Abstract
Abscess formation following intramuscular injections is rare and they are most commonly seen in immunocompromised individuals. In this case series we present a cohort of three patients presented to us in a critically ill condition with an abscess due to intramuscular injection. Vancomycin resistant staphylococcus aureus was isolated from all three patients. These patients posed a major challenge to the healthcare system and the treating physician because of the: severity of illness, virulence and resistance of the organism, rarity of the situation, immune state of the patient, and lack of supporting evidence to properly guide management in the use of health resources. To the best of our knowledge, there is no report available in the English literature on vancomycin resistant staphylococcus aureus associated with intramuscular injection abscess.
Keywords: Immunocompromised patients, Intramuscular injection, VRSA
Introduction
Intramuscular (IM) injections are a minor outpatient procedure in any healthcare institution worldwide. The IM route is a valuable mode of medication administration, utilized when requiring a relatively quick uptake of medication with a reasonably prolonged action. Even though the procedure appears to be minor, rarely it can result in major complications like abscesses, bacteremia and generalized sepsis that can lead to multi-organ failure (1). Injection abscess following IM injection has been reported by various authors. Most cases are due to Staphylococcus aureus either as methicillin sensitive S. aureus (MSSA) or methicillin-resistant Staphylococcus aureus (MRSA) (2). In this case series we report three cases of IM injection abscess due to vancomycin resistant Staphylococcus aureus (VRSA) and reviewed the literature with respect to presentation, management, and prognosis of VRSA associated injection abscess.
Case Report
Case 1
A 67-year-old male, with a known case of poorly controlled diabetes and hypertension on irregular treatment was referred to our hospital with complaints of difficulty in breathing, altered sensorium, and right gluteal swelling. On admission he was in acute on chronic renal failure with metabolic acidosis, hyperkalemia, cerebral vascular accident with right lacunar infarct on ventilator support, and altered sensorium. He gave a history of an intramuscular injection of NSAID taken on his right gluteal region a few days back from a nearby clinic. On examination there was a swelling of the right gluteal region associated with tense compartment. His laboratory values showed a total count of 29600/cubic mm and CRP values of 233.7 mg/L. His initial MRI pelvis showed pyomyositis of the gluteus maximus without any localized collection. His initial blood culture and sensitivity revealed growth of VRSA. Considering the MRI and clinical finding and laboratory values we planned for no surgical management with antibiotics and supportive management. He was stabilized with ventilatory support and dialysis. In spite of aggressive supportive care he failed to show clinical improvement and the repeat MRI after 48 hours showed a collection in his muscle pockets. Ultrasound guided aspiration was done that revealed frank pus; hence, we proceeded with wound debridement and drainage of pus in the right gluteal region. Considering the severity of the infection and muscle involvement, the wound was left open. Subsequently he underwent multiple surgical debridements under anesthesia and placed on wound VAC dressing. He also had gangrene of the distal phalanx of the 4th finger of the left hand for which amputation of the distal phalanx done. The patient showed signs of improvement with the use of linezolid injections that were started according to culture and sensitivity reports. After 60 days of hospitalization, multiple debridement, and VAC therapy the patient improved clinically and was discharged. At the time of discharge his wound was clean and granulated, CRP was near normal, WBC count was normal, renal function was stabilized, his finger wound healed, he was ambulating with a walker, and was on normal oral diet [Figure 1, 2, 3, 4].
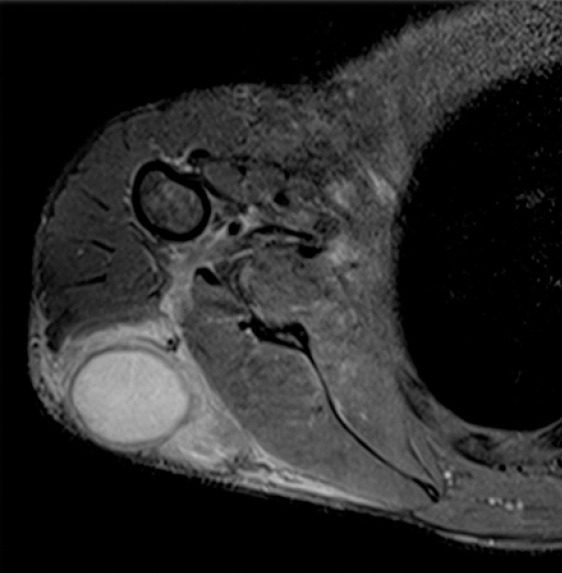
Figure 1.
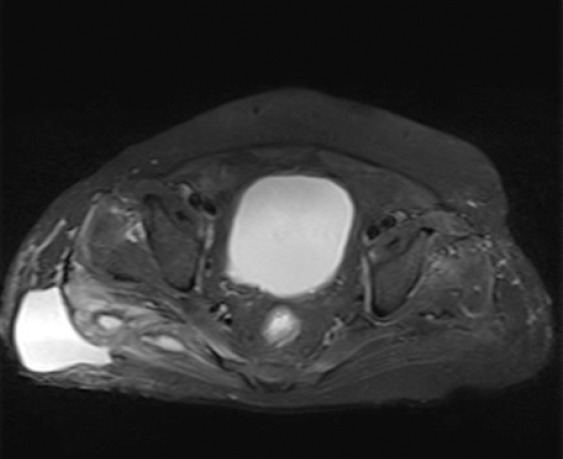
Case 1 gluteal abscess - pre operative MRI- axial view.
Figure 2.
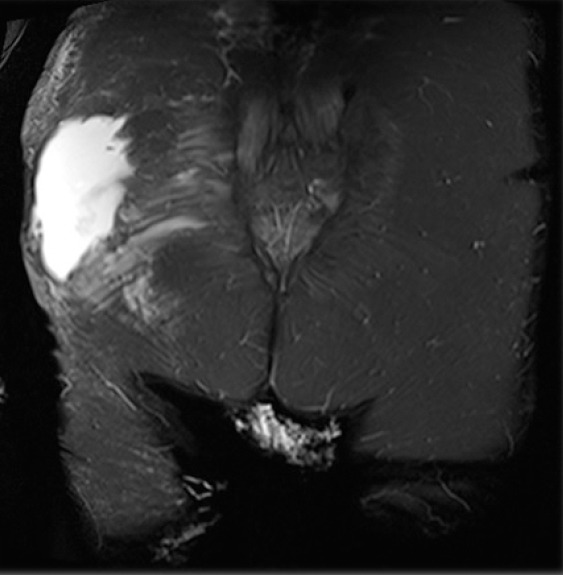
Case 1 gluteal abscess - pre operative MRI- coronal view.
Figure 3.
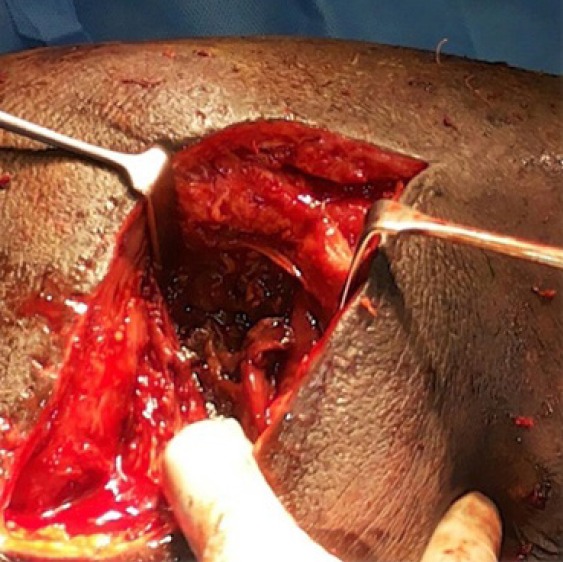
Case 1 gluteal abscess - intraoperative appearance of deep muscle.
Figure 4.
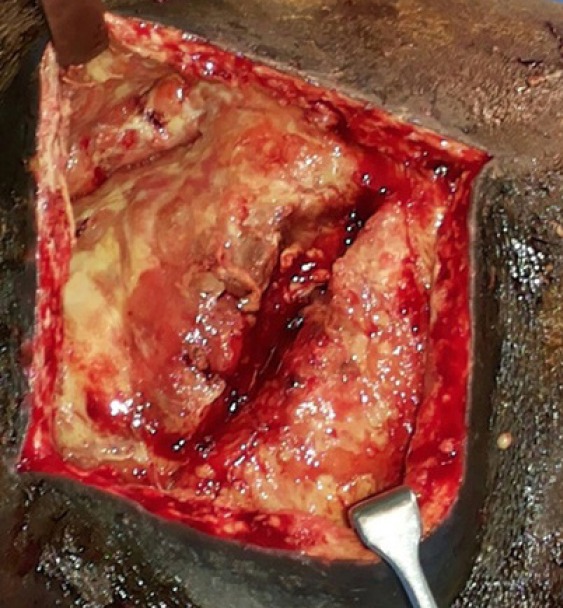
Case 1 gluteal abscess - intraoperative appearance of superficial muscle.
Case 2
A 69-year-old male, with a known case of diabetes mellitus, hypertension, coronary artery disease, and dyslipidemia on regular medication was admitted with complaints of left hip pain that radiated to the entire left lower limb since 1.5 months ago. Pain was acute at onset and gradually progressive. There was no weakness or numbness of the lower limbs. He attributed the entire event after an intramuscular injection given to the left gluteal region. On examination he had antalgic gait and tenderness over the left greater trochanter and along the anterior aspect of his left thigh. His range of movements were: 1) flexion: 120 degree, 2) abduction: 20 degree, and 3) internal and external rotation: 30 degree. There was no calf muscle tenderness and no neurovascular deficits. His laboratory values showed a total count of 15700/cubic mm and CRP values of 81.9 mg/L. MRI showed a collection in the gluteal region and around the postero-lateral corner of the greater trochanter extending into the proximal thigh. Diagnostic aspiration revealed frank pus and initial pus culture, and sensitivity revealed growth of VRSA. Under general anesthesia, the gluteal regions and upper thigh were exposed by two separate incisions and pus was drained and thorough debridement of the necrosed deep fascia, tensor fascia lata, and vastus lateralis was carried out. Tissues and pus were sent for microbiological and histopathological analysis. The wound was kept open and dressing daily. After repeated dressing, the wound granulated and secondary closure of the wound was done. After 20 days of hospitalization and intravenous antibiotics he improved clinically and was discharged. At the time of discharge his wound was clean and dry, CRP was near normal, WBC count was normal, the patient was ambulating with a walker, and was on a normal oral diet.
Case 3
This 40-year-old male patient is a known case of chronic kidney disease and hypertension and he was on regular haemodialysis awaiting renal transplant. He was admitted with complaints of acute pain in the right shoulder of three-days duration associated with swelling and he also had difficulty in using his right shoulder since then. Pain was sudden at onset, continuous, and moderate to severe in intensity and it was aggravated on activity. In addition, he had severe night and rest pain. He also gave a history of intramuscular injection of Iron in the right deltoid region 2 weeks previously, which was administered in a local clinic. On examination there was a globular swelling in the lateral aspect of the right arm extending up to the scapular region. There was a local rise of temperature and tenderness over the swelling, painful restriction of the right shoulder movements, but no neurovascular deficits. The MRI scan of the right shoulder showed pyomyositis of the posterior belly of the right deltoid muscle with central abscess formation (dimension: 5 cm x 1.2 cm x 1.2 cm) with extensive fascial, subcutaneous and muscular inflammation with no evidence of extension to the shoulder joint cavity. His initial aspiration revealed frank pus with the growth of VRSA on the culture and sensitivity, and he was started on linezolid injections (600 mg) twice daily as per the report. Under anesthesia an incision was made over the most fluctuant point and frank pus was drained. Exploration of the posterior belly of the deltoid muscle was done meticulously and 40 ml of pus was drained. Tissues and the drained pus were sent for microbiological and histo-pathological analysis. The wound was left open and packed with saline gauze and pad, and protected using iodine-impregnated incision drape (LOBAN) dressing. Subsequently the wound healed well and secondary closure was done. At the time of discharge his wound was clean and dry, CRP was near normal, and WBC count was normal [Figure 5, 6; Table 1].
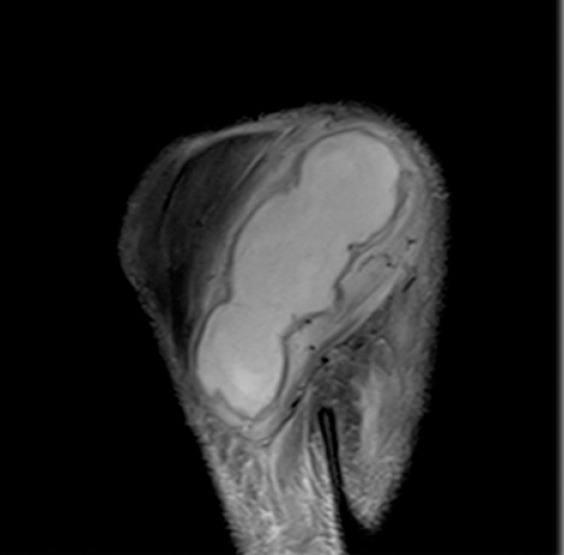
Figure 5.
Case 3 deltoid abscess - pre operative MRI- axial view.
Figure 6.
Case 3 deltoid abscess - pre operative MRI- coronal view.
Table 1.
Summary of Patient S Details
| Case No. | Age | Immune status | Initial CRP | Time taken for CRP to normalize | Treatment | Outcome |
|---|---|---|---|---|---|---|
| 1 | 67 | Diabetic | 233.7 | 60 days | IV antibiotics x 6weeks and then orally, Debridement | good |
| 2 | 69 | Diabetic | 86.5 | 20 | IV antibiotics x 3 weeks and then orally, Debridement | good |
| 3 | 40 | Anemia with CKD | 134.3 | 42 | IV antibiotics x 6weeks and then orally, Debridement | good |
Discussion
Intramuscular injections can lead to local infectious complications, such as abscesses, skin necrosis, or intra-articular infections. It can rarely progress to generalized sepsis and multi-organ failure (1). All three of our patients were immunocompromised, two of them had uncontrolled diabetes and the third patient had chronic renal failure. The first patient was in sepsis and multi organ failure that took nearly 30 days of intensive care treatment and multiple surgical debridements to normalize his clinical condition. The second case was in sepsis and multisystem complications were prevented by appropriate empirical treatment (linezolid), early surgical intervention and multidisciplinary management. The third case came to us in the early stages of bacteremia, so with appropriate management we were able to prevent sepsis. Such serious infections are more likely to occur in immuno-compromised patients, but have also been described in immune-competent persons. A study from Iraq revealed 60% of gluteal abscesses following IM injections were associated with co-morbidities like diabetes mellitus, anemia, jaundice, malignancy, and chronic steroid (3).
According to the Boston collaborative drug surveillance program in 1978, 46% of the hospitalized patients received at least one IM injection during their stay and among them only 0.4% (48 of 12134 patients) developed one of the following complications: abscess, indurations, hematoma and bleeding. The most common complication among them was abscess formation. The bacteriological cultures revealed that 66% of cases were monomicrobial, 9% poly microbial, and among them 33% were S. aureus (4). Staphylococcus aureus is one of the most common causes of pyogenic skin and soft tissue infections (1, 5). According to our study, all three organisms were VRSA It was in 1996 that the first clinical isolation of S. aureus with reduced susceptibility to vancomycin was reported in Japan and one year later the first documented case of infection by VRSA in a patient from United States (6, 7). Vancomycin resistant Staphylococcus aureus is an emerging threat that was isolated in the late nineties due to pre-existing MRSA infections, irrational use of glycopeptides antibiotics, uncontrolled use in agriculture, animal husbandry and fisheries and delays in removing the hemodialysis catheter (8, 9, 10, 11). We could not find any literature with VRSA as the causative organism for intramuscular injection abscess.
In our patients we liberally used CRP for monitoring responses to treatment and to ascertain the prognosis of our cases. A study from Belgium showed that CRP levels are a good early marker of morbidity and mortality in critically ill patients (12). In our experience CRP values in association with total white cell count and ESR were very useful in diagnosis, prognosis, and treatment of these cases. The initial CRP value correlates with the severity of the infection, the duration of IV antibiotics, and the hospital stay.
In our study all of them had a similar pattern in culture and sensitivity studies, which showed sensitivity to linezolid. Linezolid was effective and well tolerated in patients with vancomycin resistant S. aureus infection (13, 14).
In our experience all the three patients improved clinically with linezolid. After the second patient we added linezolid injection as a part of our hospital antibiotic protocol as an empirical treatment for abscesses especially in immunocompromised patients. Hence, we could prevent the third patient from going to sepsis and avoided longer hospitalization. All our patients underwent repeated radical surgical debridement until we had clinical improvement. We also believe that a tissue diagnosis before starting an empirical antibiotic is extremely important to achieve a better outcome. Vacuum assisted closure is a very effective mode of treatment for large defects after a thorough wound debridement. The VAC therapy works on the basic principles of removal of fluid and mechanical deformation (15).
According to a study by Rossi and Conen in 1995 they reported six cases of S. aureus sepsis following intramuscular injections that required surgical debridement and antibiotic treatment (16).
Another recent case report in 2009 also showed the importance of prompt surgical management and intravenous antibiotics in managing sepsis following intramuscular abscesses (1). We also had a similar experience with all our three cases. In our opinion, once we have an accessible site of abscess it is better to drain it as soon as possible. However, if the site is deep with no sizeable collection and cannot be accessed easily, we may consider appropriate empirical antibiotics for 48-72 hours, and if there is no clinical improvement and CRP continues to raise we would proceed with radical debridement along with intravenous antibiotics.
Although the procedure appears minor, IM injections need proper assessment of the patient, asepsis, and appropriate techniques to prevent the rare but dangerous complications. The Center for disease Control issued clinical guidelines in 2010 showing the importance of hand washing in the prevention of VRSA infections among clinicians and healthcare providers. Early initiation of appropriate antibiotics and prompt surgical intervention is required for better outcomes in these cases. Linezolid appears to be effective in this condition especially in immunocompromised individuals. Furthermore, the CRP value is an important tool in prognosis, treatment, and follow- up of these cases. These kinds of cases require admission in a multispecialty center and need multidisciplinary approach from various specialists for satisfactory outcome.
References
- 1.Velissaris D, Matzaroglou C, Kalogeropoulou C, Karamouzos V, Filos K, Karanikolas M. Sepsis requiring intensive care following intramuscular injections: two case reports. Cases J. 2009;2(1):7365–70. doi: 10.4076/1757-1626-2-7365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666–74. doi: 10.1056/NEJMoa055356. [DOI] [PubMed] [Google Scholar]
- 3.Abdulla Hawramy T, Saeed KA, Salih Ahmed BH. Gluteal abscess, different intramuscular drug injections as causative agents. 3rd International Conference of Medical Sciences; Dubai: 2012. [Google Scholar]
- 4.Greenblatt DJ, Allen MD. Intramuscular injection-site complications. JAMA. 1978;240(6):542–4. [PubMed] [Google Scholar]
- 5.Hare R, Thomas CG. The transmission of Staphylococcus aureus. Br Med J. 1956;2(4997):840–4. doi: 10.1136/bmj.2.4997.840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Srinivasan A, Dick JD, Perl TM. Vancomycin resistance in staphylococci. Clin Microbiol Rev. 2002;15(3):430–8. doi: 10.1128/CMR.15.3.430-438.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hiramatsu K, Hanaki H, Ino T, Yabuta K, Oguri T, Tenover FC. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J Antimicrob Chemother. 1997;40(1):135–6. doi: 10.1093/jac/40.1.135. [DOI] [PubMed] [Google Scholar]
- 8.Smith TL, Pearson ML, Wilcox KR, Cruz C, Lancaster MV, Robinson-Dunn B, et al. Emergence of vancomycin resistance in Staphylococcus aureus. Glycopeptide-Intermediate Staphylococcus aureus Working Group. N Engl J Med. 1999;340(7):493–501. doi: 10.1056/NEJM199902183400701. [DOI] [PubMed] [Google Scholar]
- 9.Tenover FC, Lancaster MV, Hill BC, Steward CD, Stocker SA, Hancock GA, et al. Characterization of Staphylococci with reduced susceptibility to vancomycin and other glycopeptides. J Clin Microbiol. 1998;36(4):1020–7. doi: 10.1128/jcm.36.4.1020-1027.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tiwari HK, Sen MR. Emergence of vancomycin resistant Staphylococcus aureus (VRSA) from a tertiary care hospital in northern parts of India. BMC Infect Dis. 2006;6:156–62. doi: 10.1186/1471-2334-6-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D’Agata EM. Antimicrobial-resistant, Gram-positive bacteria among patients undergoing chronic hemodialysis. Clin Infect Dis. 2002;35(10):1212–8. doi: 10.1086/344282. [DOI] [PubMed] [Google Scholar]
- 12.Lobo SM, Lobo FR, Bota DP, Lopes-Ferreira F, Soliman HM, Mélot C, et al. C-reactive protein levels correlate with mortality and organ failure in critically ill patients. Chest. 2003;123(6):2043–9. doi: 10.1378/chest.123.6.2043. [DOI] [PubMed] [Google Scholar]
- 13.Moise PA, Forrest A, Birmingham MC, Schentag JJ. The efficacy and safety of linezolid as treatment for Staphylococcus aureus infections in compassionate use patients who are intolerant of, or who have failed to respond to, vancomycin. J Antimicrob Chemotherapy. 2002;50(6):1017–26. doi: 10.1093/jac/dkf215. [DOI] [PubMed] [Google Scholar]
- 14.Woodford N, Livermore DM. Infections caused by Gram-positive bacteria: a review of the global challenge. J Infect. 2009;59(Suppl 1):S4–16. doi: 10.1016/S0163-4453(09)60003-7. [DOI] [PubMed] [Google Scholar]
- 15.Morykwas MJ, Simpson J, Punger K, Argenta A, Kremers L, Argenta J. Vacuum-assisted closure: state of basic research and physiologic foundation. Plast Reconstr Surg. 2006;117(7 Suppl):121S–6. doi: 10.1097/01.prs.0000225450.12593.12. [DOI] [PubMed] [Google Scholar]
- 16.Rossi L, Conen D. Intramuscular injections--an outdated form of administration? 6 cases of Staphylococcus aureus sepsis following intramuscular injections. Schweiz Med Wochenschr. 1995;125(31-32):1477–82. [PubMed] [Google Scholar]


