial cord in a single large branch, while 5 cadavers exhibited the anastomosis between the mentioned nerve and the T1 spinal root. The medial cord gave origin to the medial antebrachial cutaneous nerve in 37 plexuses (57.81%), however, the others was originated from inferior trunk, in all male cadavers. The subscapular nerve was directly formed by C5 spinal root in 6 brachial plexuses. The subscapular nerve commonly originated from posterior cord divisions. There was a variation in the origin of the upper subscapular nerve, originating from superior trunk. The medial pectoral nerve unnaturally sprouted from the anterior division of the medial trunk in 2 plexuses. No variations were seen in the lateral pectoral nerve. The results of dissection demonstrated that thoracodorsal nerve was variable in a 60 old woman in origin in both arms, emanating from the axillary nerve. In other cases, the thoracodorsal nerve normally originated from posterior cord divisions as total spinal roots from C5 to T1 partook to form the nerve [Table 2].
Table 2.
Brachial Plexus in Infra Clavicular Zone
| Mean of Length (cm) | 95% Confidence Interval | Variations | |||||
|---|---|---|---|---|---|---|---|
| Male (n=42) | Female (n=22) | Total Cadavers (n=32)* | |||||
| Right (n=21) | Left (n=21) | Right (n=11) | Left (n=11) | ||||
| Medial brachial cutaneous | 6.6 ± 1.21 | 6.3- 6.9 | 4 | 4 | 1 | 1 | 5 (15.62 %) |
| Medial antebrachial cutaneous | 9.9 ± 1.41 | 9.2-10.6 | 14 | 13 | 3 | 3 | 17 (53.12 %) |
| Subscapular | 8.83 ± 7.05 | 9.6500- 9.1806 | 2 | 2 | 1 | 1 | 3 (18.75%) |
| Thoracodorsal | 6.63 ± 1.29 | 6.2222- 7.0528 | --- | --- | 1 | 1 | 1 (3.12%) |
| Medial pectoral | 8.04 ± 1.51 | 7.5577- 8.5273 | 1 | 1 | --- | --- | 1 (3.12%) |
| Lateral pectoral | 7.04 ± 1.60 | 6.5304- 7.75546 | --- | --- | --- | --- | --- |
Some cases suffered from the variation in their both upper extremities
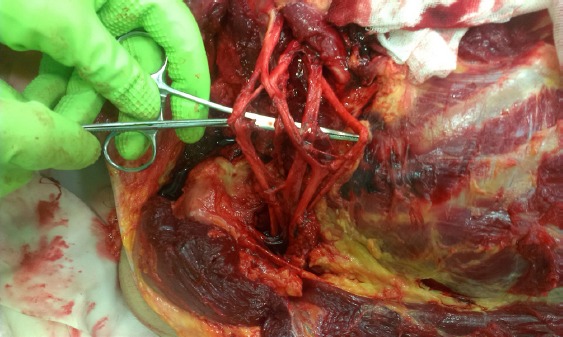
3) The Terminal Branches of Brachial Plexus: The ulnar nerve typically originates from C8 and T1 roots. Variations on the ulnar nerve were present in 3 cadavers (one male and two females). In these cases, the ulnar nerve received a communicating branch from the lateral cord. Variation on the median nerve was observed in 22 plexuses. The median nerve was formed by two lateral roots from the lateral cord and one medial root from the medial cord in 6 cadavers. In the other 5 cases, either the musculocutaneous nerve gave a communicating branch to median nerve or the median nerve took one branch from the posterior cord of the plexus [Figure 2].
Figure 2.
Unusual connection between musculocutaneous nerve and median nerve in arm.
The lateral roots of the lateral cord were classically joined to give origin to a musculocutaneous nerve. Some fibers from C7 root entered this nerve in 5 males and 3 females. We found that the radial nerve in 96.8% of cases was formed by the posterior cord (C5-T1 roots), whereas salient joined divisions of the middle and inferior trunks (C7-T1 roots) were directly projected to make the radial nerve in the reminder bilateral brachial plexus of one male cadaver. According to classical description of brachial plexus, the axillary nerve originates from posterior cord conventionally. This occurred in 54 plexuses (84.3%). The axillary nerve originated from the posterior divisions of middle trunks in 4 cases (2 males and 2 females) as well as the posterior division of mere superior trunk in one arm in a female cadaver [Table 3].
Table 3.
The terminal branches of Brachial Plexus
| Mean of Length (cm) | 95% Confidence Interval | Variations | |||||
|---|---|---|---|---|---|---|---|
| Male (n=42) | Female (n=22) | Total Cadavers (n=32)* | |||||
| Right (n=21) | Left (n=21) | Right (n=11) | Left (n=11) | ||||
| Axillary | 3.9 ± 0.5 | 3.7-4.1 | 2 | 2 | 3 | 2 | 5 (15.62 %) |
| Radial | 7.6 ± 1.3 | 7.2-8.12 | 1 | 1 | --- | --- | 1 (3.12 %) |
| Ulnar | 56.3 ± 2.7 | 55.5-57.2 | 1 | 1 | 2 | 2 | 3 (9.37 %) |
| musculocutaneous | 12.6 ± 2.2 | 12.1-13.1 | 5 | 4 | 2 | 3 | 8 (25 %) |
| Median | 58.5 ± 7.4 | 57.0-60.0 | 8 | 8 | 3 | 3 | 11 (34.37 %) |
Some cases suffered from the variation in their both upper extremities
Discussion
The anatomical variations of the brachial plexus in human infant and adult cadavers are well documented. Kerr et al (13) listed 29 forms of the brachial plexus among 175 cadaver specimens dissected between 1895 and 1910. Elsewhere, 38 variants of this plexus were observed at the several levels of the network such as trunks, cords and terminal nerves, routing mechanism and branching pattern of the nerve fibers (14). Moreover, projection of contributing branches from the fourth cervical (C4) or the second thoracic (T2) spinal root to brachial plexus was seen (13-16).
Anatomical abnormalities might affect the conduction of the various brachial plexus blockades that have been extensively utilized as a component of anesthesia for upper extremity surgeries at the last century (16). Moreover, some variations, surprisingly, cause the damage of the plexus following radical neck dissection and other surgical operations of the axilla and upper arm (17).
Furthermore, anomalies of brachial plexus could face surgeons to failure during procedures and surgical management of brachial plexus tumors or trauma (18-19).
Nowadays, the anesthetic implications such as blockage in different levels of the brachial plexus (interscalene, infra clavicular, supra clavicular and axillary) are used in different surgeries (such as the shoulder, elbow, arm, forearm or hand) or post-operative analgesia (such as shoulder arthroplasty). A better understanding of the brachial plexus variations may lead to a facilitated nerve blockage. Inasmuch as the nerve palsy syndrome can arise from a neuroanatomical variation and it’s relation with a respective muscle, descriptions of nerve variations are beneficial in clinical practice and diagnosis.
Our findings in the present study are summarized in table 4 Our data of most of neuroanatomical variations of the brachial plexus were consistent with those reported previously (13-16, 20-21). Albeit, the percentages in the present study differ from those of the preceding researches which may be due to a difference in the sample size. As we mentioned above, most of the frequencies of the variations in different parts of the brachial plexus belonged to the terminal branches. This needs to be considered by neurosurgeons or hand surgeons.
Table 4.
All of the findings in the present study
| Anomaly | Number of cases | Number of plexuses |
|---|---|---|
| C4 spinal root contributed to origin of the brachial plexus (pre-fix) | 3 | 6 |
| T2 spinal root contributed to origin of the brachial plexus (post-fix) | 1 | 2 |
| The long thoracic nerve pierced the middle scalene muscle | 6 | 12 |
| Suprascapular nerve encompassed the nerve formation from posterior division of the superior trunk | 4 | 7 |
| A anastomosis between the medial brachial cutaneous nerve and T1 spinal root | 5 | 10 |
| The inferior trunk gave origin to the medial antebrachial cutaneous nerve | 17 | 33 |
| The subscapular nerve was directly formed by C5 spinal root | 3 | 6 |
| The medial pectoral nerve sprouted from anterior division of medial trunk | 1 | 2 |
| Thoracodorsal nerve originated from the axillary nerve | 1 | 2 |
| The ulnar nerve received a communicating branch from lateral cord | 3 | 6 |
| The median nerve was formed by two lateral roots from lateral cord and one medial root from the medial cord | 6 | 12 |
| the musculocutaneous nerve gave communicating branch to median nerve or median nerve took one branch from the posterior cord of the plexus | 5 | 10 |
| C7 root enters to musculocutaneous nerve | 8 | 14 |
| C7-T1 roots were directly projected to make radial nerve | 1 | 2 |
| The axillary nerve originated from the posterior divisions of middle trunks | 4 | 8 |
| The axillary nerve originated from the posterior divisions of superior trunks | 1 | 1 |
Consistent with the findings of Fazan et al (22), our results indicated that the musculocutaneous nerve received a communicating branch from C7. Furthermore, in line with the results of Kirazliet al (23) and El Falougy et al (24), we found that appearance of communicating branches between the median and the musculocutaneous nerves was partly common. The presence of communicating branches can be of importance in the evaluation of unexplained sensory loss after trauma or surgical intervention in a particular region. The absence of the musculocutaneous nerve has been previously reported (25-26); however, such variation was not seen in any of our cases.
Sargon et al (27) reported the formation of the median nerve by three roots in that one of the lateral cord roots was located with a very close course over the axillary artery. This variation was present in 18.75% of the cadavers in the present study. It should be noted that this type of variation is attend to injury in surgical operations of the axilla and may lessen the blood supply of the upper extremity by compressing the vessel due to the very close course of the second lateral root of the median nerve to the axillary artery.
Surprisingly, the origin of the upper subscapular nerve from the superior trunk and the origin of the thoracodorsal nerve from the axillary nerve were found in the present study. To the best of our knowledge, this has not been previously reported.
This cadaveric study improves the knowledge of variations in anatomy of brachial plexus that is of great importance to anatomists, radiologists, anesthesiologists and surgeons. Further, the existence of anatomic variations of the peripheral nervous system explains unexpected clinical signs and symptoms.
A limitation of the present study was the small sample size due to the difficulty of obtaining informed constant from the legal representatives for achieving fresh cadavers for dissection and thus the correlation analysis between the variations and the demographic features of the cadavers was impossible. To produce more reliable results and make a proper approach for neurosurgeons a meta-analysis of the brachial plexus variations is recommended.
Acknowledgements
We express our gratitude to deputy of Research and Technology of Guilan University of Medical Sciences for their insightful guidance. Also, we are thankful to Dr. Zahra Haghparast Ghadim Limudahi for her critical revision of the manuscript and suggestions.
Footnotes
Author contribution: Mohammadreza Emamhadi, Shahrokh Yousefzadeh Chabok, Fariborz Samini; Data collection: Zoheir Reihanian; Draft: Babak alijani; Analysis: Hamid Behzadnia, Fariborz Ayati Firozabadi.
All authors declare that they have no conflict of interest.
This study was supported by the brachial plexus and peripheral nerve injury center.
References
- 1.Butz JJ, Shiwlochan DG, Brown KC, Prasad AM, Murlimanju BV, Viswanath S. Bilateral variations of brachial plexus involving the median nerve and lateral cord: an anatomical case study with clinical implications. Australas Med J. 2014;7(5):227–31. doi: 10.4066/AMJ.2014.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parchand MP, Patil ST. Absence of musculocutaneous nerve with variations in course and distribution of the median nerve. Anat Sci Int. 2013;88(1):58–60. doi: 10.1007/s12565-011-0126-6. [DOI] [PubMed] [Google Scholar]
- 3.Aydin ME, Kale A, Edizer M, Kopuz C, Demir MT, Corumlu U. Absence of the musculocutaneous nerve together with unusual innervation of the median nerve. Folia Morphol (Warsz) 2006;65(3):228–31. [PubMed] [Google Scholar]
- 4.Soleymanha M, Mobayen M, Asadi K, Adeli A, Haghparast-Ghadim-Limudahi Z. Survey of 2582 cases of acute orthopedic trauma. Trauma Mon. 2014;19(4):e16215. doi: 10.5812/traumamon.16215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaudhary P, Singla R, Arora K, Kalsey G. Formation and branching pattern of cords of brachial plexus-a cadaveric study in north Indian population. Int J Ana Res. 2014;2(1):225–33. [Google Scholar]
- 6.Budhiraja V, Rastogi R, Asthana AK. Variations in the formation of the median nerve and its clinical correlation. Folia Morphol (Warsz) 2012;71(1):28–30. [PubMed] [Google Scholar]
- 7.Uysal II, Seker M, Karabulut AK, Buyukmumcu M, Ziylan T. Brachial plexus variations in human fetuses. Neurosurgery. 2003;53(3):676–84. doi: 10.1227/01.neu.0000079485.24016.70. [DOI] [PubMed] [Google Scholar]
- 8.Agur AM, Dalley AF. Grant’s atlas of anatomy. 13th ed. Philadelphia: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 9.Peter L. Gray’s Anatomy. 40th ed. Great Britain: Churchill Livingstone; 2008. Williams; pp. 1266–74. [Google Scholar]
- 10.Orebaugh SL, Williams BA. Brachial plexus anatomy: normal and variant. Sci World J. 2009;9:300–12. doi: 10.1100/tsw.2009.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Snell RS. Clinical anatomy. 7th ed. Philadelphia: Lippincott Williams and Wilkins; 2004. p. 477. [Google Scholar]
- 12.Hollinshead W. Anatomy for Surgeons. New York: Hoeber-Harper; 1958. General survey of the upper limb-the back and limbs; pp. 225–8. [Google Scholar]
- 13.Kerr AT. The brachial plexus of nerves in man the variations its formation and branches. Am J Ana. 1918;23(2):285–395. [Google Scholar]
- 14.Aggarwal A, Puri N, Aggarwal AK, Harjeet K, Sahni D. Anatomical variation in formation of brachial plexus and its branching. Surg Radiol Anat. 2010;32(9):891–4. doi: 10.1007/s00276-010-0683-8. [DOI] [PubMed] [Google Scholar]
- 15.Lee HY, Chung IH, Sir WS, Kang HS, Lee HS, Ko JS, et al. Variations of the ventral rami of the brachial plexus. J Korean Med Sci. 1992;7(1):19–24. doi: 10.3346/jkms.1992.7.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aktan ZA, Öztürk L, Bilge O, Özer MA, Pinar YA. A cadaveric study of the anatomic variations of the brachial plexus nerves in the axillar region and arm. Turk J Med Sci. 2001;31(2):147–50. [Google Scholar]
- 17.Fazan VP, Amadeu AD, Caleffi AL, Rodrigues Filho OA. Brachial plexus variations in its formation and main branches. Acta Cir Bras. 2003;18(5):14–8. [Google Scholar]
- 18.Uzel AP, Bulla A, Steinmann G, LaurentJoye M, Caix P. Absence of the musculocutaneous nerve and its distribution from median nerve: about two cases and literature review. Morphology. 2011;95(311):146–50. doi: 10.1016/j.morpho.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Bala A, Sinha P, Tamang BK, Sarda RK. Anatomical variation: median nerve formation - a case vignette. J Clin Diagn Res. 2014;8(6):AD03–4. doi: 10.7860/JCDR/2014/7620.4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Radunovic M, Vukasanovic-Bozaric A, Radojevic N, Vukadinovic T. A new anatomical variation of the musculocutaneous and the median nerve anastomosis. Folia Morphol (Warsz) 2013;72(2):176–9. doi: 10.5603/fm.2013.0030. [DOI] [PubMed] [Google Scholar]
- 21.Rastogi R, Budhiraja V, Bansal K. Posterior cord of brachial plexus and its branches: anatomical variations and clinical implication. ISRN Anat. 2013;2013:1–3. doi: 10.5402/2013/501813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fazan VP, Amadeu AD, Caleffi AL, Filho OA. Brachial plexus variations in its formation and main branches. Acta Cir Bras. 2003;18(5):14–8. [Google Scholar]
- 23.Kirazlı Ö, Tatarlı N, Ceylan D, Hacıoğlu H, Uygun S, Şeker A, et al. A variation of the cords of the brachial plexus on the right and a communication between the musculocutaneous and median nerves on the left upper limb: a unique case. J Neurol Surg A Cent Eur Neurosurg. 2013;74(Suppl 1):e176–9. doi: 10.1055/s-0032-1333416. [DOI] [PubMed] [Google Scholar]
- 24.El Falougy H, Selmeciova P, Kubikova E, Stenova J, Haviarova Z. The variable communicating branches between musculocutaneous and median nerves: a morphological study with clinical implications. Bratisl Lek Listy. 2013;114(5):290–4. doi: 10.4149/bll_2013_061. [DOI] [PubMed] [Google Scholar]
- 25.Hoogbergen MM, Kauer JM. An unusual ulnar nerve-median nerve communicating branch. J Anat. 1992;181(Pt 3):513–6. [PMC free article] [PubMed] [Google Scholar]
- 26.Nakatani T, Tanaka S, Mizukami S. Two rare anomalies of the brachial plexus. J Anat. 1998;192(Pt 2):303–4. doi: 10.1046/j.1469-7580.1998.19220303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sargon MF, Uslu SS, Celik HH, Akşit D. A variation of the median nerve at the level of brachial plexus. Bull Assoc Anat (Nancy) 1995;79(246):25–6. [PubMed] [Google Scholar]


